Abstract
OBJECTIVES
To determine the rate of prostate-specific antigen (PSA) screening in men aged 80 and older in Medicare and to examine geographic variation in screening rates across the U.S.
DESIGN
Retrospective cohort study of variation across hospital referral regions using administrative data.
SETTING
National random sample in fee-for-service Medicare.
PARTICIPANTS
Medicare beneficiaries aged 80 and older in 2003.
MEASUREMENTS
Percentage of men aged 80 and older screened using the PSA test.
RESULTS
The national rate of PSA screening in men aged 80 and older was 17.2%, but there was wide variation across regions (<2–38%). Higher PSA screening in a region was positively associated with greater total costs (correlation coefficient (r) = 0.49, P<.001), greater intensive care unit use at the end of life (r = 0.46, P<.001), and greater number of unique physicians seen (r = 0.36, P<.001). PSA screening was negatively associated with proportion of beneficiaries using a primary care physician as opposed to a medical subspecialist for the predominance of ambulatory care (r = −0.38, P<.001).
CONCLUSION
PSA screening in men aged 80 and older is common practice, although its frequency is highly variable across the United States. Its association with fragmented physician care and aggressive end-of-life care may reflect less reliance on primary care and consequent difficulty informing patients of the potential harms and low likelihood of benefit of this procedure.
Keywords: elderly, screening, prostate cancer, primary care, utilization
There is growing concern that older adults are at risk for exposure to potentially harmful treatments for which the promised benefit is small, if not absent. Screening for prostate cancer with a prostate-specific antigen (PSA) blood test is an excellent example. Expert consensus has concluded that the harms of PSA screening outweigh benefits in men with a life expectancy of less than 10 years or, more recently according to the U.S. Preventive Services Task Force (USPSTF), in men aged 75 and older.1-3 Yet patient reports and surveys of physicians indicate that PSA screening in elderly men is common and increasing.4-6 Fifty percent of men aged 80 and older report that they have had a PSA screening in the previous year, and 45% have had a screening PSA in the Department of Veterans Affairs system.4,7
Little is known about PSA screening in typical clinical practice among men in fee-for-service Medicare, which covers 85% of the elderly U.S. population. To gain meaningful insights into clinical practice, investigators have used regional variations research to reveal where there are divergent practices in the use of medical technologies.8,9 For example, recent work has shown that use of technologically intensive care at the end of life is highly variable.10,11 Studies have explored the causes of this variation and have shown a relationship between available hospital beds and hospitalization rates at the end of life, and that patient preferences do not account for the observed differences.10-14 More recently, local care systems are using variation data for benchmarking and identifying opportunities for improvement.15 For PSA screening, there is disagreement as to whether age should be used as a criterion for when to stop screening, but the degree to which men at advanced age are screened or how much variation there is across regions smaller than the four large census regions of the United States is unknown.6,7,16-18
This study reports the national rate and geographic variation in PSA screening of male Medicare beneficiaries aged 80 and older in 2003, before the USPSTF age-based cutoff was recommended. The primary goal of this article is to describe clinical practice under the guideline based on life expectancy to gauge how much change of practice the new age-based guideline might entail. Eighty was chosen as the lower age limit for the investigation, because as a general rule, screening would not be recommended (median survival of 6.7 years), yet some clinicians may be uncomfortable with the general rule because the median survival in the healthiest quartile is 10.7 years.19 The study also explored the association between regional PSA screening rates and other regional patterns of use to generate hypotheses regarding the potential sources of the observed variation.
METHODS
Overview
This study used a retrospective cohort design reporting PSA screening in men aged 80 and older in fee-for-service Medicare. Screening is reported as the average for the nation and for each hospital referral region (HRR). HRRs are geographic regions developed to describe healthcare markets. The 306 HRRs are based on travel patterns for cardiothoracic and neurological surgery patients and are created by aggregating the smaller 3,566 hospital services areas developed from all Medicare hospital discharge patterns.20
The association between selected regional practice patterns and regional PSA screening rates was also tested to generate hypotheses about the causes of variation in practice. Enthusiasm for tests and procedures in general (as measured by spending on tests and procedures), aggressive approaches in advanced illness (as measured by technologically aggressive end-of-life care), and use of primary care physicians to guide care (as measured by ratio of visits that are to primary care and the degree of fragmentation) were assessed. These associations do not imply causation but are meant to suggest directions for future studies of PSA screening and quality improvement initiatives. It was expected that greater use of testing and procedures in general, greater use of aggressive treatments, and less concentration of visits with primary care physicians would be associated with greater PSA screening rates in men aged 80 and older.
