Abstract
Based on autopsy data collected in Southern China from 2001–2006, 975 cases of sudden unexplained nocturnal death syndrome (SUNDS) were surveyed. Genetic screening of SCN5A, the gene encoding the voltage dependent cardiac Na channel, was performed in 74 available SUNDS cases. The annual occurrence rate of SUNDS in the area was estimated to be 1 per 100,000 people. 80.6% of deaths occurred between the ages of 21 to 40 years and the case number peaked at age 30 years. In 75.4% of cases where witnesses were present, victims died in their sleep between 11 PM and 4 AM and many showed abrupt respiratory distress shortly preceding death. The monthly distribution of emergency fever cases in the area during the same period was positively correlated to that of SUNDS cases (rs = 0.611, P = 0.0025). Four polymorphisms in SCN5A were identified in both SUNDS and control groups. Compared with controls, the allele frequency of C5457 and C3666+69 were significant higher in SUNDS (P<0.005) while the genotypes of both 5457CC (P=0.012, OR=2.0, 95% CI=1.3–3.2) and 3666+69CC (P=0.004, OR=2.1, 95% CI=1.3–3.3) in SUNDS cases were significantly higher. This is the first report of an epidemiological survey and SCN5A gene screening in SUNDS in the Han population of China. The genotypes of 5457CC and 3666+69CC in SCN5A gene may be Chinese SUNDS susceptible polymorphisms.
Keywords: sudden unexplained nocturnal death syndrome, Chinese Han population, Epidemiology, SCN5A gene, polymorphism, arrhythmia
Introduction
First reported in 1917 in the Philippines (1,2), sudden unexplained nocturnal death syndrome (SUNDS) remains a puzzling disorder with unknown etiology. SUNDS prevails mainly in Southeast Asian ethnic groups especially among Thai, Laotian, Cambodian, Vietnamese, Japanese and Chinese. Most of these sudden deaths took place at night during the sleep of apparently healthy young males, and autopsy revealed no pathological evidence to explain death (3–6).
Detailed data including clinical records of SUNDS are laregely unavailable because deaths occur mainly in robust healthy males during sleep and out of the hospital setting. This makes in depth epidemiological study of SUNDS difficult. Consequently, a lack of epidemiological data has been a formidable bottleneck to research on the etiology of SUNDS around the world since its description nearly 100 years ago.
The reported phenotype of SUNDS was thought to be similar to Brugada syndrome (7), some cases of which were identified to be caused by the mutations of SCN5A,the gene encoding the cardiac sodium channel alpha subunit NaV1.5. To explore the genetic cause of SUNDS, we hypothesized that abnormality of SCN5A is related to some cases of Chinese SUNDS.
Although there were many SUNDS cases in Southern China, the disease epidemiology in China may have been underestimated in the absence of systemic monitoring (5). Based on collected autopsy data in Guangdong province in Southern China from 2001–2006, 975 cases of SUNDS were included in the present study. In this paper we report the first detailed epidemiological survey and SCN5A screening of SUNDS as well as their impact on the Chinese Han population with the goal of discovering clues for the etiology and mechanisms of this pernicious syndrome.
MATERIALS AND METHODS
Study population and data collection
Dongguan city, Baoan and Longgang District (except Buji Town) of Shenzhen city are geographically adjacent and relatively developed regions in Guangdong Province. All unexplained sudden deaths out of hospital must be investigated for cause of death by the forensic medical center of the Public Security Bureau in these three locations where nearly all of the SUNDS cases were recorded in a predesigned autopsy report database. The information available for 975 cases identified as SUNDS during a six-year period (from January 2001 to December 2006) in the three regions was collected from the autopsy report database. The collected data includes name, gender, age, birthplace, occupation, time of death, the investigation record of death scene, autopsy status, and description of witness.
In the survey, SUNDS cases were defined as: (1) apparently healthy individuals without medical history of significant disease; (2) sudden unexpected death during asleep; (3) age between 15 and 55 (inclusive); (4) absence of morphological changes from the forensic medical autopsies accounting for death; and (5) exclusion of deaths caused by suicide, homicide, accident, poisoning, drowning and other violent deaths (resulting from physical, chemical, biological and mechanical factors).
Of all SUNDS cases, only 74 cases (all were male) whose bloodstained gauze was available were included for screening SCN5A in this study. Genetic screening controls’ peripheral blood samples were collected from 115 unrelated healthy males in Southern China.
All studies and data collection were in strict accordance with ethics guideline.
