Abstract
INTRODUCTION:
Physiotherapy is one of the most important components of therapy for osteoarthritis of the knee. The objective of this prospective case series was to assess the efficiency of a guidance manual for patients with osteoarthritis of the knee in relation to pain, range of movement , muscle strength and function, active goniometry, manual strength test and function.
METHODS:
Thirty-eight adults with osteoarthritis of the knee (≥ 45 years old) who were referred to the physiotherapy service at the university hospital (Santa Casa de Misericórdia de São Paulo) were studied. Patients received guidance for the practice of specific physical exercises and a manual with instructions on how to perform the exercises at home. They were evaluated for pain, range of movement, muscle strength and function. These evaluations were performed before they received the manual and three months later. Patients were seen monthly regarding improvements in their exercising abilities.
RESULTS:
The program was effective for improving muscle strength, controlling pain, maintaining range of movement of the knee joint, and reducing functional incapacity.
DISCUSSION:
A review of the literature showed that there are numerous clinical benefits to the regular practice of physical therapy exercises by patients with osteoarthritis of the knee(s) in a program with appropriate guidance. This study shows that this guidance can be attained at home with the use of a proper manual.
CONCLUSIONS:
Even when performed at home without constant supervision, the use of the printed manual for orientation makes the exercises for osteoarthritis of the knee beneficial.
Keywords: Physiotherapy; Osteoarthritis; Knee, Exercise, Manuals
INTRODUCTION
Osteoarthritis (OA) is a progressive degenerative disease that affects the joint cartilage, subchondral bone, synovia and joint capsule. It has a multifactorial etiology1 and affects around 60% of individuals aged over 50 years.2,3 According to Davis et al., OA affects 9% of men and 18% of women over 65 years old and is responsible for high levels of absenteeism and retirement due to disability.4
The etiology of OA is related to repetitive mechanical loads and age. Recent studies have separated the etiological factors into three main sub-groups: sex, anatomy, and body mass.1 The clinical manifestations are joint pain, stiffness, decreased range of joint movement, muscle weakness of the quadriceps, and alterations in proprioception.5-7 Decreased strength in the muscle groups involving the joints is significant because it causes progressive loss of function. These symptoms significantly restrict the individual's ability to get up from a chair, walk, or climb stairs.5 Walking with a limp, poor alignment of the limb, and instabilities can also be observed in individuals with OA. During movements, crepitation can be heard because of arthritis of the irregular joint surfaces.8
OA often affects one of the three compartments of the knee: the patellofemoral joint or the medial or lateral joint compartment. In relation to severity, OA of the knee can be classified according to the Kellgren-Lawrence scale, which consists of five degrees of OA: 0 = no OA, 1 = doubtful, 2 = minimal, 3 = moderate, and 4 = severe.9
The treatment of OA should be multidisciplinary and aim for functional, mechanical and clinical improvement. Physiotherapy is a non-pharmacological intervention for osteoarthritis of the knee that is recommended by the American College of Rheumatology and the European League against Rheumatism.10,11 A systematic review has shown that exercise reduces pain and improves function in patients with OA of the knee.12 One of the most common forms of achieving this functional improvement is by following a program of daily exercises.13 A placebo-controlled study by Deyle et al. showed that patients with knee OA experienced significant improvements in clinical status as well as pain, stiffness, and function (walking distance) when submitted to exercises combined with manual therapy.14
The guidance of the physiotherapist guarantees that the physical exercises are being practiced correctly. Unfortunately, there is a high demand in large public health services, and it is often impossible to meet the needs of everyone, particularly those who have difficulty traveling to the training center. The physical exercises, however, can be done both in the clinic and in home-based exercising programs, provided that the patient returns for some supervised visits. The utility of home-based exercise was clearly shown by another study performed by Deyle's research staff, which compared a group of OA patients submitted to exercises, individualized manual therapy, and a home-based exercise program for four weeks with a group of OA patients receiving the same home exercise program and a clinic visit 2 weeks later. Both groups demonstrated a significant clinical improvement compared to baseline. Initially, the clinic-based patients showed a greater level of improvement, but the results of both groups were equally beneficial one year later.15 In addition, Thomas et al. showed that home-based exercise for two years could result in significant control of knee pain.16
Thus, the objective of this study was to assess the effectiveness of a guidance manual of physical activities to be performed at home by patients with osteoarthritis of the knee(s). The study evaluated pain, range of joint movement (ROM), muscle strength, and functional capacity before and after treatment. The hypothesis was that OA patients would benefit from the home-based physical therapy, with the help of the manual, and show improvements in pain, strength, ROM, and functional capacity.
