Abstract
Skin wound healing is a multi stage phenomenon that requires the activation, recruitment or activity of numerous cell types as keratinocytes, endothelial cells, fibroblast and inflammatory cells. Among the latter, macrophages appear to be central to this process. They colonize the wound at its very early stage and in addition to their protective immune role seem to organize the activity of other cell types at the following stages of the healing. Their benefit to this process is however controversial, as macrophages are described to promote the speed of healing but may also favour the fibrosis resulting from it in scars. Moreover wound healing defects are associated with abnormalities in the inflammatory phase. In this review, we summarise our knowledge on what are the Wound Associated Macrophages, and how they interact with the other cell types to control the reepithelialisation, angiogenesis and the extracellular matrix remodelling. We believe this knowledge may open new avenues for therapeutic intervention on skin wounds.
Keywords: Macrophage, skin wound, healing, inflammation, cytokines, growth factors, M1, alternatively activated
Introduction
Macrophages are mature myeloid cells, mostly derived from the differentiation of circulating monocytes after tissue infiltration. Far to be a homogeneous population, macrophages display a wide range of phenotypes and physiological properties depending on the cytokines inducing their maturation [1]. Moreover, macrophages are very plastic cells, able to switch from one functional sub-population to another depending on the stimulus received [2]. Another aspect of macrophage heterogeneity is the tissue specialisation of resident macrophages, as microglial cells in the brain, Kupffer cells in the liver or alveolar macrophages in the lung. However, it is still not clear if these resident macrophages are derived in steady state condition from circulating monocytes and if they are terminally differentiated cells [1]. After birth, macrophages are known to affect different stages of skin wound healing, modulating the function of the different cell types involved in this process. The benefit of inflammation and inflammatory cells in the wound healing is a matter of debate as in normal conditions it promotes wound closure but also the fibrosis associated with scar formation. Wound Associated Macrophages (WAM) have a central role in the control of wound inflammation. Here, we will present an overview of the main functions of WAM and their influence on the other major cell types present in the wound during the healing process and how modulating these processes might result in better wound healing.
Wound healing
In humans, and more widely in all mammalian species, the wound healing process can be subdivided in three consecutive and overlapping stages: inflammation, new tissue formation and remodelling [3]. The transition from one stage to another depends on the maturation and differentiation of the main cell populations involved, among which the keratinocytes, the fibroblasts and the macrophages.
Inflammation
The first event occurring after injury is the formation of a blood clot by activated platelets. The blood plug will be composed of various cell types including platelet, red and white blood cells. The initial plug is stabilised by fibrin fibres and will be a scaffold for the various infiltrating cells. The first inflammatory cells recruited are the neutrophils [4]. They infiltrate massively the wound during the first 24h post injury [5] attracted by the numerous inflammatory cytokines produced by the activated platelets, endothelial cells, as well as by the degradation products from pathogens. Neutrophils enter apoptosis soon after infiltrating the wound and the release of cytokines during this apoptotic process is an important component in macrophage recruitment. Macrophages infiltrate the wound massively 2 days post injury and exacerbate at this stage an intense phagocytic activity [6].
New tissue formation
The reepithelialisation process begins few hours after the wound formation. Keratinocytes from the wound edges migrate over the wound bed at the interface between the wound dermis and the fibrin clot. This migration is facilitated by the production of specific proteases such as the collagenase by the epidermal cells to degrade the extracellular matrix [7]. Activated fibroblasts also migrate to the wound bed and form, with the macrophages, the granulation tissue. A massive angiogenesis allowing the supply of oxygen and nutrients necessary for the healing process also occurs within this tissue [8]. Later, some of the fibroblasts differentiate into myofibroblasts. These contractile cells will help bridge the gap between the wound edges [9]. During the same time, growth factors produced by the granulation tissue will favour proliferation and differentiation of epithelial cells restoring the epithelial barrier integrity.
Remodelling
The last stage of the wound healing process consists in a gradual involution of the granulation tissue and dermal regeneration. This step is associated with the apoptosis of myofibroblasts, endothelial cells and macrophages. The remaining tissue is therefore composed mostly of extracellular matrix proteins, essentially collagen type III that will be remodelled by the metalloproteinase produced by the epidermal cells, endothelial cells, fibroblasts and the macrophages remaining in the scar and be replaced by collagen type I [8].