Data Sources
The data set was created using Medicare claims data for 2000 to 2004, using a 20% random sample of Medicare beneficiaries. The denominator, carrier, outpatient, and Medicare Provider Analysis and Review files were used. Beneficiary demographics were obtained from the Centers for Medicare and Medicaid Services (CMS) denominator files and clinical diagnoses from diagnostic codes listed on submitted claims, requiring one Part A or two Part B claims occurrences to count. Procedures and visits were calculated from carrier and outpatient files. Physician specialty is indicated on carrier file claims. When more than one specialty was listed, the one under which the physician billed most was used. All utilization data are reported for 2003 except for calculations of end-of-life care, to which 2002 data contributed.
Study Population
Medicare beneficiaries were eligible if they were aged 80 by January 1, 2003, and had complete claims data (fully entitled in Parts A and B and not enrolled in managed care). For the primary outcome measure, the sample was restricted to men. For other measures, the appropriate denominator was included for each measure: all decedents in 2003 for the end-of-life measures and all beneficiaries in 2003 for cost and general utilization measures.
Primary Outcome Measure
The occurrence of PSA testing was identified according to Common Procedural Terminology (CPT) codes G0103 or 84153 in the carrier and outpatient files.21 The CPT code for PSA testing encompasses not only screening, but all PSA testing. To capture men who had a PSA test for a presumed screening indication, men who had any history of prostate cancer in the prior 3 years or who had symptoms in the 3 months before a PSA test that might have triggered a suspicion of cancer according to diagnostic codes billed on visits and hospitalizations were excluded from the PSA measure. This algorithm has been previously validated.7
Use of Tests and Procedure Measures
The association between PSA testing and spending on testing and procedures relative to other types of spending was examined to explore whether the practice is related to general enthusiasm for testing. Spending measures were based on standardized prices for inpatient hospital care and physician care. Standardization of prices assigns the same dollar value to a service regardless of region, and therefore any differences in spending reflect differences in utilization and not differences in billing across regions. Spending was grouped using the Berenson-Eggers Type of Service coding system into readily understood clinical categories.22
End-of-Life Care Measures
Technologically aggressive care at the end of life was chosen as an indicator that a region employs more-aggressive approaches to advanced illness. Other studies have shown that preference for this type of care declines with advanced age but that technologically aggressive end-of-life care is wide-spread.23,24 End-of-life measures were calculated for all decedents aged 80 and older in the calendar year and were reported for the last 6 months of life. CMS validates the death indicator from the denominator file, which captures all deaths—not solely those that occur during an institutional stay.
Use of Primary Care and Fragmentation Measures
The decision to screen is typically in the domain of primary care, so PSA screening rates were compared with the degree of primary care orientation of local systems and fragmentation (as a potential barrier to effective primary care). For all beneficiaries who had at least one evaluation and management claim in 2003, the predominant physician provider of ambulatory care was determined. The method for assignment has been previously described.25 In brief, the predominant provider was defined as the primary care or medical subspecialist with whom the patient had the most ambulatory visits during the 2 years after an index visit to any provider. If there were none of these specialties involved in care, assignment was allowed to other physician types (<3% of patients). General practice, family practice, internal medicine, and geriatrics were categorized as primary care specialties.
Analysis
All HRR rates were adjusted for age, sex, and race using SAS version 9.0 (SAS Institute, Inc., Cary, NC). Using Stata 10.0 (Stata Corp., College Station, TX), the association between PSA screening and other regional utilization measures across all 306 HRRs were tested using Pearson correlation for continuous variables. HRRs were grouped into quintiles based on PSA screening rates, and one-way analysis of variance was performed to test for differences in utilization and care patterns across quintiles. Data were suppressed for any region with event rates too low for reporting according to CMS privacy rules.
