Abstract
AIM: To find out whether a newly designed big cup nitinol stent is suitable for treatment of patients with gastric outlet obstruction resulting from gastric cancer.
METHODS: The new stent is composed of a proximal big cup segment (20 mm in length and 48-55 mm in diameter), a middle part (60 mm in length and 20 mm in diameter) covered by a polyethylene membrane and a distal sphericity (20 mm in length and 28 mm in diameter). Half of the proximal big cup segment is also covered by a polyethlene membrane, which is adjacent to the middle part of the stent. The stent is preloaded in a 6.0-mm-diameter introducer system. Thirteen patients with gastric outlet obstruction resulting from gastric cancer received the new stents under endoscopic and fluoroscopic guidance.
RESULTS: Technical success was achieved in 12 of 13 (92.3%) patients. Among the 12 patients in whom endoscopic stent was placed successfully, the clinical success rate was 91.7% during a follow-up of average 6.5 mo. During the first month follow-up, the migration rate was 0%, recurrent obstruction 0% and gastric bleeding 8.3%. During the follow-up between 2-12 mo, no migration, recurrent obstruction and gastric bleeding occurred.
CONCLUSION: The proximal big cup segment seems to be effective and promising for technical efficacy, clinical outcome, and preventing migration and tumor ingrowth and increasing the emptying rate of sinus ventriculi.
Keywords: Endoscopic, Gastric outlet, Stenosis, Obstruction, Stents
INTRODUCTION
Endoscopic stent placement has been increasingly used as a nonsurgical palliative treatment option for patients with gastric outlet obstruction caused by unresectable stomach cancer. However, conventional stents result in many complications including migration, restenosis and so on. Moreover, their proximal parts are not fit for roomy gastral cavity. To overcome the migration and restenosis, and to increase the emptying rate of sinus ventriculi, we designed a new big cup nitinol stent. This report is to evaluate its clinical efficacy for gastric outlet obstruction caused by stomach cancer.
MATERIALS AND METHODS
Subjects
From April 2005 to May 2009, the newly designed big cup nitinol stent was placed in 13 patients (7 men, 6 women; mean age 77.6 years, range 71-93 yeas) with gastric outlet obstruction resulting from gastric cancer. The tumors were considered unresectable in all patients because of advanced, metastatic disease (10/13) and old age with medical comorbidity (3/13). All patients exhibited signs of gastric outlet obstruction, such as intractable vomiting and inability to eat. Endoscopic biopsy established the diagnosis of malignancy. Before endoscopy, the site and length of the stenosis were evaluated by radiography taken after oral contrast opacification. Patients were included following the criteria: (1) gastric outlet obstruction defined by symptoms resulting in decreased oral intake (nausea, vomiting, and inability to eat); and (2) the site of stenosis was between gastric body and duodenum bulb (Figure 1A). The study was approved by our hospital’s ethics committee and was performed in compliance with our hospital’s policies related to the use of animal and/or human subjects and human-derived material.
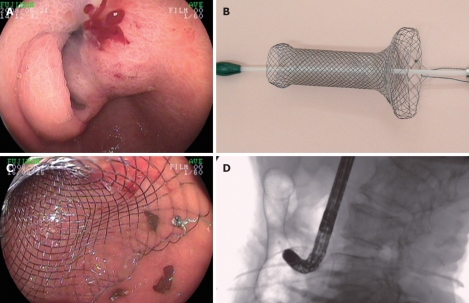
Figure 1.
Endoscopic photography taken immediately before (A) and after (C) deployment of stent, the corresponding newly designed big cup nitinol stent (B), X-ray photography (D) taken immediately after deployment of stent.
Stent
The proximal part of the newly designed stent (Figure 1B) contains a big cup with a length of 20 mm and a diameter 48-55 mm. The middle part is composed of a 60-mm-long segment with a diameter of 20 mm and the distal part presents a sphericity with a length of 20 mm and a diameter of 28 mm. Both the middle part and a half of proximal big cup segment are covered by a polyethylene membrane, but the rest part of the stent is not covered. The stent is mounted on a delivery system with an outer diameter of 6 mm and an overall length of 180 cm. The end of delivery system was adhered with 3 pieces of adhesive tape. The distance between two adhesive tapes in the neighborhood was 5 cm.
