Abstract
18F-fluorodeoxyglucose positron emission/computed tomography (18F-FDG PET/CT) imaging, an established procedure for evaluation of malignancy, shows an increased 18F-FDG uptake in inflammatory conditions. We present three patients with abdominal pain and weight loss. Conventional imaging studies indicated that abdominal neoplasm and 18F-FDG PET/CT for assessment of malignancy showed multiple lesions with intense 18F-FDG uptake in abdomen of the three cases. However, the three patients were finally diagnosed with multi-site abdominal tuberculosis (TB). Of them, two were diagnosed with TB by pathology, one was diagnosed with TB clinically. They recovered after anti-TB therapy. Few reports on accumulation of 18F-FDG in abdominal TB are available in the literature. A high index of suspicion is necessary to achieve an early diagnosis and a better outcome of the disease.
Keywords: Abdominal tuberculosis, Differential diagnosis, 18F-fluorodeoxyglucose, Positron emission tomography/computed tomography, Malignancy
INTRODUCTION
Patients with abdominal mass caused by benign lesions such as infection and benign tumor are often encountered in daily clinical practice. Sometimes, it is difficult to differentiate them from malignancy with the conventional imaging techniques, such as ultrasonography, computed tomography (CT) and magnetic resonance imaging (MRI)[1-3]. In spite of the great success achieved by 18F-fluorodeoxyglucose positron emission tomography/CT (18F-FDG PET/CT) imaging in the evaluation of malignant disorders[4-6], 18F-FDG is not specific for malignant lesions, and can accumulate in inflammatory lesions with an increased glucose metabolism[7,8].
Abdominal tuberculosis (TB) may involve the gastrointestinal tract, peritoneum, mesenteric lymph nodes, liver, spleen, or genitourinary tract. Its presentations are nonspecific and its diagnosis is frequently elusive[9,10]. Since the presentations of multi-site abdominal TB are even more atypical and insidious, its definitive diagnosis requires a high index of suspicion, various laboratory findings, imaging modalities, and histologic exclusion of malignancy[9,10].
We present three patients with abdominal mass diagnosed as malignancy by ultrasonography and/or CT. 18F-FDG PET/CT also showed an increased activity. However, these three patients were finally diagnosed with multi-site abdominal TB.
CASE REPORT
Case 1
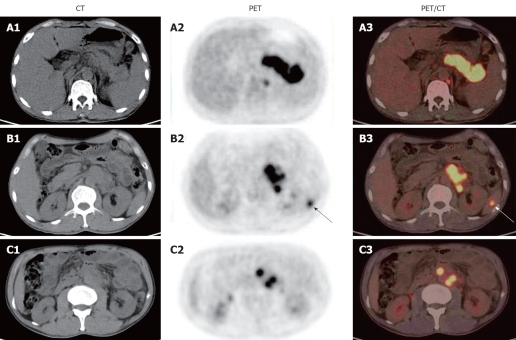
A 50-year-old male presented with a 4-mo history of left abdominal pain and body weight loss of about 6 kg in the past 2 mo. He had not any past clinical or radiological evidence of TB. Ultrasound examination imaging showed a mass behind the pancreatic body, multiple enlarged and confluent lymph nodes in retroperitoneal space and on the left side of abdominal aorta. Physical examination of the abdomen showed a slight tenderness in upper left abdominal area. Liver function tests, electrolytes, and complete blood count were normal. Whole-body 18F-FDG PET/CT scan demonstrated a mass-like area with an intense 18F-FDG uptake extending up behind the pancreatic body and tail, a focal area with an intense 18F-FDG uptake in spleen, multiple focal areas with an intense 18F-FDG uptake along the arcus minor ventriculi, around the abdominal aorta, and post crura diaphragm (Figure 1). Delayed 18F-FDG PET/CT scan was performed 120 min after 18F-FDG was injected into the patient. The maximal standardized uptake value (SUVmax) measurements of each tuberculous lesion were obtained both on early-(SUV1) and on delayed-scans (SUV2). Furthermore, we calculated the retention index (RI) of SUVmax (RI-SUVmax) from SUVmax according to the following formula: RI-SUVmax (%) = [SUV2 (delayed-phase) - SUV1 (early-phase)] × 100/SUV1 (early-phase). The images of delayed-scan demonstrated almost the same multiple areas with an intense 18F-FDG uptake. The SUVmax was increased in some lesions and decreased in others (Table 1), indicating that the patient has lymphoma or retroperitoneal tumor with multiple metastases. The subsequent laparoscopic biopsy of the mass extending up behind the pancreas and histopathological examination revealed TB in the patient (Figure 2).
