Abstract
Background
Contemporary trends in the management and outcomes of patients with chronic kidney disease who develop an acute myocardial infarction have not been adequately described, particularly from the more generalizable perspective of a population-based investigation.
Methods
The study population consisted of 6,219 residents of the Worcester (MA) metropolitan area hospitalized with acute myocardial infarction in 6 annual periods between 1995 and 2005. Patients were categorized as having either preserved kidney function (n=3,154), mild to moderate chronic kidney disease (n=2,313), or severe chronic kidney disease (n=752) at the time of hospital admission.
Results
Patients with chronic kidney disease were more likely to be older, have a greater prevalence of comorbidities, and were more likely to experience significant in-hospital complications or die during hospitalization in comparison to patients with preserved kidney function. Although patients with chronic kidney disease were less likely to receive effective cardiac medications or undergo coronary interventional procedures than patients without kidney disease, we observed a marked increase in the use of effective cardiac medications and coronary interventional procedures in patients with chronic kidney disease during the period under study. In-hospital death rates declined over time among patients with chronic kidney disease while these death rates remained unchanged among persons with normal kidney function.
Conclusion
The results of this study in residents of a large New England metropolitan area provide insights into changing trends in the treatment and impact of chronic kidney disease in patients hospitalized with acute myocardial infarction.
Keywords: renal disease, long-term trends and outcomes, acute myocardial infarction, population-based study
INTRODUCTION
Chronic kidney disease is a growing global health problem and is an important risk factor for cardiovascular disease.1,2 Chronic kidney disease is also an important predictor of adverse outcomes in patients hospitalized with acute myocardial infarction.3–5
Advances in treatment, including prompt coronary reperfusion and use of evidence-based medications including antiplatelet agents, beta-blockers, HMG CoA-reductase inhibitors, and inhibitors of the renin-angiotensin-aldosterone system, have led to significant reductions in short-term morbidity and mortality for patients with acute myocardial infarction.6–10 While these therapeutic advances have favorably altered various patient outcomes, the benefits associated with the use of these therapies have largely occurred among patients with preserved renal function; patients with chronic kidney disease have either been under-represented and/or excluded from the pivotal clinical trials of these therapies11. Previous studies have shown that patients with chronic kidney disease were less likely to receive effective medical therapies or undergo coronary revascularization for acute myocardial infarction compared to those with preserved kidney function and, not surprisingly, outcomes in these patients have lagged behind12–16. Given the current state of knowledge, it remains unknown to what extent adoption of effective therapies for acute myocardial infarction has improved hospital-associated outcomes in this high risk population.
The objectives of this observational study in a community-wide population of patients hospitalized with acute myocardial infarction were to describe changing trends in the characteristics, management practices, and short-term outcomes of patients with chronic kidney disease, as compared to those with preserved kidney function, during a recent 10-year period (1995–2005). A secondary study objective was to determine whether differences in the outcomes of patients with, as compared to those without, chronic kidney disease were attributed to differences in the treatment of these high risk patients or to other contributory factors. Data from the population-based Worcester Heart Attack Study were utilized for purposes of this investigation.12,17,18
METHODS
Study Population
The Worcester Heart Attack Study is an ongoing population-based investigation that is examining the descriptive epidemiology of acute myocardial infarction in residents of the Worcester (MA) metropolitan area (2000 census estimate 478,000) hospitalized at all central Massachusetts medical centers with independently confirmed acute myocardial infarction. Details of this study have been previously described.17,18
Data Sources
In brief, the medical records of greater Worcester residents hospitalized with a discharge diagnosis of acute myocardial infarction were individually reviewed and validated according to pre-established diagnostic criteria.17,18 Demographic and clinical characteristics including age, sex, co-morbidities, physiologic factors, hospital length of stay, acute myocardial infarction type, development of acute clinical complications during hospitalization, and the use of cardiac medications, coronary angiography, percutaneous coronary intervention (PCI), and coronary artery bypass grafting (CABG) were abstracted from hospital medical records by trained nurse and physician reviewers in whom ongoing quality control checks were performed on a regular basis. All medical history variables were considered to be present if there was mention of these comorbid conditions in hospital medical records. Each of the clinical complications examined that may have developed during hospitalization for acute myocardial infarction was considered to be present based on the review of hospital medical records using standardized definitions for each of these important clinical complications.12,17,18 In addition to examining in-hospital death rates according to degree of kidney dysfunction, we also examined 30-day case-fatality rates after hospital admission based on a comprehensive review of hospital records and death certificates. This study was approved by the Committee for the Protection of Human Subjects at the University of Massachusetts Medical School.
Measurement of Kidney Function
Serum creatinine levels were obtained at the time of admission to all greater Worcester hospitals for acute myocardial infarction. The 4-component Modification of Diet in Renal Disease equation was used to estimate the glomerular filtration rate (eGFR).19 For purposes of analysis, patients were stratified into 3 groups according to baseline levels of eGFR: ≥60 ml/min/1.73m2 (preserved kidney function; n=3,154), 31–59 ml/min/1.73m2 (mild to moderate chronic kidney disease; n=2,313), whereas those with an eGFR ≤30ml/min/1.73m2 (n=752) were considered to have severe chronic kidney disease.20 Patients who were on dialysis were included in the present analysis (n=195) and aggregated with the sample of patients with severely reduced kidney function. The final study sample consisted of 6,219 greater Worcester residents hospitalized with confirmed acute myocardial infarction during 6 study years: 1995 (n=925), 1997 (n=1009), 1999 (n=1007), 2001 (n=1233), 2003 (n=1152), and 2005 (n=893).