Procedure
The procedure was performed under endoscopic and fluoroscopic guidance as follows. The pharynx was sprayed with a topical anesthetic, lidocaine; meperidine was administered intravenously for sedation. The stomach was intubated with a endoscope (Fujinon EG 450HR, Japan) and the proximal and distal margins of the stricture were defined fluoroscopically by injection of nonionic contrast using a catheter passing through the accessory channel. Under endoscopic and fluoroscopic guidance, the locations of the proximal and the distal ends of the strictured segment were marked on the skin with metallic markers. Before implantation, an atraumatic, stiff guide wire was introduced via the endoscope through the stricture. If mild pressure was sufficient to pass the endoscope through the stricture, dilation was not performed. If there is complete obstruction, an atraumatic guide wire was placed endoscopically, and the stricture was dilated with a 15-mm diameter balloon catheter. When dilation was complete, the guide wire was exchanged for a super stiff metalic guide wire and then endoscope was removed with the guide wire left in place. Under fluoroscopic guidance, the delivery system was passed over the guide wire to a point slightly beyond the distal end of the stricture. Abdominal compression was used to aid advancement of the delivery system if necessary. This maneuver was helpful in preventing bending of the delivery device at particular locations such as the greater curvature of the stomach. If further assistance was needed to introduce the stent in patients with gastric outlet obstruction, the endoscope was reinserted to the stomach. The adhesive tape of delivery system was snatched up with a grasping forceps inserted through the endoscope accessory channel and the endoscope together with the delivery system was advanced across the stenotic region. When the stent within the delivery system was positioned between metallic markers on skin to indicate proximal and distal stricture margins, the outer sheath of the delivery system was slowly withdrawn to gradually release the stent and allowed it to lie within the stricture. With the guide wire left in place, the delivery system was removed. The endoscope is passed again to check the position of the proximal big cup of the stent (Figure 1C). If the stent was found in the correct position, the guide wire is removed. The fluoroscopic views were obtained immediately after stent placement (Figure 1D).
Follow-up study
After stent placement, the patients were arranged to resume oral intake of liquids within 24 h. The patients were not allowed to take a soft or solid diet until the follow-up showed full stent expansion. On the day after stent placement, barium contrast radiography was performed to document the position and the functionality of the stent. After this, the patients were called every month and inquired about what they ate and if there were any symptoms of obstruction such as pain and discomfort or vomiting after food intake. Follow-up barium study or endoscopy was carried out only in the patients with recurrent symptoms. The end point of this study was cessation of stent patency or patient death.
RESULTS
Stent implantation was successful in 12 patients with a technical success rate of 92.3%. All stents were transpyloric. However, one patient failed when we experienced the buckling of the delivery system in the proximal stomach and pushed over the super stiff guide wire through a narrow stenosis. All stents were 100 mm in length. The proximal port of placed stents ranged in diameter from 48 to 55 mm (mean 51.5 mm). Opacification showed that nitinol stents were integrated with sinus ventriculi residuary cavity in 11 of the 12 patients and barium could be emptied completely in all successful cases. No procedure-related complications occurred, such as perforation. Eleven of the 12 patients had relief of obstructive symptoms, allowing oral intake of liquids. One patient who was already in a pre-terminal stage (death occurred 4 wk after stent implantation), had episodes of vomiting, gastric distention, and tolerated just liquid intermittently, although radiological examination showed free passage of barium. The mean survival of all patients who eventually died was 6.5 mo (range 4 wk-12 mo).
Nine patients were able to eat soft or semi-solid diet and two patients were able to take liquid, and no migration and recurrent obstruction occurred during the follow-up period. However, one patient had hematemesis and melena 3 wk after stent placement. After proper treatment, the bleeding stopped.
DISCUSSION
Expandable metal stents have been used generally to treat malignant gastric strictures in recent years[1,2]. Lowe et al[3] thought that the primary treatment in all patients with inoperable gastric outlet obstruction should be gastroduodenal stenting. However, a major problem of the stents was that the conventional proximal ends were not designed according to the shape and diameter of sinus ventriculi residuary cavity, which was not suitable for roomy gastral cavity[3-6]. Stent occlusion in uncovered stents and migration in covered stents were also problematic[2,7]. Therefore, the newly designed stent was developed to solve the problem of the disadvantages of conventional metal stents. The proximal big cup of stent can prevent stent migration and contribute to passage of food, and the middle part of the stent can inhibit ingrowth. Compared with other studies[8-10], recurrent symptoms did not occur in our patients during a mean follow-up of 6.5 mo. Stent migration was not found. Because the shape and diameter of proximal big cup are similar to the ones of the proximol end of obstruction, the newly designed stent seems to be more appropriate for treating gastric outlet obstruction caused by stomach cancer than conventional one. In our study, opacification showed that the big cup nitinol stents were integrated with sinus ventriculi residuary cavity in 11 of the 12 patients and barium could be emptied completely in all successful cases. Moreover, the mean survival of the 12 patients who eventually died was 6.5 mo.
