Abstract
We evaluated the efficacy of a gender-specific intervention to reduce sexual risk behaviors by introducing female-initiated methods to urban women with severe mental illness. Seventy-nine women received 10 sessions of an HIV prevention intervention or a control intervention. The primary outcome was unprotected oral, anal, or vaginal intercourse, expressed using the Vaginal Episode Equivalent (VEE) score. Knowledge and use of the female condom were also assessed. Women in the HIV prevention intervention showed a three-fold reduction in the VEE score at the 3-month follow-up compared to the control group, but the difference was not significant. These women were significantly more likely to know about female condoms, have inserted one and used it with a sexual partner at the 3-month follow-up and to have inserted it at 6 months compared to controls. The female condom may be a useful addition, for a subset of women with SMI, to comprehensive HIV prevention programs.
Keywords: Severe mental illness, HIV prevention, Women, Female condoms, Pilot test
Introduction
More than two decades into the AIDS epidemic, the prevalence of HIV infection continues to rise among women in the United States. Those who live with severe mental illness (SMI) constitute a group disproportionately affected by the epidemic. Estimates of HIV prevalence among people with SMI average 6.9% (Krakow et al. 1998; McKinnon et al. 2002; Rosenberg et al. 2001b). The relationship between HIV infection and severe mental illness is evident among Medicaid recipients as well as members of rural communities (Blank et al. 2002; Rosenberg et al. 2001a).
Risk for HIV infection among people with SMI has been associated with psychiatric symptom profile (McKinnon et al. 2001; Meade 2006) and cognitive impairment (McKinnon et al. 2002; Meade and Sikkema 2005); co-morbid substance use (McKinnon et al. 2001; Meade 2006; Meade and Sikkema 2007; Parry et al. 2007; Rosenberg et al. 2001b); history of childhood physical and sexual abuse (Devieux et al. 2007; Meade et al. 2009; Meade and Sikkema 2007); history of infection with a sexually transmitted disease (Vanable et al. 2006); relationship status (Meade 2006); type of treatment setting (Wright and Gayman 2005); inadequate assessment of personal risk (Kloos et al. 2005); multiple sexual partners, unprotected sex, and transactional sex (McKinnon et al. 2002; Meade and Sikkema 2005) and interactions among these factors. Questions remain regarding the epidemiology of HIV infection among people with SMI who live outside the epicenters of the epidemic; prevalence differences among diagnostic subgroups; as well as the intersecting social networks of people with SMI, injection drug users, and other high prevalence groups (Walkup et al. 2008). Similarly, gender-specific risk and prevention require further study.
Women with SMI face a particular set of challenges. They are more likely to be sexually abused as children and to report adult sexual abuse than men with SMI (Meade et al. 2009). Women with limited social support networks may be particularly vulnerable to these HIV risk factors (Randolph et al. 2007). Otto Salaj et al. (1998) identified female gender, specifically, as a predictor of HIV risk. Women in their study sample had lower self esteem; reported more frequent exchange of sex for money, food, or housing; less intention to reduce HIV risk behavior; more frequent unprotected vaginal intercourse; and were less likely to perceive HIV risk as a “function of their internal control”.
Encouragingly, three HIV prevention studies that included women and men and analyzed the effects of gender found that women with SMI showed more responsiveness to the elements of behavioral risk reduction interventions than men (Carey et al. 2004; Kalichman et al. 2005; Otto-Salaj et al. 2001). Kalichman et al. (2005) tested the Information-Motivation-Behavior Skills (IMB) model and showed that women with SMI reported more positive attitudes and demonstrated more skill in applying male condoms than men. Positive attitudes and condom self-efficacy were associated with less unsafe sex (Kalichman et al. 2005). Yet, female gender also predicted unprotected sex. In another study, although women reported greater use of the male condom and a greater percentage of condom-protected sexual episodes, there was not a “sharp or sustained decrease in rates of unprotected sex” (Otto-Salaj et al. 2001).
Several factors may account for women’s continued sexual risk despite their willingness to use male condoms. Complex socio-cultural factors often constrain women’s ability to negotiate safer sex (Amaro 1995; Fullilove et al. 1990; Mays and Cochran 1988). The dynamics of intimate relationships, socioeconomic factors, gender-based power differentials and male-perpetrated violence against women merit special attention (Amaro and Ray 2000; Pulerwitz et al. 2002). Integrating sexual assertiveness training into an HIV risk reduction intervention for women has shown promising results in prevention interventions aimed at shifting gender power dynamics (Otto-Salaj et al. 2001; Weinhardt et al. 1998). In a pilot trial of 20 participants, Weinhardt et al. (1998) showed that women who received assertiveness training increased the amount of protected intercourse 2 months after the intervention, but found no significant group differences in the frequency of unprotected intercourse. An additional strategy for risk reduction is to offer women with SMI preventive options, such as the female condom, that can increase their choices for self-protection and provide an alternative to the male condom.
The female condom is currently the only female-initiated barrier method of protection from HIV infection. Female condoms have been found effective in increasing protected sex and decreasing the incidence of sexually transmitted infections among women while enabling women to “act on their own behalf” for self-protection (Gollub 2000). Furthermore, presenting women with choices for risk reduction that include the female condom leads to increased protection during sexual intercourse (Gollub et al. 2001). Specifically, female condom use allows women at high risk for HIV infection, who use male condoms inconsistently, to have fewer episodes of unprotected sexual intercourse by using a combination of barrier methods over time (Hardwick 2002; Macaluso et al. 2000).
Investigators have examined predictors of use of the female condom among diverse populations of urban women with mixed results. Study findings appear to be dependent on sample characteristics. Sly et al. (1997) found that among black, Hispanic, and white women, regular female condom use was associated with being black or Hispanic, age younger than 25, and being single. Trying the device was associated with living with a partner, having a previous HIV test, being black or Hispanic, having a history of sexually transmitted infection, and lack of prior knowledge of the device. Similarly, among urban women exchanging sex, female condom use was related to having a regular partner and not being homeless. Additional factors increasing use were active drug use, living with someone abusing substances, and having discussed the devise with other women or a regular sex partner (Witte et al. 1999). Holmes et al. (2008) showed that African American women without knowledge of the female condom were less likely to use it, but that women with multiple partners, high school education or more, and younger age, were more likely to use it. Qualitative and quantitative studies of women at high risk report that women liked the idea of perceived personal control and increased sexual pleasure for women and men associated with female condom use (Hirky et al. 2003; Klein et al. 1999). Physical discomfort on insertion and displeasing appearance were disadvantages (Hirky et al. 2003; Klein et al. 1999). In summary, use of the female condom may depend considerably on social context, age, partner’s response to the device, as well as knowledge and previous history of female condom use. Little is known about attitudes toward female condom among urban women with SMI living in community settings.
Project Wisdom
Project Wisdom was a mixed methods intervention study that investigated individual and contextual factors that place women with SMI at risk for HIV infection. Collins and colleagues (2001) developed a gender-specific, 10-session HIV prevention curriculum, “Ourselves, Our Bodies, Our Realities,” that introduced female and male condoms to women with SMI and assisted them in developing skills to use them. A preliminary test of this intervention showed that women who received the intervention had more positive attitudes toward the female condom 6 weeks after the intervention than women in the control group (Collins et al. 2001). This small trial focused on hospitalized women, did not examine behavioral outcomes, and did not use an attention-matched control.
