Summary
Objectives
Audits in the United Kingdom and other countries show that only a small proportion of eligible stroke patients receive thrombolysis. Providing 24-hour thrombolysis cover presents major challenges in both infrastructure and staffing. One model for improving access is to provide out-of-hours cover in a regional centre but this may present problems including greater delays to hospital admissions.
Design
Evaluation of the introduction of a ‘hub-and-spoke’ model of thrombolysis to increase access to thrombolysis for patients in south west London. One-year data are presented.
Setting
A network in south-west London comprised of a hub hospital and three district ‘spoke’ hospitals.
Participants
All suspected stroke admissions to a regional stroke centre. Main outcome measures Thrombolysis rates for acute stroke.
Results
Increased out-of-hours thrombolysis rates were achieved with only a small increase in stroke admissions (approximately 10%) in the hub hospital. Thrombolysis rates increased from 1.2 per 100 stroke admissions for the local daytime service to 6 per 100 admissions for the regional service. Most patients thrombolysed were not local to the hub hospital. Only 1 in 4 patients considered for thrombolysis was thrombolysed, in line with previous data. Ten percent of all thrombolysis calls were not stroke but represented stroke mimics. Median length of stay was 6 days (target was 3 days). Fifty percent of the thrombolysed patients from spoke hospitals were discharged directly home.
Conclusions
In an urban area, a hub-and-spoke thrombolysis model increased access to thrombolysis without resulting in a marked increase in overall stroke admission numbers for the hub hospital. Proactive plans to repatriate patients back to district hospitals are required, and repatriation protocols have to prioritize regional patients over other targets in spoke hospitals to facilitate capacity in the hub hospital.
Problem
Stroke is a leading cause of death and disability.1 In 2005 the National Audit Office report identified major deficiencies in stroke care across the UK.2 Following this the English National Stroke Strategy was developed and this called for the creation of clinical networks to help deliver on the quality markers identified in this report with a particular focus on hyperacute stroke care.3 A key component of this was access for all stroke patients to thrombolytic therapy with intravenous tissue plasminogen activator (tPA) which has been shown to reduce disability in ischaemic stroke if given within 3 hours, and more recently within 4.5 hours, of stroke onset.4,5 Administration of tPA requires rapidly responsive services with experienced clinicians, and the availability and interpretation of brain imaging to exclude cerebral haemorrhage. In common with many countries, in the UK there are currently insufficient numbers of trained specialists to provide 24-hour cover in all hospitals. A number of approaches have been used to enable 24-hour thrombolysis cover including regional services and telemedicine. Data from a recent systematic review show thrombolysis rates of 2.5–6.9 per 100 strokes for the various models, but there are limited data, and no evidence supporting one model over another.6
Centralizing services in a larger regional centre offers an attractive option, and has been suggested by bodies such as Healthcare for London. However, challenges include potentially increased travelling time delaying administration of treatment, admission of non-stroke patients or ‘mimics’, increased admission rates of patients not suitable for thrombolysis, and repatriation delays.
The thrombolysis rates in south-west London were recognized to be lower than those achievable elsewhere. All hospitals provided daytime thrombolysis services only, and in the hub hospital the rate was 1.2 per 100 stroke admissions. Scoping exercises on expanding the service to out-of-hours in the spoke hospitals showed limited potential due to brain imaging access out-of-hours and insufficient numbers of stroke specialists.
Setting
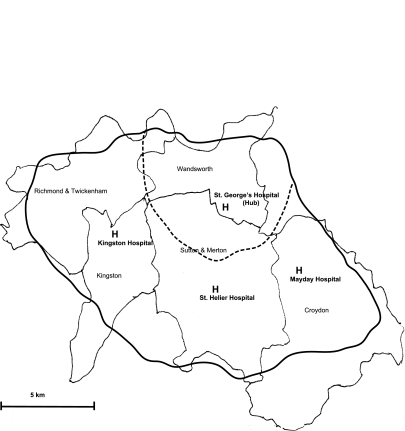
St George's Healthcare NHS Trust (the hub) is a large acute healthcare trust with a tertiary neuroscience centre in south-west London. The partner hospitals (spoke hospitals) are Mayday University Hospital, Kingston Hospital and St Helier Hospital. All the hospitals had pre-existing stroke units. The catchment areas covered by these hospitals are shown in Figure 1.
