Abstract
Purpose
The purpose of this study was to evaluate the clinical effectiveness of and patient's satisfaction with treatment of gingival melanin hyperpigmentation with a Nd:YAG laser and a high speed rotary instrument.
Methods
Three patients with melanin hyperpigmentation in the anterior parts of the gingiva were chosen for this case study. Clinical photographs were taken at the preoperative state and three patients were treated under local anesthesia. In the maxilla, the gingival deepithelization was conducted with a high speed diamond bur, whereas, in the mandible with a Nd:YAG laser. Clinical photographs were taken immediately after the procedures and at the 1st, 2nd, and 4th week to evaluate clinical color changes. A week after the procedure, the patients filled out a questionnaire about any pain or discomfort. At the 4th week after the procedure, the patients filled out questionnaires about esthetic aspects of the results of treatment.
Results
In all cases, both anterior gingival areas were depigmented with satisfaction and the patients did not complain of severe pain or discomfort. At the 1st week of healing, the gingiva showed moderate to fast epithelization. Two weeks after the procedure, clinically, the gingiva showed almost complete healing. Four weeks after the procedure, there was significant improvement in gingival melanin hyperpigmentation.
Conclusions
The Nd:YAG laser and the high speed rotary instruments seem to be effective for the esthetic treatment of gingival melanin hyperpigmentation.
Keywords: Hyperpigmentation, Laser, Melanin
INTRODUCTION
Brown or dark pigmentations and discolorations of the gingival tissues, whether physiological or pathological, can be caused by a variety of local and/or systemic factors [1]. Melanin, a nonhemoglobin-derived brown pigment produced by melanocytes of the basal layer of the epithelium [2,3], is the most common reason for the endogeneous pigments. In dark-skinned people, an oral pigmentation is likely to increase, though there is no difference in the number of melanocytes between fair-skinned and dark-skinned individuals [4]. The degree of the pigmentation seems to be related to the differences in melanocyte activity. High levels of oral pigmentation are usually observed in those of African, East Asian, or Hispanic ethnicity [5].
The hyperpigmentation of the gingiva is benign in most cases, and is not a medical concern [6]. However, it may cause esthetic problems for some individuals, especially those who have gummy smiles. Those individuals may become more conscious of the black and dark pigmentation patches and request their removal [7], particularly if the hyperpigmentation appears on the facial aspect of the gingiva, thus being, visible during smiles and speech [8].
In recent years, there is an increasing need for esthetics and growing cosmetic demands for a pleasing smile in many individuals. In particular, women are more conscious of the black or dark pigmentation patches on the facial aspects of the gingiva, which may be strikingly apparent during smiling and speaking [8]. Many clinicians have tried to remove melanin hyperpigmentation of the gingiva with various methods.
Thus, the purpose of this study was to evaluate the clinical effectiveness of and patient satisfaction with the treatment of gingival melanin hyperpigmentation with a Nd:YAG laser and a high speed rotary instrument in three cases.
CASES DESCRIPTION
Study population
The study included three patients requesting an esthetic treatment for gingival melanin hyperpigmentation in the anterior part of the maxilla and mandible at Kyungpook National University Hospital, Department of Periodontics.
Treatment procedures
All patients were treated under local anesthesia with 2% lidocaine. In the maxillary gingiva, the deepithelization was conducted with a high speed diamond bur (Dia-BURS BR-12EF®, MANI Inc., Tochigi-ken, Japan) accompanied with copious water irrigation. For bleeding control, the surgical sites were pressured with gauze soaked with normal saline. In the mandible, the gingiva was deepithelized with a Nd:YAG laser (SDL 3000®, B&B System Inc., Seoul, Korea). The Nd:YAG laser was set at 10 W, 100 mJ, 20 Hz. The patient was instructed to avoid smoking, eating spicy food, or brushing the bare wounds. All patients were prescribed analgesics and NSAIDs after the surgery for 3 days for pain management.
Clinical evaluation and patient's questionnaire
Clinical photographs were taken at the preoperative state, during the procedures, immediately after the procedures, and 1, 2, and 4 weeks after the procedures. At one week follow-up after the procedure, the patients filled out a questionnaire about pain and discomfort. At the 4-week follow-up, the patients filled out a questionnaire about the esthetic aspects of the treatment.
