Abstract
Background
Physicians report they feel ill-prepared to manage chronic noncancer pain (CNCP), in part because of inadequate training. Published studies and clinical observation demonstrate that trainees lack confidence and reflect negative attitudes about CNCP. Overall, there is minimal published guidance on specific specialty roles and responsibilities in CNCP management.
Objective
The purpose of this study was to assess resident preparation, confidence, and attitudes about CNCP across graduate medical education programs and to assess resident perception of roles and responsibilities in CNCP management.
Methods
In 2006 we surveyed residents from 13 graduate medical education programs in 3 institutions about CNCP and report quantitative and qualitative analyses of survey responses from 246 respondents.
Results
A total of 59% of respondents rated their medical school preparation and 36% rated their residency preparation as “fair” or “poor”; only 17% reported being “confident” or “very confident” in assessing patients with CNCP; and 30% used negative or derogatory terms (eg, manipulative, irritable, needy) to describe patients with CNCP. Respondents from postgraduate years 3–6 were more than twice as likely as postgraduate year 1 or postgraduate year 2 respondents (44% versus 21% and 20%, respectively) to use negative or derogatory terms (P = .0007). Respondents were significantly more likely to report that pain specialists are “good” or “excellent” in managing CNCP compared with generalists (73% versus 6%; P < .0001).
Conclusion
Education in pain management should begin in medical school and continue through graduate medical education, regardless of specialty. Early and sustained training interventions are needed to foster empathy in caring for patients with pain. Residency and fellowhip training should impart a clear understanding of each specialty's role and responsibilities in pain management to better foster patient-centered pain care.
Introduction
Physicians are ill-prepared to assess and treat chronic noncancer pain (CNCP), in part because of inadequate preparation during medical school and residency.1–3 Prior surveys have shown that residents are aware of gaps in their training in this area, with most residents rating their preparation to manage CNCP as “fair” or “poor.”4,5 Pain management is not a required clinical topic in undergraduate medical education, although the Liaison Council of Medical Education recommends that “clinical instruction must cover all organ systems, and include the important aspects of preventive, acute, chronic, continuing, rehabilitative, and end-of-life care.”6 Didactic education in pain management is not included in the Accreditation Council for Graduate Medical Education (ACGME) “Common Program Requirements,” nor is it consistently required in the specialty-specific program requirements.7
Lack of confidence in treating CNCP has been well described among physicians in practice and individuals in training.1,4,5,8,9 Reasons include lack of preparation, barriers to effective pain management, including federal and state regulatory restrictions, and competing demands at both the institutional and residency program levels.10 Attitudinal barriers to effective pain management have been observed consistently by academic faculty.11 Negative attitudes toward patients with pain are common, illustrated by the title of a recent article, “Is treating chronic pain torture?”5 The ACGME Common Program Requirements for the competencies of professionalism and patient care state, “Residents are expected to demonstrate compassion, integrity, and respect for others…” and that “Residents must be able to provide patient care that is compassionate, appropriate, and effective for the treatment of health problems and the promotion of health.”7 This makes it important to identify and address negative attitudes toward patients presenting with chronic pain.
Guidelines12–16 for CNCP management have been published, but provider, practice, and specialty variations contribute to fragmented chronic pain care. For example, an orthopedic surgeon may welcome the opportunity to address chronic knee pain by offering a total knee replacement, yet he or she may be reluctant to provide nonsurgical pain management as part of ongoing care; a rheumatologist may welcome the opportunity to treat chronic knee pain in patients with inflammatory arthritis with monoclonal antibody therapy, but he or she may be less willing to provide ongoing pain management for chronic osteoarthritis; a physiatrist may limit his or her practice to interventions for pain and defer ongoing medical management to the generalist. Generalists may be unaware of specialty-specific practice limitations, and as a result patients may “boomerang” among multiple providers. This lack of patient-centered care results in inconsistent management, inefficient health care use, and resultant high costs.17,18
Several surveys on CNCP have assessed generalist (typically internal medicine and family medicine) provider and trainee preparation, confidence, and attitudes about CNCP.3–5,19–23 To date, these surveys have not included trainees in other specialties. This study was designed to provide insight into graduate medical education (GME) trainee preparation, confidence, and attitudes, and to clarify trainee expectations about specialty-specific responsibilities in CNCP. Insight into trainees' preparation, confidence, and attitudes about CNCP is important in order to design effective educational interventions.