In preparation for testing the intervention among women living in the community, we conducted qualitative research among urban women with SMI in order to understand the intersecting influence of gender, ethnicity, poverty, and mental illness on relationship opportunities and sexual risk situations among women (Collins et al. 2008b). We revised the curriculum to include greater attention to assertiveness and negotiation skills in tandem with information on the female condom and the male condom.
In this paper, we report the results of a pilot evaluation of the efficacy of the HIV prevention intervention “Ourselves, Our Bodies, Our Realities,” using sexual behavior outcomes 3 and 6 months after the intervention. We also report knowledge, use and attitudes toward the female condom by intervention group at baseline and follow-up. We tested the hypotheses that women with SMI who received the HIV prevention intervention would (1) reduce their sexual risk behaviors; (2) demonstrate an increase in knowledge of the female condom, insertion of the female condom, and use of the female condom with a partner; and (3) and have more positive attitudes toward the female condom over the 6 months following the intervention compared to women in the control group.
Methods
Participants
We recruited women age 18 and older from two residential facilities and 4 day treatment programs in New York City. These facilities were chosen in order to sample women living with SMI in an urban community setting. The research team visited each site and described the study to the site staff and to the women receiving services. The team screened women who expressed interest in the study and had the capacity to give informed consent. Clinicians at each site assessed the women for psychiatric symptoms that would preclude them from providing informed consent. At the screening interview, women were deemed eligible to participate if they had SMI (any psychotic disorder or major affective disorder), were sexually active in the last 3 months, and had the capacity to give informed consent. Women who were eligible and interested in study participation completed a baseline assessment. Participants received $5 for completing the screening interview, $30 for completing the baseline assessment, and $15 for each follow-up assessment. The Institutional Review Boards at Columbia University Medical Center, the New York State Psychiatric Institute, and Harlem Hospital Center approved the study.
Interventions
HIV Risk-Reduction Intervention: “Ourselves, Our Bodies, Our Realities” (HIV)
“Ourselves, Our Bodies, Our Realities” is a 10-session gender specific intervention for women with SMI living in community and institutional settings (Collins et al. 2001). Collins and colleagues developed the curriculum by taking into account the social context in which urban women with SMI live. The curriculum emphasizes the theme of autonomy and the use of female-initiated HIV/sexually transmitted infection (STI) prevention methods. The theoretical foundation is social cognitive theory, with a focus on self-efficacy and skills training. In particular, we emphasize these components of behavioral change described by Bandura: an informational component as well as development of self protective skills and enhancement of self-efficacy through modeling and role play (Bandura 1994). The skills-building component also derives from the psychiatric rehabilitation literature on social skills development, which emphasizes a focus on targeted skills, demonstration, and practice (Wallace 1998).
The intervention is presented in the form of a television talk show, The Daphne Darling Show, in order to provide an engaging program that captures the attention of women who may have cognitive impairments. The two facilitators play the role of the talk show host, Daphne Darling, and the program’s expert, Professor Private Parts. The women form the talk show audience and guests.
In the course of the ten sessions of the intervention the facilitators use role-playing, interactive games, group discussions, and problem solving techniques. The sessions sequentially address (1) basic HIV and STI information, assessment of personal risk, and familiarity with sexual terms; (2) sexual anatomy; (3) the consequences of sexually transmitted diseases, myths about disease transmission for HIV and other STIs, and risk assessment of specific sexual acts; (4) a review of HIV prevention methods and contraceptive options; (5) asserting oneself and negotiating sexual encounters safely; (6) information about and demonstration of the female condom; (7) group members’ experiences using the female condom and discussion of attitudes that hinder self-protection; (8) information about and demonstration of the male condom; (9) overcoming obstacles to self-protection using problem-solving and role plays; and (10) making a commitment to self protection and practicing an AIDS prevention message to present to the Daphne Darling audience. The intervention ends with a graduation ceremony.
Control Intervention: Money Management
A control intervention matched for time and attention provided participants with a 10-session workshop on making their money last through the month. The money management intervention introduces three steps to money management (know your money, know how to keep your money, and know how to live with what you have). The ten sessions sequentially (1) review basic skills required for money transactions; (2) help participants understand their entitlements and identify all sources of income; (3) teach use of the banking system; (4) review check cashing practices and selecting appropriate bank accounts; (5) help participants to weigh the best ways of keeping cash safe; (6) review bill payment and the prioritization of expenses; (7) teach how to budget for monthly expenses; (8) focus on tips for saving and adherence to a budget; (9) address credit card use and approaches to developing a will. The money management intervention concludes in session 10 with a review of the money management steps and a graduation ceremony.
Facilitators
All group sessions were led by two master’s- or doctoral-level female facilitators. The same facilitators administered intervention and control sessions in any given wave. This allowed us to minimize effects due to different facilitator styles. Facilitators subjectively rated the success of each group following the group session.
Intervention Administration
Women randomized to the HIV prevention or control intervention entered groups consisting of 5–10 participants. In each facility, group sessions were integrated into the weekly schedule of group activities. Group sessions lasted 50 min. Both the intervention and control groups met twice a week for 5 weeks, for a total of 10 sessions. Women received $5 for each session attended. Each group session began with a lottery prize drawing and a self-esteem exercise. All sessions were video- and audio-taped.
We presented the experimental and control interventions in a total of six waves. Sixteen women were included in wave 1, followed by 17 in wave 2, 10 in wave 3, 10 in wave 4, 13 in wave 5, and 13 in wave 6.
Interviewers
Research team interviewers were required to attend a sexual desensitization and interviewer training course sponsored by the HIV Center for Clinical and Behavioral Research at the New York State Psychiatric Institute. Interviewers were subsequently trained to administer the assessment instruments. This training included audiotaped rehearsal of interviewing non-patient volunteers with supervision by the HIV Center. All interviewers were female and were blind to treatment condition.
Randomization
When baseline assessments at a given study site were completed, a statistician performed a block randomization procedure and notified the study director of the participants’ assignment to the HIV prevention intervention or money management intervention. A research assistant notified women of their group assignments and gave instructions for study participation during a group meeting at the site.
Outcome Measures
Demographic and Diagnostic Outcomes
Demographic information that included participants’ age, ethnicity, marital status, level of education, religious affiliation, description of residence, and money management practices was collected. We assessed psychiatric diagnoses using the Structured Clinical Interview for DSM-IV Diagnosis (SCID), a semi-structured instrument designed to yield DSM-IV diagnoses (Williams et al. 1992).
Main Outcomes: Sexual Risk Behavior
The primary outcome of the study was sexual risk reduction. Sexual risk behavior was ascertained using the Sexual Risk Behavior Assessment Schedule for mentally ill sheltered women (SERBAS-A-MIS-F) (Meyer-Bahlburg et al. 1991), which has been shown to be reliable in risk reduction studies of people with SMI (McKinnon et al. 1993; Sohler et al. 2000). Risk behavior data include the number, sex, and type (e.g., casual, steady, exchange) of sexual partners over the previous 3 months; the types of sexual acts performed at each encounter (vaginal, anal, and oral); whether sexual acts were male or female condom protected or whether other non-barrier methods of contraception were used; whether sex was bought or sold; and the risk behaviors of sexual partners. History of coercive sex and the obstetric and gynecologic history of the participant were also collected.
