Abstract
Objectives
To determine the effectiveness of the heart failure screening form in teaching heart failure treatment guidelines and prompting students to evaluate patients' medications to initiate patient education and provider intervention.
Design
Between 2002 and 2009, 123 students used the heart failure screeing form during an elective cardiology advanced pharmacy practice experience (APPE). A subset of 41 students were also assessed for change in heart failure knowledge and confidence pre- and post-APPE.
Assessment
A total of 1,114 heart failure patients were screened and assessed using the tool with a mean age of 71.9 ± 12.9 years. Of those, 535 (48%) patients met screening criteria and participated in heart failure education. From 2008 through 2009, there were 45 heart failure interventions with a 60% provider acceptance rate. Significant improvements were made in heart failure knowledge and in all areas of confidence at the end of the APPE for the 41 students assessed.
Discussion
The heart failure screening form is an effective tool to teach evidence-based medicine and to prompt students to initiate provider intervention and patient education. Its use is associated with significant increases in knowledge and confidence in heart failure medication therapy management in fourth-year pharmacy students.
Keywords: heart failure, cardiology, advanced pharmacy practice experience
INTRODUCTION
Heart failure treatment guidelines have been successful in delineating the standards for managing inpatient medications and patient education. According to the European Society of Cardiology (ESC) Guidelines for the Diagnosis and Treatment of Heart Failure, hospitalized patients with heart failure should understand indications, dosing, and effects of drugs, and should recognize the common side effects of each drug prescribed.1 The ESC guidelines also emphasize that patients should understand the importance of adherence and maintain motivation to follow the treatment plan. In the 2009 focused update of the American College of Cardiology Foundation (ACCF) and American Heart Association (AHA) Guidelines for the Diagnosis and Management of Heart Failure in Adults, a new set of guidelines for hospital patients was introduced.2 These guidelines state that medications should be reconciled for every patient and adjusted appropriately on admission to and discharge from the hospital (class IC recommendation), and that comprehensive written discharge instructions for all patients with a hospitalization for heart failure and their caregivers are strongly recommended (class IC recommendation), with special emphasis on the following 6 aspects of care: diet; discharge medications, with a special focus on adherence, persistence, and dose titration to recommended doses of angiotensin converting enzyme (ACE) inhibitors and beta-blockers; activity level; follow-up appointments; daily weight monitoring; and actions to take if symptoms worsen.
To meet these guidelines and improve outcomes, pharmacists must play a role in the management of heart failure in a hospital setting. Depending on the institution, pharmacist involvement may encompass medication reconciliation, medication therapy management (pharmacist-directed or collaborative), and/or patient education. A systematic review of 12 randomized trials showed that pharmacists' care of heart failure patients was associated with significant reductions in the rate of all causes of hospitalizations (OR 0.71; 95% CI 0.54-0.94).3
Heart failure is a complex disease state requiring clinical skills development for appropriate evaluation and treatment. To better prepare pharmacy students to fulfill this role after graduation, a screening tool, the heart failure screening form, was created and implemented. The purpose of the form was to provide students with a systematic method of applying the heart failure clinical guidelines to actual heart failure patients, thereby: (1) implementing evidence-based medicine in their APPE experiences, and (2) increasing the knowledge base of heart failure and appropriate care, including proper medication therapy. The heart failure screening form was used also to prompt pharmacy students to initiate patient education and provider intervention. The tool supported the Accreditation Council for Pharmaceutical Education (ACPE) pharmaceutical care educational outcome “to design, implement, monitor, evaluate, and adjust pharmaceutical care plans that are patient-specific and evidence-based,” and the Center for Advancement of Pharmacy Education (CAPE) educational outcome “formulate a patient-centered pharmaceutical care plan in collaboration with other health care professionals, patients, and/or their caregivers.”4,5
This tool has been used at our 672-bed, private, non-profit, locally-owned community medical center since 2002 during an elective cardiology APPE. The purpose of this report is to present the heart failure screening form and how it was developed, summarize patient and student outcomes related to the use of the tool, and discuss the potential to develop a similar tool for patients with other chronic diseases.
