Abstract
Background
A comprehensive evaluation and remediation program is an essential component of any residency program. The evaluation system should identify problems accurately and early and allow residents with problems to be assigned to a remediation program that effectively deals with them. Elements of a proactive remediation program include a process for outlining deficiencies, providing resources for improvement, communicating clear goals for acceptable performance, and reevaluating performance against these goals.
Intervention
In recognition of the importance of early detection and prompt remediation of the struggling resident, we sought to develop a multifaceted approach to resident evaluation with the aim of early identification and prompt remediation of difficulties. This article describes our comprehensive evaluation program and remediation program, which uses resources within our radiology department and institutional graduate medical education office.
Discussion
An effective evaluation system should identify problems accurately and early, whereas a proactive remediation program should effectively deal with issues once they are identified.
Introduction
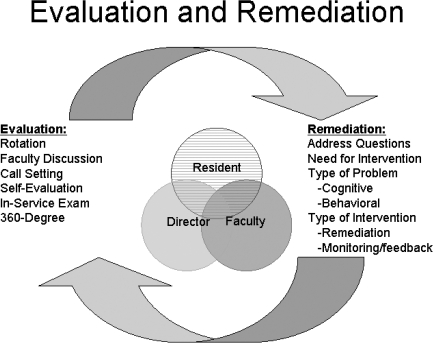
A comprehensive evaluation and remediation program is an essential component of any residency program (figure). An effective evaluation system should identify problems accurately and early, whereas a proactive remediation program should effectively deal with issues once they are identified by outlining deficiencies, providing resources for improvement, and communicating clear goals for acceptable performance.
Figure.
Evaluation and Remediation
Diagram shows the relationship between evaluation and remediation. Reprinted with permission from Boiselle.2
In recognition of the importance of early detection and prompt remediation of residents who struggle with academic performance, we sought to develop a multifaceted approach to resident evaluation with the aim of early identification and prompt remediation of difficulties. This article describes our comprehensive evaluation program and remediation program, which uses resources within our radiology department and institutional graduate medical education (GME) office.
Evaluation
Similar to other specialties, the monthly rotation evaluation is the basis of our resident assessment program in radiology. An online evaluation form1 commenting on the 6 Accreditation Council for Graduate Medical Education competencies is completed by the educational liaison of each section following discussion with the other section members to provide a complete overview of the resident's performance. In addition to the rotation evaluations, our evaluation system involves input from several complementary sources, including:
“Roundtable” faculty discussions to help identify “subthreshold” but potentially important resident performance issues that may “escape” detection on written evaluations2
Call setting evaluations to assess the ability of residents to perform independently and to identify signs of stress and fatigue
American Board of Radiology in-service written examination scores to assess general fund-of-knowledge
Departmental emergency radiology examination to assess preparedness for independent radiology call3,4
Biannual resident self-assessment evaluations to help identify learner-centered areas of need
360-degree evaluation to enhance assessment of professionalism and interpersonal/communication skills
In their article “Failure to Fail: The Perspectives of Clinical Supervisors,” Dudek et al5 discussed the reluctance of staff physicians to fail poorly performing trainees. They found that the reason for “grade inflation” was not due to the inability of evaluators to recognize deficiencies or to complete evaluations but rather was related to their unwillingness to give poor evaluations. Poor documentation of deficiencies and perceived negative consequences to faculty and to the resident were given as reasons why physician educators are reluctant to give poor but honest evaluations.
To counteract such tendencies, we schedule quarterly roundtable faculty discussions that provide the faculty an opportunity to collectively discuss resident performance. In our experience, this forum has brought to the forefront several resident issues that were not reported on written evaluations because the faculty members initially thought that the observed performance or behavior was simply due to “sampling error” or was “within the edge of a bell-shaped curve.” Upon discussion with other faculty members, however, it was often demonstrated that such concerns were more generalized. This forum has thus helped bring resident difficulties to the attention of the program directors at an earlier stage, when such problems are potentially more responsive to remediation.
Remediation
Once performance issues have been identified, an open discussion with the resident in a comfortable environment is vital. During this initial conversation, it is important to present the factual information from the evaluations without being judgmental, accusatory, or demeaning. In addition to communicating this information, one must also be a good listener. It is especially important to ask whether there are any contributing personal issues, such as increased family demands or medical illness.
When confronted with a resident performance issue, it is important to perform a fair and comprehensive assessment in a timely manner, addressing several essential and interrelated questions:
Is the perceived performance issue primarily related to a knowledge deficit, an attitude or behavioral problem, a skill deficit, or a combination of these factors?
What is the resident's perception of the issue?
What is the faculty's perception of the issue?
Are there other contributing personal issues such as depression, anxiety, or personal or family illness?