METHODS
This observational study developed in the second half of 2007 at the rehabilitation service of a public university hospital (Santa Casa de Misericórdia de São Paulo). This was a prospective case series on the application of an intervention in physiotherapy (guidance manual) for patients with osteoarthritis (OA) of the knee(s). Pain, ROM, strength, and function were assessed before and after the application of the physiotherapeutic intervention. The Research Ethics Committee of the institution (protocol 099/04) approved the study, and all of the participants signed a term of informed consent.
Participants
This study included all of the patients diagnosed with grade 2 or 3 OA of the knee(s), according to the Kellgren-Lawrence scale,9 and patients with light or moderate arthrosis who were referred to physical therapy in a public university hospital. Both males and females (≥ 45 years old) were recruited for this study. The patients must have been referred to the rehabilitation service by physicians (physiatry specialists) during the period of February 6, 2007 to December 23, 2007, and all were evaluated by radiographs. Patients with grade 1 or 4 in the Kellgren-Lawrence scale were excluded. In addition, we also excluded patients who had undergone any kind of orthopedic surgery of the lower limb during the last two years and/or other concomitant therapies, except for the use of analgesic and non-steroidal anti-inflammatory drugs (according to medical guidelines). During the study period, 98 patients were included in the study.
Initial clinical evaluation
All patients referred to the physical therapy service came to the first evaluation visit. During the first visit, the following data were collected: quantitative evaluation of the pain using the visual analog scale (VAS),17 ROM and muscle strength (as described below), qualitative evaluation of the main functions impaired (according to their main complaint), and the length of time they had been experiencing pain (in months or years). The Lequesne Algofunctional Questionnaire18 was also applied to quantify the functional limitations and incapacities.
Initial physiotherapeutic intervention
After clinical assessment, the patients were divided into groups of up to five individuals. They were given an explanation of the disease and a program of physical stretching and muscle strengthening exercises to be carried out individually at home. The patients performed each exercise in the presence of the physiotherapist so that any questions about the exercises could be clarified. All patients were given a printed manual written in simple language that contained photographs and guidance.
The patients were reassessed at one-month intervals for at least 90 days after the first assessment (where they received the manual). In these re-evaluation sessions, physical therapists observed how the patient carried out the home exercises. If the patient had no difficulty performing the exercise, then the number of repetitions was increased to a maximum of five repetitions in each series. All of the patients attended the follow-up sessions.
Clinical evaluations
To assess the intensity of pain in the knee(s), the visual analog scale (VAS) was used: zero (0) denoted the absence of pain and 10 denoted pain of unbearable intensity.17 Pain was assessed before treatment and at the end of the physiotherapeutic treatment.
The range of joint movement (ROM) of knee flexion was measured according to the criteria of Norkin and White.19 The manual muscle strength tests were applied to the extensor and flexor muscle groups of the knee, using the Kendall scale,20 and grades varied from zero (no contraction) to five degrees (maximum strength). The same evaluator carried out all of the assessments before and after the home protocol.
