SUMMARY
We have previously developed and validated a self-administered questionnaire, modeled after the Systemic Lupus International Collaborating Clinics Damage Index (SDI), the Lupus Damage Index Questionnaire (LDIQ), which may allow the ascertainment of this construct in Systemic Lupus Erythematosus (SLE) patients followed in the community and thus expand observations made about damage. We have now translated, back-translated and adapted the LDIQ to Spanish, Portuguese and French and applied it to patients followed at academic and non-academic centers in North and South America, Portugal and Spain while their physicians scored the SDI. A total of 887 patients (659 Spanish-, 140 Portuguese- and 80 French-speaking) and 40 physicians participated. Overall patients scored higher than their physicians (total score and all domains) for all versions of the LDIQ. Infrequent manifestations had less than optional clinimetric properties but overall agreement was over 95% for the majority of items. The larger sample size may explain the higher correlations observed among the Spanish-speaking patients. Pending minor adjustments, the LDIQ may prove to be useful in community-based studies. The relationship between the LDIQ and other outcome parameters is currently being investigated in a different patient sample.
INTRODUCTION
The Systemic Lupus International Collaborating Clinics (SLICC) Damage Index or SDI was developed in 1996 by SLICC investigators in an effort to uniformly quantify the impact of organ damage in systemic lupus erythematosus (SLE) 1,2. This avoided the pitfalls of the parallel development of several instruments to assess the same construct as this had already occurred with disease activity for which instruments were developed in North America and Europe 3–7. To date, the SDI has been used primarily for studies at academic centers rather than in the community and thus the current literature concerning organ damage in SLE may not be reflective of the general SLE population 8–12. Furthermore, like all physicians-completed instruments, the SDI is difficult to apply in longitudinal observational studies in population-based samples, and/or in long-term assessments in clinical trials.
In an effort to ascertain damage in SLE in an unselected population-based sample, we have developed and validated a self-administered questionnaire, the Lupus Damage Index Questionnaire (LDIQ) 13. This instrument has recently been validated using both academic and non-academic practices in North America and the United Kingdom 14. The LDIQ has now been translated into Spanish, Portuguese and French and applied to Spanish-speaking patients in Spain, the USA and Latin America, to Portuguese-speaking patients in Portugal and Brazil and to French-Canadian patients. The results of this exercise are hereby being reported.
METHODS
This study was approved by the Ethics Committee at all participating sites and was conducted according with the Declaration of Helsinki for research in humans.
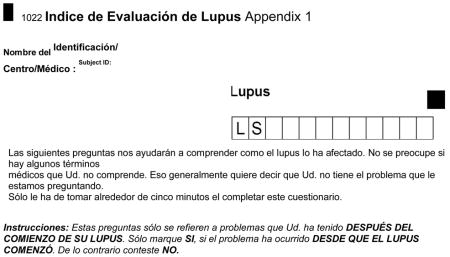
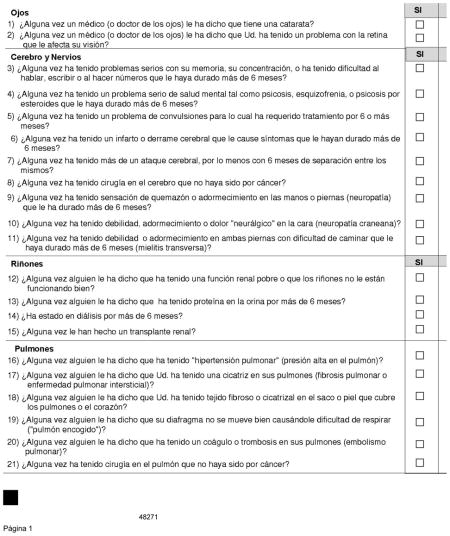
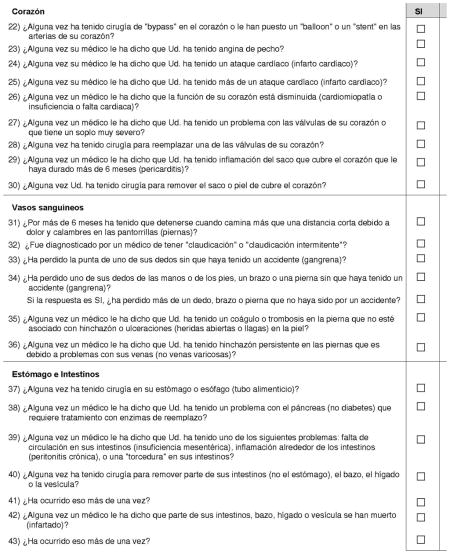
