Abstract
Introduction
Given absence of a “gold standard” for measuring self-reported nicotine dependence, particularly among less experienced smokers, there is a need to evaluate existing measures to determine how well symptoms measure the underlying nicotine dependence construct and whether symptoms function differently for less experienced smokers. Study aims were to determine 1) likelihood of endorsement of individual symptoms at different levels of a nicotine dependence construct and the ability of symptoms to discriminate between different levels of this construct and 2) whether these symptom properties varied between nondaily and daily smokers.
Methods
We used multiple group Item Response Theory analysis to evaluate nicotine dependence symptoms from the Nicotine Dependence Symptom Scale based on a nationally representative sample of 8,081 recent onset adolescent smokers from the National Surveys on Drug Use and Health.
Results
After controlling for age, gender, smoking quantity and length of smoking exposure, symptoms assessing tolerance were invariant across nondaily and daily smokers, and discriminated well between levels of the nicotine dependence construct. However, the majority of symptoms functioned differently for nondaily and daily smokers. These symptoms did not discriminate as well between levels of the nicotine dependence construct and were more likely to be endorsed at lower levels of this construct for daily smokers.
Discussion
A measure that encompasses a range of symptoms tapping different aspects of smoking may be ideally suited for nondaily adolescent smokers, while an ideal measure of nicotine dependence for daily smokers might also include more core diagnostic features of nicotine dependence such as withdrawal and tolerance.
Keywords: tobacco, nicotine, dependence, assessment, adolescence, item response theory
1. Introduction
The conventional description of the natural history of dependent smoking is that individuals first try smoking in early to mid adolescence and then gradually escalate their frequency of smoking over a two- or three-year period to the point where they are smoking daily. Daily smokers continue to escalate their cigarette use as they develop into chronic, dependent smokers. Though this description is consistent with national survey data (e.g. Breslau, Johnson, Hiripi, & Kessler, 2001; SAMHSA, 2002), it represents an average that does not convey the wide variety of patterns that occur during the emergence of nicotine dependence. More recent evidence based on longitudinal studies of adolescent smokers has consistently shown that, for some adolescents, nicotine dependence symptoms emerge very soon after the onset of smoking and at low levels of nicotine exposure (i.e. light and/or intermittent smoking) (Dierker, et al., 2007; DiFranza, Savageau, Rigotti, et al., 2002; O’Loughlin, et al., 2003).
However, it is improbable that these intermittent smokers are nicotine dependent in the way that nicotine dependence is traditionally operationalized (Goedeker & Tiffany, 2008). That is, some dependence symptoms (for example, tolerance and withdrawal) may be less relevant to the measurement of the underlying construct for these smokers than they are for those smoking daily. This is supported by recent research which suggests that there are qualitative differences in the symptom profiles of dependent smokers (primarily daily smokers) and nondependent smokers (primarily nondaily smokers) (Goedeker & Tiffany, 2008). Yet, setting aside the question of whether or not these intermittent smokers are nicotine dependent, research suggests that the symptoms experienced by novice smokers who smoke only occasionally predict smoking at heavier levels in the future (Dierker & Mermelstein, under review). If the relevance of dependence symptoms to the construct being measured (be it actual nicotine dependence in regular, heavy smokers, or perhaps more accurately, level of propensity for continued and heavier smoking in intermittent, light smokers) differs, this suggests that the psychometric properties of the symptoms in the same measure of nicotine dependence may also differ between novice smokers who smoke intermittently and novice smokers who have attained a daily level of smoking.
This difference could lead to a major confound in measuring the nicotine dependence phenomena in novice smokers who are extremely heterogeneous in their smoking experience. To put it in simple terms, the underlying construct assessed by the same symptoms may mean different things depending upon one’s current level of exposure. This can lead to problems in measurement of the construct, as well as its interpretation if potential differences in the meaning of the construct are not considered. Consequently, it is important to establish whether or not many of the most commonly measured nicotine symptoms are suitable for the measurement of “dependence” in recent onset adolescent smokers in terms of both measurement and interpretation. If the psychometric characteristics of existing measures of nicotine dependence symptoms do in fact differ for recent onset smokers with different levels of smoking exposure, then these differences need to be considered in measuring the nicotine dependence construct. This is a necessary preliminary step to fully understand the expression of the nicotine dependence phenomena along the full range of smoking exposure.
In terms of measurement properties, symptoms may differ between nondaily and daily smokers in their likelihood of endorsement and in their ability to discriminate between individuals with different levels of the nicotine dependence construct. Items that differ across groups in these symptom characteristics are said to exhibit differential item functioning (DIF). A symptom with DIF indicates that daily and nondaily smokers with the same level on the latent nicotine dependence construct have a different probability of endorsing that symptom. Evidence of such differential item functioning (DIF) suggests that there are systematic differences in symptom endorsement between the population subgroups of interest, independent of their level of the underlying nicotine dependence construct. Assessing DIF is important to gain a better understanding of systematic group differences in symptom properties. DIF across smoking exposure groups could reflect true differences between groups on the nicotine dependence construct, bias in the measurement of the construct, or both. That is, observed differences between nondaily and daily smokers in the relations between nicotine dependence scores and other outcome variables may reflect DIF related bias instead of actual differences related to smoking exposure (Horn & McArdle, 1992; Meredith, 1993). Scores on the dependence construct that do not take into account variability in the psychometric properties of the symptoms are likely to be less accurate for population subgroups that differ on these properties.
With the exception of a few studies designed specifically to evaluate the emergence of nicotine dependence, (DiFranza, et al., 2000; DiFranza, Savageau, K. Fletcher, et al., 2002; O’Loughlin, et al., 2003), symptoms have often been assessed only among respondents that meet clearly established smoking patterns (i.e. most commonly, regular or daily use), thus constraining the range of smoking levels that can be examined and limiting the ability to consider dependence symptoms at lower levels of use. More recently, surveys of large nationally representative populations have substantially expanded inclusion criteria for the administration of nicotine dependence items allowing for more careful consideration of the early emerging aspects of dependence (Dierker & Donny, 2008; Kandel, Hu, Griesler, & Schaffran, 2007; Rose, Dierker, & Donny, 2010).
Aside from measuring nicotine dependence symptoms at nondaily levels of use, understanding the expression of nicotine dependence symptoms requires measures that (1) can assess degrees of the underlying construct on a continuum, rather than its categorical presence or absence, (2) are comprehensive enough to capture unique patterns of symptoms endorsement at different levels of smoking exposure, and (3) are appropriate for measuring the nicotine dependence phenomena among light and/or infrequent as well as established smokers (Tiffany, Conklin, Shiffman, & Clayton, 2004). The Nicotine Dependence Syndrome Scale (NDSS) clearly fulfills the first two criteria in that it is designed to measure nicotine dependence on a continuum with items representing a comprehensive range of experiences and behaviors believed to characterize nicotine addiction (Shiffman, Waters, & Hickcox, 2004). To date, however, no research has directly evaluated differences in psychometric properties of NDSS symptoms related to smoking exposure.
The present study used an Item Response Theory (IRT) approach to evaluate NDSS symptom level properties in a nationally representative sample of 8,081 recent onset adolescent smokers. Data were drawn from five annual National Surveys on Drug Use and Health (NSDUH), one of the largest, nationally representative, epidemiologic studies available to date that includes substantial heterogeneity in adolescent nicotine exposure, as well as assessment of nicotine dependence symptoms among adolescents as young as 12 years old. We combined data from the five surveys to ensure an adequate sample size to evaluate symptom endorsement for both nondaily and daily recent onset smokers. The aims of the study were to determine 1) the likelihood of endorsement of individual NDSS symptoms at different levels of an underlying nicotine dependence construct and the ability of individual symptoms to discriminate between adolescents with different levels of this construct; and 2) whether these symptom properties vary according to whether smokers are engaged in nondaily vs. daily smoking behavior (i.e., whether there is evidence of DIF).
