Abstract
Background
Unhealthy diet and lack of physical activity increase rural midlife and older women’s risk for chronic diseases and premature death, and they are behind urban residents in meeting Healthy People 2010 objectives.
Objectives
To compare a tailored intervention based on the Health Promotion Model (HPM) and a generic intervention to increase physical activity and healthy eating among rural women.
Methods
In a randomized by site community-based controlled clinical trial, Wellness for Women, 225 women aged 50 to 69 years were recruited in two similar rural areas. Over 12 months, women received by mail either 18 generic newsletters or 18 newsletters computer-tailored on HPM behavior-specific cognitions (benefits, barriers, self-efficacy, and interpersonal support), activity, and eating. Outcomes at 6 and 12 months included behavioral markers and biomarkers of physical activity and eating. Data were analyzed by repeated measures ANOVA and χ2 tests (α < .05).
Results
Both groups significantly increased stretching and strengthening exercise and fruit and vegetable servings and decreased % calories from fat, while only the tailored group increased ≥ moderate intensity activity and decreased % calories from saturated fat from baseline to 6 months. Both groups increased stretching and strengthening exercise, while only the tailored group increased ≥ moderate activity and fruit and vegetable servings and decreased % calories from fat from baseline to 12 months. Both groups had several changes in biomarkers over the study. A higher proportion of women receiving tailored newsletters met Healthy People 2010 criteria for ≥ moderate activity, fruit and vegetable servings, and % calories from fat at 12 months.
Discussion
Mailed computer-tailored and generic print newsletters facilitated the adoption of change in both activity and eating over 6 months. Tailored newsletters were more efficacious in facilitating change over 12 months.
Keywords: middle-aged and aged women, rural population, exercise and eating, Health Promotion Model, randomized controlled trial
Lifestyle behaviors, particularly diet and physical activity, play a much greater role than genetics in determining how well one ages (Ory, Kinney Hoffman, Hawkins, Sanner, & Mockenhaupt, 2003). Unhealthy diet and lack of physical activity increase risk for many chronic diseases and account for more than 300,000 premature deaths annually in the United States (Mokdad, Marks, Stroup, & Gerberding, 2005).
Midlife and older rural women are high-priority targets for lifestyle behavior change. Women have a greater incidence of chronic illness, functional limitations, and disability than men as they age (Murtagh & Hubert, 2004). Rural populations have a greater incidence of chronic disease (National Center for Health Statistics, 2002) and less access to health care services (Gamm, Hutchinson, Linnae, Dabney, & Dorsey, 2003). They are less likely to obtain preventive health services and are behind urban residents in meeting Healthy People (HP) 2010 objectives (Casey, Thiede Call, & Klingner, 2001). Midlife and older rural women have higher rates of sedentary behavior (Wilcox, Castro, King, Housemann, & Brownson, 2000) and consumption of high fat diets (Gamm et al., 2003) than urban women. The HP 2010 objectives (United States Department of Health and Human Services [USDHHS], 2000) reflect consensus that midlife and older women should reduce consumption of dietary fat; increase consumption of fruits, vegetables, and grain products; and engage regularly in moderate intensity physical activity and activity to enhance muscular strength, endurance, and flexibility. Little or no progress toward these objectives has been achieved in the first half of this decade (HP 2010 Midcourse Review, 2006).
The National Institutes of Health drew attention to the need for research on multiple-behavior change interventions in 1999 (Nigg, Allegrante, & Ory, 2002). Interventions based on a single theoretical framework that addressed two or more health behaviors were expected to have greater impact on public health than attempts to change a single behavior. No intervention trials targeting comprehensive change in both physical activity and healthy eating for rural midlife and older women have been reported. Development and evaluation of distance delivery approaches to lifestyle behavior change for underserved and often isolated rural women are needed.
Mailed computer-tailored newsletters provide one such approach. Tailoring is an approach to facilitating lifestyle behavior change that has been used extensively in face-to-face interactions when health professionals interview clients and develop an individualized plan. Computers have allowed for personalized feedback and advice to population groups by generating messages based on participant responses to questionnaires (Skinner, Siegfried, Kegler, & Strecher, 1993).
The purpose of this clinical trial was to compare the efficacy of a tailored intervention framed within the Health Promotion Model (Pender, Murdaugh, & Parsons, 2002) and a generic (nontailored) intervention in facilitating change in physical activity and healthy eating among rural women aged 50 to 69 years. Primary outcomes were change from baseline to 6 and 12 months in: (a) eating behavioral markers (fruit and vegetable servings, whole grain servings, and % calories from fat and saturated fat); (b) activity behavioral markers (minutes of moderate+ activity, Kcal expended, and minutes of stretching and strength exercise) and biomarkers (estimated VO2max, flexibility and lower body strength); and (c) biomarkers influenced by eating and activity (systolic and diastolic blood pressure, % body fat, body mass index, and serum lipids). Secondary outcomes were achievement at 6 and 12 months of HP 2010 behavioral criterion standards: (a) engaging regularly in moderate or greater intensity physical activity for at least 30 minutes per day; and (b) meeting daily goals of at least 2 servings of fruits, 3 servings of vegetables, and 3 servings of whole grains; no more than 30% of calories from fat; and less than 10% of calories from saturated fat.
Literature Review
Tailoring has been defined as “any combination of information and behavior change strategies intended to reach one specific person, based on characteristics that are unique to that person, related to the outcome of interest, and derived from an individual assessment” (Kreuter, Farrell, Olevitch, & Brennan, 2000, p. 5). Noar, Benac, and Harris (2007) conducted the only metaanalytic review of 57 randomized controlled studies employing tailored print health behavior change interventions published through 2005. Eleven of the studies (19%) based messages on social cognitive theory. In 40 studies that compared tailored with nontailored messages, results favored the tailored message, though the sample size-weighted mean effect size was slightly less than small. Kroeze, Werkman, and Brug (2006) systematically reviewed 30 randomized controlled trials of computer-tailored interventions to change physical activity, nutrition, or both behaviors published from 1965 to 2004. In three of the 11 studies of physical activity and 20 of the 26 studies of nutrition behavior, significant effects of the tailored interventions were found when compared to generic interventions or to no intervention. The authors emphasized that, "although this review indicates that effects of tailored interventions are mostly small, when such small effects can be reached in the population at large, public health effects may be substantial." (p. 211).
Only five randomized controlled trials that compared print tailored with generic messages (the best test of tailoring) to address change in both eating and activity behaviors were found (Blalock et al., 2002; Demark-Wahnefried et al., 2007; Kreuter, Oswald, Bull, & Clark, 2000; Kreuter & Strecher, 1996; Smeets, Kremers, Brug, & deVries, 2007). None were targeted specifically to older female rural populations. Interventions included tailoring on eating and activity behaviors as well as on one or more behavioral influences consistent with the conceptual framework used. In three of the five studies, only a single tailored communication was delivered to participants. Behavior change outcomes, almost exclusively behavioral markers, were assessed over periods of 1 to 12 months. In only one study (Demark-Wahnefried et al., 2007) biomarkers were measured in a 25% subsample that was underpowered to detect significant group differences. Tailored print messages were more effective than generic print messages in fostering change in both behaviors in three studies and in eating alone in two studies.
