Abstract
Objective: To assess whether people who ever use any form of chewing substance in Asia are at increased risk of cardiovascular disease (CVD). Methods: PubMed and ISI Web of Science were searched for relevant studies, with no limitation on language or study year. Studies were included if they provided quantitative estimate of the association between ever use of chewing substance and the occurrence of CVD. Two authors independently implemented inclusion criteria, abstracted study characteristics, and performed meta-analysis. Summary relative risks were estimated on the basis of a random effect model. We used Q statistic and Egger’s test to examine heterogeneity across studies and potential publication bias, respectively. Results: Eight eligible studies were included. The relative risk of CVD for ever using chewing substances with or without tobacco was 1.26 (95% confidence interval (CI) 1.12–1.40), which was unchanged when restricted to cohort studies [1.25 (1.08–1.42)] or cohort studies in Taiwan [1.31 (1.12–1.51)]. The summary relative risk for ischemic heart disease was 1.27 (1.02–1.52), and was lowered to 1.26 (0.85–1.67) after exclusion of a cross-sectional study. The overall relative risk for cerebrovascular disease was 1.32 (1.08–1.56). On the basis of the Taiwan data, the summary relative risk of CVD for betel (Areca catechu) chewing was 1.30 (1.17–1.44). Data on dose-response were limited to betel chewing in Taiwan, suggesting a relationship between risk of CVD and cumulative exposure. Two large cohorts in Taiwan reported a greater risk of CVD with betel chewing than with smoking. Conclusions: An association was detected between betel chewing with or without tobacco and the risk of CVD. Betel chewing may impose a greater CVD risk than smoking. More effort is needed in developing betel chewing cessation programmes. The relationship between betel chewing and subgroups of CVD requires further investigation.
Keywords: Cardiovascular disease, Areca catechu, Betel quid, Chewing tobacco, Relative risk, Meta-analysis
1. Introduction
Various forms of smokeless tobacco, including chewing tobacco and paan, namely, Areca catechu/betel quid with tobacco, have been used in Asia for centuries. Betel quid is made up of fresh betel leaves, areca nut, and slaked lime, and can be served with or without tobacco (Gupta and Ray, 2004). Preparation of betel quid varies from region to region, with the major difference being whether tobacco is added. To avoid a possible misnomer by classifying betel quid with some types of smokeless tobacco, while sometimes tobacco is actually absent, we herein employed the term “chewing substance” to refer to any type of chewing tobacco or betel quid with or without tobacco. Betel quid with tobacco is said to be one of the most commonly used forms of smokeless tobacco in South Asia (Gupta and Ray, 2003), whereas areca nut (usually incorporated in betel quid) ranks the fourth most common addictive substance in the world after caffeine, tobacco, and alcohol (Gupta and Ray, 2004).
The complex nexus between chewing tobacco and betel quid is not easy to dissect. This, along with high prevalence of chewing tobacco and betel quid in South and Southeast Asia, exhibits a geographically unique scene of tobacco use, or more accurately, substance use other than the pandemic cigarette smoking (Rani et al., 2003; Wen et al., 2005; Teo et al., 2006). Compared to cigarette smoking, which is a well established risk factor for cardiovascular disease (CVD), chewing tobacco and betel quid, though prevailing in many parts of Asia, are relatively less explored for their potential adverse effect on cardiovascular system. To date, few epidemiological studies have been conducted in Asia (Gupta et al., 2005; Wen et al., 2005; Teo et al., 2006; Guh et al., 2007; Lan et al., 2007; Lin et al., 2008; Rahman and Zaman, 2008; Yen et al., 2008), investigating the relative risk of CVD related to chewing tobacco and betel quid, and the findings are not all comparable.
A recent meta-analysis indicated that smokeless tobacco users in Sweden and USA were at increased risk of CVD compared with nonusers (Boffetta and Straif, 2009). However, studies conducted in Asia were not included in view of heterogeneity between the contents of smokeless tobacco in Asia and those in Sweden and USA. Thus, the conclusion may not be readily applicable in the Asian context. Determining the roles of chewing tobacco and betel quid in CVD is important, given their high prevalence of usage and current high incidence and mortality of CVD in Asia. All these concerns prompted us to carry out a meta-analysis to summarize existing evidence, on the link between use of chewing substances and risk of CVD.
