Abstract
Background
Supervision is central to resident education and patient safety, yet there is little published evidence to describe a framework for clinical supervision. The aim of this study was to describe supervision strategies for on-call internal medicine residents.
Methods
Between January and November 2006, internal medicine residents and attending physicians at a single hospital were interviewed within 1 week of their final call on the general medicine rotation. Appreciative inquiry and critical incident technique were used to elicit perspectives on ideal and suboptimal supervision practices. A representative portion of transcripts were analyzed using an inductive approach to develop a coding scheme that was then applied to the entire set of transcripts. All discrepancies were resolved via discussion until consensus was achieved.
Results
Forty-four of 50 (88%) attending physicians and 46 of 50 (92%) eligible residents completed an interview. Qualitative analysis revealed a bidirectional model of suggested supervisory strategies, the “SUPERB/SAFETY” model; an interrater reliability of 0.70 was achieved. Suggestions for attending physicians providing supervision included setting expectations, recognizing uncertainty, planning communication, having easy availability, reassuring residents, balancing supervision, and having autonomy. Suggested resident strategies for seeking supervision from attending physicians included seeking input early, contacting for active clinical decisions or feeling uncertain, end of life issues, transitions in care, or help with systems issues. Common themes suggested by trainees and attending physicians included easy availability and preservation of resident decision-making autonomy.
Discussion
Residents and attending physicians have explicit expectations for optimal supervision. The SUPERB/SAFETY model of supervision may be an effective resource to enhance the clinical supervision of residents.
Background
In 2008, an Institute of Medicine report1 examined the impact of duty hour regulations that were prompted in part by the death of 18-year-old Libby Zion in a New York teaching hospital. The investigation that followed her death found contributing causes to include both resident fatigue and inadequate clinical supervision.2 The resulting media frenzy and policy changes have focused primarily on reducing resident fatigue through duty hour limits, and there has been little discussion about ways to enhance clinical supervision in postgraduate medical education.2 However, the original grand jury indictment concluded that “the most serious deficiencies can be traced to the practice of permitting… interns and junior residents to practice medicine without supervision.”2 Trainees themselves continue to identify inadequate supervision as one of the most common causes of medical errors that occur during hospitalization.2–5
Previous work on supervision has focused on applications in the general workplace,6 with some added studies of clinical supervision in nursing and other allied health professions.7,8 There has been relatively little work to develop a framework for conceptualizing effective supervisory strategies in residency training in general and internal medicine in particular. International work in the field of psychology indicates that a lack of training in how to supervise not only impacts the performance of clinical supervisors but also that of their trainees.9 Despite the need for educating supervisors in effective supervision practice, a paucity of literature exits to guide this effort.
Mixed-methods work presented in the surgical literature has examined miscommunication between resident and attending physicians and has demonstrated the differing expectations between these 2 groups and the expected role that each has of the other.10 The Accreditation Council for Graduate Medical Education standards for specialties such as anesthesiology and obstetrics and gynecology have explicit language regarding availability and physical presence of attending physicians.11 However, the formal approach to clinical supervision for internal medicine residency training remains nebulous. Recent narrative studies have suggested that a collaborative approach to supervision, coupled with constructive feedback, is preferred by trainees.12 Kennedy and colleagues13 described a conceptual model for clinical oversight, ranging from monitoring routine activities to intervening to provide direct patient care. However, there is currently no effective model describing clinical supervision in internal medicine residency training that addresses both the role of the attending or supervising physician and the resident physician in the supervisory relationship.
Using qualitative data elicited in interviews from resident and attending physicians, the aim of this study was to use an inductive qualitative analysis to identify approaches to effective clinical supervision in internal medicine residency training.
Methods
Clinical Setting
The general medicine inpatient service at the University of Chicago consists of 4 teams, each with 1 attending physician, 1 resident physician (second- or third-year categorical internal medicine resident), 2 interns (categorical internal medicine or preliminary year), and, often, 1 fourth-year student subintern. The general medicine teams take overnight call every fourth night, admitting a maximum of 10 patients per night. The attending physician is available to the general medicine teams at night via pager or telephone. The attending physician often meets and rounds with their resident team from approximately 8 am until 10 am, breaking for resident physicians to attend an educational conference, and then reconvenes at 11 am to complete patient rounds. Attending physicians maintain availability to resident physicians via numeric or text page at all times, and often provide their senior resident physician with additional contact information, including home and cellular telephone numbers.
