Abstract
Purpose
To evaluate inter- and intra-fraction esophageal motion in the right-left (RL) and anterior-posterior (AP) directions using computed tomography (CT) in esophageal cancer patients.
Methods and Materials
Eight patients underwent CT simulation and CT-on-rails imaging before and after radiotherapy. Inter-fraction displacement was defined as differences between pre-treatment and simulation images. Intra-fraction displacement was defined as differences between pre- and post-treatment images. Images were fused using bone registries, adjusted to the carina. The mean, average of the absolute, and range of esophageal motion were calculated in RL and AP directions, above and below the carina.
Results
Thirty-one CT image sets were obtained. The incidence of esophageal inter-fraction motion ≥5 was 24% and ≥10 mm was 3%; intra-fraction motion ≥ 5mm was 13% and ≥10 mm was 4%. The average RL motion was 1.8±5.1 mm, favoring leftward movement, and the average AP motion was 0.6±4.8 mm, favoring posterior movement. Average absolute motion was 4.2 mm or less in RL and AP directions. Motion was greatest in the RL direction above the carina. Coverage of 95% of esophageal mobility requires 12mm left, 8mm right, 10mm posterior, and 9mm anterior margins.
Conclusion
In all directions, the average of the absolute inter-fraction and intra-fraction displacement was 4.2 mm or less. These results support a 12 mm left, 8 mm right, 10 mm posterior, and 9 mm anterior margin for ITV and can guide margins for future IMRT trials to account for organ motion and set up error in 3-dimesional planning.
Keywords: Esophageal cancer, Radiotherapy, Treatment margin, Organ motion
Introduction
Radiotherapy (RT) plays an important role in the treatment of esophageal cancer in the pre-operative, post-operative, and definitive settings (1–5). Determination of the appropriate planning target volume (PTV) is important to minimize locoregional recurrence and limit toxicity of normal surrounding tissues. When treating esophageal malignancies with RT, block edge is often 5 cm from the gross tumor volume (GTV) in the superior-inferior directions and 2–3 cm in the lateral and anterior-posterior directions (3–5). These margins account for microscopic tumor spread and skip metastases, denoted by the clinical target volume (CTV), organ motion represented by the internal target volume (ITV), set-up variation represented by the PTV, and pneumbra. Minimization of margins, without sacrificing CTV coverage, is necessary to minimize treatment-related toxicities to the lungs and heart when treating esophageal malignancies. Lee et al. demonstrated increased postoperative pulmonary complications in patients receiving preoperative chemoradiation for esophageal cancer when the V10 was ≥40% and when the V15 was ≥30% of lung volume (6). More recently, the risk of pulmonary complications has been related to the volume of lung receiving doses as low as 5Gy (7). Cardiac toxicity has also been described following treatment of esophageal malignancies and appears to be related to fraction size (8), female gender, and cardiac dose (9).
An accurate assessment of esophageal motion is important when determining an appropriate ITV and PTV. Physiologic esophageal motion results from the respiratory cycle, cardiac motion, and esophageal peristalsis. Motion of the esophagus has been investigated in multiple settings. Using lower esophageal sphincter pressure readings, axial motion has been described as approximately 4 mm in the thoracic and 6 mm in the abdominal esophagus (10). Lateral esophageal motion using digital cine-fluoroscopic imaging performed prior to and after cardiac catheter ablation for atrial fibrillation was documented to be greater than or equal to 2 cm in two-thirds of patients (11). Computed tomography (CT) scans obtained during inhalation and exhalation phases demonstrate radial displacement of the esophagus on the order of 3 mm in the superior cervical esophagus, 5 mm at the thoracic inlet, 6–7 mm at the carina level, and 10–12 mm at the gastro-esophageal (GE) junction (12). Lorchel et al recommended a 10 mm ITV margin based on their studies using breath hold CT scans performed at inspiration and expiration (13). In breath hold CT imaging using the optic flow method, esophageal motion was noted to be up to 14 mm with greatest motion at the GE junction (14). Using 4-dimensional CT (4DCT) during normal respiration, Dielman et al determined that a lateral margin encompassing 95% of esophageal motion in the proximal, mid, and caudal esophagus would be 5 mm, 7 mm, and 9 mm, respectively. In the anterior-posterior direction, the reported margins were 5 mm, 6 mm, and 8 mm (15). Patel et al. recommended 1.5 cm superior-inferior, 0.75 cm left-right, and 0.75 cm anterior-posterior to cover >95% of esophageal primary tumors based on their study of respiratory motion of primary esophageal cancer patients using 4DCT (16). Inter-fraction esophagus motion during radiation treatment, as measured using daily CT imaging of six patients with a Siemens PRIMATOM (CT-on-rails™) system, supported a margin of 2–5 mm in all directions for esophageal motion, though this was only presented in abstract format (17). Esophageal motion during radiation therapy has not been well described in our review of the literature. The aim of the present study was to report our results concerning inter- and intra-fraction esophageal motion in patients being treated for cancer of the esophagus and its implications for appropriate treatment margins.