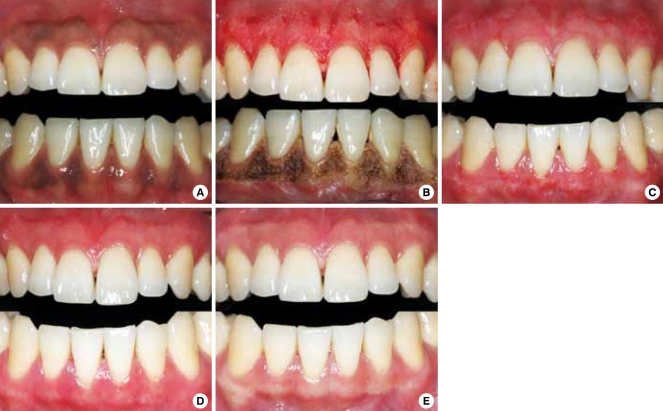
Case 1
A 32-year-old male had a chief complaint of pigmented gingiva, visible when he smiled and spoke. A severe gingival melanin hyperpigmentation was found at the labial surface of both the maxilla and the mandible (Fig. 1). The patient's medical history was noncontributory. One week after the operation, the maxillary gingiva showed fast epithelization, whereas, the mandibular gingiva showed slow epithelization with unhealed ulcerations. The patient complained of mild pain at the mandibular gingival areas. Two weeks after treatment, clinically, both gingiva were healed almost completely. One month after, there were significant improvements in gingival melanin hyperpigmentation without recurrence or gingival recessions or deformities. The patient was satisfied with the esthetically improved gingival color.
Figure 1.
Clinical photographs of case 1. (A) Preoperative appearance. (B) Immediately after operation. (C) Postoperative, 1 week. (D) Postoperative, 2 weeks. (E) Postoperative, 1 month.
Case 2
A 40-year-old male had a chief complaint of dark gingival melanin patches and a pathologic tooth migration due to chronic periodontitis on the maxillary anterior region. A moderate melanin hyperpigmentation of the gingiva was found on the labial surfaces of both maxillary and mandibular arches (Fig. 2). The patient's medical history was noncontributory. In order to prevent further migration, periodontal treatment was carried out. A month after the periodontal treatment, the melanin depigmentation procedure was performed. One week after the depigmentation, both gingiva presented similarly fast epithelization though they were still under the healing process. The patient did not complain of any discomfort. Two weeks after, both gingival areas showed almost complete healing although some ulcerated lesions remained in the maxillary gingiva. One month after, significant improvements in the gingival melanin hyperpigmentation were shown without gingival recessions or deformities. However, a slight pigmentation remained in the mandibular gingival area. However, the patient was satisfied with the esthetically improved gingival color because the mandibular gingival area was mostly not seen while he smiled and spoke.
Figure 2.
Clinical photographs of case 2. (A) Preoperative appearance. (B) Immediately after operation. (C) Postoperative, 1 week. (D) Postoperative, 2 weeks. (E) Postoperative, 1 month.
Case 3
A 40-year-old female had a chief complaint of pigmented gingiva visible while she smiled and spoke. A severely melanin hyperpigmented gingiva was found at the labial surfaces of the maxillary arch (Fig. 3). The patient's medical history was noncontributory. One week after the surgery, gingiva presented slow epithelization with immature healing. The patient complained of mild pain in the maxillary gingival area. Two weeks after, the maxillary gingiva showed almost complete healing. One month after, the gingival color was significantly improved without recurrence or gingival recessions or deformities. The patient was satisfied with the esthetically improved gingival color.
Figure 3.
Clinical photographs of case 3. (A) Preoperative appearance. (B) Immediately after operation. (C) Postoperative, 1 week. (D) Postoperative, 2 weeks. (E) Postoperative, 1 month.
DISCUSSION
There are increasing demands for cosmetic therapy for gingival melanin pigmentation. Consequently, various methods, including gingivectomy [9], gingivectomy with a free gingival autografting [10], electrosurgery [11], cryosurgery [12], chemotherapy with 90% phenol [13], and abrasion with a diamond bur [14], have been used with different degrees of success [5]. Gingivectomy results in alveolar bone loss, delayed healing by secondary intention, and excessive pain. A free gingival graft usually requires an additional surgical site and a careful concern for color matching. Furthermore, the presence of a demarcated line that is commonly visible around the graft at the recipient site may elicit an esthetic problem itself [7]. Cryosurgery requires the clinician's skillful management of complicated techniques and instruments. Chemical agents, such as 90% phenol and 95% alcohol, have been used in combination; however, these chemical agents are quite harmful to the oral soft tissues [14].
Recently, a laser has been used to ablate cells containing and producing the melanin pigment. The Nd:YAG laser produces invisible, near-infrared light with a wavelength of 1,064 nm. Because the Nd:YAG laser has rays that have an affinity for melanin or other dark pigments, it works more efficiently when the beam is applied under the presence of a pigment [15]. No significant side effects of scarring, or textural or pigmentary changes have been reported and the incidence of hypopigmentation has been reported as lower than that by other types of lasers [16]. Throughout the depigmentation procedure of the ablation, the laser was cautiously used to avoid injury to the tooth surface and the adjacent tissues. In addition, the thin gingival tissue around the root prominence was ablated gently. The same area should not be ablated several times because the laser can ablate the periosteum resulting in gingival fenestration and bone exposure [14].