A mandate from the internal medicine residency program director at the beginning of 2006 stated that “all admitting resident physicians need to contact [their] attending at least once during the call night to inform the attending of patients admitted under their name.” This policy is revisited with both attending and resident physicians at the beginning of each rotation on general medicine through written materials provided to the attending physician and oral expectations given to the resident physician.
Data Collection
Between January and November 2006, all eligible internal medicine resident physicians and attending physicians at the University of Chicago were privately interviewed within 1 week of their final call night on the inpatient general medicine rotation. A convenient meeting time for the participant was arranged and oral consent for participation was obtained prior to the beginning of the interview. Interviews lasted, on average, 45 minutes. All interviews were conducted by 1 investigator (J.M.F.) and discussions were recorded by audiotape and transcribed for analysis. The names of the participating physician, and any specific references made to individuals or patients, were blinded. Interviews were conducted at the conclusion of the rotation in order to prevent any influence on resident and attending physician behavior during the rotation. The Institutional Review Board of the University of Chicago approved this study.
During the interviews, the critical incident technique was used to elicit the resident and attending physician roles in patient care decisions made throughout the call night. For example, residents were asked, “Tell me about 2–3 important clinical decisions that you made on your most recent call night?” and “When did you contact your attending for decisions?” Initially used in the investigation of aviation accidents, this technique allows for documentation of infrequently occurring events based on personal observation and has been used by investigators in the study of handoff communication.14,15 Subsequent to discussion of patient care decisions, further probes were done using appreciative inquiry, an organizational strategy to engage individuals within a system to share their ideas and beliefs on how to improve that system.16 This technique was used to elicit resident and attending physician perspectives on ideal supervision practices and what changes or strategies could be used to improve the current state of clinical supervision.16
Data Analysis
All blinded, anonymous interview transcripts were reviewed by 3 investigators (J.M.F., V.M.A., and J.K.J.) and analyzed using the constant comparative method.17 Atlas ti (ATLAS.ti Scientific Software Development Company, GmbH, Berlin, Germany) qualitative analysis software was used to facilitate retrieving, coding, and sorting the data.
An inductive approach, without a priori hypotheses, was used to identify themes regarding clinical supervision and characteristics of effective supervisors. The units of analysis were sentences and phrases. Themes were identified and the frequency of comments in each theme was calculated. In order to establish interrater reliability, each reviewer analyzed 10% of the transcripts (8 randomly chosen transcripts, half of which were attending physician interviews and half were resident physician interviews) and analyses were compared to establish reliability and reach consensus on the thematic structure. One investigator (J.M.F.) then used this agreed-on framework to analyze the remaining transcripts to establish the strength of the themes.
Interrater agreement on themes was initially established via discussion and consensus prior to applying these themes to the remainder of the interview transcripts. Subsequently, interrater agreement was assessed using generalized κ statistics with a representative formula of agreements / (number of agreements + number of disagreements).18–21 Reconciliation of all continued discrepancies was achieved by discussion among the 3 reviewers to achieve consensus.
Results
Participant Demographics
Eighty-eight percent (44) of the 50 eligible attending physicians completed an interview; of these, 55% were men and 45% were women; 38% were academic faculty hospitalists. Ninety-two percent (46) of the eligible resident physicians completed an interview. Of these, 47% were men and 53% were women; 52% were postgraduate year-2 and 45% were postgraduate year-3. Thus, a total of 90 interview transcripts were analyzed.
Inductive Qualitative Analysis
Interrater reliability for the inductive coding of the interviews was κ = 0.70. Residents and attending physicians described practices that could be combined to establish a model to improve the supervisory relationship between the supervisor and trainee.
