Abstract
To address significant gaps in our understanding about how neurocognition, intrinsic motivation (IM), and psychosocial functioning are interrelated in schizophrenia, this study investigated the following questions: Is IM stable or dynamic over time? Does neurocognition predict change in IM over time? What is the association between change in neurocognition, change in IM, and change in psychosocial functioning? Finally, what is the causal structure of the relationships among neurocognition, IM, and psychosocial functioning over time? One hundred and thirty individuals diagnosed with schizophrenia or schizoaffective disorder were recruited from 4 community-based psychosocial rehabilitation programs in urban Los Angeles. Measures of neurocognition were taken at baseline and 12 months. Measures of IM, psychosocial functioning, and symptoms were taken at baseline, 6, and 12 months. Results of latent growth curve modeling analyses demonstrated that IM is dynamic over time. Baseline neurocognition was associated with the initial level of IM but did not predict the rate of change in motivation. However, baseline levels of IM predicted rates of subsequent improvement in neurocognition. Change in IM was strongly associated with change in psychosocial functioning, and change in neurocognition was associated with change in psychosocial functioning, but change in IM was not associated with change in neurocognition. Latent difference score analyses revealed that neurocognition caused changes in psychosocial functioning, and psychosocial functioning caused changes in IM. These findings improve our fundamental understanding of the relationships among these variables and contribute to intervention development for improving outcomes in schizophrenia.
Keywords: intrinsic motivation, neurocognition, schizophrenia, psychosocial functioning, outcome, rehabilitation
Introduction
Recent studies indicate that neurocognition and intrinsic motivation (IM) have significant functional consequences for individuals with schizophrenia.1–8 Substantial research links aspects of neurocognition to functional outcomes in work, social, and independent living domains (for review, see Green et al1). Longitudinal studies have shown that neurocognition at baseline predicts later functional outcome (for a review, see Brekke et al2 and Green et al3) and functional improvement during rehabilitation.2,4,5 There is newer but also growing literature linking intrinsic and extrinsic motivation separately to functional outcomes and treatment responsiveness (eg, Choi and Medalia6). There is also recent evidence that IM mediates the relationship between neurocognition and functional outcomes.7,8 While knowledge is growing in this area, we lack a fundamental understanding of how these variables are interrelated. A prospective approach is essential to better understand the relationships among neurocognition, IM, and functional outcomes in schizophrenia. Longitudinal multiwave data will allow for an examination of the relationships among change in these variables over time as well as for modeling the causal relationships among them. This will contribute to understanding the relationships among these variables, as well as to develop interventions for improving outcomes in schizophrenia.
Neurocognition and Functional Outcome
Numerous studies have demonstrated that individuals with schizophrenia have a variety of neurocognitive impairments including attention, episodic and working memory, language, and problem solving that are predictive of functional outcomes both cross-sectionally and longitudinally.1–3,9,10 Based on the assumption that changes in basic neurocognitive skills improve everyday life skills and functioning for persons with schizophrenia, cognitive, and functional domains are increasingly becoming primary intervention targets for individuals with schizophrenia.11–13 However, given that the variance in functional outcome explained by composite measures of neurocognition is between 20% and 40%,14 investigators have been searching for other variables that can increase our understanding of psychosocial rehabilitation outcomes15,16 as well as long-term outcomes for persons with schizophrenia.
Motivation in Schizophrenia
Motivation as a salient treatment target for reducing functional loss due to noncognitive factors has gained considerable attention.6,8,17,18 Cognitive evaluation theory categorizes sources of motivation as intrinsic and extrinsic.19,20 IM refers to behaviors that are engaged in for their own sake or for the pleasure and satisfaction derived from performing them because they produce feelings of competency and self-determination. It emphasizes the processes within the person when curiosity and interest drive the pursuit of new and stimulating activities. Extrinsic motivation pertains to behaviors that satisfy an external demand or reward contingency. Our focus is on IM as it has been seen as a core deficit in schizophrenia and has been linked to functional outcomes.7,8,21 Silverstein (this issue) focuses on the linkages between intrinsic and extrinsic motivation.
The importance of understanding motivational processes in schizophrenia was underlined at the New Approaches to Cognition Conference.22–24 Recent studies have shown that IM mediates the relationship between cognition and functional outcome.6–8,17 This suggests that IM could be a critical factor for understanding how neurocognition influences functioning in schizophrenia. Specifically, motivation difficulties have been considered to be secondary to cognitive impairments including dopamine, frontal lobes, specific networks of the limbic system including the ventral striatum and amygdala, as well as the interactions between different neural subsystems.24–29 More recently, aspects of reward processing have been implicated in conjunction with primary cognitive impairments.30–33
Components of negative symptoms of schizophrenia such as amotivation, avolition, and anhedonia have been found to mediate the relationship between symptoms and various functioning outcomes for persons with schizophrenia.34,35 Horan et al36 found that although anhedonia and social perception were not significantly correlated with each other, they were significantly correlated with different aspects of functional outcome, leading them to conclude that motivational and social cognitive variables may be particularly important in predicting different aspects of functional outcome including work, social functioning, and independent living. Alternatively, Sharma and Antova37 suggest that motivation difficulties may lead individuals to perform poorly on both cognitive tasks in the laboratory and on life functions necessary to live and work independently. Barch et al21 found that the relationship between IM and cognitive function is disrupted in schizophrenia. Interestingly, however, unlike hypotheses that suggest impairments in IM, they found that individuals with schizophrenia did not differ from controls on personal mastery and competitive excellence but reported significantly higher motivation related to anxiety using the Motivational Trait Questionnaire.21,38
Motivation Theories
Several theories explain the relationship between motivation and behavior. IM has been examined since the 1970s using attribution theory,39 social cognitive theory,40 and self-determination theory (SDT).19,20 Studies have found that IM increases if students attribute their educational results to internal factors that they can control or the amount of effort they put forth,41 believe that they are able to be effective agents in reaching desired goals,42 and are interested in mastering a topic rather than just rote learning to achieve good grades.20 High levels of intrinsic43 and task motivation44 toward mathematics are associated with high performance in mathematics. IM to read has been related to reading performance.45,46
The causal association between motivation and behavior has been considered. On the one hand, theories such as social cognitive theory,40 Vroom’s expectancy theory,47 and Hertzberg’s 2-factor theory,48 suggests that behavior is driven by an individual’s motivation. On the other hand, goal theory49,50 implies that behavior and performance leads to motivation. Studies have found that task motivation predicts subsequent academic performance,51,52 while others have demonstrated that previous achievement predicts subsequent motivation.43,53
The relationship between neurocognition, IM, and psychosocial functioning over time has not been investigated for persons with schizophrenia. Prospective studies have demonstrated that neurocognition at baseline predicts later functional outcome (for reviews, see Green et al3 and Brekke et al9). A recent longitudinal study also found a strong association between neurocognitive change and functional change during 12 months of psychosocial rehabilitation for persons with schizophrenia,5 revealing that neurocognitive improvement could be a necessary foundation for functional improvement to occur. Changes in motivation vis-a-vis behavior and performance have been examined in nonclinical samples by educational and developmental investigators.54–57 Longitudinal studies are important as they can clarify how change occurs in single variables and between variables over time. Examining the association between neurocognition, IM, and psychosocial functioning longitudinally will clearly have implications for developing psychosocial interventions in schizophrenia.
Study Questions
To address these gaps in our fundamental understanding of how neurocognition, IM, and psychosocial functioning are related in schizophrenia, this study focused on the following questions: Is IM stable or dynamic over time? Does neurocognition predict change in IM over time? What is the association between change in neurocognition, change in IM, and change in psychosocial functioning? What is the causal structure of the relationships among neurocognition, IM, and psychosocial functioning over time? Addressing these questions will improve our fundamental understanding of the relationships among these variables and will contribute to intervention development for improving functional outcomes in schizophrenia.
Methods
Subjects
Participants were recruited from the 4 community-based psychosocial rehabilitation programs in urban Los Angeles. The programs were part of a county mandated mental health initiative and were designed to provide integrated and comprehensive rehabilitative services.58 Sites were selected on the basis of data showing that they were comprehensive service environments that yielded significant improvements in functional outcomes over time.2 Diagnoses were determined using 2 sources of diagnostic information and a 3-step diagnostic checklist used by research staff. The 2 sources of information were: (1) an automated online diagnostic record system operated by the County and (2) the chart diagnosis that was completed by an onsite psychiatrist after a client interview. The 3-step process included recording the online diagnosis for most recent episode, a chart review at the admitting agency, and in the small number of instances where there was inconsistency between the 2 sets of diagnostic data, the onsite psychiatrist was consulted to reach a final study diagnosis. Selection criteria included the following: (1) diagnosis of schizophrenia or schizoaffective disorder, (2) residence in Los Angeles for at least 3 months before study admission, (3) adults age 18 years and over, and (4) no primary diagnosis of alcohol or drug dependence in the previous 6 months, no mental retardation diagnosis, and no identifiable neurological disorder. All study procedures were approved by the institutional review board at the University of Southern California.
