Abstract
Objective:
Few studies have examined the effects of brief motivational intervention components, such as change-plan completion, on treatment outcomes. This secondary analysis of an opportunistically recruited emergency-department sample of hazardous injured drinkers examines the potential predictive role of an alcohol-related change plan on treatment outcomes after accounting for pretreatment readiness. Written change plans were independently rated.
Method:
A mediational analysis framework tested directional hypotheses between pretreatment readiness, change plan, and treatment outcomes using linear regressions. The baseline total Drinker Inventory of Consequences (DrInC) score was covaried on 12-month DrInC total score, in all analyses. Participants who completed a brief motivational intervention and a change plan were included (N = 333).
Results:
Pretreatment readiness was negatively associated with alcohol consequences at 12 months, (β = -.09, t(254) = -2.07, p < .05, and good-quality change plans, (β = .18, t(320) = 4.37, p < .001. With change plan and readiness in the same model, the relationship between readiness and treatment outcomes became nonsignificant, but change plan remained a significant predictor of treatment outcomes in the expected direction, p = -.17, t(254) = -2.89, p < .01. Follow-up generalized linear modeling including an interaction term (change plan and pretreatment readiness) revealed that those with high readiness and a good-quality change plan versus those with low readiness and a poor-quality change plan had better-than-predicted outcomes for either readiness or change plan alone.
Conclusions:
Study findings suggest that the change plan in brief motivational intervention may be an active ingredient of treatment associated with better outcomes over and above the influence of pretreatment readiness.
The efficacy of motivational interviewing (MI) for substance misuse (Miller and Rollnick, 2002) is well-documented across disease domains (Burke et al., 2003; Hettema et al., 2005) and in diverse health care settings, including primary care and emergency departments (EDs; Gentilello et al., 1999; Longabaugh et al., 2001; Monti et al., 1999). The underlying principles of MI—valuing patient autonomy, collaboration, eliciting the patient's perspectives, building intrinsic motivation to change, and highlighting the discrepancy between where the patient is and where he or she wants to go—are key to its successful implementation, such that in their absence it is unlikely that MI is being delivered (Miller, 1996; Miller and Rollnick, 2002). Brief motivational interventions (BMIs) are an adaptation of MI and its principles and are predominantly used in medical or health care settings targeting a non-treatment-seeking population (Moyer et al., 2002; Rollnick et al., 1992; Saunders et al., 1995). Although BMIs are informed by MI principles, they are distinct from MI because they are more time limited (usually single session) and may include structured strategies, or treatment components, such as the use of personal feedback reports, discussion of pros and cons of use, and change-plan completion (Magill et al., 2010; Rollnick et al., 1992). The delivery of these components varies depending on the patient's readiness to change (Rollnick et al., 1992). For example, change plans are supposed to be given only when the patient is engaged in change or when the client and clinician are working on strengthening commitment to change (otherwise referred to as “Phase 2” in MI) and the patient agrees to complete one (Magill et al., 2010). Interestingly, although these components are commonly mentioned as part of a clinical trial testing BMIs, their individual effects on outcome have not been commonly reported (Zweben and Fleming, 1999). Increasing understanding of the contributions of BMI components to outcome will enhance understanding of the underlying processes that make MI effective (Dunn et al., 2001) and may help to identify MI critical ingredients, thereby enabling clinicians and investigators to tailor treatments to specific populations.
Thus far, the use of personalized feedback in conjunction with a brief or motivational interview has been associated with reduced alcohol use and reduced negative consequences (Butler and Correai, 2009; Juarez et al., 2006; McNally et al., 2005; Monti et al., 2007; Walters et al., 2009). Four studies have reported the use of the decisional balance exercise to be predictive of substance use reductions (LaBrie et al., 2006, 2008; McNally et al., 2005; Strang and McCambridge, 2004).
Although patient change talk is consistently cited as a predictor of positive treatment outcomes (Amrhein et al., 2003; Moyers et al., 2007), little, if any, research has focused on the effects of having the MI practitioner and patient complete a change plan on treatment outcomes. In the current study, we examined the effects on long-term alcohol-treatment outcomes of participants articulating and then having their therapist complete a written change plan.
The model of MI encourages clinicians to enhance their patients’ intrinsic motivation to change, which is hypothesized to increase the likelihood of behavior change (DiClemente et al., 2004; Miller and Wilbourne, 2002; Prochaska and DiClemente, 1983). Readiness to change, an important indicator of overall motivation, has been investigated for its effects on treatment outcomes. Despite its theorized importance as a factor predicting response to a BMI, little research has been conducted on readiness (Walton et al., 2008). A consistent relationship between readiness to change and treatment outcomes has not been documented because of the wide heterogeneity of study populations, clinical settings, and measurement issues.
