Abstract
Unhealthy lipid levels are among the leading controllable risk factors for coronary heart disease. To identify the psychological factors associated with dyslipidemia, this study investigates the personality correlates of cholesterol (total, LDL, and HDL) and triglycerides. A community-based sample (N=5,532) from Sardinia, Italy, had their cholesterol and triglyceride levels assessed and completed a comprehensive personality questionnaire, the NEO-PI-R. All analyses controlled for age, sex, BMI, smoking, drinking, hypertension, and diabetes. Low Conscientiousness and traits related to impulsivity were associated with lower HDL cholesterol and higher triglycerides. Compared to the lowest 10%, those who scored in top 10% on Impulsivity had a 2.5 times greater risk of exceeding the clinical threshold for elevated triglycerides (OR=2.51, CI=1.56–4.07). In addition, sex moderated the association between trait depression (a component of Neuroticism) and HDL cholesterol, such that trait depression was associated with lower levels of HDL cholesterol in women but not men. When considering the connection between personality and health, unhealthy lipid profiles may be one intermediate biomarker between personality and morbidity and mortality.
Keywords: Personality, Depression, Impulsivity, Cholesterol, Triglycerides
According to the American Heart Association, high cholesterol is a leading controllable risk factor for coronary heart disease, heart attack and stroke (American Heart Association, 2001; National Cholesterol Education Program Expert Panel, 2002). It is no surprise, then, that a considerable amount of effort has been devoted to understanding the factors, from the cellular to the psychological, that contribute to high (and low) levels of cholesterol. Interest in the interface between psychological traits and cholesterol levels has focused mainly on depression; comparatively less research has addressed the association between cholesterol and normally-distributed personality traits. The present research examines this relation within the framework of the Five-Factor Model (FFM) of personality (McCrae & Costa, 2003).
The FFM is an empirically-derived model of personality that characterizes the individual’s characteristic ways of thinking, feeling, and behaving along five broad dimensions: Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness (McCrae & Costa, 2003). Of these five factors, Neuroticism, the tendency to experience negative emotions, and Conscientiousness, the tendency to be responsible, organized, and self-disciplined, have been frequently linked to a variety of health-risk behaviors and outcomes. For example, individuals high on Neuroticism or low on Conscientiousness tend to have more chronic illnesses (Goodwin & Friedman, 2006), lower subjective (Löckenhoff, Sutin, Ferrucci, & Costa, 2008) and physician-rated health (Chapman, Lyness, & Duberstein, 2007), and ultimately die younger (Terracciano, Löckenhoff, Zonderman, Ferrucci, & Costa, 2008; Wilson, Mendes De Leon, Bienias, Evans, & Bennett, 2004). These associations raise the possibility that Neuroticism and Conscientiousness might also be associated with physiological risk factors for morbidity and mortality, such as unhealthy levels of cholesterol and triglycerides.
Necessary for the healthy functioning of cells, cholesterol is a soft, fat-like, waxy substance that is moved around in the bloodstream by lipoproteins. Elevated levels of low-density lipoprotein (LDL or “bad” cholesterol) in the blood contribute to the formation of plaque in the arteries, which make arteries less flexible and increase the risk of blood clots. In contrast, high-density lipoprotein (HDL or “good” cholesterol) carries cholesterol away from arteries back to the liver where it is processed out of the body. Finally, triglycerides, a form of fat made by the body, are typically considered the third component of lipoprotein profiles; as with LDL, elevated levels of triglycerides contribute to the development of atherosclerosis (American Heart Association, 2001; National Cholesterol Education Program Expert Panel, 2002).
Lipoprotein profiles have been studied primarily in the context of mood and anxiety disorders. Interestingly, correlational evidence suggests that depression is inversely associated with total cholesterol and positively associated with triglycerides. For example, compared to controls, total cholesterol tends to be lower among individuals suffering from major depressive disorder (Jow, Yang, & Chen, 2006) or borderline personality disorder (Atmaca, Kuloglu, Tezcan, Gecici, & Ustundag, 2002). By contrast, among young women, a lifetime major depressive episode is associated with elevated triglycerides (Kinder, Carnethon, Palaniappan, King, & Fortmann, 2004). Similarly, in non-clinical populations, depressive symptoms tend to be associated with lower levels of total cholesterol (Giltay et al., 2009; Horsten, Wamala, Vingerhoets, & Orth-Gomer, 1997; Shin, Suls, & Martin, 2008; Steegmans, Hoes, Bak, Van Der Does, & Grobbee, 2000), but higher triglycerides (Herva et al., 2006; McCaffery, Niaura, Todaro, Swan, & Carmelli, 2003). Evidence from animal models of depression supports this association: Depressed female cynomolgus monkeys tend to have lower levels of HDL cholesterol (Shively et al., 2008).
Less work has addressed whether cholesterol is related to enduring personality traits, such as trait susceptibility to either depression or anxiety, as opposed to the association with acute symptoms of psychological distress. The one exception is Suarez (1999), who found that trait depression, a component of Neuroticism, and anxiety were both associated with lower total cholesterol and lower triglycerides in a small sample of young women. The extent to which this generalizes to men or to older adults has yet to be tested. As sex differences are found when men and women are specifically compared, any potential association may differ across the sexes (Chen, Lu, Wu, & Chang, 2001; Kinder et al., 2004; Toker, Shirom, & Melamed, 2008). Large samples of both sexes are needed to explicitly test whether sex moderates the association between personality and cholesterol.