The Lequesne Algofunctional Questionnaire for osteoarthritis of the knees and hips, validated for the Portuguese language, was applied in the initial assessment and at the 90-day follow-up. The Questionnaire results in the construction of the Lequesne Algofunctional Index. The patient responded to the questions relating to the knee joint with the following scores: extremely severe (equal to or greater than 14 points), very severe (11 to 13 points), severe (8 to 10 points), moderate (5 to 7 points), or mildly affected (1 to 4 points).18
Guidance manual
The manual was 18 pages long and was presented in a small, pocket-sized format (14.8 × 21 cm). At the beginning, it gave a definition of OA and the general anatomical aspects of the knee, including diagrams. Next, it emphasized the importance of the daily exercises for improving the symptoms and functionality. This first part of the booklet also contained some important tips for day-to-day living (e.g., do not place to much strain on the knee joint by distributing heavy household tasks throughout the week, maintain an ideal body weight, avoid wearing high heels, and avoid high-impact activities). The text had a approximately 360 words, and the booklet included a small diary for taking notes of the activities performed at home. It also addressed some simple analgesic measures that could easily be applied at home, including cryotherapy and compression by local application for a maximum of 20 minutes.21-23
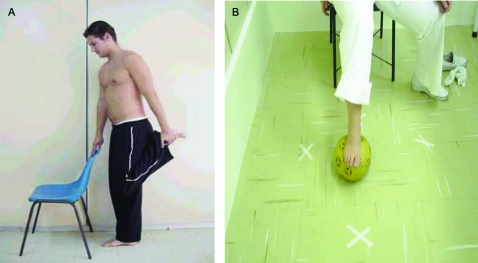
Next, the booklet presented the stretching exercises (ischiotibial, gluteus maximus, quadriceps, and sural triceps) and muscle strengthening exercises (quadriceps, ischiotibial, gluteus medius and maximus, adductors, and sural triceps) starting with some isometric exercises for the knees and isotonic exercises for the hips. Each of the 20 exercises was explained in a 20- to 40-word passage, and each exercise was accompanied by a photograph of a model performing the proposed movement. Figure 1 gives an example of the proposed exercises.
Figure 1.
Examples of two exercises proposed in the Manual, and their accompanying photographs.
(A) While standing, hold on to a chair or table to maintain your balance, bend one of your knees and with your hand, pull your foot towards your bottom..If you cannot reach your foot, pull it with the help of a folded towel.
(B) Mark the floor with adhesive tape in various directions. Sit down on a chair, step on a ball and roll it to the markings made on the floor. Repeat 10 times.
Statistical analysis
This study analyzed VAS (0 to 10), knee ROM (0° to 140°), the strength of extensor and flexor muscle groups (0 to 5 points), and the Lequesne index (1 to 14 or more points). After the data analysis, each of the variables was submitted to a standardization test to determine the types of statistical test to be used. For the quantitative variables, this analysis was done through the observation of the minimum and maximum values and the calculation of averages and standard deviations. For patients with bilateral complaints, the mean value between the measurements of both knees was calculated. For patients who only had OA in one knee, the unaffected knee was not considered.
The paired Wilcoxon test was used for VAS and ROM, which compared the data before and after the physiotherapeutic intervention. The paired t test was used to analyze the results of the Lequesne Algofunctional scale. For the qualitative variables, the absolute and relative frequencies were calculated. The Kruskal-Wallis test was used to compare the differences between pre- and post-treatment according to the age of the patient. For all analyses, the differences were considered significant when p < 0.05. All analyses were conducted with the Statistical Package for Social Sciences (SPSS) software, version 15.0.
RESULTS
As already stated, during the study period, 98 patients with osteoarthritis of the knee were seen by the physiotherapy services (with a total of 166 affected knees). All of the patients attended the follow-up sessions, but it was not possible to apply the Lequesne assessment to all of the patients because of a lack of specialized personnel. Therefore, the results presented here refer to a sample of 38 patients who were clinically evaluated and responded to the Lequesne questionnaire.
As shown in Table 1, 84% of the patients were women, 50% were between 50 and 59 years old, and 66% had bilateral pain.
Table 1.
Demographic and clinical characteristics of patients with osteoarthritis of the knee submitted to physiotherapy.
| Characteristics | Frequency | % |
| Sex | ||
| Female | 32 | 84.2 |
| Male | 6 | 15.8 |
| Age (years) | ||
| 50 to 59 | 19 | 50.0 |
| 60 to 69 | 11 | 28.9 |
| 70 or more | 8 | 21.1 |
| Main complaint | ||
| Right knee | 8 | 21.1 |
| Left knee | 5 | 13.2 |
| Bilateral | 25 | 65.8 |
| Total | 38 | 100 |
During the initial assessment, all patients reported joint pain in the knee(s) during day-to-day activities as their main complaint (e.g., difficulty going up and down stairs, crouching and kneeling). Table 2 shows that the exercise program resulted in significant changes in all measurements (VAS, ROM, muscle strength and Lequesne evaluations). All variables had mean variations of more than 50% compared to baseline (p < 0.05).