ED-based studies have documented that higher pretreatment readiness is associated with decreases in alcohol problem scores 3 months after intervention (Leontieva et al., 2005). Another ED study found that individuals contemplating changing reported poorer outcomes at 6-month follow-up compared with individuals in the precontemplation or action stages of change (Neumann et al., 2006). Walton et al. (2008) did not find any relationship between pretreatment levels of change and intervention outcomes over time (baseline to 12-month follow-up). They suggested that pretreatment readiness reflected baseline alcohol severity, in that heavier drinkers were more ready to change than lighter drinkers. To further assess this relationship, the authors suggested examining the stage of change immediately following the intervention.
Stein et al. (2009) measured whether changes in levels of readiness, from pretreatment readiness to change to increased readiness to change following an ED-based BMI, mediated the effect of BMI on 12-month treatment outcomes. They found the hypothesized mediator effect only for patients already highly motivated before the intervention (i.e., moderated mediation; Preacher et al., 2007). The authors concluded that examining change in readiness as a potential mechanism to account for the effect of the BMI on outcome was insufficient to understand the complex role it played as a mediator.
The present study is a secondary analysis of the same data (Longabaugh et al., 2001) reported by Stein et al. (2009) of an opportunistically recruited ED sample of hazardous injured drinkers receiving a BMI. In this study, we test whether the change plan is an active ingredient of BMI that enhances patient outcome over and above that achieved by patient pretreatment readiness. Our focus on change plan and its potential interaction with pretreatment readiness is conceptually distinct from the approach taken by Stein et al., who investigated the contributions of readiness alone, both before treatment and at 3-month follow-up on 12-month treatment outcomes. Also distinct is that Stein et al. examined whether mediation accounted for the difference in outcomes for those receiving the BMI versus those who did not. The present study includes only patients who were randomized to and received the BMI, testing whether variability in the quality of the change plan developed during the BMI mediates the relationship between pretreatment readiness and 12-month outcomes.
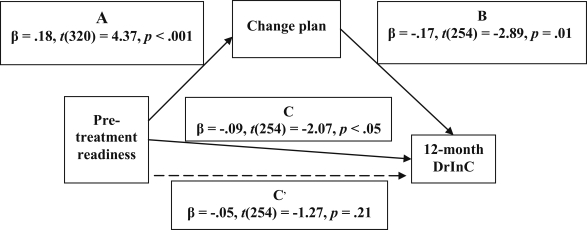
We employed a mediation analysis framework (Baron and Kenny, 1986) to test the following links in our proposed model: (a) Pretreatment readiness to change drinking would be predictive of 1-year patient negative consequences from drinking; patients more ready to change before the BMI would reduce their negative consequences from drinking more than those less ready; (b) pretreatment readiness to change drinking would also be predictive of higher quality BMI change plans, in that those who were more ready before the intervention would have a higher quality alcohol-related change plan; (c) higher quality change plans would themselves be predictive of a greater reduction of alcohol-related consequences at 1 year; (d) when the effect of higher quality change plan was partialled out from the relationship of pretreatment readiness to reduction in alcohol-related consequences, the relationship between pretreatment readiness and 1-year outcome would become nonsignificant; whereas (e) the quality of the change plan would remain as a significant predictor of outcome. Confirmation of these associations would provide support for our proposed mediation model demonstrating that among patients receiving BMI, the quality of their change plan mediated the relationship between their readiness to change and their outcome. Thus, readiness to change, without a developed quality change plan, would not be sufficient to result in better treatment outcomes (see Figure 1).
Figure 1.
Mediation of alcohol change plan on relationship of baseline readiness and 12-month Drinker Inventory of Consequences (DrInC) score (N= 333)
Method
Patient population
These data are reported from a completed trial targeting a non-treatment-seeking patient population who met criteria for hazardous drinking and who were receiving BMI (see Longabaugh et al., 2001, for a description). The original study involved three treatment groups including (a) ED treatment as usual (standard control), (b) a single brief intervention of MI (BMI), and (c) a brief intervention of MI followed by a booster session a week after the initial session (BMI-B). The present investigation is limited to participants who received either the single BMI session or the BMI plus booster session. Because standard-care patients received assessment only and no BMI session, completion of a change plan was not part of their treatment protocol. Thus, the study participants for the present analysis met the inclusion criteria for the main study but had the added criteria that they received one or two BMI sessions and also had been measured on the requisite variables necessary to conduct the planned analyses (i.e., readiness to change measured before BMI sessions, baseline and follow-up measures of alcohol-related consequences, ratings of their BMI treatment change plans, and pertinent demographic variables).