RESULTS
In a 20% national fee-for-service Medicare sample, there were 628,570 men aged 80 and older with no prior history of prostate cancer or any symptoms to indicate the need for a diagnostic PSA test. Of these men, 17% had a screening PSA test in 2003. The likelihood of having PSA screening was strongly related to the beneficiary’s HRR of residence. Screening rates across all HRRs in the United States ranged from less than 2% to 38%, as shown graphically in Figure 1, in which a circle represents the rate for each HRR. The geographic distribution of screening intensity is shown in Figure 2.
Figure 1.
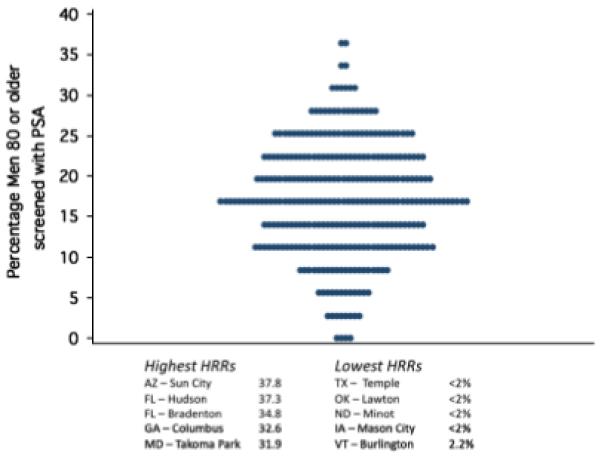
Variation across hospital referral regions (HRRs) in the percentage of men aged 80 and older who had a screening prostate-specific antigen (PSA) test in 2003. Each circle represents the PSA screening rate for each hospital referral region—age, sex, and race adjusted. The panel shows the actual screening rates in the five highest and five lowest screening regions.
Figure 2.
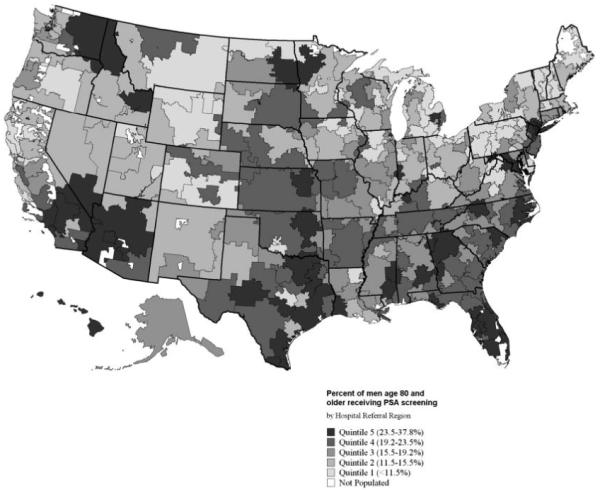
U.S. hospital referral region map of screening prostate-specific antigen (PSA) rates in men aged 80 and older categorized in quintiles.
Regions were categorized according to their quintile rank of screening PSA (Table 1), with average PSA screening rates across quintiles ranging from 7.4% in Quintile 1 to 26.9% in Quintile 5. Care patterns and costs for all Medicare beneficiaries aged 80 and older were evaluated across these screening intensity quintiles. Average costs across these quintiles were higher in high screening regions (Q1 $5,964 to Q5 $6,632). All types of spending, not only laboratory testing, were higher in high screening regions, except for spending on major procedures. The difference in major procedures reached statistical significance but not a clinically meaningful difference across quintiles ($4 from low to high quintile).
Table 1. Healthcare Usage Patterns of Fee-for-Service Medicare Beneficiaries Aged 80 and Older Nationally and Stratified According to Hospital Referral Regions (HRRs) Grouped into Quintiles from Low to High Prostate-Specific Antigen (PSA) Screening Rates*.