Methods and Materials
From 2003–2004, patients diagnosed with esophageal malignancies who presented to the Department of Radiation Oncology at the Fox Chase Cancer Center were offered an IRB-approved clinical trial evaluating inter- and intra-fraction motion of the esophagus in the right-left (RL) and anterior-posterior (AP) directions using a CT-on-rails™ system (Siemens, Erlangen, Germany). CT-on-rails™ is a diagnostic CT scanner installed in the treatment room, the technique of which has been previously described (18). As no fiducials were placed in the tumor, cranial-caudal esophageal motion was not addressed due to difficulty identifying superior to inferior esophageal motion with CT-on-rails™. The initial goal was to enroll 30 patients. Due to the non-optimal depth dose characteristics associated with the 6 MV beam available in the treatment room which houses the CT-on-rails™ system, the study was terminated prior to the planned accrual. A total of eight patients with pathologically confirmed esophageal cancer were enrolled with informed consent obtained prior to participation. The patient characteristics are summarized in Table 1. The average age was 62 years (range: 38–77) and all but one patient was male. Five patients had pathologically proven adenocarcinoma of the esophagus, while the remaining three patients were diagnosed with squamous cell carcinoma. The majority of patients were treated with concurrent chemotherapy. Three patients were treated with definitive intent, three were treated palliatively, and two were treated with pre-operative chemoradiotherapy. Malignancy location was the distal thoracic esophagus (>32cm from incisors to gastro-esophageal junction) in one-half of the patients and the mid thoracic esophagus (>24 to ≤32cm from the incisors) in the other half. Two patients were Stage II, one was Stage III, one was Stage IVa, and four were stage IVb at the time of diagnosis, staged in accordance with the AJCC Cancer Staging, sixth edition (19).
Table 1. Patient Characteristics.
Thirty-one CT image sets were obtained from eight patients. Patient characteristics include patient specific details including gender, age at treatment, stage, histology, tumor location, use of concurrent chemotherapy, and treatment intent.
| No. of patients | 8 |
| Male/female | 7/1 |
| Age (y), mean (range) | 62.3 (38–77) |
| Pathology, n (%) | |
| Adenocarcinoma | 5 (62.5) |
| Squamous cell carcinoma | 3 (37.5) |
| Stage, n (%)* | |
| II | 2 (25) |
| III | 1 (12.5) |
| IVa | 1 (12.5) |
| IVb | 4 (50) |
| Tumor Location, n (%)† | |
| Mid Esophagus | 4 (50) |
| Distal Esophagus | 4 (50) |
| Concurrent Chemotherapy, n (%) | |
| Yes | 6 (75) |
| No | 2 (25) |
| Treatment intention | |
| Definitive | 3 (37.5) |
| Neo-adjuvant | 2 (25) |
| Palliative | 3 (37.5) |
| No. of CT sets, mean (range) ‡ | 3.9 (1–5) |
Staging per AJCC Cancer Staging Manual, Sixth Edition (2002)
Mid esophagus, >24 to ≤32 cm from the incisors; distal esophagus, >32 cm from incisors.
Refers to number of simulation, pre-treatment, and post-treatment CT image sets obtained for each patient (the fractions for which pre-treatment and post-treatment CT scans were obtained).
