Abstract
Objective
Cross-sectional data indicate that persons with serious mental illness have increased risk of institution-based care, yet little is known about the long-term course of nursing home placement for persons with schizophrenia. This study describes nursing home entrance over a 10-year period among community residing Medicaid enrollees with schizophrenia compared with Medicaid enrollees with no mental illness.
Methods
The authors analyzed claims of 7,937 New Hampshire Medicaid beneficiaries aged 40 and older. Claims were followed annually from 1996 to 2005 to determine nursing home admission. Schizophrenia was identified from International Classification of Diseases: 9th Edition codes and used to model nursing home admission controlling for medical severity, physical disability, sex, and age. Cox proportional hazard models were run for the entire sample and then separately for middle-aged (40–64 years) and older-aged (65 years and older) subgroups.
Results
Persons with schizophrenia enter nursing homes earlier (median age 65) than persons with no mental illness (median age: 80). The greatest relative disparity occurs at middle age (40–64 years), where nursing home admission risk was 3.90 (95% confidence interval = 2.86–5.31) times greater for persons with schizophrenia than for persons with no mental illness.
Conclusions
Middle-aged persons with schizophrenia have almost four times greater likelihood of early institutionalization in nursing homes compared with their same age peers with no mental illness. Efforts to prevent/reduce unwarranted nursing home admission among persons with schizophrenia should focus on health status in the fifth decade of life.
Keywords: Schizophrenia, Medicaid, nursing home, older adults
Over the past 20 years, a series of laws and court decisions have been enacted to reduce unwarranted institutionalization of persons with mental illness. The aim of these regulations (e.g., the Omnibus Budget Reconciliation Act of 1987, the Preadmission Screening and Annual Resident Review, and the Olmstead decision) is to ensure the quality and appropriateness of nursing home care and to prevent unwarranted institutionalization of persons with mental illness who otherwise could live at home or in community-based care.1,2
These rulings are associated with an overall decline in nursing home admissions for persons with serious mental illness.3 However, for many older adults, nursing homes persist as a major provider of long-term, institution-based psychiatric care.2 Studies indicate that a majority of nursing facility residents have a mental disorder or clinically significant psychiatric symptoms,1,2 even though the quality of mental healthcare in many of these institutions remains poor and access to treatment is limited.1,4
Affordable and adequate housing has been shown to improve quality of life and overall functioning among persons with long-term mental illness.5,6 Many older adults express a desire to remain in their own residence6,7 and consider nursing homes the last resort.8 Given the high cost of nursing home care, particularly for individuals with schizophrenia,9 preventing unwarranted institutionalization of persons with mental illness both could reduce overall healthcare costs and improve quality of life.
Previous research has examined patterns of nursing home entrance among persons with and without mental illness.3,10–12 Institutionalization increases with age across all populations, especially for those with schizophrenia,10,13 but among nursing home residents aged 65 or older, the average age of persons with schizophrenia is much younger compared with other residents.12 Given evidence that persons with schizophrenia die 20% earlier than the general population,14–17 we expect their fifth and sixth decades of life also may be associated with increased rates of institutionalization in nursing homes.
We are not aware of any studies that directly compare the risk of early institutionalization among persons with schizophrenia to persons of similar age with no mental illness. To address this gap in the research literature, we used New Hampshire Medicaid data from 1995 to 2005 to explore the following questions:
Is the risk of being admitted to a nursing home higher among persons with schizophrenia than among persons with no mental illness?
Does the risk of nursing home admittance for persons with schizophrenia compared with persons with no mental illness differ in middle age compared with older age?
METHODS
Sample and Data Source
The baseline study sample for these analyses was extracted from electronic eligibility files and records of all New Hampshire Medicaid claims paid between January 1, 1995 and December 31, 1995. First, we eliminated anyone with current nursing home claims. Next, we used International Classification of Diseases: 9th Edition (ICD-9) claims diagnoses to identify persons with a schizophrenia spectrum disorder, including schizoaffective disorder (ICD-9 codes: 295.0–295.99). For persons with more than one psychiatric diagnosis, the schizophrenia spectrum disorder took precedence unless that individual also had a dementia. Although dementia is a predictor of nursing home admission, we removed persons with both schizophrenia and dementia because they are less likely to be eligible for alternative or community residential settings (compare Mechanic and McAlpine3). We then eliminated other individuals diag nosed with any other serious mental illness, Alzheimer Disease or other dementia, or mental retardation (developmental disorders) to form a comparison group of persons with no serious mental illness. Finally, we limited the sample to individuals of middle or older age (40 years or older).