Conceptual Framework
The Health Promotion Model (HPM), depicted in Pender et al. (2002), was used as the framework for the tailored intervention in this clinical trial. The HPM was selected because midlife and older women may be more interested in enhancing health to maintain independence than in avoiding specific diseases as they age. The theoretical underpinnings of the HPM are provided by social cognitive theory (Bandura, 1986). Four behavior-specific cognitions (perceived benefits, barriers, self-efficacy, and interpersonal influences), were selected from the HPM for use in designing the tailored intervention. These cognitions, considered modifiable through intervention, are those for which there is empirical evidence supporting predictive validity as behavioral determinants. Research supporting their association with physical activity and healthy eating has been reviewed by Walker, Pullen, Hertzog, Boeckner, and Hageman (2006). Within this framework, the intervention targeted change not only in health behaviors, but also in known influences on those behaviors.
Methods
The Wellness for Women study was a community-based clinical trial using a repeated measures experimental comparison group design with randomization of two geographical areas to intervention (computer-tailored newsletters) or comparison (generic newsletters) groups. The intervention lasted for 12 months and follow-up extended an additional 12 months. Results during the intervention period are reported here. Institutional Review Board approval was obtained prior to sample recruitment and each participant provided written informed consent at the time of the first assessment appointment.
Sample
Power analyses for RM-ANOVA for the primary outcomes--based on changes resulting from diet, physical activity, or both interventions reported in the literature--indicated that the study had .80 or higher power to detect somewhat smaller than medium differences in the amount of change between the groups (effect size, partial eta-squared of approximately .04). Power was estimated to be less than .80 for chi square analyses for the secondary outcomes, but they were conducted for their descriptive value.
University survey center personnel used random digit dialing to recruit 225 participants from two rural areas in a Midwestern state with similar demographic profiles. Women were screened for inclusion criteria: age 50–69 years; English-speaking; able to use a computer with assistance to complete a survey; access to a video recorder to view physical activity demonstration tapes; able to answer no to all questions on the Physical Activity Readiness Questionnaire (PAR-Q; American College of Sports Medicine [ACSM], 2006) or obtain physician clearance; and not undergoing cardiac or physical rehabilitation. To ensure that all participants would have the potential for change in both activity and eating, exclusion criteria were: being in the maintenance stage for all 3 components of readiness for change in physical activity (aerobic, stretching, and muscle strengthening exercise) or all 3 components of readiness for change in healthy eating (consumption of fruits and vegetables, grain products, and fat); restrictions that would preclude them from following the HP 2010 recommendations for both moderate physical activity and healthy eating; unable to walk without an assistive device (including canes, crutches, walkers, and oxygen); and unable to walk 1 mile continuously without resting. Enrollment extended from 2002 to 2003.
Assessments and Measurement Methods
Behavioral markers and biomarkers of activity and eating to measure primary and secondary outcomes were assessed at baseline, 6 months, and 12 months. Assessments of HPM behavioral determinants for tailoring purposes were completed at baseline and 3, 6, and 9 months. All assessments were conducted at two rural research offices and data were transmitted to investigators via the university’s restricted access Intranet. A research nurse at each site assessed biomarkers and supervised women individually in completing self-report questionnaires on the computer. Blood samples drawn to measure lipids were frozen and shipped on dry ice to the university hospital laboratory for analysis. Established valid and reliable measures were used for all assessments. Reliability and validity of the measures have been described previously by Walker et al. (2006) and in cited sources below.
Primary and Secondary Outcome Measures
Physical activity
Time engaged daily in moderate or greater intensity activity and associated energy expenditure were measured by the Modified 7-Day Activity Recall (Hellman, Williams, & Thalken, 1996/1997). Achievement of HP 2010 behavioral criterion standards were calculated from these data. Time engaged weekly in strengthening and stretching exercises was measured using 2 items in a format similar to that of the 7-Day Recall. Cardiorespiratory fitness was measured using the 1-mile walk test, which provides an estimate of VO2max from variables of weight, age, gender, track walk time (minutes), and 15-second final heart rate; participants were asked to walk as fast as they comfortably could for 1 mile on an indoor walk route that was the same for all women at that site (Hageman, Walker, Pullen, & Pellerito, 2001). Flexibility was measured by the modified sit-and-reach test, recommended by the American College of Sports Medicine (ACSM, 2006) as a measurement of general flexibility. Lower body muscular strength was measured by repeated timed chair stands, which required participants to complete 10 full stands from a sitting position as quickly as possible while being timed to the nearest second (Hageman et al., 2001).
Healthy eating
Self-reported daily servings of fruits, vegetables, and whole grain products and daily intake of dietary fat (% calories from total fat and saturated fat) were measured by the web-based version of the 1998 Block Health Habits and History Questionnaire (HHHQ), measuring the usual self-selected diets of individuals over a period of time (Boeckner, Pullen, Walker, Abbott, & Block, 2002). The timeframe used for this study was the past year at baseline and since the last assessment at subsequent points. Achievement of HP 2010 behavioral criterion standards were calculated from these data.
Biomarkers affected by activity and eating
Systolic and diastolic blood pressure were measured prior to physical activity testing, using a calibrated mercury sphygmomanometer and following standardized auscultatory methods (ACSM, 2006). Percent body fat was measured by bioelectrical impedance analysis (BIA) following the manufacturer’s instructions (Biodynamics Model 310e Body Composition Analyzer, Biodynamics Corporation, Seattle, WA; National Institutes of Health Consensus Statement, 1996). Serum lipids were measured by biochemical analyses of total cholesterol, high-density lipoprotein (HDL-C), low-density lipoprotein (LDL-C), and triglycerides following a 12-hour fast.
Measurement of Behavioral Determinants for Tailoring
Selected individual items from measures of the HPM behavioral determinants were used as the basis for tailored messages. These measures included: Exercise Benefits/Barriers Scales (EBBS); Healthy Eating Benefits/Barriers Scales, modeled after the EBBS by the investigators; Self-Efficacy for Exercise Habits Scale; Self-Efficacy for Eating Habits Scale, modified with the instrument author’s permission; Family Support for Exercise Habits Scale and Friend Support for Exercise Habits Scale; and Family Support for Healthy Eating Habits Scale and Friend Support for Healthy Eating Habits Scale. Detailed descriptive and psychometric information on all scales can be found in Walker et al. (2006).
Intervention
The major intervention components were tailored or generic newsletters that were mailed to the women; these were supplemented by plans of action in the tailored group and by physical activity instructional videotapes and feedback on assessment results provided to all participants.
Newsletters
Both groups received a total of 18 newsletters (tailored versus generic). During the first 6 months, newsletters were sent every 2 weeks. During the second 6 months, newsletters were sent every 4 weeks. The overall theme for each newsletter sent to women in both groups was the same, and content was targeted to midlife and older women. Both sets of newsletters were formatted with similar layout, typeface, and length to control for differences in appearance.
Each of the 18 newsletters for both groups included advice about desired behavioral changes in physical activity and healthy eating; selected newsletters also included information about HPM determinants (benefits of healthy eating and activity, overcoming barriers to behavior change, building confidence in ability to follow eating and activity guidelines, and obtaining support from family and peers). Tailored newsletters included only content relevant to the individual recipient as indicated by assessment responses, while generic newsletters included a wider range of general content on the same topics. A library of hundreds of text messages for tailoring was created to correspond to individual women’s assessment data, including activity and eating goals, self-reports, and biomarkers; and perceived most important benefits, greatest barriers, self-efficacy, and support from family and peers. Each possible response on measures of the HPM behavioral determinants was matched by computer with a unique message from the text message library to be delivered to women who selected that response.