Methods
The investigators developed an online GME Chronic Noncancer Pain Survey using Inquisite Software (Inquisite: An Allegiance Company, Austin, TX) to quantitatively and qualitatively assess trainee responses to questions on CNCP prior to a planned curricular intervention. Survey questions were adapted from previously published instruments,2,4,5,19–22 and input into survey design was solicited from faculty at the 3 institutions participating in the survey: Virginia Commonwealth University (VCU), Alpert Medical School of Brown University, and the University of Massachusetts Medical School. The survey was then piloted among program directors at VCU. The final 68-item survey included demographics and questions about preparation, confidence, and attitudes related to the management of CNCP.
In August 2006, a recruitment e-mail was sent to the program directors of 17 different GME programs at 3 institutions. At that time of the survey, these institutions lacked a residency curriculum in CNCP management. Sixteen programs were recruited to participate. One investigator met with each GME program director prior to the initiation of the survey. A total of 430 trainees received an e-mail with a description of the “Chronic Noncancer Pain Study” along with the participation consent form. Three sequential survey follow-up reminders were sent. The survey study was approved by the institutional review boards of all participating institutions.
SAS v.9.2 (SAS Institute, Cary, NC) was used to analyze the quantitative data. We report descriptive statistics; χ2 tests to assess associations between nominal variables of interest; 2-sample t tests and ANOVA tests to compare the mean responses between sexes and between postgraduate years; and paired t tests to assess for differences between pairs of continuous repeated measures. We also used content analysis to evaluate qualitative responses, including faculty review of raw responses, theme/category development, response coding into themes/categories, and discussion to consensus. The analysis of the qualitative information was done by a 5-member team representing the VCU Departments of Social and Behavioral Health, Hematology/Oncology and Palliative Care, and Internal Medicine, with input from coinvestigators in internal medicine and family medicine. Two qualitative questions were analyzed: “Describe characteristics of patients with chronic pain” and “Working with patients with chronic pain is…(complete statement).”
Results
Of the 430 trainees at the 3 institutions invited to participate in the survey, 250 consented to participate. Four surveys were eliminated because registration dates for a planned online curriculum in CNCP24 preceded the survey's completion date. Data were available from 246 trainees for a survey response rate of 57% (246 of 430). The number of responses to individual questions varied. Just more than half (55.7%) of the participants were female. Approximately 33% were in postgraduate year 1 (PGY-1), 25% were in PGY-2, and 42% were in PGY-3 or higher (table 1). The overall sample of respondents included trainees (residents and fellows) from VCU (84.6%) and other institutions (15.4%). The distribution of programs and respondents across the 3 participating institutions is shown in table 2. Respondents were divided into 3 categories: (1) generalists (69.5%), including family medicine, internal medicine, and internal medicine-pediatrics; (2) nonsurgical specialties (21.1%), including neurology, physical medicine and rehabilitation, psychiatry, and fellowships in geriatrics, hematology/oncology, infectious disease, and rheumatology; and (3) surgical specialties (9.3%), including anesthesiology, neurosurgery, and orthopedics. Most respondents (77.2%; 183 of 237) reported seeing between 1 and 10 patients with CNCP per month, whereas fewer (18.6%; 44 of 237) reported seeing more than 10 patients with CNCP per month.
Table 1.
Characteristics of Respondents
Table 2.
Participating Programs and Survey Response Rates
Preparation
Fifty-nine percent (140 of 238) of respondents rated their medical school preparation as “fair” or “poor” (Likert scale of 1 = “poor” to 5 = “excellent”), whereas 36% (84 of 235) rated their residency preparation as “fair” or “poor.” Specialists were more than twice as likely to report “good” or “excellent” medical school preparation than generalists (18% versus 7%; P = .0322).