Use of these data for this research was approved by the Committee for the Protection of Human Subjects both for Dartmouth College and the State of New Hampshire.
Measures
To identify members of this 1995 sample who subsequently entered a nursing home, we retrospectively reviewed their Medicaid claims records over a 10-year period, from 1996 to 2005. Because nursing homes also are used for short-term, rehabilitative purposes, nursing home residence was coded for individuals in a particular year only if they had nursing home claims for at least 2 months and for at least 20 bed days out of each month. Although Medicaid is not the sole payer of nursing home costs, it accounts for 50% of all expenditures and 70% of bed days.18 For each year 1996–2005, individuals received a score of “1” (residing in a nursing home) or “0” (not residing in a nursing home). Deaths also were recorded (“1” = dead, “0” = not dead) in the year that they occurred. Persons in the 1995 study sample who were still alive but had no Medicaid claims during one of these years were coded as not residing in a nursing home.
Presence of a life-threatening illness in 1995 was measured using a Charlson Comorbidity Index (CCI). This measure estimates the risk of 1-year mortality associated with 19 comorbidities;19 we used aversion modified for use with ICD-9 diagnostic codes.20,21 Comorbidities are weighed according to mortality risk and summed (e.g., myocardial infarction has a weight of “1,” HIV AIDS receives a weight of “6”) so that a higher score means greater mortality risk. We collapsed the CCI into two categories (“1” = one or more serious comorbidities, “0” = none).
We included an indicator for any individual qualifying for Medicaid under the category of “permanently and totally disabled” (“1” = presence of disability, “0” = no disability). New Hampshire defines this status as persons unable to perform “gainful activity” for 48 months subsequent to the impairment.22 Finally, age (years) and sex (female = 1) were used as control variables. We did not include race or ethnicity because 96% of the cohort was coded as “White.” These measures were calculated from 1995 Medicaid claims.
Analyses
We first used 1995 New Hampshire Medicaid claims to define a study sample of individuals that included persons with a schizophrenia spectrum disorder or no major mental illness, aged 40 years and older, and not living in a nursing home. We retro spectively reviewed their New Hampshire Medicaid claims records for each year from 1996 to 2005 to determine whether, and in what year, these individuals entered a nursing home (for at least 2 months with 20 days of claims in each month) or died.
We next used χ2 tests to compare baseline characteristics of persons with schizophrenia to those with no mental illness. Finally, we used Cox proportional hazard models to analyze the occurrence of nursing home admission among persons with schizophrenia compared with persons with no mental illness, controlling for age, sex, CCI, and disability. We estimated models for the entire sample first and then separately for middle-aged (40–64 years) and older-aged adults (65 years or older).
Cox estimation accounts both for the event occurrence (nursing home admission) and time to the event. Unlike logistic regression, this method allows us to include individuals who die during the study period, making use of all available data. Deaths are censored cases, as are individuals with no nursing home claims meeting our criteria for residency (right-censored cases). We recognize that our yearly assessment of events alternatively could be analyzed with discrete time models, but we felt that for our purposes, 10 years of data provided a reasonable approximation of continuous time. SPSS version 14.0 was used for all analyses.
RESULTS
Sample Characteristics
Our initial 1995 New Hampshire Medicaid demographic file contained 22,733 persons aged 40 or older. We excluded 11,012 individuals whose claims indicated they already were living in a nursing home. We then removed 3,784 individuals with the following primary psychiatric diagnoses: Alzheimer disease (N = 261), bipolar disorder (N = 202), major depression (N = 1,270), developmental disorder/mental retardation (N = 791), and other serious mental illness (1,260).
Our final study sample included 7,937 individuals; 7,090 (89.3%) with no mental illness diagnosis during 1995, and 847 (10.7%) with a schizophrenia spectrum disorder diagnosis. Among persons with schizophrenia, 184 (22%) were diagnosed with a second mental illness: 90 (10.6%) with an affective disorder, 125 (14.8%) with another serious mental illness, and 31 (3.7%) with a substance abuse disorder.