Inclusion criteria for the study were that patients were subcritically injured, discharged to home from the ED, and assessed as being hazardous drinkers as determined by meeting one or more of three criteria: (a) a score of 8 or greater on the Alcohol Use Disorders Identification Test (AUDIT), (b) being measured as alcohol positive (blood alcohol concentration ≥ .003 mg/dl while they were in the ED), or (c) reporting that they had consumed alcohol within the 6 hours before the injury that brought them to the ED. (A detailed description of inclusion and exclusion criteria can be found in Longabaugh et al., 2001.)
A total of 333 patients who received either one (n = 218) or two (n = 115) BMI sessions and who had the necessary data were included in the present analysis (78% of patients assigned to either of the MI conditions). Participants who received BMI did not differ from those receiving BMI-B on baseline demographics (age, gender, education level, alcohol severity) or on baseline levels of readiness to change.
Motivational intervention
Participants received either a single session of BMI in the ED or a session of BMI plus a booster (BMI-B) session scheduled a week later. Patients were first randomly assigned to receive standard care or a BMI before the first BMI session, and then at the end of the first BMI session they were again randomly assigned to receive or not receive the booster session.
Brief motivational intervention.
The BMI session lasted approximately 40-60 minutes and took place after assessment completion and before the patient left the hospital. The intervention was based on the motivational enhancement treatment implemented in Project MATCH (Matching Alcoholism Treatments to Client Heterogeneity; Miller et al., 1992), adapted for the ED setting (Nirenberg et al., 1996). BMI began with open-ended questions about the patient's injury and possible connections between the injury and alcohol use. If the patient did not make any connection, the intervention focus was broadened to include other negative effects identified by the patient on the Drinker Inventory of Consequences (DrInC) that he or she attributed to drinking. The interventionists used MI principles such as accurate empathy to enhance the patients’ intrinsic motivation to change by highlighting the discrepancy between their goals and behavior. For example, to increase awareness of the pros and cons of the targeted behavior, patients were assisted in assessing (a) how their alcohol use compared with a national sample and (b) positive and negative consequences that may be related to their alcohol use. Patients were also assisted with completing a change plan (see below for description) if they were engaged in change and were given a copy of the change plan at the end of the session.
Booster session (BMI-B).
Patients assigned to the BMI plus booster group were scheduled for a return visit to the hospital 7-10 days after the initial session. The BMI plus booster group was also based on the principles of MI. The patients were encouraged to discuss their postdischarge experiences, particularly with respect to the change plan they completed in the first session, and were then provided additional information about their use of alcohol (i.e., the results of an alcohol-expectancy questionnaire completed during the baseline assessment; Ramsey et al., 2000) in an effort to strengthen their change plan. Patients were able to alter their change plans to reflect their experiences since the first session.
Change plan
In this exercise, done during the course of the MI, the counselor asked the patient to articulate what, if any, changes he or she wanted to make to their drinking behavior, the most important reasons to make a change, the plan for making a change, potential barriers to successfully implementing the plan, and strategies to help overcome the barriers. Consistent with MI principles, change plans were completed as part of Phase 2 (strengthening commitment to change) activities with participants who were engaged in changing their alcohol use. Typically, the BMI interventionist (rather than the patient) completed each part of the change plan during the discussion with the patient. This flexible format is MI based, in that it does not impose the counselor's agenda onto the patient (Rollnick et al., 1992).
Measures
Coding of the change plan.
A coding system was developed by two of the authors (R.L. and T.N.) for categorizing the nature and quality of the change plan. Interventionists completed the change plans with their patients by hand and the resulting (written) change plans were reviewed and then coded by R.L. and T.N. After reviewing a substantial number of change plans (reviewers were blinded to treatment outcome), a change-plan code was developed to reliably code the change plan (% agreement ≥ .90). Then, each rater independently coded half of the remaining change plans. The four rating categories of change-plan quality were the following: 0 = there is a change plan present which does not include a goal of changing drinking either now or under specified circumstances; 1 = there is a goal of changing drinking, and the quality of the overall plan to do so is poor (i.e., within the bottom third of plans which include changing drinking as a goal); 2 = there is a goal to change drinking, and the quality of the plan is fair (i.e., within the middle third of plans which include changing drinking as a goal); 3 = there is a goal to change drinking, and the quality of the plan is good and complete (i.e., within the upper third of plans which include changing drinking as a goal).
Readiness to change.