DATA ANALYSIS
Differences in the characteristics of greater Worcester residents hospitalized with acute myocardial infarction with preserved kidney function, mild to moderate chronic kidney disease, and severe chronic kidney disease were examined through the use of chi square tests of statistical significance for discrete variables and ANOVA for continuous variables. A multivariable logistic regression analysis was used to examine differences in hospital treatment practices and short-term outcomes of patients with varying degrees of kidney function while controlling for a variety of demographic and clinical factors of prognostic importance. These variables were included in the regression models (Tables 2 and 3) either because they differed between the respective kidney disease comparison groups or because they have been shown to have prognostic importance in prior investigations. Multivariable adjusted odds ratios (OR) and accompanying 95% CIs were calculated in a standard fashion. Despite the nonrandomized, observational nature of the present investigation, and potential for confounding by treatment indication, we examined differences in the short-term prognosis of patients with varying degrees of kidney function while controlling for previously described patient associated characteristics as well as hospital treatment practices. This analysis was carried out for purposes of determining whether differences in short-term prognosis according to extent of kidney dysfunction were due to differences in the receipt of effective cardiac treatment practices or to other factors. Changing trends in the use of beneficial cardiac therapies and interventional procedures, within each of our kidney function groups, were assessed using the Mantel-Haenszel chi square test for trend. Trends in hospital and short-term outcomes were examined using a similar analytic test.
Table 2.
Treatment of 6,219 Patients Hospitalized with Acute Myocardial Infarction According to Levels of Estimated Glomerular Filtration Rate (eGFR)
| Total Sample |
2003/2005 Study Cohorts |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| eGFR (ml/min/1.73m2) | eGFR (ml/min/1.73m2) | eGFR (ml/min/1.73m2) | eGFR (ml/min/1.73m2) | |||||||
| ≤30 (n=752) | 31–59 (n=2,313) | ≥60 (n=3,154) | ≤ 30 Adjusted Odds Ratio (95% CI)§ | 31–59 Adjusted Odds Ratio (95% CI)§ | ≤30 (n=255) | 31–59 (n=819) | ≥60 (n=974) | ≤ 30 Adjusted Odds Ratio (95% CI)§ | 31–59 Adjusted Odds Ratio (95% CI)§ | |
| Medications (%) | ||||||||||
| ACE inhibitors/ARB's | 44.2 | 58.2 | 55.4 | 0.48 (0.40–0.58) | 0.82 (0.69–0.97) | 55.3 | 73.5 | 75.6 | 0.29 (0.21,0.40) | 0.64 (0.47,0.88) |
| Aspirin | 83.9 | 89.3 | 95.0 | 0.63 (0.46–0.86) | 0.64 (0.48–0.85) | 88.6 | 91.6 | 96.4 | 0.82 (0.46,1.48) | 1.00 (0.56,1.72) |
| Beta blockers | 74.3 | 82.5 | 89.5 | 0.64 (0.50–0.82) | 0.85 (0.68–1.08) | 87.1 | 91.8 | 95.1 | 0.57 (0.33,0.99) | 1.12 (0.64,1.95) |
| Lipid lowering agents | 37.9 | 43.8 | 50.8 | 0.85 (0.69–1.04) | 0.87 (0.73–1.05) | 60.4 | 69.0 | 77.8 | 0.67 (0.48,0.95) | 0.76 (0.56,1.03) |
| Procedures | ||||||||||
| Coronary angiography | 23.3 | 40.7 | 62.9 | 0.39 (0.32–0.49) | 0.64 (0.53–0.76) | 28.2 | 51.8 | 77.4 | 0.26 (0.18,0.37) | 0.60 (0.44,0.80) |
| Percutaneous coronary intervention | 11.9 | 22.7 | 38.5 | 0.47 (0.36–0.61) | 0.68 (0.55–0.84) | 19.2 | 35.8 | 61.5 | 0.36 (0.25,0.52) | 0.55 (0.41,0.75) |
| Coronary artery bypass grafting | 2.4 | 5.5 | 7.2 | 0.43 (0.25–0.74) | 0.76 (0.52–1.12) | 1.2 | 5.1 | 5.2 | 0.28 (0.08,0.92) | 1.06 (0.57,1.96) |
eGFR ≥60 is the referent group
adjusted for age, sex, body mass index, prior history of: angina, hypertension, diabetes, stroke, hypercholesterolemia, heart failure, acute myocardial infarction order (initial vs prior) and acute myocardial infarction type (Q wave vs non-Q wave)
Table 3.