Major themes were derived from the inductive qualitative analysis to guide attending physicians who provide supervision and the frequency with which these themes were identified in the transcripts. They included:
recognizing uncertainty and alerting trainees that it is time for attending physician-level contact (identified in 68 interviews: 45 attending physicians, 23 residents);
reassuring the residents that it is always appropriate to call, including affirming that there will not be negative repercussions for seeking the attending physician's input (such as anger for calling late, berating for lack of knowledge) (50 interviews: 15 attending physicians, 35 residents);
ready availability of the supervising attending physician by providing trainees with contact numbers and responding promptly to their requests for assistance (48 interviews: 19 attending physicians, 29 residents);
balancing providing supervision while allowing for resident decision-making autonomy (46 interviews: 22 attending physicians, 24 residents);
setting expectations, such as what types of clinical scenarios always warrant attending physician-level input (eg, patient death or cardiac arrest) and defining the role that each of the trainees will play on the team (41 interviews: 15 attending physicians, 26 residents); and
planning communication, such as specifying a regular time for contact during each on-call night (36 interviews: 25 attending physicians, 11 residents [table1]).
Table 1.
Suggestions for Attending Physicians Providing Supervision
One resident highlighted the importance of setting expectations, commenting that “it was nice to know how the team would be structured, how rounds would run, how our on call day would go and it was very helpful to have structure to know what [the attending physician] expected.” An attending physician explained how they planned for communication and stressed their easy availability: “I said if you need anything give me a call; otherwise I will plan on paging you between 9 pm and 10 pm.” A resident discussed balancing decision-making autonomy with supervision:
“[The attending and the resident] work through it together because when you work through it together it makes everyone think and then you can encourage people that have thought out a plan or thought out a complicated and expansive differential because you know that your resident or your attending may ask you and say ‘what do you think?’ or ‘what else could be going on?’ or like that, so I like attendings where it's that way, where you kind of discuss stuff and they ask you your opinion or what you think is going on or who will bring things up, you know, not confrontational but respecting your opinion that you have some knowledge and that you know the patient better than they do and stuff like that so I just like a work together kind of philosophy instead of a ‘run it by me and I will tell you what I think and then we'll talk about it’ or ‘[tell me] what your plan is and then we will do my plan.’”
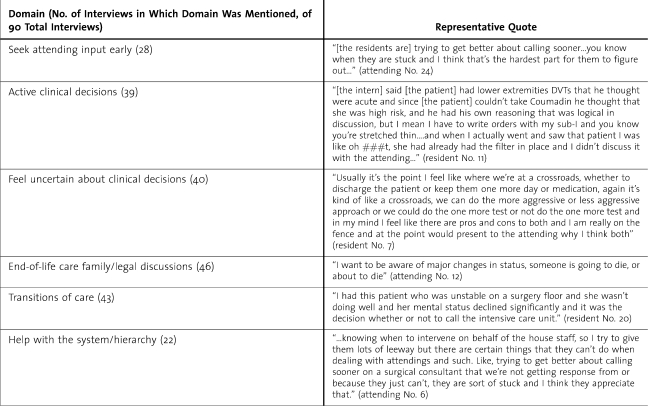
The interviews also described themes of when to seek assistance from the supervising attending physician. Specific clinical tasks and personal situations and the frequency with which they were identified are as follows:
end-of-life and legal issues, such as family meetings resulting in a change of the goals of care or patients leaving against medical advice (46 interviews: 18 attending physicians, 28 residents);
transitions in care, for example, discharging a patient to home or transferring a patient to a higher level of care, such as an intensive care unit setting (43 interviews: 19 attending physicians, 24 residents);
feeling uncertain about patient care decisions to be made (40 interviews: 15 attending physicians, 25 residents); contacting for active clinical decisions, such as patients with rapidly changing clinical presentations (39 interviews: 19 attending physicians, 20 residents);
seeking attending physician input early (28 interviews: 19 attending physicians, 9 residents); and
needing assistance with navigating difficult systems-level issues, such as expediting a subspecialty consult or procedure (22 interviews; 18 attending physicians, 4 residents [table 2]).
Table 2.
Suggestions for When to Seek Attending Input
Residents stated that in an ideal situation they recognized the need to contact attending physicians for active clinical decisions and during transitions of care: “I had this patient who was unstable on a surgery floor and declined significantly and it was the decision whether or not to call the MICU (medical intensive care unit).” Finally, attending physicians recognized their ability to help with systems issues with 1 attending physician commenting, “They have called a couple times, mainly because they were having difficulty with a service doing ‘x’ and can I intervene?”