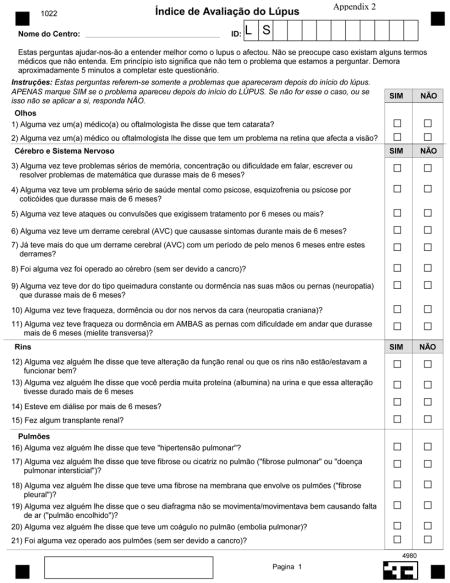
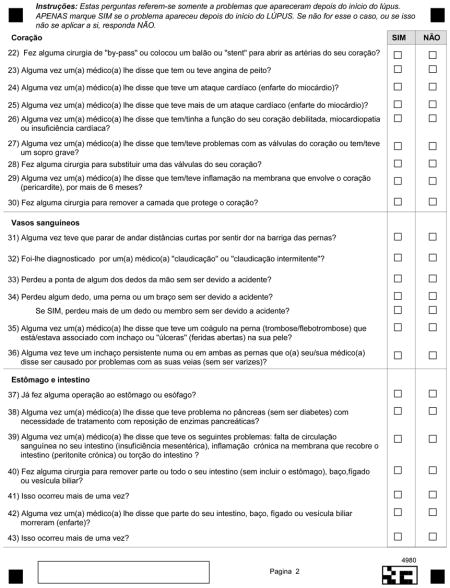
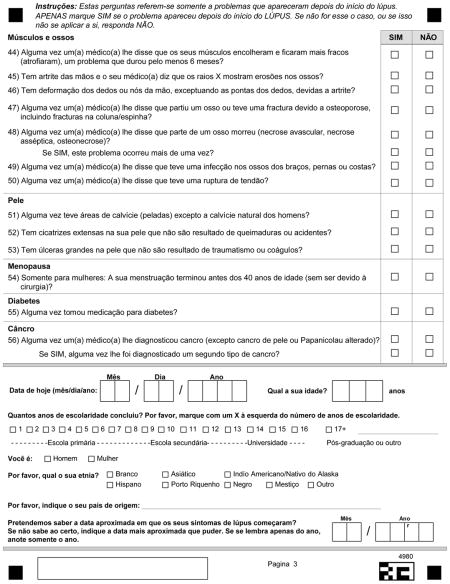
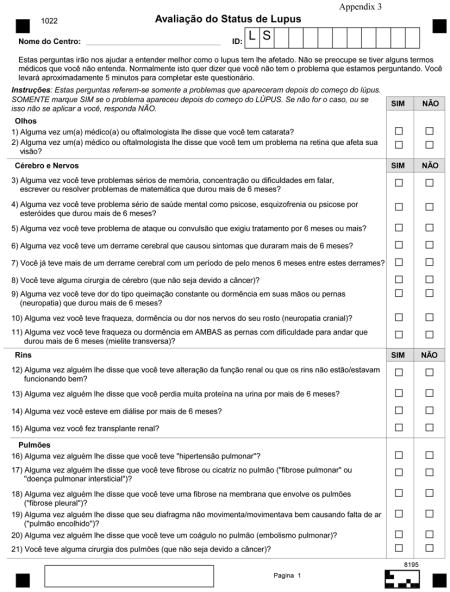
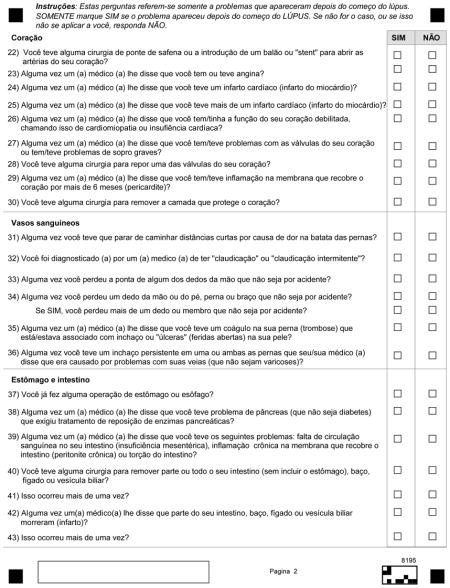
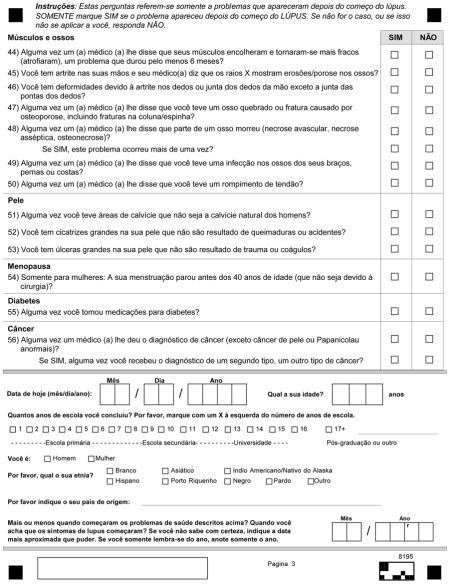
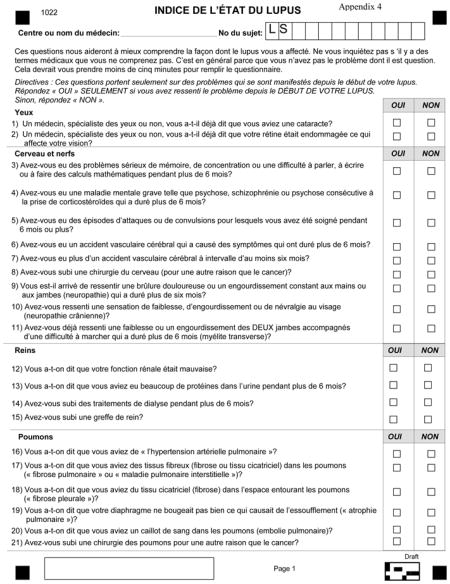
The English version of the LDIQ was translated, back-translated and culturally-adapted to Spanish, Portuguese and French using standard methodology 15. Language variations and cultural differences between Brazil and Portugal required two somewhat different Portuguese versions of the questionnaire as the Brazilian translation was not felt to be adequate by Portuguese investigators; that was not, however, the case for the Spanish questionnaire which after being applied on a pilot basis to few participants in the 31 different Spanish-speaking countries and reviewed by all investigators was felt to be culturally and linguistically-appropriate in all (Appendices 1–4). Next, GLADEL centers (Grupo Latino Americano del Estudio de Lupus or Latin America Group for the Study of Lupus) 16 and other centers in Latin America, the USA, Canada, Spain and Portugal were invited to participate in this study by enrolling consecutive SLE patients attending their practices.
Patients were asked to complete the LDIQ and physicians complete the SDI independently. SDI and LDIQ total and domain scores were computed and compared using the Student’s t-test and Pearson’s correlation coefficients. Using the SDI as the gold standard, the sensitivity, specificity, positive and negative predictive values and overall agreement were calculated for all SDI domain items. For these analyses the Stata, Version 10.1 statistical program (StataCorp College Station, TX) was used.
RESULTS
A total of 887 SLE patients and 40 physicians participated in this study; 659 of the patients completed the Spanish (611 in Latin America, 30 in the US, and 18 in Spain), 140 the Portuguese (122 in Brazil and 18 in Portugal) and 88 the French (all in Canada) versions of the LDIQ. The majority of the patients were women (91%), of middle age (38.3years) with about 10 years of disease duration and 12 years of education. As expected, the majority of the patients were of European and Amerindian and, to a lesser extent, of African ancestry and ethnic background, depending on the location of the participating centers (Table 1). Forty physicians (64% male, mean age 48 years, mean number of years in practice 17, nearly all with formal rheumatology training and experience in the application of the SDI at 33 centers participated in the exercise (Table 1). Twenty-two were GLADEL centers; the others were located in Latin America (n=2), the USA (n=5), Canada (n=2) and one each in Spain and Portugal. The centers in the USA, Canada, Spain and Portugal were all academic whereas in Latin America there were both academic and non-academic. The majority of the patients completed the LDIQ (87%) before seeing their physicians in the clinic. Physicians completed the SDI by interview and physical examination although access to medical records was allowed.
Table 1.