Length of Hospital Stay and Short-Term Outcomes in Patients Hospitalized with Acute Myocardial Infarction According to Levels of Estimated Glomerular Filtration Rate (eGFR)
| eGFR (ml/min/1.73m2) |
eGFR (ml/min/1.73m2) |
eGFR (ml/min/1.73m2) |
|||||
|---|---|---|---|---|---|---|---|
| Outcomes | ≤30 (n=752) | 31–59 (n=2,313) | ≥60 (n=3,154) | ≤30 Adjusted Odds Ratio (95% CI)* | 31–59 Adjusted Odds Ratio (95% CI)* | ≤30 Adjusted Odds Ratio (95% CI)§ | 31–59 Adjusted Odds Ratio (95% CI)§ |
| Length of hospital stay (mean, days) | 7.1 | 6.6 | 5.8 | 1.34 (1.11,1.62)# | 1.05(0.89,1.24) | 1.68 (1.38,2.04) | 1.15 (0.97,1.37) |
| Hospital Complications (%) | |||||||
| Atrial fibrillation | 23.8 | 22.1 | 13.9 | 1.20 (0.96,1.50) | 1.15 (0.94,1.41) | 1.33 (1.05,1.68) | 1.19 (0.97,1.46) |
| Cardiogenic shock | 9.7 | 8.0 | 4.1 | 2.05 (1.45,2.90) | 1.55 (1.11,2.16) | 2.33 (1.61,3.38) | 1.72 (1.22,2.44) |
| Heart failure | 61 | 48.4 | 23.9 | 2.01 (1.65,2.46) | 1.46 (1.23,1.74) | 2.21 (1.80,2.72) | 1.49 (1.25,1.79) |
| Death | 24.7 | 14.7 | 4.9 | 2.99 (2.31,3.87) | 1.96 (1.53,2.51) | 2.49 (1.89,3.28) | 1.81 (1.39,2.35) |
| 30-day mortality | 32.2 | 19.2 | 6.6 | 3.00 (2.38,3.79) | 2.01 (1.61,2.51) | 2.55 (1.99,3.26) | 1.88 (1.49,2.36) |
adjusted for age, sex, body mass index, prior history of: angina, hypertension, diabetes, stroke, hypercholesterolemia, heart failure, acute myocardial infarction order (initial vs prior) and acute myocardial infarction type (Q wave vs non-Q wave)
adjusted for variables included in the first multiple regression analysis as well as use of hospital cardiac medications and coronary interventional procedures
Compared to length of stay >median of 5 days
RESULTS
BASELINE CHARACTERISTICS
The average age of study patients was 71 years, 56% were men, and the majority (93%) were Caucasian. Of the 6,219 patients with confirmed acute myocardial infarction, 3,065 (49%) had chronic kidney disease as defined by an eGFR < 60 ml/min/1.73m2 at the time of hospital presentation (Table 1).
Table 1.
Characteristics of 6,219 Patients Hospitalized with Acute Myocardial Infarction According to Levels of Estimated Glomerular Filtration Rate (eGFR)
| Total Sample |
||||
|---|---|---|---|---|
| Characteristic | eGFR ≤30*(n=752) | eGFR 31–59 (n=2,313) | eGFR ≥60 (n=3,154) | P value# |
| Age (mean, yrs) | 77.1 (11.1)§ | 76.8 (10.7) | 64.6 (14.0) | <0.001 |
| Male (%) | 43.2 | 43.7 | 68.6 | <0.001 |
| Medical history (%) | ||||
| Angina | 23.5 | 25.4 | 20.0 | <0.001 |
| Diabetes | 51.2 | 36.8 | 24.9 | <0.001 |
| Heart failure | 50.9 | 31.7 | 10.1 | <0.001 |
| Hypertension | 82.1 | 75.5 | 57.8 | <0.001 |
| Stroke | 18.9 | 15.0 | 7.1 | <0.001 |
| Hypercholesterolemia | 38.0 | 42.9 | 47.3 | <0.001 |
| Physiologic factors (mean) | ||||
| Systolic blood pressure (mmHg) | 134.8 (37.4) | 142.4 (36.2) | 144.5 (30.9) | <0.001 |
| Diastolic blood pressure (mmHg) | 69.7 (22.8) | 74.6 (21.3) | 81.3 (19.4) | <0.001 |
| Serum glucose (mg/dl) | 230.9 (177.4) | 199.0 (131.9) | 163.9 (114.1) | <0.001 |
| Initial heart rate (bpm) | 89.3 (25.1) | 90.1 (25.4) | 83.5 (21.8) | <0.001 |
| Total cholesterol (mg/dl) | 169.3 (56.8) | 179.6 (57.2) | 187.2 (48.7) | <0.001 |
| Acute Myocardial Infarction Characteristics (%) | ||||
| Initial | 54.9 | 59.1 | 71.6 | <0.001 |
| Q-wave | 14.4 | 21.6 | 33.5 | <0.001 |
ml/min/1.73m2
standard deviation
Summary p value or ANOVA comparing differences in selected factors between the 3 primary comparison groups
In comparison to patients with preserved kidney function, patients with chronic kidney disease were more likely to be older and female (Table 1). In addition, they were more likely to have a history of previously diagnosed angina, diabetes, heart failure, hypertension, myocardial infarction, and stroke, but were less likely to have a history of hypercholesterolemia. Patients with chronic kidney disease were less likely to present with a Q-wave acute myocardial infarction. Similar differences were observed in these characteristics when we restricted our analysis to patients hospitalized for acute myocardial infarction in our 2 most recent study years of 2003 and 2005 (data not shown).