DESIGN
The study was reviewed by the Creighton University Institutional Review Board and deemed exempt. The heart failure screening form was a guide for pharmacy students to follow when evaluating heart failure patients while on elective cardiology APPEs. The form, developed in 2002, was originally based on the ACC/AHA Guidelines for the Evaluation and Management of Chronic Heart Failure in the Adult published in 2001, and included input from regional experts who reviewed the tool and provided feedback prior to implementation.6
The top portion of the screening form included demographic information about the patient and the patient's physician. The screening information section of the form consisted of 13 items. Taken directly from the 2001 ACC/AHA guidelines, the authors deemed them to be the most significant aspects for a pharmacist to consider when evaluating and monitoring a patient with heart failure.6 These 13 items were worded so that if any of the items were checked “Yes,” further investigation would be required. The 13 key indicators on the form included: medication-related admission; taking 7 or more scheduled medications; taking 2 or more medications in the same class; a serum creatinine > 2.5 mg/dl; a serum potassium > 5.6 or < 3.0 mEq/l; absence of angiotensin converting enzyme (ACE) inhibitor or angiotensis receptor blocker (ARB) therapy; absence of beta-blocker therapy; length of stay > 5 days; taking alpha blocker for hypertension treatment; not on target dose of ACE-inhibitor, taking 1 or more negative inotrope drugs; taking a class I antiarrhythmic; and New York Heart Association (NYHA) class III or IV and not receiving an aldosterone antagonist. In addition, the comments section of the form allowed space to write notes to clarify answers. The bottom portion of the form was used to record when the patient was educated about their heart failure drugs as well as a record of the physician intervention to rectify any of the 13 items marked “Yes.”
Because our institution is private and not directly affiliated with a college or school of pharmacy or medicine, pharmacy students in APPEs were assigned a certain number of patients in the cardiac unit to follow each day. All patients in this unit were followed by a provider from a partnering private cardiology practice consisting of 11 cardiologists, 2 cardiovascular surgeons, and 10 midlevel providers (3 physician assistants and 7 nurse practitioners). Students were required to monitor the drug therapy of those patients. While emphasis was placed on drug therapy, students were also required to be familiar with each patient's basic disease state(s), as well as significant laboratory values, diagnostic procedures, and/or therapeutic interventions. After initial work-up, students were required to use the heart failure screening form for all patients who met any of the following 3 criteria: (1) diagnosis of heart failure (systolic or diastolic), (2) left ventricular ejection fraction (LVEF) ≤ 40%, (3) diagnosis of cardiomyopathy.
If a patient met any of the above criteria, the form was used by the student to assess heart failure therapy. In addition to collecting baseline demographic data, students were prompted to evaluate the medication regimen to see if provider intervention was warranted and if counseling should be performed. If the student answered yes to any of the 13 key indicators, he or she was responsible for looking more closely at the patient's medical record and discussing the case with the medical staff. If a sound clinical reason could not be found by the student, he or she discussed with the preceptor the possibility of writing an intervention to the patient's provider to reconcile the issue. In addition, this form prompted the students to perform heart failure medication education prior to discharge unless there were extenuating circumstances (death, significant cognitive impairment, patient refusal, hospice, etc). This education was in addition to education performed by the nursing staff.
After independently evaluating the patients with the tool on rounds, students met with the preceptor for daily informal case presentations. These presentations occurred either at the patient's bedside with the chart readily available, or at scheduled preceptor meetings. If the heart failure screening form also had prompted a physician intervention, the student indicated this during the presentation of the plan for that patient. The preceptor carefully reviewed the recommendation for appropriateness. If approved, the intervention was communicated to the provider using the hospital-wide pharmacy communication form. Interventions of an urgent nature were also communicated by telephone call to the provider. The date of the intervention, purpose, and acceptance of the intervention were documented on the heart failure screening form. Students were asked to turn in the forms only after they had documented whether or not the intervention was accepted.
If patient education was warranted, students completed counseling prior to patient discharge and documented the event on the tool and in the patient's electronic medical record. Pharmacy student heart failure patient education encompassed a thorough explanation of each heart failure medication including purpose, use, side effects, and interactions. Students also discussed sodium and fluid intake, weight monitoring, and when the patient should call his/her provider.