In 1995, 84% of the sample resided in their own home or received housing assistance to live independently. The remainder lived in a variety of residential care/assisted living facilities. Between 1996 and 2005, 1,081 (13.6%) entered a nursing home, including 122 (14.4%) persons with schizophrenia and 959 (13.5%) persons with no mental illness. The median age of nursing home admittance was 65 (interquartile range = 59–72) for persons with schizophrenia and 80 (interquartile range = 72–87) for persons with no mental illness.
To test our measure of long-term nursing home stay, we reviewed data for 77 individuals whose nursing home claims fit our criteria in 1 year but not the next. Eleven (11.2%) of these people returned to the nursing home in a later year and remained there through the end of the study period. The remaining 66 cases were split proportionately across persons with schizophrenia (N = 6, 0.7%) and persons with no mental illness (N = 60, 0.8%). These 66 individuals may have returned to live in the community, but because omitting them did not change the results significantly, we included these cases in our final sample.
A similar approach was used to examine the effect of missing claims data. Persons with no missing claims were those who either died during the study period or had Medicaid claims records for every year during 1996–2005. Sixty-one percent of all cases, including 77% of persons with schizophrenia and 54% of persons with no mental illness met these criteria. Among the 39% of persons missing from the Medicaid claims in one of the study years, most had claims in subsequent years (e.g., present in 1996–1997, absent in 2000, present in 2001–2005). Although we cannot determine who moved out of the state, we expect that most of the missing claims are attributable either to individuals with no health claims in a given year or to those who failed to qualify for Medicaid in that year. We ran our Cox models on the 61% sample with no missing data; the results were statistically significant and in the same direction as the full sample. All cases were retained in our final analyses.
Table 1 displays characteristics of the overall sample. We used χ2 tests to evaluate differences between persons with schizophrenia and with no mental illness. Persons with schizophrenia were younger (Pearson χ2 = 221.0, df = 3, p <0.001), less ill medically by CCI score (Pearson χ2 = 55.9, df = 1, p <0.001), less likely to have a physical disability (Pearson χ2 = 204.2, df = 1, p <0.001), and less likely to be female (Pearson χ2 = 39.8, df = 1, p <0.001). Although persons with no mental illness in this sample had a higher crude mortality rate (Pearson χ2 = 67.6, df = 1, p <0.001), these differences disappear when controlling for age, gender, CCI, and disability status. Results of a logistic regression predicting death while controlling for these factors showed that persons with schizophrenia were 30% more likely than those with no mental illness to die during the 10-year study frame (odds ratio 1.30, Wald χ2 = 6.16, p <0.02).
TABLE 1.
Characteristics of the Study Population at Baseline
| Total (N = 847) |
Schizophrenia (N = 7,937) |
No. Mental Illness (N = 7,090) |
Pearson χ2 (two sided) |
p | ||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |||
| Nursing home (NH) status | ||||||||
| Admitted | 1,081 | 13.6 | 122 | 14.4 | 959 | 13.5 | 0.5 (df = 1) | 0.48 |
| Not admitted | 6,856 | 86.4 | 725 | 85.6 | 6,131 | 86.5 | ||
| Died during 1995–2005 | ||||||||
| Dead | 2,586 | 32.6 | 170 | 20.1 | 2,416 | 34.1 | 67.6 (df = 1) | <0.001 |
| Not dead | 5,351 | 67.4 | 677 | 79.9 | 4,674 | 65.9 | ||
| Age in 1995 | ||||||||
| 40–49 | 2,602 | 32.8 | 398 | 47.0 | 2,204 | 31.1 | 221.0 (df = 3) | <0.001 |
| 50–64 | 2,423 | 30.5 | 329 | 38.8 | 2,094 | 29.5 | ||
| 65–79 | 1,945 | 24.5 | 105 | 12.4 | 1,840 | 26.0 | ||
