Abstract
Background and Problem Statement
The goals of the patient-centered medical home (PCMH) include the efficient and effective delivery of patient-centered care in the context of a continuity relationship. In residency training programs, competing demands on faculty, residents, and office staff create considerable challenge in demonstrating these vital attributes of the PCMH to residents. Given the emphasis on the PCMH, primary care residency programs need to strengthen the methods for teaching and modeling continuity, office efficiency, and team-based approaches to care.
Intervention
We designed and implemented a new system of “patient care management teams” in our family medicine residency and evaluated its impact on team members. Our quality improvement interventions included the creation of team structures linking faculty advisors and residents with patients, intrateam management of office tasks, and the implementation of multidisciplinary team meetings.
Evaluation
We surveyed faculty (n = 11), residents/fellows (n = 39), and staff (n = 12) before and at 2 points after the patient care management team interventions, and we collected patient satisfaction data during the intervention time period.
Results
The intervention resulted in significant improvements in perceptions of continuity of patient care, office efficiency, and team communication before and after the team interventions. During a 2-year period, the greatest improvements were in the areas of office efficiency and continuity of care. Independent patient satisfaction scores correlated with patient care management team improvements.
Conclusions
Team structures, streamlined team-based management of routine office tasks, and consistent and frequent multidisciplinary meetings can improve the sense of continuity, office efficiency, and team collaboration in primary care residency clinics.
Background
Key features of the patient-centered medical home (PCMH) include the efficient and effective delivery of patient-centered care in the context of a continuity relationship.1–3 Residents in primary care training programs need to be exposed to effective PCMH models4,5 to allow them to create and sustain the PCMH approach in their future practices. The traditional structure of primary care residency may create barriers to providing patient-centered care efficiently and effectively.6,7 The multiple demands on faculty, residents, and staff, coupled with the complexities of our current health system, may lead to fragmentation and inefficiencies of care provided in the residency clinic. Primary care residency programs need to strengthen the methods they use to teach and model PCMH concepts in their office settings.8 Our family medicine program conducted a practice-based quality improvement project in an effort to overcome some of the existing barriers to efficient, patient-centered, collaborative team care.
Continuity of care, office efficiency, and team-based care have all been shown to be important components of high-quality care. Sustained continuity of care can improve patient health by decreasing hospitalizations and emergency department utilization, and it can enhance the delivery of preventive and primary care services.9 Continuity of care has also been associated with improved patient satisfaction10–12 and improved medication adherence.13 Systems designed to enhance office efficiency, such as electronic medical records, have also been shown to have a positive impact on members of the clinic team. Efficiency in communication is a key aspect of the improved satisfaction of providers using an electronic medical record.14 Team-based care has proven efficacy for ensuring quality care as well. Team decision making accounts for improvements in patient care as well as organizational effectiveness.15 Team-based care can be beneficial in chronic disease and terminal illness care16,17 and has improved multiple patient outcomes in the management of congestive heart failure.18 These core elements of continuity, efficiency, and team care need to be enhanced and emphasized in our primary care residency clinics so that our graduates enter practice with a better understanding of the PCMH.
Problem Statement
In MacNeal Family Medicine Center, as in other residency clinics,19 patients, staff, and/or physicians had expressed dissatisfaction with various aspects of our office functioning. After communicating with key stakeholders, we identified 3 main areas of concern: continuity of care, office efficiency, and team communication. Continuity of care was complicated by staffing patterns typical in most family medicine residencies. Faculty and residents are all part-time providers who see patients 1 to 4 half-days per week; resident availability varies by year of training and by rotation and call schedule. This scheduling limits the times that the same physician and patient can match availability for office visits.
Second, complex schedules and transitions in physician assignments created confusion in routine office tasks. When staff members received phone messages from patients, they were often unsure about which physician was responsible for addressing the patient's concerns when the primary physician was postcall, on vacation, or on an away rotation. The designated covering physician might be in another location, be unfamiliar with the patient, and not have access to the patient chart. Staff might contact 2 or 3 physicians to get an answer for a time-sensitive patient care issue; nonurgent messages might be left unanswered for several days if the primary provider was unavailable. Other inefficiencies were observed when routine laboratory reports, radiologic studies, or other results were sent to a physician who was not the primary provider of the patient. Results frequently were routed to the precepting attending rather than the resident who saw the patient at the office visit. Delays occurred while rerouting the results to the correct provider. Many test results were interpreted and managed solely by the resident unless the resident proactively sought out consultation from an available faculty member. There was no consistent faculty supervision of this aspect of patient care.