SCN5A gene screening
Genomic DNA was extracted from the bloodstained gauze of 74 SUNDS cases and from peripheral leukocytes of 115 unrelated healthy males. Using 41 pairs of primers, amplification of all SCN5A exons and relevant exon-intron boundaries on each strand was performed. Direct DNA sequencing was used to detect the SCN5A genotype
Statistical analysis
Rank correlation methods were used to determine whether the monthly distribution of SUNDS and that of emergency fever cases or average air temperature were correlated. Degree of correlation was described by correlation coefficient (rs). We used χ2 analysis to assess Hardy-Weinberg equilibrium for each polymorphism of alleles and to test for potential linkage disequilibrium. The significance of differences between SUNDS cases and controls for each genotype and allele were evaluated by χ2 analysis or Fisher’s exact test. Probability (P) value <0.05 was considered statistically significant.
RESULTS
A total of 975 cases identified as SUNDS were collected in the three regions (Table 1). Since 2002, the number of total SUNDS cases in the three regions was relatively stable. During the period of 2003–2006, the mean occurrence was 178 cases per year. According to the record provided by local governments, there were approximately 18,000,000 people per year in the study area) during the period. Based on the background population, the yearly occurrence rate of SUNDS in this area in the past several years was calculated to be around 1.0 per 100,000 people in the total population.
Table 1.
The number of SUNDS cases in Dongguan, Longgang, Baoan District in Guangdong Province during 2001–2006
| Year | Dongguan | Longgang | Baoan | Total |
|---|---|---|---|---|
| 2001 | 53 | 32 | 30 | 115 |
| 2002 | 64 | 48 | 43 | 155 |
| 2003 | 79 | 30 | 63 | 172 |
| 2004 | 62 | 51 | 75 | 188 |
| 2005 | 42 | 54 | 82 | 178 |
| 2006 | 28 | 47 | 92 | 167 |
| Total | 328 | 262 | 385 | 975 |
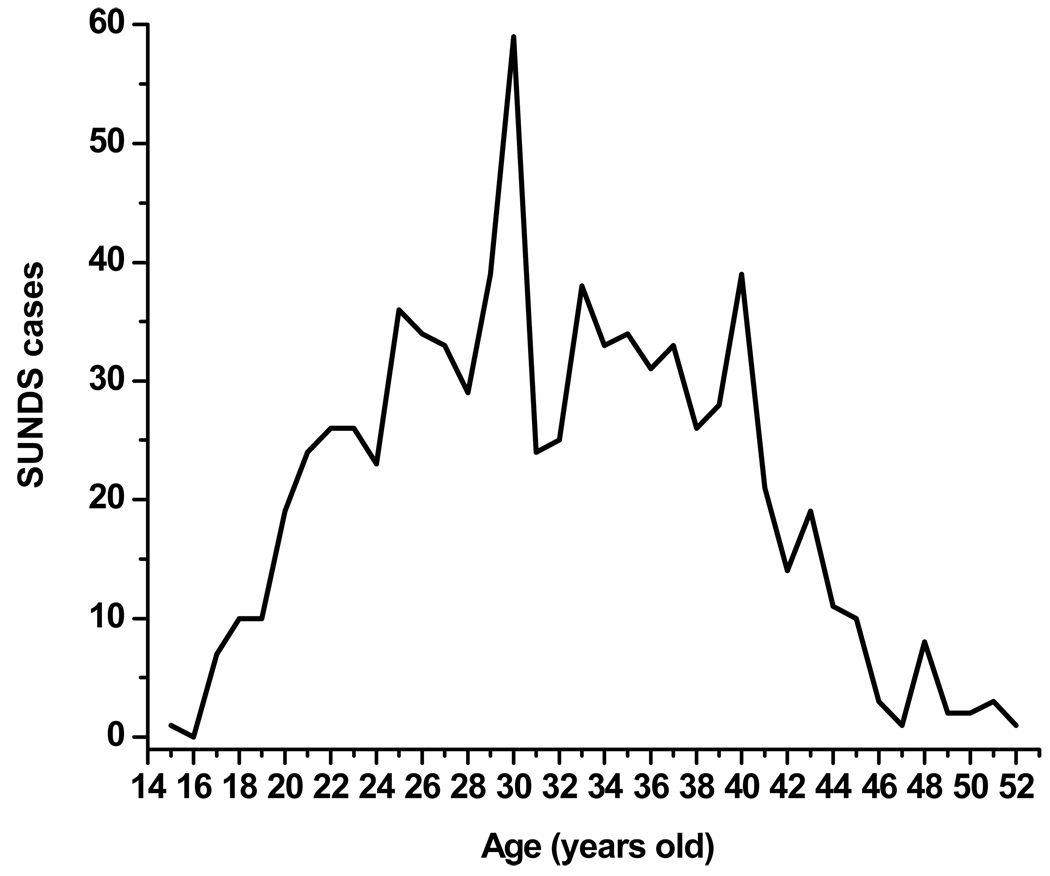
Among all 975 SUNDS victims, 909 cases (93.23%) were males while only 66 cases (6.77%) were females (ratio of 13.8:1). Out of 975 cases, 193 cases did not have an accurate age record. In the remaining 782 cases, the ages ranged from 15 to 52 years old (Figure 1). The case number was relatively small for ages 15–24 years (only 1 victim at age 15 years) but started to rise drastically from the age of 25 years (36 victims at age 25) and then peaked at the age of 30 years (59 victims at age 30). The case number was relatively stable at ages 31–40 years and dropped sharply after 41 years (21 victims at age 41) and dropped further with increase in age. Victims aged 21 to 40 years accounted for 80.56% of the 782 cases with definite age record.