Characteristics of Systemic Lupus Erythematosus Patients Participating in Study (n=887)
| Language | |
| Spanish | 659 |
| USA | 30 |
| Spain | 18 |
| Latin American | 611 |
| Portuguese | 140 |
| Brazil | 122 |
| Portugal | 18 |
| French | |
| Canada | 88 |
| Gender, % women | 91.0 |
| Age, years, mean (SD) | 38.3 (13.2) |
| Disease duration, years, mean (SD) | 10.1 (8.2) |
| Education, years, mean (SD) | 12.0 (3.9) |
| Ethnicity, % | |
| Caucasian | 54.2 |
| Hispanic (Amerindian and Caucasian) | 34.2 |
| African | 6.5 |
| Other | 5.1 |
Table 2 shows the SDI and LDIQ mean (standard deviation), SDI total and domain scores for all physicians and for the Spanish-, Portuguese-, and French-speaking patients separate and combined. As noted, patients, overall, tended to score higher than their physicians and that was the case for nearly every domain of the SDI and for the Spanish-, Portuguese-, and French-speaking patient groups. For example, the total mean (SD) damage score was 3.72 (3.15) for the Spanish-, 4.09 (3.17) for the Portuguese- and 2.69 (2.93) for the French-speaking patients; these contrast with mean (SD) damage scores of 2.13 (2.50), 1.45 (1.64) and 1.25 (1.74), respectively for their physicians. The comparisons were all significant at p<0.01. Table 3 depicts the correlations between the SDI and the LDIQ scores for the damage index overall and for its domains. These correlations were highest for the ocular domain across the three groups and were overall higher for the Spanish questionnaires than for the French and Portuguese. In Appendix 5, the sensitivity, specificity, positive and negative predictive values and overall agreement (percent of patient’s correctly classified by patients and physicians) for all items on the different domains of the SDI and LDIQ are shown. Overall, infrequent manifestations had less than optimal clinimetric properties but the overall agreement was over 95% for the majority of the items. Of interest, similar results were obtained when the data were examined by individual investigator and compared between those in academic and non-academic centers (data not shown).
Table 2.
Mean Total and Domain Scores for the SLICC Damage Index (SDI) from Forty Physicians and the Lupus Damage Index Questionnaire (LDIQ) from Eight hundred eighty-seven Patients by Language Version
| Damage Domains mean (SD) | Spanish | Portuguese | French | All | ||||
|---|---|---|---|---|---|---|---|---|
| Physicians | Patients | Physicians | Patients | Physicians | Patients | Physicians | Patients | |
| SDI | LDIQ | SDI | LDIQ | SDI | LDIQ | SDI | LDIQ | |
| n=33 | n=659 | n=6 | n=140 | n=1 | n=88 | n=40 | n=887 | |
| Ocular | 0.14 (0.38) | 0.22 (0.45)* | 0.19 (0.45) | 0.23 (0.48) | 0.17 (0.04) | 0.22 (0.05)* | 0.15 (0.01) | 0.22 (0.02) |
| Neuropsychiatric | 0.32 (0.72) | 0.61 (0.97)* | 0.21 (0.56) | 0.89 (1.11) | 0.17 (0.04) | 0.42 (0.09) | 0.29 (0.02) | 0.64 (0.03) |
| Renal | 0.29 (0.62) | 0.74 (0.87)* | 0.14 (0.44) | 0.88 (0.87) | 0.10 (0.03) | 0.44 (0.08) | 0.25 (0.02) | 0.73 (0.03) |
| Pulmonary | 0.17 (0.59) | 0.25 (0.74)* | 0.11 (0.37) | 0.25 (0.61) | 0.05 (0.02) | 0.19 (0.05) | 0.15 (0.02) | 0.25 (0.02) |
| Cardiovascular | 0.09 (0.37) | 0.18 (0.53)* | 0.12 (0.42) | 0.14 (0.38) | 0.07 (0.03) | 0.32 (0.08) | 0.09 (0.01) | 0.19 (0.02) |
| Peripheral vascular | 0.16 (0.45) | 0.18 (0.49)† | 0.08 (0.32) | 0.31 (0.64) | 0.11 (0.04) | 0.16 (0.05)† | 0.14 (0.01) | 0.20 (0.02) |
| Gastrointestinal | 0.09 (0.32) | 0.13 (0.43) | 0.02 (0.15) | 0.11 (0.50) | 0.07 (0.03) | 0.15 (0.04) | 0.08 (0.01) | 0.13 (0.01) |
| Musculoskeletal | 0.32 (0.72) | 0.45 (0.79) | 0.21 (0.52) | 0.55 (0.95) | 0.27 (0.08) | 0.38 (0.10)† | 0.30 (0.02) | 0.46 (0.03) |
| Integument | 0.38 (0.61) | 0.75 (0.73) | 0.20 (0.42) | 0.48 (0.63) | 0.14 (0.04) | 0.24 (0.06)* | 0.33 (0.02) | 0.66 (0.02) |
| Gonadal | 0.11 (0.31) | 0.14 (0.34) | 0.09 (0.28) | 0.15 (0.36) | 0.05 (0.02) | 0.09 (0.03)† | 0.10 (0.01) | 0.13 (0.01) |
| Malignancy | 0.03 (0.16) | 0.02 (0.17)† | 0.02 (0.15) | 0.04 (0.22)† | 0.05 (0.02) | 0.07 (0.02)† | 0.03 (0.01) | 0.03 (0.01)† |
| Diabetes | 0.04 (0.19) | 0.03 (0.18)† | 0.06 (0.23) | 0.08 (0.27)† | 0.01 (0.02) | 0.02 (0.01)† | 0.04 (0.01) | 0.04 (0.01)† |
| Total | 2.13 (2.50) | 3.72 (3.15) | 1.45 (1.64) | 4.09 (3.17) | 1.25 (1.74) | 2.69 (2.93) | 1.94 (2.34) | 3.68 (3.16) |
All comparisons are statistically significant at p<0.01 except as noted
p<0.05>0.01; and
non-significant.
Table 3.
Pearson’s Correlations Between the Total and Domain Scores* of the Lupus Damage Index Questionnaire and the SLICC Damage Index
| SLICC Damage Index Domains | Spanish | Portuguese | French | All |
|---|---|---|---|---|
| Ocular | 0.76 | 0.66 | 0.75 | 0.74 |
| Neuropsychiatric | 0.59 | 0.43 | 0.37 | 0.54 |
| Renal | 0.55 | 0.35 | 0.36 | 0.51 |
| Pulmonary | 0.52 | 0.54 | 0.25 | 0.51 |
| Cardiovascular | 0.55 | 0.03 | 0.11 | 0.41 |
| Peripheral vascular | 0.59 | 0.20 | 0.68 | 0.52 |
| Gastrointestinal | 0.61 | 0.26 | 0.23 | 0.52 |
| Musculoskeletal | 0.67 | 0.28 | 0.30 | 0.56 |
| Integument | 0.54 | 0.28 | 0.45 | 0.52 |
| Gonadal | 0.66 | 0.51 | 0.50 | 0.63 |
| Malignancy | 0.57 | 0.20 | 0.81 | 0.55 |
| Diabetes† | 0.70 | 0.50 | - | 0.61 |
| Total | 0.68 | 0.37 | 0.43 | 0.61 |
There were 887 patients and 40 physicians (659/33 Spanish-speaking, 140/6 Portuguese-speaking and 88/1 French-speaking); no cases of diabetes was observed among the French-speaking patients, so this correlation could not be computed
DISCUSSION
We have now translated, adapted and validated Spanish, Portuguese and French versions of the LDIQ, a self-administered questionnaire modeled after the SDI. Similar to our initial preliminary experience with the English version of the LDIQ 13 and the most recent assessment in a larger sample 14, we have shown that patients consistently score higher than physicians in the different items and domains that constitute this index. This held true across Spanish-speaking patients in Latin America, the USA and Spain, Portuguese-speaking patients in Brazil and Portugal and French-Canadian patients. One caveat is that our studies, so far, have been cross-sectional, and the properties of the LDIQ may differ in the context of longitudinal observational studies.
