Abstract
Objectives
To assess burnout, behavioral-medicine skills, and empathy among obstetrics and gynecology residents before and after implementation of Balint training.
Methods
This was a prospective educational study. Balint training was introduced into the obstetrics and gynecology residency curriculum in July 2005. All 36 residents were approached for this study. The Psychological Medicine Inventory, the Maslach Burnout Inventory, and the Jefferson Scale of Physician Empathy were administered prior to initiating training and at 12 months. Baseline and 12-month scores were compared by Wilcoxon signed rank test.
Results
Seventeen residents completed baseline and 12-month questionnaires: 6 were postgraduate year (PGY) 1, 3 were PGY-2, 6 were PGY-3, and 2 were PGY-4. At baseline, 70% of participating residents reported high burnout scores. Burnout and empathy remained unchanged at 12 months. Psychological medicine skills improved at 12 months.
Conclusions
This study showed that obstetrics and gynecology residents are at high risk for burnout. Interest and confidence in handling psychological aspects of patient care improved at 12 months after the introduction of Balint training.
Introduction
The American College of Obstetricians and Gynecologists Council on Resident Education in Obstetrics and Gynecology and the Accreditation Council for Graduate Medical Education (ACGME) have placed new emphasis on obstetrics and gynecology residents' acquisition of skills in professionalism and patient-provider communication.1 In the late 1950s, Michael and Enid Balint2 identified the therapeutic properties of the doctor-patient relationship with family physicians in the United Kingdom. They developed a group-training method, now called Balint groups, to help physicians better understand their role in the doctor-patient relationship and to help physicians gain interpersonal skills.
Balint groups involve 6 to 12 physician participants and 2 group facilitators. At the start of these case-centered discussions, a participant volunteers to provide an account of a specific patient encounter. Cases are often prompted by a difficulty the clinician is having in the relationship with a particular patient. The focus of discussion is the story of a specific encounter and the emotions and attitudes aroused by the presentation; medical or technical facts are avoided. Participants are asked to consider and imagine their own reactions, emotions, and behaviors pertaining to the specific physician-patient encounter from the perspectives of both the physician and the patient. The safety of the group is maintained through clear guidelines regarding confidentiality and respect.
Balint group training is currently used in over 50% of family medicine residency training programs.3 Balint sessions not only provide training and skills in understanding the doctor-patient relationship and help develop empathy, but they may also be a resource for improving job satisfaction and reducing physician burnout.4–8 Burnout is a psychological term that describes a condition characterized by lack of personal and professional satisfaction, symptoms of emotional exhaustion, and depersonalization in relationships. Burnout is present in many professions. It is associated with impaired performance and decreased mental and physical health. The Maslach Burnout Inventory is the most-studied measure of burnout. Burnout is very prevalent in physicians, with estimated rates of 25% to 60%.9 Studies10 suggest that burnout is also very prevalent in residents. It has been shown to affect obstetrician-gynecologists throughout their career paths—from residents to departmental chairs.12–15
Very few studies4,7,16,17 have assessed the association between Balint training and physician outcomes using validated instruments for empathy, behavioral-medicine skills, or burnout. Even fewer studies have implemented Balint training within a surgical or procedurally oriented subspecialty. Our goal was to introduce Balint training in a large academic obstetrics and gynecology residency program curriculum to help address ACGME requirements for focused training in the competencies of professionalism and interpersonal skills and communication. The aim of this study was to assess burnout, behavioral-medicine skills, and empathy among obstetrics and gynecology residents before and after implementation of this new curriculum by using validated measures.
Methods
Introduction of Balint Training
We introduced Balint group training as a required component of the obstetrics and gynecology residency program curriculum beginning in July 2005. This initiative was the collaborative effort of 4 faculty members (2 obstetrician-gynecologists, 1 pediatrician, and 1 psychiatrist), 3 of whom are credentialed as Balint leaders by the American Balint Society. These faculty members facilitated two 1-hour group sessions once a month during protected, mandatory educational time. These two sessions were held concurrently in separate rooms. One group consisted of first- and second-year residents; the other was composed of third- and fourth-year residents.
Study Methods
This study received exempt status by the University of Pittsburgh Institutional Review Board. On the first day of the new Balint curriculum, all 36 residents of the Department of Obstetrics, Gynecology, and Reproductive Sciences were approached about participating in the research study by a departmental assistant who was not involved with the residency program. The investigators and faculty members leading the groups were not present at the time of recruitment and were blinded to which residents chose to participate.
