Summary
Background:
Myoepithelial cells are widely present in the breast, and their hyperplasia may result in a spectrum of disease ranging from myoepitheliosis to myoepithelial carcinoma.
Case Report:
A 46-year-old woman presented with a palpable mass in her right breast. Mammography and ultrasonography showed a lesion in the upper quadrant of the right breast with spiculated borders and shape. Excisional biopsy showed adenomyoepithelial adenosis.
Conclusions:
Although considered benign, adenomyoepithelial lesions tend to recur due to inadequate excision. Therefore, possibility of recurrence and even metastasis should be considered during follow-up of patients with a diagnosis of adenomyoepithelial lesions.
Key Words: Breast cancer, Adenomyoepithelial adenosis, Adenomyoepithelioma, Myoepithelial lesions
Abstract
Zusammenfassung
Hintergrund:
Myoepitheliale Zellen sind überall in der Brust zu finden. Eine Hyperplasie dieser Zellen kann zu einem weiten Erkrankungsspektrum von Myoepitheliose bis hin zu myoepithelialen Karzinomen führen.
Fallbericht:
Eine 46-jährige Frau wurde mit einer tastbaren Geschwulst in der rechten Brust vorstellig. Die mammo-graphische und Ultraschalluntersuchung zeigten eine Läsion mit spikulierter Begrenzung und Form im oberen Quadranten der rechten Brust. Die Untersuchung der Ex-zisionsbiopsie ergab eine adenomyoepitheliale Adenose.
Schlussfolgerungen:
Adenomyoepitheliale Läsionen gelten zwar als gutartig, auf Grund unvollständiger Entfernung rezidivieren sie aber häufig. Deshalb sollte das mögliche Auftreten von Rezidiven und sogar Metastasen während des Follow-ups von Patienten mit adenomyo-epithelialen Läsionen im Auge behalten werden.
Introduction
Hyperplastic and neoplastic lesions of the breast usually arise from atypical proliferation of epithelial cells [1]. Myoepithelial cells are widely present in the breast, and their hyperplasia may result in a spectrum of disease ranging from myoepitheliosis to myoepithelial carcinoma [2]. Adenomyoepithelial adenosis was shown to reveal high proliferative activity in both glandular epithelial and myoepithelial cells and was considered to be prone to progress to obvious carcinoma [2, 3]. Adenomyoepithelial adenosis can be well circumscribed or consist of multiple foci of randomly arranged ductules with luminal secretion, similar to microglandular adenosis. The simultaneous alteration and hypertrophy of epithelial and myoepithelial cells is a hallmark of adenosis, particularly adenomy-oepithelial adenosis [4]. In this paper, a case of adenomyoep-ithelial adenosis is reported and discussed on the basis of clinical, radiological, and pathological findings.
Case Report
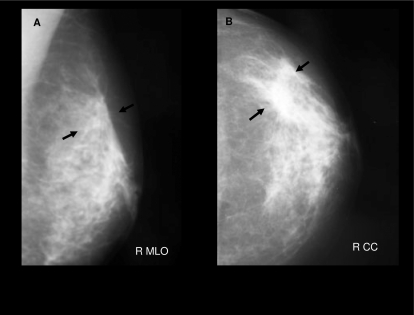
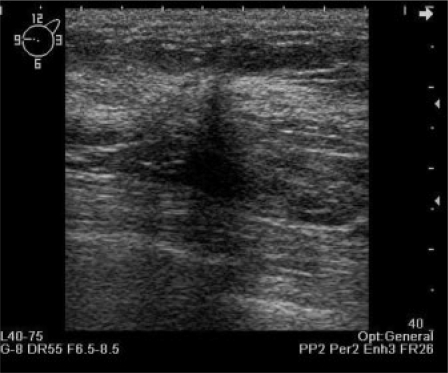
A 46-year-old woman presented with a right breast lump that had been palpable for 2 months. She did not have any history of cancer or exposure to radiotherapy. The family history of the patient revealed no cases of breast cancer. She had been under treatment for mastalgia for 6 months. She was referred to our hospital for a diagnostic mammography and ultrasonography (USG). Bilateral mammography showed an irregularly shaped mass with spiculated margins and associated pleomorphic microcalcifications in the upper quadrant of the right breast (fig. 1). USG showed an irregular spiculated hypoechoic mass of 12 × 13 mm with posterior acoustic shadowing (fig. 2). The radiological features of the lesion were defined as highly suggestive of malignancy (BI-RADS 5). There were also enlarged axillary lymph nodes on both sides. The biggest lymph node in the right axilla demonstrated ultrasonographic features suspicious for malignancy. Excisional biopsy of the breast mass was performed by another department of our hospital. The pathology report revealed fibro-cystic changes. As no radiological-pathologic correlation was found, USG was repeated, and the mass was shown to be persisting.