PHYSICIANS PRESCRIBING PRACTICES
Compared to patients with preserved kidney function, patients with chronic kidney disease were less likely to be prescribed angiotensin converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARB), aspirin, beta blockers, or lipid lowering agents during hospitalization (Table 2). These patients were also less likely to have undergone coronary angiography, a percutaneous coronary intervention (PCI), and coronary artery bypass (CABG) surgery during hospitalization. After adjustment for several important clinical and demographic covariates that may have affected physicians prescribing practices, patients with chronic kidney disease remained at lower odds for receiving effective cardiac medications, PCI, or CABG surgery in comparison to patients with preserved kidney function (Table 2). Albeit at lower utilization rates, there were no significant differences in the use of beta blockers or CABG surgery in patients with mild/moderate chronic kidney disease compared to patients with preserved kidney function. There were also no significant differences in the receipt of lipid lowering therapy in patients with either mild/moderate or severe chronic kidney disease in comparison to patients with normal kidney function.
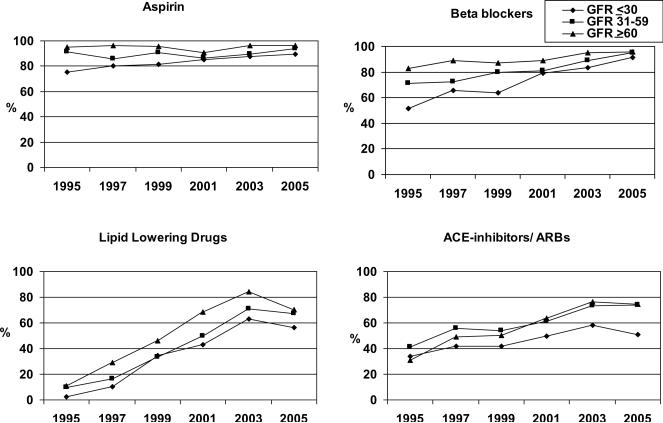
CHANGES IN PHYSICIANS MANAGEMENT PRACTICES OVER TIME
Significant changes in the management of hospitalized patients with chronic kidney disease were observed between 1995 and 2005 (Figures 1 and 2). While the use of aspirin in patients with preserved kidney function remained stable over time, an increase in aspirin use was observed in patients with chronic kidney disease, especially among those with severe chronic kidney disease (p <.05, Figure 1). Despite this encouraging trend, patients with chronic kidney disease remained less likely to be treated with aspirin during hospitalization for acute myocardial infarction even during the most recent years under study. Beta blocker use increased in all patient groups over time, with marked increases observed among patients with chronic kidney disease. The use of lipid lowering agents and ACE-inhibitors/ARBs increased in a similar fashion in all groups over time (p<.05). Despite these trends, patients with severe chronic kidney disease remained less likely than those with preserved or mild to moderately reduced kidney function to be treated with lipid lowering agents and ACE-inhibitors/ARBs in 2005.
Figure 1.
Trends in the prescribing of effective cardiac therapies in 6,219 patients hospitalized with acute myocardial infarction according to degree of kidney function
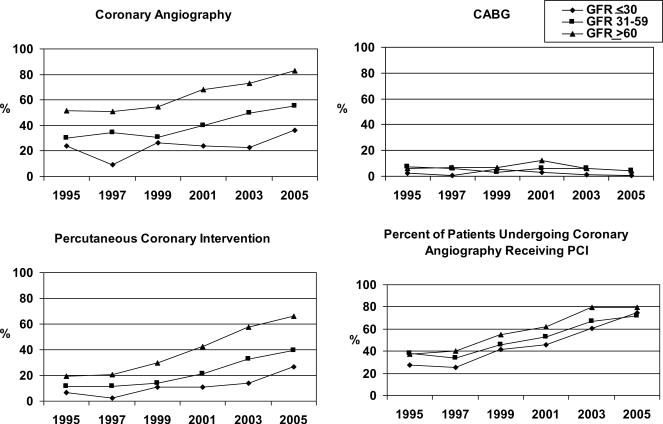
Figure 2.
Trends in the utilization of coronary interventional procedures in 6,219 patients hospitalized with acute myocardial infarction according to degree of kidney function
The utilization of coronary angiography increased over time, albeit to a greater degree among those with preserved rather than impaired renal function (Figure 2). In 2005, 35% of patients with severe chronic kidney disease, 55% of patients with mild-to-moderate chronic kidney disease, and 83% of those with preserved kidney function underwent coronary angiography during hospitalization for acute myocardial infarction. Similar increases in the use of PCI were observed over time in the respective comparison groups. The proportion of patients undergoing coronary angiography who received a PCI also increased in all groups over the decade-long period under study (p<.05). The use of CABG surgery remained relatively stable between 1995 and 2005. In 2005, 4.2% of patients with preserved renal function or mild-to-moderate chronic kidney disease underwent coronary bypass surgery during their index hospitalization as compared to <1% of patients with severe chronic kidney disease.