2. Methods
2.1. Searching strategy and selection criteria
The MOOSE guidelines for meta-analysis of observational studies in epidemiology were followed (Stroup et al., 2000). We searched PubMed (up to July 2010), using the terms: (“cardiovascular diseases” [mesh] OR (“cardiovascular” [All Fields] AND “diseases” [All Fields]) OR “cardiovascular diseases” [All Fields] OR “cerebrovascular disorders” [mesh] OR (“cerebrovascular” [All Fields] AND “disorders” [All Fields]) OR “cerebrovascular disorders” [All Fields] OR “stroke” [mesh] OR “stroke” [All Fields] OR mortality OR death*) AND (“betel quid” OR “betel-quid” OR “betel nut” OR “betel nuts” OR “areca nut” OR “areca nuts” OR “paan” OR “pan” OR snuff OR snus OR “gul” OR “gutka” OR “khaini” OR “loose leaf” OR “maras” OR “mawa” OR “mishri” OR “naswar” OR “Areca catechu” OR “tooth powder” OR “shammah” OR “tobacco chewing gum” OR “zarda” OR “tobacco, smokeless” [mesh] OR “smokeless tobacco” OR “chewing tobacco” OR “non-smoking tobacco”) AND (“cohort studies” [mesh] OR “cross-sectional studies” [mesh] OR “case control studies” [mesh] OR (“cohort” [TI] AND stud* [TI]) OR (case* [TI] AND control* [TI]) OR prospective OR retrospective OR cross-sectional OR “cross sectional”), which yielded 1006 potentially relevant references. We adapted the searching strategy for a second search in ISI Web of Science (updated July 19, 2010), and found another 739 references. We identified all observational studies including cohorts, case-control studies, and cross-sectional studies, provided that they explored the association between ever using chewing substances and the occurrence (incidence or mortality) of CVD, and reported the strength of the associations with a quantitative risk estimate. There was no limitation on language, study year, or publication status.
After excluding duplicates, two authors independently reviewed all citations with titles and abstracts that appeared to fit the criteria for inclusion. We checked references of included studies and reviews to further identify other potentially eligible studies. The numbers of citations excluded and reason for exclusion were tracked.
2.2. Outcome measurement
We conducted the meta-analysis based on selected outcome measurements including cardiovascular disease (CVD), ischemic heart disease (IHD), and cerebrovascular disease (CBVD). The following sub section will describe in detail how these outcome measurements were identified.
2.3. Data extraction
Two authors independently extracted risk estimates and characteristics of each individual study. We followed the international classification code (ICD-9 and ICD-10) when grouping the extracted outcome measurements. Accordingly, we regarded CVD as either 390–459 in ICD-9 or I00–I99 in ICD-10, IHD as either 410–414 in ICD-9 or I20–I25 in ICD-10, and CBVD as either 430–438 in ICD-9 or I60–I69 in ICD-10. When outcomes were not coded with an ICD number, we made assumptions according to the definition of diseases reported and how ascertainment was made. The extracted data were compared and any inconsistencies resolved. Wherever possible, data were extracted for fatal and non-fatal cardiovascular events.
If stratified results were presented from one study (for example, separate results for current and former use, for men and women), we combined them by carrying out a meta-analysis based on fixed effect model when Q statistic was not significant (P>0.1); otherwise we used a random effect model.
2.4. Data synthesis and statistical analysis
A meta-analysis was made of the selected primary endpoint outcomes based on a random effect model (DerSimonian and Laird, 1986). We examined heterogeneity across studies with the Q statistic (P<0.1 considered significant). Egger’s test was used to detect possible publication bias. All of analyses were conducted with the statistical package STATA (Version 11.0; Stata Corp, College Station, TX, USA).
We classified studies on the basis of the chosen outcomes (CVD, IHD, CBVD). In addition, we also classified studies by geographical region of study and study design (cohort, case-control) in the subgroup analysis. We accounted for concurrent smoking as a confounding factor, if a risk estimate was neither restricted to non-smokers nor obtained after adjustment for smoking; we considered it for sensitivity analysis by repeating the meta-analysis after exclusion of the study. Similarly, we repeated the meta-analysis after removing cross-sectional studies, and studies in which we had made any assumption about the classification of diseases. To minimize the confounding due to presence or absence of tobacco in chewing substances, which may be characteristic of different regions, we repeated the meta-analysis after stratification by geographical region. The possible influence of study design was assessed by repeating the main analysis with cohort study data only. To disentangle the effect of geographical region from that of study design, we carried out a further meta-analysis restricted to cohort studies from Taiwan.