In addition to depression, lipoprotein profiles may be associated with the different aspects of trait impulsivity. Most broadly, impulsivity reflects the inability to delay, inhibit, or control behavior. Under this broad definition, Whiteside and Lynam (2001) identified four distinct facets: (1) the tendency to give in to strong impulses and desires (N5: Impulsivity); (2) the inability to foresee the consequences of an action (C6: Deliberation); (3) the inability to stay committed to a task (or lifestyle) amid distractions and difficulties (C5: Self-Discipline); and (4) the desire to engage in risky or dangerous activities for fun (E5: Excitement-Seeking). Individuals high in impulsivity or low in self-discipline often have a difficult time controlling their impulses and, as such, tend to engage in unhealthy behaviors. Such individuals, for example, are more likely to smoke (Terracciano & Costa, 2004), abuse drugs (Terracciano, Löckenhoff, Crum, Bienvenu, & Costa, 2008), and binge eat and drink (Benjamin & Wulfert, 2005). Individuals high on impulsivity-related personality traits are also more often overweight (Terracciano et al., 2009) and thus they may be more likely to have elevated levels of cholesterol and triglycerides.
In the current study, we examine the relation between personality and cholesterol (total, LDL, and HDL) and triglycerides in a large community-based sample. Because our sample includes both sexes and the age range spans from adolescence to late adulthood, we are able to test whether these two major demographic variables moderate the association between personality and lipoprotein profiles. We examine the five broad dimensions of personality, the narrower facet of depression (N3: Depression), and the four facets related to impulsivity (N5: Impulsiveness, E5: Excitement-Seeking, C5: Self-Discipline, and C6: Deliberation).
Method
Participants
Participants were drawn from the SardiNIA project, a large multidisciplinary study that has been described in detail elsewhere (Costa et al., 2007; Pilia et al., 2006). Approximately 62% of the population (N = 6,148 individuals; 56.7% female), aged 14 to 102 years, from a cluster of four towns in the Ogliastra province enrolled in the study. In the present sample, valid personality and cholesterol data were obtained from 5,532 participants (58% female) who were not taking cholesterol-lowering medication (i.e., statins). Age ranged from 14 to 94 (M = 42.17; SD = 16.76). Compared to the full SardiNIA sample, those included in the present analyses were younger, more educated, more likely to be female, and had lower levels of total cholesterol, LDL cholesterol, and triglycerides (all ps < .05). Descriptive statistics for the current sample are shown in Table 1.
Table 1.
Descriptive Statistics for Demographics, Lipoproteins, and Personality Variables
| Variable | Sample characteristics |
|---|---|
| Demographics | |
| Age | 42.17 (16.76) |
| Gender (female) | 58% |
| Cholesterol | |
| Total | 207.96 (42.05) |
| HDL | 64.10 (14.84) |
| Derived LDL | 126.54 (35.09) |
| Triglycerides | 86.82 (67.96) |
| Personality | |
| Neuroticism | 5.53 (.91) |
| Extraversion | 4.90 (.88) |
| Openness | 4.65 (1.01) |
| Agreeableness | 4.65 (.96) |
| Conscientiousness | 4.90 (.96) |
| N3: Depression | 5.48 (.96) |
| N5: Impulsivity | 4.81 (.94) |
| E5: Excitement-Seeking | 4.76 (1.01) |
| C5: Self-Discipline | 4.81 (.92) |
| C6: Deliberation | 5.52 (1.10) |
Note. N = 5,532. Standard deviations are shown in parentheses.
Personality Assessment
Personality traits were assessed using the Italian version (Terracciano, 2003) of the Revised NEO Personality Inventory (NEO-PI-R), which measures 30 facets, six for each of the five major dimensions of personality (Costa, & McCrae, 1992). The NEO-PI-R has been shown to be a valid measure of personality in individuals as young as 12 years of age (McCrae et al., 2002). The 240 items are answered on a five-point Likert scale, from strongly disagree to strongly agree. Participants filled out the self-report questionnaire (89%) or chose to have the questionnaire read by a trained Sardinian psychologist (11%) (Costa et al., 2007). A variable (Test administration) that indicated this difference in the administration of the NEO-PI-R was used as a covariate in the analyses. In this sample, the NEO-PI-R showed good psychometric properties: internal consistency reliabilities for the five factors ranged from 0.80 to 0.87. The factor structure replicated the American normative structure at both the phenotypic and genetic level (Costa et al., 2007; Pilia et al., 2006). Raw scores were converted to T-scores (M = 5, SD = 1) using American combined-sex norms (Costa & McCrae, 1992).
Cholesterol
Standard enzymatic methods were used on fasting lipid measurements to determine serum total cholesterol, HDL cholesterol, and triglycerides. In the present sample, total cholesterol had a mean of 207.96 mg/dL (SD = 42.05), HDL cholesterol had a mean of 64.10 mg/dL (SD = 14.84), and triglycerides had a mean of 86.82 mg/dL (SD = 67.96). LDL cholesterol was derived using the Friedewald equation (Friedewald, Levy, & Fredrickson, 1972): LDL cholesterol = Total cholesterol – HDL cholesterol – (triglycerides/5). In the present sample, LDL cholesterol had a mean of 126.54 (SD = 35.09). See Supplementary Table 1 for descriptive statistics of the lipoprotein profiles by sex and age.