The data management system for generation of the tailored newsletters was developed and implemented by the project’s information technologist. Data were collected from study participants using an online assessment instrument developed with Macromedia ColdFusion maintaining a dynamic interface with a Microsoft Access database residing on a secure server at the University Medical Center. Tailored newsletters were generated from this database using a ColdFusion interface, which placed them in an Acrobat window where they were printed.
Commitment to a plan of action
While the generic group received newsletter messages to set goals for behavior change, only the tailored group committed to a plan to accomplish self-identified behavior-specific goals in each 3-month period. A computerized Plan of Action form listed possible goals for change in physical activity and healthy eating behaviors from which participants could choose. Each woman in the tailored group was asked to choose and designate frequency for one or two physical activities and to choose one healthy eating behavior in each of three categories of fruits and vegetables, fat intake, and grain intake. At each assessment period, women in the tailored group affirmed their commitment to behavior change by selecting goals on the computer.
Videotapes
A videotape and companion manual, Exercise: A Video from the National Institute on Aging, was distributed to both groups at baseline. The videotape demonstrated moderate-intensity physical activities shown to increase cardiorespiratory fitness in older adults.
A second videotape, Banding Together for Strength©, was developed for the project and distributed to both groups at the 3-month assessment. It illustrated specific methods for safe stretching and muscle strengthening with Theraband® (The Hygenic Corporation, Akron, OH) resistive bands. Each woman was given two lengths of banding with resistance based on her upper and lower body strength measurements at baseline so that she could do the muscle strengthening exercises shown on the videotape. Bands could be replaced every 3 months as her strength increased or between assessments when she was able to do 15 repetitions comfortably and requested that a higher resistance band be sent to her.
Feedback on assessment results
A descriptive report that included each woman’s periodic assessment results and an indication of desirable ranges was sent to each participant in both groups within 1 month of their baseline, 3-month, 6-month, and 9-month assessments. No advice concerning needed behavior change was included with those mailings, but the women in the tailored newsletter group were given advice in subsequent newsletters.
Motivational devices
Pedometers were given to all participants at baseline, with encouragement to record their steps and instructions to work toward a goal of 10,000 steps daily. Food pyramid magnets with recommended servings of foods from each food group were distributed as a reminder of the guidelines for healthy eating to be placed on their refrigerator.
Analysis of Data
Intervention and comparison groups were compared on sociodemographic and health-related characteristics to evaluate their baseline comparability. Analyses of change in behavioral and biomarkers of physical activity and healthy eating were based on intention to treat. Square root and logarithmic transformations were used to normalize the positively skewed distributions of several variables by reducing the effects of a small number of outliers (Tables 2 and 3). Only three variables were missing more than 6% of observations at any one time: chair stands and sit-and-reach, with 0–11% missing across the three times; and VO2max, with 4–18% missing. Ninety-four percent of cases had complete data or were missing fewer than 5% of their observations. The remaining cases tended to be missing all data for one or more collection times. Maximum likelihood estimates of missing data values at the 6-month and 12-month assessments for all variables except cardiorespiratory fitness (VO2max) were imputed via the expectation maximization (EM) algorithm (Dempster, Laird, & Rubin, 1977) as implemented in SPSS Missing Values Analysis 12.0. Missing values on VO2max were not imputed because they could not be considered missing at random, as they were due to the inability of some participants to perform the task.
Table 2.
2 x 3 Repeated Measures Analysis of Variance F Ratios for Newsletter Group x Time (Imputed Data N = 225)
| Time (T) | T x G | Effect Sizec (Partial η2) | |||
|---|---|---|---|---|---|
| Outcomes | df | F (p) | F (p) | T | T x G |
| Eating Markers | |||||
| Fruit + Veg Servings a | 2, 222 | 13.97 (< .001)* | 4.07 (.018)* | .11 | .04 |
| Whole Grain Servings a | 2, 222 | 2.75 (.066) | 0.18 (.837) | .02 | .00 |
| % Calories from Fat | 2, 222 | 9.85 (< .001)* | 1.34 (.265) | .08 | .01 |
| % Calories from Saturated Fat | 2, 222 | 6.45 (.002)* | 3.48 (.033)* | .06 | .03 |
| Activity Markers | |||||
| Moderate+ Activity (min/day) a | 2, 222 | 18.08 (< .001)* | 1.92 (.150) | .14 | .02 |
| Kcal Expended/kg/day b | 2, 222 | 12.24 (< .001)* | 2.51 (.084) | .10 | .02 |
| VO2max (ml/kg/min) | 2, 170 | 34.71 (< .001)* | 0.40 (.670) | .29 | .01 |
| Stretching Exercise (min/wk) a | 2, 222 | 42.33 (< .001)* | 2.18 (.116) | .28 | .02 |
| Strength Exercise (min/wk) a | 2, 222 | 40.63 (< .001)* | 1.86 (.159) | .27 | .02 |
| Sit-and-Reach (cm) | 2, 222 | 27.76 (< .001)* | 1.47 (.233) | .20 | .01 |
| Timed Chairstands (sec) | 2, 222 | 69.59 (< .001)* | 9.01 (<.001)* | .39 | .08 |
| Outcomes Influenced by Activity and Eating | |||||
| Systolic Blood pressure | 2, 222 | 6.39 (.002)* | 5.41 (.005)* | .05 | .05 |
| Diastolic Blood Pressure | 2, 222 | 11.37 (< .001)* | 3.85 (.023)* | .09 | .03 |
| % Body Fat (BIA) | 2, 222 | 0.17 (.844) | 4.62 (.011)* | .00 | .04 |
| Body Mass Index | 2, 222 | 6.98 (.001)* | 0.08 (.920) | .06 | .00 |
| Total Cholesterol | 2, 222 | 0.38 (.682) | 0.48 (.622) | .00 | .00 |
| Triglycerides | 2, 222 | 0.85 (.431) | 0.67 (.520) | .01 | .01 |
| HDL Cholesterol | 2, 222 | 0.81 (.447) | 0.30 (.739) | .01 | .00 |
| LDL Cholesterol | 2, 222 | 36.32 (< .001)* | 1.41 (.248) | .25 | .01 |
Notes. F-ratios are Wilk’s approximation of F-values
Square root transformed
Log10 transformed
Effect size: .01 = small, .06 = medium, .14 = large
Significant change p < .05
Table 3.
