Abstract
Objectives
To determine if the addition of a student-supported venous thromboembolism risk assessment strategy could improve rates of venous thromboembolism prophylaxis at a community teaching hospital.
Methods
After receiving education and training on venous thromboembolism risk assessment, students assessed patients and recommended therapy in a 493-bed community teaching hospital over 5 weeks. Both the quantity and quality of venous thromboembolism prophylaxis were measured and compared to a baseline rate.
Results
One hundred three recommendations were made to physicians with a 41% acceptance rate. Compared to previous rates, the percentages of patients receiving “any,” “suitable,” and “optimal” venous thromboembolism prophylaxis increased from 70.5% to 82.7% (p = 0.0005), 64.4% to 75.9% (p = 0.0022), and 56.3% to 68.5% (p = 0.0022), respectively.
Conclusions
A student-supported venous thromboembolism risk assessment strategy resulted in an increase in venous thromboembolism prophylaxis rates and could be used as a model for other institutions to integrate students into population-based care.
Keywords: pharmacy student, advanced pharmacy practice experience, venous thromboembolism
INTRODUCTION
Pharmacy education standards, adopted in 2006 by the Accreditation Council for Pharmacy Education (ACPE), require pharmacy students to provide population-based care involving the development and implementation of population-specific disease management programs and protocols.1 Pilot programs are needed that demonstrate appropriate integration of pharmacy students into health systems to enhance existing clinical services and provide added value. To address this challenge, a pilot program was created highlighting a specific population-based clinical service, which might eventually serve as a new type of advanced pharmacy practice experience (APPE) for pharmacy students.
This pilot program was conducted in a 493-bed community teaching hospital and focused on the evaluation of patients at risk for developing venous thromboembolism and the provision of appropriate prophylaxis recommendations. The American College of Chest Physicians (ACCP) recommends the implementation of an evidence-based thromboprophylaxis strategy at every institution.2 The Institute for Clinical Systems Improvement (ICSI) further defines these recommendations by proposing to: (1) increase the percentage of hospitalized adult patients who are assessed appropriately for venous thromboembolism risk within 24 hours of admission, and (2) increase the percentage of hospitalized adult patients receiving appropriate pharmacological and/or mechanical prophylaxis treatment within 24 hours of admission.3 The underuse of appropriate venous thromboembolism prophylaxis has been well documented, and hospitals have tried a variety of strategies to improve their rates of prophylaxis, including utilization of computerized alerts to physicians.4-8
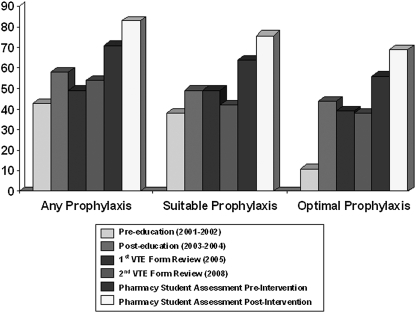
Several actions had been attempted previously at this institution to increase both the quantity and quality of venous thromboembolism prophylaxis (Figure 1). In 2004, only 43% of medical patients received venous thromboembolism prophylaxis.7 A clinical pharmacy education program was developed to educate medical house staff, nurses, and pharmacists on the importance of venous thromboembolism prophylaxis in medically ill patients through educational presentations, newsletters, quality assurance programs, and direct-patient care venous thromboembolism recommendations.8 With the addition of an educational program, venous thromboembolism prophylaxis rates increased to 58%. In 2005, a multi-disciplinary team created a venous thromboembolism prophylaxis order form. Physicians were not required but were encouraged to use the form. The form was combined with an educational component focused on the assessment tool; however, after 8 months, no changes in venous thromboembolism prophylaxis rates were observed. In January 2008, a subsequent analysis of the venous thromboembolism order form found 54% of patients receiving any form of venous thromboembolism prophylaxis. The objective of this study was to determine if the addition of a pharmacy student-supported strategy could improve the quantity and quality of the overall venous thromboembolism prophylaxis rates.
