Abstract
Context
Little is known about prevalence rates of DSM-IV disorders across age strata of older adults, including common conditions such as individual and coexisting mood and anxiety disorders.
Objective
To determine nationally representative estimates of 12-month prevalence rates of mood, anxiety, and comorbid mood-anxiety disorder across young-old, mid-old, old-old, and oldest old community-dwelling adults.
Design and Setting
The National Comorbidity Survey Replication (NCS-R) is a population-based probability sample of 9282 participants 18 years and older, conducted between February 2001 and April 2003. The NCS-R survey used the fully structured World Health Organization World Mental Health Survey version of the Composite International Diagnostic Interview.
Participants
We studied the 2575 participants 55 years and older who were part of NCS-R (43% 55-64; 32% 65-74; 20% 75-84; 5% ≥85 years). This included only non-institutionalized adults, as all NCS-R participants resided in households within the community.
Main Outcome Measures
Twelve-month prevalence of mood disorders (MDD, dysthymia, bipolar disorder), anxiety disorders (panic disorder, agoraphobia, specific phobia, social phobia, generalized anxiety disorder, posttraumatic stress disorder), and coexisting mood-anxiety disorder were assessed using DSM-IV criteria. Prevalence rates were weighted to adjust for the complex design in order to infer generalizability to the U.S. population.
Results
The likelihood of having a mood, anxiety, or combined mood-anxiety disorder generally showed a pattern of decline with age (P < .05). Twelve-month disorders showed higher rates in women compared to men; a statistically significant trend with age. In addition, anxiety disorders were as high if not higher than mood disorders across age groups (overall 12-month rates: mood=5% and anxiety=12%). No differences were found between race/ethnicity groups.
Conclusions
Prevalence rates of DSM-IV mood and anxiety disorders in late life tend to decline with age, but remain very common; especially in women. These results highlight the need for intervention and prevention strategies.
Introduction
Knowledge of the prevalence of mood and anxiety disorders and coexisting mood-anxiety disorder in older community-dwelling adults is important—these are hidden and undertreated but treatable disorders associated with poor health outcomes.1-5 Such information is imperative, especially considering the current and projected growth of the older segment of the population. Understanding these distributions has important implications for intervention and prevention strategies in geriatric research and care. However, epidemiological studies of psychiatric disorders in elderly Americans are limited. The majority of research has involved small studies, generally in clinical settings, which limit generalizability to the population.6-8 The small number of community-based studies have used symptom scales as opposed to structured clinical interviews to assess prevalence of disorders.9,10
The Epidemiologic Catchment Area (ECA) Survey,11 conducted from 1980-1984, in five U.S. cities has been used for many years as the standard to estimate the prevalence of psychiatric disorders in U.S. adults 65 and older.10 Despite its impressive impact, the ECA has two important limitations. First, the ECA is not a nationally representative probability sample. Second, it used the Diagnostic Interview Schedule (DIS),12 which allowed the determination of DSM-III13 diagnoses but not current DSM-IV.14 The original National Comorbidity Survey (NCS), unlike ECA, conducted in 1990-1992, is a national probability sample. However, the NCS did not include older adults and also examined DSM-III-R disorders.15 In contrast, the National Comorbidity Survey Replication (NCS-R) was conducted in 2001-2003 and included older adult respondents and expanded assessments based on the current diagnostic criteria of the DSM-IV.14 Additionally, the NCS-R includes a nationally representative distribution of gender and race/ethnicity. These are two important demographic factors when considering prevalence rates at the population level, but understudied in mental health research of late life.16-19 Recent examination of the NCS-R included comparison of older adults' (65 years and older) and younger adults' (18-44 years and 45-64 years) prevalence rates.20 This study did not consider detailed comparisons of older age cohorts, including the oldest old (≥ 85 years), and did not account for comorbid mood and anxiety disorder.
The purpose of our study was to determine nationally representative estimates of age-specific 12-month prevalence rates of DSM-IV mood, anxiety, and comorbid disorder among community-dwelling older adults in the NCS-R; comparing young-old, mid-old, old-old, and oldest old U.S. respondents. This study examines age-stratified diagnostic measures of psychiatric disorders, including the oldest old and gender and race/ethnic differences, in a large probability sample of older adults.
Methods
Participants
The NCS-R is a nationally representative survey of 9282 non-institutionalized participants aged 18 years and older in the coterminous United States.21-23 Respondents were selected from a multistage clustered area probability sample of households. Face-to-face interviews were conducted in respondents' homes between February 2001 and April 2003. Individuals residing in nursing homes, assisted living, and independent living facilities were therefore excluded from the sample. Any clustering of respondents by retirement communities was alleviated by the household enumeration procedures used in NCS-R to create a national probability sample. Professional interviewers from the Institute for Social Research at the University of Michigan, Ann Arbor, carried out interviews. The response rate was 70.9%.21
The current sample consisted of 2575 community-based adults aged 55 and older; data obtained from the Inter-university Consortium for Political and Social Research.24 The NCS-R was administered in two parts. The part I sample, which is the focus of this study, included all respondents assessed for core mental disorders. One thousand three hundred and seventy two of the 2575 who met criteria for any lifetime mental disorder in part I, plus a probability subsample of other participants from part I, received a part II interview.21,25,26 The part II interview included questions about risk factors, consequences, other correlates, and additional mental disorders. Assessment for posttraumatic stress disorder required lengthier introductory questions than other disorders, which precluded the quick skipout of noncases that was desired in part I.21 Thus, PTSD was only assessed in the part II survey. The NCS-R data were weighted to control for differential probabilities of selection, differential non-response, and residual differences between demographic variables of the sample and 2000 U.S. census population.23,27 A detailed description of the NCS-R sampling and weighting procedures are outlined elsewhere.23
Measures
Diagnostic Assessment
The NCS-R diagnoses were determined using the World Health Organization's World Mental Health (WMH) Survey Initiative version of the Composite International Diagnostic Interview (CIDI).28 The WMH-CIDI is a fully structured lay interview that generates lifetime and 12-month diagnoses according to the International Classification of Diseases, 10th Revision29 and DSM-IV14 criteria.21,25 In the present analyses, the DSM-IV criteria were used. The mental disorders examined included mood disorders (major depressive disorder, dysthymia, bipolar I and II disorders), anxiety disorders (panic disorder, agoraphobia without panic, specific phobia, social phobia, generalized anxiety disorder, and posttraumatic stress disorder (PTSD)), and comorbid mood-anxiety disorder (i.e., any co-occurring mood and anxiety disorders). DSM-IV organic exclusion rules and hierarchy rules were used in making diagnoses.21,25 Using a probability subsample of NCS-R respondents in a clinical calibration design,30 Kessler et al.21 found that blind clinical reinterviews with the Structured Clinical Interview for DSM-IV (SCID)31 were in good concordance with WMH-CIDI diagnoses for mood and anxiety disorders.