Confidence
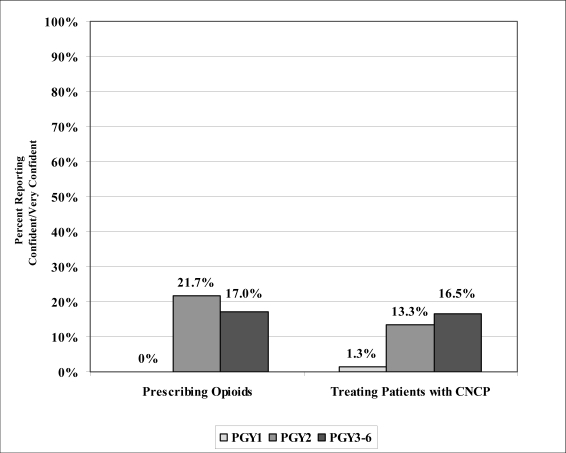
Only 17% (40 of 236) of respondents reported being “confident” or “very confident” (5-point Likert scale, 1 = “not at all confident” to 5 = “very confident”) in assessing patients with CNCP. PGY-1 respondents were less confident than their upper-level counterparts (5.3% for PGY-1 versus 20% for PGY-2 and 24% for PGYs 3–6; P = .0035). Eleven percent (25 of 233) of respondents reported being “confident” or “very confident” in treating patients with CNCP. This percentage increased with year of training (1.3% for PGY-1, 13% for PGY-2, and 17% for PGYs 3–6; P = .0045). Although only 13% (30 of 234) felt “confident” or “very confident” in their ability to prescribe opioids for CNCP, confidence in prescribing opioids increased with year of training between PGY-1 and PGY-2 (0% versus 21.7%; P = .0002; figure 1). Additionally, a higher percentage of nonsurgical respondents (23.4%) reported confidence in prescribing opioids compared with surgical respondents (13.6%) and generalists (9.7%; P = .0459).
Figure 1.
Confidence in Treating and Prescribing Opioids for Patients With Chronic Noncancer Pain by Year of Training
Almost 40% (92 of 231) of respondents “frequently” or “very frequently” (5-point Likert scale, 1 = “very rarely” to 5 = “very frequently”) prescribed short-acting opioids, and a smaller percentage (31%; 73 of 233) “frequently” or “very frequently” prescribed long-acting opioids. There was no difference in self-reported opioid prescribing by specialty. However, respondents who were “confident” or “very confident” in prescribing opioids were more likely to “frequently” or “very frequently” prescribe short-acting (P = .0014) or long-acting (P = .0003) opioids compared with those who were not “confident” or “very confident.”
Attitudes
Approximately 25% (58 of 237) of respondents “agreed” or “strongly agreed” (5-point Likert scale, 1 = “strongly disagree” to 5 = “strongly agree”) that requesting opioids for CNCP is an addictive behavior. A similar percentage (28.7%; 68 of 237) “agreed” or “strongly agreed” that requesting additional or higher-dose pain medication is an addictive behavior. There were no significant differences in response by year or specialty. Thirty-seven percent (88 of 236) of respondents felt at risk for regulatory investigation when prescribing opioids, with no difference found by year, specialty, or confidence in prescribing opioids.
Content analysis of the responses to “Describe characteristics of patients with chronic pain” (table 3) revealed that most respondents (71%; 156 of 220) used psychological terms (eg, depressed), a finding that increased with year of training (PGY-1, 62%; PGY-2, 67%; and PGYs 3–6, 80%; P = .0309). Respondents in nonsurgical specialties (91%) were more likely than surgical respondents (76%) or generalists (65%) to use psychological terms (P = .0035). Thirty percent (66 of 220) of respondents used negative or derogatory terms (eg, needy). PGYs 3–6 (44%) were more than twice as likely as PGY-1 (21%) or PGY-2 (20%) to use negative or derogatory terms (P = .0007; figure 2). Only 3.2% (7 of 220) of respondents used positive terms (eg, coping).
Table 3.
Qualitative Analysis of Responses (n = 220) to Open-Ended Question, “Describe Characteristics of Patients With Chronic Pain”a
Figure 2.
Described Characteristics of Patients by Year
Responses to the statement “Working with patients with chronic pain is….” were categorized by content analysis as neutral (eg, “complex,” “challenging”), positive (eg, “interesting,” “pleasure”), negative (eg, “aggravating,” “dissatisfying”), or conditional (eg, “difficult, however, it can be very rewarding if you can control their pain” or “difficult at best due to drug seekers using the chronic pain excuse”; table 4). Most responses were neutral (63.4%; 144 of 227). Few responses were positive (6.2%; 14 of 227). A third of responses were negative (34.4%; 78 of 227). Some responses were conditional, indicating that if “conditions” would change, the response would be different (11.5%; 26 of 227). The most reported “conditions” were management (46%), misuse (19%), and psychosocial issues (12%).