| 80+ | 967 | 12.2 | 15 | 1.8 | 952 | 13.4 | ||
| Charlson score in 1995 (risk of 1-year mortality) |
||||||||
| 0 | 6,879 | 86.7 | 804 | 94.9 | 6,075 | 85.7 | 55.9 (df = 1) | <0.001 |
| ≥1 | 1,058 | 13.3 | 43 | 5.1 | 1,015 | 14.3 | ||
| Physical disability in 1995 (permanent/total disability) |
||||||||
| Yes | 2,393 | 30.1 | 75 | 8.9 | 2,318 | 32.7 | 204.2 (df = 1) | <0.001 |
| No | 5,544 | 69.9 | 772 | 91.1 | 4,772 | 67.3 | ||
| Gender | ||||||||
| Female | 5,362 | 67.6 | 491 | 58.0 | 4,871 | 68.7 | 39.8 (df 1) | <0.001 |
| Male | 2,575 | 32.4 | 356 | 42.0 | 2,219 | 31.3 | ||
Within the study sample, 5,025 (63.3%) persons were “middle aged” (40–64 years) and 2,912 (36.7%) were “older aged” (65 years or older). Persons with schizophrenia comprised 14.5% of the younger group and 4.1% of the older group. Nursing home admission rates were greater for middle-aged persons with schizophrenia (11.3%) compared with persons with no mental illness (4.5%) (Pearson χ2 = 54.3, df = 1, p <0.001). Older persons entered nursing homes at a higher rate than middle-aged persons (27.6% versus 5.5%, respectively), but within this older age group, no statistically significant differences were found between persons with schizophrenia (33.3%) and those with no mental illness (27.4%) (Pearson χ2 = 2.1, df = 1, p < 0.15).
Cox Proportional Hazards Models
Table 2 shows the results from the Cox proportional hazard models. Three such models were evaluated: all ages, middle aged (40–64 years only), and older aged (65 years or older). These analyses model the hazard ratio (HR) or risk of nursing home entrance for each indicator in the model. Overall, persons with schizophrenia were 2.35 times more likely to be in a nursing home than persons with no mental illness. The risk of nursing home admission also was higher at older ages (HR = 1.10) and among women (HR = 1.42).
TABLE 2.
Cox Proportional Hazards Models of Nursing Home Admission
| Overall Model, All Ages (N = 7,937) |
Middle Aged, 40–64 Years (N = 5,025) |
Older Aged, 65 Years or Older (N = 2,912) |
||||
|---|---|---|---|---|---|---|
| Variable | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI | Hazard Ratio | 95% CI |
| Schizophrenia diagnosis | 2.35a | 1.91–2.87 | 3.90a | 2.86–5.31 | 1.61b | 1.17–2.22 |
| Age (years) | 1.10a | 1.09–1.10 | 1.10a | 1.08–1.12 | 1.08a | 1.07–1.09 |
| Charlson score >0 | 1.12 | 0.93–1.36 | 1.21 | 0.88–1.66 | 1.08 | 0.86–1.36 |
| Female | 1.42a | 1.21–1.65 | 1.36c | 1.05–1.76 | 1.45a | 1.19–1.76 |
| Disability (yes) | 1.19 | 0.98–1.45 | 1.72a | 1.28–2.33 | 0.59 | 0.24–1.44 |
Notes: p values based on Wald χ2 with 1 df.
p <0.001.
p <0.01.
p <0.05.
The next model in Table 2 provides results of the Cox analysis for the middle aged sample. Persons with schizophrenia aged 40–64 in 1995 have 3.90 times the risk of entering a nursing home compared with individuals of similar age with no mental illness. Other risk factors for nursing home admittance among the middle-aged cohort are age (HR = 1.10), being female (HR = 1.36), and having a physical disability (HR = 1.72). The final model in Table 2 presents results of the Cox analysis for the adults aged 65 and older. Schizophrenia remains associated with an increased risk of nursing home admission (HR = 1.61), as well as age (HR = 1.08) and being female (HR = 1.45).
We ran another Cox model with an interaction term between age category and schizophrenia to test whether the hazard ratio of 3.90 in the middle-aged sample differed significantly from the hazard ratio of 1.61 in the older-aged sample. The results of the interaction term (HR = 0.56, Wald χ2 = 5.92, df = 1, p <0.02) indicate that although the absolute risk of nursing home placement increases with age regardless of diagnosis, the difference in the effect of schizophrenia on nursing home entrance between the two age groups is greater for persons of middle age.