Are there larger educational or system problems in the residency program that may contribute to this problem?
What is the potential impact of the problem regarding patient care?
What is the potential impact of the problem regarding resident's personal health and professional growth?
What is the potential impact of the problem regarding its impact upon other residents and faculty?
It is important to perform this analysis in a fair, comprehensive, and timely manner. Based upon this analysis, a decision should be made as to whether an intervention is necessary. If an intervention is deemed appropriate, a remediation plan should be put into place with all due deliberate speed. To establish the optimal remediation plan, it is necessary to categorize the problem as either primarily cognitive (related primarily to one's knowledge base and cognitive skills) or primarily behavioral (related primarily to difficulties with professionalism and interpersonal communication) in nature. Although cognitive problems are typically amenable to traditional instructional methods, behavioral issues are more likely to respond to other methods, such as close monitoring/feedback of attitudinal and interpersonal behaviors for “mild” problems and referral to a psychologist or psychiatrist for residents with serious psychological symptoms.
Although each resident problem is unique, we sought to develop a framework for intervention that could be applied consistently among residents with various performance issues. Our remediation program uses resources from both our radiology department and our institutional GME office similar to other programs and specialties.6–9 The centerpiece is a resident/program director/faculty educational liaison agreement form that documents the problem and its significance and outlines a detailed remediation plan that contains clear goals and benchmarks, as well as a plan for reassessment to determine whether the remediation program has been successful. This intervention was designed in accordance with the principles outlined by Borus.10
A discernible strength of this framework is that it sets up an alliance between 3 parties: (1) the resident, (2) the program director, and (3) the faculty educational liaison with experience in the specific area of difficulty. With all 3 parties invested in the agreement, the “intervention” feels like a concerted team effort rather than a punitive situation and frames the intervention itself in positive rather than oppositional terms. A proactive remediation plan may include additional reading assignments, one-on-one faculty/mentor tutorials, specific assistance with reporting or procedural skills, and repeating a clinical rotation after completion of such measures.
Additionally, it is important to involve the GME office of the institution early on in the remediation process.6 Assistance in drafting various written agreements and documentation of poor performance or unprofessionalism can usually be provided by the GME office.6 Advice from the institutional legal counsel is also useful, especially in cases in which a trainee may potentially be terminated from the training program.6,11 Additional resources include occupational health and confidential physician health services to help with psychiatric issues and substance abuse problems. Involving the GME office also helps with due process in the event that a resident feels that he or she is wrongly accused and wishes an external review.
Our remediation program is widely accepted and has been approved by our departmental educational committee. Both faculty and residents alike expressed approval at having a system in place for addressing serious performance issues in a consistent and even-handed manner. Importantly, the detailed written agreement form also documents these issues, which is a critical part of due process procedures at any academic institution.
Moreover, it is important to understand the emotional toll that often occurs during this process to both the struggling resident and the physician educator. For example, the resident may experience initial feelings of denial, anger, and disappointment, which can lead to feelings of embarrassment, anxiety, and loss of self-confidence. For the staff physician, anxiety about being overcritical needs to be tempered with the satisfaction of providing honest constructive feedback. Both parties need to have a clear understanding and acceptance of the process and should be supported throughout the remediation program.
Sample Case Scenarios
We provide 2 fictional examples that illustrate the types of resident difficulties that we have addressed with our remediation program.
Case 1
Fictional resident Steven has an appropriate fund of knowledge and clinical skills for his level of training. However, he was frequently late for work, took personal cell phone calls during read-out sessions, and often left work for the incoming resident who was relieving him on the overnight call shift. His reports were adequate; however, they were rarely signed in a timely manner. Steven clearly has behavioral performance issues as opposed to cognitive ones. In his case, additional reading assignments or repeating rotations will not address the problems. During a candid discussion of these behaviors with Steven, it became clear that he had poor insight into his lack of professionalism. He was not aware of the negative impact and significance of his behaviors on faculty and fellow residents. After a review of our program's specific expectations for professionalism, a remediation program was devised that included an assignment to a faculty mentor and close monitoring and feedback of various aspects of professionalism, with specific goals for attendance, punctuality, and overall work ethic. Following successful completion of the remediation program, Steven is now consistently more professional in his behavior and reports that he feels “more like a real doctor” compared with before the intervention.
Case 2
In contrast, fictional resident Jenny is diligent and routinely arrives to work early and stays late. Yet, she struggles on her clinical rotations, lagging behind her peers in her fund of knowledge and her ability to synthesize clinical and radiographic data. Although still in the early stages of residency training, she was already involved in several research projects. Upon discussion with Jenny, it was learned that she lacked basic time management skills and that she was having difficulty juggling her clinical training with her research interests. A remediation program was devised that included time management training, maintaining a weekly logbook documenting her studying habits, and a hiatus from her research projects until she met the goals set for self-study and improved clinical performance. Upon completion of the remediation program, Jenny's clinical performance is now “on target” and she reports a greater sense of well-being compared with before the intervention. She plans to wait until she has dedicated elective time to return to her research projects.