Table 4.
Qualitative Analysis of Responses (n = 227) to Open-Ended Question, “Working With Patients With Chronic Pain Is…”
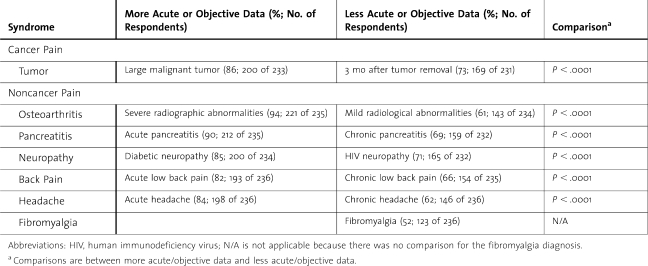
Regardless of year or specialty, 67% (153 of 227) of respondents “frequently” or “very frequently” believe patients when they describe the quality of their CNCP. Fifty-six percent “frequently” or “very frequently” believe patients when they describe the severity of their CNCP. A gradual decrease in percentage from 94% to only 52% “frequently” or “very frequently” believe patients' report of pain as the disease state becomes less acute and/or has less corroborative evidence to support the report of pain (table 5).
Table 5.
Respondents' Belief of Patient's Report of Pain (Percent Reporting “Frequently” or “Very Frequently”)a
Most respondents “agreed” or “strongly agreed” that chronic pain is treatable (84%; 199 of 237) and treatment can lead to improved outcomes (91%; 214 of 236). There was evidence that the percentage of respondents reporting “agree” or “strongly agree” to CNCP being treatable was statistically different across postgraduate years (P = .0123), with the largest increase occurring from PGY-1 (73.7%) to PGY-2 (88.5%).
Roles and Responsibilities
Although nearly 60% (139 of 237) of respondents “agreed” or “strongly agreed” that treating patients with CNCP is an efficient use of their time, surgical respondents (32%) were half as likely to endorse this as generalist (61.7%) or nonsurgical (60.4%) respondents (P = .0270). Without a difference in year or specialty, respondents were significantly more likely to report that pain specialists were “good” or “excellent” in managing CNCP (73%; 172 of 236) than were generalists (6%; 14 of 236; P < .0001). Only 6.3% of nonsurgical respondents and 4.8% of surgical respondents rated generalists as “good” or “excellent” in their ability to manage CNCP.
Discussion
Regardless of specialty, trainees reported inadequate preparation to treat chronic pain. In addition, the higher percentage of generalists' in comparison with specialists' view of medical school preparation as suboptimal may be a perceptive hindsight, given the unique pain management challenges generalists face in academic primary care clinics.
Trainees exhibited low confidence in assessing, treating, and prescribing opioids for patients with CNCP, although confidence increases with year of training. The only specialty difference was a greater confidence among nonsurgical respondents in prescribing opioids for CNCP, and this may be due to inclusion of a greater number of upper levels (PGYs 3–6) in this group. Although there was no significant difference between self-reported prescribing of short-acting versus long-acting opioids, it appears that the more confident the trainee, the more likely he or she is to prescribe opioids for CNCP.