The best correlations between patients’ and physicians scores were observed for the Spanish-speaking patients (0.52 for the pulmonary domain to 0.76 for the ocular domain and 0.68 for the total score) whereas there was significant variability for the French- and the Portuguese-speaking patients which may be due to the smaller sample size of these samples as compared to the Spanish sample or to the lack of understanding of the questions as worded which could also relate to a lower level of education among the Portuguese-speaking patients, particularly those in Brazil (10.5 years vs.12.0 for the Spanish-speaking patients). However, level of education cannot be the sole reason as the French-speaking patients were the ones with the highest level of education (~14 years). Thus, some items of the Portuguese and French versions may need to be reworded before the instrument is used in community-based longitudinal observational studies or clinical trials. Nevertheless, the large majority of the items were correctly classified by patients and physicians, with the exception of those which occurred infrequently. In all three cases, however, the highest correlations were obtained for the ocular domain of the SDI whereas the lowest were for the pulmonary domain for the Spanish-speaking patients and for the cardiovascular domain for the French- and Portuguese-speaking patients.
In summary, our study suggests that both the original SDI and the self-administered LDIQ reflect the same domains although the two instruments appear to measure these domains with different types and degrees of error; minor adjustments, however, may still need to be done to the Portuguese and French questionnaires. Additional studies to ascertain the relationship between this questionnaire and other outcome measurements are in progress. Longitudinal assessments, likewise, may provide additional information about the value of this instrument. If proven reliable in the longitudinal setting, the LDIQ would be invaluable in SLE research, longitudinal observational studies in population based samples, and long-term outcome assessments in clinical trials.
Acknowledgments
To Amy Yearout from the National Bank of Rheumatic Diseases for assisting with all administrative aspects of the study, to the many persons who help with patient recruitment at the different participating sites, to Maria Tyson, AA for her expert assistance in the preparation of this manuscript and, most importantly, to all participating patients across the different centers for given generously of their time and making this study possible.
The work of Dr. Karlson was supported by NIH grants R01AR49880, P60 AR047782 and K24 AR 052401, of Dr. Costenbader by The American College of Rheumatology, The Arthritis Foundation and NIH grants P60 AR047782, of Dr. Alarcón by NIH-P01 AR49084, and of Drs. Bonfa and Pons-Estel by the Federico Wihelm Agricola Foundation Research grant. Administrative, programming, printing, postage, and analyses costs for this study were underwritten by the National Data Bank of Rheumatic Diseases, Wichita, Kansas.
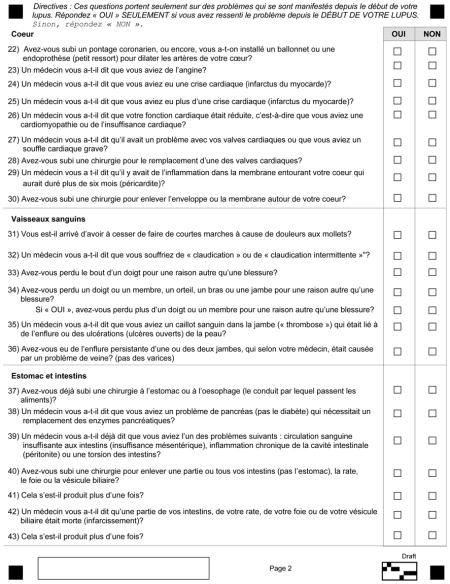
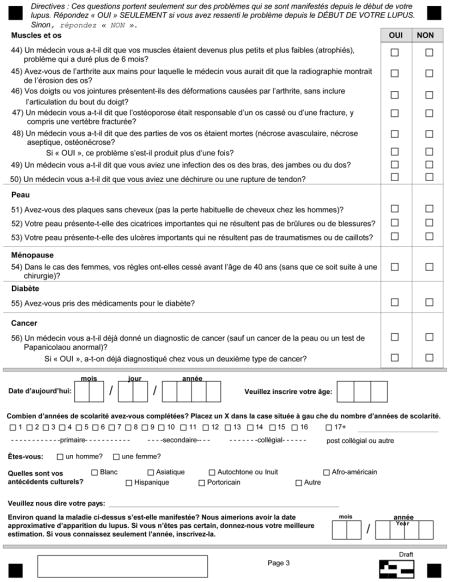
Appendix 1
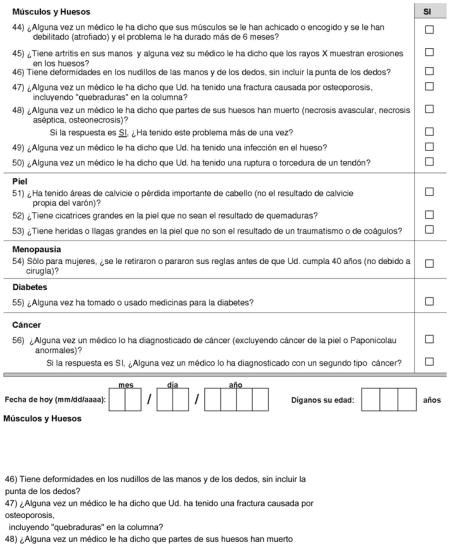
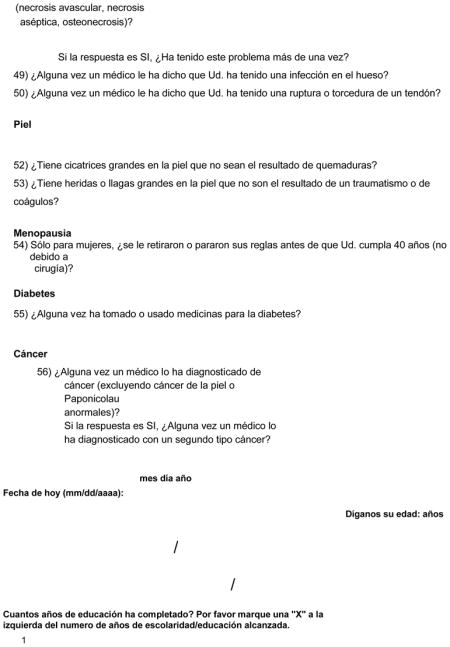
Appendix 2
Appendix 3
Appendix 4
Appendix 5
Items of the Different Domains of the Damage Index: Prevalence and Clinimetric Properties*
| Damage Item | Prevalence, % | Sensitivity, % | Specificity, % | PPV, †% | NPV, †% | Agreement, % | ROC‡ |
|---|---|---|---|---|---|---|---|
| CATARACT | |||||||
| Spanish | 9.6 | 93.7 | 97.3 | 78.7 | 99.3 | 97.0 | 0.95 |
| Portuguese | 10.0 | 78.6 | 96.0 | 68.8 | 97.6 | 94.3 | 0.87 |
| French | 14.8 | 92.3 | 93.3 | 70.6 | 98.6 | 93.2 | 0.93 |