The a priori outcome variable was the Vaginal Episode Equivalent (VEE) score (Susser et al. 1998). The VEE score assigns a greater weight to unprotected anal sex (2 points) than unprotected vaginal sex (1 point), and also allows for some contribution from unprotected oral sex (0.1 point). Counts of unprotected vaginal, anal, and oral sex are used to calculate the Vaginal Episode Equivalent (VEE) score. To compute a VEE score, one simply sums VEE points for various types of unprotected sex including anal, vaginal, and oral sex with men. Additional outcomes included total number of unprotected episodes of vaginal and anal intercourse, knowledge of the female condom, insertion of the female condom, use of the female condom with a partner, and attitudes and method-specific efficacy for the female and male condoms.
Condom Knowledge and Attitude Outcomes
The Subjective Norms of Women-Controlled Methods (SNOW-CM) was developed to assess subjective norms, attitudes, and intentions to use the male condom and the female condom (see Collins et al. 2001). The data collected included women’s familiarity with and use of female and male condoms, HIV testing and sexually transmitted infection history, attitudes and method-specific efficacy for the female and male condom, specific behavioral intentions to use male and female condoms, and general self-efficacy, and sexual communication. In this manuscript, we restrict our findings to subscales with Cronbach’s alpha greater than 0.6, and thus report on the attitudes and method-specific efficacy subscale for the female and male condom.
Women were asked if they knew there was a female condom (yes or no), whether they had ever tried to insert a female condom (yes or no), whether they had used a female condom with a partner (yes or no), and the number of times they used the female condom (never, once, 2–4, 5 or more). Women were asked if they had ever been tested for HIV (at baseline) (yes or no) or tested in the past 3 months (3- and 6-month follow-up). At baseline women were asked if they had ever had a sexually transmitted infection (yes or no), and at each follow-up assessment, whether they had a sexually transmitted infection in the past 3 months.
Fifteen items assessed women’s attitudes toward and method-specific efficacy for the female condom. Participants were asked to rate, on a four-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree), how much they agreed with each item. Items included, “Using a female condom is too much trouble,” “Using female condoms is embarrassing,” “I would be able to insert a female condom,” and “I would be able to tell my sexual partner that I would like to use a female condom.” Items were recoded such that higher scores represented more positive attitudes and efficacy. The Cronbach alpha for this scale was .84 calculated from data with the current study sample.
Twelve items assessed women’s attitudes toward and method-specific efficacy for the male condom. Participants were asked to rate, on a four-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree), how much they agreed with each item. Items included, “Using a male condom is too much trouble,” “Using a male condom is an excellent way of protecting myself against STDs and HIV,” “Asking a man to use a male condom is embarrassing,” and “You would be able to ask a sexual partner to use a male condom during vaginal or anal sex.” The Cronbach alpha for this scale was .79 calculated from data with the current study sample.
Data Collection
Data collection occurred at baseline, 3 and 6 months after the intervention. At each follow-up point interviewers administered the SERBAS, an assessment of money management skills, and the SNOW-CM.
Statistical Analysis
Sexual Risk Behavior Outcomes
A modified “intention to treat” principle was followed for analysis of the main outcome. That is, data from 79 women notified of their group assignment to the intervention or control group were analyzed according to original group assignment, regardless of whether the women completed the intervention or the follow-up. Data for women lacking complete follow-up were imputed using a multiple imputation scheme based on an urn model. Eleven replications of the imputation scheme were performed. The most conservative—that associated with the median t-test statistic for intervention versus control group difference—was chosen. The primary data analysis was a t-test comparing 3-month VEE scores, intervention versus control, with no adjustment for covariates.
We performed three secondary analyses of intervention effect on sexual behavior. First, the interaction between intervention group assignment and time (baseline, 3-month follow-up or 6-month follow-up) as a predictor of unprotected anal and vaginal episodes was examined using a generalized estimating equation (GEE) with a Poisson distribution. Second, a dose–response analysis using GEE was conducted to determine whether number of group sessions attended predicted unprotected anal and vaginal episodes at each follow-up.
Third, acknowledging that the study was underpowered for conducting a dose–response analysis using GEE, a main effect for dose was tested at each follow-up time point in two ways. For the first method control participants and any experimental participants who did not receive any sessions were coded as zero. In order to ensure adequate cell-sizes and not sacrifice statistical power, the “sessions” variable was turned into a categorical variable. Analyses were run twice, once with number of sessions attended categorized into 4 levels (0; 1–3; 4–6; 7–10 sessions), the second time with sessions as a dichotomous variable (0–3; 4–10 sessions). The rationale for the 0–3 versus 4–10 session breakdown was drawn from a review by Exner and colleagues which suggested that exposure to 4 sessions was associated with behavior change across a number of studies (Exner et al. 1997). Given the distribution and nature of the data, Kruskal–Wallis and Mann–Whitney tests were run to compare the median number of unprotected vaginal and anal episodes between the 4 and 2 session categories, respectively, for both the 3- and 6-month follow-up time points. For the second method of exploring a possible dose–response relationship between session attendance and episodes of unprotected vaginal and anal sex, intervention group assignment was disregarded and participants were aggregately categorized based on the number of sessions they attended. Again, a Kruskal–Wallis test was run for the 4-level (0; 1–3; 4–6; 7–10), and a Mann–Whitney for the 2-level (0–3; 4–10) “sessions” variable.
Condom Knowledge and Attitude Outcomes
The association between treatment group assignment and knowledge and experience with the female condom was examined using chi square tests at each time point (baseline, 3-month follow-up, and 6-month follow-up). Using hierarchical ANOVA we examined the relationship between treatment group assignment and attitudes and method-specific efficacy for the male and female condoms at each follow-up, using baseline values as a covariate in each model.