Figure 1.
Previous VTE prophylaxis rates. Definitions for VTE Endpoints: Any = Any pharmacologic or mechanical attempt to prophylaxis against VTE; Suitable = UFH 5,000 units BID or TID, any recommended dose of LMWH; Optimal = Recommendations per institution's VTE form (UFH 5,000 units TID and appropriately dosed LMWH). Abbreviations: VTE = venous thromboembolism embolism; BID = two times daily; TID = three times daily; UFH = unfractionated heparin; LMWH = low molecular weight heparin.
METHODS
This was a prospective, non-randomized, cohort trial. The methods described in this project were approved by the institutional review board at the hospital. Students participating in APPEs at this institution were educated on how to evaluate appropriately a patient's venous thromboembolism risk and provide recommendations for prophylaxis. All recommendations were reviewed by a licensed pharmacist before discussing with a physician. The primary clinical endpoint was the rate of venous thromboembolism prophylaxis compared to previously collected rates. Additional endpoints included the total numbers of patients assessed for risk, patients in need of prophylaxis, and venous thromboembolism recommendations provided. Secondary clinical endpoints that assessed the quality of venous thromboembolism prophylaxis included the number of patients receiving “any,” “suitable,” and “optimal” venous thromboembolism prophylaxis. “Any” prophylaxis was defined as any pharmacologic or mechanical attempt to prophylaxis against venous thromboembolism. “Suitable” prophylaxis was defined as unfractionated heparin (UFH) 5,000 units twice or 3 times daily or low molecular weight heparin (LMWH). “Optimal” prophylaxis was defined as UFH 3 times daily or an appropriately dosed LMWH. Despite the level of venous thromboembolism risk, mechanical prophylaxis was deemed appropriate if patients were at risk of bleeding as documented by a physician or had an active bleed. Patients already receiving pharmacological prophylaxis at the time of assessment were also evaluated for potential harm, and recommendations to discontinue therapy could also be suggested if deemed inappropriate.
All adult patients admitted to general medicine units were evaluated on weekdays for venous thromboembolism risk. Patients were excluded from risk assessment for the following reasons: receipt of therapeutic anticoagulation; patients in the labor and delivery units; age less than 18 years; patients transferred from another unit; orthopedic patients; palliative care patients; and patients enrolled in other studies. Orthopedic patients were excluded because admission to this area included a risk assessment tool and prophylaxis order set within the admission packet. Patients were excluded from the study outcomes analysis if their length of stay was less than 48 hours. Patients enrolled in other studies were excluded because pharmacy students did not have access to other study protocols.
For a 5-week period between February and March 2008, patient censuses from each nursing division were obtained daily, and new admissions were screened using the venous thromboembolism risk assessment tool. Venous thromboembolism risk assessment involved identifying risk factors in each patient, looking for contraindications to prophylaxis that may have been present, and assessing the appropriateness of current prophylaxis. Students presented these recommendations to a pharmacy resident or preceptor before providing the recommendations to a physician. When physicians were not immediately available for a direct recommendation, a pharmacy communication form was placed in the chart for physician review. Additionally, venous thromboembolism risk factors present in each patient were highlighted on the patient's risk assessment form.
Students were educated in several ways prior to participating in the venous thromboembolism program. First, students were given a reading assignment that consisted of selected pages from the 2004 ACCP guidelines on prevention of venous thromboembolism.2 Students then participated in a discussion on the topic led by a pharmacy resident and preceptor, after which time they completed an online ACPE continuing education program on preventing and managing venous thromboembolism.9 A pharmacy resident or preceptor then modeled the risk assessment process for each student on the patient floors.
Prior to any onsite student education, students were given a quiz to assess their previous knowledge on venous thromboembolism. The quiz consisted of 10 questions and was assigned a point value of 28 points. At the end of the student's APPE, students took the same knowledge assessment quiz to evaluate if scores had changed significantly following their involvement in the program. Pre- and post- interventional assessments of the students were provided to determine if this project was an effective technique for learning.