All residents participated in Balint training. Those residents who agreed to participate in the study completed the Maslach Burnout Inventory, the Psychological Medicine Inventory, and the Jefferson Scale of Physician Empathy prior to initiating the course and at 12 months. Study participants were queried about demographic information including year in training, age, race, marital status, and subspecialty interests. Additional demographics were not obtained, in order to protect the identity of participants.
The Maslach Burnout Inventory–Human Service Survey is a validated, 22-item self-report measure.18 Each item is scored using a 7-point Likert scale. The survey assesses 3 domains of burnout: emotional exhaustion (9 questions), depersonalization (5 questions), and personal accomplishment (8 questions). Scores for each subscale are recorded as high, medium, or low. For both emotional exhaustion and depersonalization subscales, higher scores correspond to higher degrees of perceived burnout. Lower scores on the personal accomplishment subscale correspond to higher degrees of perceived burnout. In this study we report the high-risk scores in each subscale. According to Maslach Burnout Inventory scoring, high-risk scores for each subscale are defined as ≥27 in emotional exhaustion, ≥10 in depersonalization, and ≤33 in personal accomplishment. Overall moderate-to-severe risk of burnout was defined as high-risk scores in 2 or more of the 3 categories.
The Psychological Medicine Inventory is a validated, 11-item self-report survey with a 9-point Likert scale that has been previously used to evaluate the effects of Balint training.4,7,19 Items are designed to assess residents' levels of interest, ability, or confidence in dealing with psychological aspects of patient care. A higher score indicates higher interest and ability in psychological medicine. As performed by Turner and Malm4 and Adams et al.16 changes in individual questions were assessed.
The Jefferson Scale of Physician Empathy is a validated quantitative measurement used to assess levels of physician empathy.20 It contains 20 statements answered using a 7-point Likert scale, from 1 (strongly disagree) to 7 (strongly agree). Ten items of this scale are positively worded and ten items are negatively worded, requiring reverse coding. The scores range from 20–140. A higher score on the scale indicates greater empathy.
Descriptive statistics were performed. Baseline and 12-month continuous data were compared using the Wilcoxon signed rank test. Statistical analysis was performed using SPSS software version 12.0.1 (SPSS Inc, Chicago, IL).
Results
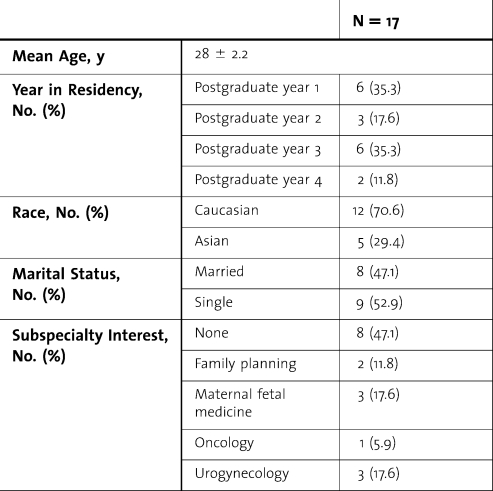
Complete data were available for 17 residents who completed both baseline and 12-month questionnaires. The baseline demographics of the respondents are summarized in table 1. Participants included the majority of first- and third-year residents. Nonparticipants were primarily second- and fourth-year residents. Additional demographics were not available for nonparticipating residents.
Table 1.
Baseline Demographics of Respondents
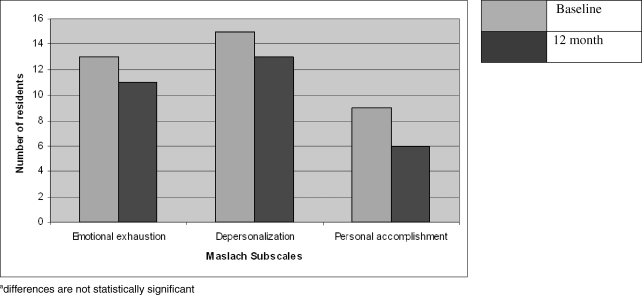
At baseline, median scores (range) for each burnout subscale were as follows: emotional exhaustion, 35 (15–44); depersonalization, 14 (4–23); personal accomplishment, 33 (26–42). At baseline, 13 of 17 residents had high burnout scores in the emotional exhaustion subscale, 15 had high burnout scores in the depersonalization subscale, 9 had high burnout scores in the personal accomplishment subscale, and 13 had high burnout scores in more than one subscale.