FIGURE 1.
The distribution of age of 782 SUNDS cases
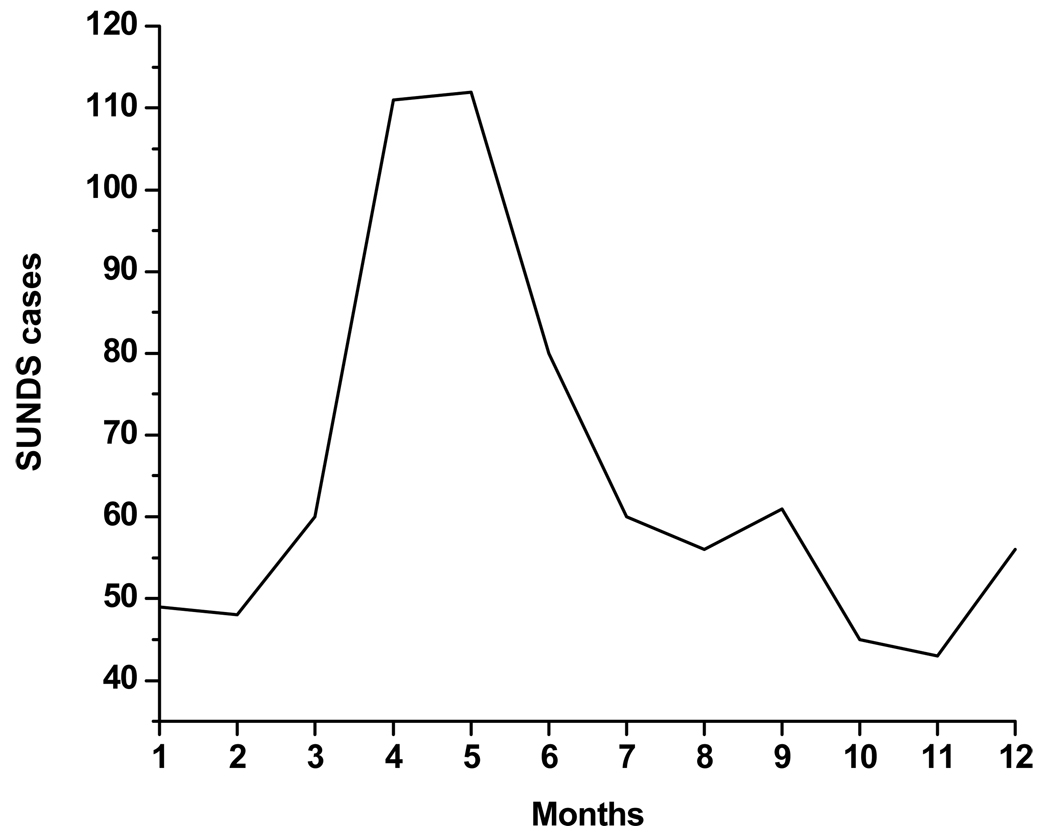
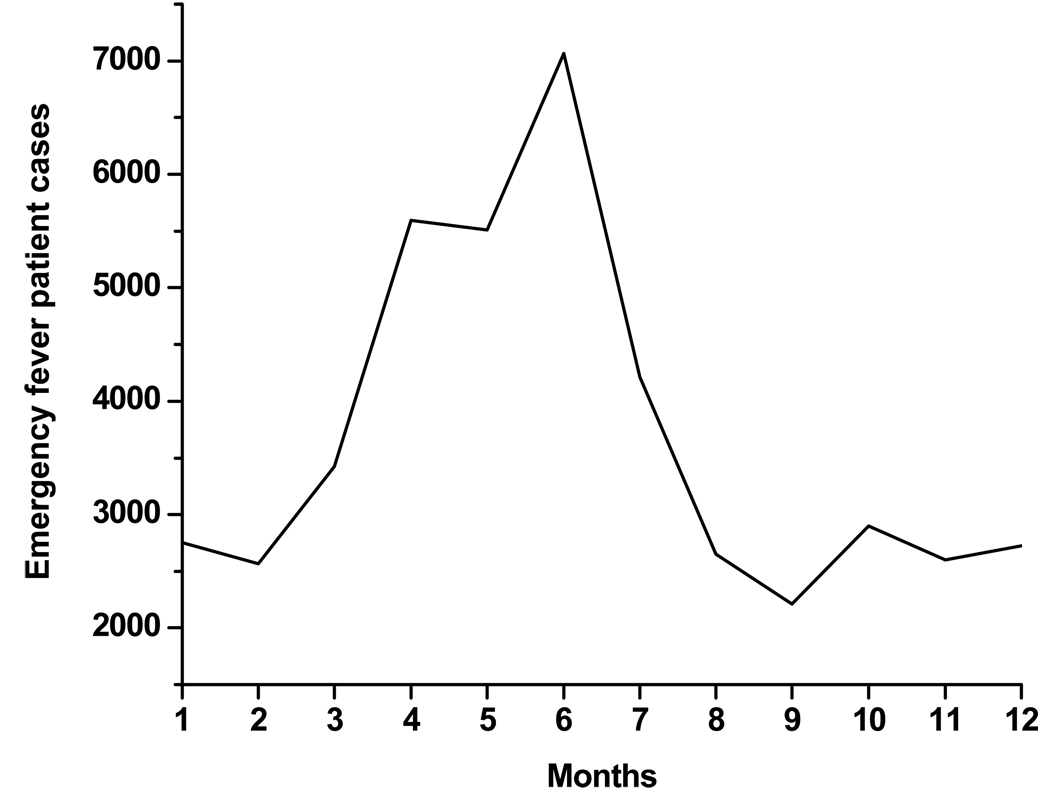
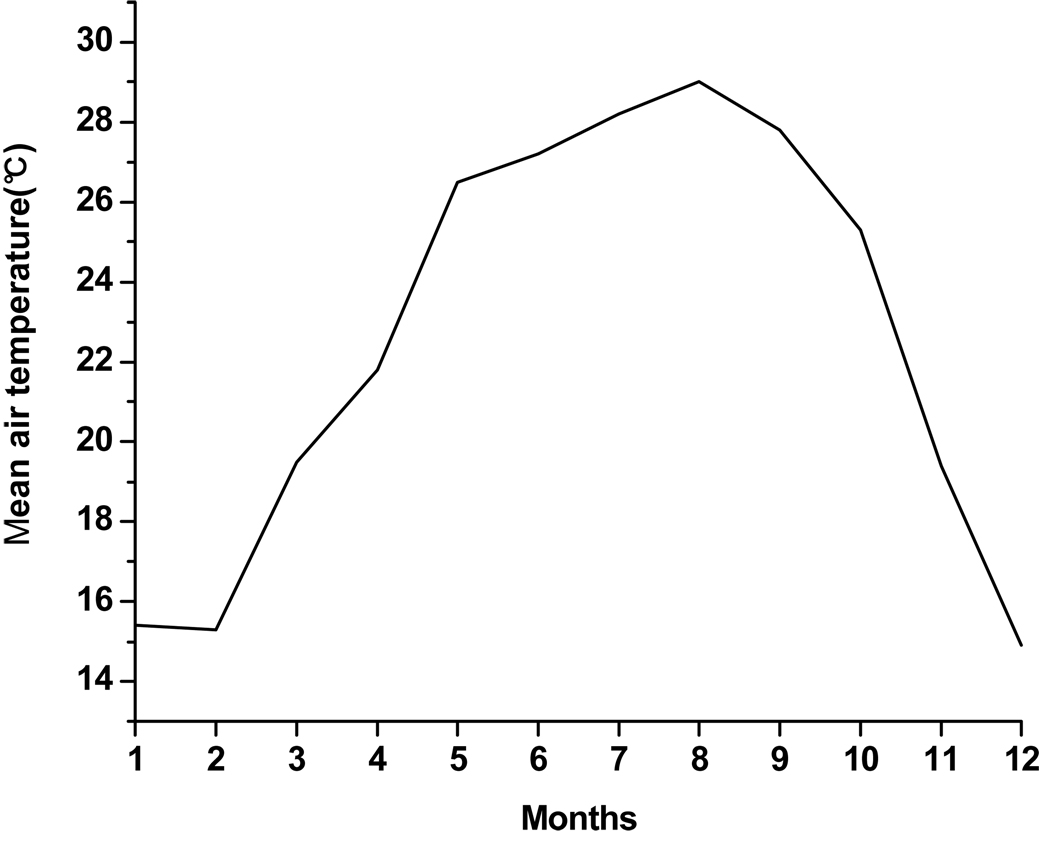
The monthly distribution of occurrence in 781 SUNDS cases with adequate records of the time of death (date/month/year) were analyzed. SUNDS occurred throughout the year with a mean occurrence of 65 cases per month. The peak months for SUNDS cases were April (111 cases), May (112 cases) and June (80 cases) while the lower incidence months were October (45 cases), November (43 cases) (Figure 2). To study the potential relationship between SUNDS and fever or air temperature, we also described the monthly distribution of emergency fever patient cases in 3 hospitals and monthly average air temperature collected in the three regions during the period (between January 2001 and December 2006) (Figures 3,4). The monthly distribution of emergency fever cases was positively correlated to that of SUNDS cases (rs = 0.611, P = 0.0025). However, the monthly average air temperature was not correlated to the monthly distribution of SUNDS cases (rs = 0.439, P = 0.154).