Fig. 1.
MLO and B CC mammograms of the patient. An irregular spic-ulated dense mass (arrows) is seen in the upper outer quadrant of the right breast.
Fig. 2.
qUltrasonog-raphy of the right breast confirms an irregular spiculated hypoechoic mass.
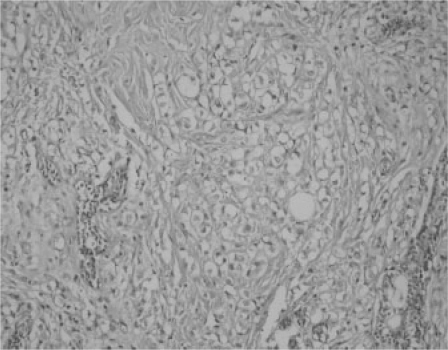
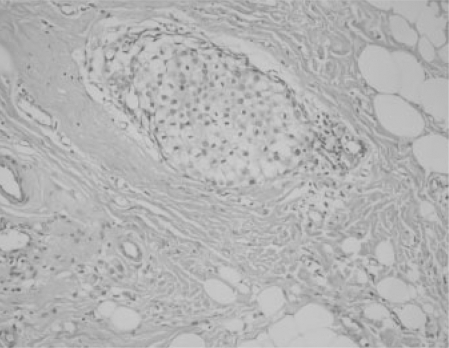
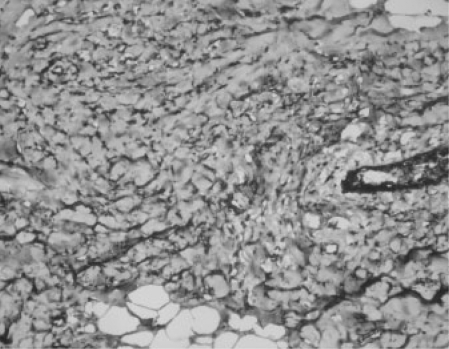
The patient was referred to our department for re-excision. On physical examination, the mass was palpable under the incisional scar. We informed the patient about biopsy techniques including core biopsy, but due to anxiety she decided to undergo excisional biopsy. Excisional biopsy was performed. A specimen mammogram was taken for approval of complete excision. Since microcalcifications were observed close to the resection margin, we re-excised an at least 1 cm wide rim of normal tissue to provide clear margins. Histopathology showed diffuse proliferation of round or irregular tubular structures lined by a cuboidal to columnar epithelium. There was a prominent focally hyperplastic myoepithelial cell layer with strikingly clear cytoplasm. There was no significant nuclear atypia or mitotic activity (figs. 3 and 4). Immunocytochemical staining showed positive staining with SMA, S100, p63, and high keratin in myoepithelial cells (fig. 5). These appearances were diagnostic for adenomyopethelial adeno-sis. Fine needle aspiration cytology (FNAC) obtained from axillary lym-phadenopathies under USG guidance showed no evidence of malignancy. Therefore, we decided to follow up the patient for her axillary lym-phadenopathies. In her control USG, the dimensions of the lymph nodes have regressed to 4 × 6 mm. There is no evidence of recurrence and lym-phadenopathy for 10 months from her last surgery.
Fig. 3.
The myoep-ithelial cells are increased in size and surrounding the duc-tus (H and E ×200).
Fig. 4.
Solid islands consisting of myoep-ithelial cells (H and E×200).
Fig. 5.
Positive brown SMA staining in the myoepithelial cytoplasm.
Discussion
Adenomyoepithelial lesions frequently appear in the salivary gland, skin, and parathyroid [5, 6]. Myoepithelial cells are normally present in the breast, and are located between the luminal cells and the basal lamina of ductules. Tavassoli [3] classified the myoepithelial lesions of the breast as myoepitheliosis, adenomyoepithelioma, and malignant myoepithelioma (myoepithelial carcinoma). She also subdivided adenomyoepithe-liomas according to their cell predominance as spindle cells, tubular, lobulated, and carcinoma arising in adenomyoepithe-lioma. Pia-Foschini et al. [7] suggested that it may be more appropriate to abandon the use of apocrine adenosis (adenomyoepithelial adenosis) and to report these lesions as tubular adenomyoepithelioma. Moinfar [4] described adenomyoepithelial adenosis as a rare variant of adenosis with a prominent myoepithelial component within the involved glands (hypertrophy and/or hyperplasia of myoepithelial cells). The tubules show a prominent myoepithelial cell component. The luminal epithelial cells and basally located myoepithelial cells not infrequently show enlarged nuclei and prominent nucleoli. Apocrine or squamous metaplasia may be present. Adenomy-oepithelial adenosis cannot reliably be separated from a small (microscopic) adenomyoepithelioma [4]. The heterogeneous cell population with simultaneous hypertrophy of epithelial and myoepithelial cells in our case proves the lesion's benign nature.