| Measures | Overall, Mean ± Standard Deviation |
Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 |
|---|---|---|---|---|---|---|
| HRRs, n | 306 | 61 | 61 | 62 | 61 | 61 |
| Beneficiaries aged ≥80 per HRR, n | 5,060 | 3,353 | 5,302 | 4,739 | 5,362 | 6,551 |
| Men aged ≥80 screened with PSA, % | 17.2 ± 7.0 | 7.4 | 13.2 | 17.2 | 21.3 | 26.9 |
| Cost for all beneficiaries aged ≥80, $ | ||||||
| Total (Diagnosis Related Group+Relative Value Unit) | 5,945 ± 883 | 5,413 | 5,619 | 5,910 | 6,153 | 6,632 |
| Part B | ||||||
| Evaluation and management | 1,016 ± 228 | 893 | 935 | 978 | 1,051 | 1,225 |
| Imaging | 239 ± 73 | 192 | 214 | 225 | 249 | 316 |
| Tests | 148 ± 49 | 106 | 127 | 137 | 163 | 207 |
| Major procedures | 47 ± 9 | 49 | 48 | 45 | 47 | 45 |
| Durable medical equipment | 133 ± 44 | 110 | 122 | 128 | 139 | 170 |
| Care in last 6 months of life for all decedents aged ≥80 | ||||||
| Any mechanical ventilation, %† | 5.9 ± 2.3 | 5.5 | 5.2 | 5.4 | 6.0 | 7.1 |
| Percutaneous feeding tube placement, %† | 5.2 ± 2.2 | 4.2 | 4.5 | 5.1 | 5.1 | 6.2 |
| Intensive care unit days, n | 2.2 ± 1.1 | 1.6 | 2.0 | 2.2 | 2.4 | 3.0 |
| Place of death in hospital, % | 26.0 ± 6.5 | 22.4 | 24.9 | 27.3 | 26.9 | 28.3 |
| Physician visits by all beneficiaries aged ≥80 | ||||||
| Seen by 10 or more unique physicians, % | 21.1 ± 5.4 | 19.0 | 19.7 | 20.4 | 21.7 | 24.5 |
| Proportion of physician visits to primary care physicians | 0.57 ± 0.06 | .60 | .57 | .58 | .56 | .53 |
| Predominant physician type for ambulatory visits is primary care, % |
83.2 ± 6.5 | 86.5 | 83.7 | 84.4 | 83.2 | 78.4 |
All rates are age, race, and when appropriate sex adjusted. All P-values for difference across groups <.001 with the exception of Part B Major Procedures, for which P = .04.
Results for percentage mechanical ventilation restricted to 210 HRRs with adequate event rate for reporting and 188 HRRs for feeding tube rates.
The type of care received during the last 6 months of life for beneficiaries aged 80 and older also varied across quintiles of PSA screening. Specifically, placement of a feeding tube was 43% higher, use of mechanical ventilation was 29% higher, and decedents had nearly twice the number of intensive care unit days in the highest as the lowest quintile of screening. In the highest quintile, decedents were also more likely to die in a hospital than in other lower-acuity settings or at home.
Beneficiaries in the highest screening quintile were 23% more likely to see 10 or more unique physicians in a year than those in the lowest, and medical subspecialists accounted for a greater proportion of visits. Finally, in low screening regions, beneficiaries were 10% more likely to use a primary care specialist as the physician seen for the predominance of ambulatory visits.
The positive associations between higher PSA screening and costs (r = 0.49), technological care at the end of life (r = 0.46), and fragmentation across multiple physicians (r = 0.36) were moderately strong (Figure 3). The percentage of beneficiaries who used a primary care physician for the largest proportion of their ambulatory care was negatively associated at a similar magnitude (r = −0.38).
Figure 3.
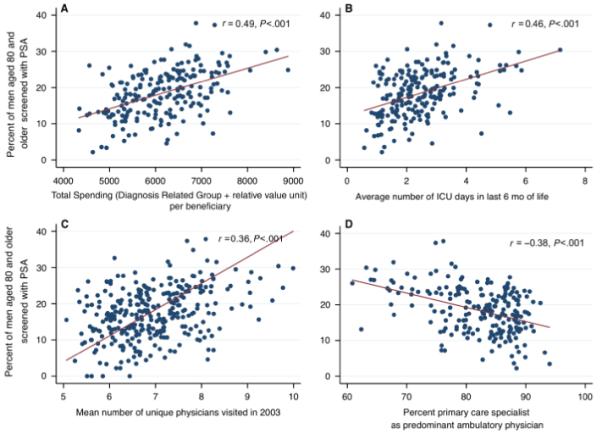
Association between percentage of men aged 80 and older who had a screening prostate-specific antigen (PSA) test and (A) total Medicare spending for beneficiaries aged 80 and older, (B) average number of intensive care unit days in the last 6 months of life for all decedents aged 80 and older, (C) average number of unique physicians visited by all beneficiaries aged 80 and older, and (D) percentage of all beneficiaries aged 80 and older whose predominant ambulatory physician was in a primary care specialty.