Covariates
In all of the analyses reported below, we controlled for a number of variables known to be associated with high cholesterol. In addition to sex, age, age squared (to account for non-linear changes in personality across the life span; Terracciano, McCrae, Brant, & Costa, 2005), education, and test administration, we included a covariates identified by the National Cholesterol Education Program Expert Panel (2002) to increase risk for elevated lipoproteins: Body Mass Index (BMI) derived from staff-assessed weight and height (M = 25.16, SD = 4.62), current smoking status (21% current vs. 79% former/never) and diagnosed hypertension (12%) and diabetes (3%). In addition, we include drinking status (45% drink alcohol), because moderate alcohol consumption may be protective (National Cholesterol Education Program Expert Panel, 2002).
Statistical overview
In a series of linear regressions, we predicted cholesterol (total, LDL, HDL) and triglycerides from the personality traits and facets, controlling for the covariates listed above. Following Aiken and West’s (1991) methodology for testing interactions, we also tested whether sex and age moderated any of the relations between personality and cholesterol, controlling for the same covariates. Finally, using a series of logistic regressions, we tested whether personality predicted above normal total and LDL cholesterol and triglyceride levels and protective levels of HDL cholesterol. According to the American Heart Association, total cholesterol levels should be less than 200 mg/dL, LDL cholesterol should be less than 130, and triglyceride levels should be less than 150 mg/dL. HDL levels >60 mg/dL are considered protective against heart disease (American Heart Association, 2001; National Cholesterol Education Program Expert Panel, 2002).
Results
The associations between personality and cholesterol, controlling for all covariates, are shown in Table 2. At the factor-level, trait Neuroticism was unrelated to total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides. In contrast, participants high on Conscientiousness had higher levels of HDL cholesterol and lower triglycerides. Openness to Experience also correlated positively with triglycerides.
Table 2.
Regression Analyses Predicting Total, LDL, and HDL Cholesterol and Triglycerides from Personality
| Cholesterol (mg/dL) |
Triglycerides (mg/dL) | |||
|---|---|---|---|---|
| Total | Derived LDL | HDL | ||
| Factor-level personality | ||||
| Neuroticism | .00 | .00 | .00 | .01 |
| Extraversion | .00 | .00 | .00 | .00 |
| Openness | −.01 | −.02 | .00 | .03* |
| Agreeableness | −.01 | −.01 | .01 | −.02 |
| Conscientiousness | .00 | .00 | .04** | −.05** |
| Facet-level personality | ||||
| N3: Depression | −.02 | −.02 | −.01 | .01 |
| Impulsivity-related traits | ||||
| N5: Impulsivity | .02 | .01 | .00 | .04** |
| E5: Excitement-seeking | .00 | .00 | .00 | .01 |
| C5: Self-Discipline | .01 | .01 | .04** | −.04** |
| C6: Deliberation | −.01 | −.01 | .03* | −.04** |
Note. N = 5,532. Standardized regression coefficients controlling for age, age squared, sex, education, test administration, smoking status, alcohol use, hypertension, diabetes, and BMI.
p < .05.
p < .01.
Turning to the specific facets, participants with personality traits associated with self-control generally had a more positive lipoprotein profile (see Table 2). Following the same pattern as domain-level Conscientiousness, C5: Self-Discipline and C6: Deliberation both correlated positively with HDL and negatively with triglycerides. Furthermore, participants who have trouble controlling their urges (N5: Impulsivity) had higher levels of triglycerides. The last component of impulsivity, E5: Excitement-Seeking, was unrelated to either cholesterol or triglycerides. Finally, trait depression did not correlate with total cholesterol, LDL, HDL, or triglycerides in the full sample. Although the associations between personality and lipoprotein profiles are modest in magnitude, they are similar to those of other established risk factors. For example, in the current sample the association between triglycerides and current smoking (β = .08, p < .01), hypertension (β = .04, p < .01), and diabetes (β = .03, p < .05) are similar in magnitude to a 1 SD difference in Conscientiousness (β = −.05, p < .01).
Sex moderated several of these associations. First, although Conscientiousness was associated significantly with higher levels of HDL for both men and women, the association was stronger in women (β C x sex = −.03, p < .05). Similarly, the positive association between N5: Impulsivity and triglycerides was significant for both sexes, but the association was stronger in men (β N5 x sex = .04, p < .05). Consistent with the research on clinical depression, higher N3: Depression was associated with lower levels of HDL cholesterol in women but not men (β N3 x sex = .03, p < .05). Finally, the association between Openness and higher triglycerides held only for men (β O x sex = .04, p < .05). Age moderated one association between personality and lipoprotein profiles: The association between Conscientiousness and triglycerides held for older participants, but not for younger ones (β C x age = −.04, p < .05). See Supplementary Table 2 for the regression analyses run separately by sex and Supplementary Table 3 for the regression analyses run separately by younger and older participants.
As discussed above, the American Heart Association has identified specific thresholds at which levels of cholesterol and triglycerides elevate risk for heart disease. Using logistic regression, we examined whether personality could predict individuals falling in the at-risk category for total cholesterol, LDL cholesterol, and triglycerides and the protective category for HDL cholesterol (see Table 3). The odds ratios in Table 3 represent risk per one standard deviation increase in personality. Results indicate that highly conscientious participants, particularly those high on C5: Discipline, were more likely to have levels of HDL cholesterol above the protective threshold of 60 mg/dL and triglyceride levels below the 150 mg/dL threshold. In addition, participants who reported that they often have difficulty controlling their urges (N5: Impulsivity) were more likely to have unhealthy levels of triglycerides, whereas those who think before they act (C6: Deliberation) were more likely to have healthy levels. Additional analyses indicate that those who scored in the top 10% of the distribution on N5: Impulsivity had more than twice the risk of exceeding clinical thresholds of at-risk levels of triglycerides compared to those in the bottom 10% of the distribution (OR = 2.51, CI = 1.56–4.07). Similarly, those who scored in the top 10% of the distribution on C6: Deliberation were nearly 50% less likely to exceed the clinical threshold (OR = .57, CI = .37–.89). Finally, consistent with the literature on depression and cholesterol (Shin et al., 2008; Troisi, 2009), those with a dispositional proneness to depression (N3: Depression) were less likely to have elevated levels of either total or LDL cholesterol. In all of the above analyses, controlling for participants on any psychoactive medication (n = 153) did not alter the findings.