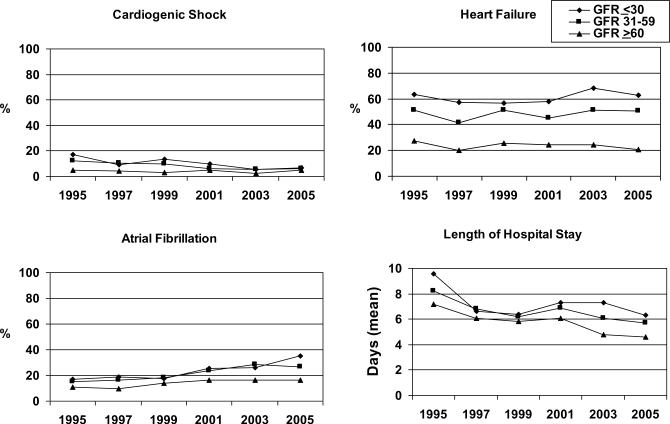
HOSPITAL AND SHORT-TERM OUTCOMES
Compared to patients with preserved kidney function, those with chronic kidney disease were more likely to have longer hospital stays and were more likely to have developed important clinical complications including atrial fibrillation, cardiogenic shock, and heart failure during hospitalization (Table 3). In-hospital and 30-day death rates were significantly higher among patients with chronic kidney disease compared to patients with preserved renal function (Table 3).
After multivariable adjustment, patients with any degree of chronic kidney disease remained at significantly increased risk for developing heart failure and cardiogenic shock compared to patients with preserved kidney function (Table 3). These patients were also significantly more likely to die during hospitalization as well as at 30-days after hospital admission. In a second multivariable regression analysis in which we controlled for the use of various medications and coronary interventional procedures, in addition to previously described demographic and clinical characteristics, attenuation in the odds of developing heart failure and cardiogenic shock during hospitalization was noted as were the odds of dying during hospitalization or in the first 30 days after hospital admission (Table 3). Similar trends were observed when we restricted our analysis to patients hospitalized with acute myocardial infarction at all greater Worcester hospitals during 2003 and 2005 (Table 4).
Table 4.
Length of Hospital Stay and Short-Term Outcomes in Patients Hospitalized with Acute Myocardial Infarction According to Levels of Estimated Glomerular Filtration Rate (eGFR)
| 2003/2005 Study Cohorts | |||||||
|---|---|---|---|---|---|---|---|
| eGFR (ml/min/1.73m2) | eGFR (ml/min/1.73m2) | eGFR (ml/min/1.73m2) | |||||
| Outcomes | ≤30 (n=255) | 31–59 (n=819) | ≥60 (n=974) | ≤30 Adjusted Odds Ratio (95% CI)# | 31–59 Adjusted Odds Ratio (95% CI)# | ≤30 Adjusted Odds Ratio (95% CI)§ | 31–59 Adjusted Odds Ratio (95% CI)§ |
| Length of hospital stay (mean, days) | 6.8 | 6.0 | 4.7* | 2.26 (1.61,3.19) | 1.34 (1.05,1.72) | 3.27 (2.26,4.74) | 1.40 (1.07,1.83) |
| Hospital Complications (%) | |||||||
| Atrial fibrillation | 29.8 | 27.6 | 16.5* | 1.31 (0.89,1.92) | 1.25 (0.95,1.65) | 1.41 (0.94,2.11) | 1.24 (0.93,1.64) |
| Cardiogenic shock | 5.9 | 5.6 | 3.6 | 1.57 (0.75,3.29) | 1.38 (0.81,2.37) | 1.79 (0.81,3.95) | 1.38 (0.80,2.39) |
| Heart failure | 66.3 | 51.0 | 22.8* | 3.04 (2.09,4.41) | 1.88 (1.46,2.43) | 3.09 (2.10,4.56) | 1.86 (1.44,2.41) |
| Death | 21.6 | 11.2 | 4.0* | 4.48 (2.58,7.77) | 2.01 (1.24,3.24) | 2.97 (1.63,5.40) | 1.68 (1.02,2.77) |
| 30-day mortality | 27.8 | 16.0 | 6.1* | 3.95 (2.43,6.41) | 2.00 (1.33,2.99) | 2.73 (1.62,4.59) | 1.72 (1.13,2.63) |
P value ≤0.05
adjusted for age, sex, body mass index, prior history of: angina, hypertension, diabetes, stroke, hypercholesterolemia, heart failure, acute myocardial infarction order (initial vs prior) and acute myocardial infarction type (Q wave vs non-Q wave)
adjusted for variables included in the first multiple regression analysis as well as use of hospital cardiac medications and coronary interventional procedures
Compared to length of stay >median of 5 days
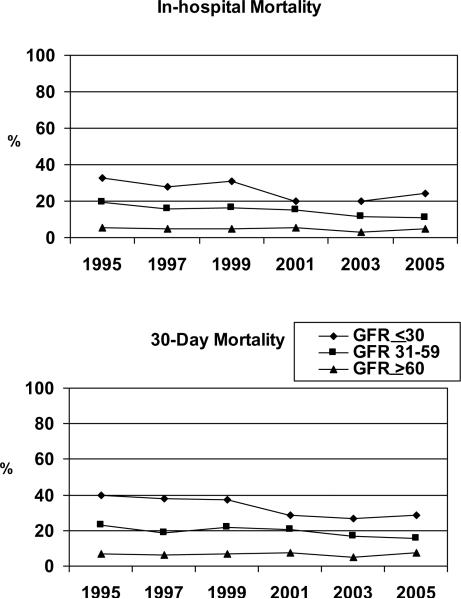
CHANGES IN HOSPITAL AND SHORT-TERM OUTCOMES OVER TIME
During all study years, patients with chronic kidney disease were more likely to have developed heart failure, atrial fibrillation, and cardiogenic shock during hospitalization as compared to patients with preserved renal function (Figure 3). In contrast to patients with preserved renal function, who had no change in short-term mortality noted over time, a significant decline in the in-hospital and 30-day death rates was observed in patients with chronic kidney disease (p<.05, Figure 4). These findings were most pronounced among persons with severe chronic kidney disease. Despite this improvement in short-term survival, patients with chronic kidney disease remained at considerably increased risk for dying after hospitalization for acute myocardial infarction compared to patients with preserved kidney function during the most recent years under study.
Figure 3.
Trends in the incidence rates of in-hospital complications and length of stay in 6,219 patients hospitalized with acute myocardial infarction according to degree of kidney function
Figure 4.
Trends in hospital and 30-day mortality in 6,219 patients hospitalized with acute myocardial infarction according to degree of kidney function
DISCUSSION