Change in Activity and Eating Outcomes Imputed Data (n = 225)
| Baseline | 6 months | Change Base to 6 Months |
12 months | Change Base to 12 Months |
|||
|---|---|---|---|---|---|---|---|
| Marker | Mean (SD) | Mean (SD) | Mean (95% CIa) | pa | Mean (SD) | Mean (95% CIa) | pa |
| Physical Activity | |||||||
| Outcomes | |||||||
| Moderate+ Activity (min/day) b | |||||||
| Tailored (n = 115) | 337.65 (675.4) | 575.02 (759.3) | 237.37 (411.16 to 63.57) | < .001* | 509.88 (749.4) | 172.23 (337.93 to 6.53) | < .001* |
| Generic (n = 110) | 238.50 (472.5) | 450.90 (600.7) | 212.40 (390.10 to 34.69) | < .001* | 280.09 (360.1) | 41.59 (211.02 to − 127.83) | .211 |
| Kcal Expended/kg/day c | |||||||
| Tailored (n = 115) | 31.77 (12.7) | 34.56 (10.6) | 2.79 (5.38 to 0.21) | .002* | 33.55 (10.5) | 1.78 (4.51 to −0.95) | .029 |
| Generic (n = 110) | 29.66 (7.9) | 32.51 (9.8) | 2.85 (5.49 to 0.21) | .008* | 28.88 (5.6) | −0.78 (2.02 to − 3.57) | .380 |
| VO2max (ml/kg/min) | |||||||
| Tailored (n = 89) | 21.59 (7.5) | 23.59 (7.0) | 1.99 (2.86 to 1.13) | < .001* | 23.22 (7.5) | 1.62 (2.53 to 0.72) | < .001* |
| Generic (n = 84) | 21.28 (6.9) | 23.53 (6.3) | 2.25 (3.14 to 1.36) | < .001* | 23.37 (6.2) | 2.09 (3.02 to 1.16) | < .001* |
| Stretching Exercise (min/wk) b | |||||||
| Tailored (n = 115) | 14.22 (26.2) | 34.78 (39.7) | 20.56 (30.94 to 10.19) | < .001* | 27.00 (39.6) | 12.78 (24.34 to 1.23) | < .001* |
| Generic (n = 110) | 17.41 (44.3) | 32.89 (45.3) | 15.48 (26.09 to 4.87) | < .001* | 36.36 (50.1) | 18.95 (30.77 to 7.14) | < .001* |
| Strength Exercise (min/wk) b | |||||||
| Tailored (n = 115) | 8.52 (22.3) | 39.19 (49.9) | 30.67 (43.83 to 17.52) | < .001* | 26.95 (49.6) | 18.43 (32.18 to 4.67) | < .001* |
| Generic (n = 110) | 12.95 (38.0) | 35.23 (58.5) | 22.28 (35.73 to 8.83) | < .001* | 32.83 (62.8) | 19.87 (33.94 to 5.81) | < .001* |
| Sit-and-Reach (cm) | |||||||
| Tailored (n = 115) | 28.16 (7.9) | 30.35 (6.9) | 2.19 (3.46 to 0.92) | < .001* | 29.99 (6.3) | 1.83 (3.20 to 0.46) | .002* |
| Generic (n = 110) | 26.68 (7.6) | 30.05 (7.3) | 3.37 (4.67 to 2.07) | < .001* | 29.82 (6.6) | 3.14 (4.55 to 1.74) | < .001* |
| Timed Chairstands (sec) | |||||||
| Tailored (n = 115) | 18.05 (4.8) | 14.63 (3.9) | −3.42 (−2.62 to −4.21) | < .001* | 14.14 (4.0) | −3.91 (−3.03 to − 4.80) | < .001* |
| Generic (n = 110) | 17.76 (4.9) | 16.15 (4.6) | −1.61 (−0.80 to −2.43) | < .001* | 15.92 (4.6) | −1.84 (−0.93 to − 2.75) | < .001* |
| Healthy Eating Outcomes | |||||||
| Fruit + Veg Servings b | |||||||
| Tailored (n = 115) | 5.67 (3.0) | 6.82 (3.3) | 1.15 (1.80 to 0.49) | < .001* | 6.59 (3.3) | 0.92 (1.60 to 0.24) | .001* |
| Generic (n = 110) | 5.44 (2.5) | 6.17 (2.7) | 0.74 (1.41 to 0.06) | .004* | 5.34 (2.7) | 0.10 (−0.60 to 0.80) | .607 |
| Whole Grain Servings b | |||||||
| Tailored (n = 115) | 1.34 (1.5) | 1.33 (1.2) | 0.0 (0.31 to −0.32) | .676 | 1.19 (1.1) | −0.15 (0.13 to −0.42) | .447 |
| Generic (n = 110) | 1.08 (1.0) | 1.06 (0.9) | 0.0 (0.30 to −0.33) | .915 | 0.95 (0.9) | −0.13 (0.15 to −0.41) | .115 |
| % Calories from Fat | |||||||
| Tailored (n = 115) | 38.11 (6.7) | 35.99 (6.4) | −2.13 (−0.54 to −3.71) | .001* | 36.60 (6.9) | −1.52 (0.11 to −3.14) | .026 |
| Generic (n = 110) | 39.99 (6.8) | 38.17 (7.3) | −1.82 (−0.20 to −3.44) | .007* | 39.84 (6.9) | −0.15 (1.51 to −1.81) | .826 |
| % Calories from Saturated Fat | |||||||
| Tailored (n = 115) | 11.28 (2.7) | 10.47 (2.4) | −0.81 (−0.24 to −1.37) | .001* | 10.52 (2.5) | −0.76 (−0.18 to − 1.33) | .002* |
| Generic (n = 110) | 11.63 (2.3) | 11.27 (2.9) | −0.37 (0.21 to −0.94) | .124 | 11.76 (2.6) | 0.12 (0.71 to −0.47) | .617 |
| Biomarkers Affected by Eating and Activity | |||||||
| Systolic Blood Pressure | |||||||
| Tailored (n = 115) | 128.29 (12.5) | 124.16 (11.7) | −4.12 (−1.49 to −6.76) | < .001* | 124.36 (10.7) | −3.92 (−1.03 to − 6.82) | .001* |
| Generic (n = 110) | 126.15 (15.1) | 126.83 (15.1) | 0.68 (3.37 to −2.01) | . 541 | 123.93 (14.7) | −2.22 (0.74 to −5.17) | .072 |
| Diastolic Blood Pressure | |||||||
| Tailored (n =115) | 80.36 (7.3) | 77.96 (7.7) | −2.40 (−0.69 to −4.09) | .001* | 77.19 (7.2) | −3.16 (−1.38 to −4.95) | < .001* |
| Generic (n = 110) | 78.16 (8.5) | 78.54 (7.8) | 0.38 (2.12 to −1.35) | .596 | 76.32 (7.1) | −1.84 (−0.01 to −3.67) | .016* |
| % Body Fat (BIA) | |||||||
| Tailored (n =115) | 35.98 (6.3) | 35.48 (6.0) | −0.50 (0.04 to −1.05) | .026 | 35.43 (6.2) | −0.55 (0.09 to −1.19) | .040 |
| Generic (n = 110) | 35.99 (5.7) | 36.34 (5.4) | 0.35 (0.90 to −0.21) | . 133 | 36.52 (5.6) | 0.53 (1.18 to 0.13) | .054 |
| Body Mass Index | |||||||
| Tailored (n =115) | 30.69 (6.8) | 30.34 (6.6) | −0.35 (0.01 to −0.71) | .021 | 30.54 (6.8) | −0.15 (0.38 to −0.68) | .499 |
| Generic (n = 110) | 29.68 (6.0) | 29.25 (5.9) | −0.43 (−0.06 to −0.80) | .006* | 29.41 (5.9) | −0.26 (0.28 to −0.80) | .239 |
| Total Cholesterol | |||||||
| Tailored (n =115) | 202.69 (34.4) | 202.42 (32.4) | 0.27 (−5.59 to 6.13) | .911 | 204.50 (33.5) | −1.82 (−8.73 to 5.11) | .528 |
| Generic (n = 110) | 205.73 (36.1) | 203.19 (32.0) | −2.54 (3.45 to −8.53) | .307 | 203.68 (37.3) | −2.05 (5.03 to −9.13) | .486 |
| Triglycerides | |||||||
| Tailored (n =115) | 125.53 (51.8) | 127.02 (57.0) | 1.49 (14.3 to −11.3) | .779 | 126.13 (61.0) | 0.60 (11.2 to −10.0) | .891 |
| Generic (n = 110) | 142.77 (72.8) | 147.39 (93.1) | 4.62 (17.7 to −8.5) | . 395 | 138.11 (65.7) | −4.66 (6.2 to −15.5) | .301 |
| HDL Cholesterol | |||||||
| Tailored (n =115) | 61.03 (15.0) | 62.16 (15.5) | 1.13 (3.2 to −1.0) | .196 | 61.96 (14.0) | 0.93 (3.4 to −1.5) | .358 |
| Generic (n = 110) | 60.81 (14.2) | 61.02 (15.3) | 0.21 (2.4 to −2.0) | .818 | 61.51 (14.7) | 0.70 (3.2 to −1.8) | .498 |
| LDL Cholesterol | |||||||
| Tailored (n =115) | 120.60 (32.6) | 111.62 (31.9) | −8.98(−3.0 to −15.0) | <.001* | 107.48 (31.5) | −13.12 (−6.2 to − 20.1) | < .001* |
| Generic (n = 110) | 125.10 (36.4) | 111.47 (34.8) | −13.6 (−7.5 to −19.8) | <.001* | 105.74 (38.2) | −19.36 (−12.3 to − 26.5) | < .001* |
Notes. CIs use Bonferroni adjustment for three comparisons; p values are unadjusted and are significant if < .017 (.05/3).