Figure 1.
Map of hub-and-spoke hospitals. St George's Hospital is the hub and provides a service to the outlying spoke hospitals. The area covered increased from the dashed line (local service) to the solid line (regional service)
Design
A hub-and-spoke model was designed with daytime thrombolysis (09:00–17:00) provided by the local hospital, and out-of-hours and weekend cover provided by the hub hospital. This model was proposed on the assumption that local services, when available, could provide more rapid access to thrombolysis. Initially, all hospitals provided daytime service only (Phase 1). The hub hospital launched a 24-hour service for local patients in September 2007 as part of a planned rollout of the regional thrombolysis service (Phase 2). The regional service started in February 2008, providing extended cover for the three local district general hospitals (Phase 3). From this date an out-of-hours service was provided in the hub hospital for patients assessed as being potentially eligible for thrombolysis. Patients were thrombolysed up to 3 hours from symptom onset. Patients were investigated and treated as appropriate, and those requiring ongoing care were transferred back to their local hospital within 72 hours of being clinically stable. Regular educational meetings were arranged between the network hospitals to discuss cases and provide a governance structure. Data from the first year of the project are presented.
Key measure for improvement
The primary improvement measure was thrombolysis rates. As secondary measures we recorded ambulance transfer times and time to thrombolysis, proportion of patients admitted with non-stroke diagnoses, and speed of repatriation.
Strategies for change
A working party was established chaired by the chief executive of the host Wandsworth Primary Care Trust (PCT) in the region with representation from local commissioners, clinicians and managers from each acute trust, public health and London Ambulance. At an operational level, repatriation protocols and agreements were drawn up by clinicians with local Trust and commissioner approval. Efforts to improve access to thrombolysis focused on examining the patient journey. This was divided into pre-hospital care, acute assessment and repatriation sections. In addition, we addressed workforce needs and governance structures.
Pre-hospital care
London Ambulance Service (LAS) staff were instructed on the Face Arm Speech Test (FAST)7,8 and directed to bring FAST-positive patients (diverts) aged 18–80 years with symptom onset of less than 2 hours (to allow for travel time and scanning) to their local hospital during working hours Monday to Friday, or divert them to the hub hospital at all other times. Emergency Department (ED) staff were educated in all participating hospitals. Stroke thrombolysis was incorporated into the ED teaching programme. Regular feedback was given to both LAS crews and ED staff on successful cases to encourage further referrals.
Acute hospital care
Patients were assessed for thrombolysis by the neurology team in the ED and admitted directly to the Acute Stroke Unit. One bed was always kept free for thrombolysis. Feedback was also given to the radiology department on the outcome of cases. The hub re-assigned six beds to acute stroke from inpatient rehabilitation and opened four more post-acute stroke beds in an offsite neurorehabilitation facility.
Repatriation
A tariff-sharing agreement was in place between the trusts to encourage repatriation. This was split 50–50 between the trusts to account for the higher cost of acute care including imaging. Patients were referred back to the local Stroke consultant and patients were transferred with copies of original brain imaging, medical notes and discharge letters. A stroke navigator was appointed at the hub to facilitate transfers back to the local hospitals.
Workforce
Work practices needed to change for stroke consultants, radiographers and the LAS. Multiprofessional input was fostered with informal and formal feedback sessions. Regular stroke network meetings allowed discussion of cases. There is a clear partnership approach between the hub-and-spoke hospitals based on regular face-to-face communication. Consultants provided support via phone and radiology support for onsite SpRs for all thrombolysis decisions. The medical workforce involved are shown in Table 1.
Table 1.