2. Methods
2.1 Participants
The sample, drawn from data combining five annual NSDUH surveys (2002–2006), consisted of N=8,081 individuals age 12 to 21 who reported smoking 1) at least once in the past month and 2) their first exposure to smoking within the past two years . The NSDUH utilizes multistage area probability sampling methods to select a representative sample of the noninstitutionalized U.S. civilian population aged 12 or older. Persons living in households, military personnel living off base, and residents of noninstitutional group quarters including college dormitories, group homes, civilians dwelling on military installations, as well as persons with no permanent residence are included. The NSDUH oversamples adolescents ages 12 to 17 to improve precision of substance use estimates.
Sample characteristics are presented in Table 1. The majority (81%) were nondaily smokers. Most nondaily smokers (63.6%) reported smoking no more than 1 cigarette on the days they did smoke and 95% reported smoking 5 or fewer cigarettes on the days they smoked. Participants smoked an average 12.2 of the past 30 days (SE=0.16, range 1–30). Half (51%) had been smoking for more than one but no more than two years, and the rest began smoking in the past year.
Table 1.
Sample Characteristics (N=8081)
| Variable | N (design adjusted %) |
|---|---|
| Female | 4083 (48.3) |
| Age | |
| 12–17 years | 5041 (55.0) |
| 18–21 years | 3040 (45.0) |
| Ethnicity | |
| Non Hispanic White | 5395 (66.6) |
| Non Hispanic Black | 887 (12.0) |
| Hispanic | 1183 (15.8) |
| Other Ethnicity | 616 (5.5) |
| Cigarette Smoking | |
| Non-daily | 6552 (81.1) |
| Smoke >1 cigarette per day | 2327 (36.4) |
| Daily | 1529 (18.9) |
| Smoke >1 cigarette per day | 1440 (94.5) |
| Length of Exposure (maximum of 2 years) | |
| Began smoking within the past year | 4201 (50.9) |
| Began smoking more than 1 year ago | 3880 (49.1) |
2.2 Measures
Smoking variables
Cigarette exposure was assessed with three items. Participants were asked how many days they smoked cigarettes in the past 30 days. Smoking quantity was also assessed by asking participants to report the average number of cigarettes they smoked on the days that they smoked cigarettes in the past 30 days, and dichotomized into no more than one vs. more than one cigarette per day. Length of exposure was assessed by subtracting the age at which participants first reported smoking a cigarette from their current age, and dichotomizing into one year or less vs. between one and two years.
Nicotine Dependence
In the NSDUH, nicotine dependence was assessed using the 19 item Nicotine Dependence Syndrome Scale (NDSS; Shiffman, et al., 2004). Participants were asked to rate how true each of the symptoms was of their smoking during the past 30 days. Items were rated using the following response options: 1) not at all true, 2) sometimes true, 3) moderately true, 4) very true, 5) extremely true. The NDSS provides a single summary score for overall nicotine dependence that includes items measuring drive (i.e. craving and withdrawal symptoms), tolerance (i.e. reduced sensitivity to tobacco products), priority (i.e. preference for smoking over other reinforcers), continuity (i.e. regularity of smoking), and stereotypy (i.e. the “sameness” of smoking contexts). The NDSS has been shown to have good psychometric properties in both adolescent (Clark, et al., 2005) and adult (Shiffman & Sayette, 2005; Shiffman, et al., 2004 ) populations, and has been found to predict future smoking (Sledjeski, et al., 2007). Due to considerable missing data from an option allowing participants to skip two of the items measuring stereotypy and priority regarding nonsmoking friends (“Do you have any friends who do not smoke cigarettes?” and “There are times when you choose not to be around your friends who don't smoke, because they won't like it if you smoke”, respectively), these items were excluded from the analysis. In addition, four symptoms were reverse scored for the analyses so that endorsement was indicative of a greater level of underlying nicotine dependence. They included “feel a sense of control over smoking”; “it is normal to smoke several cigarettes in an hour, then not have another one until hours later”; “the number of cigarettes smoker per day often changes”; “the number cigarettes smoked per day is often influenced by other things”.
In their study of adolescents, Strong et al. (2009) found that the distribution of most NDSS symptom responses were skewed such that the majority of participants endorsed the “not at all true” option and that dichotomizing the NDSS responses increased model stability without a loss of information or reliability. We found responses to be similarly distributed in the current sample and thus chose to collapse the four response options categories of “sometimes true” to extremely true” into a single category to generate a dichotomous variable for symptom endorsement (No – not at all true vs. Yes – any of the four positive responses). Although this dichotomization could potentially result in some loss of information, the considerable skew on the four levels indicating positive symptom endorsement suggested that this risk was minimal. Furthermore, evaluating the psychometric properties for so many symptoms on an ordinal scale across two levels of smoking exposure is prohibitive for two reasons: 1) the number of IRT parameters to be estimated and interpreted across the two groups would be huge and would require a sample size of recent smokers even larger than the 8,081 available for this analysis, and 2) the considerable amount of skew on the symptoms would result in inadequate coverage, particularly on the moderately, very, and extremely true response categories.
2.3 Analysis
IRT analysis has the advantage of allowing us to examine differences in the probability of symptom endorsement among smokers engaged in daily vs. nondaily smoking behavior while controlling for level of the underlying nicotine dependence construct and other covariates. Therefore, we conducted multiple group 2-parameter item response theory (IRT) probit analyses (Muthen & Lehman, 1985) comparing nondaily and daily smokers to test whether the psychometric properties of symptoms along a single latent nicotine dependence continuum differed between these groups after controlling for age, gender, quantity smoked, and length of smoking exposure. Based on mounting evidence for a single primary nicotine dependence construct underlying nicotine dependence symptoms (Courvoisier & Etter, 2008; Strong, et al., 2009) and a preliminary exploratory factor analysis that indicated that the majority of the common variance in NDSS symptoms in the current sample was explained by a single factor (eigenvalues for the first and second factors = 9.2 and 1.5, respectively; 54% of variance explained by the first factor), we assumed a single latent nicotine dependence construct for the IRT analyses.
IRT analysis provides estimates of each symptom’s difficulty (severity) and discrimination. Symptom severity is the value of the latent nicotine dependence factor (which has a mean of zero and a standard deviation of one) at which the probability of symptom endorsement is 0.50, and is a function of the estimated symptom thresholds. Symptoms that have a higher probability of being endorsed at low levels of nicotine dependence have lower severity values. The difference between severity parameters across groups can be interpreted in the same manner as small, medium, or large effect sizes using Cohen’s (1988) criteria (Steinberg & Thissen, 2006). Symptom discrimination indicates which symptoms best differentiate among adolescents with different levels of nicotine dependence. It is a function of the slope (factor loading) of the symptom where higher values indicate greater symptom discrimination. Finally, the item characteristic curve (ICC) is a plot of these parameters combined, and is examined to simultaneously evaluate symptom severity and discrimination at different values of the latent nicotine dependence construct. We used Mplus (Version 5; Muthen & Muthen, 1998–2007) to conduct the IRT analyses.