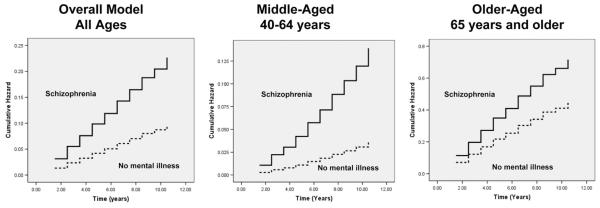
A visual display of these differences is shown in Fig. 1. The greater slope of the line for middle-aged persons with schizophrenia indicates the significantly greater likelihood of nursing home admittance compared with persons with no mental illness in this age group. The slopes of the lines within the chart for older adults aremore similar, reflecting the lower relative difference in nursing home risk between persons with schizophrenia and no mental illness at older age.
FIGURE 1. Schizophrenia Versus No Mental Illness: Hazard Plots.
Each of the plots is drawn on a separate scale. The cumulative hazard (Y axis) across the time period (X axis) for individuals over age 65 is higher (0.1– 0.7) than the cumulative hazard for the middle-aged group (0.01– 0.13), indicating the overall greater risk of nursing home entrance among older adults compared with middle-aged persons. However, the slopes of the lines within each age-group chart show the relative likelihood of nursing home entrance for persons with schizophrenia compared with those persons with no mental illness.
We conducted two additional exploratory analyses to examine whether the early institutionalization found in our middle-aged sample applies to other types of mental illness. In these final Cox models, we first substituted persons with major depression (N = 677) for those with schizophrenia. Although depressed persons overall were more likely than those with no mental illness to be institutionalized in a nursing home (HR = 1.4, Wald χ2 = 6.7, df = 1, p <0.01), the difference was significant in the older sample (HR = 2.2, Wald χ2 = 18.6, df = 1, p <0.001) but not the middle-aged one (HR = 1.0, Wald χ2 = 0.002, df = 1, p = 0.96). We next looked at persons with bipolar disorder (N = 202). We ran a single model with an interaction term for age because the numbers were very small (only 25 people were older than 65 years and only 32 ended up in a nursing home). Overall, persons with bipolar disorder did enter the nursing home at a greater rate than persons with no mental illness at all ages (HR = 2.4, Wald χ2 = 11.4, df = 1, p <0.001). However, the interaction term between age category and bipolar disorder was not significant in the model (HR = 0.9, Wald χ2 = 0.2, df = 1, p = 0.85), indicating that persons with bipolar disorder do not experience a differential risk of nursing home entrance in middle age compared with older age.
Recognizing the limits of the small sample of persons with bipolar disorder, these results suggest that the substantially greater rate of nursing home entrance in middle age is associated with schizophrenia as a specific diagnosis rather than a general phenomenon associated with a broad group of mental disorders.
DISCUSSION
These results indicate that within this sample of New Hampshire Medicaid beneficiaries, persons with schizophrenia spectrum disorders face greater risk of nursing home admittance relative to persons with no mental illness, particularly during their middle years, although the absolute risk is highest at older ages. This increased risk persists even when controlling for age, gender, medical severity, and disability status. This risk at middle age may be specific to schizophrenia as an illness, because we found an overall higher rate of nursing home admission among persons with depression and bipolar disorder but no difference at middle age.
We are unable to determine from these administrative data whether this greater rate of institutionalization is warranted. From the perspective of physical functioning, the lower disability and comorbidity levels among persons with schizophrenia in our sample suggest perhaps not. Our measure of disability is limited because it includes permanent and total disability rather than a broader measure, but at least one national data sample reported nursing home residents with schizophrenia being less disabled than their peers with no mental illness as measured by activities of daily living.12
We also know little about the influence of consumer preferences on nursing home admission.2 Perhaps, a system of decision support targeted at younger persons with schizophrenia could be used to help plan for more appropriate residential choices as these individuals age. A previous study conducted by our research group found a striking mismatch between the preferred residential options of nursing home residents with serious mental illness and the preferences of their clinicians.23 Among these nursing home residents, clinicians considered that 51% could be appropriately moved to a community-based setting, whereas 40% of the residents felt that their needs would be more appropriately met in the community. However, agreement between the clinicians and residents on which persons could be moved from the nursing home was only 27.6%, or no better than chance. In addition, for persons they considered appropriate to live in a group setting, clini cians recommended a group home for 93.7%, whereas the 90.5% of consumers said they preferred an apartment or individual home.