Through the interviews, we identified many common themes in both the resident and attending physician transcripts, including the importance of availability of the attending physician, early recognition of uncertainty in clinical decision making, and the preservation of resident decision-making autonomy.
Review of the domains established via our qualitative analysis resulted in the development of acronyms to be used for training purposes, the bidirectional SUPERB/SAFETY model. Those findings described as effective strategies for attending physician provision of supervision revealed SUPERB: Set expectations for when to be notified, Uncertainty is a time to contact, Planned communication, Easily available, Reassure fears, and Balance supervision and autonomy. Those domains that described times for residents to solicit faculty supervision revealed SAFETY: Seek attending physician input early, Active clinical decisions, Feeling uncertain about clinical decisions, End-of-life care or family/legal issues, Transitions of care, and You need help with the system/hierarchy.
Discussion
Our findings describe a new framework for clinical supervision, the SUPERB/SAFETY model, which includes recommendations for attending physicians who are providing supervision and for guiding resident physicians for seeking attending physician input. Both residents and attending physicians self-describe a relationship in which uncertainty is recognized and addressed early, autonomy is preserved, expectations are explicit, and communication is planned and easily available. Both attending and resident physicians recognize that uncertainty should be a stimulus for seeking attending physician-level input to decision making. In addition, the importance of supervision is highlighted at times that are critical to patient safety, including transitions between levels of care, and also at times of critical decision making, such as discussions of end-of-life care.
SUPERB/SAFETY Model
Our newly derived model, based on the inductive analysis of the qualitative data, reflects the specific supervisory actions that are necessary for providing clinical care in tandem with effective education and development of residents. This is evidenced not only by agreement on major themes between resident and attending physicians, but also by the frequency of the domains in the qualitative data, with many of the inductively derived domains occurring in more than half of the interview transcripts. This model is bidirectional, suggesting practices for those both providing and seeking supervision to reflect the dynamic situation of the supervisory relationship in clinical care. The acronym for the model does not reflect the frequency of comments in a domain, but rather includes domains with a significant number of comments by both attending physicians and residents, and it uses a mnemonic for ease of recall.22
Pilot testing of this model in an internal medicine setting has shown utility in the mnemonic use for recall of the items. In our new model, both residents and attending physicians describe a relationship in which expectations are explicit, communication is planned and easily available, uncertainty is recognized and addressed early, and autonomy is preserved while residents receive necessary guidance. Both attending and resident physicians recognize that uncertainty should be a stimulus for seeking attending physician-level input to decision making. In addition, effective supervision is thought by both groups to be critical at times to patient safety, including transitions between levels of care and also at times of critical decision making, such as discussions of end-of-life care.
The struggle between balancing resident autonomy and providing adequate clinical supervision is influenced by a number of factors, among them the presence of a hidden curriculum.23 Given that supervision is often resident-initiated, residents may fear they could be perceived as “weak” for contacting their supervising attending physician. This may influence their behavior and discourage attending physician-level contact during times of uncertainty. In addition, many supervising attending physicians have had little specific training for the role of supervisor and often institute ineffective strategies, such as the “micromanagerial style” in which overly controlling attending physicians hamper resident decision making, or the “absentee style” in which attending physicians, believing that they are providing their residents with autonomy, allow their trainees full decision-making power. This often results in a sense of abandonment.24 Both of these styles likely are detrimental to the trainee-supervisor relationship.25
Despite further proposed changes to residency duty hour regulations, physicians in training will continue to provide care to hospitalized patients with numerous comorbidities. Residents receive little training for managing their own uncertainty during times of active clinical decision making.26,27 To address both matters, formal education on providing, and soliciting, supervision may be key in clarifying the aims of supervision, helping to allay decision-making uncertainty and improve the quality of the clinical experience.
