Abstract
Background
In December 2008 the Institute of Medicine (IOM) released a report recommending limits on resident hours that are considerably more restrictive than the current Accreditation Council for Graduate Medical Education duty hour standards.
Intervention
In March 2009, a large pediatric residency program implemented a 1-month trial of a schedule and team structure fully congruent with the IOM recommendations to study the implications of such a schedule.
Methods
Comparison of the interns' experience in the trialed intervention schedule was made to interns working a traditional schedule with every fourth night call.
Results
The residents on the intervention schedule averaged 7.8 hours of sleep per 24-hour period compared to 7.6 hours for interns in a traditional schedule. Participation in bedside rounds and formal didactic conferences was decreased in the intervention schedule. Several factors contributed to increased perceived work intensity for interns in the intervention schedule. Redistribution of work during busy shifts altered the role of senior residents and attending physicians which may have a negative effect on senior residents' ability to develop skills as supervisors and educators.
Conclusions
The trial implementation suggests it is possible to implement the proposed duty hour limits in a pediatric residency, but it would require a significant increase in the resident workforce (at least 25% and possibly 50%) to care for the same number of patients. Furthermore, the education model would need to undergo significant changes. Further trials of the IOM recommendations are needed prior to widespread implementation in order to learn what works best and causes the least harm, disruption, and unnecessary cost to the system.
Background
In December 2008, an Institute of Medicine (IOM) report entitled Resident Duty Hours: Enhancing Sleep, Supervision, and Safety1 recommended limits on resident hours that are considerably more restrictive than the Accreditation Council for Graduate Medical Education (ACGME) common duty hour standards implemented in 2003.2 Since the release of the report, there have been a number of commentaries and editorials discussing the feasibility of these rules, yet to date there have been no feasibility studies that look at the practical implications of the suggested work hour restrictions. In March 2009, the pediatric residency program at Cincinnati Children's Hospital Medical Center (CCHMC) implemented a schedule and team structure with 2 goals: comply with the duty hour limits recommended in the IOM report and study the implications of such a schedule.
Ability to Comply With the Proposed Duty Hour Restrictions
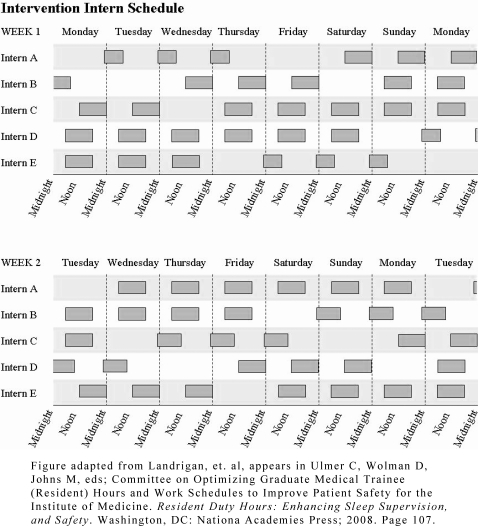
The CCHMC residency is a large pediatric residency program that follows a traditional every fourth night call schedule. The work hour changes recommended by the IOM report are significant and pose logistical challenges. A new schedule was developed by two pediatric chief residents with active input from the program director, residents, and attending physicians. The approach chosen was to limit shift length instead of implementing a schedule with extended duty periods and protected sleep time. This decision was based on both intern preference at our institution and the logistical challenges of enforcement and coverage during sleep periods. We also limited shift length to 12 hours to both increase work hour compliance and facilitate rotation of the shift schedule. In our trial of the IOM proposed duty hour limits, the recommendation stipulating no more than 4 overnight shifts in a row followed by 48 hours off posed the greatest scheduling challenge (figure).
Figure.
Representation of Intervention Work Schedule3
The interventional shift schedule implemented for the interns was as follows:
3 overnight shifts (11 hours from 11 pm to 10 am)
50 hours off
3 “evening shifts” (noon to midnight)
30 hours off
6 day shifts (6 am to 6 pm)
29 hours off
Days off were scheduled throughout the week to ensure 24 hours off every 7 days. Interns were also scheduled for one 48-hour period off every 15 days. There was no differentiation in staffing weekdays and weekends.