Each patient underwent CT simulation, immobilized supine in an alpha-cradle cast with arms abducted over their heads. Images were obtained from the apex of the lungs to the midabdominal area using a 3 mm slice thickness. The isocenter was determined on the CT simulator and tattoos were marked on the patient to align to isocenter. The CTV, carina, lungs, and esophagus were outlined and a treatment plan was created. The patients were set-up on their tattoos using lasers in the treatment room. CT scans were obtained prior to and after treatment with the CT-on-rails™ system on the first day of week 1 (1 patient), weeks 1 to 3 (1 patient), weeks 1 to 4 (3 patients), weeks 1 to 5 (2 patients), and weeks 1–2 and 5–7 (1 patient). The number of CT image sets obtained per patient is inconsistent due to patient clinical status and tolerance of the treatment position.
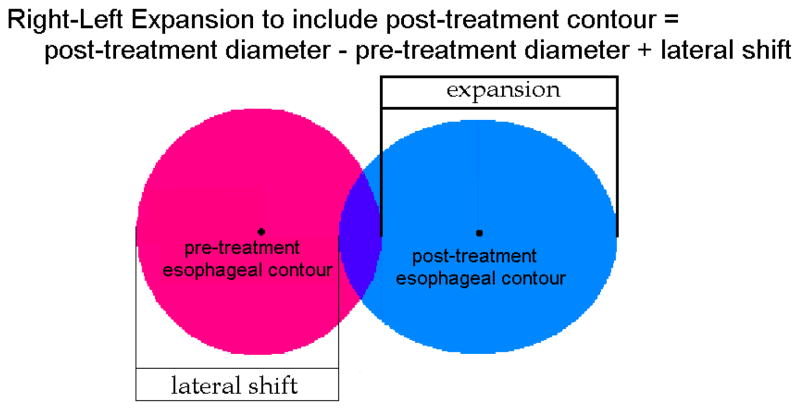
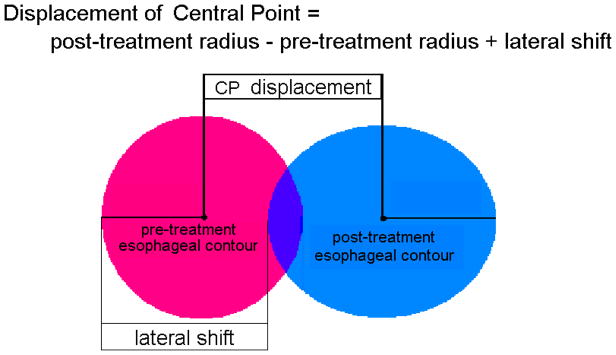
To calculate intra-fraction motion, the pre- and post-treatment CT scans were fused using bone registries and adjusted to the carina. The esophageal contours on the pre-treatment scans were transferred onto the fused post-treatment CT. The RL esophageal diameter on each scan and the distance between the right lateral aspect of the esophagus on the pre- and post-treatment CT scans (i.e., “lateral shift”) was recorded for each CT slice. Two methods of recording esophageal motion were used – expansion and central point displacement. Expansion is defined as the additional length in the RL or AP direction to include the esophageal contours from both CT images. Displacement is defined as the movement between the two CT images of the central point of the esophageal RL or AP diameter. The reason for using both parameters is to better delineate esophageal motion. For example, if the esophagus is fixed in a specific position, the expansion value increases as esophageal diameter increases, but the displacement remains zero. Likewise, if there is a shift in esophageal location, but no change in diameter, then the expansion is equal to the displacement.
The expansion was calculated by subtracting the pre-treatment esophageal diameter from the sum of the post-treatment esophageal diameter and lateral shift (Figure 1). The largest expansion above and below the carina was recorded for each patient. For each recorded expansion, the displacement of the central point in the RL direction was calculated by subtracting the pre-treatment radius from the sum of the post-treatment radius and lateral shift (Figure 2). A negative value represents motion to the patient’s right. The expansion and central point displacement in the AP direction was calculated using the same method, but the diameters were measured in the AP direction and the shift was from the anterior-most aspect of the esophagus from the pre-treatment contour. A negative value in the AP direction represents anterior motion. Inter-fraction AP and RL expansion and displacement were calculated in the same manner using the pre-treatment and CT simulation images. The calculated values for all patients were pooled and the mean, average of the absolute, and range of expansion and central point displacement was calculated with standard deviations in the RL and AP directions, above and below the carina. The percentage of expansion and displacement greater than or equal to 5mm, 10mm, and 20mm was calculated. The central point displacement and expansion values were averaged for a cumulative calculation of esophageal mobility.