At 12 months, the number of residents with high burnout scores in each subscale decreased. Two fewer residents had high burnout scores in depersonalization and emotional exhaustion, while 3 fewer residents had high burnout in personal accomplishment (figure). Median scores (range) for each subscale were as follows: emotional exhaustion, 34 (8–40); depersonalization, 15 (3–23); personal accomplishment, 35 (23–46). Changes in subcategory and total Maslach scores were not statistically significant. The majority of residents of all 4 classes (≥70%) had moderate-to-severe burnout (defined as high-risk scores in 2 or more categories) at baseline and 12 months.
Figure.
Number of Resident Responders (N = 17) With High-Risk Scores for Burnout at Baseline and 12 Months in Each of the 3 Subcategories: Emotional Exhaustion, Depersonalization, and Personal Accomplishment.a
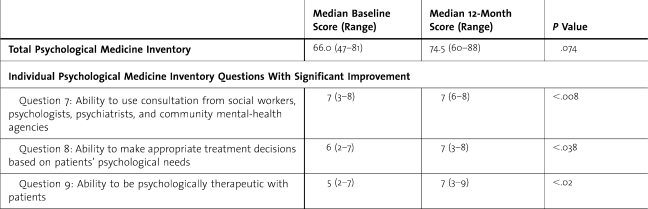
Psychological Medicine Inventory overall scores improved at 12 months when compared with baseline scores. Three of the Psychological Medicine Inventory scores for individual questions showed a statistically significant improvement at 12 months (table 2). Jefferson Scale of Physician Empathy scores remained unchanged at 12 months with a median (range) of 113 (92–129) at baseline and 12 months.
Table 2.
Median Baseline and 12-Month Total Psychological Medicine Inventory Scores and Individual Questions Showing Significant 12-Month Improvement (Higher Score Indicates Higher Interest and Ability in Psychological Medicine)
Discussion
One of the most striking findings of this study was the high levels of resident burnout. This study is one of few studies that provide objective assessment of obstetrics and gynecology residents before and after Balint training. In our study, the majority of participating obstetrics and gynecology residents (≥70%) had moderate-to-severe burnout (defined as high-risk scores in 2 or more categories) both at baseline and 12 months after Balint training began. These findings are similar to those found in the small number of studies that have examined burnout in residents. Martini et al10 described burnout among 321 residents in different specialties using the Maslach Burnout Inventory. Overall they reported that 50% of residents met the criteria for burnout, and obstetrics and gynecology residents had one of the highest burnout rates at 75%. Other studies of obstetrics and gynecology residents13–15 have reported burnout rates of 58% to 83%. Differences in criteria used in these studies to define the extent of burnout preclude a direct comparison in burnout rates. The high level of burnout is likely due to multiple factors, including challenging interactions with patients, lack of work-life balance, and demands of a surgical subspecialty. Among residents in this study, the largest number of high-risk scores was found in the depersonalization subscale, while the personal accomplishment subscale had the lowest number of high-risk scores. High personal accomplishment was thought to contribute to lower overall burnout scores in a study of obstetrics and gynecology department chairs.15
Emotional depletion and depersonalization are responses to prolonged occupational stress and lead to a sense of emotional withdrawal toward coworkers and patients.21 A better understanding of residents' experiences is needed to identify sources of emotional exhaustion and depersonalization and to identify methods to ameliorate their impact on young trainees. Although several authors have proposed Balint training as a possible antidote to burnout in physicians,4–6 no studies have examined the effects of Balint training on burnout using a validated scale. Residents in our study demonstrated a trend toward improvement of burnout levels; however, due to limitations in our study design, we are unable to substantiate this.
Our study showed improvement in some aspects of behavioral-medicine skills of obstetrics and gynecology residents at the 12-month assessment. Residents reported an improvement in ability to use consultation, ability to make appropriate treatment decisions based on patients' psychological needs, and ability to be psychologically therapeutic with patients. While individual Psychological Medicine Inventory items are not independently validated, we explored individual items, as did Turner and Malm4 and Adams et al.16 who found improvement in individual and total Psychological Medicine Inventory scores in family medicine and obstetrics and gynecology residents who completed Balint training compared with residents who did not.