DISCUSSION
Screening men aged 80 and older for prostate cancer using a PSA test is common practice in many regions across the United States, but its frequency is highly variable. Nationally, nearly 20% of men aged 80 and older had a screening PSA test in 2003, yet clinical practice in some regions is essentially not to screen any man in this category (<2%), whereas in others, nearly 40% are screened. As the map shows (Figure 2), regions with high screening rates are found across the entire United States, but low and high screening regions often directly abut one another, such as in Temple and Austin, Texas, or Flint and Lansing, Michigan.
The implication of this study is that there appeared to be little consensus in clinical practice on PSA testing of men aged 80 and older across regions before the age-based recommendation to stop screening was released. Yet low (near zero) screening rates in some regions, indicating some consensus within those HRRs, was surprising. In fact, the overall screening rate in this national sample of men was lower than reported in surveys and in the Department of Veterans Affairs (VA) system.4-7 Although survey data may lead to overestimation of screening rates,26 the regional differences in Medicare and the difference between Medicare and the VA findings (both calculated using claims) raise important questions about how different locations or payers influence screening rates; after all, screening is a clinical decision that is supposed to be highly individualized to a person’s health status and preferences.19 Any efforts to implement the USPSTF guidelines to cease screening at age 75 will need to take into consideration the baseline clinical practice in the local care system where intervention is proposed. The data from the current study show that this guideline may be controversial in high screening regions and possibly irrelevant in low screening ones.
With such large differences across regions, whether attributes of the regional delivery system are related to PSA screening at advanced age was asked. It was hypothesized that regions with high PSA screening rates would also have high use of testing and procedures in general for beneficiaries aged 80 and older, but it was found that all categories of usage except major procedures were higher in high screening regions. This exception of major procedures is difficult to explain but may suggest that these procedures, which entail higher risk, are handled differently from other types of care at advanced age. A surprisingly strong positive association was found between screening PSA and technologically aggressive end-of-life care in men aged 80 and older, considering that hospital-based and clinic-based processes were being compared. Higher rates of PSA screening in men aged 80 and older were also found in regions characterized by fragmentation of physician care and lower likelihood of using a primary care physician as the predominant provider. These associations taken together paint a picture in which very old men cared for in systems where advanced disease is treated aggressively and primary care providers have a less central role in care may be more likely to have a screening PSA test.
An alternative hypothesis to explain the regional variation is that the patients or doctors are in some way different across regions. Underlying health status could systematically vary across regions, a testable hypothesis that would be modeled best by incorporating functional status. Patient preferences for screening could also be different. Certainly enthusiasm for screening is high in the general public,27 but physicians appeared to initiate PSA screening more than patients. In a study of men who reported being screened, men aged 80 and older indicated the physician initiated testing 90% of the time.28 Physician attitudes are therefore likely to be important. Although attitudes may have changed, in 1995 primary care physicians highly favored PSA screening even in men aged 80 and older.28 In addition, practice in their region influences physician use of discretionary care.29 Further investigation of physician attitudes may be warranted, including how their normative behavior develops within a region or practice setting.
Much is already known about how to influence the process of prostate cancer screening decisions from clinical trials aimed at improving engagement of patients and provision of balanced information. Randomized trials using a standardized process of shared decision-making—the application of decision aids—have led to lower preference for screening and lower rates in the general population.30-34 The current literature suggests that men are not well informed, with 35% who had a PSA test reporting that they were unaware that they were screened, 69% reporting that the physician discussed only pros of screening and not cons, and other survey data showing poor knowledge of risks and benefits.35-41 To the authors’ knowledge, there are no published studies of decision aids that address the question of when to stop PSA screening, although it has been done for mammography.42 In the context of widely varying PSA screening rates in men aged 80 and older and consensus that many of these men would be exposed to more harm than benefit by screening, one path forward would be to institute better mechanisms for ensuring informed patient choice.