The sample consisted of 130 individuals diagnosed with schizophrenia or schizoaffective disorder who completed baseline test batteries including neurocognition, motivation, psychosocial functioning, and symptoms. Measures of neurocognition were taken at baseline and 12 months. Measures of IM, psychosocial functioning (social, work, independent living), and symptoms were taken at baseline, 6, and 12 months. Semistructured psychosocial and functional data (including motivation) were generally gathered within 2 weeks of the neuropsychological testing. The psychosocial interviews were completed by trained research interviewers who were blind to the neuropsychological results. Neuropsychological testers were blind to the scores on the psychosocial measures.
Sample characteristics for baseline and 12 months are presented in table 1. Fifty-six percent of the subjects came from program site 1, 16% from site 2, 16% from site 3, and 12% from site 4. One hundred and five subjects (81%) completed the 12-month protocol on the study variables. There was no statistically significant differential attrition across the program sites. There were no statistically significant differences between the study completers and noncompleters, nor were there significant differences across the 4 sites on the variables in table 1. Approximately 40% of the sample came from more restrictive treatment settings or homelessness and the remainder came from other residential or outpatient settings; overall, their functional status was low at study entry.
Table 1.
Characteristics of the Samples: Full Baseline Sample and 12-Month Completers
| Original (N = 130) | Completers (N = 105) | |
| Gender (%) | ||
| Male | 89 (68.5) | 72 (68.6) |
| Female | 41 (31.5) | 33 (31.4) |
| Age | ||
| Range | 18–62 years | 21–62 years |
| Mean | 37.98 | 38.19 |
| SD | 9.02 | 9.26 |
| Ethnicity (%) | ||
| White | 57 (43.8) | 48 (45.7) |
| African American | 51 (39.2) | 38 (36.2) |
| Latino | 14 (10.8) | 12 (11.4) |
| Asian | 4 (3.1) | 4 (3.8) |
| Other | 4 (3.1) | 3 (2.9) |
| Mean (SD) | Mean (SD) | |
| Education | 11.89 years (1.81) | 12.04 years (1.84) |
| Length of illness | 13.98 years (10.01) | 13.86 years (10.08) |
| Age of onset | 23.91 years (8.94) | 24.17 years (8.79) |
| Psychosocial functioninga | 8.26 (3.55) | 8.39 (3.67) |
| Intrinsic motivation | 8.48 (4.06) | 8.65 (4.07) |
| Neurocognition (summed Z score) | −0.40 (3.31) | −0.05 (3.03) |
| Symptomatologyb | 39.26 (10.22) | 39.38 (10.63) |
| Days on medication in previous 6 months | 146.64 (63.09) | 142.20 days (65.99) |
Role Functioning Scale; total of social, work, and independence subscales.
Expanded Brief Psychiatric Rating Scale.
Measures
Neurocognitive Measures.
The following 5 measures were used to assess various aspects of neurocognition including verbal fluency, immediate memory, long-term memory, sustained attention, and mental flexibility: the Controlled Oral Word Association Test,59 the Digit Span Distractibility Test,60 the California Verbal Learning Test,61 the Degraded-Stimulus Continuous Performance Test,62 and the Wisconsin Card Sorting Test.63 These measures were administered using established procedures under the supervision of a neuropsychologist at a testing facility designed for this study.25 These specific neurocognitive tests were chosen because they have been related to functional outcomes in schizophrenia, and their composite score has been used in previous research.1,2,9 Internal consistency (Cronbach’s alpha) of the 5 scores was 0.72, and a principal component analysis found a single factor which accounted for over 50% of the total score variance. In addition, a confirmatory factor analysis showed that the single-factor model fit the data well (χ2 (5, N = 120) = 4.30, P = .51) with salient loadings (0.52 for long-term memory, 0.53 for verbal fluency, 0.55 for sustained attention, 0.69 for perseverative errors, and 0.75 for immediate memory).
Motivation Measure.
IM was defined as the interest in and enjoyment of activity for its own sake19,20 and emphasizes the importance of processes within the person when curiosity and interest drive an individual to quest after new and stimulating activities.64 While there is not yet a measure of general IM in schizophrenia, in this study it was measured by the sum of 3 items from the 6-item intrapsychic deficit subscale of the Quality of Life Scale (QLS).65 The 3 items were purpose, motivation, and curiosity. After interviewer training, the intraclass correlation coefficient (ICC) among 3 interviewers on the 6 items was >0.8.
Given that this is a new measure based on items derived from a scale that was designed to measure negative or deficit symptoms in schizophrenia, the validity of the measure deserves comment. First, the selection of the 3 items is grounded in motivation and SDTs cited above. Second, the items and probes for the ratings show face validity in terms of their focus on cross-situational phenomena in life experience such as goals, plans, areas of interest, and drive. Third, using all 6 scale items from the QLS subscale, a principal components factor analysis with varimax rotation demonstrated that the first factor accounted for approximately 51% of the variance in the 6 items and that the 3 items—purpose, motivation, and curiosity—had loadings higher than 0.7 on the first factor. The alpha for the 3 items was .74. Fourth, in previous studies, this measure has performed well in theoretical contexts including neurocognition, social cognition, other symptom dimensions, and functional outcome,35,78 and in this sample, it is not significantly correlated with any of the depression items on the Brief Psychiatric Rating Scale (BPRS). Fifth, other measures of general and situation-specific IM used with nonclinical samples focus on qualities such as self-determination and purpose, activity choice, interest and curiosity, preference for mastery and challenge, enjoyment of activity, effort, and drive.19,56,66–69 The 3 items of curiosity, motivation, and purpose cover core aspects targeted by other measures of IM developed for nonclinical populations. Based on these considerations, we suggest that this measure of IM shows some construct validity and captures aspects of IM related to drive, purpose, and engagement across situations in life; however, ways to strengthen the measurement of IM in schizophrenia will be addressed in a later section.
Turning to another issue, motivation is often considered a negative symptom of schizophrenia. Recent discussions of negative symptoms state that they are multidimensional and suggest that there are 5 symptom dimensions: blunted affect, alogia, asociality, anhedonia, and avolition.70,71 Avolition is the closest to motivation, although Blanchard and Cohen70 suggest that avolition and motivation appear in some definitions of negative symptoms but not all. There appear to be at least 2 consistent factors across factor analytic studies: diminished expression (such as blunted affect and emotional withdrawal) and anhedonia/asociality.70 Kirkpatrick et al71 also assert that while the negative symptom dimensions are most likely correlated, they could each have distinct neurobiological substrates (Barch discusses the distinct psychophysiological substrates of motivation in this issue). Therefore, both Blanchard and Cohen70 and Kirkpatrick et al71 argue that there is still much to be resolved with regard to the definition and etiological understanding of negative symptoms.
To examine the relationship between our measure of IM and negative symptoms, we combined the 3 items from the BPRS72 that have been used to measure the diminished expression dimension of negative symptoms: blunted affect, motor retardation, and emotional withdrawal. The bivariate correlations between this aspect of negative symptoms and our 3 IM items were 0.19, 0.15, and 0.26. This suggests that our measure of IM is quite empirically distinct from these negative symptom items. As stated above, it is also not correlated with the depression items from the BPRS. In summary, we posit that our measure of IM appears to yield a construct that can be conceptualized as a negative symptom dimension or not but that these definitional issues are not yet resolved.
Psychosocial Measures
The psychosocial functioning measures came from the Community Adjustment Form (CAF73). The CAF uses trained interviewers to gather behavioral event data from 17 domains of community functioning such as living situation, work and social functioning, family involvement, and medication use.74 One functional outcome measure administered during the CAF interview is the Role Functioning Scale (RFS75,76), which has been selected as a scale of choice for this population.77 Interviewer ratings of work, independent living, and social functioning from the RFS were used for this study in accordance with procedures previously reported.15 After interview training, the ICC among 3 interviewers on the RFS items was >0.8. A principal components factor analysis of the 3 items found that there was a single factor with an eigen value greater than 1 that explained 55% of the item variance, lending credence to the use of the global score.9
Symptom Measure
BPRS-Expanded72 is a commonly used symptom measure for the severe and persistently mentally ill population with good interrater reliability, good concurrent validity, and a strong factor structure.78–82 Interviewers were trained to a reliability criterion using a protocol described in.83
Statistical Analysis
Structural equation modeling with latent variables84–86 was used for this study. Specifically, latent growth curve modeling (latent growth curve modeling [LGCM]87–90) was used for the first 3 research questions while latent difference score (LDS91,92) analysis was used for the last study question. Because associations have been found between negative and disorganization symptoms and functional variables93,94 as well as between positive symptoms and community outcome,95 symptoms was controlled for when estimating statistical models.