Sociodemographic Variables
Distributions of sociodemographic variables by 12-month DSM-IV/WMH-CIDI mood, anxiety, and comorbid mood-anxiety disorders were examined. The main demographic variable of interest was age defined by four categories: young-old (55-64 years), mid-old (65-74 years), old-old (75-84 years), and oldest old (≥ 85 years). These were examined overall and by gender and race/ethnicity (non-Hispanic white, non-Hispanic black, and Hispanic or other). In addition, we examined completed years of education (0-11, 12, 13-15, ≥ 16), marital status (married/cohabitating, divorced/separated/widowed, never married), and geographic region of residence (northeast, midwest, south, and west).
To create as accurate a presentation as possible of the trend of psychiatric disorders across increasing age groups, plots of figures were further refined, plotting weighted prevalence rates by 5-year age intervals.
Statistical Analyses
Prevalence rates were determined by frequency measures and cross-tabulations estimating age differences across DSM-IV disorders. Twelve-month prevalence was estimated as the percentage of respondents who had a mood, anxiety, or comorbid mood-anxiety disorder in the year prior to the interview.
Three sets of analyses were considered for mood, anxiety, and comorbid disorder. First, overall proportions were estimated by the age categories young-old, mid-old, old-old, and oldest old. Second, age differences were examined by gender. Finally, age differences were examined by race/ethnicity. To statistically test if prevalence trends across age groups were different between males and females and between race/ethnic categories, interaction terms with age modeled as continuous (and main effects) were examined in logistic regression analyses, correcting for the complex sampling design. Because overall prevalence rates were similar and prevalence patterns with age were similar across race/ethnic groups, sub-group results by race/ethnicity are not presented.
To produce nationally representative estimates, clustering and weighting techniques were implemented in order to reduce systematic bias and imprecision imbedded in the complex sampling design. Thus, the percents represent weighted proportions and statistical differences were estimated based on the Rao-Scott chi-square which corrects for the complex design.32 The standard errors were determined from a recalculation of variance using the Taylor Series linear approximation method.33 Of note, design adjusted estimates and tests are not computed when a table cell has zero frequency.
The part I sample and weights were used for all analyses, except individual analyses of posttraumatic stress disorder were conducted with part II weights, which included an additional weight adjusting for oversampling of part I cases. Because PTSD was a component of the pooled anxiety disorders, sensitivity analyses were conducted using the part II sample to examine pooled (any) anxiety disorders, as well as comorbid disorder. The results using either sample for analysis were shown to be similar. Therefore, to maintain power and precision, all final analyses of pooled disorders were conducted using the larger part I sample.
Statistical tests were two-tailed with P ≤ .05 defining statistical significance. All analyses were performed using SAS Survey procedures, version 9.1.3 (SAS Institute Inc., Cary, NC).
Results
The 2575 participants 55 years and older who were part of NCS-R included 43% 55-64, 32% 65-74, 20% 75-84, and 5% ≥85 years. The average age was approximately 68 years (SD = 9.2). The sample distribution was 59% women, 82% non-Hispanic white, 10% non-Hispanic black, and approximately 4% Hispanic. The majority of the sample had a high school education or higher, and over half the respondents were married or not living alone. The distribution of the sample by region was representative across the U.S.
In Table 1, cross-tabulations of demographic characteristics and 12-month DSM-IV/WMH-CIDI mood, anxiety, and comorbid mood-anxiety disorders are presented. Gender and marital status were prominent characteristics associated with DSM-IV disorders. Women had significantly higher rates of mood, anxiety, and comorbid disorder than men (P < .05). While being married or cohabitating were statistically significantly associated with lower rates of mood, anxiety, and comorbid disorder compared to being divorced, separated, widowed, or never married. For education, statistical differences were apparent for any anxiety disorders, where low education (incompletion of high school) and college years were associated with high rates of anxiety. There were no differences for any disorder by race/ethnicity or geographic region of residence.