Figure 1. Pictorial representation of Right-Left expansion.
Esophageal expansion was defined as the additional distance required to include the pre-treatment and post-treatment (or simulation) contours.
Figure 2. Pictorial representation of Right-Left central point displacement.
Central point displacement was defined as the shift of the central point between the fused pre-treatment and post-treatment (or simulation) contours.
Expansion and central point displacement in the RL versus AP directions, above versus below the carina, and intra- versus inter-fraction esophageal motion were statistically compared. Covariances of observations from any one patient were taken into account (20), see the appendix. Tests were based on the normal approximation (z-test) to covariance adjusted contrasts and were one-sided. We did not account for multiple comparisons made using the same data set.
Results
A total of 31 CT image sets were obtained. The carina remained fairly stable in relation to bone registries, requiring an average adjustment of 1.5 mm for inter-fraction and 0.8 mm for intra-fraction fusions (data not shown). There was no significant difference in RL or AP esophageal diameter in pre-treatment versus simulation (i.e., inter-fraction) or pre- versus post-treatment (i.e., intra-fraction) CT images.
Inter-fraction Expansion
The mean, average of the absolute value, range of expansion, and incidence of expansion greater than or equal to 5 mm and 10 mm is summarized in Table 2. The average inter-fraction RL expansion was 0.7 mm towards the patient’s left (positive value) below the carina and 1.8 mm to the left above the carina. The average absolute inter-fraction RL expansion and standard deviation was 2.8 ± 2.4 mm below and 4.0 ± 3.0 mm above the carina (p=0.002). Below the carina, inter-fraction RL expansion ≥5 mm occurred in 23% of measurements, but there was no expansion ≥10 mm. Above the carina, 35% of RL inter-fraction expansions were ≥5 mm and 6% were ≥10 mm. AP inter-fraction expansion averaged 0.8 mm anterior (negative value) below the carina and 1.3 mm posterior (positive value) above the carina. The average absolute AP inter-fraction expansion was 2.9 ± 2.2 mm below and 4.0 ± 5.2 mm above the carina (p=0.18). For inter-fraction AP expansion, 26% and 0% of measurements below the carina were ≥5 mm and ≥10 mm, respectively. Above the carina, inter-fraction AP expansion ≥5 mm occurred in 19% and ≥10 mm occurred in 6% of measurements. There was not a significant difference in inter-fraction expansion in the RL versus AP direction below (p=0.40) or above (p=0.47) the carina.
Table 2.
Expansion Results Summary.