To optimize use of the tool, the authors found that sufficient oral and written explanation at the beginning of the APPE were required as well as reinforcement during the first few weeks. At the beginning of an APPE, students typically underutilized the tool in fear that their patients did not meet the inclusion criteria for intervention or counseling. Once faculty members emphasized that the primary purpose of the tool was to aid in education, students used it more frequently.
Patient screening and counseling data were captured from 123 students from June 2002 through April 2009 during the elective cardiology APPE at BryanLGH Medical Center East in Lincoln, NE. Provider intervention data (the number of interventions, type of intervention, and whether they were accepted) were captured in a subset of 38 students between June 2008 and November 2009.
Data assessing student outcomes using the tool were captured between March 2005 and October 2006 in a subset of 41 students. Background information including age, gender, and number of APPEs completed prior to the cardiology elective were captured. Student knowledge was assessed using a written, 10-question, 10-point, multiple-choice examination given both on the first day and the last day of the APPE. The examination was developed based on current, evidence-based clinical guidelines to test students' knowledge of managing heart failure medication therapy. Prior to use in the APPE, the examination was tested in a pilot group of pharmacists during a continuing education conference.
Students' confidence to manage heart failure medication therapy and deliver patient education was also measured on the first and last days of the APPE using a 5-point Likert ranking scale with 1 being least confident and 5 being most confident. Students were asked to rate their confidence in the following 5 areas:
(1) Differentiation of acute heart failure versus chronic heart failure.
(2) Discussion of a basic treatment regimen for acute heart failure patients.
(3) Discussion of a basic treatment regimen for chronic heart failure patients.
(4) Assessment of heart failure treatment and ability to make recommendations.
(5) Ability to educate heart failure patients regarding drug therapy.
All results were de-identified, entered into a spreadsheet, and analyzed using SPSS version 18 (SPSS, Chicago, IL). Change in heart failure knowledge and confidence were analyzed by subtracting the difference (pre-post) scores and using 2-tailed paired t tests. Thus, a negative difference indicated an improvement for the parameter measured. Correlations between baseline demographics of student age and number of prior APPEs and change in heart failure knowledge and confidence were assessed using Pearson's correlation. A p value ≤ 0.05 was considered significant.
EVALUATION AND ASSESSMENT
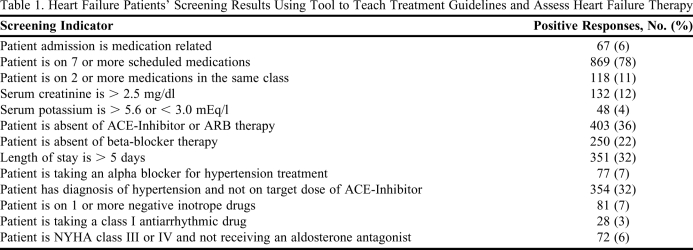
Between June 2002 and April 2009, 1,114 patients with a mean age of 71.9 ± 12.9 years were screened and accessed using the tool. The results of the initial screening of these patients are depicted in Table 1. The most common criterion prompting further evaluation and counseling by students was with patients on 7 or more scheduled medications (78%). This was followed by the absence of ACE-I or ARB therapy (36%), not on the target dose of ACE-I (32%), and a length of stay > 5 days (32%). During this time, 535 (48%) of the patients evaluated met criteria and underwent counseling by pharmacy students.
Table 1.
Heart Failure Patients' Screening Results Using Tool to Teach Treatment Guidelines and Assess Heart Failure Therapy
Abbreviations: ACE = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker; NYHA = New York Heart Association
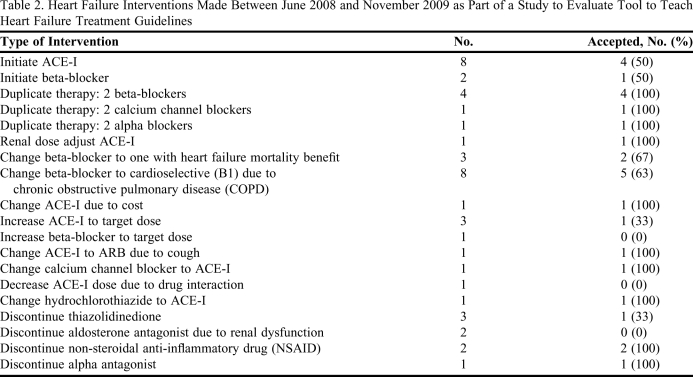
Between June 2008 and November 2009, 272 written provider interventions were made for cardiac patients in the unit, including both heart failure and non-heart failure. Providers accepted the recommendations in 114 patients (42%). Examples of non-heart failure interventions included renal adjustments, anticoagulation monitoring, drug interactions, and antibiotic kinetics. Of these, 45 interventions involved heart failure and were prompted by the tool. Providers accepted 27 (60%) of the heart failure interventions. Table 2 summarizes the heart failure interventions.