To identify symptoms with DIF, we conducted a total of 16 multiple group IRT analyses where a model constraining the slope (discrimination) and threshold (severity) parameters for one symptom to be equal across groups (constrained model) was compared to an unconstrained model in which these parameters were free to vary for all symptoms, with the exception of a single anchor symptom (one that loads highly on the nicotine dependence construct in both groups and shows no evidence of DIF), for which the parameters are constrained to be equal across groups (Stark, Chernyshenko, & Drasgow, 2006). A single anchor symptom is required to ensure a common metric across smoking groups on the underlying nicotine dependence construct. Each of these models controlled for the effects of age (12–17 vs. 18–21 years), gender, smoking quantity, and length of exposure on the nicotine dependence factor by including paths regressing the latent nicotine dependence factor onto these variables. An approximate chi-square difference test provides a p-value for the difference in model fit between the constrained and unconstrained models. A significant p-value indicates a significantly worse fit of the constrained model and provides evidence of DIF for the symptom being tested. We used the Benjamini-Hochberg procedure to adjust for multiple significance tests (Benjamini & Hochberg, 1995; Thissen, Steinberg, & Kuang, 2002).
In the last step of the IRT analysis, we tested a final multiple group IRT model in which all symptoms showing evidence of DIF in the individual IRT models described above were free to vary across groups. This final model was used to generate ICCs, to obtain effect sizes for differences in symptom severity and to calculate an estimated maximum a posteriori (MAP) nicotine dependence factor score that takes into account each individual’s pattern of endorsement and differences in symptom IRT parameter estimates.
3. Results
Fit indices for the final multiple group IRT model were reasonable (Tucker-Lewis Index=0.93, Comparative Fit Index =0.90, Root Mean Square Error of Approximation = 0.06). In addition, the p-value associated with the approximate change in chi-square for the final multiple group IRT model compared to the unconstrained model was not significant (p=0.210). This indicated that fit was unaffected by simultaneously constraining all symptoms that did not show evidence of DIF in the individual IRT models. Table 2 shows the severity and discrimination estimates from the final model for each symptom for nondaily and daily smokers. Overall, the three symptoms assessing tolerance best discriminated between levels of nicotine dependence (i.e., had the highest slope coefficients). They included: 1) amount smoked increased, 2) need to smoke more to be satisfied (the anchor symptom), and 3) smoke more before feeling anything. Symptoms that did not discriminate well between levels of nicotine dependence included loss of control, both symptoms measuring priority of smoking: 1) avoiding nonsmoking places and 2) avoiding travel by plane, and one symptom assessing stereotypy of smoking (smoking unaffected by other things).
Table 2.
NDSS Symptom Item Response Parameter Estimates
| Symptom | Nondaily Smokers | Daily Smokers | Δχ2 p value | Effect Size for Severity DIF | ||
|---|---|---|---|---|---|---|
| Discrimination (slope) | Severity (threshold) | Discrimination (slope) | Severity (threshold) | |||
| Drive | ||||||
| After not smoking for a while, you need to smoke to feel less restless and irritable | 1.20 | 1.05 | 0.84 | 0.97 | 0.009* | 0.08 |
| When you don’t smoke for a few hours, you start to crave cigarettes* | 1.39 | 1.42 | 0.96 | 1.36 | 0.000* | 0.06 |
| You sometimes have strong cravings for a cigarette where it feels like you are in the grip of a force that you can’t control | 0.94 | 1.68 | 0.94 | 1.68 | 0.766 | NA |
| You feel a sense of control over your smoking – that is you can “take it or leave it” at any timea | 0.54 | 0.31 | 0.54 | 0.31 | 0.067 | NA |
| You sometimes worry that you will run out of cigarettes | 1.44 | 1.87 | 0.87 | 1.98 | 0.000* | 0.11 |
| Priority | ||||||
| You tend to avoid places that don't allow smoking, even if you would otherwise enjoy them | 0.32 | 2.71 | 0.32 | 2.71 | 0.560 | NA |
| Even if you’re travelling a long distance, you’d rather not to travel by plane because you wouldn’t be allowed to smoke | 0.73 | 3.05 | 0.73 | 3.05 | 0.447 | NA |
| Continuity | ||||||
| It’s normal for you to smoke several cigarettes in an hour, then not have another one until hours latera | 0.81 | 1.52 | 0.46 | 1.42 | 0.000* | 0.10 |
| You smoke cigarettes fairly regularly throughout the day | 1.72 | 1.41 | 0.73 | 0.79 | 0.000* | 0.62 |
| You smoke about the same amount on weekends as on weekdays | 0.95 | 0.96 | 0.21 | −0.80 | 0.000* | 1.76 |
| You smoke just about the same number of cigarettes from day to day | 1.21 | 0.97 | 0.42 | −1.50 | 0.000* | 2.47 |
| It’s hard to say how many cigarettes you smoke per day because the number often changesa | 0.88 | 0.55 | 0.32 | 0.63 | 0.000* | 0.08 |
| Tolerance | ||||||
| Since you started smoking, the amount you smoke has increased | 1.40 | 0.84 | 1.40 | 0.84 | 0.080 | NA |
| Compared to when you first started smoking, you need to smoke a lot more now in order to be satisfied | 1.77 | 1.46 | 1.77 | 1.46 | Anchor | NA |
| Compared to when you first started smoking, you can smoke much, much more now before you start to feel anything | 1.17 | 1.12 | 1.17 | 1.12 | 0.702 | NA |
| Stereotypy | ||||||
| Your smoking is not affected much by other things. For example, you smoke the same amount whether you’re relaxing or working, happy or sad, alone or with others | 0.50 | 0.38 | 0.09 | −3.84 | 0.000* | 4.22 |
| The number cigarettes you smoke per day is often influenced by other things – how you’re doing, what you’re feeling, for examplea | 0.89 | 0.14 | 0.89 | 0.14 | 0.471 | NA |
Note: The Δχ2 p value represents the p value for the change in chi square between the model in which the discrimination and severity parameters were free to vary across groups (baseline model) and the model in which these parameters for the symptom of interest were constrained to be equal across groups.
reverse coded.
significant using the Benjamini-Hochberg procedure for Type I error rate adjustment for multiple tests (Thissen et al., 2002)
The symptom thresholds represent severity, the estimated level of nicotine dependence at which each symptom is endorsed by 50% of the population of interest. That is, symptoms with low thresholds are more likely to be endorsed at lower levels of nicotine dependence compared to other symptoms, and are therefore considered to have low severity. Overall, symptoms with the lowest severity included: loss of control, no change in amount smoked per day, and the two symptoms assessing stereotypy (smoking unaffected by other things and no influence on amount smoked per day). Symptoms with high thresholds overall, indicating a low probability of endorsement at all but the highest levels of nicotine dependence (high severity), included both symptoms measuring priority of smoking.