LGCM examines change in repeated measurements and allows investigators to estimate random intercepts and random slopes for each individual and also individual growth trajectories over time.96,97 LGCM analyses do not provide the basis for drawing conclusions about whether one of the variables predicts subsequent changes in the other variable because the parameters of the curves are based on the identical time interval. Thus, to study the temporal sequence among the variables, we conducted LDS analyses.91,92
Like the latent growth curve models, LDS models are based on repeated assessments of indicators across time, with the models accounting for the covariance structure as well as the mean structure. However, in LDS models, the indicators are explained by latent true score variables and errors. The advantage of bivariate LDS models over bivariate latent LGCM is that they allow for testing of cross-lagged effects or coupling effects between the constructs, ie, the effect of one variable on subsequent intraindividual change in the other variable. However, bivariate LDS models do not allow for clear-cut interpretation of the correlations between the growth curves, which is the reason why we conducted latent growth curve analyses first. The main advantage of bivariate LDS models over traditional cross-lagged panel models98 is that LDS models also account for intraindividual change in absolute values (ie, the mean structure of the variables).
Methods of assessing model fit in the present study were selected based on established criteria.85,99–101 The χ2 test is the fit measure most often used to denote whether the hypothesized model is significantly different from one that fits the data perfectly; thus, a nonsignificant test statistic is desired to support the model.102 The Comparative Fit Index (CFI) varies between 0 and 1 and provides an assessment of comparative fit without being affected by the sample size. Tucker–Lewis Index (TLI) is a relative fit index, which compares a chi-square for the model tested with an independence model. For CFI and TLI, values >0.95 are considered excellent and >0.90 adequate fit.84 A fit index that is based on trying to estimate the match of the model to the reality in the population using degrees of freedom and the noncentral χ2 distribution is Steiger’s Root Mean Square Error of Approximation (RMSEA). The RMSEA is fairly insensitive to sample size, adjusts for parsimony, and provides a CI for the fit statistic, which ranges from 0 (perfect fit) to 1; a statistic no greater than 0.08 is desirable.86 Analyses for this study were carried out using the statistical software program, Mplus (version 5).
Results
In order to assess for selective nonresponse bias in the data, we examined selective nonresponse in the 3 repeated measurements of psychosocial functioning using ANOVA to examine if missing patterns were associated with psychosocial functioning scores at baseline. No significant association was found. There was less than 5% missing data on the motivation or functional variables. On average, 15% of the subjects had missing data on one or more of the neurocognitive tests at baseline or 12 months. This missing data was handled in model estimation using full information maximum likelihood estimation.
Change in Intrinsic Motivation
The first research question addressed the presence of change in IM. The unconditional linear LGCM showed significant change in the IM: The initial level (β = 8.50, SE = 0.35, z = 26.46, P < .001) and the rate of change (β = .08, SE = 0.03, z = 2.30, P < .05) were both significant with excellent goodness of model fit (χ2 (1) = 0.03, CFI = 1.00, TLI = 1.00, RMSEA = 0.00). This suggests that IM is dynamic over time.
Neurocognition and Change in Motivation
The second research question addressed whether neurocognition at baseline predicted change in IM over time. We tested a conditional linear LGCM in which baseline neurocognition predicted the initial level and the rate of change in IM. The conditional linear LGCM fit well with the data (χ2 (2) = 0.04, CFI = 1.00, TLI = 1.00, RMSEA = 0.00) and showed that although baseline neurocognition significantly predicted the initial level of IM (β = .32, SE = 0.06, z = 5.70, P < .001), the rate of change was not significantly predicted (β = −.003, SE = 0.006, z = −0.448, P = .65). These results show that while there was a significant cross-sectional relationship between neurocognition and IM (as has been found in several other studies), neurocognition did not predict subsequent change in IM over time. Whereas neurocognition is a rate-limiting factor for subsequent functional change (eg, Green et al3), the rate of change in IM is independent of the level of neurocognition at baseline.
Motivation and Change in Neurocognition
While not hypothesized, the results from table 2 show that the baseline level of IM (intercept of IM) was predictive of subsequent neurocognitive improvement. In other words, higher levels of IM at baseline predicted higher rates of improvement in neurocognition.
Table 2.
Association Between Change in Neurocognition, Change in Intrinsic Motivation (IM), and Change in Psychosocial Functioning (PF)
| β | SE | z | |
| Effect of change in neurocognition on change in IM and change in PF | |||
| Change in neurocognition regressed on | |||
| Intercept of IM | 0.33** | 0.10 | 3.33 |
| Slope of IM | 0.15 | 0.16 | 0.34 |
| Intercept of PF | 0.18* | 0.09 | 1.93 |
| Slope of PF | 0.33** | 0.12 | 2.73 |
| Association between the change in IM and the change in PF | |||
| Standardized covariance of | |||
| Intercept of IM and intercept of PF | 0.73** | 0.10 | 7.07 |
| Slope of IM and slope of PF | 0.62* | 0.26 | 2.43 |
| Intercept of IM and slope of PF | 0.02 | 0.15 | 0.12 |
| Slope of IM and intercept of PF | 0.16 | 0.17 | 0.35 |
| Association between intercepts and slopes within change in IM and change in PF | |||
| Standardized covariance of | |||
| Intercept of IM and slope of IM | −0.04 | 0.29 | −0.13 |
| Intercept of PF and slope of PF | 0.07 | 0.20 | 0.35 |
Note: Parameters are standardized; intercept indicates baseline score; slope indicates rate of change.
*P < .05, **P < .01.
Associated Changes Over Time
The third research question assessed the association between change in neurocognition, change in IM, and change in psychosocial functioning over time. Preliminary analyses were conducted to assess the presence of change in neurocognition and psychosocial functioning. The unconditional linear LGCM of psychosocial functioning showed significant functional change. The initial level (β = 8.23, SE = 0.31, z = 26.82, P < .001) and the rate of change (β = .16, SE = 0.03, z = 5.42, P < .001) were both significant with excellent goodness of model fit (χ2 (1) = 0.80, CFI = 1.00, TLI = 1.00, RMSEA = 0.00). The magnitude of functional change reflected a large effect size.2,5 The change in neurocognition was tested using a latent mean difference score model. This model fit very well with the data (χ2 (42) = 48.003, CFI = 0.987, TLI = 0.983, RMSEA = 0.033), showing that the mean difference in neurocognition between baseline and 12 months was statistically significant (z (129) = 2.575, P < .01, Cohen’s d = 0.45). Essentially, this demonstrated that neurocognition increased during 12 months of community-based rehabilitation (see further details in Brekke et al5). These results, and those from above, suggest that there is significant change in neurocognition, psychosocial functioning, and IM over time. More specifically, the positive change coefficients for each construct suggest that there is significant improvement over time in neurocognition, IM, and functioning.
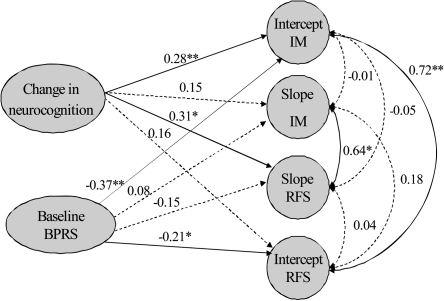
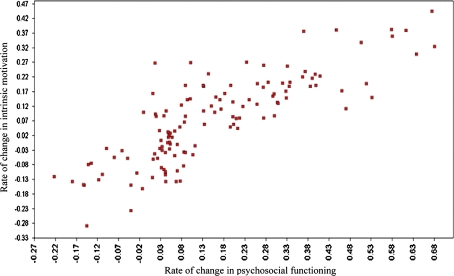
Table 2 (see also figure 1) addressed the question of whether changes among these variables were empirically associated over time. Our findings showed that there was a strong association between changes in neurocognition and psychosocial functioning and between changes in psychosocial functioning and IM (see figure 2). The direction of the unconditional betas and change coefficients suggests that the aggregate change was in the direction of improvement in all the constructs. Therefore, there was a strong association (effect sizes from medium to large) over time between improvement in neurocognition and improvement in functioning and between improvement in IM and improvement in psychosocial functioning. There was no significant relationship between change in neurocognition and change in IM.
Fig. 1.
Relationships Among Neurocognitive Change, Intrinsic Motivation, and Functioning, Controlling for Symptoms.
Note: IM, intrinsic motivation; PF, psychosocial functioning, BPRS, symptoms. Solid lines, significant paths; dashed line, nonsignificant paths. Parameters are standardized; intercept indicates baseline score; and slope indicates rate of change.
*P < .05, **P < .01.
Fig. 2.