Our third area of challenge was the limited multidisciplinary communication in our office. We had a system of horizontal team meetings—faculty met with faculty; residents with residents; and office staff had their own separate meeting. There were no systemic opportunities for multidisciplinary team communication or problem solving. Faculty, residents, and staff had little understanding about each other's roles and duties. This limited contact fostered misperceptions about each other's responsibilities and activities, and it generated frustration and rifts between these groups.
In an effort to address the issues we faced in our office and to demonstrate the PCMH concepts of continuous, efficient, team-based care, we designed and implemented patient care management teams (PCMTs) in our residency program. To evaluate their effectiveness, we surveyed the faculty, residents, and office staff before, during, and after the team system was implemented. We also reviewed independent patient satisfaction data for the same time period.
Intervention
Implementation of PCMTs
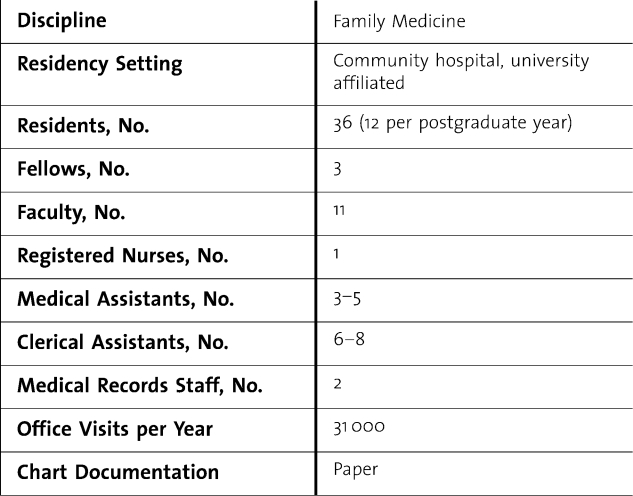
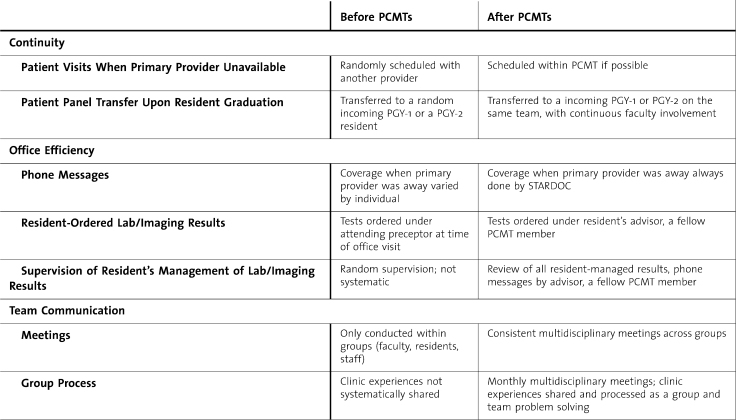
Our family medicine residency program is located in a community-based hospital near Chicago, Illinois, and our program has affiliations with several area medical schools. table 1 describes our office characteristics. The changes implemented centered around our 3 main areas of concern: randomness in continuity of care between patients and providers, poor office efficiency in managing routine medical office tasks, and limited communication between physicians and office staff. All faculty, residents, and staff participated in the implementation of the PMCTs. table 2 summarizes our interventions.
Table 1.
Office Characteristics
Table 2.
Office Functioning Before and After Patient Care Management Teams (PCMTs)
Continuity Team Structure
Our first step toward advancing continuity of care was to build a structure of 4 teams within the office. Each PCMT included 2 to 3 faculty members and their respective advisees (3–4 residents), for a total of 8 to 12 physicians in each team. Two teams were assigned to each of 2 nursing stations. The purpose of the teams was to care for patients within a consistent team of providers who were familiar with their needs and health status. Patient visits would be scheduled and routine office tasks performed within the team. The goals of the PCMTs and the guidelines for team operations were introduced at an office-wide meeting in June 2007 to all faculty, residents, and staff; the guidelines were made available on our intranet.
Office Efficiency Interventions
Another key component of our new processes involved improving efficiency of routine office activities in our busy, multiprovider medical practice. We developed the StarDoc role as a system to manage and prioritize a large volume of patient messages. There were 4 assigned StarDocs per half-day of clinic—one for each PCMT. Each nonintern physician team member served as StarDoc 4 to 6 times per month on half-days when he/she was in the office. The StarDoc was responsible for first-line decisions for the team's patient care. He/she reviewed all messages taken by staff for that team's patients and served as the primary contact point for a staff member's questions regarding care. The StarDoc also had access to resident rotation schedules, faculty and resident vacation schedules, and postcall information, and he/she could quickly determine whether a message could be triaged to the patient's primary physician or needed his/her immediate action. If any provider on the team was on vacation, the StarDoc took responsibility for answering phone messages for his/her patients. The new role helped staff members identify who would be responsible for handling patient questions and created a structure to manage and coordinate patient care by a stable group of physicians.