FIGURE 2.
The monthly distribution of 781 SUNDS cases in the studied area during 2001–2006
FIGURE 3.
The monthly distribution of Emergency fever patients cases in three hospitals in the studied area during 2001–2006
FIGURE 4.
The monthly mean air temperature in the studied area during 2001–2006
The majority of SUNDS victims were poorly educated workers who engaged in manual labor (blue-collar workers) except for 4 cases with history of higher education and administrative position. In this survey, there were only 173 SUNDS cases with a record of vocational history. In 173 cases, the largest numbers were construction workers (21 cases) and electronic appliance factory workers (19 cases). The percentage of blue-collar workers in the general population is not available.
Sixty five SUNDS cases had reports from witnesses such as spouses who could identify presence or absence of symptoms at the time of death or immediately prior to death. According to these descriptions, all 65 died instantly or within a few minutes of the onset of distress in sleep. Forty-nine out of 65 cases of sudden death occurred with obvious manifestations before death (Table 2). All cases died in their sleep. The time of death in witnessed cases was accurately provided. The number of victims and the span of corresponding time of death were as follows: 4 cases between 23:01 and 24:00, 10 cases between 0:01 a.m. to 1:00 am, 11 cases between 1:01 and 2:00, 11 cases between 2:01 to 3:00, 13 cases between 3:01 to 4:00, 6 cases between 4:01 to 5:00, 6 cases between 5:01 to 6:00, and 2 cases between 6:01 to 7:00. There were 2 cases that died in their sleep at about 18:00, 20:00 respectively.
Table 2.
The clinical manifestation of 65 witnessed SUNDS case
| Clinical manifestation immediately prior to death |
Cases number |
Percentage (%) |
|---|---|---|
| Sudden tachypnea | 13 | 20.0 |
| Abrupt tic of limbs | 10 | 15.4 |
| Strange groan or gasping | 7 | 10.8 |
| Scream | 5 | 7.7 |
| Abrupt discomfort | 5 | 7.7 |
| Abnormal snoring | 3 | 4.6 |
| Sudden cough | 3 | 4.6 |
| White froth through mouth | 2 | 3.1 |
| Feeling cold before retiring | 1 | 1.5 |
| No specific symptoms | 16 | 24.6 |
Only three victims were confirmed to have a family history of SUNDS; they were from Fujian, Guangdong and Jiangxi provinces. We traced four generations in two families with history of SUNDS and each case revealed male victims in the second and third generations at ages between 17 and 38 years. In one family, surviving relatives did not show clear evidence of significant cardiac structural defects but two male brothers (at the age of 28 and 30 years, respectively) had ECGs with unusually deep inferior Q waves in leads II, III, and aVF.
74 sporadic SUNDS cases (all were males, mean age = 31.7 years, standard deviation = 5.4) and 115 healthy unrelated subjects(all were males, mean age = 35.2 years, standard deviation = 8.9) were screened for mutations in SCN5A. In SUNDS cases, 2 rare SCN5A mutations were identified. One was a mis-sense mutation C4534T (R1512W, in exon 26, detected in the 46th case) which was previously reported in Brugada syndrome. The other is a novel synonymous mutation G3363A (A1121A, in exon 18, detected in the 63rd case). None of the confirmed disease-causing SCN5A mutations were detected in Controls. Four single nucleotide polymorphisms (SNPs) (allelic frequency > 0.5%) of SCN5A were identified in both groups. These SNPs includes A1673G (H558R, in exon 12), G3578A (R1193Q, in exon 20), C5457T (D1819D, in exon 28) and 3666+69G>C (in intron 20). Genotype distributions of all loci were in Hardy-Weinberg equilibrium in both groups (P>0.05). The genotype and allele frequencies of the identified SNPs are summarizd in Table 3. There were significant differences in genotype and allele frequencies of C5457T and 3666+69G>C between the two groups (P<0.05). The allele frequency of C5457 and C3666+69 were higher in SUNDS group than in controls (P<0.005). Compared with controls, the genotype of 5457CC (P = 0.012, OR = 2.0, 95% CI = 1.3–3.2) and 3666+69CC (P = 0.004, OR = 2.1, 95% CI = 1.3–3.3) in SUNDS cases were higher. There were no statistically significant differences in genotype and allele frequencies of the other 2 SNPs between two groups (all P>0.05).