Motivation, or readiness to make a change in drinking behavior, was measured using an adaptation from Biener and Abrams’ (1991) Readiness to Change Contemplation Ladder. The adaptation was validated on an ED treatment-seeking population of injured drinkers (Long-abaugh et al., 1995). The patient is asked to place his or her readiness to change on a rung of a contemplation ladder with response categories ranging from 0 (no thought of changing) to 10 (taking action to change; e.g., cutting down). The Readiness to Change Contemplation Ladder was grouped conceptually into the following rungs: 0 (no thought of changing), 1-3 (think I need to consider changing someday), 4-6 (think I should change but not quite ready), 7-9 (starting to think about how to change my drinking patterns), and 10 (taking action to change; e.g., cutting down) (Stein et al., 2009). These five categories correspond to the Prochaska and DiClemente (1983) five stages of change: precontemplation, contemplation, determination, preparation, and action. Readiness to change drinking was measured before the MI.
Drinker Inventory of Consequences.
The DrInC is a 45-item self-report questionnaire that asks about negative consequences experienced from drinking. The DrInC was validated on an alcohol-treatment-seeking population of 1,728 aftercare and outpatients (Miller et al., 1995). It has well-established psychometric properties (Miller et al., 1995). As validated in Project MATCH, the DrInC provides a measure of negative consequences from drinking that is sensitive to change and correlates with other outcome measures (e.g., percentage of drinking days, average number of drinks on a drinking day, subjective well-being, and psy-
chosocial functioning; Cisler and Zweben, 1999). Because the total DrInC score was not normally distributed, it was transformed using a natural-log transformation (natural log of DrInC + 1), bringing skewness and kurtosis within acceptable limits (skewness = -0.444, SE = - 0.116; kurtosis = -0.343, SE = 0.231).
We administered the lifetime version of the DrInC at baseline. At this time, we asked the patient whether he or she had ever experienced any of the consequences listed on the measure. At 1-year follow-up, we asked patients to recall how often they had experienced any of the consequences in the past year (from 0 = never to 3 = daily or almost daily). The total DrInC score at baseline served as the covariate and the total score at the 1-year follow-up point served as the dependent variable indicative of clinical outcome.
Analytic methods
First, we established that there were significant bivari-ate correlations among the putative paths in our mediation model: between baseline pretreatment readiness to change, quality of alcohol-related change plan, and baseline negative consequences from drinking (DrInC total score) (see Table 1). Consistent with our research hypotheses, we found that pretreatment readiness to change was positively correlated with good-quality change plans (see Table 1). We then followed the classic multistep approach to testing mediation (Baron and Kenny, 1986), which has been noted to correctly handle directional hypotheses of mediation subpaths (Stein et al., 2009). We conducted a series of linear regression analyses including participants who completed a motivation-ally based intervention (BMI or BMI-B) and who completed a change plan. In each regression analysis, we covaried the effects of baseline total DrInC score on our dependent variable, 12-month DrInC total score.
Table 1.
Correlations for alcohol-related change plan readiness to change, alcohol severity, and treatment assignment (BMI and BMI-B) (N= 333)
| Measure | 1. | 2. | 3. |
| 1.Alcohol-related change plan | — | ||
| 2.Readiness to change | .31*** | — | |
| 3.Baseline DrInC | .25*** | −.42*** | — |
Notes: BMI = brief motivational intervention; BMI-B = BMI plus booster session; DrInC = Drinker Inventory of Consequences.
p <.001.
Results
We found that the quality of the alcohol-related change plan was positively correlated with readiness to change (r = .31, p < .001) and baseline alcohol severity (r = .25, p < 001). Analysis of variance tests revealed that participants who completed a BMI or BMI-B did not differ on mean levels of pretreatment readiness (M BMI-B = 1.79, SD = 1.56, vs. M BMI = 1.63, SD = 1.42), F(1, 329) = 1.20, p = .25, or on the quality of the alcohol-related change plan (M BMI-B = 1.01, SD = 1.07, vs. M BMI = 0.97, SD = 1.03), F(1, 329) = 0.11,p = .74.
Following the Baron and Kenny (1986) approach to testing a mediation model, the first condition in establishing these relationships requires that pretreatment readiness differentially affects treatment outcomes. Consistent with our directional hypothesis, we found that pretreatment readiness was negatively associated (i.e., greater readiness was associated with lower negative consequences) with 12-month treatment outcomes, [β = -.09, t(254) = -2.07, p < .05. This corresponds to link C in Figure 1. The second condition requires that the level of readiness differ in its effects on the putative mediator, the quality of the change plan. Again, consistent with our directional hypothesis, participants with higher levels of readiness reported significantly better change plans than those with low levels of readiness, [β = .18, t(320) = 4.37, p < .001. This corresponds to link A in Figure 1. The third statistical condition requires that the putative mediator, the change plan, must be related to treatment outcome, independent of any effects of pretreatment readiness, β = -.17, t(254) = -2.89, p < .01. This corresponds to link B. Consistent with our directional hypothesis, we found that when including the quality of the change plan in the same model as baseline readiness, the relationship between baseline readiness and 12-month DrInC was no longer significant, β = -.05, t(254) = -1.27, p = .21. This corresponds to link C in Figure 1. We concluded that the relationship between baseline readiness and 12-month DrInC was mediated by the quality of the alcohol change plan.