The placement of the stent was technically successful in 12 patients and failed in one patient, with a technical success of 92.3%. After stent placement, 11 patients were able to ingest liquids, with a clinical success of 91.7%. The results were comparable to those of other studies (90%-100% and 75%-94%, respectively)[1,3,10-15]. Although the newly designed stent has a proximal big cup, it did not increase the difficulty of placement. Nevertheless, we found that one patient with gastric bleeding 3 wk after stent placement might have been relative to the proximal big cup, for the bleeding site was confirmed to be located on the gastric mucosa close to the proximal end of the stent by endoscope.
In conclusion, the placement of the newly designed big cup nitinol stent offers good palliation for inoperable malignant gastric outlet obstruction resulting from stomach cancer. It suggests that it seems to be a reliable and safe therapeutic tool for gastric outlet obstruction for unresectable stomach cancers which are difficult to treat with conventional ones, although more cases are needed to be studied before any valid conclusions can be made. Proper techniques and settings should be followed to avoid any procedure-related complications.
COMMENTS
Background
Expandable metal stents have been used generally to treat malignant gastric strictures in recent years. However, a major problem of the stents was that the conventional proximal ends were not designed according to the shape and diameter of sinus ventriculi residuary cavity, which was not suitable for roomy gastral cavity. The authors designed a new big cup nitinol stent. It can not only overcome the migration and restenosis, but increase the emptying rate of sinus ventriculi.
Research frontiers
The newly designed stent was developed to solve the problems of the conventional metal stents. It can prevent the migration and restenosis for gastric outlet obstruction caused by stomach cancer.
Innovations and breakthroughs
A new big cup nitinol stent is designed on the basis of shape and dimension of remnant gastral cavity. The stent is obviously superior to the double-layered and conventional stents, for it is more appropriate for remnant gastric cavity.
Applications
The newly designed big cup nitinol stent can be used more appropriately for gastric outlet obstruction caused by stomach cancer compared with the double-layered and conventional stents.
Terminology
Big cup nitinol stent: The proximal part of the newly designed stent contains a big cup with a length of 20 mm and a diameter 48-55 mm. The middle part is composed of a 60-mm-long segment with a diameter of 20 mm and the distal part presents a sphericity with a length of 20 mm and a diameter of 28 mm.
Peer review
This article is interesting and can be better if a few corrections are made.
Footnotes
Peer reviewer: Ji Kon Ryu, Professor, Department of Internal Medicine, Seoul National University College of Medicine, 28 Yeongeon-dong, Jongno-gu, Seoul 110-744, South Korea
S- Editor Wang YR L- Editor Ma JY E- Editor Ma WH
References
- 1.Kim JH, Song HY, Shin JH, Hu HT, Lee SK, Jung HY, Yook JH. Metallic stent placement in the palliative treatment of malignant gastric outlet obstructions: primary gastric carcinoma versus pancreatic carcinoma. AJR Am J Roentgenol. 2009;193:241–247. doi: 10.2214/AJR.08.1760. [DOI] [PubMed] [Google Scholar]
- 2.Acunaş B, Poyanlí A, Rozanes I. Intervention in gastrointestinal tract: the treatment of esophageal, gastroduodenal and colorectal obstructions with metallic stents. Eur J Radiol. 2002;42:240–248. doi: 10.1016/s0720-048x(02)00031-1. [DOI] [PubMed] [Google Scholar]