| Location to Carina | Average Expansion, mm (SD) | Average Absolute Expansion, mm (SD) | Range, mm | %≥5mm | %≥10mm | |
|---|---|---|---|---|---|---|
| Inter-fraction | ||||||
| RL | Below | 0.7 (3.7) | 2.8 (2.4) | −8.0 to 8.1 | 23% | 0% |
| Above | 1.8 (4.7) | 4.0 (3.0) | −6.2 to 11.5 | 35% | 6% | |
| AP | Below | −0.8 (3.6) | 2.9 (2.2) | −6.6 to 6.5 | 26% | 0% |
| Above | 1.3 (6.5) | 4.0 (5.2) | −6.3 to 28.4 | 19% | 6% | |
| Intra-fraction | ||||||
| RL | Below | 2.0 (5.6) | 3.9 ( 4.4) | −6.5 to 22.0 | 26% | 6% |
| Above | 2.2 (6.5) | 4.1 (5.4) | −17.4 to 26.4 | 19% | 6% | |
| AP | Below | −0.3 (3.2) | 2.5 (2.1) | −5.0 to 9.3 | 10% | 0% |
| Above | 1.0 (4.7) | 2.4 (4.2) | −2.7 to 23.9 | 3% | 3% | |
The inter- and intra-fraction mean, average of the absolute value, and range of esophageal expansion in the RL (right-left) and AP (anterior-posterior) directions, above and beyond the carina is reported. The percent of expansions greater than or equal to 5 mm and 10 mm is included. A negative value represents motion to the patient’s right for the RL direction and anterior for the AP directions. SD = Standard Deviation
Intra-fraction Expansion
As with inter-fraction RL motion, the esophagus tended to move to the patient’s left for intra-fraction motion, with an average of 2.0 mm below the carina and 2.2 mm above the carina. The average absolute intra-fraction RL expansion was 3.9 ± 4.4 mm below and 4.1 ± 5.4 mm above the carina (p=0.42). The incidence of intra-fraction RL expansion ≥ 5 mm and ≥ 10 mm was 26% and 6% below the carina and 19% and 6% above the carina. Average intra-fraction AP expansion was 0.3 mm anterior below the carina and 1.0 mm posterior above the carina. The average absolute AP intra-fraction expansion was 2.5 ± 2.1 mm below the carina and 2.4 ± 4.2 mm above the carina (p=0.49). There was a significant increase in the intra-fraction expansion in the RL versus AP direction below (p=0.04), but not above (p=0.13) the carina. AP expansions ≥5 mm and ≥10 mm occurred in 10% and 0% of measurements below the carina, respectively, and 3% for both above the carina. There was no difference between inter- and intra-fraction expansion below the carina in the RL (p=0.09) and AP (p=0.37) directions, or above the carina in the RL (p=0.35) and AP (p=0.09) directions.
Inter-Fraction Displacement
The average, average absolute, range, and incidence of central point displacement greater than or equal to 5 mm and 10 mm is summarized in Table 3. The average inter-fraction RL displacement was 1.8 mm left below and 1.9 mm left above the carina; average AP displacement was 0.2 mm anterior below and 1.9 mm posterior above the carina. For inter-fraction displacement, average absolute displacement was less in the RL direction below the carina (3.2 ± 2.0 mm) compared to (4.2 ± 2.6 mm) above the carina (p=0.003), but there was no difference in AP direction below (2.8 ± 2.0 mm) versus above (3.9 ± 5.6 mm) the carina (p=0.18). There was no difference in the RL versus AP direction below (p=0.39) or above (p=0.10) the carina. The incidence of inter-fraction displacements ≥5 mm and ≥ 10 mm were 19% and 0% in RL below the carina, 35% and 3% in RL above the carina, 19% and 0% in AP below the carina, and 19% and 6% in AP above the carina.
Table 3.
Central Point Displacement Results Summary.
| Location to Carina | Average Displacement, mm (SD) | Average Absolute Displacement, mm (SD) | Range, mm | %≥5mm | %≥10mm | |
|---|---|---|---|---|---|---|
| Inter-fraction | ||||||
| RL | Below | 1.8 (3.4) | 3.2 (2.0) | −5.2 to 8.3 | 19% | 0% |
| Above | 1.9 (4.6) | 4.2 (2.6) | −6.6 to 11.2 | 35% | 3% | |
| AP | Below | −0.2 (3.4) | 2.8 (2.0) | −7.1 to 6.5 | 19% | 0% |
| Above | 1.9 (6.6) | 3.9 (5.6) | −5.7 to 30.7 | 19% | 6% | |
| Intra-fraction | ||||||
| RL | Below | 2.4 (5.7) | 4.1 (4.6) | −5.2 to 23.5 | 26% | 6% |
| Above | 1.9 (6.2) | 3.6 (5.3) | −18.8 to 26.2 | 13% | 6% | |
| AP | Below | 0.6 (3.3) | 2.6 (2.1) | −4.5 to 10.7 | 6% | 3% |
| Above | 1.1 (5.1) | 2.8 (4.4) | −4.2 to 25.5 | 3% | 3% | |
The inter- and intra-fraction mean, average of the absolute value, and range of esophageal central point displacement in the RL (right-left) and AP (anterior-posterior) directions, above and beyond the carina is reported. The percent of displacements greater than or equal to 5mm and 10mm is included. A negative value represents motion to the patient’s right for the RL direction and anterior for the AP directions. SD = Standard Deviation