Table 2.
Heart Failure Interventions Made Between June 2008 and November 2009 as Part of a Study to Evaluate Tool to Teach Heart Failure Treatment Guidelines
Abbreviations: ACE = angiotensin converting enzyme inhibitor; ARB = angiotensin receptor blocker
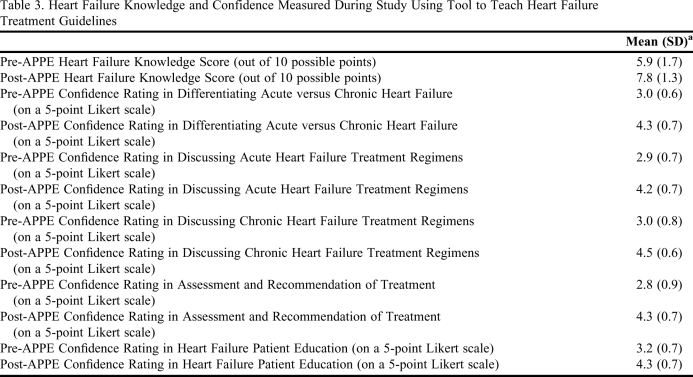
Of the 41 students assessed for knowledge and confidence, the mean age was 29.5 ± 7.4 years with 36.6% male and a mean of 4.2 ± 3.1 APPEs completed prior to the cardiology elective. Tables 3 and 4 summarize the mean scores and mean change in both knowledge and confidence of heart failure. Significant improvements were made in heart failure knowledge and in all areas of heart failure confidence. By the end of the APPE, students scored a mean of 7.8 points out of 10 in heart failure medication knowledge. For all confidence statements, the mean response was at least in agreement (4 on a 5-point scale) of the statement of confidence.
Table 3.
Heart Failure Knowledge and Confidence Measured During Study Using Tool to Teach Heart Failure Treatment Guidelines
a5-point Likert scale score: 1 = strongly disagree, 2 = disagree, 3 = undecided, 4 = agree, 5 = strongly agree
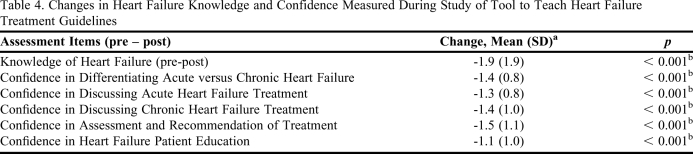
Table 4.
Changes in Heart Failure Knowledge and Confidence Measured During Study of Tool to Teach Heart Failure Treatment Guidelines
a5-point Likert scale score: 1 = strongly disagree, 2 = disagree, 3 = undecided, 4 = agree, 5 = strongly agree
bCorrelation is significant at the 0.01 level (2-tailed)
A correlation (Pearson coefficient -0.368, p = 0.020) existed between the number of completed APPEs prior to cardiology and the change in heart failure knowledge. A correlation also existed between the number of completed APPEs prior to cardiology and confidence in the ability to discuss chronic heart failure treatment (-0.379, p = 0.016). Because changes in knowledge and confidence were measured pre- minus post-intervention, these negative correlations indicated that students with more APPE experience were more likely to improve in the areas of heart failure knowledge and confidence in the ability to discuss chronic heart failure.