Macrophages and wound healing
Wound macrophage phenotypes
Macrophages used to be divided in several subpopulations depending of the way they had been activated, their cell surface markers or their functionality. [1, 10,11]. Schematically, macrophages activated by microbial agents and cytokines like Interferon gamma (IFNγ) are classified as M1 macrophages. These macrophages produce an important level of Nitric Oxide (NO) and pro inflammatory cytokines such as Tumor Necrosis Factor alfa (TNFα), IL-1β, IL-6, or IL-12, and overexpress MHC class II molecules. They bear microbicidal and antitumoral properties. M2 macrophages are a much more heterogeneous population composed of all macrophages that do not correspond to M1 characteristics [12]. M2 macrophages could be divided in 3 sub-populations. The alternatively activated macrophages or M2a, that promote a Th2 type of inflammation resulting in increased IgE as observed in allergy and parasite immunity, the M2b macrophages, that promote Th2 inflammation and bear some immunoregulation properties, and the deactivated macrophages or M2c, able to control the inflammation and implicated in tissue remodelling [12]. In another classification, M1 macrophages are considered as the classically activated macrophages as compared to the alternatively activated macrophages. The best described alternative activation consists in the stimulation of the IL-4R by IL-4 and IL-13 that induces pro Th2 macrophages [13]. Of course, all these sub populations should not be considered as distinct populations in vivo but more as different stages of a continuum of activation and differentiation of macrophage populations [14]. The phenotype of skin wound infiltrating macrophages is not yet fully characterised, but it already appears that it changes during the healing process suggesting that macrophages have different roles in the diverse phases of skin repair [15, 16].
Several reviews refer to wound macrophages as the IL4 alternatively activated macrophages because of numerous markers of tissues remodelling, such as YM1, Resistin Like Molecule Alfa (RELMα), Insulin Growth Factor 1 (IGF1), factor XIII-A or arginase that are expressed after in vitro activation of macrophages with IL4. [13, 17-20]. Recent work on aseptic wounds using an implantable sponge model described wound macrophages as cells bearing both classical activation markers, like TNFα expression, and alternatively activated markers like the mannose receptor [15]. The authors also described the evolution of the macrophage phenotype. Day 1 macrophages produced more TNFα and IL6 and less Tumor Growth Factor beta (TGFβ) compared to day 7 macrophages suggesting a transition from an inflammatory to an immunoregulatory or tissue remodelling state. However, it is important to consider that neither IL4 nor IL13 were detectable in this model, perhaps because of the aseptic experimental condition. However, it is not clear to what extent the bacterial colonization of the wound would modify Wound Associated Macrophage phenotypes and healing functions, as it is clear that parasitic and bacterial component are major macrophage activators [13].
Macrophage importance in wound healing
In order to show the implication of macrophages in the control of wound healing, several studies have analysed skin wound healing upon macrophage depletion (Table 1). The first attempt consisted in corticosteroids associated with anti macrophage sera to deplete macrophages in wounded guinea pigs. This treatment resulted in a delayed infiltration of the wound by fibroblasts and decreased fibrosis [6]. These results are in accordance with observations that fetal wounds heal without fibrosis and are not infiltrated by macrophages. In a model of PU.1 null mice where animals lacked macrophages, mast cells and functional neutrophils due to defective myelopoiesis, wounds performed on newborns additionally treated with antibiotic healed at the same speed as wild types, but without scar formation, suggesting that inflammatory cells are not needed for wound closure [21]. However, several recent models of specific inducible macrophage depletion, based on genetically modified mice resulted in detrimental effect of pre-injury depletion of macrophages [16, 22, 23]. Mice depleted before injury typically show a defect in re-epithelisation, granulation tissue formation, angiogenesis, wound cytokine production and myofibroblast associated wound contraction. Recently, the effect of a post-injury depletion of the WAM has also been investigated. Macrophage depletion during the granulation tissue formation, about 3 days after injury, is associated with vascularisation defect, delay in wound closure as well as in granulation tissue maturation [16]. Finally, in their study, Lucas et al did not find any morphological or biological differences between mice that were or were not depleted 9 days after injury suggesting no further implication of macrophages at later stages.
Table 1.
Impact of macrophages depletion strategy on wound healing
| Depletion stage | Depletion process | Wound closure | Gr T fromation/Angiogenesis | Collagen/fibrosis/αSMA | Ref |
|---|---|---|---|---|---|
| Early | Macrophage antiserum | ↓ | ND | ↓ | [6] |
| Early | CD11b DTR | ↓ | ↓ | ↓ | [22] |
| Early | lysM-Cre DTR | ↓ | ↓ | ↓ | [23] |
| Early | lysM-Cre DTR | ↓ | ↓ | ↓ | [16] |
| Middle | lysM-Cre DTR | ↓ | ↓ | ND | [16] |
| Late | lysM-Cre DTR | = | = | = | [16] |
Gr T: Granulation tissue
During the healing process numerous cytokines and growth factors are produced by the various cell types present in the wound or at the wound edge [24]. The level of production of the different cytokines depends on the regulation of the cross talk between the major cell populations in the wound: epithelial cells, endothelial cells, fibroblasts and inflammatory cells. However, the literature clearly lacks in vivo characterisation of the cytokine production kinetics by the various cell types during skin wound healing. Most of our current knowledge concerning the ability of a cell population to produce or to respond to a specific cytokine is based on in vitro studies.