| All | 10.1 | 91.1 | 96.7 | 75.9 | 99.0 | 96.2 | 0.94 |
| RETINAL DAMAGE | |||||||
| Spanish | 4.7 | 90.3 | 93.6 | 41.2 | 99.5 | 95.3 | 0.92 |
| Portuguese | 9.3 | 53.8 | 92.9 | 43.8 | 95.2 | 90.7 | 0.73 |
| French | 2.3 | 50.0 | 98.8 | 50.0 | 98.8 | 97.7 | 0.74 |
| All | 5.2 | 78.3 | 94.1 | 41.9 | 98.8 | 94.8 | 0.86 |
| SEIZURES | |||||||
| Spanish | 5.2 | 82.4 | 98.4 | 73.7 | 99.0 | 97.6 | 0.90 |
| Portuguese | 5.7 | 100.0 | 93.9 | 50.0 | 100.0 | 50.0 | 0.97 |
| French | 4.5 | 25.0 | 95.2 | 20.0 | 96.4 | 95.5 | 0.60 |
| All | 5.2 | 80.4 | 97.4 | 62.7 | 98.9 | 96.5 | 0.89 |
| STROKE | |||||||
| Spanish | 0.8 | 60.0 | 99.2 | 37.5 | 99.7 | 96.5 | 0.80 |
| Portuguese | 0.7 | 0.0 | 98.6 | 0.0 | 99.3 | 91.4 | 0.49 |
| French | - | - | - | - | - | - | - |
| All | 0.7 | 50.0 | 99.2 | 30.0 | 99.7 | 95.3 | 0.75 |
| NEUROPATHY | |||||||
| Spanish | 6.7 | 77.3 | 82.8 | 24.3 | 98.1 | 93.3 | 0.80 |
| Portuguese | 2.1 | 66.7 | 70.8 | 4.8 | 99.0 | 97.9 | 0.69 |
| French | 3.4 | 33.3 | 84.7 | 7.1 | 97.3 | 96.6 | 0.59 |
| All | 5.6 | 74.0 | 81.0 | 18.9 | 98.1 | 94.4 | 0.78 |
| TRANSVERSE MYELITIS | |||||||
| Spanish | 2.3 | 80.0 | 89.9 | 15.6 | 99.5 | 97.7 | 0.85 |
| Portuguese | 0.7 | 100.0 | 79.1 | 3.3 | 100.0 | 96.7 | 0.90 |
| French | 2.3 | 50.0 | 94.2 | 16.7 | 98.8 | 97.7 | 0.72 |
| All | 2.0 | 77.8 | 88.6 | 12.4 | 99.5 | 98.0 | 0.83 |
| COGNITIVE DYSFUNCTION/PSYCHOSIS | |||||||
| Spanish | 12.1 | 75.0 | 91.0 | 53.6 | 96.3 | 89.1 | 0.83 |
| Portuguese | 4.3 | 83.3 | 85.1 | 20.0 | 99.1 | 95.7 | 0.84 |
| French | - | - | - | - | - | - | - |
| All | 10.1 | 73.3 | 87.8 | 44.9 | 96.8 | 89.9 | 0.82 |
| PROTEINURIA/ENDSTAGE RENAL DISEASE | |||||||
| Spanish | 17.6 | 89.7 | 75.9 | 44.3 | 97.2 | 82.4 | 0.83 |
| Portuguese | 10.0 | 85.7 | 70.6 | 24.5 | 97.8 | 90.0 | 0.78 |
| French | - | - | - | - | - | - | - |
| All | 15.0 | 88.0 | 75.3 | 38.6 | 97.3 | 85.0 | 0.82 |
| DECREASED GLOMERULAR FILTRATION RATE | |||||||
| Spanish | 11.5 | 94.7 | 69.0 | 28.5 | 99.0 | 88.5 | 0.82 |
| Portuguese | 4.3 | 100.0 | 49.3 | 8.1 | 100.0 | 91.9 | 0.75 |
| French | 6.8 | 100.0 | 82.9 | 30.0 | 100..0 | 70.0 | 0.91 |
| All | 9.9 | 95.5 | 67.1 | 24.2 | 99.3 | 90.1 | 0..81 |
| PULMONARY HYPERTENSION | |||||||
| Spanish | 3.8 | 60.0 | 98.7 | 65.2 | 98.4 | 97.3 | 0.79 |
| Portuguese | 3.6 | 60.0 | 97.0 | 42.9 | 98.5 | 96.4 | 0.79 |
| French | 3.4 | 66.7 | 98.8 | 66.7 | 98.8 | 97.7 | 0.83 |
| All | 3.7 | 60.6 | 98.5 | 60.6 | 98.5 | 97.1 | 0.80 |
| PULMONARY FIBROSIS | |||||||
| Spanish | 5.2 | 61.8 | 97.3 | 55.3 | 97.9 | 95.4 | 0.80 |
| Portuguese | 4.3 | 0.0 | 98.5 | 0.0 | 95.7 | 95.6 | 0.49 |
| French | 1.1 | 100.0 | 97.7 | 33.3 | 100.0 | 66.6 | 0.99 |
| All | 4.6 | 53.7 | 97.5 | 51.2 | 97.7 | 95.5 | 0.76 |
| SHRINKING LUNG | |||||||
| Spanish | 2.1 | 57.1 | 94.3 | 17.8 | 99.0 | 97.9 | 99.4 |
| Portuguese | - | - | - | - | - | - | - |
| French | - | - | - | - | - | - | - |
| All | 1.6 | 57.1 | 93.7 | 12.7 | 99.3 | 98.4 | 0.75 |
| PLEURAL FIBROSIS | |||||||
| Spanish | 2.7 | 55.6 | 96.4 | 30.3 | 98.7 | 97.3 | 0.76 |
| Portuguese | 1.4 | 100.0 | 97.8 | 40.0 | 100.0 | 60.0 | 0.99 |
| French | - | - | - | - | - | - | - |
| All | 2.3 | 60.0 | 96.8 | 30.0 | 99.1 | 97.7 | 0.78 |
| PULMONARY INFARCTION | |||||||
| Spanish | 2.9 | 73.7 | 97.8 | 50.0 | 99.2 | 97.1 | 0.86 |
| Portuguese | 1.4 | 100.0 | 97.8 | 40.0 | 100.0 | 60.0 | 0.99 |
| French | - | - | - | - | - | - | - |
| All | 2.4 | 76.2 | 97.2 | 40.0 | 99.4 | 97.6 | 0.87 |
| ANGINA/SURGERY | |||||||
| Spanish | 0.9 | 66.7 | 98.2 | 25.0 | 99.7 | 99.1 | 0.82 |
| Portuguese | 1.4 | 0.0 | 99.3 | 0.0 | 98.6 | 98.6 | 0.50 |
| French | 1.1 | 100.0 | 95.4 | 20.0 | 100.0 | 80.0 | 0.98 |
| All | 1.0 | 55.6 | 98.1 | 22.7 | 99.5 | 99.0 | 0.77 |