Raw values shown for interpretability; reported probabilities based on analyses of square root transformed values.
Raw values shown for interpretability; reported probabilities based on analyses of log transformed values.
Significant change p < .017
For each primary outcome, two analyses were done. A 2 (group) X 3 (time) repeated-measures analysis of variance (RM-ANOVA) was performed to compare differences over time in the tailored and generic newsletter groups. Main effects for time and time X newsletter group are reported from these analyses. A second analysis utilized an approach common in the health behavior literature, planned comparisons of simple main effects of time within group. Comparisons of changes from baseline to 6 and 12 months in each group are reported for these analyses. For the secondary outcomes, a series of chi-square (χ2) tests for 2 X 2 contingency tables were used to compare the proportion of women in each group achieving the specified HP 2010 physical activity and healthy eating behavioral criterion standards at 6 and 12 months. Alpha of .05 was used for all analyses except the planned comparisons, for which a Bonferroni-adjusted value of .017 was used to adjust for the three possible pairwise comparisons.
Analyses were performed using the SPSS statistical package (SPSS v. 11.5.0 for Windows, SPSS Inc., Chicago, IL). Block Dietary Data Systems (Berkeley, CA) conducted the analysis of the online HHHQ to obtain nutrient and food group values.
Results
Participant Characteristics and Flow
Sociodemographic and health-related characteristics of women in both groups are shown in Table 1. Groups differed only on white non-Hispanic versus minority ethnic or racial background (χ2 = 9.39, p =.002), educational level (χ2 = 9.38, p =.025), and on use of lipid-lowering medications (χ2 = 6.95, p =.008), which could affect lipid outcomes.
Table 1.
Baseline Characteristics of the Women by Intervention Group (N =225)
| Tailored Newsletter Group (n = 115) | Generic Newsletter Group (n = 110) | |||
|---|---|---|---|---|
| Characteristics | n | %a | n | %a |
| Age | ||||
| 50–54 | 39 | 33.9 | 37 | 33.6 |
| 55–59 | 35 | 30.4 | 30 | 27.3 |
| 60–64 | 29 | 25.2 | 26 | 23.6 |
| 65–69 | 12 | 10.4 | 17 | 15.5 |
| Mean (SD) | 57.83 (5.4) | 58.06 (5.7) | ||
| Ethnic or Racial Background | ||||
| White Non-Hispanic | 114 | 99.1 | 98 | 89.1 |
| Hispanic | 1 | 0.9 | 7 | 6.4 |
| American Indian or Alaska | 0 | 0.0 | 4 | 3.6 |
| Native | ||||
| Marital Status | ||||
| Married | 78 | 67.8 | 80 | 72.7 |
| Not currently married | 17 | 14.8 | 20 | 18.2 |
| Location of Residence | ||||
| Farm, ranch, in country | 35 | 30.4 | 33 | 30.0 |
| Town up to 9,999 | 32 | 27.8 | 32 | 29.1 |
| Town 10,000 – 49,999 | 46 | 40.0 | 44 | 40.0 |
| Education Level | ||||
| Some high school or less | 5 | 4.3 | 3 | 2.7 |
| High school graduate | 28 | 24.3 | 20 | 18.2 |
| Some college | 52 | 45.2 | 37 | 33.6 |
| College graduate or higher | 29 | 25.2 | 49 | 44.5 |
| Employment Status | ||||
| Employed full-time | 53 | 46.1 | 52 | 47.3 |
| Employed part-time | 22 | 19.1 | 19 | 17.3 |
| Not employed outside home | 39 | 33.9 | 38 | 34.5 |
| Annual Family Income | ||||
| <10 K | 2 | 1.7 | 2 | 1.8 |
| 10–19 K | 9 | 7.8 | 12 | 10.9 |
| 20–39 K | 42 | 36.5 | 29 | 26.4 |
| 40–59 K | 36 | 31.3 | 32 | 29.1 |
| 60 K or > | 21 | 18.3 | 32 | 9.1 |
| Perceived Health Status | ||||
| Excellent | 15 | 13.0 | 7 | 6.4 |
| Very good | 50 | 43.5 | 44 | 40.0 |
| Good | 42 | 36.5 | 54 | 49.1 |
| Fair or Poor | 6 | 5.2 | 5 | 4.5 |
| Weight Classification | ||||
| Normal (BMI < 25) | 21 | 18.3 | 25 | 22.7 |
| Overweight (BMI 25–29.9) | 45 | 39.1 | 40 | 36.4 |
| Obese (BMI ≥ 30) | 49 | 42.6 | 45 | 40.9 |
| Body Mass Index Mean (SD) | 30.69 (6.80) | 29.68 (5.98) | ||
| Lipid-Lowering Medication | ||||
| Yes | 28 | 24.3 | 12 | 10.9 |
| No | 87 | 75.7 | 98 | 89.1 |
| Hormone Replacement Therapy | ||||
| Yes | 46 | 40.0 | 57 | 51.8 |
| No | 69 | 60.0 | 53 | 48.2 |
Notes. Totals may not add to 100% because of missing data.