The typical histological appearance of a benign adenomyoep-ithelioma consists of acinar structures composed of an inner layer of epithelial cells with eosinophilic cytoplasm surrounded by prominent myoepithelial cells [1]. The myoepithelial cells frequently have clear cytoplasm and are shown to be positive for smooth muscle myosin, S100 protein, and actin [8]. Adenomyoepitheliomas present as a palpable, sometimes tender and peripherally located masses [7]. Imaging may demonstrate malignant features but no uniform criteria were reported to differentiate benign adenomyoepitheliomas from malignant ones. The gross sizes range from 0.5 to 5 cm (median 1.5 cm) [9]. Howlett et al. [10] described the imaging features for discrimination of benign from malignant adenomyoepithe-lioma. Benign adenomyoepitheliomas have smooth margins without any structural abnormalities in the surrounding tissue. Malignant ones are irregularly bordered lesions with surrounding structural abnormalities, and posterior shadowing at ultrasonography was also demonstrated. In our patient, the sonographic and mammographic appearances suggested malignancy. Breitwieser et al. [11] for the first time demonstrated a benign adenomyoepithelioma characterized by magnetic resonance (MR) mammography and confirmed by MR-guided vacuum-assisted biopsy. The time course of signal enhancement determined by MR imaging gave information suggestive for malignant transformation, while the appearance on T2-weighted images was indicative of a benign lesion.
Adenomyoepitheliomas are rare and may show wide variations, and they may be confused with other myoepithelial/stromal cell-rich structures that mimic this lesion. Therefore, a core biopsy should be preferred to FNAC [12, 13]. Yahara et al. [9] reported that after excision of the lesion by mammo-tome biopsy, they provided an exact diagnosis and complete removal of benign adenomyoepithelioma. Although in our case core biopsy or stereotactic biopsy were recommended by radiologists, our patient preferred total excision which provided an exact diagnosis and surgical treatment in the same operation. Specimen mammography obtained after resection of the lesion enabled us to provide clear margins for complete treatment by supplying information about the margins of the excisional biopsy. We decided to follow up our patient's lym-phadenopathies since benign adenomyoepitheliomas have a low tendency to develop axillary lymph node metastasis [3]. On control USG and physical examination, the lymphadeno-pathies had almost disappeared. The patient has been symptom-free for 10 months.
As both benign and malignant adenomyoepitheliomas have a tendency to recur, re-excision is recommended in cases of suspected inadequate margins [14]. The best predictors of recurrence are initial incomplete or close excision margins. Therefore, correct preoperative diagnosis is important for surgical planning. Myoepithelial carcinoma may be observed if one or both cellular types have undergone malignant degeneration. Myoepithelial carcinoma shows metastases via the hematoge-nous route rather than the lymphatogenous route [15]. Preoperative imaging findings are not distinctive. A preoperative diagnosis by FNAC may be difficult, therefore core needle biopsy may be more suitable. Mammotome biopsy has been recommended instead of core needle biopsy because the latter provides a smaller amount of tissue [9].
If carcinoma is diagnosed at the final pathological examination in a totally excised adenomyoepithelioma which was pre-operatively thought to be benign, then the lesion should be re-evaluated and treated as a carcinoma thereafter. The surgical treatment of a malignant tumor is similar to other invasive types of breast tumors. Wide local excision with negative margins or mastectomy with axillary dissection is the preferred treatment [16]. There is not enough information about role of chemotherapy, radiotherapy, or hormone therapy. The metastatic sites have been reported as axillary lymph nodes, lungs, brain, bones, and thyroid gland [17].
Conclusion
Although most adenomyoepithelial lesions are benign, malignant degeneration of one or both cellular components may occur. Preoperative diagnostic evaluation is important to avoid unnecessary wide surgical resections and mastectomies. Therefore, cytopathologists should pay attention to the cytologic appearance and immunocytochemical features of the lesion. Close follow-up is recommended by both radiologists and surgeons because of the potential for recurrence and even metastasis despite the lesion being reported as benign.
Acknowledgements
The authors would like to thank Nuran Sungu, MD for preparing the pathology illustrations.