Cross talk with keratinocyte
Injured and inflamed keratinocytes produce several cytokines allowing the recruitment and activation of the WAM, including chemokines, interleukins and growth factors [25, 26]. On the other hand, the ability of immune cells to produce factors able to regulate keratinocyte growth in vitro has been described since 1988 [27]. Interestingly, conditioned medium from coculture of macrophages and allogenic T cells were much more efficient in inducing keratinocyte proliferation compared to conditioned medium from macrophages alone. However, the direct implication of WAM in producing cytokines or growth factors to influence directly or indirectly keratinocyte migration and proliferation is not clear in vivo. Several cytokines and growth factors, that can be produced by macrophages, have been associated with reepithelialisation, mostly in vitro. Among the Epithelial growth Factor family (EGF), the main members involved in wound healing are EGF, TGFα and Heparin Bound EGF (EGF-HB) [28-32]. The activation of the EGF Receptor (EGFR) on keratinocytes promotes cell migration and proliferation. Although, only TGFα and EGF-HB have been described to be produced by macrophages in vitro, their production by WAM in vivo is more enigmatic [33, 34]. TGFα has been detected in macrophages collected from sub epidermal wound cylinders 6 days after implantation in mice [35]. However, no significant wound healing abnormalities were observed in TGFα-/-mice [36]. In addition, all EGFR ligands are synthetised as membrane-anchored forms, which can be released as a soluble form after proteolysis by MMP [37]. Therefore, another possible role for WAM might be the regulation of EGF family release by the production of MMPs. Other cytokines as IL-6, IL1 and TNF-α produced by macrophages are also associated with reepithelisation. Even if the secretion of these cytokines by WAM has not been clearly demonstrated yet, the ability of macrophages activated by the inflammatory cytokine IFNγ and/or bacterial products via Toll Like Receptor 4 (TLR4) to produce IL-6, IL1β and TNFα makes this hypothesis probable [13]. The implication of IL-1 and IL-6 in the reepithelialisation is indirect and is mediated by other cell types present in the wound, at least the fibroblast [38, 39]. On the contrary, TNFα directly stimulates transcription of genes associated with numerous cell functions including inflammation, mobility, cell division and survival in keratinocytes [25]. Of note, in a model of sponge implanted under aseptic conditions in the dermis, macrophages extracted on day 1 produced more TNFα compared to day 7 [15]. Finally, the other cytokine known to be massively produced by macrophages, and highly implicated in reepithelialisation, is TGFβ, although its effect on keratinocyte proliferation and migration remains controversial [36, 40-43]. Cultured WAM extracted from implanted sponges start producing TGFβ from the very first day of the wound [15].
Influence on fibroblasts and myofibroblast
Fibroblasts begin to infiltrate the wound during the first steps of granulation tissue formation. Fibroblasts are involved in several processes of the wound healing. They contribute to the granulation tissue formation, produce the cytokines that favour keratinocyte proliferation and migration [44], and finally differentiate in myofibroblasts to promote wound closure. Several molecules, such as PDGF-bb, TNFα, IL-1 or IL-6, produced by activated macrophages are able to induce in vitro the production of proreepithelialisation molecules by fibroblasts such as KGF [45-48]. Interestingly, the effect of most of these molecules is dependent on the presence of serum in the fibroblast culture media, indicating that the stimulation resulting in their production is a cooperative process [49]. Mori et al demonstrated nicely that macrophage secretion of PDGF-bb isoform induced the production of osteopontin by fibroblasts [50]. The inhibition of osteopontin was associated with lower scar fibrosis [50]. Finally, the molecule produced by macrophages that has been the most extensively studied for its actions on wound fibroblasts is TGFβ. It is a family of three cytokines, TGFβ1, 2 and 3, produced by several cell types during the healing process, including platelets and epidermal cells, but the main and sustained source of production are the WAM [16, 51]. All TGFβ family members are secreted coupled to a “latent complex” which has the ability to bind the Extra Cellular Matrix (ECM). The latent forms have to be activated via various mechanisms to release the mature TGFβ, including proteolysis by MMPs known to be extensively secreted by macrophages as reviewed by Annes et al [52]. While TGFβ1 and 2 promote the inflammation within the wound and are associated with scar formation, TGFβ3 is associated with scar free wound healing [53]. However, the expression of TGFβ3 in adult wound is rare while the two other forms are highly expressed [53]. TGFβ1 is chemotactic for fibroblasts [54, 55]. It induces the production of several growths factors by fibroblasts, including Connective Tissue Growth Factor (CTGF) [56], that results in their proliferation by an autocrine loop [57]. But the main action of TGFβ on fibroblast is to promote their differentiation into myofibroblast and to favour collagen production [58]. The secretion of TGFβ and MMP by the macrophages is critical in the control of the ECM composition. Accordingly, macrophage depletion is associated with a defect of Alpha Smouth Muscle Actin (αSMA) positive cell in the granulation tissue [23]. However, it is estimated that 30 to 50% of the granulation tissue αSMA+ cells do not derive from fibroblasts, but more likely from bone marrow derived fibrocytes or mesenchymal stem cells [59-61]. The implication of macrophage produced cytokines in the recruitment, activation and differentiation of these marrow derived fibrocytes in the wound bed is unknown and has to be further investigated.