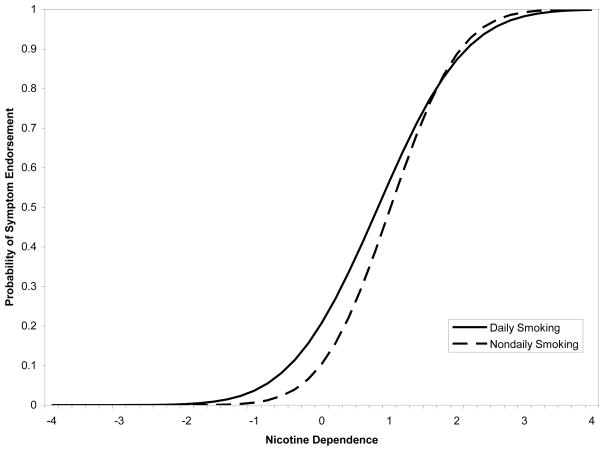
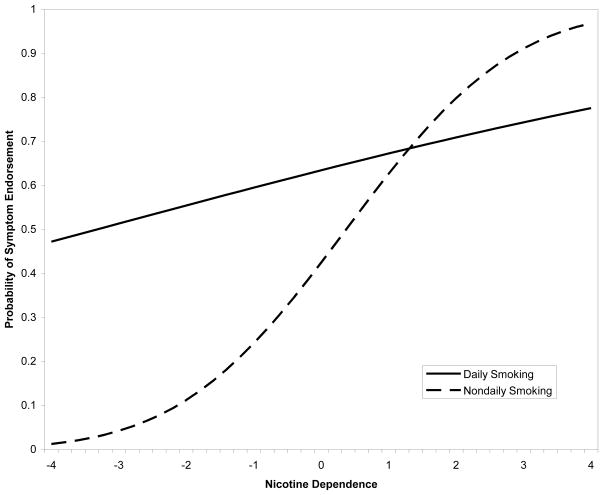
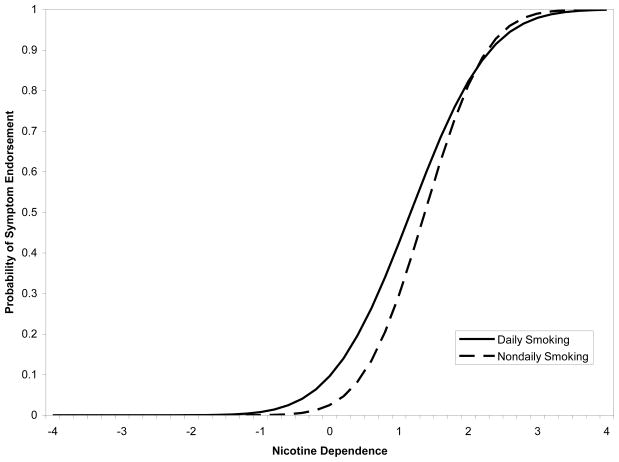
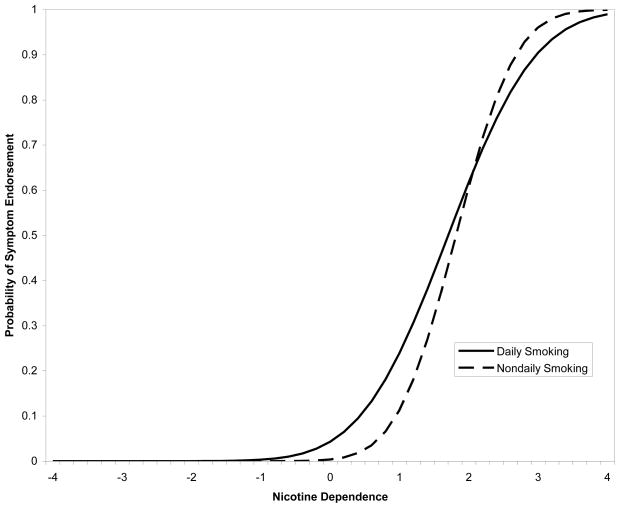
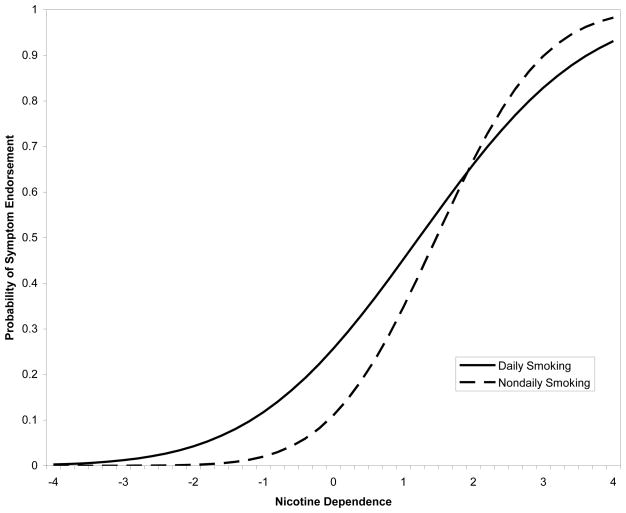
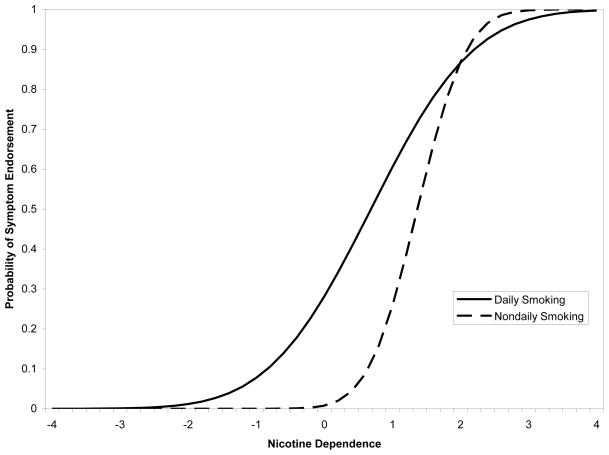
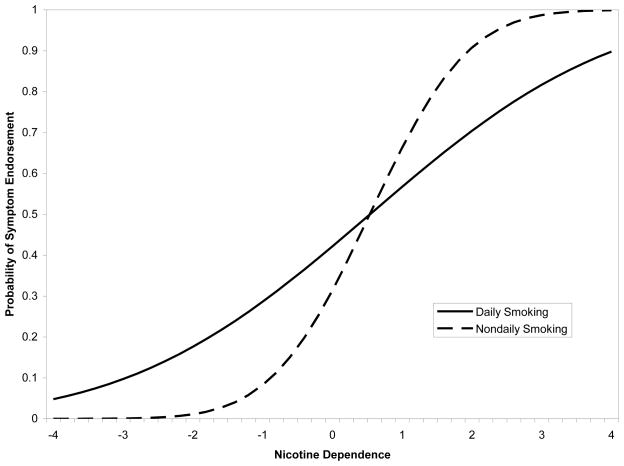
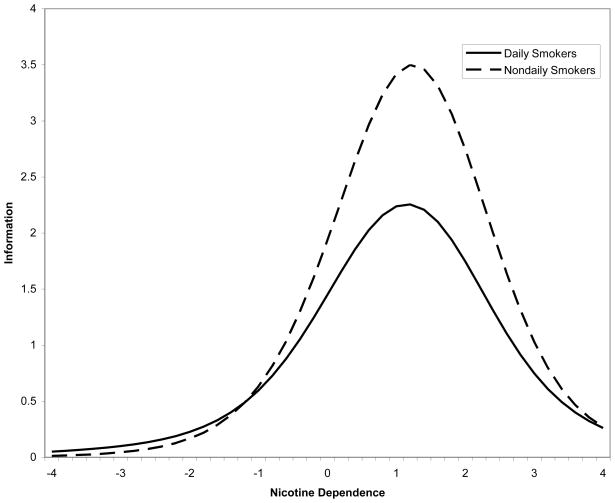
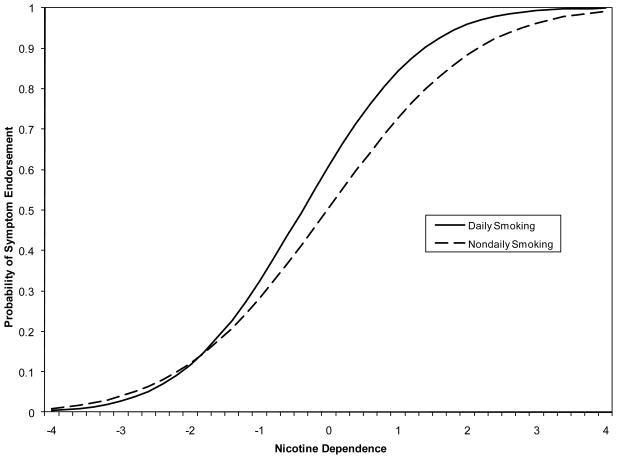
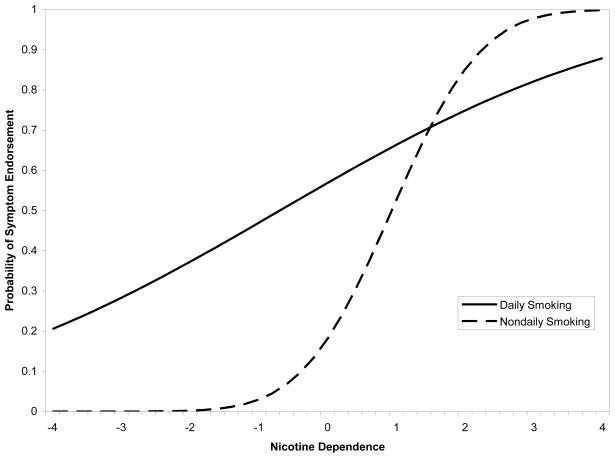
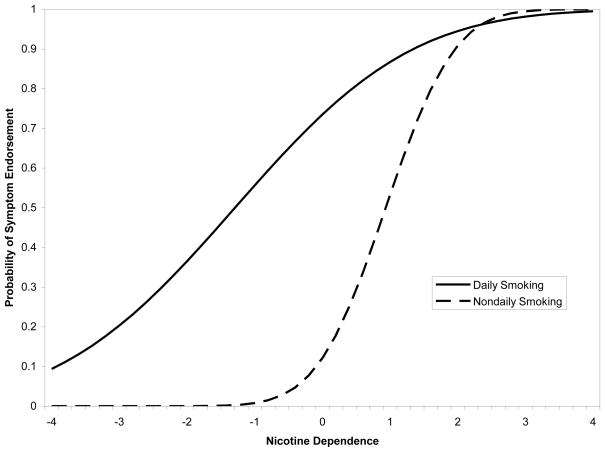
When comparing symptom endorsement for nondaily vs. daily smokers, DIF was found for 9 of the 17 of the nicotine dependence symptoms, indicating that nondaily and daily smokers differed either in symptom discrimination (estimated slope) or severity (estimated threshold), or both, after controlling for their level of the nicotine dependence construct (i.e., their IRT factor score), as well as effects of age, gender, quantity smoked, and length of exposure (Table 2). The ICCs, which show how the symptoms differ between daily and non daily smokers, are shown in Figures 1–9. For all 9 symptoms, the slopes were less steep for daily smokers compared to nondaily smokers, indicating that these symptoms did not discriminate as well between levels of the nicotine dependence construct for daily smokers as they did for nondaily smokers. That is, the likelihood of endorsement of these symptoms was less sensitive to changes in levels of the dependence construct for daily smokers, indicating that the symptoms were weaker indicators of the underlying construct for daily smokers as they were for nondaily smokers. Although, statistically significant, the difference in discrimination between the two groups was very small for irritability and craving symptoms (Figures 1 and 2). Larger differences were present for worry about running out of cigarettes and not normal to smoke a lot then go without cigarettes, however, the less steep ICCs for not normal to smoke a lot then go without indicated that that this symptom did not discriminate as well in either group (Figures 3–4). Differences in discrimination were largest for four of the five symptoms assessing continuity of smoking: 1) smoke regularly throughout the day, 2) smoke same amount on weekends and weekdays, 3) smoke same amount each day, and 4) no change in amount smoked each day (Figures 5–8). In addition, the symptom smoking unaffected by other things, which did not discriminate well between levels of dependence in either group, discriminated even more poorly among levels of dependence for daily smokers (Figure 9).
Figure 1.
Item Characteristic Curves for Irritability Symptom.
Figure 9.
Item Characteristic Curves for Smoking Not Affected by Other Things Symptom.
Figure 2.
Item Characteristic Curves for Craving Symptom.
Figure 3.
Item Characteristic Curves for Worry About Running Out of Cigarettes Symptom.
Figure 4.
Item Characteristic Curves for Not Normal to Smoke A Lot Then Go Without Symptom.
Figure 5.
Item Characteristic Curves for Smoke Regularly Throughout the Day Symptom.
Figure 8.
Item Characteristic Curves for No Change in Amount Smoked per Day Symptom.