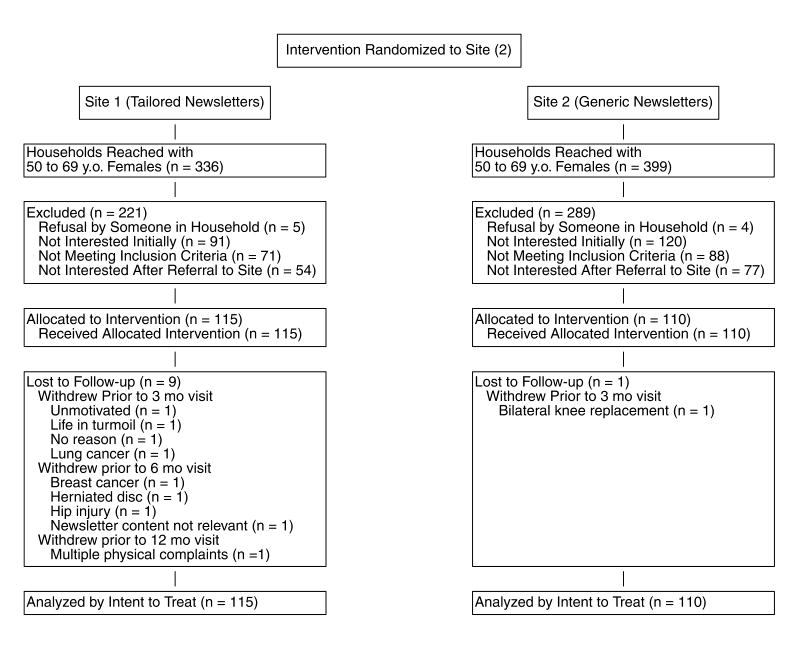
Participant flow during the trial is shown in Figure 1. Attrition remained low throughout the intervention period, with 9 of 115 women in the tailored group (7.8%) and 1 of 110 women in the generic group (1.0%) withdrawing for various reasons.
Figure 1.
Participant Flow Chart
Primary Outcomes
The RM-ANOVA results are shown in Table 2 and changes from baseline to 6 months and baseline to 12 months are shown in Table 3.
Physical activity
All behavioral and biomarkers of physical activity had significant main effects for time over the intervention period. Both groups improved significantly from baseline to 6 months on all measures. From baseline to 12 months, both groups improved on cardiorespiratory fitness, weekly stretching exercise, weekly strength exercise, flexibility, and lower body strength, while only the tailored newsletter group improved on daily moderate or greater intensity activity minutes. Nevertheless, the Time X Group interaction for daily moderate or greater intensity activity minutes was not significant. This may be due to the much larger standard deviation for the tailored group (749.4) as compared with the generic group (360.1) at 12 months. The Time X Group interaction was significant only for timed chair stands, indicating that the groups differed significantly in change in lower body strength over the three time points. Post hoc comparisons revealed that the tailored group had achieved greater strength than the generic group at both 6 months (p = .008) and 12 months (p = .002).
Healthy eating
All behavioral and biomarkers of healthy eating except for whole grain servings had significant main effects for time over the intervention period. From baseline to 6 months, both groups significantly increased fruit and vegetable servings and decreased percent calories from fat, while only the tailored group decreased percent calories from saturated fat. From baseline to 12 months, only the tailored group showed significant changes, with an increase in fruit and vegetable servings and a decrease in percent calories from saturated fat. The Time X Group interaction was significant for both fruit and vegetable servings and percent calories from saturated fat, indicating that the groups differed significantly in change in intake over the three time points. Post hoc comparisons revealed that the tailored group had sustained increased intake of fruits and vegetables at 12 months, while the generic group had dropped back to baseline levels (p = .002). The tailored group consumed a lower percent calories from saturated fat than the generic group at both 6 months (p = .028) and 12 months (p < .001).
Biomarkers of activity and eating
Systolic and diastolic blood pressure, body mass index, and LDL cholesterol had significant main effects for time over the intervention period. From baseline to 6 months, both groups had significantly lower LDL cholesterol, while only the tailored group had lower systolic and diastolic blood pressure, and only the generic group had a decreased body mass index. From baseline to 12 months, only the tailored group had lower systolic blood pressure, while both groups had lower diastolic blood pressure and lower LDL cholesterol levels. The Time X Group interaction was significant for systolic and diastolic blood pressure and for percent body fat, indicating that the groups differed significantly in change in these biomarkers over the three time points. Post hoc comparisons revealed that the pattern of change in blood pressure differed, with the generic group having higher values at 6 months and lower values at 12 months than the tailored group. Percent body fat values trended down for the tailored group and up for the generic group at both times.
Secondary Outcomes
The χ2 results for the proportion of each newsletter group achieving the physical activity and healthy eating behavioral outcome targets at 6 months and 12 months are shown in Table 4. There were no significant differences between the newsletter groups in achievement of any target at 6 months. At 12 months, a significantly higher proportion of the tailored newsletter group had achieved the eating behavioral outcome targets of at least 2 daily fruit servings, at least 3 daily vegetable servings, and not more than 30% of calories from fat daily, and the activity behavioral outcome target of at least 210 minutes of moderate or greater intensity activity weekly (30 minutes daily on 7 days each week).
Table 4.
Differences in Achievement of Behavioral Outcome Targets by Newsletter Group
| Tailored Newsletter Group (n= 115) | Target Achievement Generic Newsletter Group (n= 110) | Difference | ||||
|---|---|---|---|---|---|---|
| Behavioral Outcome Target | n | % | n | % | χ2 | p |
| Healthy Eating | ||||||
| At least 2 servings of fruit daily | ||||||
| Baseline | 37 | 32.2 | 37 | 33.6 | 0.01 | .927 |
| 6 months | 64 | 55.7 | 49 | 44.5 | 2.35 | .125 |
| 12 months | 52 | 45.2 | 28 | 25.5 | 8.74 | .003* |
| At least 3 servings of vegetables daily | ||||||
| Baseline | 67 | 58.3 | 59 | 53.6 | 0.32 | .573 |
| 6 months | 84 | 73.0 | 68 | 61.8 | 2.74 | .098 |
| 12 months | 79 | 68.7 | 54 | 49.1 | 8.15 | .004* |
| At least 3 servings of whole grains daily | ||||||
| Baseline | 8 | 7.0 | 2 | 1.8 | 2.39 | .122 |
| 6 months | 8 | 7.0 | 6 | 5.5 | 0.04 | .849 |
| 12 months | 2 | 1.7 | 3 | 2.7 | 0.00 | .960 |
| Not >30 % calories from fat daily | ||||||
| Baseline | 15 | 13.0 | 8 | 7.3 | 1.46 | .227 |
| 6 months | 17 | 14.8 | 13 | 11.8 | 0.21 | .647 |
| 12 months | 21 | 18.3 | 7 | 6.4 | 6.25 | .012* |
| <10% calories from saturated fat daily | ||||||
| Baseline | 39 | 33.9 | 22 | 20.0 | 4.83 | .028* |
| 6 months | 45 | 39.1 | 40 | 36.4 | 0.08 | .772 |
| 12 months | 44 | 38.3 | 30 | 27.3 | 2.60 | .107 |
| Physical Activity - At least 150 mins. of moderate or greater intensity activity weekly | ||||||
| Baseline | 52 | 45.2 | 45 | 40.9 | 0.27 | .605 |
| 6 months | 79 | 68.7 | 71 | 64.5 | 0.27 | .604 |
| 12 months | 73 | 63.5 | 58 | 52.7 | 2.25 | .134 |
| At least 210 min of moderate or greater intensity activity weekly | ||||||
| Baseline | 42 | 36.5 | 35 | 31.8 | 0.36 | .547 |
| 6 months | 67 | 58.3 | 64 | 58.2 | 0.00 | .999 |
| 12 months | 63 | 54.8 | 43 | 39.1 | 4.94 | .026* |
Discussion
The Wellness for Women trial provides the first reported results of a randomized computer-tailored intervention as compared with a generic intervention employing distance methodology to facilitate change in both physical activity and healthy eating in rural midlife and older women. Both the newsletters and exercise videotapes were designed for use with this population. Unlike other reported studies of randomized controlled tailored interventions to encourage change in both activity and eating, this study augmented self-reported behavioral markers with objective biomarkers of activity and eating to measure outcomes in all enrollees. While most tailored print health behavior change interventions have provided only one or two tailored communications to participants (Noar et al., 2007), this study provided multiple communications (18 newsletters) over 12 months to allow time for incorporation of behavior change into lifestyle.