Table 1. Demographic Characteristics of adults 55 years and older from the NCS-R by 12-Month DSM-IV/WMH-CIDI Mood, Anxiety, and Comorbid Disorders (N= 2575).
| Characteristic | Sample, No. [%] (Unweighted) | Any Mood % (SE) | Any Anxiety % (SE) | Comorbid % (SE) | Neither Disorder % (SE) |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 1053 [40.9] | 3.0(0.6) | 7.6(0.9) | 1.6(0.4) | 90.9(1.1) |
| Female | 1522 [59.1] | 6.4(0.7) | 14.7(0.9) | 3.7(0.6) | 82.6(0.9) |
| χ2[1]a | 8.7 | 26.7 | 9.9 | 23.5 | |
| P value | .003 | <.001 | .002 | <.001 | |
| Race/Ethnicity | |||||
| Non-Hispanic White | 2106 [81.8] | 4.7(0.4) | 11.2(0.7) | 2.6(0.3) | 86.8(0.6) |
| Non-Hispanic Black | 265 [10.3] | 5.5(1.1) | 13.1(2.0) | 3.5(0.8) | 84.8(2.1) |
| Hispanic/Other | 204 [7.9] | 6.6(2.0) | 13.7(3.3) | 4.0(1.8) | 83.7(2.9) |
| χ2[2]a | 2.0 | 1.4 | 1.9 | 2.2 | |
| P value | .372 | .486 | .387 | .332 | |
| Education, y | |||||
| 0-11 | 610 [23.7] | 4.8(0.9) | 14.4(1.6) | 3.2(0.8) | 84.0(1.7) |
| 12 | 837 [32.5] | 4.0(0.8) | 9.6(1.1) | 2.2(0.7) | 88.6(1.2) |
| 13-15 | 570 [22.1] | 6.8(1.0) | 14.0(1.6) | 3.9(0.7) | 83.2(1.8) |
| ≥16 | 558 [21.7] | 4.8(0.9) | 8.7(1.1) | 2.2(0.6) | 88.6(1.3) |
| χ2 [3] a | 4.6 | 14.5 | 4.4 | 10.3 | |
| P value | .203 | .002 | .222 | .016 | |
| Marital Status | |||||
| Married/cohabitating | 1460 [56.7] | 3.9(0.6) | 8.9(0.8) | 1.9(0.5) | 89.1(0.8) |
| Divorced/separated/widowed | 1023 [39.7] | 6.6(0.8) | 15.7(1.3) | 4.0(0.6) | 81.7(1.3) |
| Never married | 92 [3.6] | 6.2(2.7) | 14.6(3.8) | 5.3(2.4) | 84.5(4.1) |
| χ2[2]a | 8.5 | 25.9 | 9.5 | 27.4 | |
| P value | .014 | <.001 | .009 | <.001 | |
| Region | |||||
| Northeast | 520 [20.2] | 5.3(0.6) | 13.4(1.2) | 3.3(0.6) | 84.5(1.0) |
| Midwest | 699 [27.2] | 5.0(1.4) | 10.3(1.5) | 2.9(1.1) | 87.6(1.6) |
| South | 886 [34.4] | 5.0(0.3) | 11.4(1.4) | 2.7(0.6) | 86.3(1.2) |
| West | 470 [18.3] | 4.3(0.9) | 11.4(1.3) | 2.2(0.6) | 86.6(1.1) |
| χ2[3]a | 0.6 | 2.5 | 1.0 | 2.8 | |
| P value | .886 | .484 | .807 | .416 | |
Abbreviations: NCS-R, National Comorbidity Survey Replication; WMH-CIDI, World Mental Health Survey version of the Composite International Diagnostic Interview; N, unweighted; % (SE), weighted percent with standard error.
Rao-Scott χ2[df] test was used to correct for the complex survey design.
Twelve-Month Age-Specific Prevalence
Mood Disorders
The overall and age-specific 12-month rates for mood disorders are presented in Table 2. The rates mainly declined across age groups (55 and older). Twelve-month rates for any mood disorder and major depressive disorder significantly declined with age (P < .001).
Table 2. Twelve-Month Prevalence Rates of DSM-IV/WMH-CIDI Mood, Anxiety, and Comorbid Disorders in adults 55 years and older (N=2575).
| 12-Month Disorder | Total (N=2575) |
55-64 y % (SE) (n=1114) |
65-74 y % (SE) (n=813) |
75-84 y % (SE) (n=526) |
≥ 85 y % (SE) (n=122) |
Rao-Scott χ2[df] |
P Value |
|---|---|---|---|---|---|---|---|
| Mood Disorders | |||||||
| Any mood | 4.9(0.4) | 7.6(0.9) | 3.6(0.6) | 1.8 (0.6) | 2.4(1.4) | 28.2[3] | <.001 |
| Major depressive disorder | 4.0(0.4) | 6.2(0.8) | 3.1(0.6) | 1.1(0.5) | 1.8(1.3) | 25.9[3] | <.001 |
| Dysthymia | 0.8(0.3) | 1.2(0.6) | 0.5(0.2) | 0.5(0.3) | 0.5(0.6) | 3.4[3] | .34 |
| Bipolar I or II disordera | 0.9(0.2) | 1.4(0.4) | 0.5(0.3) | 0.7(0.4) | … | … | … |
| Anxiety Disorders | |||||||
| Any anxietyb | 11.6(0.7) | 16.6(1.2) | 8.9(1.1) | 6.0(0.9) | 8.1(2.5) | 52.5[3] | <.001 |
| Panic disorder | 1.3(0.3) | 2.0(0.6) | 0.6(0.3) | 1.0(0.4) | 0.5(0.5) | 8.8[3] | .03 |
| Agoraphobia without panic | 0.8(0.2) | 1.4(0.4) | 0.5(0.3) | 0.4(0.3) | … | … | … |
| Specific phobia | 6.5(0.5) | 8.8(0.9) | 4.9(0.9) | 4.4(0.9) | 5.1(2.1) | 15.5[3] | .001 |
| Social phobia | 3.5(0.4) | 5.1(0.7) | 3.1(0.6) | 1.5(0.5) | … | … | … |
| Generalized anxiety disorder | 2.0(0.3) | 3.2(0.5) | 1.4(0.5) | 0.8(0.3) | 1.8(1.2) | 12.7[3] | .005 |
| Posttraumatic stress disorderc | 2.1(0.4) | 4.7(0.9) | 0.6(0.2) | 0.1(0.1) | 0.7(0.6) | 74.8[3] | <.001 |
| Comorbid disorderbd | 2.8(0.4) | 4.8(0.8) | 1.7(0.5) | 0.9(0.4) | … | … | … |
Abbreviations: WMH-CIDI, World Mental Health Survey version of the Composite International Diagnostic Interview; N, unweighted; ellipses, data not available to compute weighted estimate/test.