Table 2.
Pain (analyzed by the visual analogue scale, VAS), range of joint movement (ROM), strength (MS) and the result of the Lequesne evaluation for function presented as mean, standard deviation (SD), median, minimum, maximum, N and p values according to the moment of evaluation.
| Variable | Mean | SD | Median | Minimum | Maximum | N | p |
| VAS Pre | 7.87 | 1.12 | 8 | 5 | 10 | 38 | < 0.001 |
| VAS Post | 3.58 | 0.92 | 3.5 | 2 | 5 | 38 | |
| ROM Pre | 87.25 | 8.85 | 89 | 63 | 106 | 38 | < 0.001 |
| ROM Post | 123.71 | 7.60 | 124 | 107 | 137 | 38 | |
| MS hip Pre | 3.32 | 0.46 | 3.5 | 2 | 4 | 38 | < 0.001 |
| MS hip Post | 4.78 | 0.38 | 5 | 4 | 5 | 38 | |
| MS hamstring Pre | 3.70 | 0.39 | 4 | 3 | 4 | 38 | < 0.001 |
| MS hamstring Post | 4.97 | 0.11 | 5 | 4.5 | 5 | 38 | |
| Lequesne Pre | 16.17 | 1.52 | 16 | 13.5 | 19.5 | 38 | < 0.001 |
| Lequesne Post | 7.57 | 2.19 | 7.75 | 4 | 12 | 38 |
The patients were subdivided into three age groups for comparison. There was no association between pain and age either before or after the treatment, nor was age associated with ROM, muscle strength, or functional status after the treatment. Table 3 shows that age did not interfere with the results (p > 0.05); all patients benefited from the treatment regardless of their age.
Table 3.
Changes in the measurements of pain (analyzed by the visual analogue scale, VAS), range of joint movement (ROM), muscle strength (MS) and functional status (by the Lequesne Algofunctional Questionnaire for Osteoarthritis of the Knees) according to age and results of the comparisons between the age brackets.
| Variable | Age (years) | Mean | SD | Median | Minimum | Maximum | N | P |
| VAS | 0.385 | |||||||
| 50 to 59 | 4.05 | 1.54 | 4 | 2 | 8 | 19 | ||
| 60 to 69 | 4.45 | 1.04 | 4 | 3 | 6 | 11 | ||
| 70 or + | 4.63 | 1.06 | 4.5 | 3 | 6 | 8 | ||
| Total | 4.29 | 1.31 | 4 | 2 | 8 | 38 | ||
| ROM | 0.097 | |||||||
| 51 to 59 | 38.95 | 8.67 | 40 | 20 | 53 | 19 | ||
| 61 to 69 | 35.50 | 7.76 | 34 | 26 | 51.5 | 11 | ||
| 71 or + | 31.88 | 4.45 | 33.5 | 25 | 37 | 8 | ||
| Total | 36.46 | 8.04 | 35 | 20 | 53 | 38 | ||
| MS hip | 0.575 | |||||||
| 52 to 59 | 1.55 | 0.47 | 1.5 | 1 | 2.5 | 19 | ||
| 62 to 69 | 1.41 | 0.63 | 1.5 | 0 | 2 | 11 | ||
| 72 or + | 1.31 | 0.46 | 1.5 | 0.5 | 2 | 8 | ||
| Total | 1.46 | 0.51 | 1.5 | 0 | 2.5 | 38 | ||
| MS hamstring | 0.836 | |||||||
| 53 to 59 | 1.29 | 0.38 | 1 | 1 | 2 | 19 | ||
| 63 to 69 | 1.23 | 0.47 | 1 | 0.5 | 2 | 11 | ||
| 73 or + | 1.31 | 0.37 | 1.25 | 1 | 2 | 8 | ||
| Total | 1.28 | 0.40 | 1 | 0.5 | 2 | 38 | ||
| Lequesne | 0.514 | |||||||
| 54 to 59 | 8.32 | 1.25 | 8 | 7 | 11 | 19 | ||
| 64 to 69 | 8.95 | 1.84 | 8.5 | 6.5 | 12.5 | 11 | ||
| 74 or + | 8.81 | 1.41 | 9 | 6.5 | 10.5 | 8 | ||
| Total | 8.61 | 1.46 | 8.5 | 6.5 | 12.5 | 38 |
DISCUSSION
Both immobilization and intense physical exercise can contribute to degeneration of the joint and increase the risk of developing the most severe form of OA, which requires arthroplasty, osteotomy or arthroscopy.24 In a study carried out in the United States, the authors observed that strength, speed of muscular contraction, and endurance were 30 to 50% lower in individuals with osteoarthritis compared with age-matched individuals without OA. OA leads to difficulty performing daily activities and a lack of physical activity as a result of pain.25 Weakness of the quadriceps muscle is considered one of the most important risk factors in the progression of OA of the knee.26 The strength of this muscle naturally decreases with age, leading to functional limitation and possible degeneration of the knee joint cartilage.27 In our study, strength was evaluated by the Kendall scale, which is a subjective measurement that is applicable when dynamometers are not available. Although a significant increase in strength (25%) was observed after the home-based exercises, a greater change probably could have been detected with dynamometry.