References
- 1.Rosen PP. Adenomyoepithelioma of the breast. Hum Pathol. 1987;18:1232–1237. doi: 10.1016/s0046-8177(87)80406-9. [DOI] [PubMed] [Google Scholar]
- 2.Tsuda H, Mukai K, Fukutomi T, Hirohashi S. Malignant progression of adenomyoepithelial adenosis of the breast. Pathol Int. 1994;44:475–479. doi: 10.1111/j.1440-1827.1994.tb01713.x. [DOI] [PubMed] [Google Scholar]
- 3.Tavassoli FA. Myoepithelial lesions of the breast. Myoepitheliosis, adenomyoepithelioma, and myoepithelial carcinoma: Am J Surg Pathol. 1991;15:554–568. doi: 10.1097/00000478-199106000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Moinfar F. Adenosis. In: Moinfar F, editor. Essentials of Diagnostic Breast Pathology. Berlin: Springer; 2007. p. 31. [Google Scholar]
- 5.Tsuji N, Tateishi R, Ishiguro S, Terao T, Higashiyama M. Adenomyoepitheloma of the lung. Am J Surg Pathol. 1995;19:956–962. doi: 10.1097/00000478-199508000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Sciubba JJ, Brannon RB. Myoepithelioma of salivary glands: report of 23 cases. Cancer. 1982;49:562–572. doi: 10.1002/1097-0142(19820201)49:3<562::aid-cncr2820490328>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 7.Pia-Foschini Mi, Reis-Filho JS, Eusebi V, Lakhani SR. Salivary gland-like tumours of the breast: surgical and molecular pathology. J Clin Pathol. 2003;56:497–506. doi: 10.1136/jcp.56.7.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosen PP. Myoepithelial neoplasms. In: Rosen PP, editor. Rosen's Breast Pathology. Philadelphia: Lippincott Williams and Wilkins; 2001. pp. 121–138. [Google Scholar]
- 9.Yahara T, Yamaguchi R, Yokoyama G, Yamaguchi M, Nakagawa S, Toh U, Shirouzu K, Kage M, Fujii T. Adenomyoepithelioma of the breast diagnosed by a mammotome biopsy: report of a case. Surg Today. 2008;38:144–146. doi: 10.1007/s00595-007-3591-8. [DOI] [PubMed] [Google Scholar]
- 10.Howlett DC, Mason CH, Biswas S, Sangle PD, Rubin G, Allan SM. Adenomyoepithelioma of the breast: spectrum of disease with associated imaging and pathology. AJR Am J Roentgenol. 2003;180:799–803. doi: 10.2214/ajr.180.3.1800799. [DOI] [PubMed] [Google Scholar]
- 11.Breitwieser C, Diekmann F, Diekmann S, Mora-wietz L, Taupitz M. Adenomyoepithelioma of the breast: MR mammography and histologic confirmation by MR guided vacuum assisted biopsy. European J Rad Extra. 2005;53:59–62. [Google Scholar]
- 12.Iyengar P, Ali SZ, Brogi E. Fine needle aspiration cytology of mammary adenomyoepithelioma: a study of 12 patients. Cancer. 2006;108:250–256. doi: 10.1002/cncr.21839. [DOI] [PubMed] [Google Scholar]
- 13.Catena F, Santini D, Di Saverio S, Ansaloni L, Taffurelli M. Adenomyoepithelioma of the breast: an intricate diagnostic problem. Breast Care. 2008;3:125–127. doi: 10.1159/000119727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nadelman CM, Leslie KO, Fishbein MC. Benign, metastasizing adenomyoepithelioma of the breast: a report of 2 cases. Arch Pathol Lab Med. 2006;130:1349–1353. doi: 10.5858/2006-130-1349-BMAOTB. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed AA, Heller DS. Malignant adenomyoepithelioma of the breast with malignant proliferation of epithelial and myoepithelial elements: a case report and review of the literature. Arch Pathol Lab Med. 2000;124:632–636. doi: 10.5858/2000-124-0632-MAOTBW. [DOI] [PubMed] [Google Scholar]
- 16.Woo EK, James AD, Mercer J, Allan SM, Howlett DC. Case report: myoepithelial carcinoma of the breast: a case report with imaging and pathological findings. Br J Radiol. 2005;78:444–446. doi: 10.1259/bjr/73238635. [DOI] [PubMed] [Google Scholar]
- 17.Chen PC, Chen CK, Nicastri AD, Wait RB. Myoepithelial carcinoma of the breast with distant metastasis and accompanied by adenomyoepitheliomas. Histopathology. 1994;24:543–548. doi: 10.1111/j.1365-2559.1994.tb00573.x. [DOI] [PubMed] [Google Scholar]