Intra-Fraction Displacement
The average intra-fraction RL displacement was 2.4 mm left below the carina and 1.9 mm left above the carina; average AP displacement was 0.6 mm posterior below and 1.1 mm posterior above the carina. Average absolute displacement was 4.1 ± 4.6 mm below and 3.6 ± 5.3 mm above the carina in the RL direction (p=0.31) and 2.6 ± 2.1 mm below and 2.8 ± 4.4 mm above the carina in the AP direction (p=0.46). There was no statistical difference in the magnitude of the RL versus AP intra-fraction displacement above the carina (p=0.27) and a trend for increased motion in the RL direction below the carina (p=0.06). The incidence of intra-fraction displacements ≥ 5 mm and ≥ 10 mm were 26% and 6% in RL below the carina, 13% and 6% in RL above the carina, 6% and 3% in AP below the carina, and 3% and 3% in AP above the carina. There was no difference between inter- and intra-fraction displacement below the carina in the RL (p=0.17) and AP (p=0.46) directions, or above the carina in the AP (p=0.19) directions. Above the carina, there was greater inter-fraction RL displacement compared to intra-fraction RL displacement (p=0.05).
Combined Expansion and Displacement Results
There was no significant difference in central point displacement compared to expansion in any direction, above or below the carina. When both motion parameters (expansion and displacement) were considered together, the average RL motion was 1.8 ± 5.1 mm and the average AP motion was 0.6 ± 4.8 mm. The average esophageal motion in any direction was 1.2 ± 4.7 mm. Coverage of 95% of esophageal mobility would therefore require a 12 mm left, 8 mm right, 10 mm posterior, and 9 mm anterior margin. Overall inter-fraction motion ≥ 5 mm was 24% and ≥ 10 mm was 3%; intra-fraction motion ≥ 5 mm was 13% and ≥ 10 mm was 4%. The inter- and intra-fraction incidence of esophageal motion ≥ 20 mm in any direction was 1.6%.
Discussion
The average absolute inter- and intra-fraction esophageal displacement and expansion was 4.2 mm or less in RL and AP directions, above and below the carina. Our data indicates that 95% of measurements would be included using the asymmetric margins of 12 mm left, 8 mm right, 10 mm posterior, and 9 mm anterior. For example, in our institution, we would advocate a 24 mm leftward expansion from GTV to block edge, i.e., 12 mm for GTV to ITV, 5 mm from ITV to PTV, and 7 mm from PTV to block edge. The right and AP margins would be calculated in the same manner. Our results indicate that esophageal motion is related to directional shifts of the esophagus, not changes in esophageal diameter.
The measured esophageal motion in this study is similar to slightly larger than that reported in previous studies. Dieleman et al. found margins that would have incorporated 95% of RL motion were 5 mm proximally, 7 mm in the mid-esophagus, and 9 mm in distal esophagus. In the AP direction, the corresponding margins were 5 mm, 6 mm, and 8 mm, respectively (15). Our sample size and population distribution did not permit subset analysis of esophageal motion in relation to esophageal location. Yaremko et al. studied esophageal tumors of varying locations and found that 95% of tumors moved less than 8 mm radially, and the authors recommended using this margin if 4D CT was not available (21). As described in our methodology, the recorded data points represent the greatest motion above and below the carina for each patient, offering an explanation as to why our results may be slightly higher than those reported in earlier studies.
Our results suggest the use of asymmetric margins, as did Zhao et al., who studied GE junction tumors using respiratory-induced target motion with 4DCT. The authors recommended 10 mm left, 8 mm right, 11 mm anterior, and 6 mm posterior margins (22). We also found greater esophageal motion to the left, likely related to cardiac motion. In contrast, our results indicate an increased tendency for posterior motion, which may in part be due to inclusion of a wider range of tumor locations in this study than in Zhao’s study population, with only one-half of our patients having cancer in the distal esophagus.