Federally supported initiatives have been introduced to promote person-centered care and to find ways to prevent early and unwarranted institutionalization in a nursing home. Medicaid spending on home and community-based services waivers increased nationally from 15% in 1992 to 34% in 2003,24 and the Centers for Medicare and Medicaid Services have awarded grants to all 50 states to help communities integrate disability and long-term under the Real-Choice Systems Change Grants for Community Living.
Recent developments in integrated psychosocial skills training to promote community tenure and independent living for older adults with serious mental illness also have the potential to prevent excess institutionalization. These approaches, and other models specifically focusing on psychosocial skills training,25–30 hold promise for potentially decreasing the disproportionate nursing home placement of older persons with schizophrenia. Future models for the aging population of persons with serious mental illness will benefit from interventions aimed at promoting independence, community tenure, and opportunities that enhance quality of life.
Limitations
The results of this study should be interpreted with caution due to several limitations. Our study sample consists solely of New Hampshire residents who are Medicaid beneficiaries. New Hampshire is a predominantly rural and Caucasian state, which limits our ability to generalize these results to larger, urban, and more ethnically diverse areas. In addition, both Medicaid eligibility rules and long-term care systems vary from state to state, so New Hampshire’s configuration of institution and home-based care may not match service delivery systems in other states. Of particular interest would be to compare whether states with better residential alternatives or higher levels of community services allow more people with serious mental illness to remain in the community, because the absence of appropriate community services31 and residential alternatives2 may result in a bias toward nursing homes as the principal option. In addition, the use of Medicaid data and the lack of data from other payers (e.g., Medicare, private insurance) prevent us from estimating nursing home risk for the general population and limit our interpretation of these analyses to the accuracy of the claims.
Finally, the use of Medicaid claims precludes several measures that are likely to contribute to early institutionalization. Our two health status measures, physical disability and the CCI, were derived from Medicaid claims. More robust health indicators would be preferable, along with measures of mental illness severity or cognitive decline, a precursor to functional decline among older persons with schizophrenia.32,33 We also lack measures of social support and social network size, factors that affect institutionalization rates and community tenure.33–37 Perhaps, the lower perceived quality of life among persons with schizophrenia compared with their peers38 contributes to early institutionalization as well. Despite these limitations, a significant strength of this study is our ability to analyze these data over a 10-year period and to be able to document nursing home admissions among middle-aged persons with schizophrenia to peers with no mental illness.
CONCLUSION
In summary, this study contributes to the knowledge base addressing the question of early and potentially unwarranted institutionalization of persons with schizophrenia. These results indicate a need for researchers to investigate further the interrelation ships among health, function, and living situation among persons with schizophrenia, particularly during middle age.
Acknowledgments
This study was supported by NIMH training grant number NIMH T32 MH 073553 and 2K24 MH066282 (PI Bartels).
Footnotes
Presented at the American Association for Geriatric Psychiatry Annual Meeting, New Orleans, LA, March 1–4, 2007.