3. Results
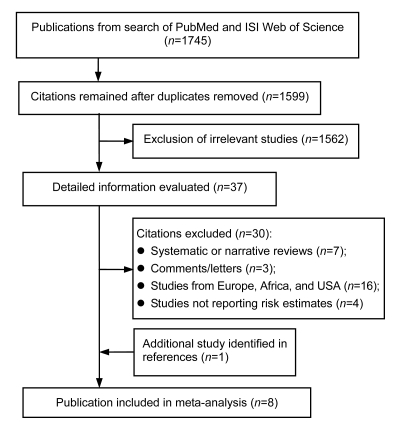
Fig. 1 shows details of study identification, inclusion, and exclusion. A total of 1599 publications were initially screened. Eight studies met the criteria for inclusion in the present study.
Fig. 1.
Flow diagram of the study selection process
3.1. Characteristics of included studies
Table 1 shows the characteristics of the included studies. All of the epidemiological studies were undertaken in South and East Asia in recent years. Five cohort studies were from India and Taiwan (China) (Gupta et al., 2005; Wen et al., 2005; Lan et al., 2007; Lin et al., 2008; Yen et al., 2008), two used case-control design, one of which is a multi-center study (Teo et al., 2006; Rahman and Zaman, 2008), and another one used cross-sectional design (Guh et al., 2007). Of the eight studies included, four studies reported increased risk for use of chewing substance (Teo et al., 2006; Lin et al., 2008; Rahman and Zaman, 2008; Yen et al., 2008), two showed inconsistent results between women and men (Gupta et al., 2005; Guh et al., 2007), one found inconsistency between subtypes of CVD (Lan et al., 2007), and still another one reported negative results (Wen et al., 2005). Four studies (Gupta et al., 2005; Teo et al., 2006; Lin et al., 2008; Rahman and Zaman, 2008) reported risk estimates of substance chewers restricted to never tobacco smokers, whereas the others all included cigarette smokers in both categories (Wen et al., 2005; Lan et al., 2007; Guh et al., 2007; Yen et al., 2008), and could not report the relative risk of chewing betel quid alone. In the latter, however, risk estimates were all adjusted for cigarette smoking, except in one study (Wen et al., 2005).
Table 1.
Characteristics of included epidemiological studies on chewing substances and risk of CVD
| Study | Geographical region, gender, recruitment, follow-up, No. of participants | Study design | Exposure | Outcome | Definition and ascertainment | No. of cases or deaths# | RR (95% CI) | Adjustment factors |
| Teo et al., 2006 | Mainly South Asia, both sexes, 1999–2003, NR, 27 098 | Case-control | Chewing tobacco | Acute myocardial infarction | Characteristic manifestation and ECG (specific criteria available) | NA | 2.23 (1.41–3.52) | Age, gender, diabetes, abdominal obesity, hypertension, exercise, diet |
| Wen et al., 2005 | Taiwan (China), men, 1982–1992, 1982–2000, 19 719 | Cohort | Betel quid | CVD [390–459], IHD [410–414], stroke [430–438] | ICD-9, death registry system | 275/39/86 | 1.1 (0.8–1.6), 1.0 (0.5–2.4), 1.3 (0.8–2.2) | Age, alcohol, education |
| Gupta et al., 2005 | India, both sexes, 1992–1994, 1992–1999, 97 244 | Cohort | Betel quid, areca nut, mishri | CVD [I00–I99], IHD [I10, I11, I13, I21, I24, I25, I46, I50], CBVD [I61–I64, I66, I67] | ICD-10, death registry system | 1876/1372/386 | 1.06 (0.84–1.33)*, 1.05 (0.76–1.47)*, 1.23 (0.97–1.55)* | Age, education |
| Rahman and Zaman, 2008 | Bangladesh, both sexes, 2006–2007, NR, 207 | Case-control | Betel quid, dried tobacco leaf | Coronary heart disease (acute myocardial infarction and angina pectoris) | Clinical findings and ECG | NA | 2.8 (1.1–7.3) | Gender, age, hypertension |