Our study examined decade long trends in the use of effective cardiac medications, coronary reperfusion and revascularization strategies, as well as short-term outcomes in a community-based population of patients hospitalized at all Central Massachusetts medical centers with chronic kidney disease and acute myocardial infarction between 1995 and 2005. The use of evidence-based cardiac medications increased over the decade long period under study in all patients with acute myocardial infarction, irrespective of underlying kidney function, with the most profound improvements noted in patients with chronic kidney disease; an effect most prominently observed among patients with the most severe kidney dysfunction. The rates of cardiogenic shock and short-term mortality declined significantly for patients with chronic kidney disease over time. While a trend toward increased use of coronary angiography and PCI was observed in patients with chronic kidney disease, these encouraging trends must be tempered by the fact that patients with impaired kidney function remained less aggressively treated with evidenced-based cardiac medications and coronary reperfusion strategies as compared to patients with preserved kidney function. In addition, patients with chronic kidney disease remained at markedly increased risk for dying and developing clinically significant in-hospital complications compared to those with preserved kidney function.
Previous studies have shown an association between the presence of severe chronic kidney disease, and adverse cardiovascular outcomes after acute myocardial infarction, particularly among those on hemodialysis.2,14 The current study builds on this prior work by demonstrating that patients with mild-to-moderate chronic kidney disease are less likely to be treated with effective treatment strategies than patients with preserved kidney function and are more likely to experience adverse short-term outcomes following acute myocardial infarction. Our data, obtained in a population-based cohort of hospitalized patients, extends the results of prior investigations12,13 by documenting improving trends in the use of effective cardiac medications and intervention strategies in patients with chronic kidney disease.
Renal dysfunction has long been recognized as an important risk factor for cardiovascular disease in general, and for increased morbidity and mortality in patients with acute myocardial infarction.1–5,14–16,21,22 The increased risk of adverse outcomes after acute myocardial infarction remained present in the current investigation, even after adjusting for differences in several baseline characteristics and treatment practices; however, adherence to guideline recommended treatment practices appeared to slightly reduce the odds of dying during hospitalization and at 30 days after hospital admission, though one needs to be careful in interpreting these findings given the nonrandomized nature of the present investigation.
Under-utilization of therapies for acute myocardial infarction in patients with chronic kidney disease has previously been reported and remained evident in our community-based hospitalized patient population.12,13,23 The encouraging trends in the use of various effective treatment regimens were paralleled by improved short-term survival in patients with chronic kidney disease. These findings suggest that the adoption of proven and effective therapeutic measures in patients with chronic kidney disease during hospitalization for acute myocardial infarction may result in an improvement in short-term survival. The nonrandomized, observational nature of our study did not, however, allow for the systematic assessment of the effects of specific cardiac therapies in patients with chronic kidney disease, and it remains unclear which of these therapies may have been associated with particular benefit.
Despite the increased use of coronary angiography and PCI in patients with preserved renal function, as well as in those with chronic kidney disease, no discernible changes in the rates of cardiogenic shock or short-term mortality were observed in patients with preserved kidney function during the period under study. Thus, the increased adoption of effective medical therapies may have had a more important effect on the improved outcomes noted in patients with chronic kidney disease. Caution needs to be exercised in the interpretation of these findings, however, since, when we controlled for the use of cardiac treatment modalities in patients with chronic kidney disease, the absolute values of the adjusted odds of developing heart failure or cardiogenic shock slightly increased in those with more severe chronic kidney disease, raising the possibility of a greater risk of complications associated with certain interventions (e.g., coronary angiography) in these patients.