The most appropriate non-surgical treatment for osteoarthritis (OA) of the knee is physical exercise therapy. Physiotherapy reduces pain and improves function, muscle strength, range of movement (ROM), joint stability and aerobic conditioning.12-14
The regular practice of exercises by patients with osteoarthritis of the knee(s), in a program of intervention through appropriate guidance, can help prevent the loss of muscle strength and restriction of day-to-day activities. In addition, regular exercises can enable pain control and prevent the loss of ROM. Instructions on how to sit, lift, carry heavy objects and walk correctly are useful and important in the treatment of OA. Strength-building exercises designed for the flexor musculature of the knee are just as important for the quadriceps in the rehabilitation of knee OA because of the dynamic stability of this joint.28
Various works have already shown good results with treatment protocols consisting of stretching of the quadriceps, ischiotibial and sural triceps, and free active resistant and dynamic exercises of the hip and knee with isometric and isotonic contractions. These exercises result in an improvement in range of joint movement, strength of the hips and ischiotibia, and dynamic activities, even when the exercises are performed in the patient's home.14,15,29 Compared with the suspension of physiotherapy after discharge of the patient, both isokinetic and isotonic exercises have shown good results in the maintenance of pain treatment at home following physiotherapy in a health service center (as evaluated by the VAS score). Functional capacity, assessed by the Lequesne Questionnaire, showed an improvement in patients carrying out isokinetic exercises.
In the guidance manual given to the patients in the present study, the proposed strength exercises began with isometric training and then progressed to the isotonic exercises. The literature search suggested that progressive isometric and isotonic exercises promote the strengthening of muscles and improvements in functionality. Studies have reported that the gain in strength, which occurs through intramuscular adaptation, is obtained after 12 weeks of training with resistant exercises.14,27 These findings justified the 90-day follow-up period in the present study, and we obtained excellent results. Increasing the amount of exercising stimuli (increase in repetitions and in weight) is possible when the patient shows improvement or stability in signs and symptoms of OA (i.e., when pain, inflammation and edema are not getting worse or when these signs are progressively diminished).15 In this study, the monthly visits allowed the doctors to check each patient's clinical status and exercise progression to determine cases where OA signs and symptoms improved.
In the present study, a significant reduction was observed in pain and functional incapacity according to the VAS and the Lequesne Algofunctional Questionnaire, respectively. These results were similar to a study by Doi et al.,30 which found that a group of patients who performed isometric exercises of the quadriceps every day for eight weeks achieved a significant reduction in pain (assessed by VAS) compared with the control group, which was medicated with non-steroidal anti-inflammatories.30 The improvement in function, as evaluated by Lequesne Questionnaire, was also statistically significant (p = 0.001) in our study.
