Abstract
Aims/hypothesis
Gastrin has been implicated in islet growth/neogenesis, and proton pump inhibitors (PPIs) have been shown to increase endogenous gastrin levels in animals and humans. Therefore, we investigated the effect of PPIs in a model of type 2 diabetes, Psammomys obesus.
Methods
P. obesus (morning blood glucose [mBG] 16.9 ± 0.6 mmol/l) were treated with vehicle or different doses (1–15 mg/kg) of lansoprazole for 17 days.
Results
Treatment with lansoprazole resulted in up to ninefold dose-dependent increases in endogenous gastrin levels (p < 0.05 for 10 mg/kg lansoprazole vs vehicle). There was a significant reduction in mBG levels in all animals in the high-dose lansoprazole groups during the 17 day treatment period, whereas there was no significant improvement in mBG in animals in the vehicle groups. The mBG at end of study was 18.2 ± 2.1, 8.7 ± 2.2 (p < 0.01), and 6.1 ± 2.3 (p < 0.001) mmol/l for vehicle and lansoprazole 10 and 15 mg/kg, respectively. The animals treated with 15 mg/kg lansoprazole, compared with vehicle, had a 2.3-fold increase in the intensity of insulin staining in beta cells (p=0.0002) and 50% higher beta cell mass (p=0.04).
Conclusions/interpretations
The PPI lansoprazole had significant glucose-lowering effects in an animal model of type 2 diabetes, an effect that is most likely mediated through an increase in endogenous gastrin levels.
Keywords: Animal model, Beta cell mass, Gastrin, Glycaemic control, Proton pump inhibitor, Type 2 diabetes
Introduction
The consistent finding of reduced functional pancreatic beta cell mass (BCM) not only in type 1 diabetes but also in type 2 diabetes has increased the focus on finding new treatments that may increase and/or cause regeneration of functional BCM. Gastrin has been shown to increase proliferation of human and rodent duct-like pancreatic cells in culture, and administration of gastrin stimulates beta cell neogenesis and expansion of the BCM in rodents [1, 2]. During treatment with proton pump inhibitors (PPIs), endogenous gastrin levels are increased in humans and rodents, and in a recent publication Suarez-Pinzon et al. showed that PPI treatment of mice in a model of type 1 diabetes resulted in an almost threefold increase in endogenous gastrin levels and improvement in glycaemia [3].
Since no data have been published on the effect of gastrin or PPIs in type 2 diabetes, we decided to investigate whether treatment with the PPI lansoprazole would have beneficial effects on glycaemic control in a type 2 diabetes animal model, the gerbil Psammomys obesus. When this gerbil is fed a high-energy diet, morning blood glucose (mBG) levels are distinctly increased, with subsequent/concomitant loss of beta cell function and mass [4].
Methods
Animals
Male and female P. obesus (Harlan, Jerusalem, Israel) were fed low-energy (10 kJ/g) chow until the age of 14–15 weeks, after which they were transferred to an ad libitum high-energy (13 kJ/g) diet during which body weight (BW), mBG and HbA1c were monitored for 4 weeks. The animals that showed increased mBG levels, defined as mBG >10 mmol/l on two consecutive readings, were used in the treatment study.
P. obesus were treated with vehicle (n = 5) or 1 mg/kg (n = 8), 3 mg/kg (n = 11) or 10 mg/kg (n = 7) lansoprazole in the first study. At the start of the experiment there were 10–12 animals in each group, except for the 10 mg/kg group, which was smaller due to lack of compound. During the study, five animals in the vehicle group and two in the 1 mg/kg group had to be killed due to severely elevated mBG and ketoacidosis. Two animals, one from the 3 mg/kg group and one from the 10 mg/kg group, died due to dosing into the lungs. They were removed from all the analyses. The second study consisted of animals dosed with vehicle (n = 8) or 10 mg/kg (n = 8) or 15 mg/kg (n = 8) lansoprazole. Both studies were conducted over 2.5 weeks, during which mBG, BW and HbA1c were monitored, and gastrin levels were measured at the end of the study. Pancreases from the groups receiving 10 and 15 mg/kg were evaluated histologically for insulin content and BCM.