The schedule mandated an increase of 1 additional intern to a total of 5 interns on a general pediatric team. The general inpatient teams at CCHMC cover only general pediatric patients (and none of the subspecialty services) under the supervision of academic general pediatric attending physicians. Traditionally interns on these teams take call every fourth night. Each of the 5 interns on the team trialing the IOM-recommended limits rotated through the intervention shift schedule shown in the figure twice during the monthlong intervention period. Their experience was compared with interns working concurrently on a separate, typical general pediatric team taking every fourth night call in compliance with the 2003 ACGME work hour restrictions. Of note, the intervention month, March, is traditionally one of the busiest general pediatric months at CCHMC.
Implications of the Schedule Change
Effect on Sleep
During the intervention, we asked residents on both the intervention and comparison teams to keep daily wok and sleep logs.3 Residents on the traditional schedule worked an average of 76.2 hours per week. By comparison, residents on the intervention schedule worked an average of 67.3 hours per week. There were no instances where the interns on the intervention schedule worked more than 16 hours. The residents on the traditional schedule averaged 7.6 hours of sleep per 24-hour period, compared to interns on the intervention schedule who averaged 7.8 hours of sleep per 24-hour period. Despite working fewer hours, preliminary analysis indicates that the difference in total sleep time is unlikely to be statistically significant. However, additional analysis adjusting for individual variation in sleep patterns is ongoing. An interesting observation is that the interns on the traditional schedule averaged 6.3 instances per month during which they slept fewer than 5 hours in a 24-hour period. Interns on the intervention schedule averaged 2.4 times per month of sleeping fewer than 5 hours in a 24-hour period.
Effect on Education
In a traditional call month, residents receive the majority of their education during morning rounds with the attending and through didactic conferences at prescribed times (eg, morning report and noon conferences). In a traditional schedule, interns at CCHMC are present on morning rounds approximately 24 of 28 days. In the intervention schedule, interns were scheduled to be present during at least a portion of morning rounds only approximately 17 times in 28 days. Attendance at didactic conferences was also decreased due to the design of the interns' schedule. During a traditional call month, an intern is able to attend 20 morning report and approximately 16 noon conference teaching sessions. The intervention schedule limited conference attendance to 12 morning report and 12 noon conference sessions.
The decrease in attending led bedside teaching opportunities and formal didactic sessions was anticipated prior to the implementation of the new schedule. In order to overcome this challenge, the general pediatric attending physicians agreed to extend their in-house time from a traditional daytime schedule to an extended day and evening shift-based schedule. While the extended attending in-house presence did not necessitate hiring of additional physicians during the intervention, the long-term implication of this schedule would be a 20% increase in the attending physician complement on the inpatient service. No attempt was made to change the didactic lecture schedule to facilitate attendance by the interns on the intervention team. The post-intervention surveys, although limited by the small sample size, indicate there may be a trend toward lower perceived educational quality for interns on the intervention team.
The findings for education suggest that if the limits proposed by the IOM report are implemented without extending the length of residency training, an education overhaul will be necessary. Because bedside education is essential for resident development, education from attending physicians must be extended beyond the traditional morning rounds. Attending physicians must be available during the other hours of the day for supervision and education of the residents. The timing and format of didactic teaching sessions will need to be reworked. The traditional morning report and noon conference may need to be supplemented with small group conferences throughout the day. In addition, dinner didactics and midnight mastery sessions may need to be developed.
Effect on Work Load and Intensity—An Unintended Consequence
Even with an increase in intern staffing by 25%, the interns felt that, ideally, there should have been a sixth team member to help with the very high level of work intensity. Despite working fewer hours, the interns reported feeling more stressed and having a larger workload. While the increased workload to some degree offered added educational opportunities, the relationship between workload and education may be comparable to a Starling curve.4 Lower levels of added workload and/or intensity proportionately increase educational attainment, but at a higher level, the added work and/or intensity overload the resident, and the educational value becomes negative. The IOM report1 also stated that beyond a certain point, added workload or intensity may lead to decreased learning opportunities and decreased overall well-being.