To further examine the relationship between change plan and pretreatment readiness, interaction tests using SAS (SAS Institute Inc., Cary, NC) Proc GLM (generalized linear mod-eling) adjusting for differences in cell sizes were conducted. The goal was to examine whether different combinations of readiness and quality of change plan would interact to affect treatment outcome. Participants were grouped into those with high readiness and a high-quality alcohol change plan, those with high readiness and a low-quality alcohol change plan, those with low readiness and a high-quality alcohol change plan, and those with low readiness and a low-quality alcohol change plan. Using a generalized linear model with 12-month alcohol-related negative consequences as the outcome, the model was significant, F(3, 259) = 5.37, p = .001, indicating that the interaction term of readiness and quality of the change plan differentially affected participants. We found that readiness did interact with the change plan, such that those with high readiness who completed a high-quality alcohol change plan had a better outcome (12-month DrInC score: M = 1.72, SD = 1.14) than would be predicted by either the change plan or baseline readiness alone. Table 2 shows the adjusted 12-month mean DrInC scores for each of these groups.
Table 2.
Adjusted 12-month Drinker Inventory of Consequences group means by quality of alcohol-related change plan and pretreatment readiness to change alcohol use
| Quality of alcohol-related change plana |
||||||
| Good |
Poor |
|||||
| Readinessb | M | SD | n | M | SD | n |
| High | 1.72 | 1.14 | 18 | 2.18 | 1.19 | 84 |
| Low | 2.21 | 1.21 | 20 | 2.50 | 1.17 | 136 |
Scores defining categories for quality of alcohol-related change plan are as follows: poor plan (goal of change plan not alcohol related or change plan not complete) = 0.0-2.0; good plan (goal of change plan alcohol related, change plan complete and detailed) = 3.0;
readiness: low readiness = 0.0-6.0; high readiness = 7.0-10.00.
Discussion
Despite the accumulation of evidence that BMIs are effective in reducing alcohol-related outcomes, identification of how they work to bring about these outcomes has not yet been accomplished (Apodaca and Longabaugh, 2009). Examination of the active ingredients of BMIs is sparse, and for those studies reporting such examinations, positive evidence is far from conclusive.
The present study examines one BMI component, change-plan completion, as a potential mechanism through which BMI works to enhance outcomes. As noted earlier, change plans are typically completed when participants are interested in changing their alcohol use and are working with the clinician on strengthening their commitment to change. We found that, among this group, pretreatment readiness did predict treatment outcomes but that this relationship attenuated when the effects of change plan were removed from the analysis. This finding suggests that the change plan potentiates the baseline effects of treatment readiness, over and above how ready the participant is to change. Included in the conceptual model was the influence of pretreatment readiness on outcome and whether the presence of a good-quality alcohol-focused change plan interacted with baseline readiness to influence outcome. Readiness was included in this examination because of its theoretical importance in the MI model. Although not fully explicated (Miller and Rose, 2009), the premise is that high readiness to change potentiates positive outcomes because high readiness manifests itself in stronger orientation toward change, articulated in change talk, which has positively predicted the reduction of unhealthy drug or alcohol use and associated consequences (Amrhein et al., 2003; Gaume et al., 2008). Of note, prior change talk has been found to precede the development of a change plan (Magill et al., 2010), demonstrating that talking about change, and then completing a change plan, may be interrelated and synergistic events.
Consistent with another ED-based study using an in-person-based intervention, we found that higher baseline readiness predicted decreases in alcohol negative consequences (Leontieva et al., 2005). It is possible that something happens during the course of treatment that affects ED patients who are alcohol involved and who are higher in readiness, leading to better outcomes after treatment. It could be that patients’ readiness to change may enhance their treatment participation, such as creating a better quality change plan, or may lead to increased change talk through improved patient-therapist interaction. The potential link between pretreatment readiness and the different ways people participate in treatment is an important area to investigate.
Our present study extends prior findings by linking readiness to actual treatment behavior (Leontieva et al., 2005; Walton et al., 2008). Our findings (a) suggest that heavier drinkers who are more ready to change may be more likely to complete a good-quality change plan and (b) emphasize the necessity of seizing the “teachable opportunity” presented during an ED-based BMI to complete a change plan and to maximize the likelihood that the participant will commit to change.