| MYOCARDIAL INFARCTION | |||||||
| Spanish | 0.9 | 16.7 | 99.8 | 50.0 | 99.2 | 99.1 | 0.58 |
| Portuguese | 0.7 | 0.0 | 99.3 | 0.0 | 99.3 | 99.3 | 0.50 |
| French | - | - | - | - | - | - | - |
| All | 0.8 | 14.3 | 99.7 | 25.0 | 99.3 | 99.0 | 0.57 |
| CARDIOMYOPATHY | |||||||
| Spanish | 1.8 | 83.3 | 96.8 | 32.3 | 99.7 | 98.2 | 0.90 |
| Portuguese | 5.0 | 14.3 | 97.0 | 20.0 | 95.6 | 95.0 | 0.56 |
| French | - | - | - | - | - | - | - |
| All | 2.1 | 57.9 | 96.8 | 28.2 | 99.1 | 97.9 | 0.77 |
| VAVULAR DISEASE | |||||||
| Spanish | 2.0 | 69.2 | 97.1 | 32.1 | 99.4 | 98.0 | 0.83 |
| Portuguese | - | - | - | - | - | - | - |
| French | 2.3 | 0.0 | 93.0 | 0.0 | 97.6 | 97.6 | 0.47 |
| All | 1.7 | 60.0 | 96.4 | 22..5 | 99.3 | 98.3 | 0.78 |
| PERICARDITIS/PERICARDIECTOMY | |||||||
| Spanish | 3..5 | 73.9 | 97.3 | 50.0 | 99.0 | 96.5 | 0.86 |
| Portuguese | 5.0 | 14.3 | 97.7 | 25.0 | 95.6 | 95.0 | 0.56 |
| French | 3.4 | 0.0 | 88.2 | 0.0 | 96.2 | 96.2 | 0.44 |
| All | 3.7 | 54.5 | 96.5 | 37.5 | 98.2 | 96.3 | 0.76 |
| CLAUDICATION | |||||||
| Spanish | 3.9 | 15.4 | 99.1 | 40.0 | 96.6 | 96.1 | 0.57 |
| Portuguese | 0.7 | 0.0 | 95.7 | 0.0 | 99.3 | 99.3 | 0.48 |
| French | - | - | - | - | - | - | - |
| All | 3.0 | 14.8 | 98.5 | 23.5 | 97.4 | 97.0 | 0.57 |
| MINOR TISSUE LOSS | |||||||
| Spanish | 2.4 | 62.5 | 99.4 | 71.4 | 99.1 | 98.5 | 0.81 |
| Portuguese | 2.9 | 50.0 | 97.8 | 40.0 | 98.5 | 97.1 | 0.74 |
| French | - | - | - | - | - | - | - |
| All | 2.5 | 54.5 | 99.2 | 63.2 | 98.8 | 98.1 | 0.77 |
| SIGNIFICANT TISSUE LOSS | |||||||
| Spanish | 0.3 | 0.0 | 100.0 | 0.0 | 99.7 | 98.9 | 0.50 |
| Portuguese | 0.7 | 0.0 | 99.3 | 0.0 | 99.3 | 99.3 | 0.50 |
| French | - | - | - | - | - | - | - |
| All | 0.3 | 33.3 | 99.4 | 16.7 | 99.8 | 98.9 | 0..66 |
| VENOUS THROMBOSIS | |||||||
| Spanish | 7.4 | 77.6 | 92.8 | 46.3 | 98.1 | 92..6 | 0.85 |
| Portuguese | 3.6 | 80.0 | 82..2 | 14.3 | 99.1 | 96.4 | 0.81 |
| French | - | - | - | - | - | - | - |
| All | 6.5 | 75.9 | 91.1 | 37.3 | 98..2 | 93.5 | 0.83 |
| GASTRO INTESTINAL INFARCTION | |||||||
| Spanish | 5.9 | 10.3 | 99.5 | 57.1 | 94.6 | 94.2 | 0.55 |
| Portuguese | 2.1 | 0.0 | 99.3 | 0.0 | 97.8 | 97.1 | 0.50 |
| French | - | - | - | - | - | - | - |
| All | 5.2 | 8.7 | 99.5 | 50.0 | 95.2 | 94.8 | 0.54 |
| MESENTERIC INSUFFICIENCY | |||||||
| Spanish | 1.2 | 100.0 | 97.8 | 36.4 | 100.0 | 63.6 | 0.99 |
| Portuguese | - | - | - | - | - | - | - |
| French | - | - | - | - | - | - | - |
| All | 1.0 | 88.9 | 97.4 | 25.8 | 99.9 | 99.0 | 0.93 |
| GASTRO INTESTINAL STRICTURE/SURGERY | |||||||
| Spanish | 1.1 | 0.0 | 99.2 | 0.0 | 98.9 | 98.9 | 0.50 |
| Portuguese | - | - | - | - | - | - | - |
| French | - | - | - | - | - | - | - |
| All | 0.8 | 0.0 | 99.0 | 0.0 | 99.2 | 99.2 | 0.49 |
| PANCREATIC INSUFFICIENCY | |||||||
| Spanish | 0.5 | 100.0 | 99.7 | 60.0 | 100.0 | 60.0 | 1.00 |
| Portuguese | - | - | - | - | - | - | |
| French | - | - | - | - | - | - | - |
| All | 0.3 | 100.0 | 99.4 | 37.5 | 100.0 | 62.5 | 1.00 |
| MUSCLE ATROPHY | |||||||
| Spanish | 7.1 | 55.3 | 95.9 | 51.0 | 96.5 | 93.0 | 0..76 |
| Portuguese | 7.1 | 10.0 | 93.8 | 11.1 | 93.1 | 92.9 | 0.52 |
| French | - | - | - | - | - | - | - |
| All | 6.8 | 45.0 | 95.5 | 42.2 | 96.0 | 93.2 | 0.70 |
| ARTHRITIS (DEFORMING) | |||||||
| Spanish | 11.1 | 84.9 | 85.8 | 42.8 | 97.9 | 88.9 | 0.85 |
| Portuguese | 2.9 | 75.0 | 78.7 | 9.4 | 99.1 | 97.1 | 0.77 |
| French | - | - | - | - | - | - | - |
| All | 9.5 | 79.8 | 84.7 | 35..3 | 97.6 | 90.5 | 0.82 |
| OSTEOPOROTIC FRACTURE | |||||||
| Spanish | 3.3 | 59.1 | 98.7 | 61.9 | 98.6 | 97.4 | 0.79 |
| Portuguese | 2.9 | 50.0 | 97.1 | 33.3 | 98.5 | 97.1 | 0.74 |
| French | - | - | - | - | - | - | - |
| All | 3.2 | 57.1 | 98.1 | 50.0 | 98.0 | 96.8 | 0.78 |
| AVASCULAR NECROSIS | |||||||