Summary
In summary, a comprehensive resident evaluation and remediation program is an essential component of any residency program. Having an evaluation program with a multifaceted approach has the potential to detect problems early, when they are potentially more responsive to remediation. Moreover, a proactive remediation program that effectively identifies performance issues and incorporates departmental and institutional resources is necessary to effectively deal with issues once they are recognized.
Although remediation successfully addresses most resident performance issues, it is important to realize that there are some instances in which residents are unable to meet the professional expectations of their specialty despite our best efforts. For such residents, prompt referral for supportive psychological and career counseling is essential for helping them to find an alternative career path that is better suited to their strengths. Such referral ensures that we as physician educators meet our professional responsibilities to both our physician trainees and our patients.
Footnotes
All authors are at Beth Israel Deaconess Medical Center and Harvard Medical School. Jim S. Wu, MD, is Program Director of the Radiology Residency Program; Bettina Siewert, MD, is former Program Director of the Radiology Residency Program; and Phillip M. Boiselle, MD, is former Associate Program Director of the Radiology Residency Program.
Editor's Note: The online version (33KB, doc) of this article includes the sample questions for the multiple choice test and the faculty scoring sheet for the OSCE for the cardiac exam station.
References
- 1.Collins J., Hyde C., Gray L., et al. Radiology resident evaluation: a form that addresses the six competencies of the accreditation council for graduate medical education. Acad Radiol. 2002;9(7):815–816. doi: 10.1016/s1076-6332(03)80354-9. [DOI] [PubMed] [Google Scholar]
- 2.Boiselle P. M. A remedy for resident evaluation and remediation. Acad Radiol. 2005;12(7):894–900. doi: 10.1016/j.acra.2005.03.056. [DOI] [PubMed] [Google Scholar]
- 3.Ganguli S., Pedrosa I., Yam C. S., Appignani B., Siewert B., Kressel H. Y. Part I: preparing first-year radiology residents and assessing their readiness for on-call responsibilities. Acad Radiol. 2006;13(6):764–769. doi: 10.1016/j.acra.2006.02.057. [DOI] [PubMed] [Google Scholar]
- 4.Ganguli S., Camacho M., Yam C. S., Pedrosa I. Preparing first-year radiology residents and assessing their readiness for on-call responsibilities: results over 5 years. AJR Am J Roentgenol. 2009;192(2):539–544. doi: 10.2214/AJR.08.1631. [DOI] [PubMed] [Google Scholar]
- 5.Dudek N. L., Marks M. B., Regehr G. Failure to fail: the perspectives of clinical supervisors. Acad Med. 2005;80(10):S84–S87. doi: 10.1097/00001888-200510001-00023. [DOI] [PubMed] [Google Scholar]
- 6.Ratan R. B., Pica A. G., Berkowitz R. L. A model for instituting a comprehensive program of remediation for at-risk residents. Obstet Gynecol. 2008;112(5):1155–1159. doi: 10.1097/AOG.0b013e31818a6d61. [DOI] [PubMed] [Google Scholar]
- 7.Hauer K. E., Ciccone A., Henzel T. R., et al. Remediation of the deficiencies of physicians across the continuum from medical school to practice: a thematic review of the literature. Acad Med. 2009;84(12):1822–1832. doi: 10.1097/ACM.0b013e3181bf3170. [DOI] [PubMed] [Google Scholar]
- 8.Saxena V., O'Sullivan P. S., Teherani A., Irby D. M., Hauer K. E. Remediation techniques for student performance problems after a comprehensive clinical skills assessment. Acad Med. 2009;84(5):669–676. doi: 10.1097/ACM.0b013e31819fa832. [DOI] [PubMed] [Google Scholar]
- 9.Torbeck L., Canal D. F. Remediation practices for surgery residents. Am J Surg. 2009;197(3):397–402. doi: 10.1016/j.amjsurg.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Borus J. F. Recognizing and managing residents' problems and problem residents. Acad Radiol. 1997;4(7):527–533. doi: 10.1016/s1076-6332(97)80241-3. [DOI] [PubMed] [Google Scholar]
- 11.Irby D. M., Milam S. The legal context for evaluating and dismissing medical students and residents. Acad Med. 1989;64(11):639–643. doi: 10.1097/00001888-198911000-00001. [DOI] [PubMed] [Google Scholar]