Cross talk with endothelial cell
Neo-angiogenesis in the granulation tissue is an important process allowing the supply of nutrients necessary for the healing process. The main angiogenic factor in the wound is the Vascular Endothelial Growth Factor (VEGF) and its reduced expression results in a wound healing defect [62]. VEGF promotes wound vascularisation by multiple mechanisms targeting directly or indirectly endothelial cells as reviewed by Eming et al [63]. VEGF promotes endothelial cell and precursor recruitment [64] but it also acts as a mitogen and survival factor on the endothelial cells [65-67]. The increase of VEGF production in the wound is described in migratory keratinocytes and in macrophages infiltrating the granulation tissue [62]. The keratinocyte production of VEGF is indirectly promoted by macrophages as well through the secretion of cytokines as TNFα or TGFβ [68]. CTGF produced by fibroblasts [56], also favours endothelial cell proliferation and new vessel formation [69, 70]. VEGF family members, mostly VEGF-C and VEGF -D, have also been recognized for their ability to modulate lymphangiogenesis [71]. Decreased macrophage numbers and activation has been associated with reduced lymphatic vessel formation in diabetic mouse wounds [72]. It is important to note that double positive F4/80/Lyve1 cells have been described to be integrated in lymphatic vessels in several models of neolymphangiogenesis suggesting that macrophages could be directly implicated in their formation [72, 73].
The other main pro-antigenic molecule during the wound healing is the Placental Growth Factor (PlGF), a member of the VEGF family [67] [74]. PlGF expression is induced in vitro by TGFα and TGFβ, and is produced during the angiogenic stage of the healing process [75]. The effects of PlGF are similar to those of VEGF, promoting monocytes and endothelial precursor cell migration [76] and favouring endothelial cell survival [77]. PlGF stimulates also the secretion of VEGF by the monocyte/macrophages [78]. Interestingly, even if PlGF is described to have chemotactic properties by his own on VEGFR1+ expressing cells, the synergy between PlGF and VEGF is important in angiogenesis [79]: i) VEGFR1 homodimers may be a decoy receptor. Binding of PlGF homodimer to VEGFR1 homodimer make more VEGF available to bind to activated VEGFR2. ii) VEGF/PlGF heterodimers bind to VEGFR1/VEGFR2 heterodimer and induce more potent angiogenic signals iii) binding of PlGF homodimers to VEGFR1 homodimers favours VEGFR2 homodimer phosphorylation [80]. Overall, PlGF seems to potentiate the effect of VEGF in wound angiogenesis. These results altogether point to the important role of macrophages in coordinating the angiogenic signal during wound healing.
Macrophages and defective wound healing
Despite their heterogeneous aetiology, most chronic wounds have in common a defect in the progression from the inflammatory to the tissue formation stage. Loots et al reported increased infiltration of chronic and diabetic wounds by WAM compared to control acute wounds. In addition they observed higher amounts of ECM in the wound edge [81]. Similarly, in diabetic db/db mice, wounds are characterising by a prolonged expression of inflammatory cytokines and larger infiltration and persistence of the WAM [82]. However, these cells seem to have altered sensitivity towards exogenous signals such as VEGF or IGF1 [83, 84] as well as altered ability to release cytokine [85]. Several studies have targeted macrophages, by different strategies in order to improve defective wound healing (Table 2). In the obese diabetic db/db mouse model, the injection of peritoneal macrophages activated by IL-1β at the wound site was associated with an increased production of prolymphangiogenic molecules such as VEGF-C, resulting in improved lymphangiogenesis and wound healing [72]. Local application of GM-CSF is associated with better healing both in human and mouse pathological wounds in a clinical setting. In Streptozotocin induced diabetic mice, GM-CSF is associated with a stronger infiltration of the wound by macrophages, increased angiogenesis and a better healing, while no effect was observed in normal wound healing [86] [87]. Similarly, in a pilot study in humans, GM-CSF treatment improves chronic vascular ulcers, probably by promoting the secretion of VEGF by macrophages [88]. With a similar strategy, Deiters et al injected Macrophage-Activating Lipopeptide-2 (MALP-2) in wounds on obese diabetic db/db mice. MALP2 induced the transcription of several genes associated with wound healing, including GMCSF and IL-1 [89] and resulted in increased infiltration by WAM and more rapid wound closure. In opposition to these activating approaches, Goren et al used a depleting strategy based on the systemic injection of a neutralizing anti-TNFα in ob/ob mice [90]. The treatment resulted in a systemic and local depletion of macrophages that was associated with a faster healing. Taken together, these results sustain the hypothesis that in chronic or diabetic wounds different strategies that might affect macrophage phenotype might modify the healing.
Table 2.