- 3.Lowe AS, Beckett CG, Jowett S, May J, Stephenson S, Scally A, Tam E, Kay CL. Self-expandable metal stent placement for the palliation of malignant gastroduodenal obstruction: experience in a large, single, UK centre. Clin Radiol. 2007;62:738–744. doi: 10.1016/j.crad.2007.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Telford JJ, Carr-Locke DL, Baron TH, Tringali A, Parsons WG, Gabbrielli A, Costamagna G. Palliation of patients with malignant gastric outlet obstruction with the enteral Wallstent: outcomes from a multicenter study. Gastrointest Endosc. 2004;60:916–920. doi: 10.1016/s0016-5107(04)02228-x. [DOI] [PubMed] [Google Scholar]
- 5.Maetani I, Ukita T, Inone H, Yoshida M, Igarashi Y, Sakai Y. Knitted nitinol stent insertion for various intestinal stenoses with a modified delivery system. Gastrointest Endosc. 2001;54:364–367. doi: 10.1067/mge.2001.116882. [DOI] [PubMed] [Google Scholar]
- 6.Lee JM, Han YM, Kim CS, Lee SY, Lee ST, Yang DH. Fluoroscopic-guided covered metallic stent placement for gastric outlet obstruction and post-operative gastroenterostomy anastomotic stricture. Clin Radiol. 2001;56:560–567. doi: 10.1053/crad.2001.0700. [DOI] [PubMed] [Google Scholar]
- 7.Nevitt AW, Vida F, Kozarek RA, Traverso LW, Raltz SL. Expandable metallic prostheses for malignant obstructions of gastric outlet and proximal small bowel. Gastrointest Endosc. 1998;47:271–276. doi: 10.1016/s0016-5107(98)70326-8. [DOI] [PubMed] [Google Scholar]
- 8.Adler DG, Baron TH. Endoscopic palliation of malignant gastric outlet obstruction using self-expanding metal stents: experience in 36 patients. Am J Gastroenterol. 2002;97:72–78. doi: 10.1111/j.1572-0241.2002.05423.x. [DOI] [PubMed] [Google Scholar]
- 9.Soetikno RM, Lichtenstein DR, Vandervoort J, Wong RC, Roston AD, Slivka A, Montes H, Carr-Locke DL. Palliation of malignant gastric outlet obstruction using an endoscopically placed Wallstent. Gastrointest Endosc. 1998;47:267–270. doi: 10.1016/s0016-5107(98)70325-6. [DOI] [PubMed] [Google Scholar]
- 10.Kim JH, Song HY, Shin JH, Choi E, Kim TW, Jung HY, Lee GH, Lee SK, Kim MH, Ryu MH, et al. Metallic stent placement in the palliative treatment of malignant gastroduodenal obstructions: prospective evaluation of results and factors influencing outcome in 213 patients. Gastrointest Endosc. 2007;66:256–264. doi: 10.1016/j.gie.2006.12.017. [DOI] [PubMed] [Google Scholar]
- 11.Lee SM, Kang DH, Kim GH, Park WI, Kim HW, Park JH. Self-expanding metallic stents for gastric outlet obstruction resulting from stomach cancer: a preliminary study with a newly designed double-layered pyloric stent. Gastrointest Endosc. 2007;66:1206–1210. doi: 10.1016/j.gie.2007.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Aviv RI, Shyamalan G, Khan FH, Watkinson AF, Tibballs J, Caplin M, Winslett M. Use of stents in the palliative treatment of malignant gastric outlet and duodenal obstruction. Clin Radiol. 2002;57:587–592. doi: 10.1053/crad.2002.0934. [DOI] [PubMed] [Google Scholar]
- 13.Mosler P, Mergener KD, Brandabur JJ, Schembre DB, Kozarek RA. Palliation of gastric outlet obstruction and proximal small bowel obstruction with self-expandable metal stents: a single center series. J Clin Gastroenterol. 2005;39:124–128. [PubMed] [Google Scholar]
- 14.Lee KM, Choi SJ, Shin SJ, Hwang JC, Lim SG, Jung JY, Yoo BM, Cho SW, Kim JH. Palliative treatment of malignant gastroduodenal obstruction with metallic stent: prospective comparison of covered and uncovered stents. Scand J Gastroenterol. 2009;44:846–852. doi: 10.1080/00365520902929849. [DOI] [PubMed] [Google Scholar]
- 15.Cho YK, Kim SW, Hur WH, Nam KW, Chang JH, Park JM, Lee IS, Choi MG, Chung IS. Clinical outcomes of self-expandable metal stent and prognostic factors for stent patency in gastric outlet obstruction caused by gastric cancer. Dig Dis Sci. 2010;55:668–674. doi: 10.1007/s10620-009-0787-3. [DOI] [PubMed] [Google Scholar]