The mechanisms underlying the association between chronic kidney disease and increased acute myocardial infarction associated mortality are likely to be multifactorial. The occurrence of arrhythmias, hemodynamic disturbances, and left ventricular dysfunction are more common in patients with chronic kidney disease following acute myocardial infarction.4 Endothelial and vascular dysfunction, left ventricular hypertrophy, decreased oxygen carrying capacity, and accelerated underlying atherosclerosis may all contribute to the development of complications in the setting of acute myocardial infarction and mediate the increased morbidity and mortality observed in patients with chronic kidney disease.4, 24,25 Lastly, as documented in previous investigations, patients with chronic kidney disease were older and possessed a greater number of serious co-morbidities than patients with preserved renal function which may have, in part, contributed to their increased risk for dying after acute myocardial infarction.
Further understanding of how these and other non-traditional risk factors4,24,25 play a role in the development of atherosclerosis in patients with chronic kidney disease, and how these factors impact short and long-term prognosis in these high risk patients, will hopefully lead to the development of novel therapeutic strategies aimed at slowing the progression of vascular disease and/or improving the outcomes of chronic kidney disease patients hospitalized with acute coronary syndromes.
Study Strengths and Limitations
The strengths of the present study include our population-based design that included all patients hospitalized with acute myocardial infarction from a well-characterized central New England metropolitan area. The relatively large number of patients hospitalized with acute myocardial infarction, multiple years under study, and the independent validation of each case of acute myocardial infarction are additional strengths of this study. Study limitations include the inability to more systematically measure, and thereby control for, other clinical factors (e.g., hemodynamic instability, degree of vascular stiffness) that may affect or mediate the observed relationship between chronic kidney disease and increased short-term mortality in patients with acute myocardial infarction. Additionally, eGFR was estimated using the admission serum creatinine level. The duration of renal dysfunction and its relationship with outcomes after hospitalization for acute myocardial infarction could not be evaluated from the available data. Due to our methods of data abstraction we were unable to assess the role of provider type (e.g., cardiologist, nephrologist) on patient management practices and related outcomes. We also did not collect more detailed data on the therapeutic management of hospitalized patients, including dosage and frequency of selected medications.
Conclusions
The results of this large community-wide study suggest that while chronic kidney disease continues to negatively impact short-term prognosis after acute myocardial infarction, increased adoption of effective medical treatment regimens and coronary reperfusion/revascularization approaches was noted in patients with renal dysfunction. The most dramatic improvements in the adoption of effective cardiac therapies and in-hospital and 30-day survival rates occurred in patients with severe chronic kidney disease. Our study provides suggestive evidence for the hypothesis that the under-utilization of effective cardiac therapies in patients with renal dysfunction plays a role in mediating the association between chronic kidney disease and increased acute myocardial infarction-related mortality. It remains important to heighten awareness among health care providers, especially primary care physicians, about the association between, and impact of, chronic kidney disease and prognosis after acute myocardial infarction, including the use of targeted educational programs, quality control initiatives, and use of health care reminders. Given the possible increased risk of certain complications associated with the use of various interventional approaches in patients with chronic kidney disease, however, more research remains needed to identify which treatment modalities as well as other factors are associated with enhanced hospital and more long-term outcomes in patients with varying severity of chronic kidney disease to improve the prognosis of these patients.
Acknowledgement
This research was made possible by the cooperation of participating hospitals in the Worcester metropolitan area. Funding support was provided by the National Institutes of Health (RO1 HL35434).
Funding support was provided by the National Institutes of Health (RO1 HL35434).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
There are no conflicts of interest to report on behalf of any of the authors and they all had access to the data and had a role in writing the manuscript.