Figure 1.
18F-fluorodeoxyglucose positron emission/computed tomography images of patient 1 showing a mass-like area with an intense 18F-fluorodeoxyglucose uptake extending up behind the pancreatic body and tail (A1-A3), a focal area with an intense 18F-fluorodeoxyglucose uptake in spleen (arrows) (B1-B3), and multiple focal areas with an intense 18F-fluorodeoxyglucose uptake around the abdominal aorta (C1-C3). CT: Computed tomography; PET: Positron emission tomography.
Table 1.
Maximum standardized uptake values and retention index of maximal standardized uptake value
| Lesion location | SUV1 | SUV2 | RI-SUVmax (%) |
| Patient 1 | |||
| Behind pancreas | 17.7 | 16.5 | -6.78 |
| In retroperitoneal space | 14.4 | 12.1 | -15.97 |
| In spleen | 6.7 | 9.2 | 37.31 |
| Patient 3 | |||
| In liver hilum | 13.2 | 15.3 | 15.91 |
| Near the pancreatic head | 13.7 | 12.8 | -8.03 |
| Peritoneum lesion | 13.9 | 14.3 | 2.88 |
| In retroperitoneal space | 12.4 | 11.8 | -4.84 |
SUV1: Maximal standardized uptake value obtained on early-scan; SUV2: Maximal standardized uptake value obtained on delayed-scan; RI-SUVmax: Retention index of maximal standardized uptake value [RI-SUVmax (%)] = (SUV2 - SUV1) × 100/SUV1.
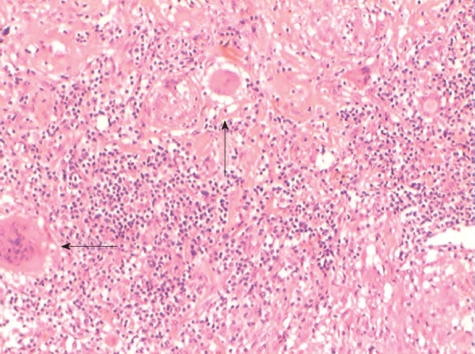
Figure 2.
Hematoxylin and eosin staining of laparoscopic biopsy specimen (× 200) from mass extending to behind the pancreas showing amorphous, eosinophilic and granular debris, as well as Langhans giant cells (arrows) in granulomas.
The patient was diagnosed with multi-site abdominal TB. Six months after anti-TB therapy, a second 18F-FDG PET/CT scan showed remission of all his prior lesions. Three weeks after anti-TB therapy, his abdominal pain disappeared and 10 mo after anti-TB therapy, his general condition including body weight loss was much improved.
Case 2
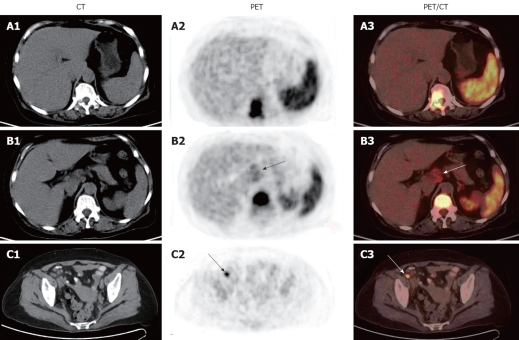
A 61-year-old female was admitted to our hospital due to right abdominal pain for 1 wk and a body weight loss of about 5 kg in the past 2 mo. The patient had a 3-year history of hypertension but no past clinical or radiological evidence of TB. Liver function tests, electrolytes, and complete blood count were normal. The serum levels of α-fetoprotein, carcinoembryonic antigen, carbohydrate antigen 50, carbohydrate antigen 125, carbohydrate antigen 153, and carbohydrate antigen 199 were normal. Ultrasound and abdominal CT showed a mass in the hepatic hilar region, and multiple enlarged lymph nodes around the abdominal aorta. Whole-body 18F-FDG PET/CT scan demonstrated multiple lesions with an intense 18F-FDG uptake in the hepatic hilar region, para-abdominal aorta, right iliac arterial region, thoracic and lumbar vertebrae (Figure 3), suggesting malignancy with multiple metastases. A biopsy of the 1st lumbar vertebra showed osteomyelitis (Figure 4A). Subsequently laparoscopic biopsy of the mass in hepatic hilar region and histopathological examination revealed TB (Figure 4B).