Targeting of macrophages to control healing of pathological wound
| Molecules /cells | Delivery | Stage | Pathological model | Wound model | Effect on MΘ | Effect on healing | Ref |
|---|---|---|---|---|---|---|---|
| MALP-2 | local | Early to middle | Diabetic C57BI6 db/db | Acute | ↑ recruitment | ↑ | [89] |
| GM-CSF | local | NA | Human CVLU | Chronic | ↑ VEGF production | ↑ | [88] |
| Anti TNFα | Systemic | Early to late | Diabetic ob/ob | Acute | ↓ recruitment | ↑ | [90] |
| IL1β activated db/db MΘ | Local | Early | Diabetic C57BI6 db/db | Acute | ↑ VEGFC/VEGFR3 transcription | ↑ | [72] |
| GM-CSF | local | Early | Strpz induce diabetic mice | Acute | ↑ Recruitment | ↑ | [86] |
CVLU: Chronic Veinous Leg Ulcer. Strpz : streptozotocin
Conclusions
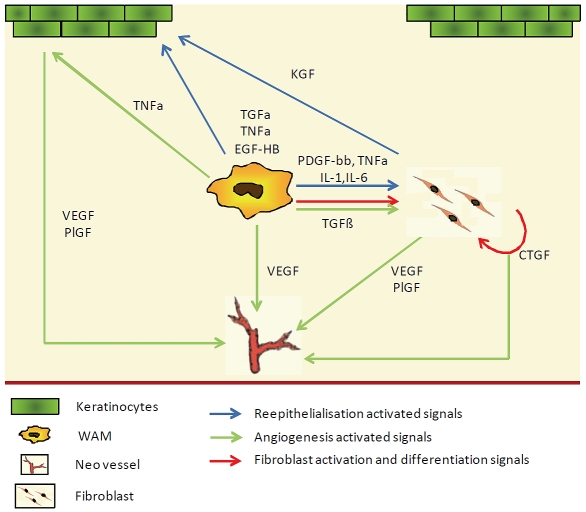
Our current knowledge points to macrophages as key players in skin wound healing after birth. Healing is a complex and evolving process, and because of their plasticity, WAM progress with the wound, adapting their cytokine expression profile [15]. Because of this plasticity and of their central position, WAM seem to be the ideal target for clinical interventions in chronic wounds, to accelerate closure or to attenuate fibrosis (Figure 1). For this purpose, there is still a need to further characterise this population. It seems obvious that, similar to other inflammation models, WAM are essentially composed of infiltrating blood monocytes that change from an inflammatory phenotype to a repair one [15, 91, 92]. It is not clear if the multiple functions of WAM are exclusive to a unique macrophage population or fulfilled by specialised sub populations at different time points? Should the future therapeutic strategies consist in the control of the WAM polarisation or in the specific recruitment or depletion of sub populations? These strategies will also have to define the appropriate timing for their effectiveness as WAM bear different functions during the healing time course [16].
Figure 1.
Direct and indirect control of reepithelialisation, angiogenesis and fibroblast activation by macrophages.
Acknowledgments
This work was supported by the Ramaciotti foundation.
References
- 1.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 2.Stout RD, Suttles J. Functional plasticity of macrophages: reversible adaptation to changing microenvironments. J Leukoc Biol. 2004;76:509–513. doi: 10.1189/jlb.0504272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gurtner GC, Werner S, Barrandon Y, Longaker MT. Wound repair and regeneration. Nature. 2008;453:314–321. doi: 10.1038/nature07039. [DOI] [PubMed] [Google Scholar]
- 4.Ross R, Odland G. Human wound repair. II. Inflammatory cells, epithelial-mesenchymal interrelations, and fibrogenesis. J Cell Biol. 1968;39:152–168. doi: 10.1083/jcb.39.1.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim MH, Liu W, Borjesson DL, Curry FR, Miller LS, Cheung AL, Liu FT, Isseroff RR, Simon SI. Dynamics of neutrophil infiltration during cutaneous wound healing and infection using fluorescence imaging. J Invest Dermatol. 2008;128:1812–1820. doi: 10.1038/sj.jid.5701223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leibovich SJ, Ross R. The role of the macrophage in wound repair. A study with hydrocortisone and antimacrophage serum. Am J Pathol. 1975;78:71–100. [PMC free article] [PubMed] [Google Scholar]
- 7.Pilcher BK, Dumin JA, Sudbeck BD, Krane SM, Welgus HG, Parks WC. The activity of collagenase-1 is required for keratinocyte migration on a type I collagen matrix. J Cell Biol. 1997;137:1445–1457. doi: 10.1083/jcb.137.6.1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singer AJ, Clark RA. Cutaneous wound healing. N Engl J Med. 1999;341:738–746. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 9.Gabbiani G. The myofibroblast in wound healing and fibrocontractive diseases. J Pathol. 2003;200:500–503. doi: 10.1002/path.1427. [DOI] [PubMed] [Google Scholar]
- 10.Gordon S. Alternative activation of macrophages. Nat Rev Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 11.Mantovani A, Sozzani S, Locati M, Allavena P, Sica A. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol. 2002;23:549–555. doi: 10.1016/s1471-4906(02)02302-5. [DOI] [PubMed] [Google Scholar]