Results
Participant Flow
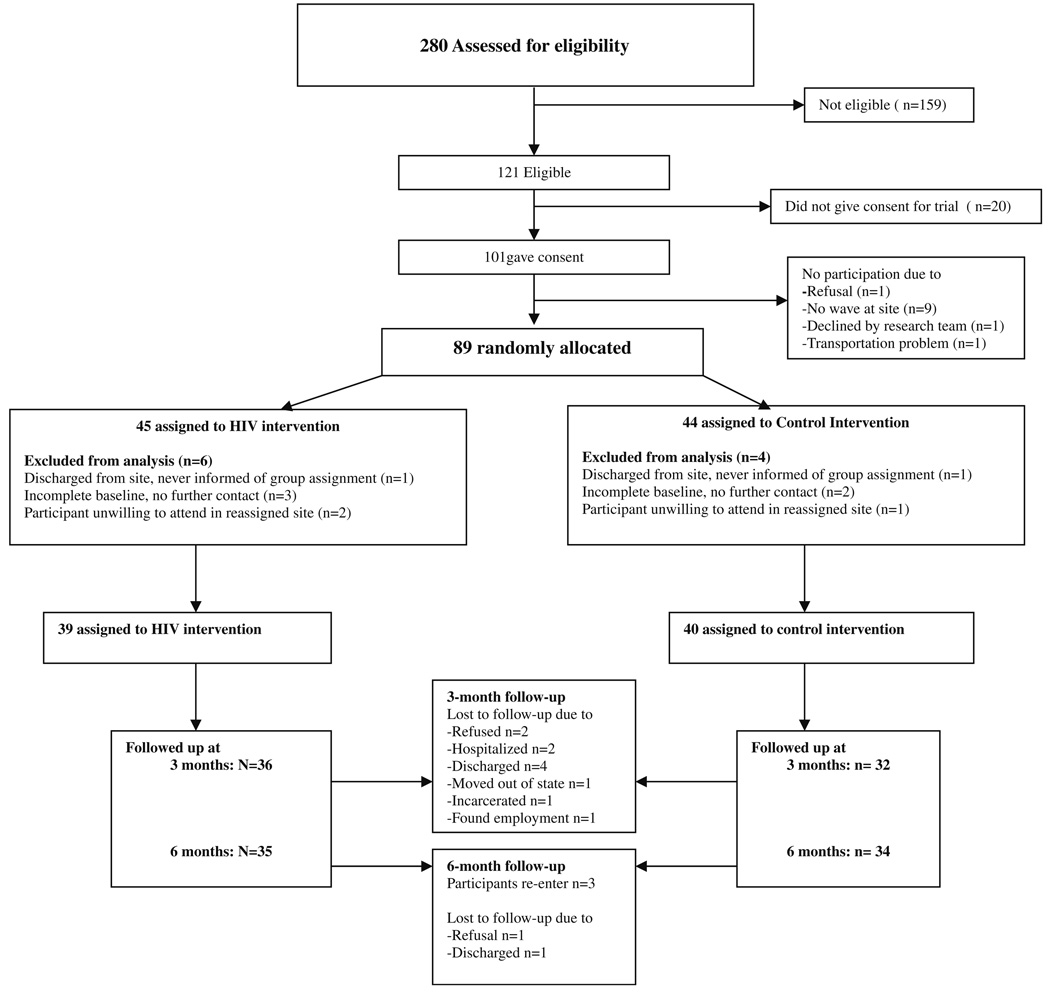
The study was conducted between March 2001 and April 2003. Of the 280 women screened, 121 (43%) were eligible to participate in the trial based on reported sexual activity and a preliminary screening of psychiatric diagnosis. Of those eligible, 101 (83%) gave consent to enter the trial and 89 women were randomized to the HIV or control interventions. Of these, ten women were later eliminated from the analysis because they did not contribute data due to (1) their discharge from the study site before receiving their group assignment, (2) inadvertent inclusion in the randomization although baseline assessments were incomplete (these women had no further communication with the research team), or (3) refusal to attend the group sessions in the designated location. This last category included three women who declined group participation when told that groups would occur at a facility near their program. The study sample comprised the remaining 79 women, 65% of those eligible. Sixty-eight and 69 women completed the 3-month follow-up and 6-month follow-up assessments, respectively (Fig. 1).
Fig. 1.
Project wisdom random allocation of study participants and participant flow
Intervention Session Attendance
Seven women, two assigned to the HIV intervention and 5 assigned to the control intervention, did not attend any session. Thirty-four (89.5%) women attended five or more sessions of the HIV group. Twenty-nine (72.5%) women attended 5 or more of the money management sessions.
Demographics
Table 1 shows baseline demographic data for the sample. Of the 79 participants, the majority was Black or Latina, had never been married, had a high school education or less, and had a psychotic disorder. The HIV and control groups differed in marital status and income distribution, with more women in the control group represented among the never married and the lower income groups. A baseline difference in education was also found χ2 (1, N = 79) = 3.79, P = .051; fewer women in the control group completed high school. These group differences were also present among the N = 89 women who were initially randomized.
Table 1.
Characteristics of 79 women participating in the Project Wisdom Pilot Study
| HIV intervention group Mean (SD) |
Money mgt group Mean (SD) |
Total | |
|---|---|---|---|
| Age (years) | 42.8 (8.7) | 41.7 (7.8) | 42.3 (8.3) |
| N (%) | N (%) | N (%) | |
| Race/ethnicity | |||
| Black | 19 (49) | 29 (72.5) | 48 (61) |
| Latina | 11 (28) | 5 (12.5) | 16 (20) |
| White | 5 (13) | 4 (10) | 9 (11) |
| Other | 4 (10) | 2 (5) | 6 (8) |
| Education | |||
| Less than 12th grade | 12 (31) | 22 (55) | 34 (43) |
| 12th grade or GED | 13 (33) | 12 (30) | 25 (32) |
| Greater than 12th grade | 14 (36) | 6 (15) | 20 (25) |
| Marital status* | |||
| Never married | 14 (37) | 28 (70) | 42 (54) |
| Married | 5 (13) | 2 (5) | 7 (9) |
| Divorced | 9 (24) | 4 (10) | 13 (17) |
| Separated | 9 (24) | 3 (7.5) | 12 (15) |
| Widowed | 1 (3) | 3 (7.5) | 4 (5) |
| Children | |||
| No | 13 (33) | 11 (28) | 24 (31) |
| Yes | 26 (67) | 28 (72) | 47 (69) |
| Ever worked | |||
| No | 2 (5) | 7 (17.5) | 9 (11) |
| Yes | 37 (95) | 33 (82.5) | 70 (89) |
| Annual income* | |||
| Under $8,000 | 8 (21) | 11 (28) | 19 (25) |
| $8,000 to $11,999 | 17 (45) | 24 (62) | 41 (53) |
| $12,000 or more | 13 (34) | 4 (10) | 17 (22) |
| Diagnosis | |||
| Schizophrenia | 14 (37) | 25 (62) | 39 (50) |
| Schizoaffective/Psychosis NOS | 7 (18) | 4 (10) | 11 (14) |
| Mood disorder with psychosis | 6 (16) | 4 (10) | 10 (13) |
| Mood disorder without psychosis | 11 (29) | 7 (18) | 18 (23) |
| Lifetime substance abuse, use or dependence | |||
| No | 12 (32) | 6 (15) | 18 (23) |
| Yes | 26 (68) | 34 (85) | 60 (77) |
| Current substance use (past month) | |||
| No | 34 (89) | 37 (92.5) | 71 (91) |
| Yes | 4 (11) | 3 (7.5) | 7 (9) |
| Living in unsupervised housing done | |||
| No | 28 (72) | 25 (62.5) | 53 (67) |
| Yes | 11 (28) | 15 (37.5) | 26 (33) |
Baseline differences in income and marital status between the two groups achieved significance at the P < .05 level using Chi square
Baseline Sexual Behavior and Risk factors for HIV
Thirty-three women (42%) reported having no unprotected oral, vaginal, or anal sex in the 3 months prior to the study. The majority of the sample reported one or more episodes of unsafe sex in the previous 3 months. Seventeen women (21.5%) had at least one episode of unprotected oral, vaginal or anal sex, and 29 women (36.7%) had not used any protection during sex in the previous 3 months. Forty-nine women (62%) reported having been forced to have sex with a man during their lifetime, and 8 women (10.1%) reported forced sex with a woman. Nearly half of the women (45%) reported ever having a STI. The majority (73 of 78) women had received an HIV test in the past.