Statistical analysis was performed using GraphPad QuickCalcs program by GraphPad Software, Inc (GraphPad, Inc, La Jolla, CA). A chi-square test was utilized to determine the difference between pre- and post- recommendation percentages. A paired t test was used to determine the difference between student scores pre-activity and post-activity. A p value of < 0.05 was set a priori to determine statistical significance.
RESULTS
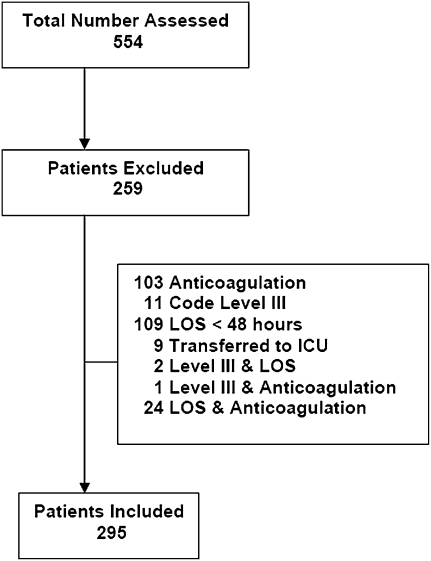
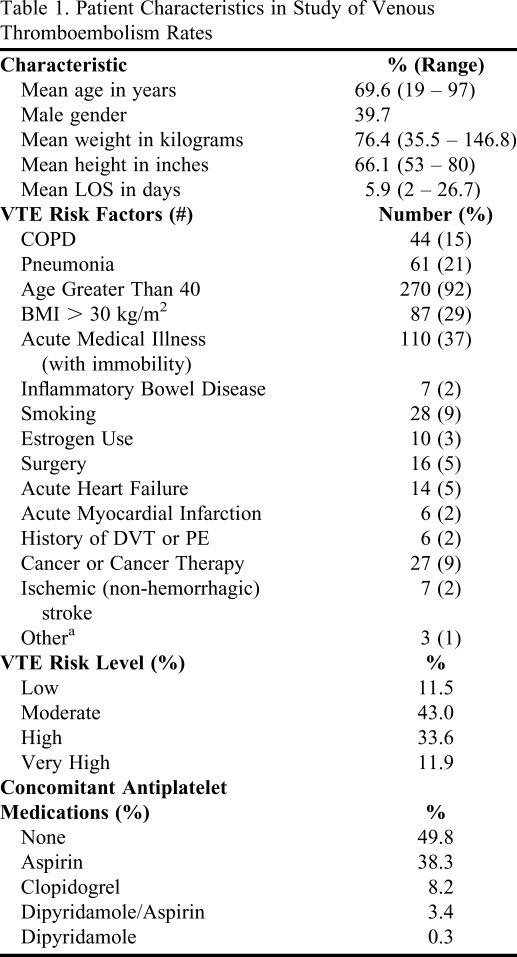
During this study, 554 newly admitted patients were assessed. Of those, 295 patients (53.3%) met inclusion criteria. Patients were excluded primarily due to being on anticoagulation (39.8%) or length of stay less than 48 hours (42.1%) (Figure 2). For patients included in the study, the average time to venous thromboembolism risk assessment post admission was 22 hours, and the average length of stay was approximately 6 days. Patients of all venous thromboembolism risk levels were enrolled in this investigation, although most patients were at moderate (43.1%) or high (33.6%) risk for developing venous thromboembolism (Table 1).
Figure 2.
Study diagram of patients assessed in venous thromboembolism study. Abbreviations: LOS = length of stay; ICU = intensive care unit; Level III = palliative care patients.
Table 1.