Our study found no difference in baseline and 12-month Jefferson Scale of Physician Empathy scores. Similarly, Cataldo et al15 found no difference in empathy scores between practicing physicians who had attended Balint training during residency versus those who had not attended. Hojat et al21 reported empathy scores for physicians in various specialties and found the highest scores in practicing psychiatrists (mean score of 127 ± 5.5). Practicing family physicians and obstetrician-gynecologists scored significantly lower than psychiatrists (mean scores of 120.5 ± 12.6 and 119 ± 10, respectively). Our resident participants' mean score was 112 ± 12. While this score falls within the standard deviation of the scores reported by Hojat et al, it is 7 points below the mean of practicing obstetrician-gynecologists. Numerous explanations can be offered for lower scores in this study. Skills in empathy may develop through experience and may be lower in trainees. Ability to be empathetic may be affected by stress level and degree of burnout. Empathy scores may also reflect the amount of emphasis that is placed on interpersonal skills during training.
Our study had several limitations. The small sample size limited our precision, power, and generalizability. The participation of only 47% of the residents increased the significant potential for selection bias and likely lead to the lack of statistically significant results. Participants may have been more receptive to or interested in Balint training. Participants may also have been more distressed and willing to participate, biasing results to a higher prevalence of burnout. Since we lacked a comparison or control group, we were unable to tease out the numerous potential confounding variables, including time, curriculum, or other experiences, that could explain some of the results. The effect of collective resident experiences over the course of the year may explain the change in Psychological Medicine Inventory scores. Although to our knowledge our study had the longest assessment period of any other study evaluating the effects of Balint training, 12 months may still be too short a period to see measurable changes in more complex characteristics such as empathy. The study findings presented in this article focus only on the results of 3 quantitative questionnaires, which may not present a full picture of how Balint training impacted the attitudes, understanding, and experiences of the obstetrics and gynecology residents. All of the instruments utilized in this study rely on resident self-report. Many of these limitations could be addressed in future studies by employing a study design involving control and intervention groups, recruitment from multiple institutions, and mixed methods.
As 1 of only 2 studies that evaluate outcomes of Balint training in an obstetrics and gynecology residency, this study adds to existing work in this challenging area of residency-curriculum development. This is the only study that examined the effects of Balint training as a mandatory part of the residency curriculum using 3 different validated measures.
The value of Balint training in obstetrics and gynecology residency programs remains unclear. Balint groups do address the ACGME competencies of professionalism and interpersonal skills and communication in a humanistic group environment. However, due to the process-oriented nature of Balint training and the significant limitations of our study, it is difficult to measure the resident outcomes as a direct consequence of Balint training. However, our study clearly revealed a high level of burnout. It also suggested that empathy scores in residents may be lower that that of practicing physicians. Improving physician-patient communication may be a way to lower levels of burnout.22,23 Balint training is a safe and supportive method of fostering reflection, challenging assumptions, and suggesting alternative approaches regarding difficult provider-patient relationships. Such experiential learning may be difficult to assess using quantitative measurement instruments. Further work using other methods of assessment, such as qualitative evaluation, longitudinal observation, and multicenter design, may be necessary to assess the impact of Balint training. More importantly, this study calls attention to the imminent need to identify the extent of burnout in training physicians and to determine the best way to address burnout in this specialty and across specialties.
Acknowledgments
We would like to thank and acknowledge Paul Scott, MD, and William Cohen, MD, for substantive guidance and support of Balint training in our residency program and for reviewing the manuscript.
This manuscript was completed in partial fulfillment of the requirements for the APGO/Solvay Educational Scholars Development Program. The program faculty and program advisor, William Herbert, MD, provided substantive guidance and advice in the preparation of this paper.
Footnotes
Chiara Ghetti, MD, is Assistant Professor at the Division of Urogynecology, Department of Obstetrics, Gynecology and Reproductive Sciences, University of Pittsburgh School of Medicine; Judy Chang, MD, is Assistant Professor at the Division of Gynecologic Specialties, Department of Obstetrics, Gynecology and Reproductive Sciences, University of Pittsburgh School of Medicine; and Gabriella Gosman, MD, is Associate Professor at the Division of Reproductive Endocrinology and Infertility, Department of Obstetrics, Gynecology and Reproductive Sciences, University of Pittsburgh School of Medicine.