Figure 3.
18F-fluorodeoxyglucose positron emission/computed tomography images of patient 2 showing diffuse intense uptake of 18F-fluorodeoxyglucose in spleen and intense 18F-fluorodeoxyglucose uptake in thoracic vertebrae (A1-A3), a mass-like area with an intense 18F-fluorodeoxyglucose uptake in hepatic hilar region (arrows) and thoracic vertebrae (B1-B3), and a focal intense uptake of 18F-fluorodeoxyglucose in right iliac arterial region (arrows) (C1-C3). CT: Computed tomography; PET: Positron emission tomography.
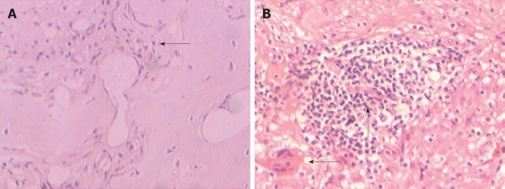
Figure 4.
Hematoxylin and eosin staining of the biopsy specimen from the 1st lumbar vertebra and the mass in hepatic hilar region showing thickened irregular bone trabeculae with a slight infiltration of lymphocytes and plasmocytes (arrow) (A), granulomatous lymphadenitis and amorphous, eosinophilic and granular debris, and Langhans giant cells in granulomas (arrows) (B).
The patient was diagnosed with multi-site abdominal and bone TB. Ten months after anti-TB therapy, a second 18F-FDG PET/CT scan showed remission of all her prior lesions. Two weeks after anti-TB therapy, her abdominal pain disappeared. Twelve months after anti-TB therapy, her general condition including body weight loss was much improved.
Case 3
A 37-year-old male presented with malaise and abdominal pain in the past 6 mo, as well a body weight loss of about 3 kg in the past 3 mo. He had not any past clinical or radiological evidence of TB. Ultrasound and abdominal CT showed multiple enlarged nodes in hepatic hilar region, pancreatic head, retroperitoneal space, and disorganization of the pancreatic head. Laboratory test showed an elevated white-cell count (15 250 per cubic millimeter) with an increased neutrophil differential count (12 060 per cubic millimeter). His serum biochemistry values, including liver-function test, were normal. Whole-body 18F-FDG PET/CT scan demonstrated multiple focal or lamellar lesions with an intense 18F-FDG uptake in hepatic hilar region, curvatura ventriculi minor, radix mesenterii region, retroperitoneal space, pancreatic body and tail, peritoneum, and around the pancreatic head (Figure 5), suggesting TB or cancer. Delayed 18F-FDG PET/CT scan, 112 min after 18F-FDG injection, demonstrated almost the same multiple areas with an intense 18F-FDG uptake. The SUVmax was increased in some lesions and decreased in others (Table 1). Blood tests showed an accelerated erythrocyte sedimentation rate of 96 mm/h. Based on the experience with the reported two patients, this patient was suspected to have TB, a Mantoux test was thus done. The size of induration on Mantoux test was 35 mm (strongly positive). The patient was diagnosed with multi-site abdominal TB.
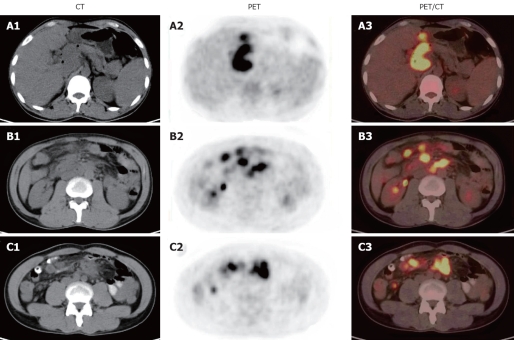
Figure 5.
18F-fluorodeoxyglucose positron emission/computed tomography images of patient 3 A showing a mass-like area with an intense 18F-fluorodeoxyglucose uptake in hepatic hilar region (A1-A3), multiple focal lesions (B1-B3) or multiple lamellar lesions (C1-C3) with an intense 18F-fluorodeoxyglucose uptake in peritoneal cavity, retroperitoneal space, and peritoneum. CT: Computed tomography; PET: Positron emission tomography.