Scatterplot of Association Between Changes in Psychosocial Functioning and Changes in Intrinsic Motivation.
Before turning to our final question, we will summarize the results regarding neurocognition and motivation. Baseline neurocognition and baseline IM were significantly related which corroborates other findings (eg, Nakagami et al8). Baseline neurocognition was not related to change in IM over time, nor were changes in neurocognition and changes in IM associated. However, baseline level of motivation was significantly predictive of subsequent change in neurocognition such that higher levels of baseline motivation are predictive of more neurocognitive improvement over time.
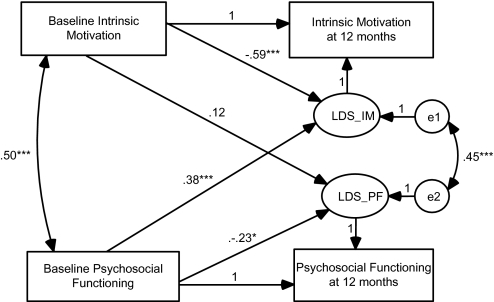
Causal Relationships Over Time
The final study question concerned the causal structure of the relationships among neurocognition, IM, and psychosocial functioning over time. These LDS analyses are predicated on a relationship between baseline values and change over 12 months, as well as on the associations between changes in the selected variables (neurocognition, IM, and psychosocial functioning) over time. Because there was no relationship between baseline neurocognition and change in IM and no association between changes in IM and neurocognition over time, these causal analyses focused on the relationship between IM and psychosocial functioning and the relationship between neurocognition and psychosocial functioning. Table 3 shows that the coefficient from baseline functioning to the latent construct difference score for IM was significant, while the coefficient from baseline motivation to the latent difference construct for psychosocial functioning was not significant (see also figure 3). This is consistent with an interpretation which suggests that psychosocial functioning is associated with subsequent change in motivation but that IM is not associated with subsequent change in functioning. In causal terms, this implies that functioning causes change in IM but IM does not cause change in functioning. Concerning the causal relationship between neurocognition and functioning, table 3 shows that the coefficient from baseline neurocognition to the LDS construct for psychosocial functioning was significant, while the coefficient from baseline functioning to the LDS construct for functioning was not significant. This finding suggests that neurocognition causes change in functioning.
Table 3.
Bivariate Latent Difference Score Model of Intrinsic Motivation (IM) and Psychosocial Functioning (PF)
| Path | b (β) | SE | z |
| Baseline PF → Latent change score in PF | −0.23 (−0.23)* | 0.12 | −2.04 |
| Baseline PF → Latent change score in IM | 0.45 (0.38)** | 0.11 | 3.98 |
| Baseline IM → Latent change score in PF | 0.11 (0.12) | 0.10 | 0.28 |
| Baseline IM → Latent change score in IM | −0.61 (−0.59)** | 0.10 | −6.01 |
*P < .05, **P < .001.
Fig. 3.
Latent Difference Score Model of Intrinsic Motivation and Psychosocial Functioning.
Table 4.
Bivariate Latent Difference Score Model of Neurocognition (NC) and Psychosocial Functioning (PF)
| Path | b (β) | SE | z |
| Baseline PF → Latent change score of PF | −0.22 (−0.21)* | 0.09 | −2.29 |
| Baseline PF → Latent change score of NC | 0.03 (0.06) | 0.04 | 0.68 |
| Baseline NC → Latent change score of PF | 0.20 (0.25)* | 0.07 | 2.41 |
| Baseline NC → Latent change score of NC | 0.06 (0.19)* | 0.03 | 2.17 |
*P < .05.
Discussion
This study provided the first examination of the prospective as well as causal relationships between neurocognition, IM, and psychosocial functioning for persons with schizophrenia. Our first study question paralleled nonclinical studies46,55,103–107 which have found that IM does change over time, particularly with regard to achievement and learning. Similarly, we found the dynamic nature of IM for persons with schizophrenia. This suggests that there might be important factors that are related to changes in IM that are relevant to functional and treatment outcomes for individuals with schizophrenia.
Concerning the factors related to IM, we found that although the initial level of neurocognition significantly predicted baseline IM, it did not significantly predict the rate of change in IM. Neurocognitive factors including episodic memory, long-term memory, vigilance, and executive functioning have been found to be a rate-limiting factor for functional change (eg, Green et al3). However, the finding that the degree of change in IM was independent of the level of neurocognition at baseline is quite notable as it suggests that neurocognition does not impede improvements in IM. In other words, individuals may increase their IM regardless of their initial level of neurocognition. This corroborates Barch et al21 who noted that cognitive function is less related to IM for persons with schizophrenia than for healthy controls. Clearly, there may be other rate-limiting factors for motivational change that have yet to be identified. Clinically, our findings indicate that treatments designed to enhance motivation might not need to be tailored to baseline neurocognitive performance, although more research is needed to address this issue because our study did not include interventions to improve motivation. Moreover, while many studies have found a strong cross-sectional association between IM and cognition, the longitudinal relationship does not mirror those findings.
A significant post hoc finding revealed that higher baseline level of IM predicted the subsequent improvement in neurocognition. Therefore, although changes in neurocognition and changes in IM were not linked, higher IM at baseline could be one of the conditions that provide the basis for higher rates of neurocognitive improvement. This supports the Neuropsychological Education Approach to Rehabilitation (NEAR) program which focuses on enhancing IM and learning.18,108,109 Other cognitive remediation models should consider attending to the initial levels of IM because enhancing IM might facilitate subsequent rates of neurocognitive improvement. These findings are also relevant to other psychosocial rehabilitation interventions, where a focus on motivation for change is featured.
Another intriguing finding concerned the significant longitudinal relationship between changes in neurocognition, IM, and psychosocial functioning. This study is the first to link changes in IM with changes in psychosocial functioning. We found a significant association between improvement in psychosocial functioning and improvement in IM. Similar to other studies (see Brekke et al5), a strong relationship between improvement in neurocognition and improvement in psychosocial functioning was also demonstrated.
The relationships described above suggest that neurocognition, IM, and psychosocial functioning may be causally linked in important respects. In addition, the aggregate change in all variables was in the direction of improvement, which indicates that prospective improvement in all of these areas is not only possible but are also associated in ways that should guide how we assess and treat deficits in any or all of these areas. Distinct interventions are available that seek to improve neurocognition,18,108–113 IM,18,108,114, and psychosocial functioning.115,116 Our findings suggest that recent efforts to blend these interventions (eg, McGurk et al12) should focus on ways to include strategies for impacting all 3 domains. Strategies for these composite interventions must be based on a well-developed understanding of how these variables are causally related as this would suggest the best approach to order and target these domains as well as discerning to what degree outcomes may emerge over time as one or more of these constructs is impacted.
Some investigators have already embarked on this work and have shown that manipulations of extrinsic motivation (eg, through monetary reinforcers) are not enough to improve cognitive performance in schizophrenia117–119 but adding enhanced instruction may help to enhance performance.117,118,120 Cognitive rehabilitation such as the previously mentioned NEAR program that enhances IM has been found to improve cognition. NEAR enhances IM by employing more engaging and interesting software packages for cognitive practice, involving consumers in choosing the focus of training and having the NEAR leader serve as a coach to engage the consumers in active guidance of their own treatment program.18,108 Silverstein (this issue) argues that the use of extrinsic motivators can trigger the development of IM in cognitive remediation interventions. Clearly, much more needs to be investigated to link these variables in treatment sequences to capitalize on their strong empirical associations.
This study was the first to examine the causal structure of the relationships between neurocognition and psychosocial functioning. Our findings suggest that neurocognition causes changes in psychosocial functioning, which is consistent with an upward generalization model where causal effects move from more basic biological processes upward to more psychosocial processes.5,10 We did not find support for a downward generalization model which would predict that variations in psychosocial functioning would cause changes in neurocognition.
This study was also the first to investigate the causal association between IM and psychosocial functioning. In this sample, we found that psychosocial functioning predicted subsequent change in IM. This is consistent with an interpretation that functioning causes changes in motivation rather than motivation causing changes in functioning. It can be speculated that experiencing a certain amount of functional improvement may enhance aspects of goal attainment49,50 including mastery orientation, one’s wish to become proficient in a topic, and task involvement. One’s self-concept (eg, self-esteem, self-efficacy) may also increase after successfully attaining a goal or completing an activity, which may well increase motivation. Self-attributions of efficacy play a key role in the self-regulation of motivation.40 Emerging literature suggests that defeatist, negativistic beliefs, and negative expectancies may contribute to the avoidance of constructive and pleasurable activity seen in individuals with schizophrenia.121,122 Improvements in functioning can be linked to these efficacy attributions. For example, the sample in this study was participating in a community-based program that embraces a psychosocial rehabilitation and recovery model where providers engage in collaborative goal setting with the clients. Clients in this sample may have been assisted in setting personally meaningful goals and/or given choices in their treatment goals.