References
- 1.Council on Resident Education in Obstetrics and Gynecology. Educational Objectives, A Core Curriculum in Obstetrics and Gynecology. 8th ed. New York, NY: Professional Publishing Group, Ltd; 2005. [Google Scholar]
- 2.Balint M. The Doctor, His Patient and the Illness. London, England: Pitman; 1957. [DOI] [PubMed] [Google Scholar]
- 3.Johnson A. H., Brock C. D., Hamadeh G., Stock R. The current status of Balint groups in US family practice residencies: a 10-year follow-up study, 1990–2000. Fam Med. 2001;33(9):672–677. [PubMed] [Google Scholar]
- 4.Turner A. L., Malm R. L. A preliminary investigation of Balint and non-Balint behavioral medicine training. Fam Med. 2004;36(2):115–117. [PubMed] [Google Scholar]
- 5.Addison R. B. An antidote to physician burnout: the Balint group as a hermeneutic clearing for the possibility of finding meaning in medicine. In: Salinsky J., editor. Proceedings of the Eleventh International Balint Congress. Southport, England: Limited Edition Press; 1999. pp. 191–199. [Google Scholar]
- 6.Benson J., Magraith K. Compassion, fatigue and burnout. Aust Fam Physician. 2005;34(6):497–498. [PubMed] [Google Scholar]
- 7.Kjeldmand D., Holmström I., Rosenqvist U. Balint training makes GPs thrive better in their job. Patient Educ Couns. 2004;55:230–236. doi: 10.1016/j.pec.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 8.Bellet P., Maloney M. The importance of empathy as an interviewing skill in medicine. JAMA. 1991;266(13):1831–1832. [PubMed] [Google Scholar]
- 9.Shanafelt T. D., Bradley K. A., Wipf J. E., Back A. L. Burnout and self-reported patient care in an internal medicine residency program. Ann Intern Med. 2002;136(5):358–367. doi: 10.7326/0003-4819-136-5-200203050-00008. [DOI] [PubMed] [Google Scholar]
- 10.Thomas N. K. JAMA. 2004;292(23):2880–2889. doi: 10.1001/jama.292.23.2880. [DOI] [PubMed] [Google Scholar]
- 11.Martini S., Arfken C. L., Churchill A., Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240–242. doi: 10.1176/appi.ap.28.3.240. [DOI] [PubMed] [Google Scholar]
- 12.Becker J. L., Milad M. P., Klock S. C. Burnout, depression, and career satisfaction: cross-sectional study of obstetrics and gynecology residents. Am J Obstet Gynecol. 2006;195:1444–1449. doi: 10.1016/j.ajog.2006.06.075. [DOI] [PubMed] [Google Scholar]
- 13.Castelo-Branco C., Figueras F., Eixarch E. Stress symptoms and burnout in obstetric and gynaecology residents. BJOG. 2007;114:94–98. doi: 10.1111/j.1471-0528.2006.01155.x. [DOI] [PubMed] [Google Scholar]
- 14.Gabbe S., Melville J., Mandel L., Walker E. Burnout in chairs of obstetrics and gynecology: diagnosis, treatment, and prevention. Am J Obstet Gynecol. 2002;166:601–612. doi: 10.1067/mob.2002.122391. [DOI] [PubMed] [Google Scholar]
- 15.Cataldo K. P., Peeden K., Geesey M. E., Dickerson L. Association between Balint training and physician empathy and work satisfaction. Fam Med. 2005;35(5):328–331. [PubMed] [Google Scholar]
- 16.Adams K., O'Reilly M., Romm J., James K. Effect of Balint training on resident professionalism. Am J Obstet Gynecol. 2006;195:1431–1437. doi: 10.1016/j.ajog.2006.07.042. [DOI] [PubMed] [Google Scholar]
- 17.Maslach C., Jackson S. E., Leiter M. P. Maslach Burnout Inventory Manual. 3rd ed. Palo Alto, CA: Consulting Pscyhologists; 1996. [Google Scholar]
- 18.Ireton H. R., Sherman M. Self-ratings of graduating family practice residents' psychological medicine abilities. Fam Pract Res J. 1988;7(4):236–245. [PubMed] [Google Scholar]
- 19.Hojat M., Mangione S., Nasca T. J. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. [Google Scholar]
- 20.Maslach C., Jackson S. E. The measurement of experienced burnout. J Occup Behav. 1981;2:99–113. [Google Scholar]
- 21.Hojat M., Gonnella J. S., Nasca T. J., Mangione S., Vergare M., Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 22.Kuerer H. M., Breslin T., Shanafelt T. D., Baile W. F., Crawford W., Balch C. M. Road map for maintaining career satisfaction and balance in surgical oncology. J Am Coll Surg. 2008;207(3):435–442. doi: 10.1016/j.jamcollsurg.2008.03.026. [DOI] [PubMed] [Google Scholar]
- 23.Sharma A., Sharp D. M., Walker L. G., Monson J. R. Stress and burnout in colorectal and vascular surgical consultants working in the UK National Health Service. Psychooncology. 2008;17(6):570–576. doi: 10.1002/pon.1269. [DOI] [PubMed] [Google Scholar]