The second office efficiency strategy focused on the consistent management of lab and radiology reports within the team. When residents ordered labs and imaging studies, they now co-ordered them under their faculty advisor's name, a fellow team member. This process ensured that both the resident and the faculty advisor would review the lab and imaging results. The resident documented his/her course of action on the results form and forwarded these forms for their advisor/team member to review. This process allowed for consistent supervision of residents' postvisit decision making and patient care. The office staff also had clearer guidelines on who should receive copies of the patients' test results. In addition, faculty advisors reviewed all phone message documentation after the resident handled a message. Faculty now were actively supervising the management of their resident advisees' patient care while becoming more familiar with the medical issues and needs of the PCMT's patients. The new processes clarified who was responsible for managing and supervising these routine office tasks within each PCMT.
Team Meetings and Megaclinic
The third goal was to improve the vertical team communication between faculty, residents, medical assistants, and clerical assistants. The PCMTs were introduced in June 2007 during an office-wide meeting, which was 1 of 6 bimonthly multidisciplinary team meetings for the first year. During the second year, team meeting frequency increased to monthly. These office-wide meetings set the stage to improve team communication, team identity, and group cohesion. Faculty, residents, and staff were all invited to attend meetings, which occurred during a noon conference time. During the course of 24 months there were 18 multidisciplinary team meetings. In the first year, a variety of team-building methods were used to address challenges of our new system, clarify changes in roles and responsibilities, and facilitate multidisciplinary team communication and problem solving. In the second year, we implemented a megaclinic model during these meetings to foster understanding and enhance team problem solving among faculty, residents, and staff.20 In the megaclinic, we asked a faculty member, resident, or staff person to share the details of how his/her busy clinic day progressed. This team member described the multiple tasks, roles, and demands of typical clinic day, which helped other team members “walk in his/her shoes.” Team members shared their expectations, frustrations, and personal emotional experiences as they interacted with patients, staff, and physicians throughout their clinic session. These discussions were powerful in increasing understanding and building a sense of cohesion and teamwork. Team meetings provided new opportunities for direct communication and problem-solving strategies between team members of various roles.
Evaluation
Practice-Based Evaluation of PCMTs
The process of building PCMTs into our health clinic provided a natural opportunity to evaluate our practice-based quality improvement project. We used this model with residents to teach practice-based evaluation while simultaneously assessing the effectiveness of the PCMT approach. Once we identified the problems and developed and implemented solutions, we measured the impact of the interventions on the team members. Our questions were as follows:
Do PCMT structures and strategies improve the faculty, resident, and staff's perceptions of patient continuity of care, office efficiency, and team communication?
Are there significant differences between the perceptions of faculty, residents, and staff in continuity of care, office efficiency, or team communication?
Do the PCMT changes correlate with patient satisfaction ratings?
Survey Method
A time series analysis using a survey method was used to evaluate the team members' perceptions of the effectiveness of the PCMT structure and strategies. A PCMT survey was administered to 3 different groups (faculty, residents, and staff) at 3 time points: time 1, before the team structure and strategies were introduced; time 2, 9 months after the PCMTs started; and time 3, 20 months after the PCMT system was in place.
The PCMT survey was composed of 16 questions, with responses made on a 5-point Likert scale. The survey consisted of questions related to 3 factors—(1) patient continuity of care (CC; 6 items), (2) office efficiency (OE; 4 items), and (3) team communication (TC; 6 items)—and a total score. Factor analysis was used to verify independence of the 3 subscales of this instrument. This confirmed that subscales were independent factors with loadings ranging from 3.40 to 1.74 to 0.81 and all 3 factors accounting for 91% of the survey's variance.
Survey participants included 11 faculty, 39 residents/fellows, and 11 staff in our residency program from 2007–2009. Thirty-nine team members completed surveys in the first year, 45 at 9 months, and 38 in the second year. Response rates ranged from 63% to 70% during the 3 time periods.
Results
The mean scores on 3 subscales—continuity of care, office efficiency, and communication—and the total score were compared using an analysis of variance (ANOVA) to determine whether there were significant differences during the 3 time periods—before the PCMT intervention, after 9 months, and after 20 months. Initially, we determined whether there were significant differences between the PCMT scores among the 3 groups—faculty, resident/fellows, and staff. An ANOVA showed that there were no significant differences between these groups. Consequently, the group scores were used to determine significant differences in the PCMT factors during the 3 time periods.