The study was approved by the Animal Experiments Inspectorate, Ministry of Justice, Denmark.
Formulation of lansoprazole
Lansoprazole (L8533; Sigma-Aldrich, Broendby, Denmark) was suspended in vehicle (0.6% carboxymethylcellulose, 0.2% NaHCO3) to the final dose volume of 2 ml/kg.
mBG and HbA1c
Blood samples were collected from the tail, and mBG and HbA1c measured as previously described [5].
Endogenous gastrin
Gastrin levels were measured in samples collected from the aorta using a competition scintillation proximity assay (SPA). Briefly, SPA beads, coated with anti-rabbit antibody, were incubated with rabbit anti-gastrin antibody and 125I-labelled Tyr12-gastrin (human). Sample, standard or control was added to the plates, followed by 10 μl of antibody rabbit-anti-gastrin serum (#2609 11/10-73; gift from J. Rehfeld, University Hospital, Copenhagen, Denmark) diluted in assay buffer, 10 μl tracer ([125I-Tyr12]-gastrin I [human]), 0.37 MBq/ml NEX176 (Amersham, Cardiff, UK) and 10 μl bead solution (Anti-Rabbit Coupled Polystyrene SPA RPQ0742; GE Healthcare, Umeå, Sweden). The plates were mixed and left for 6–24 h, after which they were centrifuged and counted (LEADseeker; GE Healthcare).
Pancreas histology
The pancreases were examined histologically, as previously described [5]. Briefly, pancreases were fixed in paraformaldehyde and sectioned according to the smooth fractionator principle with F = 1/4 of the fragments in each of the two capsules [6]. The sections were stained for insulin to visualise beta cells. BCM was evaluated stereologically in two to three sections with the observer blinded to the origin of the sections. The insulin staining intensity was graded semiquantitatively on a scale of 0–5, with 0 being equal to islets characterised by absence of insulin staining while 5 equals islets with insulin staining as seen in normal rat pancreas. The grading was carried out with the observer blinded to the origin of the sections.
Statistical analysis
Data were analysed using non-parametric (Kruskal–Wallis) ANOVA with Dunn’s multiple comparisons as post test or a non-parametric paired t test (Wilcoxon). p ≤ 0.05 was considered significant. Data are presented as mean ± SEM.
Results
Glycaemic control
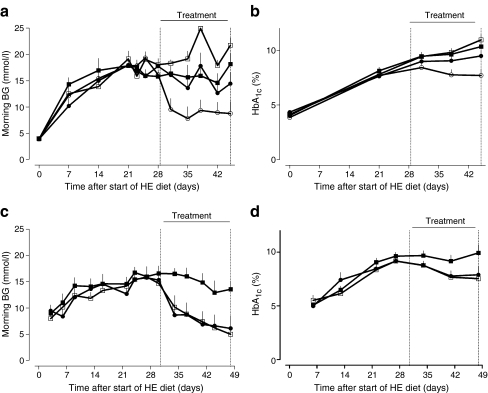
In the first experimental setup, 2.5 weeks of treatment had no significant effects on mBG in the vehicle and low-dose lansoprazole (1 and 3 mg/kg) groups. mBG at end of study was 18.2 ± 2.1, 21.7 ± 1.5 and 14.4 ± 2.2 mmol/l for vehicle (n = 5) and lansoprazole 1 mg/kg (n = 8) and 3 mg/kg (n = 11), respectively (Fig. 1a). The animals treated with the highest dose (10 mg/kg) had significantly lower mBG (8.7 ± 2.2 mmol/l, p < 0.01) at the end of the study. At start of treatment, there were no significant differences in mBG and HbA1c for the different treatment groups (Fig. 1a, b). At the end of the study period, HbA1c levels in the animals treated with the highest dose (10 mg/kg) of lansoprazole were significantly lower (7.7 ± 0.6%) than with vehicle (10.3 ± 0.5%, p < 0.05) or with 1 mg/kg (11.0 ± 0.5, p < 0.05) or 3 mg/kg lansoprazole (9.5 ± 0.5%, p < 0.05; Fig. 1b).
Fig. 1.