Table 3.
The distributions of genotype and allele frequencies of SCN5A SNPs in 74 sporadic SUNDS cases and 115 healthy males
| Groups | genotype frequency (percentage) | Allele frequency (percentage) | |||||
|---|---|---|---|---|---|---|---|
| H558R | AA | AG | GG | P value | A | G | P value |
| SUNDS(n=74) | 67(90.5%) | 7(9.5%) | 0(0%) | 0.869 | 141(95.3%) | 7(4.7%) | 0.872 |
| Control(n=103) | 94(91.3%) | 9(8.7%) | 0(0%) | 197(95.6%) | 9(4.4%) | ||
| R1193Q | GG | GA | AA | G | A | ||
| SUNDS(n=74) | 66(89.2%) | 7(9.5%) | 1(1.3%) | 0.489 | 139(93.9%) | 9(6.1%) | 0.583 |
| Control(n=105) | 95(90.5%) | 10(9.5%) | 0(0%) | 200(95.2%) | 10(4.8%) | ||
| D1819D | CC | CT | TT | C | T | ||
| SUNDS(n=74) | 29(39.2%) | 29(39.2%) | 16(21.6%) | 0.012 | 87(58.8%) | 61(41.2%) | 0.0015 |
| Control(n=96) | 19(19.8%) | 42(43.8%) | 35(36.4%) | 80(41.7%) | 112(58.3%) | ||
| 3666+69G>C | GG | GC | CC | G | C | ||
| SUNDS(n=74) | 13(17.6%) | 25(33.8%) | 36(48.6%) | 0.004 | 51(34.5%) | 97(65.5%) | 0.0011 |
| Control(n=115) | 38(33%) | 47(40.9%) | 30(21.6%) | 123(53.5%) | 107(46.5%) | ||
DISCUSSION
The occurrence rates of SUNDS among Southeast Asian populations need further clarification. In northeast Thailand the annual mortality of death was reported to be 38 per 100,000 people aged 20–49 (4), which is the highest reported incidence in the world. However, the figure may have been overestimated because the cause of death in these cases was not confirmed by autopsies and microscopic examination. China is geographically close to Thailand and might also be expected to have a high occurrence rate. According to our initial investigation for SUNDS cases in Dongguan City during 1990–2001, the yearly occurrence rate of SUNDS in the region was approximately 0.6–1.5/100,000 (5). This study showed that the mean annual mortality of SUNDS in the three regions in the past three years was about 0.9–1.2/100,000. Based on these findings, we infer that the occurrence rate of the sudden death in southern China is about 1.0/100,000/year. Although the rate is not as high as other reported rates, the absolute number of annual SUNDS cases in China may be considerable because of the large population.
Young males between the ages of 21 and 40, and especially those around 30, are dominant in the SUNDS population. The population aged 21–40 may be confronted with the largest stress in both psychological and physical aspects, and perhaps subjects are at particular risk due to high levels of fatigue. From this point of view, the cause of some SUNDS cases may be focused on the factors related to overwork. Alternatively, the age of incidence may result from developmental factors combined with a genetic predisposition. Male victims occupied 93.23% of all cases and the prominent sex difference suggests possible pathogenesis of the lethal disease. Valladares found that during the rapid eye movement sleep, the male cardiac vagal tone significantly declined while sympathetic nerve activity markedly increased as compared with women and that the gender differences may be closely related to higher incidence of heart related problems in males (8).
SUNDS has been known to occur frequently in Southeast Asian regions with tropical or subtropical climates and hot weather. Tungsanga discovered that the majority of SUNDS in Thailand took place in summer (4), while our investigation showed a similar prominent characteristic of seasonal distribution (the peak months were April, May and June). Our study indicated that seasonal distribution of emergency fever patients rather than average air temperature in Southern China were positively correlated to that of SUNDS, which suggests that fever may be a factor in the occurrence of this fatal syndrome. Infection was once suspected to be the cause of SUNDS. Yap found the high infection rates of melioidosis bacteria among Thai in Singapore and the rate of SUNDS among them were significantly higher (9). Pyrogenic toxins of Staphylococcus aureus or other toxins with superantigen properties were also suspected to induce strong inflammatory responses (toxic shock syndrome) leading to sudden unexpected nocturnal deaths (10). The hypotheses of these infectious causes have not been verified. However, we cannot ignore an important fact that infection in SUNDS can cause fever. According to the above information and research, we have sufficient reasons to support that the epidemiological factors related to high body temperature (such as fever) may be one of crucial risk factors in the occurrence of SUNDS and the detailed mechanism deserves further exploration.