References
- 1.Shea DG, Russo PA, Smyer MA. Use of mental health services by persons with a mental illness in nursing facilities: initial impacts of OBRA87. J Aging Health. 2000;12:560–578. doi: 10.1177/089826430001200406. [DOI] [PubMed] [Google Scholar]
- 2.Bartels SJ, Van Citters AD. Community-based alternatives for older adults with serious mental illness: the Olmstead decision and deinstitutionalization of nursing homes. Ethics Law Aging Rev. 2005;11:3–22. [Google Scholar]
- 3.Mechanic D, McAlpine DD. Use of nursing homes in the care of persons with severe mental illness: 1985 to 1995. Psychiatr Serv. 2000;51:354–358. doi: 10.1176/appi.ps.51.3.354. [DOI] [PubMed] [Google Scholar]
- 4.Linkins KW, Lucca AM, Housman M, et al. Use of PASRR programs to assess serious mental illness and service access in nursing homes. Psychiatr Serv. 2006;57:325–332. doi: 10.1176/appi.ps.57.3.325. [DOI] [PubMed] [Google Scholar]
- 5.Browne G, Courtney M. Housing, social support and people with schizophrenia: a grounded theory study. Issues Ment Health Nurs. 2005;26:311–326. doi: 10.1080/01612840590915694. [DOI] [PubMed] [Google Scholar]
- 6.Browne G, Courtney M. Measuring the impact of housing on people with schizophrenia. Nursing Health Sci. 2004;6:37–44. doi: 10.1111/j.1442-2018.2003.00172.x. [DOI] [PubMed] [Google Scholar]
- 7.Gitlin LN. Conducting research on home environments: lessons learned and new directions. Gerontologist. 2003;43:628–637. doi: 10.1093/geront/43.5.628. [DOI] [PubMed] [Google Scholar]
- 8.Golant SM. Do impaired older persons with health care needs occupy U.S. assisted living facilities? An analysis of six national studies. J Gerontol B Psychol Sci Soc Sci. 2004;59:S68–S79. doi: 10.1093/geronb/59.2.s68. [DOI] [PubMed] [Google Scholar]
- 9.Bartels SJ, Clark RE, Peacock WJ, et al. Medicare and Medicaid costs for schizophrenia patients by age cohort compared with depression, dementia, and medically ill patients. Am J Geriatr Psychiatry. 2003;11:648–657. doi: 10.1176/appi.ajgp.11.6.648. [DOI] [PubMed] [Google Scholar]
- 10.Miller EA, Rosenheck RA. Risk of nursing home admission in association with mental illness nationally in the Department of Veterans Affairs. Med Care. 2006;44:343–351. doi: 10.1097/01.mlr.0000204008.83633.ed. [DOI] [PubMed] [Google Scholar]
- 11.Dobbs D, Hayes J, Chapin R, et al. The relationship between psychiatric disorders and the ability to age in place in assisted living. Am J Geriatr Psychiatry. 2006;14:613–620. doi: 10.1097/01.JGP.0000209268.37426.69. [DOI] [PubMed] [Google Scholar]
- 12.McAlpine D. Patterns of care for persons 65 years and older with schizophrenia. In: Cohen C, Arlington VA, editors. Schizophrenia Into Later Life. American Psychiatric Publishing; 2003. pp. 3–18. [Google Scholar]
- 13.Gupta S, Steinmeyer C, Frank B, et al. Older patients with schizo phrenia: nature of dwelling status and symptom severity. Am J Psychiatry. 2003;160:383–384. doi: 10.1176/appi.ajp.160.2.383. [DOI] [PubMed] [Google Scholar]
- 14.Brown S. Excess mortality of schizophrenia. A meta-analysis. Br J Psychiatry. 1997;171:502–508. doi: 10.1192/bjp.171.6.502. [DOI] [PubMed] [Google Scholar]
- 15.Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177:212–217. doi: 10.1192/bjp.177.3.212. [DOI] [PubMed] [Google Scholar]
- 16.Saha S, Chant D, McGrath J. A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry. 2007;64:1123–1131. doi: 10.1001/archpsyc.64.10.1123. [DOI] [PubMed] [Google Scholar]
- 17.Laursen TM, Munk-Olsen T, Nordentoft M, et al. A comparison of selected risk factors for unipolar depressive disorder, bipolar affective disorder, schizoaffective disorder, and schizophrenia from a danish population-based cohort. J Clin Psychiatry. 2007;68:1673–1681. doi: 10.4088/jcp.v68n1106. [DOI] [PubMed] [Google Scholar]
- 18.Grabowski DC. Medicaid reimbursement and the quality of nursing home care. J Health Econ. 2001;20:549–569. doi: 10.1016/s0167-6296(01)00083-2. [DOI] [PubMed] [Google Scholar]
- 19.Charlson M, Pompei P, Ales K, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 20.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 21.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. discussion 81–90. [DOI] [PubMed] [Google Scholar]