| Yen et al., 2008 | Taiwan (China), men, 1999–2004, duration (2.81±1.50) years, 21 906 | Cohort | Betel quid | CVD [402, 410–414, 425–428, 430–438, 440–448] | ICD-9, incidence identified in hospital, mortality by registry system | 3163 | 1.24 (1.11–1.39) | Age, education, occupation, smoking, alcohol, intake of fish, milk, coffee, physical activity, family history |
| Lan et al., 2007 | Taiwan (China), both sexes, 1989–2003; 1996–2003, 6511 | Cohort | Betel quid | CVD [390–459], IHD [410–414], CBVD [430–438] | ICD-9, death registry system | 684/153/305 | 1.41 (1.12–1.77), 1.22 (0.73–2.04), 1.66 (1.19–2.30) | Gender, age, living area, hypertension, anemia, heart disease, liver disease, arthritis, physical difficulty, smoking, alcohol |
| Lin et al., 2008 | Taiwan (China), men, 1998–1999, 998–2005, 56 116 | Cohort | Betel quid | CVD [390–459] | ICD-9, death registry system | 309 | 1.77 (1.31–2.40)* | Age, BMI, diabetes, hypertension, cholesterol, triglyceride, alcohol, smoking, physical activity, income, education |
| Guh et al., 2007 | Taiwan (China), both sexes, 1993–1996, NR, 1932 | Cross-sectional | Betel quid | Heart disease | Questionnaires on self-report | NA | 1.34 (1.12–1.62)* | Age, abdominal obesity, cholesterol, hypertension, diabetes, smoking, fruit intake |
Number of cases or deaths from a certain outcome, cardiovascular disease (CVD), ischemic heart disease (IHD), cerebrovascular disease (CBVD), etc. (listed in order in the fifth column). Cases or deaths of non-chewing smokers were not included. The numbers are listed in the same order to accompany their corresponding outcomes
Results of meta-analysis
RR: relative risk; CI: confidence interval; NR: not relevant; NA: not available; ECG: electrocardiograph, ICD: international classification code; BMI: body mass index
Three studies (Wen et al., 2005; Lan et al., 2007; Lin et al., 2008) mentioned that betel quid in Taiwan was generally chewed without tobacco. The betel quid was commonly used with added tobacco elsewhere in South Asia (Gupta and Ray, 2004), though it was not the case in the Mumbai cohort, where betel quid was chewed without tobacco (Gupta et al., 2005). Meta-analyses of stratified results were performed for three studies to obtain a summary relative risk (Gupta et al., 2005; Guh et al., 2007; Lin et al., 2008).
3.2. Chewing substances and risk of CVD
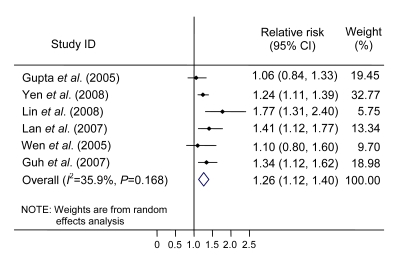
On the basis of six risk estimates, the overall relative risk of CVD (ICD-9: 390–459; ICD-10: I00–I99) for ever using chewing substances was 1.26 (95% confidence interval (CI) 1.12–1.40), with no evidence of heterogeneity among studies (Table 2, Fig. 2; test for publication bias P=0.68). Restricting the meta-analysis to cohort studies yielded a summary relative risk of 1.25 (1.08–1.42) based on five risk estimates. The summary relative risk of CVD for betel chewing was 1.30 (1.17–1.44) based on five studies from Taiwan. Data from cohort studies in Taiwan gave a summary relative risk of 1.31 (1.12–1.51) based on four risk estimates. An increased risk of death from CVD was present, 1.28 (1.00–1.56) based on four risk estimates. After removing one study that did not report a risk estimate after adjustment for smoking (Wen et al., 2005), the positive direction of relative risks all persisted, except for the fatal form of CVD (data not shown).
Table 2.