Patient Characteristics in Study of Venous Thromboembolism Rates
aOther = inherited or acquired thrombophilia, central venous catheter, or trauma/acute spinal cord injury/paralysis
Abbreviations: LOS = length of stay; VTE = venous thromboembolism; BMI = body mass index; COPD = chronic obstructive pulmonary disease; PE = pulmonary embolism
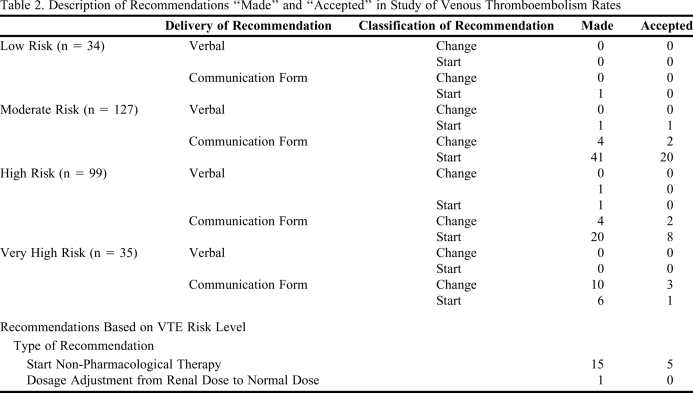
One hundred three recommendations were made to physicians and 41% were accepted. Compared to previous rates, the percentages of patients receiving “any,” “suitable,” and “optimal” prophylaxis increased from 70.5% to 82.7% (p = 0.0005), 64.4% to 75.9% (p = 0.0022), and 56.3% to 68.5% (p = 0.0022), respectively. Almost all (98%) of the recommendations to physicians were made utilizing communication forms. Nearly 60% of the recommendations made were to start therapy for moderate or high risk patients. Approximately 14% of recommendations were to start non-pharmacologic therapy (Table 2).
Table 2.
Description of Recommendations “Made” and “Accepted” in Study of Venous Thromboembolism Rates
Abbreviation: VTE = Venous Thromboembolism
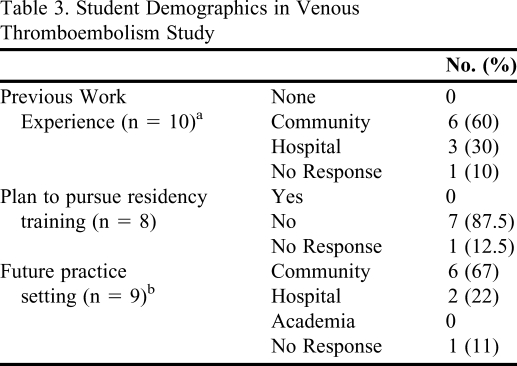
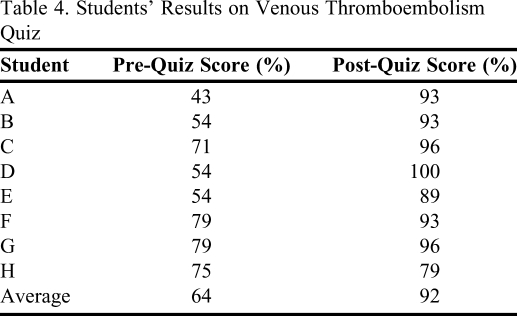
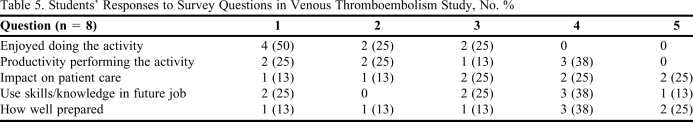
The demographics of the 8 students who participated in the venous thromboembolism risk assessment study are shown in Table 3. Most students did not plan to pursue pharmacy residency training, and the majority had plans for employment in a community pharmacy setting upon graduation. Students' post-activity quiz scores increased 28% as an average from pre-activity scores (p = 0.0016) (Table 4). The venous thromboembolism examination used in this investigation was not validated due to small sample size. The examination is provided for informational purposes only. Students estimated that they assessed an average of 6 patients daily and spent approximately 10 minutes evaluating each chart. Student responses to the project survey instrument are described in Table 5. While many students did not enjoy participating in the project, most found the experience to have an impact on patient care.
Table 3.
Student Demographics in Venous Thromboembolism Study
a2 students had previous experience in both community and hospital settings
b1 student has plans to work in 2 different practice settings
Table 4.