Staffing of the spoke stroke service. SpR = specialist registrar, an intermediate specialty training grade; Consultant = accredited fully trained specialist
| 09:00–17:00 | 17:00–09:00 and weekends | |
|---|---|---|
| SpR | 2.5 Stroke SpRs | Neurology on call 1 in 12 |
| Stroke consultant/consultant neurologist | Onsite 1 in 4 rota | Offsite 1 in 6 rota |
| Neuroradiology consultant | Onsite | Offsite 1 in 5 rota |
Governance
Prospective data were recorded for evaluation of the pilot. There was a six- and 12-month analysis by the PCT. Data were presented at internal audit meetings and at stroke network meetings. A separate mortality audit was performed. All thrombolysed cases were entered into the European Safe Implementation of Thrombolysis in Stroke Register (SITS, www.acutestroke.org ).
Effects
In the year prior to the regional 24-hour thrombolysis service (Phase 3), there was a daytime service (Phase 1, 7 months) and a local 24-hour service (Phase 2, 5 months). During Phase 1 the mean (SD) number of admissions per month was 58.3 (4.2) and increased slightly to 61.6 (7.1) during Phase 2, and further to 64.3 (6.1) during Phase 3. This represented an increase in admissions of 10% over the local service of one year previously. The proportion of admissions to the hub coming from the catchment areas of spoke hospitals increased from 38.2% when only a local service was operating to 48.5%. Fifty-two percent of the regional patients were from the nominated spoke hospitals, but the remainder were from outside the network. Although the regional service was only planned to operate out-of-hours, 75 regional patients (9.7% of all admissions) were admitted during daytime hours during the pilot year. Of these 75 admissions, 57% were from outside the network.
Demographic details of patients admitted during the pilot are shown in Table 2. Ten percent of total admissions were non-stroke syndromes (or stroke mimics). Median length of stay from admission to discharge from the acute stroke unit was 6 days for both local and regional patients.
Table 2.
Patient demographics. Local and regional patients admitted during the day, local patients admitted out-of-hours, and regional patients admitted out-of-hours during Phase 3. Inpatients, direct admissions from OPD and other hospitals (e.g. for carotid surgery or complex stroke) are excluded from this (n=78)
| Local 09:00–17:00 | Regional 09:00–17:00 | Local out-of-hours | Regional out-of-hours | |
|---|---|---|---|---|
| Patients (n) | 139 | 75 | 202 | 214 |
| Age (median) | 75 | 77 | 72 | 75 (not significant) |
| Men (%) | 47 | 45.9 | 45.5 | 54.6 |
| Time from stroke to A&E in hours (median) | 3.530 | 2.88 | 3.730 | 1.850 (p<0.01) |
| Median LOS on hub stroke unit in days | 6 | 6 | 6 | 6 |
Thrombolysis calls
A total of 190 thrombolysis calls were made to the stroke team during Phase 3 (24.6% of admissions). Nineteen of these were non-stroke diagnoses giving a stroke mimic rate for thrombolysis calls of 10% ( Table 3). Forty-five patients (24%) were thrombolysed with intravenous tPA and one patient received intra-arterial. Reasons for not thrombolysing are shown in Table 4.
Table 3.
Stroke mimic diagnoses (n=19)
| Stroke mimic diagnoses | Cases (n) |
|---|---|
| Seizure | 5 |
| Migraine | 3 |
| Functional | 3 |
| Bell's palsy | 1 |
| Delirium | 1 |
| Brain tumour | 1 |
| Anxiety disorder | 1 |
| Middle cerebral artery aneurysm | 1 |
| CN VI palsy | 1 |
| Possible MS | 1 |
| Cervical myelopathy | 1 |
Table 4.