Morning blood glucose (BG) (a, c) and HbA1c (b, d) in Psammomys obesus before and during treatment with vehicle or different doses of lansoprazole. a, b Black squares, vehicle (n = 5); white squares, lansoprazole 1 mg/kg (n = 8); black circles, lansoprazole 3 mg/kg (n = 11); white circles, lansoprazole 10 mg/kg (n = 7). c, d Black squares, vehicle (n = 8); white squares, lansoprazole 10 mg/kg (n = 8); black circles, lansoprazole 15 mg/kg (n = 8). HE, high energy. Data are expressed as mean ± SEM
In a subsequent study, primarily focusing on pancreas histology and a higher dose of lansoprazole, similar results were obtained (Fig. 1c, d). There was no reduction in mBG in the vehicle-treated group (n = 8); mBG at end of study was 13.6 ± 1.5 mmol/l. In the lansoprazole 10 mg/kg group mBG was significantly reduced to 5.0 ± 1.4 (p < 0.001) and in the 15 mg/kg group to 6.1 ± 2.3 mmol/l (p < 0.001 compared with vehicle) (Fig. 1c). Likewise, HbA1c in the animals treated with 10 and 15 mg/kg of lansoprazole was significantly lower (6.9 ± 0.3% and 7.0 ± 0.3% respectively, p < 0.01) than in the vehicle-treated animals (10.4 ± 0.7%; Fig. 1d).
BW
During the study, no difference was observed in BW gain between the groups (data not shown).
Endogenous gastrin
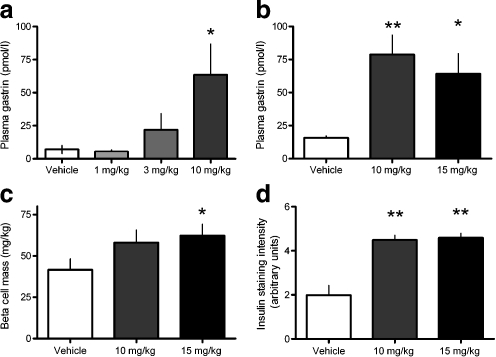
After 17 days of treatment with lansoprazole (1, 3 and 10 mg/kg), endogenous gastrin levels were dose-dependently increased by up to ninefold in the animals treated with 10 mg/kg (p < 0.05 vs vehicle, Fig. 2a); no further increase was seen in the 15 mg/kg group (Fig. 2b).
Fig. 2.
Plasma gastrin levels (a, b), beta cell mass (c) and intensity of insulin staining in pancreatic sections (d) from Psammomys obesus after 17 days of treatment with vehicle or different doses of lansoprazole. a White bar, vehicle (n = 5); very pale grey bar, lansoprazole 1 mg/kg (n = 8); pale grey bar, lansoprazole 3 mg/kg (n = 11); dark grey bar, lansoprazole 10 mg/kg (n = 7). b White bar, vehicle (n = 5); dark grey bar, lansoprazole 10 mg/kg (n = 7); black bar, lansoprazole 15 mg/kg (n = 8). c, d White bar, vehicle (n = 5); dark grey bar, lansoprazole 10 mg/kg (n = 7); black bar, lansoprazole 15 mg/kg (n = 8). Data are expressed as mean ± SEM. *p < 0.05 vs vehicle-treated animals; **p < 0.01 vs vehicle-treated animals
BCM and intensity of insulin staining
Stereological quantification of BCM revealed that the animals treated with 10 and 15 mg/kg lansoprazole had 40% (NS) and 50% (p = 0.04) higher BCM, respectively, compared with vehicle-treated animals (Fig. 2c).
Immunohistochemical analysis of the pancreas showed a 2.3-fold increase in the intensity of the insulin staining in the lansoprazole-treated animals compared with the vehicle-treated animals (p = 0.0002; Fig. 2d).
Discussion
Our results show that the PPI lansoprazole increases endogenous gastrin levels in P. obesus, glycaemic control is almost normalised and BCM and insulin content of the pancreas are increased. Several studies have shown that PPIs elevate gastrin levels in both rodents and humans, and in this study we show this also to be the case in P. obesus. It has been shown that treatment with gastrin alone can induce formation of new beta cells under different conditions [1, 2]; however, from the present study we cannot determine whether the increased beta cell mass is due to an increase in neogenesis and/or proliferation or a decrease in apoptosis. Further studies that directly address these mechanisms are warranted also in light of the possibility that rodents have a higher capacity for regeneration of BCM than humans.