All of the nine symptoms differed across groups in both discrimination and severity, as evidenced by the crossing over of the ICC curves shown in Figures 1–9. However, the majority of the differences in symptom severity were very small (ranging from 0.06 for craving to 0.11 for worrying about running out of cigarettes), indicating that the observed DIF between nondaily and daily smokers was primarily due to differences in symptom discrimination rather than differences in severity. In contrast, large differences in symptom severity between nondaily and daily smokers were observed for smoking unaffected by other things (effect size=4.22) and three of the five continuity symptoms: 1) smoke regularly throughout the day (effect size=0.62), 2) smoke same amount on weekends and weekdays (effect size=1.76), and 3) smoke same amount each day (effect size=2.47). For these symptoms, severity appeared to be lower for daily smokers, meaning that daily smokers were more likely than nondaily smokers to endorse these symptoms at lower levels of the nicotine dependence construct, after controlling for age, gender, smoking quantity, and length of exposure.
Figure 10 shows the total information function curves for all 17 NDSS symptoms for nondaily and daily smokers. The total information function curve shows the amount of information in the underlying nicotine dependence construct that is explained by the NDSS symptoms as a whole across a range of levels of the nicotine dependence construct. Higher levels of information indicate more precise measurement of the construct. Examining the total information curve is valuable for understanding which levels of the underlying construct are best captured by the full measure for each smoking exposure group. This is important because a single total NDSS dependence score is often used to represent nicotine dependence in studies of this phenomena, and the total information curve helps to shed light on levels of the nicotine dependence construct that are not represented as well by the measured symptoms. It can also reveal important differences between levels of smoking exposure on overall measurement of the construct. The curves in Figure 10 suggest that, while the NDSS symptoms appear to be most precise for higher levels of nicotine dependence in both groups of smokers, they are more precise for nondaily smokers than for daily smokers.
Figure 10.
NDSS Total Information Curves.
Finally, we examined whether symptoms showing DIF as a function of smoking frequency changed if we had not controlled for variability in smoking quantity. We did this by following the same DIF testing procedure with the exception that we removed smoking quantity as a covariate in the models. The results of these analyses did not differ, with the exception of the symptom assessing the extent to which the adolescent felt a sense of control over smoking. This symptom was invariant in the analyses controlling for smoking quantity, but exhibited a DIF effect when smoking quantity was not controlled (p=0.009 for the change in chi-square; see Figure 11). Loss of control did not discriminate between levels of the ND construct as well as other symptoms in either group and showed slightly lower discrimination in nondaily smokers (discrimination parameters = 0.52 and 0.61 for nondaily and daily smokers, respectively). There was a moderately small difference between groups in severity for this symptom (effect size = 0.43), such that severity was lower for daily smokers (severity = −0.45) compared to nondaily smokers (severity = −0.02).