Bipolar I and II disorder represents proportion of respondents who endorsed either bipolar I, II, or subthreshold bipolar.
Estimated in the part I sample. No adjustment is made for the fact that PTSD in the category was directly assessed in part II. Sensitivity analyses performed with part II showed similar results.
Analyses conducted using the part II sample (PTSD directly assessed), which included all part I respondents with lifetime disorder plus a probability subsample of other respondents (n = 1372).
Comorbid disorder defined as any co-occurring mood-anxiety disorders.
For stratified analyses by gender, Figure 1a shows the prevalence rates of pooled mood disorders for females and males; twelve-month prevalence rates declined with age for both females and males. However, the twelve-month rates with increasing age were statistically significantly more prominent for females than males [β-interaction = .06; Wald χ21 = 3.7; P-interaction = .05]. There were no differences in the prevalence of mood disorders with increasing age by race or ethnicity.
Figure 1.
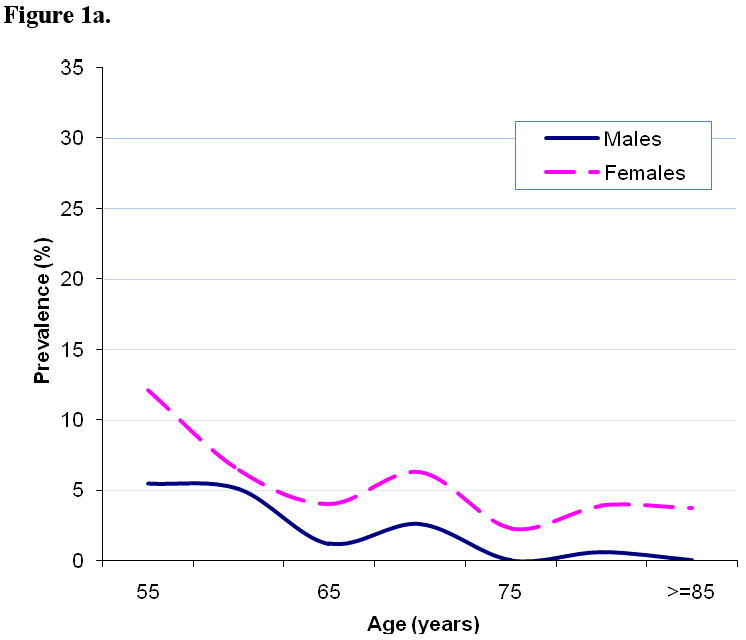
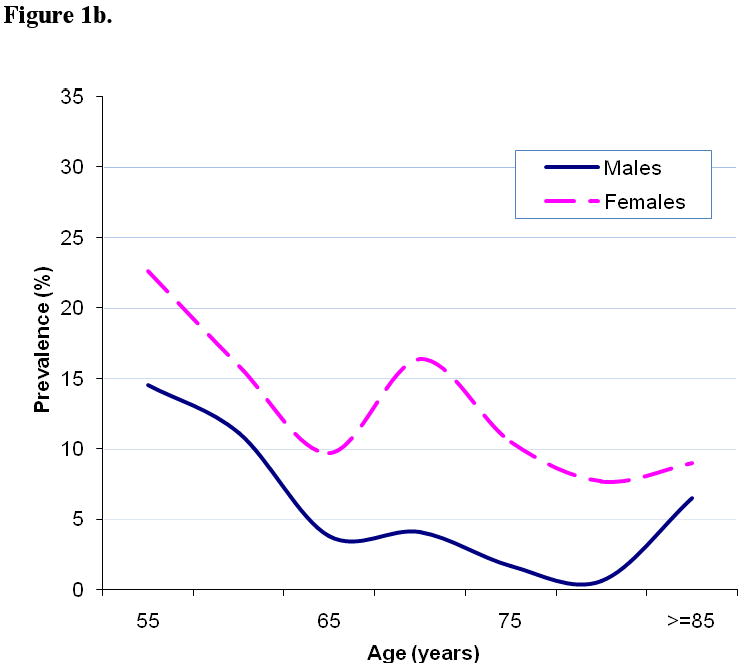
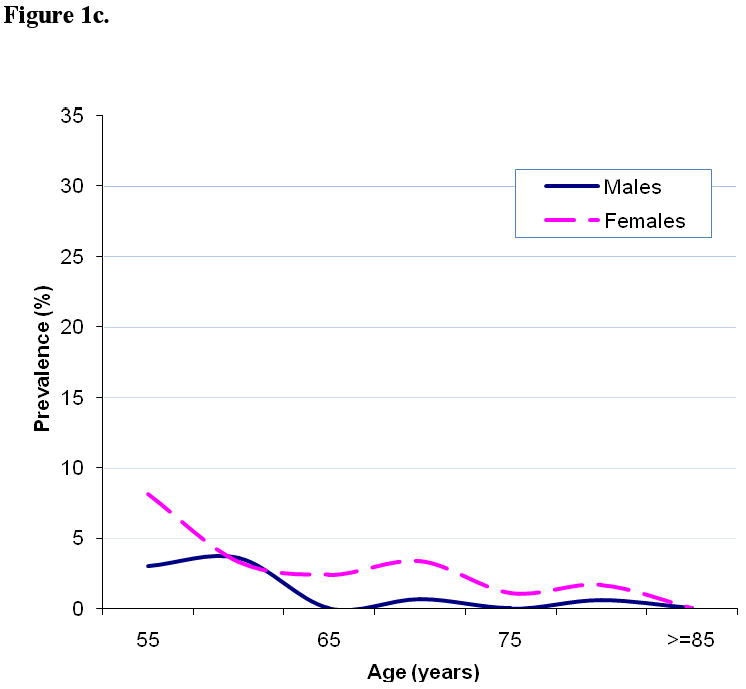
Figure 1a. Twelve-Month Prevalence Rates of Any DSM-IV/WMH-CIDI Mood Disorder in Males (N=1053) and Females (N=1522)
Figure 1b. Twelve-Month Prevalence Rates of Any DSM-IV/WMH-CIDI Anxiety Disorder in Males (N=1053) and Females (N=1522)
Figure 1c. Twelve-Month Prevalence Rates of DSM-IV/WMH-CIDI Comorbid Disorder in Males (N=1053) and Females (N=1522)
Anxiety Disorders
The overall and age-specific 12-month rates for anxiety disorders are presented in Table 2. The most prevalent 12-month anxiety disorder was specific phobia, followed by social phobia, posttraumatic stress disorder, generalized anxiety disorder, panic disorder, and agoraphobia. Differences in 12-month prevalence rates across the four age categories for the pooled and for most individual anxiety disorders were statistically significant (P < .05).