Results of meta-analysis on risk of CVD and chewing substances with or without tobacco
| Outcome and subgroups | No. of risk estimates | P* | RR (95% CI) |
| CVD | |||
| Overall | 6 | 0.17 | 1.26 (1.12–1.40) |
| Cohort | 5 | 0.13 | 1.25 (1.08–1.42) |
| Taiwan | 5 | 0.29 | 1.30 (1.17–1.44) |
| Cohort Taiwan | 4 | 0.19 | 1.31 (1.12–1.51) |
| Fatal | 4 | 0.07 | 1.28 (1.00–1.56) |
| IHD | |||
| Overall | 6 | 0.29 | 1.27 (1.02–1.52) |
| Cohort | 3 | 0.89 | 1.08 (0.78–1.38) |
| South Asia | 3 | 0.07 | 1.64 (0.60–2.68) |
| Taiwan | 3 | 0.77 | 1.31 (1.08–1.53) |
| Cohort Taiwan | 2 | 0.71 | 1.15 (0.61–1.70) |
| Fatal | 3 | 0.89 | 1.08 (0.78–1.38) |
| CBVD | |||
| Overall | 3 | 0.40 | 1.32 (1.08–1.56) |
| Taiwan | 2 | 0.43 | 1.52 (1.09–1.96) |
P for heterogeneity
CVD: cardiovascular disease; IHD: ischemic heart disease; CBVD: cerebrovascular disease; RR: relative risk; CI: confidence interval
Fig. 2.
Forest plot of risk estimates for CVD among users of chewing substances
Dose-response analysis for CVD was reported in three studies in Taiwan (Lan et al., 2007; Lin et al., 2008; Yen et al., 2008), and significant trends in risk by cumulative exposure were detected in two studies (Lan et al., 2007; Yen et al., 2008). In the third study (Lin et al., 2008), though the analysis for trend was not reported, the relative risk of fatal CVD was the highest in the groups of subjects using betel quid most often. In addition, two of these large cohorts (Lin et al., 2008; Yen et al., 2008) reported a greater risk of CVD caused by betel chewing than smoking. In Yen et al. (2008)’s study, the relative risks (95% CI) of CVD for betel chewing and smoking were 1.24 (1.11–1.39) and 0.96 (0.89–1.04), respectively. Lin et al. (2008) calculated that betel nut chewers had a higher risk of CVD mortality (relative risk 2.10; P<0.05) than did smokers.
3.3. Chewing substances and risk of IHD
An increased risk of IHD (ICD-9, 410–414; ICD-10: I20–I25) was observed, with a summary relative risk of 1.27 (1.02–1.52) on the basis of six risk estimates (Table 2; test for publication bias P=0.60). However, the relative risk effect became insignificant after the removal of the cross-sectional study of Guh et al. (2007), resulting in a summary risk estimate of 1.26 (0.85–1.67). The inconsistency between main analysis and subsequent sensitivity analysis indicated that a significant effect reached by main analysis may be heavily influenced by one single study. Thus, the result should be interpreted with caution. Restricting the meta-analysis to cohort studies (three risk estimates) or studies in South Asia (three risk estimates) did not show a marked increased risk, though the trend was toward positive (Table 2). Studies carried out in Taiwan revealed an increased risk of 1.31 (1.08–1.53), but again the effect appeared non-significant after exclusion of the same cross-sectional study where “heart disease” was recalled by patients rather than being diagnosed in hospital or classified with specific criteria (Guh et al., 2007).
Of note, there were two case-control studies that investigated the incidences of “coronary heart disease” and “acute myocardial infarction” (one of them being a multi-center study), and both showed marked increase of risk in tobacco chewers in South Asia (Teo et al., 2006; Rahman and Zaman, 2008).
3.4. Chewing substances and risk of CBVD
Only three estimates (Gupta et al., 2005; Wen et al., 2005; Lan et al., 2007) were available for CBVD (ICD-9: 430–438; ICD-10: I60–I69; all in fatal form), resulting in an overall relative risk of 1.32 (1.08–1.56) (Table 2; test for publication bias P=0.76). No heterogeneity was observed. Given the limited number of studies, we did not perform further subgroup analysis.
4. Discussion
Our meta-analysis showed an increased risk of CVD among users of chewing substances with or without tobacco compared with non-users. Study data from Taiwan indicated significantly increased CVD risk in relation to betel chewing. When meta-analyses were confined to cohort studies or cohort studies in Taiwan, the positive effects remained significant. This was further confirmed by subsequent sensitivity analysis by removing the studies that either did not report an adequately adjusted risk estimate (Wen et al., 2005) or defined the outcome measurement less clearly (Guh et al., 2007). The magnitudes of the excess risks for CVD and CBVD were both small, but the results were produced on the basis of several studies with large numbers of participants. The consistency of results among studies, and their robustness for study design and quality also added to their credibility. The meta-analysis for IHD, however, showed inconsistency, when a sensitivity analysis was undertaken. Further grouping the meta-analysis by study design or geographical region did not show the evidence of excess risk for IHD.