Continuity, Office Efficiency, Team Communication, and Total PCMT Factors
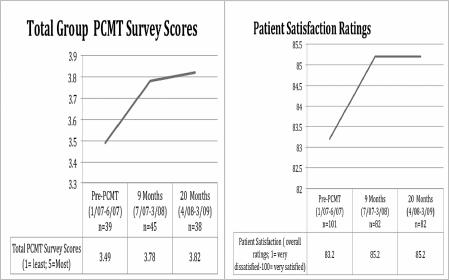
When mean scores for all participants were compared, there were significant differences from the pre-PCMT scores to the 9-month and to the 20-month follow-up scores on all 3 scales and the total scores (table 3) The greatest improvement was in the area of office efficiency (eg, StarDoc and supervision of test results); the second area of greatest improvement was in continuity. Perceptions of the areas of least to most improvement were consistent among faculty, residents, and staff over time. Overall group results indicated significant improvement in our continuity of care for patients, efficiency of routine office tasks, and communication among team members. These changes were maintained during the 20-month timeframe.
Table 3.
We also compared our patient satisfaction results from our independent consulting firm, Press Ganey, with our PCMT scores during the 3 time periods: before PCMT (January 2007–June 2007) and at 9 months (July 2007–March 2008) and 20 months after the intervention (April 2008–March 2009). Press Ganey scores are an overall rating of patients' satisfaction (1 = very dissatisfied to 100 = very satisfied) on a range of health care services at our center. This showed a positive association between patient satisfaction scores and the PCMT survey scores. The greatest increase in scores was between the pre-PCMT and 9 months after implementation, and the data show the positive changes have been maintained. A comparison between patient satisfaction scores and total PCMT scores during the 3 time periods is shown in table 4.
Table 4.
Patient satisfaction and PCMT Survey Scores
Discussion
Results from this project confirm that our structure and strategies for addressing the challenges of continuity, office inefficiency, and limited team communication in residency clinics are perceived positively by faculty, residents, and staff. Our solutions focused on 4 PMCTs comprising faculty physicians and their resident advisees. Office tasks were managed by identifying a StarDoc for each team to triage patient messages and faculty advisors to review the lab and imaging results of their team members. We also instituted multidisciplinary meetings to encourage frequent and consistent communication. These meetings promoted discussions around clinic challenges and problem solving and resulted in a noticeable improvement in clinic climate and team morale.
We also experienced unexpected effects that generated new operational challenges. The StarDoc system of answering patient messages efficiently was so successful that patients called more frequently. StarDocs became overwhelmed at times with callbacks and patient requests; the front desk experienced increased call volumes that stressed our office's telephone system.
Limitations
There were several limitations to this study. First, change was measured via group change scores, not within-subject changes from the pretests to the posttests. Participants completing the pretest were not always the same participants at the posttest. We also had a small number of faculty participants (n = 7), which limited the power of our data analysis. Two of the evaluators were developers of this project, which may have biased the results. There is a positive association between the patient satisfaction scores and PCMT interventions; however, it is unclear whether the association is causal.
Future Directions
The results from our practice-based quality improvement project will assist us in continuing to improve our new PCMT structure. We saw the least improvement in team communication. To address this, we have included medical and clerical assistants as members of one of our teams, in the hope that adding them as permanent team members will further increase cohesion and enhance problem-solving capabilities. Second, we are addressing the issue of too many phone calls by coaching StarDocs to avoid overuse of telemedicine and refer patients to the clinic for care. This practice should increase our residents' office visits. We also plan to implement an electronic medical record, which will allow physicians not in the office to answer phone messages remotely while referring to the patient record, allowing us to rely less heavily on the StarDocs.
Conclusions
Overall, this project helped us improve continuity of care, reduce inefficiencies, and work more cohesively as a team. Our initial results have created opportunities for other areas of future progress in further improving team functioning. We have a stronger foundation for training family medicine physicians on how to ensure that the core values of the PCMH can be achieved in a busy, multiphysician practice. The intervention showed us that the competing goals of continuity, efficiency, and residency training can be achieved by creating and clearly structuring PCMTs.
Footnotes
Tricia Hern, MD, is from the Community Health Network Family Medicine Residency Program; Mary Talen, PhD, is from the MacNeal Family Medicine Residency Program; Christopher Babiuch, MD, is from the MacNeal Family Medicine Residency Program; and Ramon Durazo-Arvizu, PhD, is from the Department of Preventive Medicine and Epidemiology, Loyola University Chicago.
This work was presented in May 2008 at the Society of Teachers of Family Medicine Annual Conference, Baltimore, MD.