Table 3.
Logistic Regressions Predicting Clinical Thresholds of Total, LDL, and HDL Cholesterol and Triglycerides from Personality
| Cholesterol (mg/dL) |
Triglycerides (mg/dL) | |||
|---|---|---|---|---|
| Total | Derived LDL | HDL | ||
| Factor-level personality | ||||
| Neuroticism | .96 (.89–1.05) | .98 (.90–1.06) | 1.08 (1.00–1.17) | 1.03 (.90–1.17) |
| Extraversion | .95 (.87–1.04) | .96 (.88–1.05) | 1.02 (.94–1.11) | 1.03 (.81–1.19) |
| Openness | 1.02 (.94–1.10) | 1.00 (.92–1.08) | 1.00 (.93–1.08) | 1.04 (.92–1.18) |
| Agreeableness | .96 (.89–1.03) | .97 (.90–1.04) | 1.07 (.99–1.14) | .92 (.82–1.04) |
| Conscientiousness | 1.08 (1.01–1.17)* | 1.03 (.95–1.11) | 1.09 (1.11–1.18)* | .86 (.76–.97)** |
| Facet-level personality | ||||
| N3: Depression | .91 (.86–.97)** | .93 (.87–.99)* | 1.00 (.94–1.06) | 1.02 (.91–1.14) |
| Impulsivity-related traits | ||||
| N5: Impulsivity | .99 (.92–1.06) | 1.00 (.93–1.07) | .99 (.93–1.06) | 1.19 (1.06–1.33)** |
| E5: Excitement-seeking | 1.02 (.95–1.09) | 1.01 (.94–1.08) | .97 (.91–1.04) | .99 (.88–1.11) |
| C5: Self-Discipline | 1.08 (1.01–1.15)* | 1.03 (.96–1.10) | 1.10 (1.04–1.18)** | .89 (.80–.99)* |
| C6: Deliberation | 1.03 (.97–1.09) | 1.00 (.95–1.06) | 1.04 (.98–1.10) | .86 (.78–.94)** |
Note. N = 5,532. Odds Ratios (95% Confidence Intervals) controlling for age, age squared, sex, education, test administration, smoking status, alcohol use, hypertension, diabetes, and BMI. Clinical thresholds are ≥ 200 mg/dL for Total cholesterol, ≥ 130 mg/dL for LDL cholesterol, ≤ 60 mg/dL for HDL cholesterol, and ≥ 150 mg/dL for triglycerides.
p < .05.
p < .01.
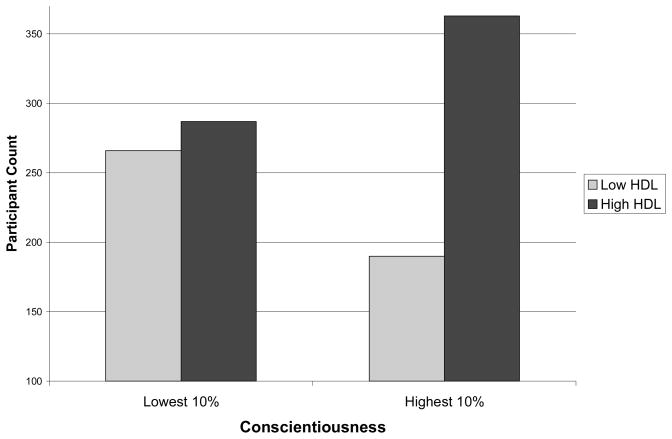
Although both domain-level Conscientiousness and C5: Self-Discipline were associated with higher levels of total cholesterol, this association did not hold when controlling for levels of HDL cholesterol. In fact, individuals who scored in the top 10% of the distribution on Conscientiousness were almost 1.8 times more likely to have levels of HDL cholesterol in the protective range (OR = 1.77; 95% CI = 1.39–2.26; see Figure 1).
Figure 1.
Number of participants with HDL levels above and below the protective threshold (> 60 mg/dL) in the lowest and highest 10% of the distribution of Conscientiousness in the current sample.
Finally, we examined whether the remaining personality facets assessed by the NEO-PI-R were associated with at-risk thresholds for total cholesterol, LDL, HDL, and triglycerides. The strongest (i.e., p < .01) findings were for E4: Activity and HDL cholesterol (OR = 1.12, 95% CI = 1.05–1.20) and C3: Dutifulness and triglycerides (OR = .87, 95% CI = .78–.97). Active individuals maintain a vigorous and fast-paced lifestyle (Costa & McCrae, 1992) and they tend to exercise more (Hoyt, Rhodes, Hausenblas, & Giacobbi, 2009), which may contribute to their protective levels of HDL. Likewise, dutiful individuals tend to adhere to their principles (Costa & McCrae, 1992), including maintaining a healthy lifestyle, which may also help keep their triglyceride levels down.