Implications for Practice and Education
Our findings have several implications for clinical education as well as patient safety. Resident and faculty training on the importance of clinical supervision, and tips for providing and seeking supervision, may help to improve the overall experience in clinical education for the trainee and also ensure that quality care is delivered. In addition, faculty and trainee development should focus on the use of a theoretical framework, such as the SUPERB/SAFETY model, to teach supervisory strategies as well as to describe a method for evaluating and improving the current strategies.28 Future research should focus on establishing formal relationships between clinical supervision and patient care outcomes in order to quantify the impact of formal supervisory training and the efficacy of the proposed supervisory framework.
Limitations
There are several limitations to this study. It was conducted at 1 academic institution and thus raises issues of generalizability. The perspectives on ideal or effective supervision may reflect institutional culture and norms and may not adequately and objectively represent more generally applicable elements of effective clinical supervision. However, given the congruence between our qualitative results and previously collected qualitative data related to clinical supervision13 we expect that these findings will be applicable to clinical supervision at other institutions. There were also many common themes identified by both resident and attending physician describing ideal behaviors.
In addition, these findings are subject to the limitations of the critical incident interview technique. Interviewer effects may have influenced data collection, such that the interviewer may have inadvertently influenced participants' responses to produce answers consistent with interviewer expectations.29 Given that all participants were interviewed at the conclusion of their month-long rotation, our findings are subject to hindsight bias due to retrospective analyses of the patient care incidents.30 These findings cannot be considered to be definitive but they provide a preliminary view of ideal strategies for clinical supervision in residency training as described by residents and attending physicians themselves.
Conclusions
Despite these limitations, this study suggests that there are behaviors that can be used to guide the attending physician's supervisory style and actions as well as the residents' management of their clinical uncertainty. Formal faculty and resident education using the SUPERB/SAFETY model may help to improve the balance between clinical supervision and resident autonomy.
References
- 1.Ulmer C., Wolman D. M., Johns M. M. E. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC:: National Academies Press; 2008. [PubMed] [Google Scholar]
- 2.Bell B. M. Resident duty hour reform and mortality in hospitalized patients. JAMA. 2007;298(24):2865–2866. doi: 10.1001/jama.298.24.2865-c. [DOI] [PubMed] [Google Scholar]
- 3.Jagsi R., Kitch B. T., Weinstein D. F., Campbell E. G., Hutter M., Weissman J. S. Residents report on adverse events and their causes. Arch Intern Med. 2005;165(22):2607–2613. doi: 10.1001/archinte.165.22.2607. [DOI] [PubMed] [Google Scholar]
- 4.Conigliaro J., Frishman W. H., Lazar E. J., Croen L. Internal medicine housestaff and attending physician perceptions of the impact of the New York State Section 405. J Gen Intern Med. 1993;8:502–507. doi: 10.1007/BF02600112. [DOI] [PubMed] [Google Scholar]
- 5.Singh H., Thomas E. J., Petersen L. A., Studdert D. M. Medical errors involving trainees: a study of closed malpractice claims from 5 insurers. Arch Intern Med. 2007;167(19):2030–2036. doi: 10.1001/archinte.167.19.2030. [DOI] [PubMed] [Google Scholar]
- 6.Likert R. Effective supervision: an adaptive and relative process. Pers Psychol. 2006;11(3):317–332. [Google Scholar]
- 7.Hyrkas K., Appelqvist-Schmidlechner K., Haataja R. Efficacy of clinical supervision: influence on job satisfaction, burnout and quality of care: nursing and healthcare management and policy. J Adv Nurs. 2006;55(4):521–535. doi: 10.1111/j.1365-2648.2006.03936.x. [DOI] [PubMed] [Google Scholar]
- 8.Fone S. Effective supervision for occupational therapists: the development and implementation of an information package. Aust Occup Ther J. 2006;53(4):277–283. [Google Scholar]
- 9.Johnson E. A., Stewart D. W. Clinical supervision in Canadian academic and service settings: The importance of education, training, and workplace support for supervisor development. Canadian Psychology. 2000;41(2):124–130. [Google Scholar]
- 10.Phitayakorn R., Williams R., Yudowsky R. Patient care related telephone communication between general surgery residents and attending surgeons. J Am Coll Surg. 2008;206(4):724–750. doi: 10.1016/j.jamcollsurg.2007.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Obstetrics and gynecology residency program requirements. Available at: http://www.acgme.org/acWebsite/downloads/RRC_progReq/220obstetricsandgynecology01012008.pdf. Accessed January 7, 2010.