Approximately one fourth of respondents view requesting opioids or requesting more or higher doses of opioids as addictive behaviors. This may be due to a direct association—although often inaccurate—of aberrant medication-taking behaviors (AMTBs) with the disease of addiction. To address this, pain education can highlight the differential diagnosis of AMTBs (inability to adhere to treatment, self-medication, inadequate pain control, criminal intent) in an attempt to elicit thoughtful interpretation of these behaviors.25–27 Educational emphasis in pain management should also focus on medication safety, as evidenced by a recent study on overdose deaths in noncancer pain syndromes treated with opioids28 and supported by the Food and Drug Administration's focus on risk-mitigation strategies,29 as well as a clearer understanding of the role of the Drug Enforcement Administration and state boards of medicine to dissipate fear of regulatory monitoring and investigation that has an impact on opioid prescribing.2,3
Use of psychologic terms to describe patient characteristics increased with year of training. More frequent use of psychologic terms in the nonsurgical respondents may reflect the presence of fellows (upper-level PGYs) and psychiatry residents, or it may indicate an increasing awareness of psychologic comorbidity with chronic pain.30,31 The use of negative or derogatory terms increased with year of training, similar to the findings of other studies.32–34 Other studies also have shown that negative perceptions of CNCP patients can be deleterious to pain care outcomes, because empathy is a component of an effective pain management plan.35,36 That trainees frequently do not believe a patient's report of pain is problematic, because pain is subjective, and chronic pain typically lacks the vital sign alterations and facial expressions that accompany acute pain.37,38 This finding is consistent with vignette studies that have shown that medical students and physicians tend to underestimate a patient's level of pain when objective medical evidence to support the report of pain is absent.39–41
Despite increasingly negative attitudes as year of training increases, trainees view chronic pain as treatable and feel that treatment can lead to improved outcomes. The significant change from PGY-1 to PGY-2 suggests that PGY-1–targeted interventions, including the promotion of professionalism, may have the greatest impact on the learners' confidence and attitudes.33 The finding that “management,” “misuse,” and “psychosocial issues” prompted conditional responses in response to “Working with patients with chronic pain is…” suggests that attitudes may improve if pain management training specifically addresses these areas.
Trainees' responses suggest a mismatch between perception of who is effective and the reality of who should be effective at managing CNCP. Chronic pain management takes a significant amount of time, especially when one attempts to follow recommendations from the Federation of State Medical Boards Model Policy,42 Universal Precautions in Pain Management,26 or other clinical guidelines. These time requirements may make pain management outside of the perioperative and postoperative periods less appealing to surgical specialites. Sure enough, in this survey, surgical respondents were half as likely as generalists and nonsurgical respondents to agree that managing CNCP was an efficient use of their time. Surgical specialists should, however, be comfortable managing acute or subacute pain that becomes chronic or pain that presents to them as nonoperable chronic pain until transfer of care to a primary pain provider has been accomplished. With the time required for visits, the comorbid psychiatric conditions, the need for continuity and monitoring, and the paucity of pain specialists that manage controlled substances, generalists are increasingly taking responsibility for CNCP management.43,44 As education and better training improve generalists' confidence and the ability to manage chronic pain and as the concept of a “medical home” for pain mangement becomes more universally accepted, the gap between expectation and reality should narrow.
Limitations
Although this was designed to be a multi-institutional study, trainees from VCU programs provided most responses (84.6% versus 15.4% non-VCU). Additionally, although 13 GME programs were represented, responses were heavily weighted toward generalists (69.5%). Most respondents (81.4%) saw fewer than 10 patients with CNCP per month, likely reflecting the emphasis on inpatient training.
Small sample sizes may have interfered with the detection of differences among subgroups. These limitations reduce the ability to generalize from this study to other settings. Future multi-institutional, cross-GME studies will be needed to verify our findings.
Conclusions and Implications
Our findings suggest that generalists as well as nongeneralist trainees feel ill-prepared and lack confidence in treating CNCP. Thus, education in pain management should begin in medical school and continue, regardless of specialty through residency and fellowship. A troubling finding is that increasing confidence with years of training was accompanied by erosion of professionalism, as evidenced by upper-level trainees' descriptions of the characteristics of patients with CNCP. Our survey suggests that trainees across GME programs find disease states with acute or demonstratable findings more “believeable” than chronic pain or pain without demonstratable findings. Early and sustained training interventions are needed to foster empathy in caring for patients with pain. Generalist and specialty trainees view pain specialists as being best equipped to manage CNCP but are less clear about their own responsibilities toward CNCP patients. Clearer definition of roles and responsibilities early in training would benefit the care of this population by contributing to a “medical home” for patients with CNCP and improved patient-centered pain management.