Reasons patients were not thrombolysed
| Improved | 27 |
| Haemorrhage | 24 |
| Time >3 hours | 21 |
| Unclear time of onset | 17 |
| Age | 13 |
| Seizures | 6 |
| Warfarin | 6 |
| Malignancy | 5 |
| Blood pressure | 3 |
| Recent stroke | 3 |
| Non-stroke | 3 |
| Delayed recognition in A&E | 3 |
| Mild stroke | 3 |
| Migraine | 2 |
| Atrophy | 1 |
| Misdiagnosed | 1 |
| Intra-arterial-tPA | 1 |
| Unstable | 1 |
| Diagnosis unclear | 1 |
| Delayed transfer from referring hospital | 1 |
| Prior intracerebral haemorrhage | 1 |
Thrombolysis rates
While a daytime-only service was operating prior to launching the regional service, thrombolysis rates were 1.2 per 100 stroke admissions. The provision of a local 24-hour local service caused a marked increase in the number of patients thrombolysed (5.4 per 100 admissions). This was slightly enhanced by the regional expansion (6 per 100 admissions). When stroke mimics are excluded, this gives a thrombolysis rate of 6.6 per 100 total stroke admissions. Forty-three percent of patients were thrombolysed between 09:00 and 17:00, 41% were thrombolysed between 17:00 and 24:00 with 15% receiving treatment between midnight and 09:00. Six of the 32 diverts were from outside the network. Fifty percent of the patients thrombolysed from spoke hospitals were discharged directly home. This is consistent with the 40% of patients significantly improved at 24 hours post-thrombolysis in the NINDS trial.4 Fifteen patients were repatriated to their local hospitals. Three patients died.
Ambulance transfer times and time to thrombolysis
There was no delay in seeing regional patients compared with local patients out of hours (Table 2).
Repatriation
A total of 332 regional patients were admitted during the pilot year: 49% of patients went directly home; 25.4% patients were repatriated to spoke hospitals; 9.6% died; and 9.3% went to rehabilitation centres. Twenty percent of the patients had been thrombolysed. Length of stay (LOS) refers to the hub hospital stay only. Median LOS was 9 days for repatriated patients, which was longer than the median LOS of all admissions (6 days).
Median delay from acceptance for transfer by the district hospital to repatriation was 4 days (95% C.I. 2.979–5.628). For the three spoke hospitals (n=56), the median delay was 3 days (mean = 4.3, 95% CI 3–5.6, p = not significant). Although numbers were small, thrombolysed patients were not repatriated quicker than other patients (median 4 days, p= not significant).
Lessons learnt
Implementing a hub-and-spoke model providing 24-hour cover resulted in a marked (up to fivefold) increase in thrombolysis rates with only a modest (approximately 10%) increase in total stroke admissions. A significant service reconfiguration was required to achieve this, involving the Acute Hospital Trust, the ambulance service and spoke hospitals and the support of local commissioners. The commitment to improve services was strong from all participants.
There was concern that transfer of patients from a longer distance would delay thrombolysis but there was no evidence of this, although the situation may differ in a more rural setting.
We relied on the ambulance service using a validated screening tool to identify patients with stroke. Approximately 10% of patients did not have stroke, presenting with a variety of other diagnoses.
Providing a superior service attracts more admissions from areas bordering the usual catchment area. Some of the increase in admissions is due to admissions coming from outside the network due to ambulance staff diverting patients to our centre for thrombolysis. This is a consequence of the density of hospitals in the London area and the opportunity for individuals, and ambulance crews, to preferentially refer to centres where they feel the care may be better. Some of the surrounding regions had limited thrombolysis services during the period of this evaluation.
Maintaining free beds to receive thrombolysis patients was problematic at times. This depended on rapid repatriation of patients back to their spoke hospital stroke units. If a spoke hospital stroke unit is full, accepting the hub patient is delayed with the result of reduced capacity in the hub for managing local stroke patients. Proactive management of repatriation proved key to running this service model, and we found it helpful to identify patients who will require repatriation at the time of admission to the stroke unit, rather than waiting for stabilisation on day 2 or 3. Nevertheless, we missed our target of repatriation within 3 days. In addition, where patients may have been discharged directly home within the first week, they were usually kept in the hub until discharge or repatriation, which increased our overall time to repatriation.
All UK acute hospitals have nationally set ED targets and hospitals are penalised if emergency admissions wait in the ED longer than 4 hours before being transferred to a hospital bed. Our repatriation policy did not supersede these targets and, therefore, repatriation was sometimes delayed when spoke hospitals had bed pressures. We tried to discharge patients directly home whenever possible but used an escalation policy when required to prioritize repatriation over competing demands for beds. We did not have a penalty system for delays in repatriation and the split tariff may have reduced the incentive for spoke hospitals to accept patients for repatriation.