Sexual Risk Behavior Outcomes
Women in the HIV intervention had a mean VEE score of 9.94 (SD = 43.23) 3 months following the intervention, compared with a VEE score of 31.89 (SD = 146.94) among women in the control intervention (Table 2). The increased VEE score in the control group at the 3-month follow-up can be attributed to high scoring outliers in the sample. Using an intent-to-treat analysis comparing mean VEE scores of the HIV and control groups revealed no significant difference between groups (t = −.905; P = .37). At the 6-month follow-up, the VEE score for women in the intervention group was greater than the baseline score and slightly higher than that of the control group, though not significantly different. The GEE approach showed there was no significant effect of the treatment over time for either group, but the positive parameter estimate for the 3-month follow-up indicates an increase in the incidence of unprotected anal and vaginal sex in the control group at 3 months compared to baseline (Table 3). Using a GEE model that controlled for sessions, treatment group and time, session attendance in both groups was associated with less unprotected anal and vaginal sex (Estimate −.282; Standard Error, 0.087; 95% Confidence Intervals −0.452, −0.111; Z = −3.24; P = 0.0012).
Table 2.
Mean VEE scores for 79 women randomized to the HIV and control interventions using an intention-to-treat analysis
| VEE | Group assignment | Mean VEE score (SD) | S.E. | T-test | P | Effect size |
|---|---|---|---|---|---|---|
| VEE | HIV | 9.47 (23.20) | 3.71 | −.178 | .86 | −.04 |
| Baseline | Money mgt | 10.34 (20.36) | 3.22 | |||
| VEE | HIV | 9.94 (43.23) | 6.92 | −.905 | .37 | −.20 |
| 3 months | Money mgt | 31.89 (146.94) | 23.23 | |||
| VEE | HIV | 12.23 (28.30) | 4.53 | .116 | .91 | .03 |
| 6 months | Money mgt | 11.58 (20.99) | 3.32 |
N = 79
Table 3.
The relationship of intervention group assignment and follow-up time to unprotected anal and vaginal sex
| Parameter | Estimate | Standard error | 95% confidence limits | Z | P | ||
|---|---|---|---|---|---|---|---|
| Intercept | 2.2644 | 0.2998 | 1.6768 | 2.8519 | 7.55 | <.0001 | |
| HIV group | −0.1019 | 0.4944 | −1.0708 | 0.8670 | −0.21 | 0.84 | |
| Baseline | 0 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | ||
| 3-month f/u | 1 | 0.8679 | 0.5033 | −0.1185 | 1.8542 | 1.72 | 0.08 |
| 6-month f/u | 2 | 0.1082 | 0.3109 | −0.5012 | 0.7176 | 0.35 | 0.74 |
| HIV group*baseline | 0 | 0.0000 | 0.0000 | 0.0000 | 0.0000 | ||
| HIV group*3-month f/u | 1 | −0.7804 | 0.7534 | −2.2571 | 0.6963 | −1.04 | 0.30 |
| HIV group*6-month f/u | 2 | 0.1706 | 0.4686 | −0.7478 | 1.0890 | 0.36 | 0.72 |
Analysis of general estimating equation parameters with a Poisson log link function. The reference group for “HIV group” is the control intervention, and the reference group for “time” is baseline
The additional dose–response analysis showed that though no significant difference in median number of unprotected sexual episodes between the 4 session categories at either follow-up time point was found, the analyses yielded a statistically significant difference between those participants who received 0–3 and those who attended 4–10 sessions of either intervention arm. Participants who attended between 0 and 3 sessions had a median of 52.04 unprotected vaginal and anal episodes compared to their counterparts who attended 4–10 sessions, who had a median of 37.22 episodes of unprotected sexual intercourse (U = 245.5, Z = −2.381, P = .017). At 6-month follow-up, the median difference was not statistically significant, though clinically important and hence noteworthy: 48.92 versus 37.39 unprotected sexual episodes among the 0–3 and 4–10 sessions groups, respectively (U = 283, Z = −1.683, P = .092). However, because the two distributions are unequally shaped, the significance levels are better interpreted as trends. Nonetheless, these findings are consistent with the trend observed from the initial GEE dose–response analysis, which showed that exposure to any group sessions (intervention or control) led to a decrease in sexual risk behavior. One further observation is noteworthy: there was only minor variability in median number of unprotected sexual episodes between time points, even showing a minor increase from the 3- to 6-month follow-up.
Condom Knowledge and Attitude Outcomes
Female condom knowledge, insertion and use at all three time points is displayed in Table 4. At baseline, the majority of women in the HIV intervention and the money-management intervention knew about the female condom, but few women had ever tried to insert a female condom or use it with a sexual partner. At the 3-month follow-up, women in the HIV intervention group were more likely to report knowing about the female condom, inserting the female condom or using it with a male partner. At the 6-month follow-up, these women were more likely to have inserted the female condom.
Table 4.
Knowledge, insertion, and use of the female condom among Project Wisdom participants at three time points
| Time | Treatment assignment | χ2a | P | |
|---|---|---|---|---|
| HIV n (%) | Control n (%) | |||
| Baseline | ||||
| Know about the female condom | ||||
| Yes | 32 (82.1) | 31 (77.5) | 0.823 | 0.82 |
| No | 7 (17.9) | 9 (22.5) | ||
| Ever tried to insert the FC | ||||
| Yes | 3 (8.1) | 7 (17.5) | 0.784 | 0.38 |
| No | 34 (91.9) | 33 (82.5) | ||
| Ever used the FC with a partner | ||||
| Yes | 2 (5.6) | 5 (12.5) | 0.42 | 0.52 |
| No | 34 (94.4) | 35 (87.5) | ||
| 3-month follow-up | ||||
| Know about the FC | ||||
| Yes | 35 (100) | 28 (87.5) | 2.7 | 0.1 |
| No | 0 | 4 (12.5) | ||
| Tried to insert the FC in the past 3 months | ||||
| Yes | 19 (54.3) | 2 (6.2) | 15.76 | 0.0001 |
| No | 16 (45.7) | 30 (93.8) | ||
| Used the FC with a partner in the past 3 months | ||||
| Yes | 10 (28.6) | 2 (6.2) | 4.25 | 0.04 |
| No | 25 (71.4) | 30 (93.8) | ||
| 6-month follow-up | ||||
| Know about the FC | ||||
| Yes | 35 (100) | 33 (97.1) | 0 | 0.99 |
| No | 0 | 1 (2.9) | ||
| Tried to insert the FC in the past 3 months | ||||
| Yes | 14 (40.0) | 4 (11.8) | 5.74 | 0.02 |
| No | 21 (60.0) | 30 (88.2) | ||
| Used the FC with a partner in the past 3 months | ||||
| Yes | 9 (26.5) | 3 (8.8) | 2.53 | 0.11 |
| No | 25 (73.5) | 31 (91.2) | ||
Degrees of freedom = 1
Pearson Chi-Square with continuity correction
Table 5 presents the mean scores for attitudes and method-specific efficacy for the female and male condom by group assignment at each time point. Using a hierarchical ANOVA, there was no significant main effect of intervention group assignment on female condom attitudes and method-specific efficacy at the 3-month follow up (F (df = 1) = 2.66, P = .11) or the 6-month follow-up (F (df = 1) = 1.15, P = .29). Similarly, there was no main effect of the intervention group assignment on male condom attitudes and method-specific efficacy at the 3-month follow-up (F (df = 1) = .558, P = .46) and 6-month follow-up (F (df = 1) = .052, P = .82).