Wong reported high occurrence rates for SUNDS among Thai construction workers in Singapore (11). Tungsanga discovered that about 75% of SUNDS cases had an annual income per household of less than the mean per capita income in Thailand (4). This study indicated SUNDS most probably occurred among the workers with poor education and high labor intensity (blue-collar workers) especially in construction and electronic appliance factory workers. Although we didn’t know the exact percentage of blue-collar workers in the general population, it seemed that blue-collar workers may be the most susceptible SUNDS population in our study. A clinical experiment suggested the increasing nocturnal hypoxemia with over fatigue may be the primary abnormalities of SUNDS (12). It is reasonable to suggest that close attention should be paid to the relationship between excessive physical load (including fatigue and nocturnal working hours) and pathogenesis of SUNDS.
All the SUNDS patients died in nocturnal sleep and among 65 witnessed cases, 69.23% died between 0:00 and 4:00 am. Of these 65 cases, the chief clinical symptoms were abrupt breathing disorders in sleep such as outbursts of tachypnea, strange groans or gaspings, screams, and abnormal snores. It suggested that sudden breathing abnormalities in nocturnal sleep may be a key trigger for SUNDS. Previous studies hypothesized that disordered rapid eye movement sleep was probably associated with SUNDS or SIDS (13,14). Recently Paterson discovered that the abnormalities of the serotonergic system (role in regulating autonomic and respiratory function) in the medulla oblongata were responsible for the sudden death in some SIDS cases (15). Based on the above research, we assume that not only the cardiac but also the respiratory abnormalities in sleep and their interactions maybe involved in SUNDS.
Due to the similarities of the phenotype, SUNDS was presumed to be a disease allelic to Brugada syndrome. Vatta (7) first reported some SUNDS cases with family history were detected to have SCN5A mutations which accounted for 20–30% of Brugada syndrome. Recent studies in Australia also found SCN5A mutations in SUNDS (16). The present SCN5A gene screening showed two sporadic cases were detected to carry SCN5A mutations (one was previously confirmed to cause Brugada syndrome, the other is a novel synonymous mutation). We identified 4 SNPs in both SUNDS and control populations and found that there were significant difference in genotype and allele frequencies of C5457T, 3666+69G>C between two groups(P<0.05). It suggested that males with the genotype of 5457CC (OR=2.0, 95%CI=1.3–3.2) and 3666+69CC (OR=2.1, 95%CI=1.3–3.3) may be more at risk for SUNDS. The allele frequency of C5457T in Asian ethnics was reported to be significantly higher than that in Americans(17). Gouas (18) found C5457T minor alleles were significantly more frequent in the group with the shortest heart-rate corrected QT (QTc) interval compared with the group with the longest QTc interval from a cohort of 2,008 healthy subjects. This synonymous polymorphism C5457T may play an important role in the etiology of Chinese SUNDS. The pathological mechanisms at the molecular level, however, are unknown and further studies on mechanisms at the electrophysiological or molecular level are requried. 3666+69G>C is a novel intronic polymorphism and the possible mechanisms for its potential impact on SUNDS also requires further study. Between the two groups, there were no statistically significant differences in genotype and allele frequencies of A1673G (H558R) which has been found to have higher frequency in Brugada syndrome (17), which suggests that SUNDS may not be identical to Brugada syndrome in pathogenic mexhanisms.
In summary, we studied the epidemiological characteristics of SUNDS in China Han population for the first time. SUNDS mostly affects males aged 20–40 especially around 30 years. Fever and abrupt respiratory disorder may be correlated with the occurrence of SUNDS. According to our genetic screening data, the mutations or polymorphisms of SCN5A gene may be associated with Chinese SUNDS and the genotype of 5457CC and 3666+69CC may be Chinese SUNDS susceptible polymorphisms. The present survey is largely a descriptive research of epidemiology and has the limitation in lacking some basic data in general population. Further investigation on this nocturnal fatal disorder will be carried out with both epidemiological and genetic methods in the further case-control study.
ACKNOWLEDGEMENTS
This study was supported by Chinese National Natural Science Foundation grant 30500581 (to Cheng). This work was performed successfully due to the great help of many medico-legal experts including Dr Xing-Wu Chen of the institute of Criminal Science and technology of Dongguan, Dr Xue-Song Ye of the forensic medical center of Baoan District of Shenzhen Public Security Bureau , Dr Lu Yin of the forensic medical center of Longgang District of Shenzhen Public Security Bureau. We also express appreciation to Prof. Jiazhen Zhu for helpful discussion and the manuscript’s review. We also thank Dr. Yanrong Li, Haowei Xing, Zongfeng Ding for the analysis of the data.