One potential limitation of a study looking at two sequential patterns of care is that other factors external to the intervention could have accounted for some of the changes. In particular thrombolysis depends on public awareness of the symptoms of stroke. There has been a recent National FAST public awareness campaign which could have influenced our results but this was launched the week after our pilot stopped and, therefore, did not influence our results.
Discussion
The principal finding from our pilot is that the hub-and-spoke model improves access to thrombolysis for regional patients. This quality improvement was achieved with a modest increase in total admissions. A recent systematic review compared thrombolysis rates for five different service configurations including local services, redirection of patients to stroke centres and the use of telemedicine services.6 The authors concluded regional collaborations were superior to local provision as thrombolysis rates were significantly higher than in local services. The hub-and-spoke model allows more patients to have access to thrombolysis while minimizing the increase in workload for the hub hospital, and allowing care closer to home for the majority of stroke patients.
There are several factors that we think were important to this project and that are transferable to other projects:
Evidence-based medicine: Thrombolysis is the only licensed treatment for acute ischaemic stroke. There is considerable evidence regarding its efficacy and safety. Trying to implement change where the evidence is less clear-cut would be more challenging;
Clinical leadership: The stroke physicians in both hub and spoke hospitals wanted to improve care. This non-competitive collaboration greatly facilitated overcoming resistance to change. The thrombolysis service is consultant delivered and all decisions are peer-reviewed at a weekly meeting that provides consistency of service delivery;
Communication and training: The service change required change in work practices across the network hospitals. Regular positive feedback to all groups leading to shared ownership of the new service helped move it from pilot project to the de facto service model. Ongoing training to ambulance and A&E staff support the ongoing delivery of the service;
Audit: A driver for this came from data showing a low baseline thrombolysis rate. Implementation of service delivery change requires regular audit. The data from the audit were presented within the acute trust and in the stroke network. Mortality data and thrombolysis data (including national register) throughout the pilot provided participants with positive feedback and would have identified concerns at an early stage.
The timely delivery of thrombolysis in acute stroke reduces disability and improves outcomes.4 Our data suggest that a hub-and-spoke model can increase thrombolysis rates while limiting the increase in admissions to the hub hospital.
Footnotes
DECLARATIONS —
Competing interests None declared
Funding None
Ethical approval Not applicable
Guarantor BM
Contributorship All authors contributed equally
Reviewer Ian Reckless
Acknowledgements
None
References
- 1.MacKay J, Mensah G . The atlas of heart disease and stroke . Geneva: : World Health Organization; ; 2004 [Google Scholar]
- 2.National Audit Office Reducing Brain Damage: Faster access to better stroke care. London: NAO; 2005 [Google Scholar]
- 3.Department of Health National Stroke Strategy. London: Department of Health; 2007 [Google Scholar]
- 4.Tissue plasminogen activator for acute ischemic stroke. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. N Engl J Med 1995;333:1581–7 [DOI] [PubMed] [Google Scholar]
- 5.Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317–29 [DOI] [PubMed] [Google Scholar]
- 6.Price CI, Clement F, Gray J, Donaldson C, Ford GA. Systematic review of stroke thrombolysis service configuration. Expert Rev Neurother 2009;9:211–33 [DOI] [PubMed] [Google Scholar]
- 7.Nor AM, McAllister C, Louw SJ, et al. Agreement between ambulance paramedic- and physician-recorded neurological signs with Face Arm Speech Test (FAST) in acute stroke patients. Stroke 2004;35:1355–9 [DOI] [PubMed] [Google Scholar]
- 8.Harbison J, Hossain O, Jenkinson D, Davis J, Louw SJ, Ford GA. Diagnostic accuracy of stroke referrals from primary care, emergency room physicians, and ambulance staff using the face arm speech test. Stroke 2003;34:71–6 [DOI] [PubMed] [Google Scholar]