Figure 11.
Item Characteristic Curves for DIF in Loss of Control When Smoking Quantity is not Controlled.
4. Discussion
Given the absence of a “gold standard” for measuring self-reported nicotine dependence symptoms, particularly among less experienced smokers (Colby, Tiffany, Shiffman, & Niaura, 2000; DiFranza, et al., 2002; DiFranza, et al., 2007; Kassel, 2000; O'Loughlin, Tarasuk, DiFranza, & Paradis, 2002), there is a need to evaluate existing measures to determine how well individual symptoms measure the underlying nicotine dependence construct and whether individual symptoms function differently for less experienced smokers. Ideally, measures should be designed so that all items 1) discriminate well between levels of the underlying construct and are therefore considered strong indicators of the construct, 2) capture the full range of severity of the underlying construct, 3) and are equivalent in these psychometric properties across population subgroups. If nonequivalence is identified, then the scoring of the construct for further analysis should take this into account.
The current study examined these symptom properties in nondaily and daily recent onset adolescent smokers using symptoms from the NDSS. Symptoms assessing tolerance for smoking were found to be invariant across nondaily and daily smokers, and appeared to discriminate well between levels of nicotine dependence for both groups, indicating that these symptoms were most strongly related to the underlying nicotine dependence construct, regardless of level of smoking exposure. This suggests that these symptoms may be important and consistent features of the underlying nicotine dependence symptom construct for both nondaily and daily smokers. In addition, despite statistically significant DIF across the two groups for symptoms of irritability and craving, this DIF was relatively small. Of the wide range of symptoms assessed by the NDSS, irritability, craving, and tolerance symptoms may best characterize the nicotine dependence construct in both nondaily and daily smokers, and therefore may be considered among the most important symptoms to assess in any self-report measure of this construct among recent onset smokers.
On the other hand, symptoms assessing priority of smoking (avoiding places where smoking is not allowed and preferring not to travel by plane because smoking is not allowed) did not discriminate well between levels of the nicotine dependence construct. In addition, the estimated probability of endorsing either priority symptom was very low across all but the highest levels of the construct. This suggests that these two symptoms may not be ideal for measuring a nicotine dependence construct in recent onset adolescent smokers. It is likely that adolescents generally have fewer opportunities to avoid places or to make decisions about how they will travel, and thus these symptoms are less applicable in this population. Consequently, a measure of nicotine dependence symptoms for use with adolescents may not suffer a loss of precision if symptoms tapping this particular aspect of dependence are excluded.
Despite some consistencies in NDSS symptoms across nondaily and daily smokers, the majority of NDSS symptoms appeared to work differently for the two smoking exposure groups. Overall, the results indicated that these symptoms did not appear to be as strongly related to the underlying nicotine dependence construct for daily smokers compared to nondaily smokers. That is, all of the symptoms that differed across smoking groups did not discriminate between levels of nicotine dependence for daily smokers as well as they did for nondaily smokers. Four of the symptoms also showed large differences in severity. Symptoms of smoking un affected by other things, smoke regularly throughout the day, smoke same amount on weekends and weekdays, and smoke same amount each day had lower severity for daily smokers suggesting that they are more likely to be endorsed by daily smokers with low levels of the nicotine dependence symptom construct than nondaily smokers with low levels of this construct. For these symptoms, symptom discrimination and severity appear strongly linked, such that there was a higher probability of endorsement of these symptoms among daily smokers even at low levels of the nicotine dependence construct (low severity), and therefore the probability of endorsement did not change as much as the nicotine dependence construct level increased (low discrimination). In other words, daily smokers appear to have a relatively high probability of endorsing these symptoms regardless of their level of the nicotine dependence construct. For those who are already smoking daily, continuity may already be established, and therefore may have less of an impact on level of the nicotine dependence construct. However, for those who are smoking at nondaily levels, the probability of endorsing continuity symptoms increased rapidly for small changes in the level of the underlying construct. This could indicate that the development of continuity of smoking may be more closely tied to increasing dependence, and that continuity symptoms may represent particularly good markers of this trend in nondaily smokers. Previous research on this population has shown that endorsement of symptoms reflecting continuity or regularity of smoking increases as the number of smoking days increases for nondaily smokers, whereas these symptoms are highly endorsed by daily smokers regardless of the amount they smoke each day (Rose, Dierker, & Donny, 2010).
Another possibility for the observed DIF in the continuity items may be that the frame of reference for what constitutes “regular” smoking may differ between nondaily and daily smokers. That is, relatively novice daily smokers may already see themselves as regular in their smoking, just by virtue of having achieved daily smoking, compared to their likely recent history of non-daily smoking or their peer-group norm of non-daily smoking. In other words, their reference for assessing their current regularity may be highly intermittent non-daily smoking. By contrast, daily smokers may assess their regularity on a different basis, for example by the degree of regularity of smoking within a day as opposed to the degree of regularity between days. Differences in the frame of reference may also apply to the loss of control symptom that showed DIF when smoking quantity was not controlled for. That is, those who smoke more each day may already see themselves as having lost control over smoking and therefore may be more likely to endorse this symptom at a lower level of the nicotine dependence construct, and this may be particularly true for daily smokers.
The other symptoms showing DIF also tended to have a higher probability of endorsement at lower levels of nicotine dependence for daily smokers compared to nondaily smokers, and the NDSS total information curves indicate that the NDSS as a whole appeared to be a less precise measure of the nicotine dependence construct for daily smokers. Taken together, these results suggest that many of the symptoms from the NDSS may be less sensitive for measuring the nicotine dependence construct for daily smokers. Symptoms that appeared sensitive to changes in the nicotine dependence construct in both nondaily and daily smokers were those symptoms that tapped craving, irritability and tolerance. The tolerance symptoms are consistent with tolerance symptoms from the DSM-IV, and cravings may reflect withdrawal. Indeed, symptoms from the DSM-IV have been found to more precisely measure nicotine dependence for smokers with higher levels on the underlying dependence construct (Strong, et al., 2009). NDSS symptoms have also been shown to predict future smoking behavior above and beyond current level of smoking exposure (Dierker & Mermelstein, under review; Sledjeski, et al., 2007). It appears as though tolerance and withdrawal may be considered defining characteristics of a dependence construct at both low and high levels of smoking exposure, and consequently, important to include as part of any self-report measure of nicotine dependence.
Strong et al. (2009) suggest that improved self-report measures of an underlying continuum of nicotine dependence may be developed by drawing on symptoms from multiple measures of dependence. The current study provides support for this approach by revealing that the symptoms that best measure a nicotine dependence symptom construct vary across different subpopulations of adolescent smokers even after controlling for the influence of age, gender, smoking quantity, and smoking exposure on this construct. The NDSS, which includes a range of symptoms that tap multiple aspects of dependence, may best capture a full range of levels on a nicotine dependence symptom construct in less frequent recent onset smokers. However, for more frequent daily smokers in this group, a measure that best captures nicotine dependence may be one that replaces symptoms assessing continuity of smoking with additional items that tap core diagnostic features of tolerance and withdrawal.
A major strength of this study is that it involved a large, nationally representative data set, which allowed us to evaluate nicotine dependence symptoms in larger subgroups of nondaily and daily smokers than past research has allowed and in a broader population of recent onset adolescent smokers. The sample size also allowed us to focus exclusively on smokers who had begun smoking within the past two years, which reduced the potential confounding effect of smoking behavior or dependence prior to those years on symptom endorsement. We were also able to evaluate a wide range of nicotine dependence symptoms that measured a number of aspects of dependence beyond more frequently evaluated symptoms of dependence such as tolerance and withdrawal. Finally, our study examined DIF in nicotine dependence symptoms between nondaily and daily smokers controlling for important covariates such as gender, age, smoking quantity and length of exposure.