The causal findings may contradict the approaches that propose to enhance IM in order to improve various domains of outcome.19,20,103,104,106 However, it is important to note that our results do not shed light on the potentially reciprocal and iteratively reinforcing relationship between psychosocial functioning and IM. It is possible that the changes in psychosocial functioning and IM mutually reinforce and causally interact over time. In addition, it is possible that there is a population effect for individuals with schizophrenia whose functional levels are often compromised, such that when functioning levels are compromised an initial functional increase might be required to trigger subsequent improvements in IM. Finally, we also found that baseline levels of motivation were predictive of subsequent change in neurocognition (higher baseline motivation was related to higher rates of neurocognitive improvement). Because neurocognitive improvement is strongly related to functional improvement and the causal direction suggests that neurocognition changes functioning, it is possible that baseline motivation is a potentiating factor for this relationship between neurocognition and functioning. Baseline motivation could be a kind of moderator of this relationship, which suggests that improving baseline motivation could yield higher rates of cognitive change and therefore produce more functional change. These are speculations that can be addressed in future studies.
There are several critical avenues for future research. SDT posits that IM may be facilitated in social contexts where individuals’ basic psychological needs for autonomy (ie, to have input in determining one’s own behavior), competence (ie, to experience productivity and to control outcomes), and relatedness (ie, to be related to or care for others) are satisfied.19,123 SDT emphasizes that environments experienced as controlling decrease IM.124 Furthermore, the theory posits that people are naturally inclined to interact with the environment in ways that promote learning and mastery20 and that goal and activity choice results in an increase in motivation and positive performance outcomes.19,20 On this basis, educational psychologists have used SDT to examine the ways in which socio-contextual factors play a role in motivation, subsequent behavior, and development.105,125 Students and clients whose teachers or providers were nurturing and encouraging about motivational choices and targets acquired a positive sense of choice and control over outcomes.126 Furthermore, individuals whose basic needs for autonomy and choice are met will internalize positive values and attitudes associated with a behavior. On the other hand, providers who do not facilitate the individual’s basic needs for autonomy, competence and relatedness, or provide predominantly negative feedback tend to diminish or undermine IM.20
Individuals with schizophrenia participating in community-based psychosocial rehabilitation programs do not exist in a vacuum but are rather influenced by the socio-context in which they engage in everyday activities. The sample in this study is no exception as they are influenced not only by providers and clients but also the program climate and culture. Mental health professionals may facilitate the IM of individuals with schizophrenia by providing a supportive rather than a controlling context. A collaborative goal-setting process whereby the consumer and the rehabilitation team negotiate a treatment plan is a fundamental component of any sound rehabilitation program127 and a key to accomplishing treatment goals.128–131 It also supports the emergence of IM. Providers may also give choices to consumers by structuring the demands of the environment to match the client’s feelings of effectiveness, making sure that the environment is meaningful for the individual and ensuring the individual experiences feelings of personal control and competence.132,133 Choi and Medalia114 recently integrated the 3 pronged motivational enhancement approach134 that has been found to increase IM to learn: context, personalizing, and choices. Their results illustrated that incorporating intrinsically motivating instructional methods into a difficult cognitive task increased learning of the material, yielded higher IM and better levels of self-efficacy and achievement to learn.114
Socio-contextual variables that pertain to enhancing autonomy and motivation20 such as personalization, choice, goal setting, and self-efficacy must be examined longitudinally alongside neurocognition and psychosocial functioning for persons with schizophrenia. These theoretical propositions should be integrated into future efforts to link cognition, motivation, and functional change in rehabilitation models for schizophrenia. They also suggest critical environmental and program climate factors that could be related to changes in IM and psychosocial functioning. Finally, we need studies that actively manipulate cognition, motivation, and psychosocial functioning to more adequately understand the causal relationships among these variables.
This study has several limitations. First, we did not use a measure designed to assess IM. While the 3-item scale appeared to perform well, the construct validity of the current scale has not been fully assessed. There are no scales we are aware of that measure general IM in schizophrenia. Investigators may consider using measures such as the recently adapted Intrinsic Motivation Inventory for individuals with schizophrenia (IMI-SR135) which assesses 3 relevant areas of motivation including interest/enjoyment, perceived choice, and value/usefulness. Although the IMI-SR135 measures task-oriented motivation rather than general motivation, assessing the perception of choice and task value along with the degree to which one’s sociocontext is autonomous or controlling will offer valuable clinical data on aspects that are essential to IM for treatment and task engagement for persons with schizophrenia.
Potential improvements to the current measure of IM are suggested by motivation theories which integrate an individual’s cognitive processes, factors related to self-concept, along with how social contexts shape one’s motivation and behavior.20 SDT takes into account the socio-contextual factors such as positive and negative feedback that facilitate or impede humans’ innate needs for competence, autonomy, and relatedness.20 Our measure of IM does not include a consideration the socio-contextual factors that shape IM. These could be seen as moderating factors but they appear to be essential theoretical elements in assessing IM. Second, as mentioned above, our measure attempts to assess general or domain-specific motivation instead of task-specific motivation, such as that measured by Choi and Medalia’s135 IMI-SR. Third, to be more comprehensive the scale could include rating items about intrinsically rewarding activities and how individuals cognitively appraise themselves in terms of motivation, competence, efficacy, and self-determination. In other words, our items capture part of IM related to drive, purpose, and engagement across situations in life but not about how this manifests cognitively in terms of confidence, efficacy, and self-determination which are also critical aspects of the motivation construct.
While our modeling of causal relationships was based on prospective data which increases our confidence in causal assertions,91,92,136 we did not actively manipulate cognition, motivation, or functioning. This limits the degree to which we can posit causal relationships in our data. In addition, some literature suggests that antipsychotics may impact the variables studied here, although the direct influence is uncertain.137 It should be noted that this sample is in rehabilitation and is largely made up of medication users. In addition, the relationships between motivation scores and role functioning scores may be inflated because they are rated during the same interview, although raters are trained to avoid these problems. The study sample was also not randomly selected and involved only clinically stable outpatients participating in a community-based psychosocial rehabilitation program; therefore, the generalizability of these findings to other clinical populations is unknown.
Funding
National Institute of Mental Health (R01 MH53282, R24 MH071794) to J.S.B.