Table 5.
Attitudes and method specific efficacy for female and male condoms at three time points
| Treatment group | Baseline | 3-month follow-up | 6-month follow-up | |||
|---|---|---|---|---|---|---|
| Mean (SD) | N | Mean (SD) | N | Mean (SD) | N | |
| Female condom attitudes and method specific efficacy (range 1–4) | ||||||
| HIV | 2.798 (.341) | 39 | 2.930 (.327) | 35 | 2.868 (.344) | 35 |
| Control | 2.801 (.353) | 40 | 2.778 (.417) | 32 | 2.774 (.377) | 34 |
| Male condom attitudes and method specific efficacy (range 1–4) | ||||||
| HIV | 3.025 (.392) | 39 | 2.988 (.348) | 35 | 2.965 (.297) | 35 |
| Control | 2.936 (.342) | 40 | 2.972 (.377) | 32 | 2.912 (.361) | 34 |
Higher means indicate more positive attitudes and perceived efficacy
Discussion
This paper presents the results of an evaluation of the efficacy of an HIV prevention intervention, centered on skills for use of female and male condoms. We hypothesized that, compared to women in the control group, women receiving the HIV prevention intervention would reduce the number of unprotected sexual occasions over the 6 months following the intervention. We found no significant effect of the intervention on sexual risk behavior at either post intervention time point. Our secondary hypotheses were that women receiving the HIV intervention would demonstrate an increase in knowledge of the female condom, insertion of the female condom, use of the female condom with a partner, and have more positive attitudes toward the female and male condom compared to the control group. We observed significant differences in female condom knowledge, insertion, and use with a partner between the HIV and control group at the 3-month follow-up, but no significant group differences in attitudes. Differences in female condom insertion persisted at 6 months.
Our findings suggest that the intervention was not effective in reducing sexual risk behavior. The lack of efficacy for sexual risk reduction is supported by the fact that differences in the VEE scores and mean number of unprotected sexual episodes at 3 months may have been driven by outliers in the control group who reported much more unsafe sex at 3 months. This accounts for the large standard deviation notable for the control group in particular. Other factors may have also been at play. First, the study may have lacked sufficient power to detect differences between the groups. Although we recruited participants at several community sites, we were able to screen 280 women, and less than half of these women met our sexual behavior criterion. Our study differs from other trials of HIV prevention among women in that women with schizophrenia-spectrum disorders composed the majority of the sample (64% vs. 33–52% in trials cited here); this may have affected recruitment and retention of participants. Second, our data also show that by the 6-month follow-up, almost all of the women in the control group (97%) knew about the female condom, compared to 77% at baseline, suggesting contamination of the sample. Interestingly, however, although women in both groups reported similar histories of STIs at baseline, by the 6-month follow-up, women in the control group reported four times the number of STIs in the past 3 months than women in the HIV group.
Limited acceptability of the female condom may have also diminished efficacy of the intervention. Although women in the intervention group were more likely to insert a female condom 3 and 6 months after the intervention, relatively few women attempted to use it with a partner. The female condom has been found to have variable acceptability in the United States (Hirky et al. 2003; Holmes et al. 2008; Klein et al. 1999; Sly et al. 1997; Witte et al. 1999), and there are a number of issues that may make it challenging for this population. Women with medication side-effects that include tremors or other movement disorders may find insertion of the female condom difficult. Our intervention sessions included practice inserting the female condom into a pelvic model, but women may need to practice inserting the condom in vivo with the assistance of a nurse (or other designated provider) to help answer questions and circumvent difficulties. Cost and availability may also prevent female condom use. Women were provided with free male and female condoms throughout the intervention, and, because of the government entitlements they received, they could also obtain the female condom with a doctor’s prescription in New York State. But women need to be motivated to request condoms from a doctor, and women may not associate their psychiatrists (the doctor they are likely to see most frequently in these settings) with provision of contraception or HIV prevention methods. Previous work suggests that few women with SMI feel encouraged to discuss their sexual lives with their mental health providers (Collins et al. 2008a). Despite these difficulties, the increased mean score in positive attitudes and method-specific efficacy for the female condom among HIV group participants at 3 months showed a trend in the direction of our hypothesis.
An unintended consequence of the intervention was a reduction in sexual activity at the 3-month follow-up. Discussions during the group sessions revealed that several women left their partners over the course of the intervention, possibly because other women in the group encouraged them to leave relationships that were disrespectful or abusive. The intervention group sessions served as a place for women to encourage and empower each other, and receive attention to their social and sexual lives. These effects may have also occurred for women in the control group, as evidenced by the significant relationship between attending at least 4 sessions of either group and reduced unprotected anal or vaginal sex. This finding reinforces the need for exposure to a minimum number of sessions to achieve behavior change (Exner et al. 1997).
Previous intervention studies that included women with SMI found significant effects on use of the male condom for up to 1 year (Carey et al. 2004; Otto-Salaj et al. 2001). Carey et al. (2004) demonstrated greater reductions in unsafe sex among women compared to men. Patients with depression, in particular, benefitted from this intervention, and approximately half of the study sample had a depressive disorder. The role of psychiatric diagnosis in the responsiveness to HIV interventions warrants further study. However, the finding of persistent risk behavior for women even in the setting of increased condom use (Otto-Salaj et al. 2001) suggests that behavioral interventions in this population that have shown success cannot stand on their own.
Effective and sustained HIV prevention among women with SMI must tackle other factors linked to HIV risk such as substance use, traumatic abuse, social support network, psychiatric symptoms, stigma related to mental illness (Collins et al. 2008a; Devieux et al. 2007; Elkington et al. 2010; McKinnon et al. 2001; Meade and Sikkema 2007; Randolph et al. 2007) as well as broader social and economic factors detrimental to women. Effective prevention for women with SMI will require a comprehensive approach to prevention that employs multiple interventions at different levels (Coates et al. 2008) directed toward the individual woman; her partner and/or family; her clinic, day program or residential facility; and her wider community. Such an approach to prevention requires research as well as policy interventions that might range from an understanding of transmission dynamics in the communities where women live to establishing co-located treatment for mental illness and HIV services in community mental health clinics and ensuring that women’s needs for intimacy and support in the context of a serious mental illness are thoughtfully addressed.
Limitations of our study include a short duration of effect (3 months), recruitment of a convenience sample whose responses to the intervention may not be generalizable to all populations of women with SMI, and differences in group baseline characteristics that may be related to factors that influence insertion and use of the female condom. Loss of randomization may have introduced additional selection bias that affected the study outcomes. However, there were no demographic or baseline sexual behavior differences between women excluded from the analysis and those retained.