Students' Results on Venous Thromboembolism Quiz
Table 5.
Students' Responses to Survey Questions in Venous Thromboembolism Study, No. %
Scale: 1 = a little; 5 = a lot
DISCUSSION
One observation from the study was the increase of venous thromboembolism prophylaxis rates during the time of the study, prior to the students making recommendations. When preparing to start the student-supported assessment program, physicians at our institution were educated through a grand rounds presentation on the new program the pharmacy department was planning to implement. As a part of this presentation, previous and current venous thromboembolism prophylaxis rates within the institution were shared with the physicians. Once physicians saw previous prophylaxis rates, we believe many physicians independently started more of their patients on venous thromboembolism prophylaxis. Despite physicians ordering prophylaxis at a higher rate during the study, pharmacy students were able to increase venous thromboembolism prophylaxis rates with their recommendations.
Another observation from the study was the low physician acceptance rate for pharmacy student recommendations, which was even lower than rates found in the literature.10 One explanation of this could be that most recommendations presented to physicians were in a written form, which is a less effective means of ensuring acceptance of recommendations.10 At this community hospital, verbal recommendations were often difficult to communicate because formalized rounding did not occur on the general medicine units.
The benefits of a student-supported strategy are multifactorial. Pharmacy preceptors benefit from development of educational activities for pharmacy students to perform while on APPEs. Colleges and schools of pharmacy may benefit from the creation of advanced clerkship experiences that allow students to provide population-based care for a single disease state, thus helping to meet requirements set forth by the ACPE. Hospitals benefit by expanding and optimizing clinical pharmacy services, and the methods associated with this project could be expanded to other disease states, allowing for the provision of additional pharmacy services.
Ultimately, patients benefit from this student-supported strategy through the evaluation and optimization of their pharmacotherapy. In addition to increasing prophylaxis rates, most assessments were completed within the recommended timeframe of 24 hours. In spite of the beneficial impact of this project, the results show that approximately 1 in 5 patients did not receive venous thromboembolism prophylaxis despite having risk factors warranting therapy. A similar incidence of untreated patients at risk of developing venous thromboembolism has been observed in other large randomized trials.11-12 Of interest, moderate and high risk patients, who would seem to be the easiest to identify, required the most interventions to initiate therapy (Table 2).
Previous studies have been published demonstrating the impact pharmacy students can have during their APPEs, but few have detailed a process for integrating students into a specific disease management program.13-15 The methods associated with this project could be expanded to other disease states allowing for the provision of more comprehensive pharmaceutical care.
One limitation of this study is that the venous thromboembolism risk assessments were time consuming for both students and pharmacists. In a non-study setting, a streamlined process would need to be more efficient and assessable to all new admissions. This could be accomplished because less documentation may be needed outside of a study setting. Also, this project was designed originally to have all recommendations reviewed by a single pharmacy resident. Because every recommendation needed to be presented to a licensed pharmacist, a project preceptor was called upon on most days to help review the recommendations. In the future, involving additional pharmacy personnel to review student recommendations would be advantageous.
Another limitation to the venous thromboembolism student assessment program was that risk assessments did not occur on weekends. Because this was a pilot program, students had additional APPE assignments that did not allow for weekend coverage. This service could be improved if students and residents were able to cover all new admissions to the hospital. A pharmacy student APPE designed solely for population-based care of patients may afford the time and opportunity to implement these improvements.
CONCLUSION
This student-supported venous thromboembolism risk assessment program found that pharmacy students could increase the quantity and quality of venous thromboembolism prophylaxis in a community teaching hospital. This program could be used as a model for colleges and schools of pharmacy to meet ACPE requirements, as well as for health care institutions to help meet ICSI and ACCP recommendations regarding timely venous thromboembolism assessment and prophylaxis in hospitalized patients.
REFERENCES
- 1. Accreditation Council for Pharmacy Education. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. Adopted January 15, 2006. http://www.acpe-accredit.org. Accessed June 1, 2010.