Several important limitations of this study need to be mentioned. These data are cross-sectional and do not support any causal relationships. The goal in comparing PSA screening with other clinical practices was to look for system-level factors worthy of future research. For example, further studies with a prospective design would be necessary to test the hypothesis that better-engaged and -informed men aged 80 and older would opt for PSA screening less frequently. As mentioned earlier, important relevant domains such as patient preferences and physician attitudes cannot be assessed. Future studies using a prospective design would also be needed to test whether an individual’s use of primary care independent of regional practices influences PSA screening. Claims data also have limitations in the accuracy of diagnosis, and hence there may be some contamination of the sample by men with prostate cancer. There is no reason to suspect this contamination would be different across regions, and it is likely that the broad exclusion criteria of prostate diagnoses, procedures, and symptoms led to conservative estimates of screening.
The 20-fold variation in the percentage of men aged 80 and older who receive PSA screening suggests that routine clinical practice patterns had not converged in spite of growing expert consensus in the early 2000s. With less than one-quarter of men in this age range likely to survive 10 years, screening rates in excess of that rate suggest that many men are being exposed to a test that poses more risk for harm than benefit. Whether efforts to inform patients better, strengthen primary care, or benchmark physician performance could reduce that exposure are questions that warrant further investigation. As we face rapidly increasing numbers of people aged 80 and older, the ability to apply current evidence in treatment of a population with limited life expectancy needs to be improved such that high quality is maintained while effective care is still delivered.
ACKNOWLEDGMENTS
Julie Bynum, Yunjie Song, and Elliott Fisher received direct grant funding to support this work.
This work was funded by the Robert Wood Johnson Physician Faculty Scholars Program and Paul B. Beeson Career Development Award in Aging, National Institute on Aging Grant AG-07-001.
Sponsor’s Role: The sponsors had no role in the design, methods, subject recruitment, data collections, analysis, or preparation of the manuscript.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
[see editorial comments by Dr. Jeff Whittle, pp 000–000]
REFERENCES
- 1.Anonymous, American Urological Association Prostate-specific antigen (PSA) best practice policy. Oncology. 2000;14:267–272. 277–268, 280. [PubMed] [Google Scholar]
- 2.Smith RA, Cokkinides V, von Eschenbach AC, et al. American Cancer Society guidelines for the early detection of cancer. CA Cancer J Clin. 2002;52:8–22. doi: 10.3322/canjclin.52.1.8. [DOI] [PubMed] [Google Scholar]
- 3.Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;149:185–191. doi: 10.7326/0003-4819-149-3-200808050-00008. [DOI] [PubMed] [Google Scholar]
- 4.Sirovich BE, Schwartz LM, Woloshin S. Screening men for prostate and colorectal cancer in the United States: Does practice reflect the evidence? JAMA. 2003;289:1414–1420. doi: 10.1001/jama.289.11.1414. [DOI] [PubMed] [Google Scholar]
- 5.Lu-Yao G, Stukel T, Yao S-L. Prostate-specific antigen screening in elderly men. J Natl Cancer Inst. 2003;95:1792–1797. doi: 10.1093/jnci/djg104. [DOI] [PubMed] [Google Scholar]