Despite its limitations, this study suggests that an intervention for women with SMI can increase knowledge and use of the female condom. While further research must explore the characteristics (diagnostic, social, and demographic) that underlie female condom use in this population, the device may be an appropriate HIV risk reduction tool for a subset of women with SMI. In the context of a comprehensive, multilevel HIV prevention intervention, this approach could be a useful addition for clinical and residential community settings for women with SMI.
Acknowledgments
This study was supported by NIMH K01 MH01691 (PI Pamela Y. Collins) and a grant from the Robert Wood Johnson Harold Amos Medical Faculty Development Program, and the research was conducted while Dr. Collins was based at Columbia University and the New York State Psychiatric Institute. The views expressed in this article do not necessarily represent the views of the NIMH or the Federal Government. We are grateful to investigators from the HIV Center for Clinical and Behavioral Studies (PI Anke Ehrhardt) (New York State Psychiatric Institute and Columbia University) for their helpful comments. The authors wish to thank Dr. Patricia Zybert, Dr. Bruce Levin, Dr. Emilia Bagiella, Ms. Helena Chang, Ms. Sarah Joestl and members of the HIV Center Statistics, Epidemiology, and Data Management Core for their data analytic contributions. We are grateful to Dr. Stephanie LeMelle and Dr. Henry McCurtis for their contributions to intervention development, administration, and site procurement.
Contributor Information
Pamela Y. Collins, Columbia University, New York, NY, USA
Hella von Unger, Social Science Research Center Berlin (WZB), Research Group Public Health, Berlin, Germany.
Susan Putnins, Mc Lean Hospital, Belmont, MA, USA.
Natalie Crawford, Columbia University, New York, NY, USA.
Ragini Dutt, UNICEF Headquarters, New York, NY, USA.
Marcela Hoffer, Columbia University, New York, NY, USA.
References
- Amaro H. Love, sex, and power: Considering women’s realities in HIV prevention. American Psychologist. 1995;50:437–447. doi: 10.1037//0003-066x.50.6.437. [DOI] [PubMed] [Google Scholar]
- Amaro H, Ray A. On the margin: Power and women’s HIV risk reduction strategies. Sex Roles. 2000;42(7/8):723–749. [Google Scholar]
- Bandura A. Social cognitive theory and exercise control of HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and methods of behavioral interventions. New York: Plenum Press; 1994. pp. 25–59. [Google Scholar]
- Blank MB, Mandell DS, Aiken L, Hadley TR. Cooccurrence of HIV and serious mental illness among medicaid recipients. Psychiatric Services. 2002;53(7):868–873. doi: 10.1176/appi.ps.53.7.868. [DOI] [PubMed] [Google Scholar]
- Carey MP, Carey KB, Maisto SA, Gordon CM, Schroder KEE, Vanable PA. Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: Results from a randomized clinical trial. Journal of Consulting and Clinical Psychology. 2004;72(2):252–268. doi: 10.1037/0022-006X.72.2.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates TJ, Richter L, Caceres C. Behavioral strategies to reduce HIV transmission: How to make them work better. The Lancet. 2008;372:669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Elkington KS, von Unger H, Sweetland A, Wright ER, Zybert P. The relationship of stigma to HIV risk behavior among women with mental illness. American Journal of Orthopsychiatry. 2008a;78(4):498–506. doi: 10.1037/a0014581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, Geller PA, Miller S, Toro P, Susser E. Ourselves, Our Bodies, Our Realities: An HIV preventive intervention for women with mental illness. Journal of Urban Health. 2001;78(1):162–175. doi: 10.1093/jurban/78.1.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins PY, von Unger H, Armbrister A. Church ladies, good girls, and locas: Stigma and the intersection of ethnicity, gender, mental illness, and sexuality. Social Science & Medicine. 2008b;67:389–397. doi: 10.1016/j.socscimed.2008.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devieux JG, Malow R, Lerner BG, Dyer JG. Triple jeopardy for HIV: Substance using severely mentally ill adults. Journal of Prevention & Intervention in the Community. 2007;33(1/2):5–18. doi: 10.1300/J005v33n01_02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkington KS, McKinnon K, Mann CG, Collins PY, Leu C-S, Wainberg ML. Perceived mental illness stigma and HIV risk behaviors among adult psychiatric outpatients in Rio de Janeiro, Brazil. Community Mental Health Journal. 2010;46(1):56–64. doi: 10.1007/s10597-009-9209-4. doi: 10.1007/s10597-009-9209-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Exner TM, Seal D, Ehrhardt A. A review of HIV interventions for at-risk women. AIDS and Behavior. 1997;1(2):93–124. [Google Scholar]
- Fullilove M, Fullilove R, Haynes K, Gross S. Black women and AIDS prevention: A view towards understanding the gender rules. The Journal of Sex Research. 1990;27(1):47–64. [Google Scholar]
- Gollub E. The female condom: Tool for women’s empowerment. American Journal of Public Health. 2000;90:1377–1381. doi: 10.2105/ajph.90.9.1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gollub E, French P, Latka M, Rogers C, Stein Z. Achieving safer sex with choice: Studying a women’s sexual risk reduction hierarchy in an STD clinic. Journal of Women’s Health and Gender-Based Medicine. 2001;10(8):771–783. doi: 10.1089/15246090152636532. [DOI] [PubMed] [Google Scholar]
- Hardwick D. The effectiveness of a female condom intervention on women’s use of condoms. The Canadian Journal of Human Sexuality. 2002;11(2):63–76. [Google Scholar]
- Hirky AE, Kirshenbaum SB, Melendez RM, Rollet C, Perkins SL, Smith RA. The female condom: Attitudes and experiences among HIV-positive heterosexual women and men. Women and Health. 2003;37(1):71–89. doi: 10.1300/J013v37n01_05. [DOI] [PubMed] [Google Scholar]
- Holmes L, Ogungbade GO, Ward DD, Garrison O, Peters RJ, Kalichman SC, et al. Potential markers of female condom use among inner city African American women. AIDS Care. 2008;20(4):470–477. doi: 10.1080/09540120701867016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman S, Malow R, Devieux J, Stein JA, Piedman F. HIV risk reduction for substance-using mentally-ill adults: Test of the Information-Motivation-Behavior Skills (IMB) model. Community Mental Health Journal. 2005;41(3):277–290. doi: 10.1007/s10597-005-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein H, Eber M, Crosby H, Welka DA, Hoffman JA. The acceptability of the female condom among substance-using women in Washington, DC. Women and Health. 1999;29(3):97–115. doi: 10.1300/j013v29n03_07. [DOI] [PubMed] [Google Scholar]
- Kloos B, Gross SM, Meese KJ, Meade CS, Doughty JD, Hawkins DD, et al. Negotiating risk: Knowledge and use of HIV prevention by persons with serious mental illness living in supportive housing. American Journal of Community Psychology. 2005;36(3–4):357–372. doi: 10.1007/s10464-005-8631-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krakow DS, Galanter M, Dermatis H, Westreich LM. HIV risk factors in dually diagnosed patients. American Journal on Addictions. 1998;7(1):74–80. [PubMed] [Google Scholar]