Women were not required to leave their rural areas for either assessments or intervention. The intervention was entirely home-based, with newsletters mailed directly to their homes. The convenience of this approach may have contributed to the exceptionally low 4.4% overall attrition rate. Differential dropout between study arms (7.8% in the tailored newsletter group and 1.8% in the generic newsletter group) is recognized, but is not of great concern because the reasons for dropping out seem unrelated to the intervention.
For the primary outcomes, time effects were significant for most behavioral and biomarkers of activity and eating over the three study time points, with moderate to large rather than small effect sizes as reported in other studies (Kroeze et al., 2006). The only eating behavior that did not change was whole grain servings, which remained about one daily despite repeated encouragement in the newsletters to increase intake to three. This may have been influenced by public media attention to the value of low carbohydrate diets during the intervention period. Women may not have discriminated between whole grains and carbohydrates in general when they heard such advice. Significant group differences over the three study time points, favoring the tailored group, were found for fruit and vegetable servings, percent calories from saturated fat, lower body muscular strength, systolic and diastolic blood pressure, and percent body fat.
Newsletter effects were most apparent when examining the simple main effects tests of each group’s change in behavior separately at 6 and 12 months. From baseline to 6 months, both groups improved on all three activity and two eating behaviors, while only the tailored group improved a third eating behavior. From baseline to 12 months, both groups improved on stretching and strength exercise, but only the tailored group improved on moderate or greater intensity physical activity. Women who received tailored newsletters increased their weekly minutes of activity by 74%, an impressive change. The generic group had no change in eating behavior, while the tailored group increased their average daily servings of fruits and vegetables from 5.7 at baseline to 6.6 at 12 months, and decreased their percent calories from saturated fat from 11.3% to 10.5% daily but were still above the recommended 10% or less. It was apparent that tailored newsletters, based on women’s individual assessment data, had a stronger effect on behavior over a longer time and may lead to more permanent lifestyle change.
Fairly similar changes in biomarkers were evident from baseline to 6 months and 12 months, with the tailored newsletter group improving on one and two more biomarkers than the generic newsletter group, respectively. Some clinically important changes in biomarkers were noted. Both groups improved their cardiorespiratory fitness (VO2max) from baseline to 12 months; the tailored group by 7.4% and the generic group by 5.8%. This exceeded the 5% increase in VO2max achieved in several randomized clinical trials of physical activity counseling with sedentary adults ages 30–75 years (Writing Group for the Activity Counseling Trial Research Group, 2001), and was impressive considering the women’s baseline fitness levels (X = 20.22ml/kg/min) were well below the average of 24.5 ml/kg/min for their age and gender (ACSM, 2006). From baseline to 12 months, women lowered their LDL cholesterol levels to near optimal levels, by 13 points in the tailored group and 19 points in the generic group. Counteracting the rise in LDL that women experience after menopause is a primary focus in preventing atherosclerosis and heart attacks. Women in the tailored group improved lower body strength by 21.2% from baseline to 12 months, while the generic group improved by 9.5%. Such improvements in fitness and strength have been shown to lower risk of functional decline and mortality in women (Blair et al., 1996).
For the secondary outcomes, there was no newsletter group difference in achievement of HP 2010 physical activity and healthy eating behavioral criterion standards at 6 months. At 12 months, a significantly higher proportion of the tailored newsletter group had achieved three of the five outcome targets for eating and the outcome target for activity. However, at least 30% of the women in the tailored group and at least 47% of the women in the generic group did not meet each of the criterion standards. Considerably more work is needed to help midlife and older rural women to achieve a healthy lifestyle as reflected by these standards.
Several limitations to the study design are acknowledged. The measurement of behavioral markers of activity and eating by self-report may have been biased by social desirability of response, but those reports were supplemented by biomarkers. Generalizability was limited by the randomization of sites rather than participants to intervention groups. However, the possibility of cross-intervention contamination within rural communities where women in both groups would have a high likelihood of interaction at commercial and social settings was considered a greater threat to validity. The dearth of minorities in the areas from which participants were recruited also limits generalizability of results. However, the sample was representative of a hard-to-reach older rural underserved population of women that has been an infrequent target of such intervention. Although random digit dialing was employed to randomly select eligible women in the target counties, not all those contacted consented to participate, potentially biasing the sample in favor of those who had greater interest in changing their health behaviors. While the use of random digit dialing for recruitment may appear to limit inclusion of women without telephones, 97.6% of rural households had telephones at that time.
More than a quarter of older women live in rural areas, where the public health structure is often fragmented and underfunded if it exists at all (Lafronza & Inoglia, 2005). Access to health care in many rural areas is limited due to shortages of health professionals and the distances that women must travel to a provider. Many overworked and underreimbursed rural providers do not provide their clients with lifestyle modification advice. Thus, there is a need to expand access to lifestyle guidance with effective interventions delivered by methods other than face-to-face encounters, such as the distance model evaluated here. The considerable investment of time and resources required for computer tailoring seems justified by the greater changes in healthy eating and physical activity achieved.
Acknowledgments
This research was supported by Grant No. R01 NR04861 from the National Institute of Nursing Research, National Institutes of Health, with supplemental funding from a grant from the Nebraska Medical Center and the University of Nebraska Medical Center for lipid testing and from The Hygenic Corporation Thera-Band® Academy. Thank you to Cathy Vasko, BSN, RN, and Dawn Garcia, BSN, RN for their work as the research nurses and site coordinators.
Footnotes
Copyright
Nursing Research copyright statement has been signed by all authors. That should not be construed to exclude submission to PubMed Central. The NIH is mandating that as of April 7, 2008, all peer-reviewed manuscripts arising from NIH funds must be submitted to PubMed Central upon acceptance for publication.
Statement of Authorship
Dr. Walker was the principal investigator, Dr. Pullen was the co-principal investigator, Drs. Boeckner and Hageman were investigators, Dr. Hertzog was the statistician, Ms. Oberdorfer was the coordinator, and Mr. Rutledge designed and managed the data management system for this research project.
Notifications of Conflicts of Interest
No conflicts of interest are recognized.
Ethical Adherence
Institutional Review Board approval was obtained prior to sample recruitment and each participant provided written informed consent.
Contributor Information
Susan Noble Walker, Professor and Dorothy Hodges Olson Chair in Nursing Emeritus, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska.