- 6.Farwell WR, Linder JA, Jha AK. Trends in prostate-specific antigen testing from 1995 through 2004. Arch Intern Med. 2007;167:2497–2502. doi: 10.1001/archinte.167.22.2497. [DOI] [PubMed] [Google Scholar]
- 7.Walter LC, Bertenthal D, Lindquist K, et al. PSA screening among elderly men with limited life expectancies. JAMA. 2006;296:2336–2342. doi: 10.1001/jama.296.19.2336. [DOI] [PubMed] [Google Scholar]
- 8.Skinner J, Weinstein JN, Sporer SM, et al. Racial, ethnic, and geographic disparities in rates of knee arthroplasty among Medicare patients. N Engl J Med. 2003;349:1350–1359. doi: 10.1056/NEJMsa021569. [DOI] [PubMed] [Google Scholar]
- 9.Wennberg JE, Gittelsohn A, Shapiro N. Health care delivery in Maine, III: Evaluating the level of hospital performance. J Mar Med Assoc. 1975;66:298–306. [PubMed] [Google Scholar]
- 10.Wennberg JE, Fisher ES, Stukel TA, et al. Use of hospitals, physician visits, and hospice care during last six months of life among cohorts loyal to highly respected hospitals in the United States. BMJ. 2004;328:607–611. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wennberg JE, Fisher E, Goodman D, et al. Tracking the Care of Patients with Severe Chronic Illness. The Trustees of Dartmouth College; Hanover: 2008. [PubMed] [Google Scholar]
- 12.Earle CC, Neville BA, Landrum MB, et al. Trends in the aggressiveness of cancer care near the end of life. J Clin Oncol. 2004;22:315–321. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- 13.Barnato AE, Herndon MB, Anthony DL, et al. Are regional variations in end-of-life care intensity explained by patient preferences?: A study of the US medicare population. Med Care. 2007;45:386–393. doi: 10.1097/01.mlr.0000255248.79308.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anthony DL, Herndon MB, Gallagher PM, et al. How much do patients’ preferences contribute to resource use? Health Aff. 2009;28:864–873. doi: 10.1377/hlthaff.28.3.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Robert Wood Johnson Foundation [Accessed October 19, 2008];Quality/Equality Press Kit: Aligning Forces for Quality. 2008 [on-line]. Available at http://www.rwjf.org/quality-equality/af4q/about.jsp.
- 16.Konety BR, Cooperberg MR, Carroll PR. Are age-based criteria the best way to determine eligibility for prostate cancer screening? Ann Intern Med. 2009;150:220–221. doi: 10.7326/0003-4819-150-3-200902030-00018. [DOI] [PubMed] [Google Scholar]
- 17.Gogol M. Are age-based criteria the best way to determine eligibility for prostate cancer screening? Ann Intern Med. 2009;150:221. doi: 10.7326/0003-4819-150-3-200902030-00019. [DOI] [PubMed] [Google Scholar]
- 18.Ross LE, Berkowitz Z, Ekwueme DU. Use of the prostate-specific antigen test among U.S. men: Findings from the 2005 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2008;17:636–644. doi: 10.1158/1055-9965.EPI-07-2709. [DOI] [PubMed] [Google Scholar]
- 19.Walter LC, Covinsky KE. Cancer screening in elderly patients—a framework for individualized decision making. JAMA. 2001;285:2750–2756. doi: 10.1001/jama.285.21.2750. [DOI] [PubMed] [Google Scholar]
- 20.Wennberg JE, Cooper MM, editors. The Dartmouth Atlas of Health Care. American Hospital Publishing; Chicago, IL: 1998. [PubMed] [Google Scholar]
- 21.Centers for Medicare and Medicaid Services [Accessed November 23, 2009];HCPCS—General Information. 2009 [on-line]. Available at http://www.cms.hhs.gov/MedHCPCSGeninfo/
- 22.Centers for Medicare and Medicaid Services [Accessed March 9, 2009];Berenson-Eggers Type of Services. [on-line]. Available at http://www.cms.hhs.gov/hcpcsreleasecodesets/20_betos.asp.