Discussion
In the present research, we examined the association between personality traits and lipoprotein levels. Previous research on psychological traits and cholesterol has focused primarily on clinical depression and depressive symptoms. To date, this is the largest study that has examined the association between a trait susceptibility to negative emotions and levels of cholesterol and triglycerides. We found little evidence that Neuroticism was correlated with cholesterol or triglyceride levels in men, but consistent with data from clinical (Kinder et al., 2004), community (Chen et al., 2001; Horsten et al., 1997), and animal populations (Shively et al., 2008), women who scored higher on trait depression had lower levels of HDL cholesterol. Also consistent with the clinical literature (Jow et al., 2006; Shin et al., 2008; Steegmans et al., 2000), we found that those who scored higher on trait depression were less likely to have either total or LDL cholesterol levels that surpass the clinical at-risk threshold. Finally, those high on N5: Impulsivity were more likely to have elevated triglycerides. Their triglyceride levels may be due, in part, to dietary preferences: Impulsive individuals prefer foods and drinks that are sweet (Saliba, Wragg, & Richardson, in press), and a high carbohydrate diet has been linked to elevated triglycerides (National Cholesterol Education Program Expert Panel, 2002).
Several hypotheses have been offered for why lower cholesterol would be associated with greater depressive symptoms. Some have suggested, based on post-mortem studies, that lower cholesterol in the brain may decrease synaptic density or function, contributing to mood disorders (Beasley et al., 2005). Yet, the use of cholesterol-lowering drugs is not associated with increased depression (Stewart et al., 2000) and long-term statin use may even be beneficial for psychological well-being (Young-Xu, Chan, Liao, Ravid, & Blatt, 2003). The serotonergic system may perhaps be more sensitive to naturally-occurring low levels of cholesterol than medically-induced ones. Others have proposed (Shin et al., 2008) that depression may be associated with lower cholesterol because the increased cytokine activation associated with depression impairs cholesterol synthesis (Feingold & Grunfeld, 1992). Or, the association may be due to a mechanism common to both personality and depression, such as inflammation (Shively et al., 2008; Sutin et al., in press). These different possibilities have yet to be teased apart.
To our knowledge, this is the first report of the association between Conscientiousness and levels of cholesterol and triglycerides. This omission in the literature is surprising because Conscientiousness has long been linked to both health behaviors and outcomes (Goodwin & Friedman, 2006). In particular, individuals who score low in Conscientiousness tend to engage in the risky behaviors that contribute to poor physical health. That is, these individuals tend to smoke (Terracciano & Costa, 2004), have larger waists (Terracciano et al., 2009), a tendency towards binge eating and drinking (Rush, Becker, & Curry, 2009), and sedentary lifestyles (Rhodes & Smith, 2006). In the current study, Conscientiousness remained a significant predictor of higher HDL cholesterol and lower triglycerides even after the inclusion of several lifestyle factors. These associations suggest that there are either direct physiological links between Conscientiousness and cholesterol or that other lifestyle factors not included in the current study, such as physical activity, may account for these relations. For example, conscientious individuals may have healthier lipoprotein profiles because they are more likely to exercise regularly. In current and future follow-up assessments of the SardiNIA cohort, we will attempt to assess both diet and physical activity, so that future research will be able to test this mediational pathway.
Given this association between Conscientiousness and health behaviors, it is not a surprise that low Conscientiousness is a consistent predictor of mortality (Kern & Friedman, 2008; Terracciano, Löckenhoff, Zonderman et al., 2008; Wilson et al., 2004). The physiological mechanisms responsible for the association between Conscientiousness and mortality are less well understood. Recent evidence suggests that individuals lower in Conscientiousness have higher levels of interleukin-6, a marker of inflammation. This association is due, in part, to their poor health behaviors, such as smoking and higher BMI (Sutin et al., in press). This study adds cholesterol and triglycerides as potential biomarkers that may mediate the association between Conscientiousness and mortality.
Of note, we found no association between Agreeableness and lipoprotein profiles. The early research linking the Type A behavior pattern to coronary heart disease (CHD) (Booth-Kewley & Friedman, 1987; Dembroski, MacDougall, Costa, & Grandits, 1989; Williams, Haney, & Lee, 1980) suggested that constructs related to antagonism may also be associated with other risk factors for CHD. But, just as the association between Type A and CHD has proven difficult to replicate (Ikeda, Iso, Kawachi, Inoue, & Tsugane, 2008; Shekelle, Hulley, & Neaton, 1985), so too has its association with lipoproteins (Almada et al., 1991; Richards, Hof, & Alvarenga, 2000; Scherwitz et al., 1992). The mixed findings may be due, in part, to psychometric limitations of the Type A construct. Traits related to antagonism and hostility, however, do seem to play a role in the development of coronary heart disease (Chida & Steptoe, 2009; Nabi et al., 2008; Smith, 1992). Such traits may be more strongly associated with aggregated cardiovascular risk factors, such as the metabolic syndrome, rather than the individual components, such as lipoprotein profiles.