- 2.Geerts WH, Pineo GF, Heit JA, et al. Prevention of venous thromboembolism: the seventh ACCP conference on antithrombotic and thrombolytic therapy. Chest. 2004;126(3):338S–400S. doi: 10.1378/chest.126.3_suppl.338S. [DOI] [PubMed] [Google Scholar]
- 3. Institute for Clinical Systems Improvement (ICSI). Venous Thromboembolism Prophylaxis. Bloomington, MN: Institute for Clinical Systems Improvement; 2007. www.icsi.org. Accessed June 1, 2010.
- 4.Francis CW. Clinical practice: prophylaxis for thromboembolism in hospitalized medical patients. N Engl J Med. 2007;356(14):1438–1444. doi: 10.1056/NEJMcp067264. [DOI] [PubMed] [Google Scholar]
- 5.Dexter PR, Perkins S, Overhage JM, Maharry K, Kholer RB, McDonald CJ. A computerized reminder system to increase the use of preventive care for hospitalized patients. N Engl J Med. 2001;345(13):965–970. doi: 10.1056/NEJMsa010181. [DOI] [PubMed] [Google Scholar]
- 6.Kucher N, Koo S, Quiroz R, et al. Electronic alerts to prevent venous thromboembolism among hospitalized patients. N Engl J Med. 2005;352(10):969–977. doi: 10.1056/NEJMoa041533. [DOI] [PubMed] [Google Scholar]
- 7.Enders JM, Dobesh PP, Abu-Shanab JR, Lakamp JE. Utilization of venous thromboembolism prophylaxis in acute medical illness [abstract] Pharmacotherapy. 2002;22(10):1344. doi: 10.1592/phco.22.17.1564.34124. [DOI] [PubMed] [Google Scholar]
- 8.Dobesh PP, Stacy ZA. Effect of a clinical pharmacy education program on improvement in the quantity and quality of venous thromboembolism prophylaxis for medically ill patients. J Manag Care Pharm. 2005;11(9):755–762. doi: 10.18553/jmcp.2005.11.9.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Fanikos, J. Pharmacist essentials in preventing and managing venous thromboembolism. ASHP Advantage. www.ashpadvantage.com. Accessed June 1, 2010.
- 10.Lundquist LM, Moye PM. Resident physicians' acceptance of pharmacy student pharmacotherapy recommendations during an ambulatory care advanced pharmacy practice experience. Am J Pharm Educ. 2009;73(8) doi: 10.5688/aj7308145. Article 145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Samama MM, Sohen AT, Darmon J, et al. A comparison of enoxaparin with placebo for the prevention of venous thromboembolism in acutely ill medical patients. N Engl J Med. 1999;341(11):793–800. doi: 10.1056/NEJM199909093411103. [DOI] [PubMed] [Google Scholar]
- 12.Leizorovicz A, Cohen AT, Turpie AG, Olsson C, Vaitkus PT, Goldhaber SZ. Randomized, placebo-controlled trial of dalteparin for the prevention of venous thromboembolism in acutely ill medical patients. Circulation. 2004;110(7):874–879. doi: 10.1161/01.CIR.0000138928.83266.24. [DOI] [PubMed] [Google Scholar]
- 13.Slaughter RL, Erickson SR, Thompson PA. Clinical interventions provided by doctor of pharmacy students. Ann Pharmacother. 1994;28(5):665–670. doi: 10.1177/106002809402800519. [DOI] [PubMed] [Google Scholar]
- 14.Thompson AN, Osgood TS, Ragucci KR. Patient care interventions by pharmacy students in the intensive care unit. Am J Health-Syst Pharm. 2007;64(17):1788–1789. doi: 10.2146/ajhp060476. [DOI] [PubMed] [Google Scholar]
- 15.Pham DQ. Evaluating the impact of clinical interventions by PharmD students on internal medicine clerkships: the results of a 3 year study. Ann Pharmacother. 2006;40(9):1541–1545. doi: 10.1345/aph.1H142. [DOI] [PubMed] [Google Scholar]