Based on our results, we do not recommend differential margins based on CTV location in relation to the carina, although there was significantly increased inter-fraction expansion and displacement in the RL direction below, but not above, the carina. Multiple studies have demonstrated larger esophageal motion in the distal esophagus (12, 14–16), which is not surprising as the organ is fixed superiorly at the cricopharygeus muscles. The only study that consisted solely of esophageal cancer patients is by Patel et al (16). All of the patients in Dieleman’s study had non-small cell lung cancer (NSCLC) (15). Guerrero’s study contained one NSCLC patient and one GE junction cancer patient (14). Pan’s abstract refers to six patients with “intrathoracic malignancies” (12). Our hypothesis is that typical esophageal motion was disrupted by the esophageal tumor, resulting in greater motion above the carina. This stresses the importance of studying esophageal motion in esophageal cancer patients.
To our knowledge, this is the first manuscript to report inter- and intra-fraction esophageal motion, although it has been reported previously in abstract format (12, 17). Although a small population limits our study, a total of 31 image sets were obtained. This study supports the continued use of a 20–30 mm radial expansion from GTV to block edge as used in recent RTOG studies utilizing 3-dimensional conformal RT for treatment of esophageal malignancies. As IMRT is utilized more frequently in an effort to improve conformality and limit normal tissue toxicity, the question of margins becomes increasingly important. Additional studies with a larger esophageal cancer patient population should be performed to confirm these results.
Appendix
To test a hypothesis of equality when patients contribute unequal numbers of correlated observations, the following mathematical methodology was used. Let Uij and Vij be the jth matched observations from patient i for the two quantities to be compared. Let Xij = Uij − Vij be their differences. The null hypothesis is that of no difference, therefore the expectation E[Xij ] = 0 for all i, j in this case. Let
where p is the number of patients and n(i) is the number of correlated observations made on patient i. Under the null hypothesis E[T] = 0. Since the several patients are independent
and since E⌊Xij = 0⌋
Hence, an unbiased estimate of Var[ΣjXij] is
Thus, Var[T] may be estimated by summing independent components. Finally, the null hypothesis is tested using Z = T/√Var[T] which is approximately normally, N (0, 1), distributed.
Footnotes
Presented at 90th Annual Meeting of the American Radium Society, May 3–7, 2008, Laguna Nigel, California.
Conflict of Interest Notification.
No actual or potential conflicts of interest exist.
References
- 1.Herskovic A, Martz K, al-Sarraf M, et al. Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med. 1992;326:1593–1598. doi: 10.1056/NEJM199206113262403. [DOI] [PubMed] [Google Scholar]
- 2.Macdonald JS, Smalley SR, Benedetti J, et al. Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med. 2001;345:725–730. doi: 10.1056/NEJMoa010187. [DOI] [PubMed] [Google Scholar]
- 3.Minsky BD, Pajak TF, Ginsberg RJ, et al. INT 0123 (Radiation Therapy Oncology Group 94-05) phase III trial of combined-modality therapy for esophageal cancer: high-dose versus standard-dose radiation therapy. J Clin Oncol. 2002;20:1167–1174. doi: 10.1200/JCO.2002.20.5.1167. [DOI] [PubMed] [Google Scholar]
- 4.Tepper J, Krasna MJ, Niedzwiecki D, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol. 2008;26:1086–1092. doi: 10.1200/JCO.2007.12.9593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walsh TN, Noonan N, Hollywood D, et al. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med. 1996;335:462–467. doi: 10.1056/NEJM199608153350702. [DOI] [PubMed] [Google Scholar]
- 6.Lee HK, Vaporciyan AA, Cox JD, et al. Postoperative pulmonary complications after preoperative chemoradiation for esophageal carcinoma: correlation with pulmonary dose-volume histogram parameters. Int J Radiat Oncol Biol Phys. 2003;57:1317–1322. doi: 10.1016/s0360-3016(03)01373-7. [DOI] [PubMed] [Google Scholar]