Several explanations may be given for the discrepancy in results between CVD in total and subtypes of CVD, such as IHD. First of all, numbers of IHD cases included may be relatively small. For example, four out of six studies had included no more than 200 IHD cases or deaths in each (Wen et al., 2005; Lan et al., 2007; Guh et al., 2007; Rahman and Zaman, 2008). Small study population may be underpowered to detect a possible association. However, this was not the case in the Mumbai cohort study (Gupta et al., 2005), which documented a total of 1372 IHD deaths (631 men and 741 women), though an increased risk was found only in women. Gupta et al. (2005) reasoned that cause-specific death rates could be underestimated, since nearly a quarter of total deaths could not be matched. Of note, identification of IHD deaths in this cohort showed a wider range than those in the other studies (Table 1), which might be a source of inconsistent results among studies. Furthermore, it was also noted that misclassification for the cause of death may well be possible even within a high quality death registering system (Gupta et al., 2005). It is unclear, however, how misclassification of fatal IHD could generate a false negative result in cohort studies, since misclassification would most likely be non-discriminatory for the exposure status (Rothman and Greenland, 1998). In any case, misclassification could have little influence on the identification of CVD in total. Since diseases of other systems were much less likely to be classified as circulatory diseases, while various diseases within the group of recognized CVD may be mistaken for each other.
Moreover, the meta-analysis for the risk of CVD in total was largely based on four cohort studies in Taiwan (Wen et al., 2005; Lan et al., 2007; Lin et al., 2008; Yen et al., 2008) where betel quid was chewed without tobacco (Wen et al., 2005). Meta-analysis based on Taiwan data showed increased risk of CVD for betel chewing, relative risk 1.30 (1.17–1.44) based on five risk estimates. When it was confined to cohort studies in Taiwan, the positive direction persisted, and was not swerved by exclusion of the very study in which risk estimate was not adjusted for cigarette smoking (Wen et al., 2005). In addition, two large cohorts in Taiwan (Lin et al., 2008; Yen et al., 2008) reported a greater risk of CVD from betel chewing than from smoking. The consistency between main analysis and sensitivity analysis, together with dose-response effect in several of these studies, attested to the evidence that betel chews free of tobacco can be harmful to cardiovascular system, though further classified subtypes of CVD were less studied for betel chewing. On the other hand, however, concerning chewing substances with tobacco, only one cohort study (Gupta et al., 2005) was available for the risk estimate of CVD in total, where increased relative risk was found only in women. In contrast, the two case-control studies including both sexes (Teo et al., 2006; Rahman and Zaman, 2008) have explored exclusively the relationship between coronary heart disease and use of chewing tobacco, which supported a positive link. Given these concerns, more investigations are needed to explore the risks for specific subgroups of CVD in relation to the use of betel chews with or without tobacco, but this would have to rely on specific and accurate classification of specific CVD forms and of specific CVD events.
The underlying mechanisms for the link between chewing substance and CVD may be multiple. Nicotine and arecoline, the predominant alkaloids that were found, respectively, in tobacco and betel quid (Areca catechu), are recognized for their short-term effects in causing increased heart rate and blood pressure (Benowitz and Gourlay, 1997; Boucher and Mannan, 2002). Recent studies both in India and Taiwan have found that tobacco chewers and betel chewers were more prone to have dyslipidemia and hypertension (Khurana et al., 2000; Chung et al., 2006; Gupta et al., 2007; Tseng, 2008), which are traditional risk factors of CVD. It may well raise the suspicion that some chemicals from these chewing substances may trigger specific biochemical reactions related to dyslipidemia and hypertension, which in turn lead to cardiovascular events. In addition, chewing itself may lead to susceptibility to periodontal diseases, which are potentially associated with cardiovascular malfunction (Ling et al., 2001; Janket et al., 2003). The detailed mechanism by which these processes are involved in the development of CVD remains unclear and merits further investigation.