Several aspects of the new schedule appeared to contribute to increased work intensity. One was that the intervention team accepted admissions every day instead of individual interns accepting admissions every fourth day. Due to the discontinuity of the schedule, patients were shared by the entire team (as opposed to each patient having a primary intern). In a traditional call month, overnight cross-coverage primarily is an issue of triage and problem solving. Interns on the intervention model who were called with a relatively nonurgent issue could not defer a decision until the primary intern arrived in the morning. Essentially, because patients did not have a primary intern, all patients belonged to the team of interns. This posed several challenges. When an intern was pre-rounding on a patient they had never met before, they could not be expected to know the patient as well as the “primary” intern in a traditional call model. At the same time, to maintain the same level of care, someone needed to know the patient on that level. The number of patients that encountered each intern on the intervention team was equal to the entire team census during his or her shift. When the overall workload went beyond a certain level, senior residents and attending physicians had to help with history and physicals, sign-outs, and other duties that are traditionally intern responsibilities.
The redistribution of work altered the role of senior residents and attending physicians. This may affect the ability of senior residents to develop skills as supervisors and educators. Due to a change in focus, attending physicians who assisted with this work may have been left with reduced overall situational awareness. The high workload and intensity suggested a need for at least a 25% increase and ideally a 50% increase in resident or other medical personnel to cover the same number of patients, as well as an additional 20% increase in attending workforce.
Conclusion
The 1-month experiment in the pediatric residency program at CCHMC suggests that it is possible to implement the proposed duty hour limits in the current pediatric residency model. Congruent with the IOM conclusions, widespread implementation of the recommendations would require a significant increase in resident-provider workforce (of at least 25% and possibly up to 50%) to care for the same number of patients; the educational model would need to undergo a groundbreaking overhaul. In order for resident training to continue to thrive, programs and their leadership must strive to provide an ample amount of education, with time for reflective learning without significantly increasing workload intensity. Further trials and quality improvement projects will be needed prior to the widespread implementation of the new recommendations to learn what works best while causing the least harm, disruption, and unnecessary cost to the current resident education systems. Because of the diversity of residency programs, other unanticipated consequences, and severely limited resources, information from these projects is needed to guide the scale and pace of national revisions to the duty hour standards.
The authors intend to publish the complete study and data regarding this intervention—including details of our schedule and implementation process, additional results from sleep logs, and qualitative assessment of education, professionalism, resident well-being, and safety—in the upcoming months.
Footnotes
Katherine Auger, MD, and Kira Sieplinga, MD, are Attending Physicians at the Division of General Pediatrics, Cincinnati Children's Hospital Medical Center. Both were Pediatric Chief Residents during the 2008–2009 year and served as co–primary investigators of this project. Jeffrey Simmons, MD, MSc, is Assistant Professor of Pediatrics and a member of the Division of General Pediatrics at Cincinnati Children's Hospital Medical Center. He is Associate Director of the General Inpatient Services for research and has served as a research mentor on this project. Javier Gonzalez-del-Rey, MD, MEd, is Program Director of the Pediatric Residency Program at Cincinnati Children's Hospital Medical Center. He is Professor of Pediatrics and Associate Director of the Division of Pediatric Emergency Medicine.
References
- 1.Ulmer C., Wolman D., Johns M., editors. Committee on Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedules to Improve Patient Safety for the Institute of Medicine. Resident Duty Hours: Enhancing Sleep, Supervision, and Safety. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 2.Accreditation Council for Graduate Medical Education. Common program requirements: VI. Resident duty hours in the learning and working environment. Available at: http://www.acgme.org/acWebsite/dutyHours/dh_ComProgrRequirmentsDutyHours0707.pdf. Accessed October 8, 2009.
- 3.Figure adapted from Landrigan, et. al, as appears Ulmer C, Wolman D, Johns M, eds; Committee on Optimizing Graduate Medical Trainee (Resident) Hours and Work Schedules to Improve Patient Safety for the Institute of Medicine. Resident Duty Hours: Enhancing Sleep Supervision, and Safety. Washington, DC: National Academies Press; 2008. Page 107.
- 4.Landrigan C. P., Fahrenkopf A. M., Lewin D., Sharek P. J., Barger L. K., Eisner M., Edwards S., Chiang V. W., Wiedermann B. L., Sectish T. C. Effects of the accreditation council for graduate medical education duty hour limits on sleep, work hours, and safety. Pediatrics. 2008;122(2):250–258. doi: 10.1542/peds.2007-2306. [DOI] [PubMed] [Google Scholar]
- 5.Frank-Starling curve. Dictionary.com. The American Heritage® Stedman's Medical Dictionary. Houghton Mifflin Company. http://dictionary.reference.com/browse/Frank-Starling curve (accessed: November 08, 2009).