| Spanish | 2.3 | 40.0 | 99.4 | 60.0 | 98.6 | 97.3 | 0.70 |
| Portuguese | 2.1 | 0.0 | 98.5 | 0.0 | 97.8 | 93.6 | 0.49 |
| French | - | - | - | - | - | - | - |
| All | 2.5 | 40.9 | 99.3 | 60.0 | 98.5 | 95.6 | 0.70 |
| OSTEOMYELITIS | |||||||
| Spanish | 1.2 | 75.0 | 99.4 | 60.0 | 99.7 | 99.1 | 0.87 |
| Portuguese | - | - | - | - | - | - | - |
| French | - | - | - | - | - | - | - |
| All | 1.0 | 66.7 | 98.2 | 27.3 | 99.7 | 99.0 | 0.82 |
| RUPTURED TENDON | |||||||
| Spanish | 1.7 | 81.8 | 96.1 | 26.5 | 99.7 | 98.3 | 0.89 |
| Portuguese | - | - | - | - | - | - | - |
| French | - | - | - | - | - | - | - |
| All | 1.2 | 81.8 | 96.0 | 20.5 | 99.8 | 98.8 | 0.89 |
| ALOPECIA | |||||||
| Spanish | 28.1 | 95.7 | 67.5 | 53.5 | 97.6 | 75.4 | 0.82 |
| Portuguese | 17.1 | 62.5 | 79.3 | 38.5 | 91.1 | 82.9 | 0.71 |
| French | - | - | - | - | - | - | - |
| All | 24.7 | 90.0 | 72.6 | 51.8 | 95.7 | 76.9 | 0.81 |
| SKIN SCARRING | |||||||
| Spanish | 10.3 | 86.8 | 82.1 | 35.8 | 98.2 | 89.7 | 0.84 |
| Portuguese | 2.9 | 50.0 | 80.9 | 7.1 | 98.2 | 97.1 | 0.65 |
| French | - | - | - | - | - | - | - |
| All | 8.3 | 85.1 | 82.7 | 30.9 | 98.4 | 91.7 | 0.84 |
| PREMATURE GONADAL FAILURE | |||||||
| Spanish | 10.8 | 78.9 | 94.2 | 62.2 | 97.4 | 92.6 | 0.87 |
| Portuguese | 8.6 | 75.0 | 90.6 | 42.9 | 97.5 | 91.4 | 0.83 |
| French | - | - | - | - | - | - | - |
| All | 9.8 | 78.2 | 93.6 | 57.1 | 97.5 | 92.1 | 0.86 |
| MALIGNANCY | |||||||
| Spanish | 2.7 | 11.1 | 99.8 | 66.7 | 97.6 | 98.3 | 0.55 |
| Portuguese | 2.1 | 0.0 | 99.3 | 0.0 | 97.8 | 97.9 | 0.50 |
| French | - | - | - | - | - | - | - |
| All | 2.8 | 8.0 | 99.8 | 50.0 | 97.4 | 97.2 | 0.54 |
| DIABETES | |||||||
| Spanish | 3.8 | 68.0 | 99.1 | 73.9 | 98.7 | 97.9 | 0.84 |
| Portuguese | 5.7 | 62.5 | 95.5 | 45.5 | 97.7 | 94.3 | 0.79 |
| French | - | - | - | - | - | - | - |
| All | 3.8 | 64.7 | 98.4 | 61.1 | 98.6 | 97.1 | 0.82 |
Blanks in this table correspond to cases in which these metrics could not be calculated with the statistical program used;
positive and negative predictive values, respectively;
Receiving operating curve.
Appendix 6
AFFILIATIONS OF GLADEL AUTHORS
Bernardo A. Pons-Estel
Servicio de Reumatología, Hospital Provincial de Rosario. Rosario, Argentina.
Antonio Iglesias-Gamarra
Facultad de Medicina, Universidad Nacional de Colombia, Bogotá, Colombia.
Eloisa Bonfa
Divisao de Reumatología, Faculdade da Medicina, Universidade da São Paulo, São Paulo, Brazil.
Eduardo Ferreira Borba Neto
Divisao de Reumatología, Faculdade da Medicina, Universidade da São Paulo, São Paulo, Brazil.
Samuel K. Shinjo
Divisao de Reumatología, Faculdade da Medicina, Universidade da São Paulo, São Paulo, Brazil.
Mercedes A. Garcia
Servicio de Reumatología, Hospital Interzonal General de Agudos General San Martín, La Plata, Argentina.
Juan Carlos Marcos
Servicio de Reumatología, Hospital Interzonal General de Agudos General San Martín, La Plata, Argentina
Ângela Duarte
Disciplina de Reumatología, Centro de Ciências da Saúde, Universidade Federal da Pernambuco, Pernambuco, Brazil.
Guillermo A. Berbotto
Servicio de Reumatología Hospital Escuela Eva Perón, Granadero Baigorria, Rosario, Argentina.
Hugo R. Scherbarth
Servicio de Reumatología, Hospital Interzonal General de Agudos “Dr Oscar Alende”, Mar del Plata, Argentina.
Claudia D. Marquez
Disciplina de Reumatología, Centro de Ciências da Saúde, Universidade Federal da Pernambuco, Pernambuco, Brazil.
Laura Onetti
Servicio de Reumatología, UHMI1, Hospital Nacional de Clínicas, Córdoba, Argentina.
Veronica Saurit
Servicio de Reumatología, Hospital Privado, Centro Médico de Córdoba, Córdoba, Argentina.
Emilia Sato
Disciplina de Reumatología, Universidade Federal da São Paulo (UNIFESP), São Paulo, Brazil.