Every provider encounters patients with pain, thus making the topic of pain management as important to medical training as cultural competency and ethics. The Joint Commission requires hospitals to train staff in pain management, without singling out a particular discipline or specialty.45 Similarly, the Liaison Council of Medical Education and ACGME should enact GME-wide accreditation requirements in pain management. Content for chronic pain management can be used to teach chronic disease management, as well as specialty roles and responsibilities when cross-specialty management is needed. This survey was part of a larger study to determine outcomes from an online pain management curriculum (www.paineducation.vcu.edu) for GME trainees.24 To conserve resources, this or a similar program can be incorporated into medical student and residency training to impart medical knowledge about pain, address professionalism, and delineate specialty roles and responsiblities. Trainees need a clear message about shared responsibility in managing pain before training is complete and they enter the health care workforce. This would be the first step in breaking down barriers and creating an interconnected environment of patient-centered pain care.
Footnotes
Leanne M. Yanni, MD, is an Associate Professor in the Department of Internal Medicine, Virginia Commonwealth University Medical Center; Jessica L. McKinney-Ketchum, PhD, is an Assistant Professor in the Department of Biostatistics, Virginia Commonwealth University; Sarah B. Harrington, MD, is an Assistant Professor in the Department of Hematology/Oncology and Palliative Care, University of Arkansas School of Medicine; Christine Huynh, MD, is Assistant Professor in the Department of Internal Medicine, Virginia Commonwealth University Medical Center; Saad Amin, BS, is at the Virginia Commonwealth University School of Medicine; Robin Matsuyama, PhD, is Assistant Professor in the Department of Social and Behavioral Health Virginia Commonwealth University; Patrick Coyne, MSN, APRN, FAAN, is Clinical Director of the Thomas Palliative Care Program Virginia Commonwealth University/Massey Cancer Center; Betty Anne Johnson, MD, PhD, is Professor in the Department of Internal Medicine, Virginia Commonwealth University Medical Center; Mark Fagan, MD, is Professor in the Department of Internal Medicine, Alpert Medical School of Brown University; Linda Garufi-Clark, MD, is Assistant Professor in the Department of Family Medicine and Community Health, University of Massachusetts Medical School.
The authors wish to thank the program directors for their support of this project and the residents for their time and thoughts on this topic.
Editor's Note: For more information regarding the chronic noncancer pain treatment curriculum, visit http://www.paineducation.vcu.edu/curriculum/index.html.
References
- 1.Weinstein S. M., Laux L. F., Thornby J. I., et al. Physicians' attitudes toward pain and the use of opioid analgesics: results of a survey from the Texas cancer pain initiative. South Med J. 2000;93(5):479–487. [PubMed] [Google Scholar]
- 2.Upshur C. C., Luckmann R. S., Savageau J. A. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med. 2006;21(6):652–655. doi: 10.1111/j.1525-1497.2006.00412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wolfert M. Z., Gilson A. M., Dahl J. L., Cleary J. F. Opioid analgesics for pain control: Wisconsin physicians' knowledge, beliefs, attitudes, and prescribing practices. Pain Med. 2009;11(3):425–434. doi: 10.1111/j.1526-4637.2009.00761.x. [DOI] [PubMed] [Google Scholar]
- 4.Yanni L. M., Weaver M. F., Johnson B. A., Morgan L. A., Harrington S. E., Ketchum J. M. Management of chronic nonmalignant pain: a needs assessment in an internal medicine resident continuity clinic. J Opioid Manag. 2008;18(4):201–211. doi: 10.5055/jom.2008.0026. [DOI] [PubMed] [Google Scholar]
- 5.Chen J. T., Fagan M. J., Diaz J. A., Reinert S. E. Is treating chronic pain torture?: internal medicine residents' experience with patients with chronic nonmalignant pain. Teach Learn Med. 2007;19(2):101–105. doi: 10.1080/10401330701332144. [DOI] [PubMed] [Google Scholar]
- 6.Liaison Committee on Medical Education (LCME) LCME accreditation standards 2008. Available at: http://www.lcme.org/standard.htm. Accessed December 3, 2009.
- 7.The Accreditation Council for Graduate Medical Education (ACGME) ACGME homepage. Available at: http://www.acgme.org/acWebsite/home/home.asp. Accessed December 3, 2009.