- 12.Mantovani A, Sica A, Sozzani S, Allavena P, Vecchi A, Locati M. The chemokine system in diverse forms of macrophage activation and polarization. Trends Immunol. 2004;25:677–686. doi: 10.1016/j.it.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 13.Martinez FO, Helming L, Gordon S. Alternative activation of macrophages: an immunologic functional perspective. Annu Rev Immunol. 2009;27:451–483. doi: 10.1146/annurev.immunol.021908.132532. [DOI] [PubMed] [Google Scholar]
- 14.Stout RD, Jiang C, Matta B, Tietzel I, Watkins SK, Suttles J. Macrophages sequentially change their functional phenotype in response to changes in microenvironmental influences. J Immunol. 2005;175:342–349. doi: 10.4049/jimmunol.175.1.342. [DOI] [PubMed] [Google Scholar]
- 15.Daley JM, Brancato SK, Thomay AA, Reichner JS, Albina JE. The phenotype of murine wound macrophages. J Leukoc Biol. 2010;87:59–67. doi: 10.1189/jlb.0409236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucas T, Waisman A, Ranjan R, Roes J, Krieg T, Muller W, Roers A, Eming SA. Differential Roles of Macrophages in Diverse Phases of Skin Repair. J Immunol. 2009 doi: 10.4049/jimmunol.0903356. [DOI] [PubMed] [Google Scholar]
- 17.Mosser DM, Edwards JP. Exploring the full spectrum of macrophage activation. Nat Rev Immunol. 2008;8:958–969. doi: 10.1038/nri2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Raes G, Noel W, Beschin A, Brys L, de Baetselier P, Hassanzadeh GH. FIZZ1 and Ym as tools to discriminate between differentially activated macrophages. Dev Immunol. 2002;9:151–159. doi: 10.1080/1044667031000137629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wynes MW, Riches DW. Induction of macrophage insulin-like growth factor-I expression by the Th2 cytokines IL-4 and IL-13. J Immunol. 2003;171:3550–3559. doi: 10.4049/jimmunol.171.7.3550. [DOI] [PubMed] [Google Scholar]
- 20.Torocsik D, Bardos H, Nagy L, Adany R. Identification of factor XIII-A as a marker of alternative macrophage activation. Cell Mol Life Sci. 2005;62:2132–2139. doi: 10.1007/s00018-005-5242-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Martin P, D'Souza D, Martin J, Grose R, Cooper L, Maki R, McKercher SR. Wound healing in the PU.1 null mouse–tissue repair is not dependent on inflammatory cells. Curr Biol. 2003;13:1122–1128. doi: 10.1016/s0960-9822(03)00396-8. [DOI] [PubMed] [Google Scholar]
- 22.Mirza R, DiPietro LA, Koh TJ. Selective and specific macrophage ablation is detrimental to wound healing in mice. Am J Pathol. 2009;175:2454–2462. doi: 10.2353/ajpath.2009.090248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goren I, Allmann N, Yogev N, Schurmann C, Linke A, Holdener M, Waisman A, Pfeilschifter J, Frank S. A transgenic mouse model of inducible macrophage depletion: effects of diphtheria toxin-driven lysozyme M-specific cell lineage ablation on wound inflammatory, angiogenic, and contractive processes. Am J Pathol. 2009;175:132–147. doi: 10.2353/ajpath.2009.081002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen L, Tredget EE, Wu PY, Wu Y. Paracrine factors of mesenchymal stem cells recruit macrophages and endothelial lineage cells and enhance wound healing. PLoS One. 2008;3:e1886. doi: 10.1371/journal.pone.0001886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Banno T, Gazel A, Blumenberg M. Effects of tumor necrosis factor-alpha (TNF alpha) in epidermal keratinocytes revealed using global transcriptional profiling. J Biol Chem. 2004;279:32633–32642. doi: 10.1074/jbc.M400642200. [DOI] [PubMed] [Google Scholar]
- 26.McKay IA, Leigh IM. Epidermal cytokines and their roles in cutaneous wound healing. Br J Dermatol. 1991;124:513–518. doi: 10.1111/j.1365-2133.1991.tb04942.x. [DOI] [PubMed] [Google Scholar]
- 27.Hancock GE, Kaplan G, Cohn ZA. Keratinocyte growth regulation by the products of immune cells. J Exp Med. 1988;168:1395–1402. doi: 10.1084/jem.168.4.1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rheinwald JG, Green H. Epidermal growth factor and the multiplication of cultured human epidermal keratinocytes. Nature. 1977;265:421–424. doi: 10.1038/265421a0. [DOI] [PubMed] [Google Scholar]