Our findings extend the conclusion reached by a previous meta-analysis which indicated an association between smokeless tobacco and risk of CVD based on studies carried out in the United States and Sweden (Boffetta and Straif, 2009). To explore the associations of tobacco/betel chewing and CVD risks in Asia, we carried out a meta-analysis based on explicit criteria for inclusion of studies, extraction, and pooling of results. By summarizing the existing evidence quantitatively, we obtained a more precise risk estimate with a narrowed confidence interval, and thus increased the power to detect a link between use of betel quid and risk of CVD. The results included in the meta-analysis were adjusted for other known risk factors of CVD, such as hypertension, obesity, and education level.
Our study also has some limitations. First, it was unclear whether substance chewers would change their habit during follow-up in the cohort study. It might generate a false positive effect if chewers shifted to smoking. However, evidence supporting chewing tobacco or betel quid as a “gateway” to smoking was lacking in Asia. In fact, Taiwan data indicated that smoking appeared a “gateway” for betel quid chewing while smokers rarely started chewing first (Wen et al., 2005). Second, confounding by cigarette smoking might be a potential source of bias. Still this meta-analysis has very few studies suitable to use, and not all studies reported the relative risk confined to non-smokers. However, the numbers of participants in most of these studies were large, and in three of the four studies (Guh et al., 2007; Lan et al., 2007; Yen et al., 2008) where smokers were included, risk estimates were all reported after adjustment of smoking status. The other study (Wen et al., 2005) was removed in the sensitivity analysis, without altering the findings. Third, we did not perform meta-analysis stratified by gender, given lack of data. Very few women in Taiwan use betel quid (Wen et al., 2005; Lin et al., 2008), and in fact, three large cohorts in Taiwan investigated male participants exclusively (Wen et al., 2005; Lin et al., 2008; Yen et al., 2008). Furthermore, only one large cohort (Gupta et al., 2005) and another two studies (Guh et al., 2007; Rahman and Zaman, 2008) reported relative risk for females separately. However, the latter two included far less cases compared to other studies, making it meaningless to stratify the data by gender. Finally, in consideration of possible heterogeneity, we used a random effect model which may result in wider confidence intervals, and thus a more conservative estimate of effect.
In conclusion, a meta-analysis was carried out on studies of betel chewing in Asia, with and without tobacco, in relation to CVD risks. A direct association was detected, though the results on subgroups of CVD were less convincing. Furthermore, betel chewing may impose a greater CVD risk than smoking. More effort on developing betel chewing cessation programmes is urgently warranted. Further studies are needed to elucidate whether a similar effect is present for different subgroups of CVD and to clarify the mechanisms of the effect of chewing tobacco and betel quid on the occurrence of CVD.
Acknowledgments
The authors express their sincere thanks to the international peer referees for improving this paper.
Footnotes
Project (No. 2004C30067) supported by the Zhejiang Provincial Science and Technology Plan Project, China
References
- 1.Benowitz NL, Gourlay SG. Cardiovascular toxicity of nicotine: implications for nicotine replacement therapy. J Am Coll Cardiol. 1997;29(7):1422–1431. doi: 10.1016/S0735-1097(97)00079-X. [DOI] [PubMed] [Google Scholar]
- 2.Boffetta P, Straif K. Use of smokeless tobacco and risk of myocardial infarction and stroke: systematic review with meta-analysis. BMJ. 2009;339:b3060. doi: 10.1136/bmj.b3060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boucher BJ, Mannan N. Metabolic effects of the consumption of Areca catechu . Addict Biol. 2002;7(1):103–110. doi: 10.1080/13556210120091464. [DOI] [PubMed] [Google Scholar]