References
- 1.Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the 'right stuff'? Schizophr Bull. 2000;26(1):119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 2.Brekke JS, Hoe M, Long J, Green MF. How neurocognition and social cognition influence functional change during community-based psychosocial rehabilitation for individuals with schizophrenia. Schizophr Bull. 2007;33:1247–1256. doi: 10.1093/schbul/sbl072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Green MF, Kern RS, Heaton RK. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for MATRICS. Schizophr Res. 2004;72(1):41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 4.Dickerson F, Boronow JJ, Ringel N, Parente F. Social functioning and neurocognitive deficits in outpatients with schizophrenia: a 2-year follow-up. Schizophr Res. 1999;37(1):13–20. doi: 10.1016/s0920-9964(98)00134-0. [DOI] [PubMed] [Google Scholar]
- 5.Brekke JS, Hoe M, Green MF. Neurocognitive change, functional change and service intensity during community-based psychosocial rehabilitation for schizophrenia. Psychol Med. 2009;39:1637–1647. doi: 10.1017/S003329170900539X. [DOI] [PubMed] [Google Scholar]
- 6.Choi J, Medalia A. Cognitive rehabilitation in schizophrenia. CML Psychiatry. 2009;1:25–31. [Google Scholar]
- 7.Gard DE, Fisher M, Garrett C, Genevsky A, Vinogradov S. Motivation and its relationship to neurocognition, social cognition, and functional outcome in schizophrenia. Schizophr Res. 2009;115:74–81. doi: 10.1016/j.schres.2009.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nakagami E, Xie B, Hoe M, Brekke JS. Intrinsic motivation, neurocognition and psychosocial functioning in schizophrenia: testing mediator and moderator effects. Schizophr Res. 2008;105(1–3):95–104. doi: 10.1016/j.schres.2008.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Brekke JS, Kay DD, Kee KS, Green MF. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–225. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 11.Kern RS, Liberman RP, Becker DR, Drake RE, Sugar CA, Green MF. Errorless learning for training individuals with schizophrenia at a community mental health setting providing work experience. Schizophr Bull. 2009;35:807–815. doi: 10.1093/schbul/sbn010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McGurk SR, Twamley EW, Sitzer DI, McHugo GJ, Mueser KT. A meta-analysis of cognitive remediation in schizophrenia. Am J Psychiatry. 2007;164:1791–1802. doi: 10.1176/appi.ajp.2007.07060906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szoke A, Trandafir A, Dupont ME, Meary A, Schurhoff F, Leboyer M. Longitudinal studies of cognition in schizophrenia: meta-analysis. Br J Psychiatry. 2008;192:248–257. doi: 10.1192/bjp.bp.106.029009. [DOI] [PubMed] [Google Scholar]
- 14.Couture SM, Penn DL, Roberts DL. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;32(suppl 1):S44–S63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brekke JS, Long J, Nesbitt N, Sobel E. The impact of service characteristics on functional outcomes from community support programs for persons with schizophrenia: a growth curve analysis. J Consult Clin Psychol. 1997;65:464–475. doi: 10.1037//0022-006x.65.3.464. [DOI] [PubMed] [Google Scholar]
- 16.Brekke JS, Long JD. Community-based psychological rehabilitation and prospective change in functional, clinical, and subjective experience variables in schizophrenia. Schizophr Bull. 2000;26:667–680. doi: 10.1093/oxfordjournals.schbul.a033485. [DOI] [PubMed] [Google Scholar]
- 17.Barch DM. The relationships among cognition, motivation, and emotion in schizophrenia: how much and how little we know. Schizophr Bull. 2005;31:875–881. doi: 10.1093/schbul/sbi040. [DOI] [PubMed] [Google Scholar]
- 18.Velligan DI, Kern RS, Gold JM. Cognitive rehabilitation for schizophrenia and the putative role of motivation and expectancies. Schizophr Bull. 2006;32:474–485. doi: 10.1093/schbul/sbj071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Deci EL, Ryan RM. Intrinsic Motivation and Self-Determination in Human Behavior. New York, NY: Plenum; 1985. [Google Scholar]
- 20.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 21.Barch DM, Yodkovik N, Sypher-Locke H, Hanewinkel M. Intrinsic motivation in schizophrenia: relationships to cognitive function, depression, anxiety, and personality. J Abnorm Psychol. 2008;117:776–787. doi: 10.1037/a0013944. [DOI] [PubMed] [Google Scholar]
- 22.Green MF, Nuechterlein KH. The MATRICS initiative: developing a consensus cognitive battery for clinical trials. Schizophr Res. 2004;72(1):1–3. doi: 10.1016/j.schres.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Green MF, Nuechterlein KH, Gold JM, et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-MATRICS conference to select cognitive domains and test criteria. Biol Psychiatry. 2004;56:301–307. doi: 10.1016/j.biopsych.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 24.Marder SR, Fenton W. Measurement and treatment research to improve cognition in schizophrenia: NIMH MATRICS initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72:5019. doi: 10.1016/j.schres.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Adolphs R. The neurobiology of social cognition. Curr Opin Neurobiol. 2001;11:231–239. doi: 10.1016/s0959-4388(00)00202-6. [DOI] [PubMed] [Google Scholar]
- 26.Boydell KM, Gladstone BM, Volpe T. Interpreting narratives of motivation and schizophrenia: a biopsychosocial understanding. Psychiatr Rehabil J. 2003;26:422–426. doi: 10.2975/26.2003.422.426. [DOI] [PubMed] [Google Scholar]
- 27.Brown RG, Pluck G. Negative symptoms: the ‘pathology’ of motivation and goal-directed behaviour. Trends Neurosci. 2000;23:412–417. doi: 10.1016/s0166-2236(00)01626-x. [DOI] [PubMed] [Google Scholar]
- 28.Ernst MP, Paulus M. Neurobiology of decision making: a selective review from a neurocognitive and clinical perspective. Biol Psychiatry. 2005;58:596–604. doi: 10.1016/j.biopsych.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 29.Grossberg S. Neural models of normal and abnormal behavior: what do schizophrenia, parkinsonism, attention deficit disorder, and depression have in common? Prog Brain Res. 1999;121:375–406. doi: 10.1016/s0079-6123(08)63084-8. [DOI] [PubMed] [Google Scholar]
- 30.Gard DE, Kring AM, Gard MG, Horan WP, Green MF. Anhedonia in schizophrenia: distinctions between anticipatory and consummatory pleasure. Schizophr Res. 2007;93:253–260. doi: 10.1016/j.schres.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gold JM, Waltz JA, Prentince KJ, Morris SF, Heerey EA. Reward processing in schizophrenia: a deficit in the representation of value. Schizophr Bull. 2008;34:835–847. doi: 10.1093/schbul/sbn068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Heerey EA, Gold JM. Patients with schizophrenia demonstrate dissociation between affective experience and motivated behavior. J Abnorm Psychol. 2007;116:268–278. doi: 10.1037/0021-843X.116.2.268. [DOI] [PubMed] [Google Scholar]
- 33.Heerey EA, Robinson BM, McMahon RP, Gold JM. Delay discounting in schizophrenia. Cogn Neuropsychiatry. 2007;12:213–221. doi: 10.1080/13546800601005900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kee K, Green MF, Mintz J, Brekke JS. Is emotion processing a predictor of functional outcome in schizophrenia? Schizophr Bull. 2003;29:487–497. doi: 10.1093/oxfordjournals.schbul.a007021. [DOI] [PubMed] [Google Scholar]
- 35.Yamada A, Lee K, Dinh TQ, Barrio C, Brekke JS. J Nerv Ment Dis. Intrinsic motivation as a mediator of relationships between symptoms and functioning among individuals with schizophrenia-spectrum disorders in a diverse urban community. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Horan WP, Green MF, Kring AM, Nuechterlein KH. Anhedonia in schizophrenia: a review of assessment strategies. Schizophr Bull. 2006;32:259–273. doi: 10.1093/schbul/sbj009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sharma T, Antonova L. Cognitive function in schizophrenia: deficits, functional consequences, and future treatment. Psychiatr Clin North Am. 2003;26(1):25–40. doi: 10.1016/s0193-953x(02)00084-9. [DOI] [PubMed] [Google Scholar]
- 38.Heggestad ED, Kanfer R. Individual differences in trait motivation: development of the Motivational Trait Questionnaire. Int J Educ Res. 2000;33:751–776. [Google Scholar]
- 39.Heider F. The Psychology of Interpersonal Relations. New York, NY: John Wiley & Sons; 1958. [Google Scholar]
- 40.Bandura A. Self-efficacy: The exercise of control. New York, NY: Worth Publishers; 1997. [Google Scholar]
- 41.Weiner B. An attributional theory of achievement motivation and emotion. Psychol Bull. 1985;92:548–573. [PubMed] [Google Scholar]
- 42.Zimmerman BJ. A social cognitive view of self-regulated learning. J Educ Psychol. 1989;82:297–306. [Google Scholar]