Although we did not directly measure beta cell function, there was a significant reduction in mBG and HbA1c, which are both clinically relevant variables to measure for any agent that influences beta cell function or BCM.
Even though it is known that PPIs stimulate gastrin production, treatment with PPIs will result in very different pharmacokinetic profiles as compared with gastrin injections. Therefore, it could not be expected that PPIs would have the same effect on expansion of beta cell mass and function as has previously been demonstrated with gastrin. Whereas gastrin, in the doses used in the in vivo rodent studies, has a short half-life in rodents (less than 10 min; T. B. Bödvarsdóttir, L. Pridal, unpublished results), which results in a high exposure for a short time period, PPI treatment, in contrast, will result in a chronic elevation of gastrin levels to a few times above normal. A direct comparison of gastrin and PPIs is needed in order to clarify whether PPI treatment is superior to gastrin or vice versa. But, since PPIs are readily available as oral agents with a long-standing record of safety, the data presented here from lansoprazole-treated P. obesus warrant further studies of the clinical benefits of PPIs in type 2 diabetes.
In conclusion, the PPI lansoprazole has significant glucose-lowering effects in an animal model of type 2 diabetes, and thus PPIs might have the potential to become a new class of safe glucose-lowering agents, provided these findings can be extrapolated to other PPIs and humans.
Acknowledgements
We thank H. Jensen-Holm, M. Jorgensen, S. Primdahl, P. Rothe and A. Hansen, Novo Nordisk Diabetes & Obesity Pharmacology, Måløv, Denmark for expert technical assistance and J. Rehfeld, University Hospital, Copenhagen, Denmark for the kind provision of gastrin antibodies.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Abbreviations
- BCM
Beta cell mass
- BW
Body weight
- mBG
Morning blood glucose
- PPI
Proton pump inhibitor
- SPA
Scintillation proximity assay
References
- 1.Suarez-Pinzon WL, Lakey JRT, Brand SJ, Rabinovitch A. Combination therapy with epidermal growth factor and gastrin induces neogenesis of human islet β-cells from pancreatic duct cells and an increase in functional β-cell mass. J Clin Endocrinol Metab. 2005;90:3401–3409. doi: 10.1210/jc.2004-0761. [DOI] [PubMed] [Google Scholar]
- 2.Rooman I, Lardon J, Bouwens L. Gastrin stimulates β-cell neogenesis and increases islet mass from transdifferentiated but not from normal exocrine pancreas tissue. Diabetes. 2002;51:686–690. doi: 10.2337/diabetes.51.3.686. [DOI] [PubMed] [Google Scholar]
- 3.Suarez-Pinzon WL, Cembrowski GS, Rabinovitch A. Combination therapy with a dipeptidyl peptidase-4 inhibitor and a proton pump inhibitor restores normoglycaemia in non-obese diabetic mice. Diabetologia. 2009;52:1680–1682. doi: 10.1007/s00125-009-1390-z. [DOI] [PubMed] [Google Scholar]
- 4.Kaiser K, Yuli M, Üçkaya G, et al. Dynamic changes in ß-cell mass and pancreatic insulin during the evolution of nutrition-dependent diabetes in Psammomys obesus: impact of glycemic control. Diabetes. 2005;54:138–145. doi: 10.2337/diabetes.54.1.138. [DOI] [PubMed] [Google Scholar]
- 5.Vedtofte L, Bödvarsdóttir TB, Gotfredsen CF, Karlsen AE, Knudsen LB, Heller RS. Liraglutide, but not vildagliptin, restores normoglycaemia and insulin content in the animal model of type 2 diabetes, Psammomys obesus. Regul Pept. 2010;160:106–114. doi: 10.1016/j.regpep.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Gundersen HJG. The smooth fractionator. J Microsc. 2002;207:191–210. doi: 10.1046/j.1365-2818.2002.01054.x. [DOI] [PubMed] [Google Scholar]