In the present study, pain was cited as the main complaint of all patients. The assessment of pain is individual and subjective because the individual is the authority on his or her own experience of pain. The evaluation was carried out using the visual analog scale to identify the intensity of the pain. In the re-evaluation following the procedure and physiotherapeutic guidance for the practice of the exercises, a statistically significant decrease was observed in the intensity of the pain, which showed that the intervention had an effect on pain reduction.
As an analgesic resource, local cryotherapy was always used in conjunction with compression and elevation of the limb for approximately 20 minutes21,31 after the exercises or when there was pain in the knee(s). Cryotherapy is a resource that is easy to apply at home. It is indicated in cases of pain, inflammation, and muscular spasms because it acts directly on the nerve endings, which decreases the conductibility of the impulse, causes the threshold of excitation of the nerve cells to increase, promotes a decrease in local cell metabolism, promotes lower oxygen consumption, and prevents lesions by secondary hypoxia.32
With the aim of maintaining or improving ROM, stretching exercises were included in the manual given to the patients. Joint mobility should be maintained or improved in patients with osteoarthritis because the loss of ROM causes shortening and contraction of the muscles and capsular structures, and it can impair functionality. The individuals included in this study presented a statistically significant improvement in knee flexion ROM as a result of the muscle stretching exercises. A greater ROM has also been reported by other authors.14,33
The short-term benefits of exercises for patients with knee OA levels 2 and 3 have been demonstrated, such as in pain reduction and functional improvement,34 but studies with a longer-term evaluation are necessary, e.g., nine months, as proposed by van Baar et al.35 In fact, Deyle et al. has shown that short-term improvements can be seen with exercise programs for OA, but the maintenance of the benefits over one year depended on the patient's compliance with the protocol.14 Theoretically, the maintenance of benefits can only be verified when regular checkups are performed, as proposed in the present study. When patients can be prescribed a home-based exercise program, more health workers are available for other patients, especially those in acute conditions or in post-surgical treatment. Thus, selecting patients who can benefit from a home-based exercise program is a cost-reducing measure.14,15
We believe that the results of this study can be achieved in any public service with similar patient characteristics: male or female, middle-aged or older patients with OA of the knee(s) who are able to read, and patients who do not have easy access to health services (few re-evaluation sessions were necessary to obtain positive results). The results would probably be even better in samples of patients who had easier access to physical therapy supervision.
There is a possibility that the close contact with the physical therapist in this study produced an effect similar to the placebo effect, which is known as the Hawthorne effect. However, our patients showed improvements in subjective symptoms, such as pain, as well as objectively measured clinical status variables, such as function, flexion ROM, and muscular strength for both extensors and flexors.
There is a possibility that the close contact with the physical therapist in this study produced an effect similar to the placebo effect, which is known as the Hawthorne effect. However, our patients showed improvements in subjective symptoms, such as pain, as well as objectively measured clinical status variables, such as function, flexion ROM, and muscular strength for both extensors and flexors.
CONCLUSION
The use of a guidance manual for physical exercises at home, along with monthly reassessment by a physiotherapist, enabled patients with OA of the knee(s) to achieve a significant improvement in pain, ROM knee flexion, muscle strength, and functional capacity.