Personality contributes not only to the development of high cholesterol, but continues to have an effect on the individual’s health after diagnosis. As such, personality may have translational implications as well. Conscientiousness, for example, is strongly associated with compliance to medication regimens. Despite the clear benefits of cholesterol-lowering medications, it has been estimated that up to six in 10 patients discontinue medication use within the first year of treatment (Avorn et al., 1998, Simons, Levis, & Simons, 1996). Perhaps not surprisingly, differences in adherence have significant consequences: Non-adherers have a much greater risk of both non-fatal myocardial infarction and all-cause mortality than adherers (for a review see Liberopoulos, Florentin, Mikhailidis, & Elisaf, 2008). Just as Conscientiousness is associated with health-protective behaviors, it is also a strong predictor of adherence. In one study, for example, over the course of 24 weeks, Conscientiousness predicted adherence to cholesterol-lowering medication, as measured by an electronic medication event monitoring system (Stilley, Sereika, Muldoon, Ryan, & Dunbar-Jacob, 2004). Thus, interventions aimed at both prevention and treatment need to take personality into account when tailored towards the individual.
Although long-term prospective studies are needed to fully evaluate the translational implications of our findings, the present research is, to date, the largest study of the association between personality traits and cholesterol in a community sample that spans from adolescence through old age. This study is also the first to use a detailed measure of personality traits to assess their associations with complete lipoprotein profiles. In addition to the broad domains, our comprehensive measure of traits revealed associations at the facet level: Those high on impulsivity were over twice as likely to have exceeded established clinical thresholds for elevated triglycerides, whereas those high on deliberation had half the risk of exceeding this threshold. Despite these strengths, this study also had limitations. The cross-sectional nature of the study, for example, precludes inferences about causality. In addition, the number of analyses may increase the chance of Type I errors. We focus, however, on theoretically-meaningful associations that were hypothesized from the personality-health literature; this focus should help reduce false positives. In summary, the present study provides evidence that personality traits are associated with clinically-important biomarkers that are the leading controllable risk factors for cardiovascular disease.
Supplementary Material
Acknowledgments
This research was supported in part by the Intramural Research Program of the NIH, National Institute on Aging. Paul Costa receives royalties from the Revised NEO Personality Inventory.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Almada SJ, Zonderman AB, Shekelle RB, Dyer AR, Daviglus ML, Costa PT, et al. Neuroticism and cynicism and risk of death in middle-aged men: The Western Electric study. Psychosomatic Medicine. 1991;53:165–175. doi: 10.1097/00006842-199103000-00006. [DOI] [PubMed] [Google Scholar]
- Association AH. 2000 heart and stroke statistical update. Dallas, TX: 2001. [Google Scholar]
- Atmaca M, Kuloglu M, Tezcan E, Gecici O, Ustundag B. Serum cholesterol and leptin levels in patients with borderline personality disorder. Neuropsychobiology. 2002;45:167–171. doi: 10.1159/000063665. [DOI] [PubMed] [Google Scholar]
- Avorn J, Monette J, Lacour A, Bohn RL, Monane M, Mogun H, et al. Persistence of use of lipid-lowering medications: A cross-national study. Journal of the American Medical Association. 1998;279:1458–1462. doi: 10.1001/jama.279.18.1458. [DOI] [PubMed] [Google Scholar]
- Beasley CL, Honer WG, von Bergmann K, Falkai P, Lütjohann D, Bayer TA. Reductions in cholesterol and synaptic markers in association cortex in mood disorders. Bipolar Disorders. 2005;7:449–455. doi: 10.1111/j.1399-5618.2005.00239.x. [DOI] [PubMed] [Google Scholar]
- Benjamin L, Wulfert E. Dispositional correlates of addictive behaviors in college women: Binge eating and heavy drinking. Eating Behaviors. 2005;6:197–209. doi: 10.1016/j.eatbeh.2003.08.001. [DOI] [PubMed] [Google Scholar]
- Booth-Kewley S, Friedman HS. Psychological predictors of heart disease: A quantitative review. Psychological Bulletin. 1987;101:343–362. [PubMed] [Google Scholar]
- Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosomatic Medicine. 2007;69:277–282. doi: 10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CC, Lu FH, Wu JS, Chang CJ. Correlation between serum lipid concentrations and psychological distress. Psychiatry Research. 2001;102:153–162. doi: 10.1016/s0165-1781(01)00231-1. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. The association of anger and hostility With future coronary heart disease: A meta-analytic review of prospective evidence. Journal of the American College of Cardiology. 2009;53:936–946. doi: 10.1016/j.jacc.2008.11.044. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory (NEO-PI-R) and the NEO Five-Factor Inventory (NEO-FFI) professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Costa PT, Terracciano A, Uda M, Vacca L, Mameli C, Pilia G, et al. Personality traits in Sardinia: Testing founder population effects on trait means and variances. Behavior Genetics. 2007;37:376–387. doi: 10.1007/s10519-006-9103-6. [DOI] [PubMed] [Google Scholar]