Ten days after anti-TB therapy, his abdominal pain disappeared and his white-cell count returned to normal. A second 18F-FDG PET/CT scan 5 mo after anti-TB therapy showed remission of all his prior lesions. His treatment was terminated 4 mo after the second PET/CT. Nine months after anti-TB therapy, his general condition including body weight loss and malaise was much improved. Five months after anti-TB therapy, the patient was in good health.
DISCUSSION
Differentiation of TB from malignancy is very important, because the treatment modalities for them are different. Abdominal TB and malignancy often have common clinical features, such as weight loss, abdominal mass, and malaise. Overlap of symptoms of multi-site abdominal TB and metastatic carcinoma makes their differential diagnosis rather difficult and sometimes confusing. Histology is the only way of making its diagnosis as all available imaging methods are not sufficiently specific[1-3]. It has been shown that laparoscopic biopsy is a good diagnostic tool for doubtful abdominal TB[11]. Laparoscopic biopsy confirmed the diagnosis of abdominal TB in our two patients.
Few reports are available on 18F-FDG accumulation in abdominal TB lesions[12,13]. The abdominal appearance on TB 18F-FDG PET/CT image is nonspecific and various[12,13]. These 18F-FDG positive lesions are often proliferative lesions composed of epithelioid cells, Langhans giant cells, and lymphocytes. These cells highly metabolize glucose and show a high uptake of 18F-FDG. In this study, a focal accumulation pattern (Figure 1) and a diffuse accumulation pattern (Figure 3) of 18F-FDG were observed in spleen TB. Although a SUVmax, greater than 2.5, is attributed to malignant lesions[14], in this study, the peak SUVmax value was 17.7 for abdominal TB (include TB of the spleen, lymph nodes, and peritoneum) (Figures 1, 3 and 5). It has been shown that inflammatory lesions show an increased 18F-FDG washout on delayed images obtained 90-120 min after 18F-FDG injection, whereas cancerous lesions usually exhibit a further accumulation of tracer[15,16]. However, it was reported that TB exhibits a further accumulation of tracer, mimicking malignant lesions[17,18]. In our study, the SUVmax was reduced in some TB lesions and increased in others.
In conclusion, it is difficult to distinguish multi-site abdominal TB from malignancy even with 18F-FDG PET/CT. A high index of suspicion is necessary to achieve an early diagnosis and a better outcome of the disease.
Footnotes
Peer reviewer: Dr. Ram Prakash Galwa, MD, MBBS, Department of Diagnostic Imaging, The Ottawa Hospital, 751 Parkdale Avenue, Apartment 803, Ottawa, k1y1j7, Canada
S- Editor Wang YR L- Editor Wang XL E- Editor Zheng XM
References
- 1.Hu ML, Lee CH, Kuo CM, Huang CC, Tai WC, Chang KC, Lee CM, Chuah SK. Abdominal tuberculosis: analysis of clinical features and outcome of adult patients in southern Taiwan. Chang Gung Med J. 2009;32:509–516. [PubMed] [Google Scholar]
- 2.Daniel SV, Vani DH, Smith AM, Hill QA, Menon KV. Obstructive jaundice due to a pancreatic mass: a rare presentation of acute lymphoblastic leukaemia in an adult. JOP. 2010;11:72–74. [PubMed] [Google Scholar]
- 3.Mlika M, Farah F, Jarboui S, Abdessalem M, Zaouche A, Jilani SB, Zermani R. A benign cystic mass of the pancreas mimicking a malignant lesion. Pathologica. 2009;101:261–262. [PubMed] [Google Scholar]