For analyses by gender, Figure 1b shows that for females [Rao-Scott χ23 = 22.7; P < .001] and males [Rao-Scott χ23 = 41.8; P < .001] the prevalence of pooled anxiety disorder declined with age, with rates among females significantly more prominent than males [β-interaction = .05; Wald χ21 = 5.0; P-interaction = .03]. There were no differences in the prevalence of anxiety disorders with increasing age by race or ethnicity.
Comorbid Mood-Anxiety Disorder
With regard to comorbid mood-anxiety disorder, the overall 12-month prevalence rate was 3% (Table 2). The twelve-month rates for comorbid disorder showed a general decline with age (55 and older). Figure 1c portrays a similar decreasing prevalence pattern by gender for the diagnosis of 12-month comorbid mood-anxiety disorder across age groups; with no statistically significant difference between females and males (P-interaction = .22).
Comment
The purpose of this paper was to document nationally representative age-specific prevalence rates of DSM-IV mood, anxiety, and comorbid mood-anxiety disorder for adults 55 years and older. There are three key findings in the present study: 1) Declining prevalence with age; 2) Rates of anxiety disorders as high as mood disorders; and 3) The common co-occurrence of these disorders. Rates were generally higher for women in each age group, but did not vary by race or ethnicity.
The first and general finding from our study was the overall trend found for adults of increasing age – a general decline in the 12-month prevalence of mood, anxiety, and comorbid disorder. Statistically, prevalence rates with increasing age were more prominent for 12-month rates among women compared to men (P < .05). Earlier studies of both clinical and community-based studies suggest such a pattern of decline with age.6,10,34 The ECA found a consistent trend of lower DSM mental disorders in late life when grouping age categories together. Work by Gum et al.20 found a similar trend in the NCS-R with lower rates in older adults (≥ 65 years) vs younger adults (aged 18-64 years). Recent international research by Kohn and colleagues found the same decreasing pattern with age in a sample of adults from Latin America.35 Further, studies have found women to have higher prevalence rates of symptoms of depression, anxiety, and co-existing depression-anxiety than men, while racial differences are less consistent.16-18 Our study found no statistically significant difference across race/ethnicity; however, small cell counts for minority groups equated to lower power to detect a difference.
The second key finding was that rates of anxiety disorders were as high or even higher (with pooled rates higher; overall 12-month = 12%) than mood disorders (overall 12-month = 5%). The age-specific rates of anxiety were higher than mood disorders in each age group, with 12-month rates 17% for those 55 to 64 years old (vs 8% for mood) and 8% for those 85 and older (vs 2% for mood). Similarly, anxiety disorders were the most prevalent disorders among those aged 65 years and older in the ECA with phobic disorder the most prevalent individual disorder.10 Interestingly, we found high prevalence of specific and social phobias, disorders not often investigated and often under appreciated. Of note, unlike our study, the Longitudinal Aging Study Amsterdam (LASA) determined high rates of generalized anxiety disorder (7.3% vs. 2.0% in our study).36 This discrepancy between reported prevalence rates highlights largely methodological differences (e.g., sampling procedures and attrition rates, definition and operationalization of anxiety) and potential cultural differences between population-based studies. Most studies of anxiety disorders among U.S. older adults have been examined relative to their occurrence in patients with depression. Research by Lenze et al.37 found a high rate of at least one current (23%) anxiety disorder in depressed older adults (60 and older) from primary care and psychiatric settings. Work from our group investigating anxiety symptoms in a cohort of community-dwelling older adults (aged 70-79 years) found that 19% of participants reported current anxiety symptoms, where women (20%) had higher rates than men (12%) (P < .001).16 Our present findings suggest similar results with diagnostic anxiety disorders, which are prominent and pervasive in older adults even into the oldest years.
The third finding was the high rate of co-existing mood and anxiety disorders in NCS-R respondents (overall 12-month = 3%). Geriatric psychiatry research is struggling to understand the comorbid depression-anxiety outcomes and treatment needs. Thus far, the impact of comorbid depression-anxiety is greater than initially estimated. Most U.S. studies have been clinically-based and, as mentioned above, found high prevalence rates of comorbid anxiety in patients with depression.37-39 In contrast, the NCS-R's advantage is that it allows the examination of a nationally representative group—highlighting the impact of comorbid and individual mood and anxiety disorders in the population. Our results showed that the co-occurrence of mood and anxiety disorders in the community was high, common and significant across age strata 55 years and older, investigating overall trends as well as by gender and race/ethnicity.