- 29.Li Y, Fan J, Chen M, Li W, Woodley DT. Transforming growth factor-alpha: a major human serum factor that promotes human keratinocyte migration. J Invest Dermatol. 2006;126:2096–2105. doi: 10.1038/sj.jid.5700350. [DOI] [PubMed] [Google Scholar]
- 30.Schultz G, Rotatori DS, Clark W. EGF and TGF -alpha in wound healing and repair. J Cell Biochem. 1991;45:346–352. doi: 10.1002/jcb.240450407. [DOI] [PubMed] [Google Scholar]
- 31.Marikovsky M, Vogt P, Eriksson E, Rubin JS, Taylor WG, Joachim S, Klagsbrun M. Wound fluid -derived heparin-binding EGF-like growth factor (HB-EGF) is synergistic with insulin-like growth factor-I for Balb/MK keratinocyte proliferation. J Invest Dermatol. 1996;106:616–621. doi: 10.1111/1523-1747.ep12345413. [DOI] [PubMed] [Google Scholar]
- 32.Shirakata Y, Kimura R, Nanba D, Iwamoto R, Tokumaru S, Morimoto C, Yokota K, Nakamura M, Sayama K, Mekada E, Higashiyama S, Hashimoto K. Heparin-binding EGF-like growth factor accelerates keratinocyte migration and skin wound healing. J Cell Sci. 2005;118:2363–2370. doi: 10.1242/jcs.02346. [DOI] [PubMed] [Google Scholar]
- 33.Edwards JP, Zhang X, Mosser DM. The expression of heparin-binding epidermal growth factor-like growth factor by regulatory macrophages. J Immunol. 2009;182:1929–1939. doi: 10.4049/jimmunol.0802703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hallbeck AL, Walz TM, Wasteson A. Interleukin-6 enhances transforming growth factor-alpha mRNA expression in macrophage-like human monocytoid (U-937-1) cells. Biosci Rep. 2001;21:325–339. doi: 10.1023/a:1013238300100. [DOI] [PubMed] [Google Scholar]
- 35.Rappolee DA, Mark D, Banda MJ, Werb Z. Wound macrophages express TGF-alpha and other growth factors in vivo: analysis by mRNA phenotyping. Science. 1988;241:708–712. doi: 10.1126/science.3041594. [DOI] [PubMed] [Google Scholar]
- 36.Grose R, Werner S. Wound-healing studies in transgenic and knockout mice. Mol Biotechnol. 2004;28:147–166. doi: 10.1385/MB:28:2:147. [DOI] [PubMed] [Google Scholar]
- 37.Massague J, Pandiella A. Membrane-anchored growth factors. Annu Rev Biochem. 1993;62:515–541. doi: 10.1146/annurev.bi.62.070193.002503. [DOI] [PubMed] [Google Scholar]
- 38.Gallucci RM, Sloan DK, Heck JM, Murray AR, O'Dell SJ. Interleukin 6 indirectly induces keratinocyte migration. J Invest Dermatol. 2004;122:764–772. doi: 10.1111/j.0022-202X.2004.22323.x. [DOI] [PubMed] [Google Scholar]
- 39.Chedid M, Rubin JS, Csaky KG, Aaronson SA. Regulation of keratinocyte growth factor gene expression by interleukin 1. J Biol Chem. 1994;269:10753–10757. [PubMed] [Google Scholar]
- 40.Ashcroft GS, Yang X, Glick AB, Weinstein M, Letterio JL, Mizel DE, Anzano M, Greenwell-Wild T, Wahl SM, Deng C, Roberts AB. Mice lacking Smad3 show accelerated wound healing and an impaired local inflammatory response. Nat Cell Biol. 1999;1:260–266. doi: 10.1038/12971. [DOI] [PubMed] [Google Scholar]
- 41.Li AG, Wang D, Feng XH, Wang XJ. Latent TGFbeta1 overexpression in keratinocytes results in a severe psoriasis-like skin disorder. EMBO J. 2004;23:1770–1781. doi: 10.1038/sj.emboj.7600183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sellheyer K, Bickenbach JR, Rothnagel JA, Bund-man D, Longley MA, Krieg T, Roche NS, Roberts AB, Roop DR. Inhibition of skin development by overexpression of transforming growth factor beta 1 in the epidermis of transgenic mice. Proc Natl Acad Sci U S A. 1993;90:5237–5241. doi: 10.1073/pnas.90.11.5237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Werner S, Grose R. Regulation of wound healing by growth factors and cytokines. Physiol Rev. 2003;83:835–870. doi: 10.1152/physrev.2003.83.3.835. [DOI] [PubMed] [Google Scholar]
- 44.Werner S, Krieg T, Smola H. Keratinocytefibroblast interactions in wound healing. J Invest Dermatol. 2007;127:998–1008. doi: 10.1038/sj.jid.5700786. [DOI] [PubMed] [Google Scholar]
- 45.Hubner G, Brauchle M, Smola H, Madlener M, Fassler R, Werner S. Differential regulation of pro-inflammatory cytokines during wound healing in normal and glucocorticoid-treated mice. Cytokine. 1996;8:548–556. doi: 10.1006/cyto.1996.0074. [DOI] [PubMed] [Google Scholar]