This project was conducted while Dr Hern was a member of the faculty of the MacNeal Family Medicine Residency Program.
Editor's Note: The online version of this article includes additional materials (37.5KB, doc) such as data tables, survey or interview forms or assessment tools.
References
- 1.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home. 2007. http://www.acponline.org/advocacy/where_we_stand/medical_home/approve_jp.pdf?hp, accessed August 24, 2009.
- 2.Robert Graham Center: Center for Policy Studies in Family Medicine and Primary Care. The Patient Centered Medical Home: History, Seven Core Features, Evidence and Transformational Change. November 2007.
- 3.Task Force 1. Report of the Task Force on patient expectations, core values, reintegration, and the new model of family medicine. Ann Fam Med. 2004;2(suppl 1):S33–S50. [Google Scholar]
- 4.Residency Program Solutions Criteria for Excellence. 7th ed. Leawood, KS: American Academy of Family Physicians; 2008. [Google Scholar]
- 5.Larsen E., Fihn S. D., Kirk L. M. The future of general internal medicine: report and recommendations from the Society of General Internal Medicine (SGIM) Task Force on the Domain of General Internal Medicine. J Gen Intern Med. 2004;19:69–77. doi: 10.1111/j.1525-1497.2004.31337.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xakellis G., Bennett A. Improving clinic efficiency of a family medicine teaching clinic. Fam Med. 2001;33(7):533–538. [PubMed] [Google Scholar]
- 7.Dumont-Driscoll M., Barbian L., Pollock B. Pediatric residents' continuity clinics: how are we really doing? Pediatrics. 1995;96(4):616–621. [PubMed] [Google Scholar]
- 8.Weinberger S., Smith L., Collier V. for Education Committee of the American College of Physicians. Redesigning training for internal medicine. Ann Intern Med. 2006;144(12):927–932. doi: 10.7326/0003-4819-144-12-200606200-00124. [DOI] [PubMed] [Google Scholar]
- 9.Cabana M., Jee S. Does continuity of care improve patient outcomes? J Fam Pract. 2004;53(12):975–980. [PubMed] [Google Scholar]
- 10.Morgan E., Pasquarella M., Holman J. Continuity of care and patient satisfaction in a family practice clinic. J Am Board Fam Pract. 2004;17(5):341–346. doi: 10.3122/jabfm.17.5.341. [DOI] [PubMed] [Google Scholar]
- 11.Fan V., Burman M., McDonell M., Fihn S. Continuity of care and other determinants of patient satisfaction with primary care. J Gen Intern Med. 2005;20:226–233. doi: 10.1111/j.1525-1497.2005.40135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sualtz J., Albedaiwi W. Interpersonal continuity of care and patient satisfaction: a critical review. 2004;2:445–451. doi: 10.1370/afm.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brookhart M. A., Patrick A. R., Schneeweiss S. Physician follow-up and provider continuity are associated with long-term medication adherance: a study of the dynamics of statin use. Arch Intern Med. 2007;167(8):847–852. doi: 10.1001/archinte.167.8.847. [DOI] [PubMed] [Google Scholar]
- 14.Joos D., Chen Q., Jirjis J., Johnson K. An electronic medical record in primary care: impact on satisfaction, work, efficiency and clinic processes. AMIA Annu Symp Proc. 2006. pp. 394–398. [PMC free article] [PubMed]
- 15.Lemiux-Charles L., McGuire W. What do we know about health care team effectiveness?: a review of the literature. Med Care Res Rev. 2006;63(3):263–300. doi: 10.1177/1077558706287003. [DOI] [PubMed] [Google Scholar]
- 16.Bodenheimer T., Wagner E., Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288:1775–1779. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 17.Zimmer J., Groth-Juncker A., McCusker J. A randomized controlled study of a home health care team. Am J Public Health. 1985;75(2):134–141. doi: 10.2105/ajph.75.2.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grady K., Dracup K., Kennedy G. Team management of patients with heart failure: a statement for healthcare professionals from the Cardiovascular Nursing Council of the American Heart Association. Circulation. 2000;102:2443–2456. doi: 10.1161/01.cir.102.19.2443. [DOI] [PubMed] [Google Scholar]
- 19.Yancy W. S., Jr, Macpherson D. S., Hanusa B. H. Patient satisfaction in a resident and attending ambulatory care clinics. J Gen Intern Med. 2001;16:755–762. doi: 10.1111/j.1525-1497.2001.91005.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sternlieb J. Teaching housekeeping: learning to manage the emotional impact of patient care. Families, Systems, and Health. 2008;26(3):356–364. [Google Scholar]