Investigation of the oldest age cohort (85 years and older), which maintained prominent prevalence rates, warrants comment. Because individuals 85 years and older are not always captured in geriatric psychiatric research, the present examination suggests the need for more research in this group and confronting potential challenges specific to the study of this group. For example, the oldest old are less available for study except in institutional settings and experience heterogeneity of comorbid diseases—creating difficult study of pure disorders in the population.40 Epidemiological evidence for age-specific trends of depression in older adults often measured with the CES-D scale41 or Geriatric Depression Scale (GDS)42 have shown an increase in symptomatology in the oldest cohort,1,9,10,40,43 while in most clinical studies6,10 rates of diagnosed depression consistently decline in older age groups. Thus, understanding diagnostic patterns in the oldest old is complex and requires more investigation than the present study provides.
In contrast, given the strong effect of cognitive and physical health as predictors and outcomes of mental health disorders,1-5 the finding of a general decline in mood, anxiety, and comorbid mood-anxiety disorders with age is counter-intuitive. Three possible explanations for this general decline with age include: 1) Cohort effect (i.e., as the young-old age they will maintain higher levels of mental disorders); 2) Healthy survivor bias or differential mortality, institutionalization (i.e., those institutionalized were not sampled); and 3) Epidemiological methods and diagnostic issues in assessing older adults for psychiatric disorders (e.g., difficulty remembering symptoms, stigma related to the reporting of mental health disorders, somatic symptoms reported but determined to be related to chronic conditions instead of mental health disorders).
The strengths of this study include a nationally representative probability sample, current DSM diagnostic assessment, and precise age-stratification to define trends for young-old, mid-old, old-old, and oldest old cohorts. This study helps to describe the prevalence of mood, anxiety, and comorbid mood-anxiety disorder in a nationally representative sample of older U.S. adults. It highlights those disorders with the greatest potential for intervention and prevention, research and services—translating back into science those diseases with the greatest potential impact on the older public's health.
The implications of the study findings include the public health relevance of anxiety disorders in older adults and the need for more research focused on the oldest old age group, females, and minority groups. Given the high prevalence of anxiety disorders in the community, the lack of attention in research and program policy statements to anxiety disorders in older adults is disturbing.44,45 The literature has shown that comorbid anxiety in depressed elderly patients leads to poorer treatment outcomes than depression alone.38 Thus, the high prevalence of comorbid mood-anxiety disorders found in our study suggests the modifying influence of anxiety on antidepressant treatment outcomes is a serious concern.
The oldest old are the fastest growing age group in the United States.40 The oldest old are often underrepresented so estimates from community samples have been difficult to obtain. Because mental disorders are associated with declining physical health that occurs with frequency in older age,1-5 the assessment of psychiatric disorders is an important indicator of health and increased risk of mortality in this older population.
In addition, these results expand beyond the field of geriatric psychiatry; highlighting the importance of diagnosis, treatment, and management of psychiatric symptoms and disorders in younger years. Given the chronicity of these disorders, preventing their occurrence in later life implies that clinicians and researchers outside geriatrics need to be more vigilant about diagnosis and treatment in early years. These disorders are common in younger adults and most have early age-of-onset, but often are not diagnosed or under-diagnosed and under-treated.21,27
There are three main limitations of this study. First, the NCS-R underrepresents homeless, institutionalized, and non-English speaking older adults. Second, there may be issues of stigma, whereby older adults with mental illness might be less inclined to participate in a mental health survey. Third, even though the WMH-CIDI was shown to have good concordance with the SCID,21 it is still a lay-administered interview rather than a clinically-administered assessment, especially in the context of medical illness, disability, and cognitive decline. Thus, given the above limitations, the estimates herein are probably conservative.
Additional limitations include details associated with surveying older populations that were not available in the NCS-R. These include assessment of the response rate in those aged 55 years and older and demonstration of acceptable reliability of the NCS-R instruments for older adults. Further, the NCS-R was limited in its assessment of mood disorders, as we were unable to determine prevalence rates of some disorders that would be considered common in older adults, e.g., depression NOS, dementia with depression, mood disorders secondary to medical disorders, adjustment disorders with depression, and bereavement. Because depression in older adults may present differently (more apathy, social withdrawal, irritability), the criteria for a major depression diagnosis may not be met, although the other symptoms may be severe, suggesting an underestimation of the prevalence rate in NCS-R older adults. This underestimation is probably large considering the potential for reporting bias in older adults due to difficulty recalling symptoms or difficulty associating symptoms with psychological distress.
The study of nationally representative samples provides evidence for research and policy planning that helps to define community-based priorities for future psychiatric research. The findings of this study emphasize the importance of individual and co-existing mood and anxiety disorders when studying older adults, even the oldest cohorts. Further study of risk factors, course, and severity is needed in order to target intervention, prevention, and health care needs. Given the rapid aging of the U.S. population, the potential public health burden of late-life mental health disorders will likely grow as well, suggesting the importance of continued epidemiologic monitoring of the mental health status of the young-old, mid-old, old-old, and oldest old cohorts.
Acknowledgments
This research used the National Comorbidity Survey Replication (NCS-R), 2001-2003 data set [made accessible in 2007, machine-readable data files]. The NCS-R is part of the Collaborative Psychiatric Epidemiology Surveys (CPES), 2001-2003. The Inter-university Consortium for Political and Social Research (ICPSR; Ann Arbor, Michigan) is responsible for the preparation, organization, and access of the public use of this data [http://www.icpsr.umich.edu/CPES]. We thank the NCS-R researchers who participated in collecting the data that made this project possible.