Carol H. Pullen, Professor, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska.
Linda Boeckner, Professor and Extension Nutrition Specialist, Department of Nutrition and Health Sciences, University of Nebraska Panhandle Research and Extension Center, Scottsbluff, Nebraska.
Patricia A. Hageman, Professor and Director, Division of Physical Therapy Education, College of Medicine, University of Nebraska Medical Center Omaha, Nebraska.
Melody Hertzog, Assistant Professor and Research Analyst, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska.
Maureen K. Oberdorfer, Wellness for Women Project Coordinator, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska.
Matthew J. Rutledge, Information Technologist, College of Nursing, University of Nebraska Medical Center, Omaha, Nebraska.
References
- American College of Sports Medicine. ACSM's Guidelines for Exercise Testing and Prescription. 7. Philadelphia: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Blair SN, Kampert JB, Kohl HW, 3rd, Barlow CE, Macera CE, Paffenbarger RS, Jr, et al. Influences of cardiorespiratory fitness and other precursors on cardiovascular disease and all-cause mortality in men and women. JAMA. 1996;276(3):205–210. [PubMed] [Google Scholar]
- Blalock SJ, DeVellis BM, Patterson CC, Campbell MK, Orenstein DR, Dooley MA. Effects of an osteoporosis prevention program incorporating tailored educational materials. American Journal of Health Promotion. 2002;16(3):146–156. doi: 10.4278/0890-1171-16.3.146. [DOI] [PubMed] [Google Scholar]
- Boeckner LS, Pullen CH, Walker SN, Abbott GW, Block T. Use and reliability of the World Wide Web version of the Block Health Habits and History Questionnaire with older rural women. Journal of Nutrition Education and Behavior. 2002;3(Suppl 1):S20–S24. doi: 10.1016/s1499-4046(06)60307-2. [DOI] [PubMed] [Google Scholar]
- Casey MM, Thiede Call K, Klingner JM. Are rural residents less likely to obtain recommended preventive healthcare services? American Journal of Preventive Medicine. 2001;21(3):182–188. doi: 10.1016/s0749-3797(01)00349-x. [DOI] [PubMed] [Google Scholar]
- Demark-Wahnefried W, Clipp EC, Lipkus IM, Lobach D, Snyder DC, Sloane R, et al. Main outcomes of the FRESH START trial: A sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. Journal of Clinical Oncology. 2007;25(19):2709–2718. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the $EM$ algorithm. Journal of the Royal Statistical Society Series B (Methodological) 1977;39(1):1–38. [Google Scholar]
- Gamm LD, Hutchinson LL, Linnae L, Dabney BJ, Dorsey AM. Rural healthy people 2010: A companion document to healthy people 2010. College Station TX: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- Hageman PA, Walker SN, Pullen CH, Pellerito P. Test-retest reliability of the Rockport Fitness Walking Test and other fitness measures in women ages 50–69 years. Issues on Aging. 2001;24:7–11. [Google Scholar]
- [Accessed 2/29/08];HealthyPeople 2010 Midcourse Review. 2006 at http://www.healthypeople.gov/data/midcourse/default.htm#pubs.
- Hellman EA, Williams MA, Thalken L. Construct validity of the Modified 7-Day Activity Interview used with older adults with cardiac problems. Rehabilitation Nursing Research. 1996/1997;5(4):126–133. [Google Scholar]
- Kreuter M, Farrell D, Olevitch L, Brennan L. Tailoring health messages: Customizing communication with computer technology. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. [Google Scholar]
- Kreuter MW, Oswald DL, Bull FC, Clark EM. Are tailored health education materials always more effective than non-tailored materials? Health Education Research. 2000;15(3):305–315. doi: 10.1093/her/15.3.305. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Strecher VJ. Do tailored behavior change messages enhance the effectiveness of health risk appraisal? Results from a randomized trial. Health Education Research. 1996;11(1):97–105. doi: 10.1093/her/11.1.97. [DOI] [PubMed] [Google Scholar]
- Kroeze W, Werkman A, Brug J. A systematic review of randomized trials on the effectiveness of computer-tailored education on physical activity and dietary behaviors. Annals of Behavioral Medicine. 2006;31(3):205–223. doi: 10.1207/s15324796abm3103_2. [DOI] [PubMed] [Google Scholar]
- Lafronza V, Inoglia JN. The edge of America: Struggling for health and justice. Journal of Public Health Management and Practice. 2005;11(2):178–179. doi: 10.1097/00124784-200503000-00014. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual causes of death in the United States, 2000. JAMA. 2005;293(3):293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- Murtagh KN, Hubert HB. Gender differences in physical disability among an elderly cohort. American Journal of Public Health. 2004;94(8):1406–1411. doi: 10.2105/ajph.94.8.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. DHHS Publication No.1232. Hyattsville, MD: 2002. Health, United States, 2002 with chartbook on trends in the health of Americans. [Google Scholar]
- National Institutes of Health Consensus Statement. Bioelectrical impedance analysis in body composition measurement. National Institutes of Health Technology Assessment Conference Statement. December 12–14, 1994. Nutrition. 1996;12(11–12):749–762. [PubMed] [Google Scholar]
- Nigg CR, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: Common themes advancing health behavior research. Health Education Research. 2002;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychological Bulletin. 2007;133(4):673–693. doi: 10.1037/0033-2909.133.4.673. [DOI] [PubMed] [Google Scholar]
- Ory M, Kinney Hoffman M, Hawkins M, Sanner B, Mockenhaupt R. Challenging aging stereotypes: Strategies for creating a more active society. American Journal of Preventive Medicine. 2003;25(3 Suppl 2):164–171. doi: 10.1016/s0749-3797(03)00181-8. [DOI] [PubMed] [Google Scholar]
- Pender N, Murdaugh C, Parsons M. Health promotion in nursing practice. 4. Upper Saddle River, NJ: Haworth Press; 2002. [Google Scholar]
- Skinner C, Siegfried JC, Kegler MC, Strecher VJ. The potential of computers in patient education. Patient Education and Counseling. 1993;22(1):27–34. doi: 10.1016/0738-3991(93)90086-c. [DOI] [PubMed] [Google Scholar]
- Smeets T, Kremers SPJ, Brug J, de Vries H. Effects of tailored feedback on multiple health behaviors. Annals of Behavioral Medicine. 2007;33(2):117–123. doi: 10.1007/BF02879892. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services. With Understanding and Improving Health and Objectives for Improving Health. 2. Vol. 2. Washington, DC: United States Government Printing Office; 2000. Healthy People 2010. [Google Scholar]
- Walker SN, Pullen CH, Hertzog M, Boeckner L, Hageman PA. Determinants of older rural women’s activity and eating. Western Journal of Nursing Research. 2006;28(4):449–468. doi: 10.1177/0193945906286613. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Castro C, King AC, Housemann R, Brownson RC. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. Journal of Epidemiology and Community Health. 2000;54(9):667–672. doi: 10.1136/jech.54.9.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Writing Group for the Activity Counseling Trial Research Group. Effects of physical activity counseling in primary care: The Activity Counseling Trial, A randomized controlled trial. JAMA. 2001;286(6):677–687. doi: 10.1001/jama.286.6.677. [DOI] [PubMed] [Google Scholar]