- 22.NH-US Department of Health and Human Services Department of Health and Human Services; New Hampshire: Eligibility for the Medicaid Program. 2008
- 23.Bartels SJ, Miles KM, Dums AR, et al. Are nursing homes appropriate for older adults with severe mental illness? Conflicting consumer and clinician views and implications for the olmstead decision. J Am Geriatr Soc. 2003;51:1571–1579. doi: 10.1046/j.1532-5415.2003.51508.x. [DOI] [PubMed] [Google Scholar]
- 24.Kaiser Family Foundation . Medicaid 1915(c) Home and Community-Based Service Programs: Data Update. Kaiser Family Foundation; Washington, DC: 2006. [Google Scholar]
- 25.Pratt SI, Van Citters AD, Bartels SJ, et al. Psychosocial rehabilitation in older adults with serious mental illness: a review of the research literature and suggestions for development of rehabilitative approaches. Am J Psychiatric Rehabil. 2008;11:7–40. [Google Scholar]
- 26.Granholm E, McQuaid JR, McClure FS, et al. A randomized controlled pilot study of cognitive behavioral social skills training for older patients with schizophrenia. Schizophr Res. 2002;53:167–169. doi: 10.1016/s0920-9964(00)00186-9. [DOI] [PubMed] [Google Scholar]
- 27.Granholm E, McQuaid JR, McClure FS, et al. A randomized, controlled trial of cognitive behavioral social skills training for middle-aged and older outpatients with chronic schizophrenia. Am J Psychiatry. 2005;162:520–529. doi: 10.1176/appi.ajp.162.3.520. [DOI] [PubMed] [Google Scholar]
- 28.McQuaid JR, Granholm E, McClure FS, et al. Development of an integrated cognitive-behavioral and social skills training intervention for older patients with schizophrenia. J Psychother Pract Res. 2000;9:149–156. [PMC free article] [PubMed] [Google Scholar]
- 29.Patterson TL, McKibbin C, Taylor M, et al. Functional Adaptation Skills Training (FAST): a pilot psychosocial intervention study in middle-aged and older patients with chronic psychotic disorders. Am J Geriatr Psychiatry. 2003;11:17–23. [PubMed] [Google Scholar]
- 30.Patterson TL, Bucardo J, McKibbin CL, et al. Development and pilot testing of a new psychosocial intervention for older Latinos with chronic psychosis. Schizophrenia Bull. 2005;31:922–930. doi: 10.1093/schbul/sbi036. [DOI] [PubMed] [Google Scholar]
- 31.Borson S, Bartels SJ, Colenda CC, et al. Geriatric mental health services research: strategic plan for an aging population. Report of the health services work group of the American Association for Geriatric Psychiatry. Am J Geriatr Psychiatry. 2001;9:191–204. [PubMed] [Google Scholar]
- 32.Harvey PD, Bertisch H, Friedman JI, et al. The course of functional decline in geriatric patients with schizophrenia: cognitive functional and clinical symptoms as determinants of change. Am J Geriatr Psychiatry. 2003;11:610–619. doi: 10.1176/appi.ajgp.11.6.610. [DOI] [PubMed] [Google Scholar]
- 33.Bartels SJ, Mueser KT, Miles KM. A comparative study of elderly patients with schizophrenia and bipolar disorder in nursing homes and the community. Schizophr Res. 1997;27:181–190. doi: 10.1016/S0920-9964(97)00080-7. [DOI] [PubMed] [Google Scholar]
- 34.Cohen CI, Sokolovsky J. Schizophrenia and social netowrks: expatients in the inner city. Schizophr Bull. 1978;4:546–559. doi: 10.1093/schbul/4.4.546. [DOI] [PubMed] [Google Scholar]
- 35.Meeks S, Carstensen LL, Stafford PB, et al. Mental health needs of the chronically mentally ill elderly. Psychol Aging. 1990;5:163–171. doi: 10.1037//0882-7974.5.2.163. [DOI] [PubMed] [Google Scholar]
- 36.Albert M, Becker T, McCrone P, et al. Social networks and mental health service utilisation–a literature review. Int J Soc Psychiatry. 1998;44:248–266. doi: 10.1177/002076409804400402. [DOI] [PubMed] [Google Scholar]
- 37.Nihtila E, Martikainen P. Why older people living with a spouse are less likely to be institutionalized: the role of socioeconomic factors and health characteristics. Scand J Public Health. 2008;36:35–43. doi: 10.1177/1403494807086421. [DOI] [PubMed] [Google Scholar]
- 38.Bankole AO, Cohen CI, Vahia I, et al. Factors affecting quality of life in a multiracial sample of older persons with schizophrenia. Am J Geriatr Psychiatry. 2007;15:1015–1023. doi: 10.1097/JGP.0b013e31805d8572. [DOI] [PubMed] [Google Scholar]