DISCUSSION
For interventions prompted mainly by the use of this form, the provider acceptance rate was close to 60%. Previous literature reports for pharmacy students in institutions where pharmacists do not round with the team, eg pharmacist-directed care, an average of 54.2% of written recommendations are accepted, compared to 82.8% of oral recommendations as part of collaborative care.7 Therefore, systems to optimize the number of interventions detected by students become important in institutions where students are not rounding with other providers.
Screening tools like the Heart Failure Screening Form increase the number of drug-related problems identified by both pharmacists and pharmacy students.8 Snyder, Lee et al demonstrated that a tool to assist with geriatric medication therapy review increased the number of identified drug problems when compared to not using the tool in sample cases.
In a previous analysis of pharmacy student interventions, the most common inpatient student intervention involved dosage (wrong dosage, inappropriate frequency, inappropriate duration, incorrect storage or incorrect administration), followed by adverse drug reaction (toxicity, allergic reaction, incorrect administration, drug-drug interaction, drug-disease interaction, drug-food interaction, or side effect), and drug product selection (drug needed but not prescribed, drug prescribed but not needed, drug duplication, cost of therapy, or ease of use).9 This study did not include patient education as a reason for intervention. In another study evaluating clinical interventions by pharmacy students, patient education was the most common reason for pharmacy intervention, followed by additional drug needed and laboratory test needed.10
The number of student interventions on clinical APPEs varies. Dennehy et al found that students performed 4.3 interventions per week and that interventions involving optimization of drug therapy were the most frequent.11 Students' interventions were accepted by physicians 92.5% of the time. Other reports have found the number of student interventions range from 2.9 to 5.5 per week.12-14
Optimizing pharmacy student provider interventions is important not only from a pedagogical standpoint, but also may lead to a cost avoidance and/or cost savings for the hospital.11, 15 Dennehy et al calculated a net drug cost savings of $578.75 per student over a 15-day study period.11 Brockmiller found an annualized total cost benefit of $354,752, of which $255,421 was cost savings and $99,332 was cost avoidance from pharmacy student drug therapy recommendations.15
The heart failure screening form was associated with significant improvements in both heart failure knowledge and in all areas of heart failure confidence. Of interest, a correlation existed between the number of completed APPEs prior to the cardiology elective and both the change in heart failure knowledge and confidence in the ability to discuss chronic heart failure treatment. Thus, more clinical experience prior to an APPE was associated with greater improvements in heart failure knowledge and confidence in chronic heart failure.
While not a measured outcome for this study, the more experience students have in a hospital setting, the more effective they are at evaluating patients and generating provider interventions. Dennehy et al demonstrated in a 6-week inpatient APPE that on average, pharmacy students each performed 1.8, 4.9, and 6.2 interventions per week in weeks 1, 3, and 5, respectively, of their APPE (p = 0.042).11 The authors could not state with certainty that the increase in intervention numbers were definitely due to advancement of student learning. They suggested that increased familiarity with the institution and the reporting form could have played a role.
The heart failure screening form is a tool used to apply systematically the clinical guidelines in everyday practice. The general format of the tool is not specific to the condition of heart failure, but can be adopted for use in other chronic disease management settings. Chronic conditions such as asthma, chronic obstructive pulmonary disease (COPD), diabetes mellitus, human immunodeficiency virus, coronary artery disease, and many others could use a similar format to teach pharmacy students how to apply the clinical guidelines to everyday practice. For pharmacists, the tool worked well when multiple drugs and laboratory assessments were essential to the appropriate medication therapy management of a patient. The tool can be modified to fit the needs of a specific institution and/or to prompt students to educate patients on specific disease state topics that relate to the boxes checked in the “screening information” section. Additionally, the tool can be used as a reliable source of data collection on student progress throughout an APPE.
There are limitations to the data due to the self-reported nature of the collection process. This could introduce reporter bias as well as under- or overreporting, due to the time involved in completing the form. However, it should be noted that heart failure assessment comprised 40% percent of the students' final grade for the APPE under the category of medication therapy management. Also, because this tool was evaluated only at 1 private, not-for-profit institution, its effectiveness at other institutions may be different. We cannot be certain that the tool alone contributed to the students' improved knowledge and confidence of heart failure as they were receiving other information about the disease simultaneously. Last, even though students were required to complete the heart failure screening form on all patients admitted to any of the beds they were following, it is reasonable to assume that the numbers reported in this manuscript do not encompass every heart failure patient admitted to the medical center during the study period.