- Dembroski TM, MacDougall JM, Costa PT, Grandits GA. Components of hostility as predictors of sudden death and myocardial infarction in the Multiple Risk Factor Intervention Trial. Psychosomatic Medicine. 1989;51:514–522. doi: 10.1097/00006842-198909000-00003. [DOI] [PubMed] [Google Scholar]
- Expert panel on detection evaluation and treatment of high blood cholesterol in adults: Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- Feingold KR, Grunfeld C. Role of cytokines in inducing hyperlipidemia. Diabetes. 1992;41:97–101. doi: 10.2337/diab.41.2.s97. [DOI] [PubMed] [Google Scholar]
- Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clinical Chemistry. 1972;18:499–502. [PubMed] [Google Scholar]
- Giltay EJ, van Reedt Dortland AKB, Nissinen A, Giampaoli S, van Veen T, Zitman FG, et al. Serum cholesterol, apolipoprotein E genotype and depressive symptoms in elderly European men: The FINE study. Journal of Affective Disorders. 2009;115:471–477. doi: 10.1016/j.jad.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Friedman HS. Health status and the five-factor personality traits in a nationally representative sample. Journal of Health Psychology. 2006;11:643–654. doi: 10.1177/1359105306066610. [DOI] [PubMed] [Google Scholar]
- Herva A, Räsänen P, Miettunen J, Timonen M, Läksy K, Veijola J, et al. Co-occurrence of metabolic syndrome with depression and anxiety in young adults: The Northern Finland 1966 Birth Cohort Study. Psychosomatic Medicine. 2006;68:213–216. doi: 10.1097/01.psy.0000203172.02305.ea. [DOI] [PubMed] [Google Scholar]
- Horsten M, Wamala SP, Vingerhoets A, Orth-Gomer K. Depressive symptoms, social support, and lipid profile in healthy middle-aged women. Psychosomatic Medicine. 1997;59:521–528. doi: 10.1097/00006842-199709000-00009. [DOI] [PubMed] [Google Scholar]
- Hoyt AL, Rhodes RE, Hausenblas HA, Giacobbi PR. Integrating five-factor model facet-level traits with the theory of planned behavior and exercise. Psychology of Sport and Exercise. 2009;10:565–572. [Google Scholar]
- Ikeda A, Iso H, Kawachi I, Inoue M, Tsugane S. Type A behaviour and risk of coronary heart disease: The JPHC Study. International Journal of Epidemiology. 2008;37:1395–1405. doi: 10.1093/ije/dyn124. [DOI] [PubMed] [Google Scholar]
- Jow GM, Yang TT, Chen CL. Leptin and cholesterol levels are low in major depressive disorder, but high in schizophrenia. Journal of Affective Disorders. 2006;90:21–27. doi: 10.1016/j.jad.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Kern ML, Friedman HS. Do conscientious individuals live longer? A quantitative review. Health Psychology. 2008;27:505–512. doi: 10.1037/0278-6133.27.5.505. [DOI] [PubMed] [Google Scholar]
- Kinder LS, Carnethon MR, Palaniappan LP, King AC, Fortmann SP. Depression and the metabolic syndrome in young adults: Findings from the Third National Health and Nutrition Examination Survey. Psychosomatic Medicine. 2004;66:316–322. doi: 10.1097/01.psy.0000124755.91880.f4. [DOI] [PubMed] [Google Scholar]
- Liberopoulos EN, Florentin M, Mikhailidis DP, Elisaf MS. Compliance with lipid-lowering therapy and its impact on cardiovascular morbidity and mortality. Expert Opinion on Drug Safety. 2008;7(6):717–725. doi: 10.1517/14740330802396984. [DOI] [PubMed] [Google Scholar]
- Löckenhoff CE, Sutin AR, Ferrucci L, Costa PT. Personality traits and subjective health in the later years: The association between NEO-PI-R and SF-36 in advanced age is influenced by health status. Journal of Research in Personality. 2008;42:1334–1346. [Google Scholar]
- McCaffery JM, Niaura R, Todaro JF, Swan GE, Carmelli D. Depressive symptoms and metabolic risk in adult male twins enrolled in the National Heart, Lung, and Blood Institute Twin Study. Psychosomatic Medicine. 2003;65:490–497. doi: 10.1097/01.psy.0000041545.52924.82. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT, Terracciano A, Parker WD, Mills CJ, De Fruyt F, et al. Personality trait development from age 12 to age 18: Longitudinal, cross-sectional, and cross-cultural analyses. Journal of Personality and Social Psychology. 2002;83:1456–1468. [PubMed] [Google Scholar]
- McCrae RR, Costa PT. Personality in adulthood: A Five-Factor Theory perspective. 2. New York: Guilford Press; 2003. [Google Scholar]
- Nabi H, Kiviméki M, Zins M, Elovainio M, Consoli SM, Cordier S, et al. Does personality predict mortality: Results from the GAZEL French prospective cohort study. International Journal of Epidemiology. 2008;37:386–396. doi: 10.1093/ije/dyn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilia G, Chen WM, Scuteri A, Orrú M, Albai G, Dei M, et al. Heritability of cardiovascular and personality traits in 6,148 Sardinians. PLoS Genetics. 2006;2:1207–1223. doi: 10.1371/journal.pgen.0020132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, Smith NEI. Personality correlates of physical activity: A review and meta-analysis. British Journal of Sports Medicine. 2006;40:958–965. doi: 10.1136/bjsm.2006.028860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards JC, Hof A, Alvarenga M. Serum lipids and their relationships with hostility and angry affect and behaviors in men. Health Psychology. 2000;19:393–398. doi: 10.1037//0278-6133.19.4.393. [DOI] [PubMed] [Google Scholar]
- Rush CC, Becker SJ, Curry JF. Personality factors and styles among college students who binge eat and drink. Psychology of Addictive Behaviors. 2009;23:140–145. doi: 10.1037/a0013167. [DOI] [PubMed] [Google Scholar]
- Saliba AJ, Wragg K, Richardson P. Sweet taste preference and personality traits using a white wine. Food Quality and Preference in press. [Google Scholar]