- 7.Tucker SL, Liu HH, Wang S, et al. Dose-volume modeling of the risk of postoperative pulmonary complications among esophageal cancer patients treated with concurrent chemoradiotherapy followed by surgery. Int J Radiat Oncol Biol Phys. 2006;66:754–761. doi: 10.1016/j.ijrobp.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 8.Martel MK, Sahijdak WM, Ten Haken RK, et al. Fraction size and dose parameters related to the incidence of pericardial effusions. Int J Radiat Oncol Biol Phys. 1998;40:155–161. doi: 10.1016/s0360-3016(97)00584-1. [DOI] [PubMed] [Google Scholar]
- 9.Konski AA, Li T, Cohen SJ, et al. The Effect of Gender and Dose on the Development of Symptomatic Cardiac Toxicity after Chemoradiotherapy for Esophageal Carcinoma [Abstract] International Journal of Radiation Oncology*Biology*Physics. 2008;72:S254–S254. [Google Scholar]
- 10.Welch RW, Gray JE. Influence of respiration on recordings of lower esophageal sphincter pressure in humans. Gastroenterology. 1982;83:590–594. [PubMed] [Google Scholar]
- 11.Good E, Oral H, Lemola K, et al. Movement of the esophagus during left atrial catheter ablation for atrial fibrillation. J Am Coll Cardiol. 2005;46:2107–2110. doi: 10.1016/j.jacc.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 12.Pan CC, Kashani R, Hayman JA, et al. Intra- and inter-fraction esophagus motion in 3D-conformal radiotherapy: Implications for ICRU 62 definitions of internal target volume and planning organ at risk volume [Abstract] International Journal of Radiation Oncology Biology Physics. 2004;60:S580–S581. [Google Scholar]
- 13.Lorchel F, Dumas JL, Noel A, et al. Esophageal cancer: determination of internal target volume for conformal radiotherapy. Radiother Oncol. 2006;80:327–332. doi: 10.1016/j.radonc.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 14.Guerrero T, Zhang G, Huang TC, et al. Intrathoracic tumour motion estimation from CT imaging using the 3D optical flow method. Phys Med Biol. 2004;49:4147–4161. doi: 10.1088/0031-9155/49/17/022. [DOI] [PubMed] [Google Scholar]
- 15.Dieleman EM, Senan S, Vincent A, et al. Four-dimensional computed tomographic analysis of esophageal mobility during normal respiration. Int J Radiat Oncol Biol Phys. 2007;67:775–780. doi: 10.1016/j.ijrobp.2006.09.054. [DOI] [PubMed] [Google Scholar]
- 16.Patel AA, Wolfgang JA, Niemierko A, et al. Implications of respiratory motion as measured by four-dimensional computed tomography for radiation treatment planning of esophageal cancer. Int J Radiat Oncol Biol Phys. 2009;74:290–296. doi: 10.1016/j.ijrobp.2008.12.060. [DOI] [PubMed] [Google Scholar]
- 17.Sasidharan S, Allison R, Jenkins T, et al. Interfraction Esophagus Motion Study in Image Guided Radiation Therapy (IGRT) [Abstract] International Journal of Radiation Oncology Biology Physics. 2005;63:S91–S92. [Google Scholar]
- 18.Ma CM, Paskalev K. In-room CT techniques for image-guided radiation therapy. Med Dosim. 2006;31:30–39. doi: 10.1016/j.meddos.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 19.Greene FL American Joint Committee on Cancer., American Cancer Society. AJCC cancer staging handbook: from the AJCC cancer staging manual. 6. New York: Springer; 2002. [Google Scholar]
- 20.Kendall MG, Stuart A, Ord JK, et al. Kendall’s advanced theory of statistics. 6. New York: Halsted Press; 1994. [Google Scholar]
- 21.Yaremko BP, Guerrero TM, McAleer MF, et al. Determination of respiratory motion for distal esophagus cancer using four-dimensional computed tomography. Int J Radiat Oncol Biol Phys. 2008;70:145–153. doi: 10.1016/j.ijrobp.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 22.Zhao KL, Liao Z, Bucci MK, et al. Evaluation of respiratory-induced target motion for esophageal tumors at the gastroesophageal junction. Radiother Oncol. 2007;84:283–289. doi: 10.1016/j.radonc.2007.07.008. [DOI] [PubMed] [Google Scholar]