- 4.Sun L, Su XH, Guan YS, Pan WM, Luo ZM, Wei JH, Zhao L, Wu H. Clinical usefulness of 18F-FDG PET/CT in the restaging of esophageal cancer after surgical resection and radiotherapy. World J Gastroenterol. 2009;15:1836–1842. doi: 10.3748/wjg.15.1836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee MJ, Yun MJ, Park MS, Cha SH, Kim MJ, Lee JD, Kim KW. Paraaortic lymph node metastasis in patients with intra-abdominal malignancies: CT vs PET. World J Gastroenterol. 2009;15:4434–4438. doi: 10.3748/wjg.15.4434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sun L, Su XH, Guan YS, Pan WM, Luo ZM, Wei JH, Wu H. Clinical role of 18F-fluorodeoxyglucose positron emission tomography/computed tomography in post-operative follow up of gastric cancer: initial results. World J Gastroenterol. 2008;14:4627–4632. doi: 10.3748/wjg.14.4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Makino I, Yamaguchi T, Sato N, Yasui T, Kita I. Xanthogranulomatous cholecystitis mimicking gallbladder carcinoma with a false-positive result on fluorodeoxyglucose PET. World J Gastroenterol. 2009;15:3691–3693. doi: 10.3748/wjg.15.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeh CL, Chen LK, Chen SW, Chen YK. Abnormal FDG PET imaging in tuberculosis appearing like mesothelioma: anatomic delineation by CT can aid in differential diagnosis. Clin Nucl Med. 2009;34:815–817. doi: 10.1097/RLU.0b013e3181b81e09. [DOI] [PubMed] [Google Scholar]
- 9.Xi X, Shuang L, Dan W, Ting H, Han MY, Ying C, Quan M, Chaoyang S, Zhilan C, Cui F, et al. Diagnostic dilemma of abdominopelvic tuberculosis:a series of 20 cases. J Cancer Res Clin Oncol. 2010:Epub ahead of print. doi: 10.1007/s00432-010-0842-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan CH, Kontoyiannis DP, Viswanathan C, Iyer RB. Tuberculosis: a benign impostor. AJR Am J Roentgenol. 2010;194:555–561. doi: 10.2214/AJR.09.3055. [DOI] [PubMed] [Google Scholar]
- 11.Chahed J, Mekki M, Mansour A, Ben Brahim M, Maazoun K, Hidouri S, Krichene I, Sahnoun L, Jouini R, Belgith M, et al. Contribution of laparoscopy in the abdominal tuberculosis diagnosis: retrospective study of about 11 cases. Pediatr Surg Int. 2010;26:413–418. doi: 10.1007/s00383-010-2555-z. [DOI] [PubMed] [Google Scholar]
- 12.Shimamoto H, Hamada K, Higuchi I, Tsujihata M, Nonomura N, Tomita Y, Okuyama A, Aozasa K, Hatazawa J. Abdominal Tuberculosis: peritoneal involvement shown by F-18 FDG PET. Clin Nucl Med. 2007;32:716–718. doi: 10.1097/RLU.0b013e318123f813. [DOI] [PubMed] [Google Scholar]
- 13.Takalkar AM, Bruno GL, Reddy M, Lilien DL. Intense FDG activity in peritoneal tuberculosis mimics peritoneal carcinomatosis. Clin Nucl Med. 2007;32:244–246. doi: 10.1097/01.rlu.0000255239.04475.c2. [DOI] [PubMed] [Google Scholar]
- 14.Low VJ, Delbeke D, Coleman RE. Applications of PET in oncologic imaging. In: Sandler MP, Coleman RE, Patton JA, Wackers FJ, Gottschalk A, et al., editors. Diagnostic nuclear medicine. 4th ed. Philadelphia: Lippincott Williams and Wilkins; 2003. pp. 987–1014. [Google Scholar]
- 15.Zhuang H, Pourdehnad M, Lambright ES, Yamamoto AJ, Lanuti M, Li P, Mozley PD, Rossman MD, Albelda SM, Alavi A. Dual time point 18F-FDG PET imaging for differentiating malignant from inflammatory processes. J Nucl Med. 2001;42:1412–1417. [PubMed] [Google Scholar]
- 16.Matthies A, Hickeson M, Cuchiara A, Alavi A. Dual time point 18F-FDG PET for the evaluation of pulmonary nodules. J Nucl Med. 2002;43:871–875. [PubMed] [Google Scholar]
- 17.Laffon E, de Clermont H, Begueret H, Vernejoux JM, Thumerel M, Marthan R, Ducassou D. Assessment of dual-time-point 18F-FDG-PET imaging for pulmonary lesions. Nucl Med Commun. 2009;30:455–461. doi: 10.1097/MNM.0b013e32832bdcac. [DOI] [PubMed] [Google Scholar]
- 18.Lee IS, Lee JS, Kim SJ, Jun S, Suh KT. Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography imaging in pyogenic and tuberculous spondylitis: preliminary study. J Comput Assist Tomogr. 2009;33:587–592. doi: 10.1097/RCT.0b013e318187fef8. [DOI] [PubMed] [Google Scholar]