- 23.Somogyi-Zalud E, Zhong Z, Hamel MB, et al. The use of life-sustaining treatments in hospitalized persons aged 80 and older. J Am Geriatr Soc. 2002;50:930–934. doi: 10.1046/j.1532-5415.2002.50222.x. [DOI] [PubMed] [Google Scholar]
- 24.Hamel MB, Lynn J, Teno JM, et al. Age-related differences in care preferences, treatment decisions, and clinical outcomes of seriously ill hospitalized adults: Lessons from SUPPORT. J Am Geriatr Soc. 2000;48:S176–S182. doi: 10.1111/j.1532-5415.2000.tb03129.x. [DOI] [PubMed] [Google Scholar]
- 25.Bynum JPW, Bernal-Delgado E, Gottlieb D, et al. Assigning ambulatory patients and their physicians to hospitals: A method for obtaining population-based provider performance measurements. Health Serv Res. 2007;42:45–62. doi: 10.1111/j.1475-6773.2006.00633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.May DS, Trontell AE. Mammography use by elderly women: A methodological comparison of two national data sources. Ann Epidemiol. 1998;8:439–444. doi: 10.1016/s1047-2797(98)00010-6. [DOI] [PubMed] [Google Scholar]
- 27.Schwartz LM, Woloshin S, Fowler FJ, Jr., et al. Enthusiasm for cancer screening in the United States. JAMA. 2004;291:71–78. doi: 10.1001/jama.291.1.71. [DOI] [PubMed] [Google Scholar]
- 28.Han PK, Coates RJ, Uhler RJ, et al. Decision making in prostate-specific antigen screening National Health Interview Survey, 2000. Am J Prevent Med. 2006;30:394–404. doi: 10.1016/j.amepre.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 29.Sirovich B, Gallagher PM, Wennberg DE, et al. Discretionary Decision making by primary care physicians and the cost of U.S. health care. Health Aff. 2008;27:813–823. doi: 10.1377/hlthaff.27.3.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Volk RJ, Cass AR, Spann SJ. A randomized controlled trial of shared decision making for prostate cancer screening. Arch Fam Med. 1999;8:333–340. doi: 10.1001/archfami.8.4.333. [DOI] [PubMed] [Google Scholar]
- 31.Frosch DL, Kaplan RM, Felitti VJ. A randomized controlled trial comparing Internet and video to facilitate patient education for men considering the prostate specific antigen test. J Gen Intern Med. 2003;18:781–787. doi: 10.1046/j.1525-1497.2003.20911.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gattellari M, Ward JE. Does evidence-based information about screening for prostate cancer enhance consumer decision-making? A randomised controlled trial. J Med Screen. 2003;10:27–39. doi: 10.1258/096914103321610789. [DOI] [PubMed] [Google Scholar]
- 33.Partin MR, Nelson D, Radosevich D, et al. Randomized trial examining the effect of two prostate cancer screening educational interventions on patient knowledge, preferences, and behaviors. J Gen Intern Med. 2004;19:835–842. doi: 10.1111/j.1525-1497.2004.30047.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gattellari M, Ward JE. A community-based randomised controlled trial of three different educational resources for men about prostate cancer screening. Patient Educ Couns. 2005;57:168–182. doi: 10.1016/j.pec.2004.05.011. [DOI] [PubMed] [Google Scholar]
- 35.Chan EC. Promoting informed decision making about prostate cancer screening. Compr Ther. 2001;27:195–201. doi: 10.1007/s12019-001-0014-4. [DOI] [PubMed] [Google Scholar]
- 36.Chan EC, Vernon SW, O’Donnell FT, et al. Informed consent for cancer screening with prostate-specific antigen: How well are men getting the message? Am J Public Health. 2003;93:779–785. doi: 10.2105/ajph.93.5.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.O’Dell KJ, Volk RJ, Cass AR, et al. Screening for prostate cancer with the prostate-specific antigen test: Are patients making informed decisions? J Fam Pract. 1999;48:682–688. [PubMed] [Google Scholar]
- 38.Ransohoff DF, McNaughton Collins M, Fowler FJ. Why is prostate cancer screening so common when the evidence is so uncertain? A system without negative feedback. Am J Med. 2002;113:663–667. doi: 10.1016/s0002-9343(02)01235-4. [DOI] [PubMed] [Google Scholar]
- 39.Steele CB, Miller DS, Maylahn C, et al. Knowledge, attitudes, and screening practices among older men regarding prostate cancer. Am J Public Health. 2000;90:1595–1600. doi: 10.2105/ajph.90.10.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Federman DG, Goyal S, Kamina A, et al. Informed consent for PSA screening: Does it happen? Eff Clin Pract. 1999;2:152–157. [PubMed] [Google Scholar]
- 41.Hoffman RM, Couper MP, Zikmund-Fisher BJ, et al. Prostate cancer screening decisions: Results from the National Survey of Medical Decisions (DECISIONS Study) Arch Intern Med. 2009;169:1611–1618. doi: 10.1001/archinternmed.2009.262. [DOI] [PubMed] [Google Scholar]
- 42.Mathieu E, Barratt A, Davey HM, et al. Informed choice in mammography screening: A randomized trial of a decision aid for 70-year-old women. Arch Intern Med. 2007;167:2039–2046. doi: 10.1001/archinte.167.19.2039. [DOI] [PubMed] [Google Scholar]