- 43.Gottfried AE. Academic intrinsic motivation in young elementary school children. J Educ Psychol. 1990;82:525–538. [Google Scholar]
- 44.Aunola K, Leskinen E, Nurmi JE. Developmental dynamics between mathematical performance, task motivation, and teachers’ goals during the transition to primary school. Br J Educ Psychol. 2006;76:21–40. doi: 10.1348/000709905X51608. [DOI] [PubMed] [Google Scholar]
- 45.Patall EA, Cooper H, Robinson JC. The effects of choice on intrinsic motivation and related outcomes: a meta-analysis of research findings. Psychol Bull. 2008;134:270–300. doi: 10.1037/0033-2909.134.2.270. [DOI] [PubMed] [Google Scholar]
- 46.Wigfield A, Harold RD, Freedman-Doan C, et al. Change in children's competence beliefs and subjective task values across the elementary school years: a 3-year study. J Educ Psychol. 1997;89:451–469. [Google Scholar]
- 47.Vroom VH. Work and Motivation. New York, NY: Wiley; 1964. [Google Scholar]
- 48.Herzberg F, Mausner B, Snyderman BB. The Motivation to Work. New York, NY: Wiley; 1959. [Google Scholar]
- 49.Ames C. Classrooms: goals, structures, and student motivation. J Educ Psychol. 1992;84:261–271. [Google Scholar]
- 50.Locke E, Latham G. A Theory of Goal Setting and Task Performance. Englewood Cliffs, NJ: Prentice–Hall; 1990. [Google Scholar]
- 51.Gottfried AE, Fleming JS, Gottfried AW. Role of parental motivational practices in children's academic intrinsic motivation and achievement. J Educ Psychol. 1994;86:104–113. [Google Scholar]
- 52.Viljaranta J, Lerkkanen MK, Poikkeus AM, Aunola K, Nurmi JE. Cross-lagged relations between task motivation and performance in arithmetic and literacy in kindergarten. Learning and Instruction. 2009;19:335–344. [Google Scholar]
- 53.Deci EL, Vallerand RJ, Pelletier LG, Ryan RM. Motivation and education: the self-determination perspective. Educ Psychol. 1991;26:325–346. [Google Scholar]
- 54.Fredricks JA, Eccles JS. Children's competence and value beliefs from childhood through adolescence: growth trajectories in two male-sex-typed domains. Dev Psychol. 2002;38:519–533. [PubMed] [Google Scholar]
- 55.Gottfried AE, Fleming JS, Gottfried AW. Continuity of academic intrinsic motivation from childhood through late adolescence: a longitudinal study. J Educ Psychol. 2001;93:3–13. [Google Scholar]
- 56.Harter S. A new self-report scale of intrinsic versus extrinsic orientation in the classroom: motivational and informational components. Dev Psychol. 1981;17:300–312. [Google Scholar]
- 57.Otis N, Grouzet FME, Pelletier LG. Latent motivational change in an academic setting: a 3-year longitudinal study. J Educ Psychol. 2005;97(2):170–183. [Google Scholar]
- 58.Young A, Sullivan G, Murata D, Sturm D, Koegel P. Implementing publicly funded risk contracts with community mental health organizations. Psychiatr Serv. 1998;49:1579–1584. doi: 10.1176/ps.49.12.1579. [DOI] [PubMed] [Google Scholar]
- 59.Lezak MD. Neuropsychological Assessment. New York, NY: Oxford University Press; 1995. [Google Scholar]
- 60.Oltmanns TF, Neale JM. Schizophrenic performance when distractors are present: attentional deficit or differential task difficulty? J Abnorm Psychol. 1975;84:205–209. doi: 10.1037/h0076721. [DOI] [PubMed] [Google Scholar]
- 61.Delis DC, Kramer JH, Kaplan E, Ober BA. The California Verbal Learning Test. New York, NY: Psychological Corporation; 1987. [Google Scholar]
- 62.Nuechterlein LK, Asarnow RF. UCLA Continuous Performance Test [manual and computer program] Los Angeles, CA. 1992;4. [Google Scholar]
- 63.Heaton RK. A Manual for the Wisconsin Card Sorting Task. Odessa, FL: Psychological Assessment Resources; 1981. [Google Scholar]
- 64.Murphy H, Roopchand N. Intrinsic motivation and self-esteem in traditional and mature students at a post-1992 university in the north-east of England. Educ Stud. 2003;29:243–259. [Google Scholar]
- 65.Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- 66.Amabile TM, Hill KG, Hennessey BA, Tighe EM. The Work Preference Inventory: assessing intrinsic and extrinsic motivational orientations. J Pers Soc Psychol. 1994;66:950–967. doi: 10.1037//0022-3514.66.5.950. [DOI] [PubMed] [Google Scholar]
- 67.Ryan RM. Control and information in the interpersonal sphere: an extension of cognitive evaluation theory. J Pers Soc Psychol. 1982;43:450–461. [Google Scholar]
- 68.Pelletier LG, Fortier MS, Vallerand RJ, Tuson KM, Briere NM, Blais MR. Toward a new measure of intrinsic motivation, extrinsic motivation, and amotivation in sports: the sport motivation scale (SMS) J Sport Exerc Psychol. 1995;17:35–53. [Google Scholar]
- 69.Vallerand RJ, Pelletier LG, Blais MR, Briere NM, Senecal C, Vallieres EF. Academic Motivation Scale: a measure of intrinsic, extrinsic, and amotivation in education. Educ Psychol Meas. 1992;52:1003–1017. [Google Scholar]
- 70.Blanchard JJ, Cohen AS. The structure of negative symptoms within schizophrenia: implications for assessment. Schizophr Bull. 2006;32:238–245. doi: 10.1093/schbul/sbj013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kirkpatrick B, Wayne S, Fenton WS, Carpenter WT, Marder SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. 2006;32:214–219. doi: 10.1093/schbul/sbj053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lukoff D, Nuechterlein K, Ventura J. Manual for the expanded Brief Psychiatric Rating Scale. Schizophr Bull. 1986;12:594–602. [Google Scholar]
- 73.Test MA, Knoedler WH, Allness DJ, Burke SS, Brown RL, Wallisch LS. Long-term community care through an assertive continuous treatment team. In: Tamminga CA, Schulz SC, editors. Advances in Neuropsychiatry and Psychopharmacology. Schizophrenia Research. Vol 1. New York, NY: Raven Press; 1991:239–246. [Google Scholar]
- 74.Brekke JS, Levin S, Wolkon GH, Sobel E, Slade ES. Psychosocial functioning and subjective experience in schizophrenia. Schizophr Bull. 1993;19:599–608. doi: 10.1093/schbul/19.3.599. [DOI] [PubMed] [Google Scholar]
- 75.Goodman SH, Sewell DR, Cooley EL, Leavitt N. Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment Health J. 1993;29:119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- 76.McPheeters HL. Statewide mental health outcome evaluation: a perspective of two southern states. Community Ment Health J. 1984;20:44–55. doi: 10.1007/BF00754103. [DOI] [PubMed] [Google Scholar]
- 77.Green MF, Gracely EJ. Selecting a rating scale for evaluating services to the chronically mentally ill. Community Ment Health J. 1987;23:91–102. doi: 10.1007/BF00757163. [DOI] [PubMed] [Google Scholar]
- 78.Hedlund JL, Vidweg BW. The Brief Psychiatric Rating Scale (BPRS): a comprehensive review. J Oper Psychiatry. 1980;11:49–65. [Google Scholar]
- 79.Newcomer JW, Faustman WO, Yeh W, Csernansky JG. Distinguishing depression and negative symptoms in unmedication patients with schizophrenia. Psychiatry Res. 1990;31:243–250. doi: 10.1016/0165-1781(90)90093-k. [DOI] [PubMed] [Google Scholar]
- 80.Rhoades HM, Overall JE. The semistructured BPRS interview and rating guide. Psychopharmacol Bull. 1988;24(1):101–104. [PubMed] [Google Scholar]
- 81.Thiemann S, Csermamslu JG, Berger PA. Rating scales in research: the case of negative symptoms. Psychiatry Res. 1987;20:47–55. doi: 10.1016/0165-1781(87)90122-3. [DOI] [PubMed] [Google Scholar]
- 82.Long JD, Brekke JS. Longitudinal factor structure of the Brief Psychiatric Rating Scale in schizophrenia. Psychol Assess. 1999;11:498–506. [Google Scholar]
- 83.Ventura J, Green MF, Shaner A, Liberman RP. Training and quality assurance with the Brief Psychiatric Rating Scale: the drift busters. Int J Methods Psychiatr Res. 1995;3:221–244. [Google Scholar]
- 84.Bentler PM. EQS: Structural Equations Program Model. Los Angeles, CA: Multivariate Software Inc.; 1995. [Google Scholar]
- 85.Kline RB. Principles and Practice of Structural Equation Modeling. 2nd ed. New York, NY: Guildford Press; 2005. [Google Scholar]
- 86.Loehlin JC. Latent Variable Models: An Introduction to Factor, Path, and Structural Analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 87.McArdle JJ. Latent variable growth within behavior genetic models. Behav Genet. 1986;16:163–200. doi: 10.1007/BF01065485. [DOI] [PubMed] [Google Scholar]
- 88.McArdle JJ, Epstein D. Latent growth curves within developmental structural equation models. Child Dev. 1987;58:110–133. [PubMed] [Google Scholar]
- 89.Meredith W, Tisak J. Latent curve analysis. Psychometrika. 1990;55:107–122. [Google Scholar]
- 90.Rogosa DR, Willett JB. Understanding correlates of change by modeling individual differences in growth. Psychometrika. 1985;50:203–228. [Google Scholar]
- 91.McArdle JJ. A latent difference score approach to longitudinal dynamic structural analysis. In: Cudeck R, du Toit S, Sörbom D, editors. Structural Equation Modeling: Present and future. A Festschrift in honor of Karl Jöreskog. Lincolnwood, IL: Scientific Software International; 2001. pp. 341–380. [Google Scholar]