Funding/Support and Role of Sponsor: Dr. Byers is supported by a K01 Career Development Award (MH079093) from the National Institute of Mental Health. Dr. Yaffe is supported, in part, by a K24 Midcareer Investigator Award (AG031155) from the National Institute on Aging. The National Comorbidity Survey Replication (NCS-R) was supported by the National Institute of Mental Health (U01-MH60220), with supplemental support from the National Institute of Drug Abuse, the Substance Abuse and Mental Health Services Administration, the Robert Wood Johnson Foundation (044708), and the John W. Alden Trust. The sponsors had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; or the preparation, review, or approval of the manuscript.
Footnotes
Portions of this manuscript were presented at the 61st Annual Scientific Meeting of the Gerontological Society of America, National Harbor, Maryland, November 21-25, 2008.
Author Contributions: All authors had access to the NCS-R data. Dr. Byers conducted the data analysis, and takes responsibility for the integrity of the data and the accuracy of the statistical results.
Conflicts of interest: The authors have no competing interests, including specific financial interests or relationships or affiliations relevant to the subject of this manuscript.
Publisher's Disclaimer: Disclaimer: We acknowledge that the original collector of the data, ICPSR, sponsoring organizations, agencies, or the U.S. government bear no responsibility for use of the data or for interpretations or inferences based upon such uses. The views and opinions expressed in this report are those of the authors and should not be construed otherwise.
References
- 1.Blazer DG, Hybels CF. Origins of depression in later life. Psychol Med. 2005;35(9):1241–1252. doi: 10.1017/S0033291705004411. [DOI] [PubMed] [Google Scholar]
- 2.Walke LM, Byers AL, Tinetti ME, Dubin JA, McCorkle R, Fried TR. Range and severity of symptoms over time among older adults with chronic obstructive pulmonary disease and heart failure. Arch Intern Med. 2007;167(22):2503–2508. doi: 10.1001/archinte.167.22.2503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry. 2001;9(2):102–112. [PubMed] [Google Scholar]
- 4.Yaffe K, Edward ER, Covinsky KE, Lui LY, Eng C. Depressive symptoms and risk of mortality in frail, community-living elderly persons. Am J Geriatr Psychiatry. 2003;11(5):561–567. [PubMed] [Google Scholar]
- 5.Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, Schulz R, Reynolds CF. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. Am J Geriatr Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- 6.Jeste DV, Blazer DG, First M. Aging-related diagnostic variations: need for diagnostic criteria appropriate for elderly psychiatric patients. Biol Psychiatry. 2005;58(4):265–271. doi: 10.1016/j.biopsych.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 7.Kelsey JL, Whittemore AS, Evans AS, Thompson WD. Methods in Observational Epidemiology. 2nd. New York, NY: Oxford University Press Inc.; 1996. [Google Scholar]
- 8.Bruce ML. Psychosocial risk factors for depressive disorders in late life. Biol Psychiatry. 2002;52(3):175–184. doi: 10.1016/s0006-3223(02)01410-5. [DOI] [PubMed] [Google Scholar]
- 9.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58A(3):249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 10.Hybels CF, Blazer DG. Epidemiology of late-life mental disorders. Clin Geriatr Med. 2003;19(4):663–696. doi: 10.1016/s0749-0690(03)00042-9. [DOI] [PubMed] [Google Scholar]
- 11.Regier DA, Myers JK, Kramer M, Robins LN, Blazer DG, Hough RL, Eaton WW, Locke BZ. The NIMH Epidemiologic Catchment Area program: historical context, major objectives, and study population characteristics. Arch Gen Psychiatry. 1984;41(10):934–941. doi: 10.1001/archpsyc.1984.01790210016003. [DOI] [PubMed] [Google Scholar]
- 12.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 13.American Psychiatric Association. DSM-III: Diagnostic and Statistical Manual of Mental Disorders. 3rd. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 14.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 15.Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51(1):8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 16.Mehta KM, Simonsick EM, Penninx BW, Schulz R, Rubin SM, Satterfield S, Yaffe K. Prevalence and correlates of anxiety symptoms in well-functioning older adults: findings from the Health Aging and Body Composition study. J Am Geriatr Soc. 2003;51(4):499–504. doi: 10.1046/j.1532-5415.2003.51158.x. [DOI] [PubMed] [Google Scholar]
- 17.Skarupski KA, Mendes de Leon CF, Bienias JL, Barnes LL, Everson-Rose SA, Wilson RS, Evans DA. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60B(3):P136–P142. doi: 10.1093/geronb/60.3.p136. [DOI] [PubMed] [Google Scholar]
- 18.Cohen CI, Magai C, Yaffee R, Walcott-Brown L. The prevalence of anxiety and associated factors in a multiracial sample of older adults. Psychiatr Serv. 2006;57(12):1719–1725. doi: 10.1176/ps.2006.57.12.1719. [DOI] [PubMed] [Google Scholar]
- 19.Ford BC, Bullard KM, Taylor RJ, Toler AK, Neighbors HW, Jackson JS. Lifetime and 12-month prevalence of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition disorders among older African Americans: findings from the National Survey of American Life. Am J Geriatr Psychiatry. 2007;15(8):652–659. doi: 10.1097/JGP.0b013e3180437d9e. [DOI] [PubMed] [Google Scholar]