- 4.Chung FM, Chang DM, Chen MP, Tsai JC, Yang YH, Shieh TY, Shin SJ, Chen TH, Tai TY, Lee YJ. Areca nut chewing is associated with metabolic syndrome: role of tumor necrosis factor-alpha, leptin, and white blood cell count in betel nut chewing-related metabolic derangements. Diabetes Care. 2006;29(7):1714. doi: 10.2337/dc06-0628. [DOI] [PubMed] [Google Scholar]
- 5.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 6.Guh JY, Chen HC, Tsai JF, Chuang LY. Betel-quid use is associated with heart disease in women. Am J Clin Nutr. 2007;85(5):1229–1235. doi: 10.1093/ajcn/85.5.1229. [DOI] [PubMed] [Google Scholar]
- 7.Gupta BK, Kaushik A, Panwar RB, Chaddha VS, Nayak KC, Singh VB, Gupta R, Raja S. Cardiovascular risk factors in tobacco-chewers: a controlled study. J Assoc Phys India. 2007;55:27–31. [PubMed] [Google Scholar]
- 8.Gupta PC, Ray CS. Smokeless tobacco and health in India and South Asia. Respirology. 2003;8(4):419–431. doi: 10.1046/j.1440-1843.2003.00507.x. [DOI] [PubMed] [Google Scholar]
- 9.Gupta PC, Ray CS. Epidemiology of betel quid usage. ANNALS Acad Med Singapore. 2004;33(Suppl. 4):31–36. [PubMed] [Google Scholar]
- 10.Gupta PC, Pednekar MS, Parkin DM, Sankaranarayanan R. Tobacco associated mortality in Mumbai (Bombay) India. Results of the Bombay cohort study. Int J Epidemiol. 2005;34(6):1395–1402. doi: 10.1093/ije/dyi196. [DOI] [PubMed] [Google Scholar]
- 11.Janket SJ, Baird AE, Chuang SK, Jones JA. Meta-analysis of periodontal disease and risk of coronary heart disease and stroke. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;95(5):559–569. doi: 10.1067/moe.2003.107. [DOI] [PubMed] [Google Scholar]
- 12.Khurana M, Sharma D, Khandelwal PD. Lipid profile in smokers and tobacco chewers: a comparative study. J Assoc Phys India. 2000;48(9):895–897. [PubMed] [Google Scholar]
- 13.Lan TY, Chang WC, Tsai YJ, Huang YL, Lin HS, Tai TY. Areca nut chewing and mortality in an elderly cohort study. Am J Epidemiol. 2007;165(6):677–683. doi: 10.1093/aje/kwk056. [DOI] [PubMed] [Google Scholar]
- 14.Lin WY, Chiu TY, Lee LT, Lin CC, Huang CY, Huang KC. Betel nut chewing is associated with increased risk of cardiovascular disease and all-cause mortality in Taiwanese men. Am J Clin Nutr. 2008;87(5):1204–1211. doi: 10.1093/ajcn/87.5.1204. [DOI] [PubMed] [Google Scholar]
- 15.Ling LJ, Hung SL, Tseng SC, Chen YT, Chi LY, Wu KM, Lai YL. Association between betel quid chewing, periodontal status and periodontal pathogens. Oral Microbiol Immunol. 2001;16(6):364–369. doi: 10.1034/j.1399-302X.2001.160608.x. [DOI] [PubMed] [Google Scholar]
- 16.Rahman MA, Zaman MM. Smoking and smokeless tobacco consumption: possible risk factors for coronary heart disease among young patients attending a tertiary care cardiac hospital in Bangladesh. Public Health. 2008;122(12):1331–1338. doi: 10.1016/j.puhe.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 17.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tobacco Control. 2003;12(4):e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rothman KJ, Greenland S. Precision and Validity in Epidemiologic Studies. In: Rothman KJ, Greenland S, editors. Modern Epidemiology. 2 Ed. Philadelphia, PA: Lippincott-Raven; 1998. pp. 15–34. [Google Scholar]
- 19.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 20.Teo KK, Ounpuu S, Hawken S, Pandey MR, Valentin V, Hunt D, Diaz R, Rashed W, Freeman R, Jiang L, et al. Tobacco use and risk of myocardial infarction in 52 countries in the INTERHEART study: a case-control study. The Lancet. 2006;368(9536):647–658. doi: 10.1016/S0140-6736(06)69249-0. [DOI] [PubMed] [Google Scholar]
- 21.Tseng CH. Betel nut chewing is associated with hypertension in Taiwanese type 2 diabetic patients. Hypertens Res. 2008;31(3):417–423. doi: 10.1291/hypres.31.417. [DOI] [PubMed] [Google Scholar]
- 22.Wen CP, Tsai SP, Cheng TY, Chen CJ, Levy DT, Yang HJ, Eriksen MP. Uncovering the relation between betel quid chewing and cigarette smoking in Taiwan. Tobacco Control. 2005;14(Suppl. 1):i16–i22. doi: 10.1136/tc.2004.008003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yen AM, Chen LS, Chiu YH, Boucher BJ, Chen TH. A prospective community-population-registry based cohort study of the association between betel-quid chewing and cardiovascular disease in men in Taiwan. Am J Clin Nutr. 2008;87(1):70–78. doi: 10.1093/ajcn/87.1.70. [DOI] [PubMed] [Google Scholar]