- Scherwitz LW, Perkins LL, Chesney MA, Hughes GH, Sidney S, Manolio TA, et al. Hostility and health behaviors in young adults: The CARDIA study. American Journal of Epidemiology. 1992;136:136–145. doi: 10.1093/oxfordjournals.aje.a116480. [DOI] [PubMed] [Google Scholar]
- Shekelle RB, Hulley SB, Neaton JD. The MRFIT behavior pattern study II. Type A behavior and incidence of coronary heart disease. American Journal of Epidemiology. 1985;122:559–570. doi: 10.1093/oxfordjournals.aje.a114135. [DOI] [PubMed] [Google Scholar]
- Shin JY, Suls J, Martin R. Are cholesterol and depression inversely related? A meta-analysis of the association between two cardiac risk factors. Annals of Behavioral Medicine. 2008;36:33–43. doi: 10.1007/s12160-008-9045-8. [DOI] [PubMed] [Google Scholar]
- Shively CA, Register TC, Adams MR, Golden DL, Willard SL, Clarkson TB. Depressive behavior and coronary artery atherogenesis in adult female cynomolgus monkeys. Psychosomatic Medicine. 2008;70:637–645. doi: 10.1097/PSY.0b013e31817eaf0b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons LA, Levis G, Simons J. Apparent discontinuation rates in patients prescribed lipid-lowering drugs. Medical Journal of Australia. 1996;164:208–211. doi: 10.5694/j.1326-5377.1996.tb94138.x. [DOI] [PubMed] [Google Scholar]
- Smith TW. Hostility and health: Current status of a psychosomatic hypothesis. Health Psychology. 1992;11:139–150. doi: 10.1037//0278-6133.11.3.139. [DOI] [PubMed] [Google Scholar]
- Steegmans PHA, Hoes AW, Bak AAA, Van Der Does E, Grobbee DE. Higher prevalence of depressive symptoms in middle-aged men with low serum cholesterol levels. Psychosomatic Medicine. 2000;62:205–211. doi: 10.1097/00006842-200003000-00009. [DOI] [PubMed] [Google Scholar]
- Stewart RA, Sharples KJ, North FM, Menkes DB, Baker J, Simes J. Long-term assessment of psychological well-being in a randomized placebo-controlled trial of cholesterol reduction with pravastatin. Archives of Internal Medicine. 2000;160:3144–3152. doi: 10.1001/archinte.160.20.3144. [DOI] [PubMed] [Google Scholar]
- Stilley CS, Sereika S, Muldoon MF, Ryan CM, Dunbar-Jacob J. Psychological and cognitive function: Predictors of adherence with cholesterol lowering treatment. Annals of Behavioral Medicine. 2004;27:117–124. doi: 10.1207/s15324796abm2702_6. [DOI] [PubMed] [Google Scholar]
- Suarez EC. Relations of trait depression and anxiety to low lipid and lipoprotein concentrations in healthy young adult women. Psychosomatic Medicine. 1999;61:273–279. doi: 10.1097/00006842-199905000-00004. [DOI] [PubMed] [Google Scholar]
- Sutin AR, Terracciano A, Deiana B, Naitza S, Ferrucci L, Uda M, et al. High neuroticism and low conscientiousness are associated with interleukin-6. Psychological Medicine. doi: 10.1017/S0033291709992029. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A. The Italian version of the NEO PI-R: Conceptual and empirical support for the use of targeted rotation. Personality and Individual Differences. 2003;35:1859–1872. doi: 10.1016/S0191-8869(03)00035-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Costa PT. Smoking and the Five-Factor Model of personality. Addiction. 2004;99:472–481. doi: 10.1111/j.1360-0443.2004.00687.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Crum RM, Bienvenu OJ, Costa PT., Jr Five-factor model personality profiles of drug users. BMC Psychiatry. 2008;8 doi: 10.1186/1471-244X-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Löckenhoff CE, Zonderman AB, Ferrucci L, Costa PT. Personality predictors of longevity: Activity, emotional stability, and conscientiousness. Psychosomatic Medicine. 2008;70:621–627. doi: 10.1097/PSY.0b013e31817b9371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, McCrae RR, Brant LJ, Costa PT. Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore Longitudinal Study of Aging. Psychology and Aging. 2005;20:493–506. doi: 10.1037/0882-7974.20.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Terracciano A, Sutin AR, McCrae RR, Deiana B, Ferrucci L, Schlessinger D, et al. Facets of personality linked to underweight and overweight. Psychosomatic Medicine. 2009;71:682–689. doi: 10.1097/PSY.0b013e3181a2925b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toker S, Shirom A, Melamed S. Depression and the metabolic syndrome: Gender-dependent associations. Depression and Anxiety. 2008;25:661–669. doi: 10.1002/da.20379. [DOI] [PubMed] [Google Scholar]
- Troisi A. Cholesterol in coronary heart disease and psychiatric disorders: Same or opposite effects on morbidity risk? Neuroscience and Biobehavioral Reviews. 2009;33:125–132. doi: 10.1016/j.neubiorev.2008.09.003. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The five factor model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. [Google Scholar]
- Williams RB, Haney TL, Lee KL. Type A behavior, hostility, and coronary atherosclerosis. Psychosomatic Medicine. 1980;42:539–549. doi: 10.1097/00006842-198011000-00002. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Mendes De Leon CF, Bienias JL, Evans DA, Bennett DA. Personality and mortality in old age. Journals of Gerontology - Series B Psychological Sciences and Social Sciences. 2004;59:110–116. doi: 10.1093/geronb/59.3.p110. [DOI] [PubMed] [Google Scholar]
- Young-Xu Y, Chan KA, Liao JK, Ravid S, Blatt CM. Long-term statin use and psychological well-being. Journal of the American College of Cardiology. 2003;42:690–697. doi: 10.1016/S0735-1097(03)00785-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.