Despite the numerous strengths of this study, there are some limitations that should be noted. First, although the NDSS assesses a large and comprehensive number of symptoms that tap several aspects of nicotine dependence, it is only one of several existing measures of nicotine dependence symptoms. It is important to determine whether DIF across smoking exposure groups is present for other measures of nicotine dependence symptoms. Second, we analyzed symptoms as dichotomous (not endorsed vs. any endorsement) variables, and assumed a single underlying nicotine dependence factor. Although past research, the distribution of the symptom responses, and preliminary factor analysis all supported our data analytic decisions, the results might have differed had we tested a polytomous or multidimensional IRT model. In addition, we did not include sample weights in the analysis. Using sample weights estimated from a full sample on a selected subset of the sample may result in inaccurate weighting in the analyses. While statistical methods to accurately handle the problems associated with using full sample estimated weights on data analytic subsamples have been developed (Muthen & Muthen, 1998–2007), they are not available for multiple sample analyses. Therefore, we are cautious in generalizing these results to the national population. However, the lack of sample weights in this study’s analyses do not present a significant problem because we focused on the relation between the symptoms and the underlying construct and whether there are differences in these relations as a function of smoking exposure. That is, we used a model based method, as opposed to a design based method, where the goal was not inference to the broader population about specific relations between the construct and other variables that might be associated with this construct.
These data and the IRT analyses do not identify other possible mechanisms that might underlie the observed symptom DIF. Although symptom endorsement could reflect the neurobiological consequences of nicotine use, other factors may also influence symptom reporting. For example, expectations about smoking may influence the extent to which adolescents endorse symptoms as they begin to identify themselves as smokers, although new research has not found evidence to support this hypothesis (Ursprung, DiFranza, Costa, & DiFranza, 2009). Likewise, an adolescent particularly low in response inhibition or with high negative affect may be more likely to report a loss of control over smoking. Indeed, recent studies have demonstrated that individual differences in nicotine dependence are related to a history of major depression (Dierker & Donny, 2008) and the rate in which monetary rewards are discounted over time (Sweitzer, Donny, Dierker, Flory, & Manuck, 2008). These mechanisms may also influence the pattern of symptom endorsement, which is likely to vary substantially at different levels of smoking exposure. One advantage of IRT analysis is that it provides an estimated individual level score on the underlying construct that takes into account not only DIF, but also each individual’s pattern of symptom endorsement. As a result, this score may be more reliable and valid across the full range of smoking exposure than traditional methods for scoring nicotine dependence that do not take into account these sources of variability. Although beyond the scope of this study, this score can be used in further analyses designed to test theoretically and empirically driven analyses of risk factors for and consequences of nicotine dependence symptoms.
Finally, we did not explore DIF in other population subgroups. While recent research on DIF in nicotine dependence symptoms across racial/ethnic subgroups has not found meaningful differences in properties of symptoms from the Fagerstrom Test for Nicotine Dependence (Johnson, Morgan-Lopez, Breslau, Hatsukami, & Bierut, 2008), more research is required to determine whether a lack of differences is found in additional demographic subgroups.
In sum, the current study revealed that NDSS symptoms assessing irritability, tolerance and withdrawal were strongly related to an underlying continuum of a nicotine dependence symptom construct in both nondaily and daily adolescent smokers who had begun smoking within the past two years, even after controlling for age, gender, smoking quantity and length of smoking exposure. However, the majority of the nicotine dependence symptoms as measured by the NDSS did not discriminate as well between levels of nicotine dependence for daily smokers compared to nondaily smokers, suggesting that these symptoms may not be as well suited for assessing the nicotine dependence construct in this population. Continuity symptoms, in particular, appeared to be strong indicators of increases in the level of the underlying nicotine dependence construct only for nondaily smokers. This suggests that if the NDSS is used in a population of recent onset smokers with a heterogeneous range of smoking exposure, the psychometric properties of the symptoms may vary as a function of smoking exposure. Consequently, the scoring of the NDSS measure for inferential analysis should take into account these differences. Although there is no straightforward algorithm to create a dependence score that accounts for DIF across different studies, the methods used to obtain this score (multiple group IRT/binary confirmatory factor analysis) are relatively straightforward and statistical software to conduct these analyses has become considerably more accessible. It certainly requires more preliminary work to obtain these scores; however the benefits may outweigh the cost, particularly when the primary goal is to examine group differences in nicotine dependence.
Assessing nicotine dependence symptoms, particularly in novice adolescent smokers, has proven a significant challenge, but the development of a measure that combines symptoms from a number of different existing measures of nicotine dependence symptoms may be a promising approach to improving our ability to measure a nicotine dependence construct via self report (Strong, et al., 2009). Given the apparent complexity of nicotine dependence, as well as the number of existing measures and potential symptoms, the process of selecting the ideal list of symptoms for such a measure is daunting, and as this study indicates, the types of symptoms may vary depending on the frequency of smoking. This study suggests that a measure that encompasses a wide range of symptoms tapping different aspects of smoking may be ideally suited for less frequent adolescent smokers, while an ideal measure of nicotine dependence for daily adolescent smokers might be one that more fully taps core diagnostic features of nicotine dependence such as withdrawal and tolerance.
Figure 6.
Item Characteristic Curves for Smoke Same Amount on Weekends and Weekdays Symptom.
Figure 7.
Item Characteristic Curves for Smoke Same Amount Each Day Symptom.
Acknowledgments
Role of Funding Source
Financial support for the conduct of this research was provided by grants DA024260, DA15454 and DA022313 (Dierker) from the National Institute on Drug Abuse, by a Center Grant (DA010075) awarded the Methodology Center, Penn State University and by awards from the Patrick and Catherine Weldon Donaghue Medical Research Foundation and the Peter F. McManus Charitable Trust (Dierker). These agencies had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
We would like to thank an anonymous reviewer for providing the alternative explanation that differential item functioning in symptoms assessing continuity of smoking may be due to nondaily and daily smokers having a different frame of reference for what might constitute regular smoking.
Footnotes
Contributors
All authors participated in the preparation of this manuscript. Authors Jennifer Rose and Lisa Dierker designed the study and wrote the first draft of the manuscript. Author Jennifer Rose undertook the statistical analysis. All authors contributed to and have approved the final manuscript.