Findings unique to the present study were (a) that completion of a high-quality alcohol-related change plan is predictive of reduced alcohol-related consequences 1 year after the intervention, (b) the quality of the change plan is itself related to pretreatment readiness to change drinking, and (c) the quality of the change plan uniquely predicts alcohol-related outcomes over and above pretreatment readiness to change. Together, this pattern of findings suggests that change-plan completion in the context of a BMI is a potential active ingredient in improving outcomes.
The interaction of readiness to change with the change plan in affecting outcomes suggests that the combination of high readiness with an alcohol-focused change plan that is comprehensive and well detailed potentiates the effect of either alone. Patients with low readiness to change are less likely to complete quality change plans and more likely to have poor alcohol-related outcomes. Patients with high readiness are more likely to complete an alcohol-focused change plan and, when they do so, are likely to have the best outcomes relative to participants with low readiness or who have poor change plans. This interaction of change plan with readiness helps to fill in the causal chain relating BMI to better alcohol-related outcomes for this population. Another study (Stein et al., 2009) showed that the superior effectiveness of the combination of a brief intervention and booster session over standard care in this population can be attributed to MI increasing motivation from pretreatment to 3 months. That study also demonstrates that high readiness at 3 months is predictive of fewer 12-month alcohol-related consequences only for those patients who are also ready to change before the BMI. Putting the results of the two studies together suggests that readiness to change before a BMI increases the likelihood of developing a change plan that is comprehensive and thoughtful for reducing alcohol-related consequences, as well as maintaining high readiness 3 months after the intervention (perhaps because of success in reducing negative consequences of drinking, itself a consequence of an effective change plan).
Although the present study is correlational in nature rather than a reflection of an experimental manipulation of hypothesized active ingredients of BMI, it nevertheless provides a first piece of evidence to suggest that the change-plan exercise in BMI may be an active ingredient of treatment that leads to better outcomes. As all evidence-based treatments for alcohol use disorders do not include change plans, this suggests that the change plan may be a distinctive ingredient of BMI that partially accounts for its effectiveness. Because identification of active ingredients of behavioral treatments is a high priority for mechanisms-of-change research in alcohol (Huebner and Tonigan, 2007) and other psychiatric disorders (Kazdin and Nock, 2003), the present findings suggest a significant step toward identifying a mechanism of change.
Limitations
The present study is limited to opportunistically identified injured hazardous drinkers in an ED setting. As noted earlier, we provided a BMI, which involved a single session and booster. In contrast, MI is an approach to counseling that may take place over several sessions. Therefore, findings in this study may be valid only for studies of BMI, and applications of the findings to MI may be hypothetical. Further, it may well be that, in alcohol-treatment-seeking populations, completing an alcohol-focused change plan may be less important. In terms of internal validity questions, the 22% loss of subjects may challenge the representativeness of the findings. Measurement issues may suppress the robustness of the findings. Readiness to change drinking is measured by a brief change ladder scale. In the main study alcohol-related consequences was the primary outcome variable most affected by treatment condition. Alcohol consumption, measured by the AUDIT, was not. This may be attributable to the focus of the intervention (on reducing negative consequences from drinking rather than drinking itself) or to the relative insensitivity of AUDIT questions measuring alcohol consumption. Irrespective of the reason, the present analysis was limited to examining the relationship of change plan to negative consequences. Measurement of the quality of the change plan was based on the written recording of the interventionist, which might vary to some extent with the quality of the change plan that was verbally developed by the patient and interventionist. Perhaps coding of tape-recorded transcripts of the BMI session would yield a more direct, potentially unbiased account of the session, and this would allow us to demonstrate that high levels of readiness are evidenced by the intensity and frequency of patient change talk, which in turn affects the development of an alcohol-focused change plan. It may be that the development and completion of an alcohol-related change plan is another expression of a patients’ commitment to change their alcohol use. Finally, although attempts to rule out competing explanations for the findings were made, it is always possible that other, unmeasured variables could provide a more parsimonious explanation or display a more robust relationship.
Future directions
Mechanisms-of-change research for BMI, MI, and indeed all evidence-based treatments for alcohol-use disorders is necessary for the field to identify how treatments work and for whom. The present study is only a first step in attempting to identify one active ingredient of a BMI treatment. A com-ponential experimental study of BMI change plans would provide more conclusive evidence. The present findings need to be replicated on other opportunistically identified patients as well as treatment-seeking patients to assess the reliability and generalizability of these results. Other MI active ingredients also need to be subjected to empirical test (Apodaca and Longabaugh, 2009), both individually and in combinations. Finally, the scope of variables that may moderate the effectiveness of the change plan needs to be widened.