- 92.McArdle JJ, Hamagami F. Latent difference score structural models for linear dynamic analyses with incomplete longitudinal data. In: Collins L, Sayer A, editors. New Methods for the Analysis of Change. Washington, DC: American Psychological Association; 2001. pp. 139–175. [Google Scholar]
- 93.Kurtz MM, Moberg PJ, Ragland JD, Gur RC, Gur RE. Symptoms versus neurocognitive test performance as predictors of psychosocial status in schizophrenia: a 1- and 4-year prospective study. Schizophr Bull. 2005;31(1):167–174. doi: 10.1093/schbul/sbi004. [DOI] [PubMed] [Google Scholar]
- 94.Milev P, Ho BC, Arndt S, Andreasen NC. Predictive values of neurocognition and negative symptoms in functional outcome in schizophrenia: a longitudinal first-episode study with 7-year follow-up. Am J Psychiatry. 2005;162:495–506. doi: 10.1176/appi.ajp.162.3.495. [DOI] [PubMed] [Google Scholar]
- 95.Wittorf A, Wiedemann G, Buchkremer G, Klingberg S. Prediction of community outcome in schizophrenia 1 year after discharge from impatient treatment. Eur Arch Psychiatry Clin Neurosci. 2008;258(1):48–58. doi: 10.1007/s00406-007-0761-z. [DOI] [PubMed] [Google Scholar]
- 96.Bollen KA, Curran PJ. Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- 97.Curran PJ, Hussong AM. The use of latent trajectory models in psychopathology research. J Abnorm Psychol. 2003;112:526–544. doi: 10.1037/0021-843X.112.4.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Finkel SE. Causal Analysis with Panel Data. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- 99.Bentler PM. Comparative fit indexes in structural models. Psychol Bull. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 100.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long GS, editors. Testing Structural Equation Models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 101.Kelloway EK. Using LISREL for Structural Equation Modeling. Thousands Oaks, CA: Sage; 1988. [Google Scholar]
- 102.Pedhazur EJ. Multiple Regression in Behavioral Research: Explanation and Prediction. 3rd ed. New York, NY: Harcourt Brace; 1997. [Google Scholar]
- 103.Gottfried AE, Marcoulides GA, Gottfried AW, Oliver P, Guerin D. Modeling the developmental decline in academic intrinsic math motivation: childhood through adolescence. Int J Behav Dev. 2007;31:317–327. [Google Scholar]
- 104.Lepper MR, Corpus JH, Iyengar SS. Intrinsic and extrinsic motivational orientations in the classroom: age differences and academic correlates. J Educ Psychol. 2005;97:184–196. [Google Scholar]
- 105.Martin AJ. Examining a multidimensional model of student motivation and engagement using a construct validation approach. Br J Educ Psychol. 2007;77:413–440. doi: 10.1348/000709906X118036. [DOI] [PubMed] [Google Scholar]
- 106.Spinath B, Spinath FM. Longitudinal analysis of the link between learning motivation and competence beliefs among elementary school children. Learn Instr. 2005;15:87–102. [Google Scholar]
- 107.Turner JC, Patrick H. How does motivation develop and how does it change? Reframing motivation research. Educ Psychol. 2008;43:119–131. [Google Scholar]
- 108.Medalia A, Revheim N, Casey M. Remediation of problem-solving skills in schizophrenia: evidence of a persistent effect. Schizophr Res. 2002;57(2–3):165–171. doi: 10.1016/s0920-9964(01)00293-6. [DOI] [PubMed] [Google Scholar]
- 109.Medalia A, Richardson R. What predicts a good response to cognitive remediation interventions? Schizophr Bull. 2005;31:942–953. doi: 10.1093/schbul/sbi045. [DOI] [PubMed] [Google Scholar]
- 110.Brenner H, Roder V, Hodel B, Kienzie N, Reed D, Liberman R. Integrated Psychological Therapy for Schizophrenic Patients. Seattle, WA: Hogrefe & Huber; 1994. [Google Scholar]
- 111.Hogarty GE, Flesher S, Ulrich R, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61:866–876. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]
- 112.Wexler BE, Bell MD. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr Bull. 2005;31:931–941. doi: 10.1093/schbul/sbi038. [DOI] [PubMed] [Google Scholar]
- 113.Wykes T, Reeder C. Cognitive Remediation Therapy for Schizophrenia: an Introduction. New York, NY: Brunner-Routledge; 2005. [Google Scholar]
- 114.Choi J, Medalia A. Intrinsic motivation and learning in a schizophrenia spectrum sample. Schizophr Res. 2009;118:12–19. doi: 10.1016/j.schres.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Bustillo JR, Lauriello J, Horan WP, Keith SJ. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2002;158:163–175. doi: 10.1176/appi.ajp.158.2.163. [DOI] [PubMed] [Google Scholar]
- 116.Dixon LB, Dickerson F, Bellack AS, et al. The 2009 schizophrenia PORT psychosocial treatment recommendations and summary statements. Schizophr Bull. 2010;36(1):48–70. doi: 10.1093/schbul/sbp115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bellack AS, Mueser KT, Morrison RL, Tierney A, Podell K. Remediation of cognitive deficits in schizophrenia. Am J Psychiatry. 1990;147:1650–1655. doi: 10.1176/ajp.147.12.1650. [DOI] [PubMed] [Google Scholar]
- 118.Green MF, Satz P, Ganzell S, Vaclav JF. Wisconsin Card Sorting Test performance in schizophrenia: remediation of a stubborn deficit. Am J Psychiatry. 1992;149:62–67. doi: 10.1176/ajp.149.1.62. [DOI] [PubMed] [Google Scholar]
- 119.Hellman SG, Kern RS, Neilson LM, Green MF. Monetary reinforcement and Wisconsin Card Sorting performance in schizophrenia: why show me the money? Schizophr Res. 1998;34:67–75. doi: 10.1016/s0920-9964(98)00088-7. [DOI] [PubMed] [Google Scholar]
- 120.Kern RS, Green MF, Goldstein MJ. Modification of performance on the span of apprehension, a putative marker of vulnerability to schizophrenia. J Abnorm Psychol. 1995;104:385–389. doi: 10.1037//0021-843x.104.2.385. [DOI] [PubMed] [Google Scholar]
- 121.Grant PM, Beck AT. Defeatist beliefs as a mediator of cognitive impairment, negative symptoms, and functioning in schizophrenia. Schizophr Bull. 2009;35:798–806. doi: 10.1093/schbul/sbn008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rector NA, Beck AT, Stolar NM. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. 2005;50:247–257. doi: 10.1177/070674370505000503. [DOI] [PubMed] [Google Scholar]
- 123.Vallerand RJ. Toward a hierarchical model of intrinsic and extrinsic motivation. In: Zanna M, editor. Advances in Experimental Social Psychology. New York, NY: Academic Press; 1997. pp. 271–360. [Google Scholar]
- 124.Deci EL, Connell JP, Ryan RM. Self-determination in a work organization. J Appl Psychol. 1989;74:580–590. [Google Scholar]
- 125.Ryan RM, Niemic CP. Self-determination theory in schools of education. Theor Res Educ. 2009;7:263–272. [Google Scholar]
- 126.Eccles JS, Wigfield A. Motivational beliefs, values, and goals. Annu Rev Psychol. 2002;53:109–132. doi: 10.1146/annurev.psych.53.100901.135153. [DOI] [PubMed] [Google Scholar]
- 127.Anthony WA, Liberman RP. The practice of psychiatric rehabilitation: historical, conceptual, and research base. Schizophr Bull. 1986;12:542–559. doi: 10.1093/schbul/12.4.542. [DOI] [PubMed] [Google Scholar]
- 128.Arnsten SM. Intrinsic motivation. Am J Occup Ther. 1990;44:462–463. doi: 10.5014/ajot.44.5.462. [DOI] [PubMed] [Google Scholar]
- 129.Burke JP. A clinical perspective on motivation: pawn versus origin. Am J Occup Ther. 1977;31:254–258. [PubMed] [Google Scholar]
- 130.Florey LL. Intrinsic motivation: the dynamics of occupational therapy theory. Am J Occup Ther. 1969;23:319–322. [PubMed] [Google Scholar]
- 131.Wu C, Hwang MT. Evaluating motivational deficits in individuals with mental illness: the Chinese General Causality Orientations Scale. Occup Ther Int. 2006;7(1):57–77. [Google Scholar]
- 132.Doble S. Intrinsic motivation and clinical practice: the key to understanding the unmotivated client. Can J Occup Ther. 1988;55:75–81. [Google Scholar]
- 133.Kielhofner G, Burke J. A model of human occupation, part one. Conceptual framework and content. Am J Occup Ther. 1980;34:572–581. doi: 10.5014/ajot.34.9.572. [DOI] [PubMed] [Google Scholar]
- 134.Cordova DI, Lepper MR. Intrinsic motivation and the process of learning: beneficial effects of contextualization, personalization, and choice. J Educ Psychol. 1993;88:715–730. [Google Scholar]
- 135.Choi J, Mogami T, Medalia A. Intrinsic Motivation Inventory (IMI): an adapted scale for schizophrenia research. Schizophr Bull. September 21, 2009 doi: 10.1093/schbul/sbp030. doi: 10.1093/schbul/sbp030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Granger CWJ. Investigating causal relations by econometric models and cross-spectral methods. Econometrica. 1969;37:424–438. [Google Scholar]
- 137.Bozikas VP, Kosmidis MH, Anezoulaki D, Giannakou M, Andreou C, Karavatos A. Impaired perception of affective prosody in schizophrenia. J Neuropsychiatry Clin Neurosci. 2006;18:81–85. doi: 10.1176/jnp.18.1.81. [DOI] [PubMed] [Google Scholar]