- Macaluso M, Demand M, Artz L, Fleenor M, Robey L, Kelaghan J, et al. Female condom use among women at high risk of sexually transmitted disease. Family Planning Perspectives. 2000;32(3):138–144. [PubMed] [Google Scholar]
- Mays V, Cochran S. Issues in the perception of AIDS risk and risk reduction activities by Black and Hispanic/Latina women. American Psychologist. 1988;43(11):949–957. doi: 10.1037//0003-066x.43.11.949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinnon K, Cournos F, Meyer-Bahlburg H, Guido J, Caraballo L, Margoshes E, et al. Reliability of sexual risk behavior interviews with psychiatric patients. American Journal of Psychiatry. 1993;150(6):972–974. doi: 10.1176/ajp.150.6.972. [DOI] [PubMed] [Google Scholar]
- McKinnon K, Cournos F, Herman R. A lifetime alcohol or other drug use disorder and specific psychiatric symptoms predict sexual risk for HIV infection among people with severe mental illness. AIDS and Behavior. 2001;5(3):233–240. [Google Scholar]
- McKinnon K, Cournos F, Herman R. HIV among people with chronic mental illness. Psychiatric Quarterly. 2002;73(1):17–31. doi: 10.1023/a:1012888500896. [DOI] [PubMed] [Google Scholar]
- Meade CS. Sexual risk behavior among persons dually diagnosed with severe mental illness and substance use disorder. Journal of Substance Abuse Treatment. 2006;30(2):147–157. doi: 10.1016/j.jsat.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Meade CS, Kershaw TS, Hansen NB, Sikkema KJ. Long-term correlates of childhood abuse among adults with severe mental illness: Adult victimization, substance abuse, and HIV sexual risk behavior. AIDS and Behavior. 2009;13(2):207–216. doi: 10.1007/s10461-007-9326-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. HIV risk behavior among adults with severe mental illness: A systematic review. Clinical Psychology Review. 2005;25(4):433–457. doi: 10.1016/j.cpr.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Meade CS, Sikkema KJ. Psychiatric and psychosocial correlates of sexual risk behavior among adults with severe mental illness. Community Mental Health Journal. 2007;43(2):153–169. doi: 10.1007/s10597-006-9071-6. [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg H, Ehrhardt A, Exner TM, Gruen RS. Sexual risk behavior assessment schedule—Adult—Armory interview. New York: New York State Psychiatric Institute and Columbia University; 1991. [Google Scholar]
- Otto-Salaj L, Heckman T, Stevenson L, Kelly J. Patterns, predictors and gender differences in HIV risk among severely mentally ill men and women. Community Mental Health Journal. 1998;34(2):175–190. doi: 10.1023/a:1018745119578. [DOI] [PubMed] [Google Scholar]
- Otto-Salaj L, Kelly J, Stevenson L, Hoffmann R, Kalichman S. Outcomes of a randomized small-group HIV prevention intervention trial for people with serious mental illness. Community Mental Health Journal. 2001;37(2):123–143. doi: 10.1023/a:1002709715201. [DOI] [PubMed] [Google Scholar]
- Parry CD, Blank MB, Pithey AL. Responding to the threat of HIV among persons with mental illness and substance abuse. Current Opinion in Psychiatry. 2007;20(3):235–241. doi: 10.1097/YCO.0b013e3280ebb5f0. [DOI] [PubMed] [Google Scholar]
- Pulerwitz J, Amaro A, Jong WD, Gortmaker S, Rudd R. Relationship power, condom use and HIV risk among women in the USA. AIDS Care. 2002;14(6):789–800. doi: 10.1080/0954012021000031868. [DOI] [PubMed] [Google Scholar]
- Randolph ME, Pinkerton SD, Somlai AM, Kelly JA, McAuliffe TL, Gibson RH, et al. Severely mentally ill women’s HIV risk: The influence of social support, substance use, and contextual risk factors. Community Mental Health Journal. 2007;43(1):33–47. doi: 10.1007/s10597-006-9069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SD, Goodman LA, Osher FC, Swartz MS, Essock SM, Butterfield MI, et al. Prevalence of HIV, Hepatitis B, and Hepatitis C in people with severe mental illness. American Journal of Public Health. 2001a;91(1):31–37. doi: 10.2105/ajph.91.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg SD, Trumbetta SL, Mueser KT, Goodman LA, Osher FC, Vidaver RM, et al. Determinants of risk behavior for Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome in people with severe mental illness. Comprehensive Psychiatry. 2001b;42(4):263–271. doi: 10.1053/comp.2001.24576. [DOI] [PubMed] [Google Scholar]
- Sly D, Quadagno D, Harrison DF, Eberstein IW, Riehman K, Bailey M. Factors associated with use of the female condom. Family Planning Perspectives. 1997;29:181–184. [PubMed] [Google Scholar]
- Sohler N, Colson PW, Meyer-Bahlburg HFL, Susser E. Reliability of self-reports about sexual risk behavior for HIV among homeless men with severe mental illness. Psychiatric Services. 2000;51(6):814–816. doi: 10.1176/appi.ps.51.6.814. [DOI] [PubMed] [Google Scholar]
- Susser E, Desvarieux M, Wittkowski KM. Reporting sexual risk behavior for HIV: A practical risk index and a method for improving risk indices. American Journal of Public Health. 1998;88(4):671–674. doi: 10.2105/ajph.88.4.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanable PA, Carey MP, Carey KB, Maisto SA. Differences in HIV-related knowledge, attitudes, and behavior among psychiatric outpatients with and without a history of a sexually transmitted infection. Journal of Prevention and Intervention in the Community. 2006;33(1–2):79–94. doi: 10.1300/J005v33n01_07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walkup J, Blank MB, Gonzalez JS, Safren S, Schwartz R, Brown L, et al. The impact of mental health and substance abuse factors on HIV prevention and treatment. Journal of Acquired Immune Deficiency Syndromes. 2008;47(Suppl. 1):S15–S19. doi: 10.1097/QAI.0b013e3181605b26. [DOI] [PubMed] [Google Scholar]
- Wallace C. Social skills training in psychiatric rehabilitation: Recent findings. International Review of Psychiatry. 1998;10:9–19. [Google Scholar]
- Weinhardt LS, Carey MP, Carey KB, Verdecias N. Increasing assertiveness skills to reduce HIV risk among women living with a severe and persistent mental illness. Journal of Consulting and Clinical Psychology. 1998;66(4):680–684. doi: 10.1037//0022-006x.66.4.680. [DOI] [PubMed] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, et al. The structured clinical interview for DSM-III-R (SCID) II: Multi-site test–retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- Witte SS, El-Bassel N, Wada T, Gray O, Wallace J. Acceptability of female condom use among women exchanging street sex in New York City. International Journal of STD and AIDS. 1999;10:162–168. doi: 10.1258/0956462991913826. [DOI] [PubMed] [Google Scholar]
- Wright ER, Gayman M. Sexual networks and HIV risk of people with severe mental illness in institutional and community-based care. AIDS and Behavior. 2005;9(3):341–353. doi: 10.1007/s10461-005-9008-z. [DOI] [PubMed] [Google Scholar]