Conflict of Interest
All other authors declare that they have no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: A practical and powerful approach to multiple significance testing. Journal of the Royal Statistical Society, Series B. 1995;57:289–300. [Google Scholar]
- Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine Dependence in the United States: Prevalence, Trends, and Smoking Persistence. 2001;58(9):810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- Clark DB, Wood DS, Martin CS, Cornelius JR, Lynch KG, Shiffman S. Multidimensional assessment of nicotine dependence in adolescents. Drug and Alcohol Dependence. 2005;77(3):235–242. doi: 10.1016/j.drugalcdep.2004.08.019. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale: Laurence Erlbaum Associates; 1988. [Google Scholar]
- Colby SM, Tiffany ST, Shiffman S, Niaura RS. Measuring nicotine dependence among youth: a review of available approaches and instruments. Drug and Alcohol Dependence. 2000;59(Supplement 1):23–39. doi: 10.1016/s0376-8716(99)00163-5. [DOI] [PubMed] [Google Scholar]
- Courvoisier D, Etter JF. Using item respose theory to study the convergent and discriminant validity of three questionnaires measuring cigarette dependence. Psychology of Addictive Behaviors. 2008;22:391–401. doi: 10.1037/0893-164X.22.3.391. [DOI] [PubMed] [Google Scholar]
- Dierker L, Donny E. The role of psychiatric disorders in the relationship between cigarette smoking and DSM-IV nicotine dependence among young adults. Nicotine & Tobacco Research. 2008;10:439–446. doi: 10.1080/14622200801901898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dierker LC, Donny E, Tiffany S, Colby SM, Perrine N, Clayton RR Tobacco Etiology Research Network (TERN) The association between cigarette smoking and DSM-IV nicotine dependence among first year college students. Drug & Alcohol Dependence. 2007;86:106–114. doi: 10.1016/j.drugalcdep.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Dierker L, Mermelstein R. Early Emerging Nicotine Dependence Symptoms: A signal of propensity for chronic smoking behavior among experimental adolescent smokers. Pediatrics. doi: 10.1016/j.jpeds.2009.11.044. under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Rigotti NA, Fletcher K, Ockene JK, McNeill AD, Coleman M, Wood C. Development of symptoms of tobacco dependence in youths: 30 month follow up data from the DANDY study. Tobacco Control. 2002;11:228–235. doi: 10.1136/tc.11.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Rigotti NA, McNeill AD, Ockene JK, Savageau JA, St Cyr D, Colemanm M. Initial symptoms of nicotine dependence in adolescents. Tobacco Control. 2000;9:313–319. doi: 10.1136/tc.9.3.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Fletcher K, Ockene JK, Rigotti NA, McNeill AD, Coleman M, Wood C. Measuring the loss of autonomy over nicotine use in adolescents: The DANDY (Development and Assessment of Nicotine Dependence in Youths) study. Archives of Pediatrics & Adolescent Medicine. 2002;156(4):397–403. doi: 10.1001/archpedi.156.4.397. [DOI] [PubMed] [Google Scholar]
- DiFranza JR, Savageau JA, Fletcher K, Pbert L, O'Loughlin J, McNeill AD, Ockene JK, Friedman K, Hazelton J, Wood C, Dussault G, Willman RJ. Susceptibility to Nicotine Dependence: The Development and Assessment of Nicotine Dependence in Youth 2 Study. Pediatrics. 2007;120:e974–983. doi: 10.1542/peds.2007-0027. [DOI] [PubMed] [Google Scholar]
- Goedeker KC, Tiffany ST. On the Nature of Nicotine Addiction: A Taxometric Analysis. Journal of Abnormal Psychology. 2008;117(4):896–909. doi: 10.1037/a0013296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horn JL, McArdle JJ. A practical and theoretical guide to measurement invariance in aging research. Experimental Aging Research. 1992;18:117–144. doi: 10.1080/03610739208253916. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Morgan-Lopez AA, Breslau N, Hatsukami DK, Bierut LJ. Test of measurement invariance of the FTND across demographic groups: Assessment, effect size, and prediction of cessation. Drug and Alcohol Dependence. 2008;93(3):260–270. doi: 10.1016/j.drugalcdep.2007.10.001. [DOI] [PubMed] [Google Scholar]
- Kandel D, Hu M, Griesler P, Schaffran C. On the development of nicotine dependence in adolescence. Drug & Alcohol Dependence. 2007;91:26–39. doi: 10.1016/j.drugalcdep.2007.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kassel J. Are adolescent smokers addicted to nicotine? The suitability of the nicotine dependence construct as applied to adolescents. Journal of Child & Adolescent Substance Abuse. 2000;9:27–49. [Google Scholar]
- Meredith W. Measurement invariance, factor analysis, and factorial invariance. Psychometrika. 1993;58:525–543. [Google Scholar]
- Muthen BO, Lehman J. Multiple group IRT modeling: Applications to item bias analysis. Journal of Educational Statistics. 1985;10:133–142. [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide. 5. Los Angeles, CA: Muthen & Muthen; 1998–2007. [Google Scholar]
- O'Loughlin J, Tarasuk J, DiFranza J, Paradis G. Reliability of selected measures of nicotine dependence among adolescents. Annals of Epidemiology. 2002;5:353–362. doi: 10.1016/s1047-2797(01)00312-x. [DOI] [PubMed] [Google Scholar]
- O’Loughlin J, DiFranza J, Tyndale RF, Meshefedjian G, McMillan-Davey E, Clarke P, Hanley J, Paradis G. Nicotine-dependence symptoms are associated with smoking frequency in adolescents. American Journal of Preventive Medicine. 2003;25:219–225. doi: 10.1016/s0749-3797(03)00198-3. [DOI] [PubMed] [Google Scholar]
- Rose J, Dierker L, Donny E. Nicotine dependence symptoms among recent onset adolescent smokers. Drug & Alcohol Dependence. 2010;106:126–132. doi: 10.1016/j.drugalcdep.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA. Office of Applied Studies, National Survey on Drug Use and Health 2002 [Google Scholar]
- Shiffman S, Sayette MA. Validation of the nicotine dependence syndrome scale (NDSS): a criterion-group design contrasting chippers and regular smokers. Drug and Alcohol Dependence. 2005;79:45–52. doi: 10.1016/j.drugalcdep.2004.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Waters AJ, Hickcox M. The Nicotine Dependence Syndrome Scale: A multidimensional measure of nicotine dependence. Nicotine & Tobacco Research. 2004;6(2):327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Dierker LC, Costello D, Shiffman S, Donny E, Flay BR. Predictive validity of four nicotine dependence measures in a college sample. Drug and Alcohol Dependence. 2007;87(1):10–19. doi: 10.1016/j.drugalcdep.2006.07.005. [DOI] [PubMed] [Google Scholar]
- Stark S, Chernyshenko OS, Drasgow F. Detecting differential item functioning with confirmatory factor analysis and item response theory: Toward a unified strategy. Journal of Applied Psychology. 2006;91(6):1292–1306. doi: 10.1037/0021-9010.91.6.1292. [DOI] [PubMed] [Google Scholar]
- Strong DR, Kahler CW, Colby SM, Griesler PC, Kandel D. Linking measures of adolescent nicotine dependence to a common latent continuum. Drug and Alcohol Dependence. 2009;99:296–308. doi: 10.1016/j.drugalcdep.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweitzer MM, Donny EC, Dierker LC, Flory JD, Manuck SB. Delay discounting and smoking: Association with the Fagerstrom Test for Nicotine Dependence but not cigarettes smoked per day. Nicotine & Tobacco Research. 2008;10:1571 – 1575. doi: 10.1080/14622200802323274. [DOI] [PubMed] [Google Scholar]
- Thissen D, Steinberg L, Kuang D. Quick and Easy Implementation of the Benjamini-Hochberg Procedure for Controlling the False Positive Rate in Multiple Comparisons. Journal of Educational and Behavioral Statistics. 2002;27(1):77–83. [Google Scholar]
- Tiffany ST, Conklin CA, Shiffman S, Clayton RR. What can dependence theories tell us about assessing the emergence of tobacco dependence? Addiction. 2004;99(S1):78–86. doi: 10.1111/j.1360-0443.2004.00734.x. [DOI] [PubMed] [Google Scholar]
- Ursprung WWSA, DiFranza SM, Costa AD, DiFranza JR. Might expectations explain early self-reported symptoms of nicotine dependence? Addictive Behaviors. 2009;34(2):227–231. doi: 10.1016/j.addbeh.2008.10.013. [DOI] [PubMed] [Google Scholar]