- 8.Weinstein S. M., Laux L. F., Thornby J. I., et al. Medical students' attitudes toward pain and the use of opioid analgesics: implications for changing medical school curriculum. South Med J. 2000;93(5):472–478. [PubMed] [Google Scholar]
- 9.O'Rorke J. E., Chen I., Genao I., Panda M., Cykert S. Physicians' comfort in caring for patients with chronic nonmalignant pain. Am J Med Sci. 2007;333(2):93–100. doi: 10.1097/00000441-200702000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Niv D., Devor M. European Federation of IASP Chapters. Position paper of the European Federation of IASP Chapters (EFIC) on the subject of pain management. Eur J Pain. 2007;11(5):487–489. doi: 10.1016/j.ejpain.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Ogle K. S., McElroy L., Mavis B. No relief in sight: postgraduate training in pain management. Am J Hosp Palliat Care. 2008;25(4):292–297. doi: 10.1177/1049909108315915. [DOI] [PubMed] [Google Scholar]
- 12.Chou R., Fanciullo G. J., Fine P. G., et al. Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113–130. doi: 10.1016/j.jpain.2008.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.American Geriatrics Society Panel on the Pharmacological Management of Persistent Pain in Older Persons. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331–1346. doi: 10.1111/j.1532-5415.2009.02376.x. [DOI] [PubMed] [Google Scholar]
- 14.Trescot A. M., Helm S., Hansen H., et al. Opioids in the management of chronic non-cancer pain: an update of American Society of the Interventional Pain Physicians' (ASIPP) guidelines. Pain Physician. 2008;11(suppl):S5–S62. [PubMed] [Google Scholar]
- 15.Trescot A. M., Boswell M. V., Atluri S. L., et al. Opioid guidelines in the management of chronic non-cancer pain. Pain Physician. 2006;9(1):1–39. [PubMed] [Google Scholar]
- 16.Chou R., Qaseem A., Snow V., et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 17.Lynch M. E., Campbell F., Clark A. J., et al. A systematic review of the effect of waiting for treatment for chronic pain. Pain. 2008;136(1–2):97–116. doi: 10.1016/j.pain.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 18.Wilsey B. L., Fishman S. M., Crandall M., Casamalhuapa C., Bertakis K. D. A qualitative study of the barriers to chronic pain management in the ED. Am J Emerg Med. 2008;26(3):255–263. doi: 10.1016/j.ajem.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 19.Wilson J. F., Brockopp G. W., Kryst S., Steger H., Witt W. O. Medical students' attitudes toward pain before and after a brief course on pain. Pain. 1992;50(3):251–256. doi: 10.1016/0304-3959(92)90028-A. [DOI] [PubMed] [Google Scholar]
- 20.Green C. R., Wheeler J. R., Marchant B., LaPorte F., Guerrero E. Analysis of the physician variable in pain management. Pain Med. 2001;2(4):317–327. doi: 10.1046/j.1526-4637.2001.01045.x. [DOI] [PubMed] [Google Scholar]
- 21.Potter M., Schafer S., Gonzalez-Mendez E., et al. Opioids for chronic nonmalignant pain. attitudes and practices of primary care physicians in the UCSF/Stanford collaborative research network: University of California, San Francisco. J Fam Pract. 2001;50:145–151. [PubMed] [Google Scholar]
- 22.Chen I., Goodman B., Galicia-Castillo M., Quidgley-Nevares A., Krebs M., Gliva-McConvey G. The EVMS pain education initiative: a multifaceted approach to resident education. J Pain. 2007;8(2):152–160. doi: 10.1016/j.jpain.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 23.The National Center on Addiction and Substance Abuse at Columbia University. Missed opportunity: national survey of primary care physicians and patients on substance abuse. Available at: http://www.casacolumbia.org. Accessed April 28, 2010.