Luis J. Catoggio
Sección Reumatología, Servicio de Clínica Médica Hospital Italiano and Fundación Dr. Pedro M. Catoggio para el Progreso de la Reumatología, Buenos Aires, Argentina.
Oscar J. Neira Quiroga
Sección Reumatología, Hospital del Salvador, Facultad de Medicina, Universidad de Chile, Santiago, Chile.
Paula Burgos
Departamento de Inmunología Clínica y Reumatología, Escuela de Medicina, Pontificia Universidad Católica de Chile, Santiago, Chile.
Luis Alberto Ramírez
Sección de Reumatología, Universidad de Antioquia, Hospital Universitario San Vicente de Paúl. Medellín, Colombia.
José Fernando Molina
Servicio de Reumatología, Hospital Pablo Tobon Uribe, Medellín, Colombia.
Ignacio García De La Torre
Departamento de Inmunología y Reumatología, Hospital General de Occidente de la Secretaría de Salud, Guadalajara, Jalisco, México.
Ricardo Silvariño Di Rago
Clínica Médica C, Hospital de Clínicas, Universidad de la República, Montevideo, Uruguay.
Jorge A. Manni
Departamento de Inmunología, Instituto de Investigaciones Médicas “Alfredo Lanari”, Buenos Aires, Argentina.
Margarita Portela
Unidad de Investigación Médica en Epidemiología Clínica, Hospital de Especialidades Centro Médico Nacional SXXI, Instituto Mexicano del Seguro Social, México D.F., México.
Maria Hercilia Esteva Spinetti
Unidad de Reumatología, Hospital Central de San Cristóbal, San Cristóbal, Venezuela.
Eduardo M. Acevedo Vásquez
Servicio de Reumatología, Hospital Nacional Guillermo Almenara Irigoyen, Essalud, Lima, Perú.
Maria Inés Segami Salazar
Servicio de Reumatología, Hospital Nacional Edgardo Rebagliatti Martins, Essalud, Lima, Perú.
Silvana B. Gentiletti
Servicio de Reumatología, Hospital Provincial de Rosario. Rosario, Argentina
Reference List
- 1.Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. The development and initial validation of the systemic lupus international collaborating clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 1996;39:363–9. doi: 10.1002/art.1780390303. [DOI] [PubMed] [Google Scholar]
- 2.Gladman DD, Urowitz MB, Goldsmith CH, Fortin P, Ginzler E, Gordon C, et al. The reliability of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology Damage Index in patients with systemic lupus erythematosus. Arthritis Rheum. 1997;40:809–13. doi: 10.1002/art.1780400506. [DOI] [PubMed] [Google Scholar]
- 3.Hay E, Bacon P, Gordon C. The BILAG index: a reliable and valid instrument for measuring clinical disease activity in systemic lupus erythematosus. QJM. 1993;86:447–58. [PubMed] [Google Scholar]
- 4.Vitali C, Bencivelli W, Mosca M, Carrai P, Sereni M, Bombardieri S. Development of a clinical chart to compute different disease activity indices for systemic lupus erythematosus. J Rheumatol. 1999;26:498–501. [PubMed] [Google Scholar]
- 5.Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH the Committee on Prognosis Studies in SLE. Derivation of the SLEDAI. A disease activity index for lupus patients. Arthritis Rheum. 1992;35:630–40. doi: 10.1002/art.1780350606. [DOI] [PubMed] [Google Scholar]
- 6.Gladman DD, Goldsmith CH, Urowitz MB, Bacon P, Bombardier C, Isenberg D, et al. Sensitivity to change of 3 systemic lupus erythematosus disease activity indices: International validation. J Rheumatol. 1994;21:1468–71. [PubMed] [Google Scholar]
- 7.Hawker G, Gabriel S, Bombardier C, Goldsmith C, Caron D, Gladman D. A reliability study of SLEDAI: A disese activity index for systemic lupus erythematosus. J Rheumatol. 1993;20:657–60. [PubMed] [Google Scholar]
- 8.Gladman DD, Urowitz MB, Rahman P, Ibanez D, Tam LS. Accrual of organ damage over time in patients with systemic lupus erythematosus. J Rheumatol. 2003;30(9):1955–9. [PubMed] [Google Scholar]
- 9.Zonana-Nacach A, Barr SG, Magder LS, Petri M. Damage in systemic lupus erythematosus and its association with corticosteroids. Arthritis Rheum. 2000;43(8):1801–8. doi: 10.1002/1529-0131(200008)43:8<1801::AID-ANR16>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 10.Maddison P, Farewell V, Isenberg D, Aranow C, Bae S, Barr S, et al. The rate and pattern of organ damage in late onset systemic lupus erythematosus. J Rheumatol. 2002;29(5):913–7. [PubMed] [Google Scholar]
- 11.Alarcon GS, McGwin G, Jr, Bartolucci AA, Roseman J, Lisse J, Fessler BJ, et al. Systemic lupus erythematosus in three ethnic groups. IX. Differences in damage accrual. Arthritis Rheum. 2001;44:2797–806. doi: 10.1002/1529-0131(200112)44:12<2797::aid-art467>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 12.Zonana-Nacach A, Camargo-Coronel A, Yanez P, de Lourdes Sanchez M, Jímenez-Balderas FJ, Aceves-Avila J, et al. Measurement of damage in 210 Mexican patients with systemic lupus erythematosus: relationship with disease duration. Lupus. 1998;7:119–23. doi: 10.1191/096120398678919831. [DOI] [PubMed] [Google Scholar]
- 13.Sanchez ML, Costenbader KH, Karlson EW, Alarcón GS, Wolf F. Is it possible to ascertain damage in lupus utilizing a self-reported questionnaire? Preliminary data on the lupus damage index questionnaire (LDIQ) Arthris Rheum. 2007;56:S777. [Google Scholar]
- 14.Costenbader KH, Khamashta M, Ruiz-Garcia S, Perez-Rodriguez MT, Petri M, Elliott J, et al. Multicenter validation of the self-reported lupus damage index questionnaire (LDIQ) Arthris Rheum. 2008;58(9):S802–S803. [Google Scholar]
- 15.Dominguez R, Vila JF, Augustovski F, Irazola V, Castillo PR, Rotta ER, et al. Spanish cross-cultural adaptation and validation of the National Institutes of Health Stroke Scale. Mayo Clin Proc. 2006 Apr;81(4):476–80. doi: 10.4065/81.4.476. [DOI] [PubMed] [Google Scholar]
- 16.Pons-Estel BA, Catoggio LJ, Cardiel MH, Soriano ER, Gentiletti S, Villa AR, et al. The GLADEL multinational Latin American prospective inception cohort of 1,214 patients with systemic lupus erythematosus: ethnic and disease heterogeneity among “Hispanics”. Medicine. 2004;83(1):1–17. doi: 10.1097/01.md.0000104742.42401.e2. [DOI] [PubMed] [Google Scholar]