When the deepithelization is performed with a high speed diamond procedure, it is recommended to use the largest size of diamond bur. Small burs cannot make smooth surfaces easily and have a tendency to make small pits in the surgical sites which require further correction [7]. All pigmented gingival areas should be removed completely to prevent possible repigmentation. The procedure selected in this study is relatively simple and versatile; moreover, it requires a minimum of time and effort. If repigmentation occurs, the procedure can be done repeatedly in the same areas without clinical limitations or causing any permanent damage [7].
In the present study, both the Nd:YAG laser and the high speed rotary instrument were found to be clinically effective in the treatment of melanin hyperpigmentation. All patients were satisfied with the esthetically improved gingival color and did not report any severe pain or discomforts during and/or after the procedure.
In summary, both the Nd:YAG laser and the high speed rotary instrument seem to be effective in the esthetic treatment of gingival melanin hyperpigmentation.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Dummett CO. Oral tissue color changes. Ala J Med Sci. 1979;16:274–283. [PubMed] [Google Scholar]
- 2.Ozbayrak S, Dumlu A, Ercalik-Yalcinkaya S. Treatment of melanin-pigmented gingiva and oral mucosa by CO2 laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;90:14–15. doi: 10.1067/moe.2000.106396. [DOI] [PubMed] [Google Scholar]
- 3.Carranza AC, Saglie FR. Clinical features of gingivitis. In: Glickman I, Carranza FA, editors. Glickman's clinical periodontology. 7th ed. Philadelphia: Saunders; 1990. pp. 109–125. [Google Scholar]
- 4.Dummett CO. Clinical observations on pigment variations in healthy oral tissues of the Negro. J Dental Res. 1945;24:7–13. [Google Scholar]
- 5.Rosa DS, Aranha AC, Eduardo Cde P, Aoki A. Esthetic treatment of gingival melanin hyperpigmentation with Er:YAG laser: short-term clinical observations and patient follow-up. J Periodontol. 2007;78:2018–2025. doi: 10.1902/jop.2007.070041. [DOI] [PubMed] [Google Scholar]
- 6.Esen E, Haytac MC, Oz IA, Erdogan O, Karsli ED. Gingival melanin pigmentation and its treatment with the CO2 laser. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:522–527. doi: 10.1016/j.tripleo.2004.02.059. [DOI] [PubMed] [Google Scholar]
- 7.Farnoosh AA. Treatment of gingival pigmentation and discoloration for esthetic purposes. Int J Periodontics Restorative Dent. 1990;10:312–319. [PubMed] [Google Scholar]
- 8.Dummett CO. Overview of normal oral pigmentations. Ala J Med Sci. 1979;16:262–273. [PubMed] [Google Scholar]
- 9.Bergamaschi O, Kon S, Doine AI, Ruben MP. Melanin repigmentation after gingivectomy: a 5-year clinical and transmission electron microscopic study in humans. Int J Periodontics Restorative Dent. 1993;13:85–92. [PubMed] [Google Scholar]
- 10.Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int. 1996;27:555–558. [PubMed] [Google Scholar]
- 11.Gnanasekhar JD, al-Duwairi YS. Electrosurgery in dentistry. Quintessence Int. 1998;29:649–654. [PubMed] [Google Scholar]
- 12.Yeh CJ. Cryosurgical treatment of melanin-pigmented gingiva. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86:660–663. doi: 10.1016/s1079-2104(98)90199-8. [DOI] [PubMed] [Google Scholar]
- 13.Hasegawa A, Okagi H. Removing melagenous pigmentation using 90 percent phenol with 95 percent alcohol. Dent Outlook. 1973;42:673–676. [Google Scholar]
- 14.Atsawasuwan P, Greethong K, Nimmanon V. Treatment of gingival hyperpigmentation for esthetic purposes by Nd: YAG laser: report of 4 cases. J Periodontol. 2000;71:315–321. doi: 10.1902/jop.2000.71.2.315. [DOI] [PubMed] [Google Scholar]
- 15.Goldstein A, White JM, Pick RM. Clinical applications of the Nd:YAG laser. In: Miserendino L, Pick RM, editors. Lasers in dentistry. Chicago: Quintessence Publishing Co.; 1995. pp. 199–216. [Google Scholar]
- 16.Wheeland RG. Basic laser physics and visible light laser surgery. In: Wheeland RG, editor. Cutaneous surgery. Philadelphia: WB Saunders; 1994. pp. 1027–1058. [Google Scholar]