Footnotes
This study was funded by National Institute on Alcohol Abuse and Alcoholism grant 5R01AA09835 (Richard Longabaugh, principal investigator).
References
- Amrhein PC, Miller WR, Yahne CE, Palmer M, Fulcher L. Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology. 2003;71:862–878. doi: 10.1037/0022-006X.71.5.862. [DOI] [PubMed] [Google Scholar]
- Apodaca T, Longabaugh R. Mechanisms of change in motivational interviewing: A review and preliminary evaluation of the evidence. Addiction. 2009;104:704–715. doi: 10.1111/j.1360-0443.2009.02527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Biener L, Abrams D. The Contemplation Ladder: Validation of a measure of readiness to consider smoking cessation. Health Psychology. 1991;10:360–365. doi: 10.1037//0278-6133.10.5.360. [DOI] [PubMed] [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;7:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Butler LH, Correai CJ. Brief alcohol intervention with college student drinkers: Face-to-face versus computerized feedback. Journal of Consulting and Clinical Psychology. 2009;23:163–167. doi: 10.1037/a0014892. [DOI] [PubMed] [Google Scholar]
- Cisler RA, Zweben A. Development of a composite measure for assessing alcohol treatment outcome: Operationalization and validation. Alcoholism: Clinical and Experimental Research. 1999;23:263–271. [PubMed] [Google Scholar]
- DiClemente CC, Schlundt D, Gemmell L. Readiness and stages of change in addiction treatment. American Journal of Addiction. 2004;13:103–119. doi: 10.1080/10550490490435777. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Daeppen JB. Brief alcohol interventions: Do counsellors’ and patients’ communication characteristics predict change? Alcohol and Alcoholism. 2008;43:62–69. doi: 10.1093/alcalc/agm141. [DOI] [PubMed] [Google Scholar]
- Gentilello LM, Rivara FP, Donovan DM, Jurkovich GJ, Daran-ciang E, Dunn CW, Ries RR. Alcohol interventions in a trauma center as a means of reducing the risk of injury recurrence. Annals of Surgery. 1999;230:473–483. doi: 10.1097/00000658-199910000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Huebner RB, Tonigan JS. The search for mechanisms of behavior change in evidence-based behavioral treatments for alcohol use disorders: Overview. Alcoholism: Clinical and Experimental Research. 2007;31(Suppl 3):1–s-3s. doi: 10.1111/j.1530-0277.2007.00487.x. [DOI] [PubMed] [Google Scholar]
- Juarez P, Walters ST, Daugherty M, Radi C. A randomized trial of motivational interviewing and feedback with heavy drinking college students. Journal of Drug Education. 2006;36:233–246. doi: 10.2190/753N-8242-727T-G63L. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. Journal of Child Psychology and Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Pedersen ER, Earleywine M, Olsen H. Reducing heavy drinking in college males with the decisional balance: Analyzing the element of motivational interviewing. Addictive Behaviors. 2006;31:254–263. doi: 10.1016/j.addbeh.2005.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaBrie JW, Pederson ER, Thompson AD, Earleywine M. A brief decisional balance intervention increases motivation and behavior regarding condom use in high-risk heterosexual college men. Archives of Sexual Behavior. 2008;37:330–339. doi: 10.1007/s10508-007-9195-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leontieva L, Horn K, Haque A, Helmkamp J, Ehrlich P, Williams J. Readiness to change problematic drinking assessed in the emergency department as a predictor of change. Journal of Critical Care. 2005;20:251–256. doi: 10.1016/j.jcrc.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Minugh PA, Nirenberg TD, Clifford PR, Becker B, Woolard R. Injury as a motivator to reduce drinking. Academic Emergency Medicine. 1995;2:817–825. doi: 10.1111/j.1553-2712.1995.tb03278.x. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Woolard RF, Nirenberg TD, Minugh AP, Becker B, Clifford PR, Gogineni A. Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. Journal of Studies on Alcohol. 2001;62:806–816. doi: 10.15288/jsa.2001.62.806. [DOI] [PubMed] [Google Scholar]
- Magill M, Apodaca TR, Barnett NP, Monti PM. The route to change: Within-session predictors of change plan completion in a motivational interview. Journal of Substance Abuse Treatment. 2010;38:299–305. doi: 10.1016/j.jsat.2009.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally AM, Palfai TP, Kahler CW. Motivational interventions for heavy drinking college students: Examining the role of discrepancy-related psychological processes. Psychology of Addictive Behaviors. 2005;19:79–87. doi: 10.1037/0893-164X.19.1.79. [DOI] [PubMed] [Google Scholar]