- 24.Yanni L. M., Priestley J. W., Schlesinger J. B., Ketchum J. M., Johnson B. A., Harrington S. E. Development of a comprehensive E-learning resource in pain management. Pain Med. 2008;10(1):95–105. doi: 10.1111/j.1526-4637.2008.00511.x. [DOI] [PubMed] [Google Scholar]
- 25.Gourlay D. L., Heit H. A., Almahrezi A. Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med. 2005;6(2):107–112. doi: 10.1111/j.1526-4637.2005.05031.x. [DOI] [PubMed] [Google Scholar]
- 26.Savage S. R., Joranson D. E., Covington E. C., Schnoll S. H., Heit H. A., Gilson A. M. Definitions related to the medical use of opioids: evolution towards universal agreement. J Pain Symptom Manage. 2003;26(1):655–667. doi: 10.1016/s0885-3924(03)00219-7. [DOI] [PubMed] [Google Scholar]
- 27.Savage S. R. Assessment for addiction in pain-treatment settings. Clin J Pain. 2002;18(suppl):S28–S38. doi: 10.1097/00002508-200207001-00004. [DOI] [PubMed] [Google Scholar]
- 28.Dunn K. M., Saunders K. W., Rutter C. M., et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med. 2010;152(2):85–92. doi: 10.1059/0003-4819-152-2-201001190-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fishman S. M. Responsible Opioid Prescribing. Washington, DC: Waterford Life Sciences; 2007. [Google Scholar]
- 30.Bair M. J., Wu J., Damush T. M., Sutherland J. M., Kroenke K. Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med. 2008;70(8):890–897. doi: 10.1097/PSY.0b013e318185c510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tunks E. R., Crook J., Weir R. Epidemiology of chronic pain with psychological comorbidity: prevalence, risk, course, and prognosis. Can J Psychiatry. 2008;53(4):224–234. doi: 10.1177/070674370805300403. [DOI] [PubMed] [Google Scholar]
- 32.Hojat M., Vergare M. J., Maxwell K., et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 33.Crandall S. J., Marion G. S. Commentary: identifying attitudes towards empathy: an essential feature of professionalism. Acad Med. 2009;84(9):1174–1176. doi: 10.1097/ACM.0b013e3181b17b11. [DOI] [PubMed] [Google Scholar]
- 34.Bellini L. M., Baime M., Shea J. A. Variation of mood and empathy during internship. JAMA. 2002;287(23):3143–3146. doi: 10.1001/jama.287.23.3143. [DOI] [PubMed] [Google Scholar]
- 35.Passik S. D., Byers K., Kirsh K. L. Empathy and the failure to treat pain. Palliat Support Care. 2007;5(2):167–172. doi: 10.1017/s1478951507070241. [DOI] [PubMed] [Google Scholar]
- 36.Brody H. The placebo response: recent research and implications for family medicine. J Fam Pract. 2000;49(7):649–654. [PubMed] [Google Scholar]
- 37.McCaffery M. The patient's report of pain. Am J Nurs. 2001;101(suppl):73–74. doi: 10.1097/00000446-200112000-00039. [DOI] [PubMed] [Google Scholar]
- 38.Herr K., Coyne P. J., Key T., et al. Pain assessment in the nonverbal patient: position statement with clinical practice recommendations. Pain Manag Nurs. 2006;7(2):44–52. doi: 10.1016/j.pmn.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 39.Chibnall J. T., Dabney A., Tait R. C. Internist judgments of chronic low back pain. Pain Med. 2000;1(3):231–237. doi: 10.1046/j.1526-4637.2000.00029.x. [DOI] [PubMed] [Google Scholar]
- 40.Chibnall J. T., Tait R. C., Ross L. R. The effects of medical evidence and pain intensity on medical student judgments of chronic pain patients. J Behav Med. 1997;20:257–271. doi: 10.1023/a:1025504827787. [DOI] [PubMed] [Google Scholar]
- 41.Tait R. C., Chibnall J. T. Physician judgments of chronic pain patients. Soc Sci Med. 1997;45(8):1199–1205. doi: 10.1016/s0277-9536(97)00033-6. [DOI] [PubMed] [Google Scholar]
- 42.Federation of State Medical Boards of the United States, Inc. Model policy for the use of controlled substances for the treatment of pain. J Pain Palliat Care Pharmacother. 2005;19(2):73–78. [PubMed] [Google Scholar]
- 43.Bair M. J. Primary care and health services section: an opportunity for pain medicine and primary care to come together. Pain Med. 2008;189(9):487–489. doi: 10.1111/j.1526-4637.2008.00489.x. [DOI] [PubMed] [Google Scholar]
- 44.Bope E. T., Douglass A. B., Gibovsky A., et al. Pain management by the family physician: the family practice pain education project. J Am Board Fam Pract. 2004;17(suppl 1):S1–S12. doi: 10.3122/jabfm.17.suppl_1.s1. [DOI] [PubMed] [Google Scholar]
- 45.Dahl J. L. New JCAHO standards focus on pain control. Oncol Issues. 1999;14(5):27–28. [Google Scholar]