Abbreviations
- SUNDS
sudden unexplained nocturnal death syndrome
- SNPs
the single nucleotide polymorphisms
- CI
confidence interval
- OR
odds ratio
REFERENCES
- 1.Guazon MP. Algunas notas sobre bangungut. Revista Filipina de Medicina Y Farmacia. 1917;8:437–442. [Google Scholar]
- 2.Cheng JD, Shi NQ, Makielski JC, et al. Epidemiology and genetic cause of sudden unexplained nocturnal death syndrome in southern China (abstract) Circulation. 2007;116:II–791. [Google Scholar]
- 3.Munger RG, Booton EA. Bangungut in Manila: sudden and unexplained death in sleep of adult Filipinos. Int J Epidemiol. 1998;27:677–684. doi: 10.1093/ije/27.4.677. [DOI] [PubMed] [Google Scholar]
- 4.Tungsanga K, Sriboonlue P. Sudden unexplained death syndrome in north-east Thailand. Int J Epidemiol. 1993;22:81–87. doi: 10.1093/ije/22.1.81. [DOI] [PubMed] [Google Scholar]
- 5.Cheng JD, Chen YC, Zeng JL, Li J, et al. A preliminary study of epidemiology of sudden manhood death syndrome in the peasant derived workers in Dongguan city (in Chinese) J Forensic Med. 2002;18:135–136. [PubMed] [Google Scholar]
- 6.Gervacio DG, Punzalan FE, Amarillo ML, et al. Sudden unexplained death during sleep occurred commonly in the general population in the Philippines: a sub study of the National Nutrition and Health Survey. J Clin Epidemiol. 2007;60:567–571. doi: 10.1016/j.jclinepi.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Vatta M, Dumaine R, Varghese G, et al. Genetic and biophysical basis of sudden unexplained nocturnal death syndrome(SUNDS), a disease allelic to Brugada syndrome. Human Molecular Genetics. 2002;11:337–345. doi: 10.1093/hmg/11.3.337. [DOI] [PubMed] [Google Scholar]
- 8.Valladares EM, Eljammal SM, Motivala S, et al. Sex differences in cardiac sympathovagal balance and vagal tone during nocturnal sleep. Sleep Med. 2008;9:310–316. doi: 10.1016/j.sleep.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 9.Yap EH, Chan YC, Goh KT, et al. Sudden unexplained death syndrome - a new manifestation in melioidosis? Epidemiol Infect. 1991;107:577–584. doi: 10.1017/s095026880004927x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Madani OA, Gordon AE, Weir DM, et al. Pyrogenic toxins of Staphylococcus aureus in sudden unexpected nocturnal deaths in adults and older children: factors influencing the control of inflammatory responses to toxic shock syndrome toxins. FEMS Immunology and Medical Microbiology. 1999;25:207–219. doi: 10.1111/j.1574-695X.1999.tb01345.x. [DOI] [PubMed] [Google Scholar]
- 11.Wong ML, Ong CN, Tan TC, et al. Sudden unexplained death syndrome: A review and update. Trop Geogr Med. 1992;44 (suppl):S1–S19. [PubMed] [Google Scholar]
- 12.Charoenpan P, Muntarbhorn K, Boongird P, et al. Nocturnal physiological and 15 biochemical changes in sudden unexplained death syndrome: a preliminary report of a case control study. Southeast Asian J Trop Med Public Health. 1994;25:335–340. [PubMed] [Google Scholar]
- 13.Vertes RP. A life-sustaining function for REM sleep: A theory. Neurosci & Biobehavioral Reviews. 1986;10:371–376. doi: 10.1016/0149-7634(86)90002-3. [DOI] [PubMed] [Google Scholar]
- 14.Tanchaiswad W. Is sudden unexplained nocturnal death a breathing disorder? Psychiatry Clin Neurosci. 1995;49:111–114. doi: 10.1111/j.1440-1819.1995.tb01872.x. [DOI] [PubMed] [Google Scholar]
- 15.Paterson DS, Trachtenberg FL, Thompson EG, et al. Multiple Serotonergic Brainstem abnormalities in Sudden Infant Death Syndrome. JAMA. 2006;296:2124–2144. doi: 10.1001/jama.296.17.2124. [DOI] [PubMed] [Google Scholar]
- 16.Doolan A, Langlois N, Chiu C, et al. Postmortem molecular analysis of KCNQ1 and SCN5A genes in sudden unexplained death in young Australians. Int J Cardiol. 2008;127:138–141. doi: 10.1016/j.ijcard.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Chen JZ, Xie XD, Wang XX, et al. Single nucleotide polymorphisms of the SCN5A gene in Han Chinese and their relation with Brugada syndrome. Chinese Medical Journal. 2004;117:652–656. [PubMed] [Google Scholar]
- 18.Gouas L, Nicaud V, Berthet M, et al. Association of KCNQ1, KCNE1, KCNH2 and SCN5A polymorphisms with QTc interval length in a healthy population. Eur J Hum Genet. 2005;13:1213–1222. doi: 10.1038/sj.ejhg.5201489. [DOI] [PubMed] [Google Scholar]