- 12.Busari J. O., Weggelaar N. M., Knottnerus A. C., Greidanus P. M., Scherpbier A. J. How medical residents perceive the quality of supervision provided by attending doctors in the clinical setting. Med Educ. 2005;39:696–703. doi: 10.1111/j.1365-2929.2005.02190.x. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy T. J., Lingard L., Baker G. R., Kitchen L., Regehr G. Clinical oversight: conceptualizing the relationship between supervision and safety. J Gen Intern Med. 2007;22:1080–1085. doi: 10.1007/s11606-007-0179-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flanagan J. C. The critical incident technique. Psychol Bull. 1954;51(4):327–359. doi: 10.1037/h0061470. [DOI] [PubMed] [Google Scholar]
- 15.Arora V., Johnson J., Lovinger D., Humphrey H., Meltzer D. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care. 2005;14:401–407. doi: 10.1136/qshc.2005.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Appreciative inquiry commons. Available at: http://appreciativeinquiry.case.edu/ Accessed October 16, 2009.
- 17.Strauss A., Corbin J. Basics of Qualitative Research. 2nd ed. Thousand Oaks, CA:: Sage Publications; 1998. [Google Scholar]
- 18.Fraenkel J. R., Wallen N. E. How to Design and Evaluate Research in Education. New York, NY:: McGraw Hill; 2003. [Google Scholar]
- 19.Miles M. B., Huberman A. M. Qualitative Data Analysis. Thousand Oaks, CA:: Sage; 1994. [Google Scholar]
- 20.Morse J., Barratt M., Olson K., et al. Verification strategies for establishing reliability and validity in qualitative research. Int J Qual Methods. 2002;1:11–23. [Google Scholar]
- 21.Berry K. A. Generalization of Cohen's kappa agreement measure to interval measurement and multiple raters. Educ Psychol Meas. 1998;48(4):921–933. [Google Scholar]
- 22.Stadler D. R. Learning and motivational benefits of acronym use in introductory psychology. Teach Psychol. 2005;32(4):222–228. [Google Scholar]
- 23.Hundert E. M., Hafferty F., Christakis D. Characteristics of the informal curriculum and trainees' ethical choices. Acad Med. 1996;71:624–642. doi: 10.1097/00001888-199606000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Farnan J. M., Johnson J. K., Meltzer D. O., Humphrey H. J., Arora V. M. Assessing supervision in internal medicine residency training: a mixed methods study. Am J Med. 2009;122(8):784–788. doi: 10.1016/j.amjmed.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 25.Farnan J. M., Johnson J. K., Meltzer D. O., Humphrey H. J., Arora V. M. Resident uncertainty in clinical-decision making: a qualitative analysis. Qual Saf Health Care. 2008;17:122–126. doi: 10.1136/qshc.2007.023184. [DOI] [PubMed] [Google Scholar]
- 26.Farnan J. M., Humphrey H. J., Arora V. Supervision: a 2-way street. Arch Intern Med. 2008;168(10):1117. doi: 10.1001/archinte.168.10.1117-a. [DOI] [PubMed] [Google Scholar]
- 27.Wilkerson L., Irby D. M. Strategies for improving teaching practices: a comprehensive approach to faculty development. Acad Med. 1998;73:387–396. doi: 10.1097/00001888-199804000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Kilminster S., Jolly B., van der Vleuten C. P. A framework for effective training for supervisors. Med Teach. 2002;24:385–389. doi: 10.1080/0142159021000000834. [DOI] [PubMed] [Google Scholar]
- 29.Holden J. Hawthorne effects and research into professional practice. J Eval Clin Pract. 2001;7:65–770. doi: 10.1046/j.1365-2753.2001.00280.x. [DOI] [PubMed] [Google Scholar]
- 30.Cook R., Woods D., Miller C. A tale of two stories: contrasting views on patient safety. National Patient Safety Foundation conference, Chicago, IL; 1998. Available at http://www.ctlab.org/documents/A%20Tale%20of%20Two%20Stories.pdf. Accessed on January 7, 2010.