CONCLUSION
When used in cardiology APPEs, the heart failure screening form is an effective tool to educate students on evidence-based medicine. The tool prompted students to initiate provider intervention and patient education. Its use also demonstrated increased knowledge and confidence in heart failure medication therapy management for fourth-year pharmacy students. Students with greater clinical experience prior to this cardiology APPE were associated with improved heart failure knowledge and confidence in chronic heart failure. While this tool will need to be updated as evidence-based guidelines change, its use continues at our practice site as an important part of the elective cardiology APPE.
REFERENCES
- 1.Dickstein K, Cohen-Solal A, Filippatos , et al. European society of cardiology guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur J Heart Fail. 2008;29(19):2388–2442. doi: 10.1093/eurheartj/ehn309. [DOI] [PubMed] [Google Scholar]
- 2.Jessup M, Abraham WT, Casey DE, et al. 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults. J Am Coll Cardiol. 2009;53(15):1–40. doi: 10.1161/CIRCULATIONAHA.109.192064. [DOI] [PubMed] [Google Scholar]
- 3.Koshman SL, Charrois TL, Simpson SH, McAlister FA, Tsuyuki RT. Pharmacist care of patients with heart failure: a systematic review of randomized trials. Arch Intern Med. 2008;168(7):687–694. doi: 10.1001/archinte.168.7.687. [DOI] [PubMed] [Google Scholar]
- 4. Accreditation Council for Pharmacy Education. Accreditation Standards. http://www.acpe-accredit.org/deans/standards.asp. Accessed May 27, 2010.
- 5. American Association of Colleges of Pharmacy, Center for the Advancement of Pharmaceutical Education. http://aacp.org/resources/education/Pages/CAPEEducational Outcomes.aspx. Accessed May 27, 2010.
- 6.Hunt SA, Baker DW, Chin MH, et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult: executive summary: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (committee to revise the 1995 guidelines for the evaluation and management of heart failure) Circulation. 2001;104(24):2996–3007. doi: 10.1161/hc4901.102568. [DOI] [PubMed] [Google Scholar]
- 7.Pound MW, Miller SM. Written versus oral recommendations made by pharmacy students during internal medicine rounds. Ann Pharmacother. 2007;41(5):772–776. doi: 10.1345/aph.1H668. [DOI] [PubMed] [Google Scholar]
- 8.Snyder Lee S, Schwemm A, Reist J, et al. Pharmacists' and pharmacy students' ability to identify drug-related problems using TIMER (tool to improve medications in the elderly via review) Am J Pharm Educ. 2009;73(3) doi: 10.5688/aj730352. Article 110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MacKinnon GE. Analysis of pharmacy student interventions collected via an internet based system. Am J Pharm Educ. 2003;67(3) Article 90. [Google Scholar]
- 10.Reddick JB, Murphy JE. Evaluating the clinical interventions of students during clerkships using a cognitive services claim form. Am J Pharm Educ. 2000;64(1):38–43. [Google Scholar]
- 11.Dennehy CE, Kroon LA, Byrne M, Koda-Kimble MA. Increase in number and diversity of clinical interventions by PharmD students over a clerkship rotation. Am J Pharm Educ. 1998;62(4):373–379. [Google Scholar]
- 12.Slaughter RL, Erickson SR, Thomson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 2004;28(5):665–669. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 13.Chisholm MA, Hawkins DW, Taylor AT. Providing pharmaceutical care: are pharmacy students beneficial to patients? Hosp Pharm. 1997;32(3):371–373. [Google Scholar]
- 14.Chisholm MA, Hawkins DW. Analysis of pharmacotherapy recommendations provided by doctor of pharmacy clerkship students. J Pharm Teach. 1996;5(4):3–12. [Google Scholar]
- 15.Brockmiller H, Abel SR, Koh-Knox CP, Birk CW. Cost impact of PharmD candidates' drug therapy recommendations. Am J Health-Syst Pharm. 1999;56(9):882–884. doi: 10.1093/ajhp/56.9.882. [DOI] [PubMed] [Google Scholar]