REFERENCES
- 1.Weiss E, Jurmain R. Osteoarthritis revisited: a contemporary review of aetiology. International Journal of Osteoarchaeology. 2007;17:437–50. 10.1002/oa.889 Available from: http://www3.interscience.wiley.com/journal/114109900/abstract?CRETRY = 1&SRETRY = 0. Accessed in 2009 (Jul 15). [Google Scholar]
- 2.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, et al. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–99. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V [DOI] [PubMed] [Google Scholar]
- 3.Guccione AA, Felson DT, Anderson JJ, Anthony JM, Zhang Y, Wilson PW, et al. The effects of specific medical conditions on the functional limitations of elders in the Framingham Study. Am J Public Health. 1994;84:351–8. doi: 10.2105/ajph.84.3.351. 10.2105/AJPH.84.3.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Davis MA, Ettinger WH, Neuhaus JM, Mallon KP. Knee osteoarthritis and physical functioning: evidence from the NHANES I Epidemiologic Followup Study. J Rheumot. 1991;18:591–8. [PubMed] [Google Scholar]
- 5.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34:907–915. doi: 10.1016/s0021-9290(01)00036-7. 10.1016/S0021-9290(01)00036-7 [DOI] [PubMed] [Google Scholar]
- 6.Hurley MV, Scott DL, Rees J, Newham DJ. Sensorimotor changes and functional performance in patients with knee osteoarthritis. Ann Rheum Dis. 1997;56:641–8. doi: 10.1136/ard.56.11.641. 10.1136/ard.56.11.641 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCloskey DI. Kinesthetic sensibility. Physiol Rev. 1978;58:763–820. doi: 10.1152/physrev.1978.58.4.763. [DOI] [PubMed] [Google Scholar]
- 8.Easton BT. Evaluation and treatment of the patient with osteoarthritis. J Fam Pract. 2001;50:791–7. [PubMed] [Google Scholar]
- 9.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. 10.1136/ard.16.4.494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT) Ann Rheum Dis. 2003;62:1145–55. doi: 10.1136/ard.2003.011742. 10.1136/ard.2003.011742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on Osteoarthritis Guidelines. Arthritis Rheum. 2000;43:1905–15. doi: 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P. 10.1002/1529-0131(200009)43:9<1905::AID-ANR1>3.0.CO;2-P [DOI] [PubMed] [Google Scholar]
- 12.Puett DW, Griffin MR. Published trials of nonmedicinal and noninvasive therapies for hip and knee osteoarthritis. Ann Inter Med. 1994;121:133–40. doi: 10.7326/0003-4819-121-2-199407150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Dekker J, Boot B, van der Woude LH, Bijlsma JW. Pain and disability in osteoarthritis: a review of biobehavioral mechanisms. J Behav Med. 1992;15:189–214. doi: 10.1007/BF00848325. 10.1007/BF00848325 [DOI] [PubMed] [Google Scholar]
- 14.Deyle GD, Henderson NE, Matekel RL, Ryder MG, Garber MB, Allison SC. Effectiveness of manual physical therapy and exercise in osteoarthritis of the knee. A randomized, controlled trial. Ann Intern Med. 2000;132:173–81. doi: 10.7326/0003-4819-132-3-200002010-00002. [DOI] [PubMed] [Google Scholar]
- 15.Deyle GD, Allison SC, Matekel RL, Ryder MG, Stang JM, Gohdes DD, et al. Physical therapy treatment effectiveness for osteoarthritis of the knee: a randomized comparison of supervised clinical exercise and manual therapy procedures versus a home exercise program. Phys Ther. 2005;85:1301–17. [PubMed] [Google Scholar]
- 16.Thomas KS, Muir KR, Doherty M, Jones AC, O'Reilly SC, Bassey EJ. Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ. 2002;325:752. doi: 10.1136/bmj.325.7367.752. 10.1136/bmj.325.7367.752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Huskisson EC, Melzack R. Visual analogue scales. In: Melzack R, editor. Pain measurement and assessment. New York: Raven Press; 1983. pp. 33–7. [Google Scholar]
- 18.Marx FC, Oliveira LM, Bellini CG, Ribeiro MCC. Tradução e validação cultural do questionário algofuncional de Lequesne para osteoartrite de joelhos e quadris para a língua portuguesa. [Translation and cultural validation of the Lequesne Algofunctional questionnaire for osteoarthritis of knee and hip for Portuguese language] Rev Bras Reumatol. 2006;64:253–60. [Google Scholar]