REFERENCES
- 1.Shlipak MG, Fried LF, Crump C, et al. Cardiovascular disease risk status in elderly persons with renal insufficiency. Kidney Int. 2002;62:997–1004. doi: 10.1046/j.1523-1755.2002.00522.x. [DOI] [PubMed] [Google Scholar]
- 2.Fried LF, Shlipak MG, Crump C, et al. Renal insufficiency as a predictor of cardiovascular outcomes and mortality in elderly individuals. J Am Coll Cardiol. 2003;41:1364–1372. doi: 10.1016/s0735-1097(03)00163-3. [DOI] [PubMed] [Google Scholar]
- 3.Smith GL, Masoudi FA, Shlipak MG, et al. Renal impairment predicts long-term mortality risk after acute myocardial infarction. J Am Soc Nephrol. 2008;19:141–150. doi: 10.1681/ASN.2007050554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright RS, Reeder GS, Herzog CA, et al. Acute myocardial infarction and renal dysfunction: a high-risk combination. Ann Intern Med. 2002;137:563–570. doi: 10.7326/0003-4819-137-7-200210010-00007. [DOI] [PubMed] [Google Scholar]
- 5.Risk of myocardial infarction and death during treatment with low dose aspirin and intravenous heparin in men with unstable coronary artery disease. The RISC Group. Lancet. 1990;336:827–830. [PubMed] [Google Scholar]
- 6.Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of Patients with Acute Myocardial Infarction) 2004 doi: 10.1016/j.jacc.2004.07.014. Available at www.acc.org/clinical/guidelines/stemi/index.pdf. [DOI] [PubMed]
- 7.Antithrombotic Trialists' Collaboration Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. Br Med J. 2002;324:71–86. doi: 10.1136/bmj.324.7329.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Freemantle N, Cleland J, Young P, et al. Beta-blockade after myocardial infarction: systematic review and meta regression analysis. Br Med J. 1999;318:1730–1737. doi: 10.1136/bmj.318.7200.1730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Afilalo J, Majdan AA, Eisenberg MJ. Intensive statin therapy in acute coronary syndromes and stable coronary heart disease: a comparative meta-analysis of randomised controlled trials. Heart. 2007;93:914–921. doi: 10.1136/hrt.2006.112508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.ACE Inhibitor Myocardial Infarction Collaborative Group Indications for ACE inhibitors in the early treatment of acute myocardial infarction. Systematic overview of individual data from 100 000 patients in randomized trials. Circulation. 1998;97:2202–2212. doi: 10.1161/01.cir.97.22.2202. [DOI] [PubMed] [Google Scholar]
- 11.Coca SG, Krumholz HM, Garg AX, Parikh CR. Underrepresentation of renal disease in randomized controlled trials of cardiovascular disease. JAMA. 2006;296:1377–1384. doi: 10.1001/jama.296.11.1377. [DOI] [PubMed] [Google Scholar]
- 12.Menon V, Sarnak MJ, Lessard D, Goldberg RJ. Recent trends in hospital management practices and prognosis after acute myocardial infarction in patients with kidney disease. Am J Cardiol. 2004;94:1290–1293. doi: 10.1016/j.amjcard.2004.07.116. [DOI] [PubMed] [Google Scholar]
- 13.Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003;42:201–208. doi: 10.1016/s0735-1097(03)00572-2. [DOI] [PubMed] [Google Scholar]
- 14.Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35:1044–1051. doi: 10.1016/s0272-6386(00)70038-2. [DOI] [PubMed] [Google Scholar]
- 15.Gibson CM, Pinto DS, Murphy SA, et al. Association of creatinine and creatinine clearance on presentation in acute myocardial infarction with subsequent mortality. J Am Coll Cardiol. 2003;42:1535–1543. doi: 10.1016/j.jacc.2003.06.001. [DOI] [PubMed] [Google Scholar]
- 16.Beattie JN, Soman SS, Sandberg KR, et al. Determinants of mortality after myocardial infarction in patients with advanced renal dysfunction. Am J Kidney Dis. 2001;37:1191–1200. doi: 10.1053/ajkd.2001.24522. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg RJ, Gore JM, Alpert JS, Dalen JE. Recent changes in attack and survival rates of acute myocardial infarction (1975 through 1981). The Worcester Heart Attack Study. JAMA. 1986;255:2774–2779. [PubMed] [Google Scholar]
- 18.Floyd KC, Yarzebski J, Spencer FA, et al. A 30 year perspective (1975–2005) into the changing landscape of patients hospitalized with initial acute myocardial infarction: Worcester Heart Attack Study. Circ Cardiovasc Qual Outcomes. 2009;2:88–95. doi: 10.1161/CIRCOUTCOMES.108.811828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levey AS, Bosch JP, Lewis JB, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 20.K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(2 Suppl 1):S1–266. [PubMed] [Google Scholar]
- 21.McCullough PA, Li S, Jurkovitz CT, et al. chronic kidney disease and cardiovascular disease in screened high-risk volunteer and general populations: the Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Exacute myocardial infarctionnation Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 Suppl 2):S38–45. doi: 10.1053/j.ajkd.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 22.McCullough PA, Li S, Jurkovitz CT, et al. Chronic kidney disease, prevalence of premature cardiovascular disease, and relationship to short-term mortality. Am Heart J. 2008;156:277–283. doi: 10.1016/j.ahj.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 23.Tessone A, Gottlieb S, Barbash IM, et al. Underuse of standard care and outcome of patients with acute myocardial infarction and chronic renal insufficiency. Cardiology. 2007;108:193–199. doi: 10.1159/000096777. [DOI] [PubMed] [Google Scholar]
- 24.Shlipak MG, Fried LF, Crump C, et al. Elevations of inflammatory and procoagulant biomarkers in elderly persons with renal insufficiency. Circulation. 2003;107:87–92. doi: 10.1161/01.cir.0000042700.48769.59. [DOI] [PubMed] [Google Scholar]
- 25.Sarnak MJ, Levy AS. Cardiovascular disease and chronic renal disease: A new paradigm. Am J Kidney Dis. 2000;35(Suppl 4):S117–S131. doi: 10.1016/s0272-6386(00)70239-3. [DOI] [PubMed] [Google Scholar]