- 20.Gum AM, King-Kallimanis B, Kohn R. Prevalence of mood, anxiety, and substance-abuse disorders for older Americans in the National Comorbidity Survey-Replication. Am J Geriatr Psychiatry. 2009;17(9):769–781. doi: 10.1097/JGP.0b013e3181ad4f5a. [DOI] [PubMed] [Google Scholar]
- 21.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 22.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. Int J Methods Psychiatr Res. 2004;13(2):60–68. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kessler RC, Berglund P, Chiu WT, Demler O, Heeringa S, Hiripi E, Jin R, Pennell BE, Walters EE, Zaslavsky A, Zheng H. The US National Comorbidity Survey Replication (NCS-R): design and field procedures. Int J Methods Psychiatr Res. 2004;13(2):69–92. doi: 10.1002/mpr.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alegria M, Jackson JS, Kessler RC, Takeuchi D. ICPSR20240-v2. 2007. Aug 15, Collaborative Psychiatric Epidemiology Surveys (CPES), 2001-2003 [United States] [Computer file] Ann Arbor, MI: Institute for Social Research, Survey Research Center [producer], 2007. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor] [Google Scholar]
- 25.Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kessler RC, Demler O, Frank RG, Olfson M, Pincus HA, Walters EE, Wang P, Wells KB, Zaslavsky AM. Prevalence and treatment of mental disorders, 1990 to 2003. NEJM. 2005;352(24):2515–2523. doi: 10.1056/NEJMsa043266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, Rush AJ, Walters EE, Wang PS. The epidemiology of major depressive disorder: results from The National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289(23):3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) Int J Methods Psychiatr Res. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.World Health Organization. International Classification of Diseases. 10th rev (ICD-10) Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- 30.Kessler RC, Abelson J, Demler O, Escobar JI, Gibbon M, Guyer ME, Howes MJ, Jin R, Vega WA, Walters EE, Wang P, Zaslavsky A, Zheng H. Clinical calibration of DSM-IV diagnoses in the World Mental Health (WMH) version of the World Health Organization (WHO) Composite International Diagnostic Interview (WMH-CIDI) Int J Methods Psychiatr Res. 2004;13(2):122–139. doi: 10.1002/mpr.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis-I Disorders. Research version, non-patient ed (SCID-I/NP) New York: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 32.Rao J, Scott A. The analysis of categorical data from complex sample surveys: chi-squared tests for goodness of fit and independence in two-way tables. J Am Stat Assoc. 1981;76:221–230. [Google Scholar]
- 33.Levy PS, Lemeshow S. Sampling of Populations. New York: John Wiley & Sons; 1999. [Google Scholar]
- 34.Henderson AS, Jorm AF, Korten AE, Jacomb P, Christensen H, Rodgers B. Symptoms of depression and anxiety during adult life: evidence for a decline in prevalence with age. Psychol Med. 1998;28(6):1321–1328. doi: 10.1017/s0033291798007570. [DOI] [PubMed] [Google Scholar]
- 35.Kohn R, Vicente B, Saldivia S, Rioseco P, Torres S. Psychiatric epidemiology of the elderly population in Chile. Am J Geriatr Psychiatry. 2008;16(12):1020–1028. doi: 10.1097/JGP.0b013e31818a0e1c. [DOI] [PubMed] [Google Scholar]
- 36.Beekman AT, Bremmer MA, Deeg DJ, van Balkom AJ, Smit JH, de Beurs E, van Dyck R, van Tilburg W. Anxiety disorders in later life: a report from the Longitudinal Aging Study Amsterdam. Int J Geriatr Psychiatry. 1998;13(10):717–726. doi: 10.1002/(sici)1099-1166(1998100)13:10<717::aid-gps857>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]
- 37.Lenze EJ, Mulsant BH, Shear MK, Schulberg HC, Dew MA, Begley AE, Pollock BG, Reynolds CF. Comorbid anxiety disorders in depressed elderly patients. Am J Psychiatry. 2000;157(5):722–728. doi: 10.1176/appi.ajp.157.5.722. [DOI] [PubMed] [Google Scholar]
- 38.Lenze EJ. Comorbidity of depression and anxiety in the elderly. Curr Psychiatry Rep. 2003;5(1):62–67. doi: 10.1007/s11920-003-0011-7. [DOI] [PubMed] [Google Scholar]
- 39.Lenze EJ, Mulsant BH, Shear MK, Alexopoulos GS, Frank E, Reynolds CF. Comorbidity of depression and anxiety disorders in later life. Depress Anxiety. 2001;14(2):86–93. doi: 10.1002/da.1050. [DOI] [PubMed] [Google Scholar]
- 40.Blazer DG. Psychiatry and the oldest old. Am J Psychiatry. 2000;157(12):1915–1924. doi: 10.1176/appi.ajp.157.12.1915. [DOI] [PubMed] [Google Scholar]
- 41.Radloff L. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 42.Yesavage JA. Geriatric Depression Scale. Psychopharmacol Bull. 1988;24:709–711. [PubMed] [Google Scholar]
- 43.Gatz M, Hurwicz ML. Are old people more depressed? Cross-sectional date on Center for Epidemiological Studies Depression Scale factors. Psychol Aging. 1990;5(2):284–290. doi: 10.1037//0882-7974.5.2.284. [DOI] [PubMed] [Google Scholar]
- 44.Wetherell JL, Kim DS, Lindamer LA, Thorp SR, Hawthorne W, Kim K, Hough RL, Garcia P, Jeste DV. Anxiety disorders in a public mental health system: clinical characteristics and service use patterns. J Affect Disord. 2007;104(1-3):179–183. doi: 10.1016/j.jad.2007.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Flint AJ. Epidemiology and comorbidity of anxiety disorders in the elderly. Am J Psychiatry. 1994;151(5):640–649. doi: 10.1176/ajp.151.5.640. [DOI] [PubMed] [Google Scholar]