- Miller WR. Motivational interviewing: Research, practice, and puzzles. Addiction. 1996;21:835–842. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change. 2nd ed. New York: Guilford Press; 2002. [Google Scholar]
- Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist. 2009;64:527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Tonigan JS, Longabaugh R. The Drinker Inventory of Consequences (DrInC): An instrument for assessing adverse consequences of alcohol abuse: Test manual (NIAAA Project MATCH Monograph Series, Vol. 4, NIH Publication No. 95-3911) Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Miller WR, Wilbourne PL. Mesa grande: A methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction. 2002;97:265–277. doi: 10.1046/j.1360-0443.2002.00019.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence (NIAAA Project MATCH Monograph Series, Vol. 2, DHHS Publication No. [ADM] 92-1894) Washington, DC: Government Printing Office; 1992. [Google Scholar]
- Monti PM, Barnett NP, Colby SM, Gwaltney CJ, Spirito A, Rohsenow DJ, Woolard R. Motivational interviewing vs. feedback only in emergency care for young adult problem drinking. Addiction. 2007;102:1234–1243. doi: 10.1111/j.1360-0443.2007.01878.x. [DOI] [PubMed] [Google Scholar]
- Monti PM, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers M, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- Moyer A, Finney JW, Swearingen CE, Vergun P. Brief interventions for alcohol problems: A meta-analytic review of controlled investigations in treatment-seeking and non-treatment seeking populations. Addiction. 2002;97:279–292. doi: 10.1046/j.1360-0443.2002.00018.x. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM, Tonigan JS, Amrhein PC. Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism: Clinical and Experimental Research. 2007;31(Suppl. 3):40s–47s. doi: 10.1111/j.1530-0277.2007.00492.x. [DOI] [PubMed] [Google Scholar]
- Neumann T, Neuner B, Weiss-Gerlach E, Tønnesen H, Gentilello LM, Wenecke K-D, Spies CD. The effect of computerized tailored brief advice on at-risk drinking in subcritically injured trauma patients. Journal of Trauma. 2006;61:805–814. doi: 10.1097/01.ta.0000196399.29893.52. [DOI] [PubMed] [Google Scholar]
- Nirenberg T, Sparadeo F, Longabaugh R. Brief motivational interventions for drinking injured emergency department patients. Providence, RI: Unpublished manual, Center for Alcohol and Addiction Studies, Brown University Medical School; 1996. [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51:390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Ramsey SE, Gogineni A, Nirenberg TD, Sparadeo F, Longabaugh R, Woolard R, Minugh PA. Alcohol expectancies as a mediator of the relationship between injury and readiness to change drinking behavior. Psychology of Addictive Behaviors. 2000;14:185–191. doi: 10.1037//0893-164x.14.2.185. [DOI] [PubMed] [Google Scholar]
- Rollnick S, Heather N, Bell A. Negotiating behavior change in medical settings: The development of brief motivational interviewing. Journal of Mental Health. 1992;1:25–37. [Google Scholar]
- Saunders B, Wilkinson C, Phillips M. The impact of a brief motivational intervention with opiate users attending a methadone programme. Addiction. 1995;90:415–424. doi: 10.1046/j.1360-0443.1995.90341510.x. [DOI] [PubMed] [Google Scholar]
- Stein LAR, Minugh PA, Longabaugh R, Wirtz P, Baird J, Nirenberg TD, Gogineni A. Readiness to change as a mediator of the effect of a brief Motivational Intervention on posttreatment alcohol-related consequences of injured emergency department hazardous drinkers. Psychology of Addictive Behaviors. 2009;23:185–195. doi: 10.1037/a0015648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, McCambridge J. Can the practitioner correctly predict outcome in motivational interviewing? Journal of Substance Abuse Treatment. 2004;27:83–88. doi: 10.1016/j.jsat.2004.05.003. [DOI] [PubMed] [Google Scholar]
- Walters ST, Vader AM, Harris TR, Field CA, Jouriles EN. Dismantling motivational interviewing and feedback for college drinkers: A randomized clinical trial. Journal of Consulting and Clinical Psychology. 2009;77:64–73. doi: 10.1037/a0014472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Goldstein AL, Chermack ST, McCammon RJ, Cunningham RM, Barry KL, Blow FC. Brief alcohol intervention in the emergency department: Moderators of effectiveness. Journal of Studies on Alcohol and Drugs. 2008;69:550–560. doi: 10.15288/jsad.2008.69.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zweben A, Fleming MF. Brief interventions for alcohol and drug problems. In: Tucker JA, Donovan DM, Marlatt GA, editors. Changing addictive behavior: Bridging clinical and public health strategies. New York: Guilford Press; 1999. pp. 251–282. [Google Scholar]