- 19.Norkin CC, White DJ. Measurement of joint motion: a guide to goniometry. Philadelphia: FA Davis Company; 1986. [Google Scholar]
- 20.Kendall HO, Kendall FP, Bierman W, Licht S. Physical medicine in general practice. New York: Paul B Hoeber; 1952. Functional muscle testing; pp. 339–84. [Google Scholar]
- 21.Janwantanakul P. Cold pack/skin interface temperature during ice treatment with various levels of compression. Physiotherapy. 2006;92:254–9. 10.1016/j.physio.2006.05.006 [Google Scholar]
- 22.Enwemeka CS, Allen C, Avila P, Bina J, Konrade J, Munns S. Soft tissue thermodynamics before, during, and after cold pack therapy. Med Sci Sports Exerc. 2002;34:45–50. doi: 10.1097/00005768-200201000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Jutte LS, Merrick MA, Ingersoll CD, Edwards JE. The relationship between intramuscular temperature, skin temperature, and adipose thickness during cryotherapy and rewarming. Arch Phys Med Rehabil. 2001;82:845–50. doi: 10.1053/apmr.2001.23195. 10.1053/apmr.2001.23195 [DOI] [PubMed] [Google Scholar]
- 24.Manninen P, Riihimaki H, Heliovaara M, Suomalainen O. Physical exercise and risk of severe knee osteoarthritis requiring arthroplasty. Rheumatology (Oxford.) 2001;40:432–7. doi: 10.1093/rheumatology/40.4.432. 10.1093/rheumatology/40.4.432 [DOI] [PubMed] [Google Scholar]
- 25.Fisher NM, Kame VD, Jr, Rouse L, Pendergast DR. Quantitative evolution of a home exercise program on muscle and functional capacity of patients with osteoarthritis. Am J Phys Med Rehabil. 1994;73:413–20. doi: 10.1097/00002060-199411000-00006. 10.1097/00002060-199411000-00006 [DOI] [PubMed] [Google Scholar]
- 26.Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA (2006) Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55:690–9. doi: 10.1002/art.22245. 10.1002/art.22245 [DOI] [PubMed] [Google Scholar]
- 27.O'Reilly SC, Jones A, Muir KR, Doherty M. Quadriceps weakness in knee osteoarthritis: the effect on pain and disability. Ann Rheum Dis. 1998;57(10):588–94. doi: 10.1136/ard.57.10.588. 10.1136/ard.57.10.588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tan J, Balci N, Sepici V, Gener FA. Isokinetic and isometric strength in osteoarthrosis of the knee. A comparative study with healthy women. Am J Phys Med Rehabil. 1995;74:364–9. 10.1097/00002060-199509000-00008 [PubMed] [Google Scholar]
- 29.O'Reilly SC, Muir KR, Doherty M. Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Ann Rheum Dis. 1999;58:15–9. doi: 10.1136/ard.58.1.15. 10.1136/ard.58.1.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Doi T, Akai M, Fujino K, Iwaya T, Kurosawa H, Hayashi K, et al. Effect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal antiinflammatory drugs: a randomized controlled trial. Am J Phys Med Rehabil. 2008;87:258–69. doi: 10.1097/PHM.0b013e318168c02d. 10.1097/PHM.0b013e318168c02d [DOI] [PubMed] [Google Scholar]
- 31.Knight KL. Cryotherapy in sport injury management. Champaign: Human Kinetics Publishers; 1995. [Google Scholar]
- 32.Staff PH. The effects of physical activity on joints, cartilage, tendons and ligaments. Scand J Soc Med. 1982;(Suppl 29):59–63. [PubMed] [Google Scholar]
- 33.van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Lemmens JA, et al. The effectiveness of exercise therapy in patients with osteoarthritis of the hip or knee: a randomized clinical trial. J Rheumatol. 1998;25:2432–9. [PubMed] [Google Scholar]
- 34.Iwamoto J, Takeda T, Sato Y. Effect of muscle strengthening exercises on the muscle strength in patients with osteoarthritis of the knee. Knee. 2007;14:224–30. doi: 10.1016/j.knee.2007.03.002. 10.1016/j.knee.2007.03.002 [DOI] [PubMed] [Google Scholar]
- 35.van Baar ME, Dekker J, Oostendorp RA, Bijl D, Voorn TB, Bijlsma JW. Effectiveness of exercise in patients with osteoarthritis of hip or knee: nine months' follow up. Ann Rheum Dis. 2001;60:1123–30. doi: 10.1136/ard.60.12.1123. 10.1136/ard.60.12.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]