- 46.Brauchle M, Angermeyer K, Hubner G, Werner S. Large induction of keratinocyte growth factor expression by serum growth factors and pro-inflammatory cytokines in cultured fibroblasts. Oncogene. 1994;9:3199–3204. [PubMed] [Google Scholar]
- 47.Takehara K. Growth regulation of skin fibroblasts. J Dermatol Sci. 2000;24(Suppl 1):S70–77. doi: 10.1016/s0923-1811(00)00144-4. [DOI] [PubMed] [Google Scholar]
- 48.Beer HD, Florence C, Dammeier J, McGuire L, Werner S, Duan DR. Mouse fibroblast growth factor 10: cDNA cloning, protein characterization, and regulation of mRNA expression. Oncogene. 1997;15:2211–2218. doi: 10.1038/sj.onc.1201383. [DOI] [PubMed] [Google Scholar]
- 49.Wang X, Waldeck H, Kao WJ. The effects of TGF-alpha, IL-1beta and PDGF on fibroblast adhesion to ECM-derived matrix and KGF gene expression. Biomaterials. 31:2542–2548. doi: 10.1016/j.biomaterials.2009.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mori R, Shaw TJ, Martin P. Molecular mechanisms linking wound inflammation and fibrosis: knockdown of osteopontin leads to rapid repair and reduced scarring. J Exp Med. 2008;205:43–51. doi: 10.1084/jem.20071412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Stramer BM, Mori R, Martin P. The inflammation-fibrosis link? A Jekyll and Hyde role for blood cells during wound repair. J Invest Dermatol. 2007;127:1009–1017. doi: 10.1038/sj.jid.5700811. [DOI] [PubMed] [Google Scholar]
- 52.Annes JP, Munger JS, Rifkin DB. Making sense of latent TGFbeta activation. J Cell Sci. 2003;116:217–224. doi: 10.1242/jcs.00229. [DOI] [PubMed] [Google Scholar]
- 53.Occleston NL, Fairlamb D, Hutchison J, O'Kane S, Ferguson MW. Avotermin for the improvement of scar appearance: a new pharmaceutical in a new therapeutic area. Expert Opin Investig Drugs. 2009;18:1231–1239. doi: 10.1517/13543780903130594. [DOI] [PubMed] [Google Scholar]
- 54.Postlethwaite AE, Keski-Oja J, Moses HL, Kang AH. Stimulation of the chemotactic migration of human fibroblasts by transforming growth factor beta. J Exp Med. 1987;165:251–256. doi: 10.1084/jem.165.1.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Border WA, Noble NA. Transforming growth factor beta in tissue fibrosis. N Engl J Med. 1994;331:1286–1292. doi: 10.1056/NEJM199411103311907. [DOI] [PubMed] [Google Scholar]
- 56.Grotendorst GR, Okochi H, Hayashi N. A novel transforming growth factor beta response element controls the expression of the connective tissue growth factor gene. Cell Growth Differ. 1996;7:469–480. [PubMed] [Google Scholar]
- 57.Igarashi A, Okochi H, Bradham DM, Grotendorst GR. Regulation of connective tissue growth factor gene expression in human skin fibroblasts and during wound repair. Mol Biol Cell. 1993;4:637–645. doi: 10.1091/mbc.4.6.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Desmouliere A, Geinoz A, Gabbiani F, Gabbiani G. Transforming growth factor-beta 1 induces alpha-smooth muscle actin expression in granulation tissue myofibroblasts and in quiescent and growing cultured fibroblasts. J Cell Biol. 1993;122:103–111. doi: 10.1083/jcb.122.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Direkze NC, Forbes SJ, Brittan M, Hunt T, Jeffery R, Preston SL, Poulsom R, Hodivala-Dilke K, Alison MR, Wright NA. Multiple organ engraftment by bone-marrow-derived myofibroblasts and fibroblasts in bone-marrow-transplanted mice. Stem Cells. 2003;21:514–520. doi: 10.1634/stemcells.21-5-514. [DOI] [PubMed] [Google Scholar]
- 60.Ishii G, Sangai T, Sugiyama K, Ito T, Hasebe T, Endoh Y, Magae J, Ochiai A. In vivo characterization of bone marrow-derived fibroblasts recruited into fibrotic lesions. Stem Cells. 2005;23:699–706. doi: 10.1634/stemcells.2004-0183. [DOI] [PubMed] [Google Scholar]
- 61.Herdrich BJ, Lind RC, Liechty KW. Multipotent adult progenitor cells: their role in wound healing and the treatment of dermal wounds. Cytotherapy. 2008;10:543–550. doi: 10.1080/14653240802345820. [DOI] [PubMed] [Google Scholar]
- 62.Brown LF, Yeo KT, Berse B, Yeo TK, Senger DR, Dvorak HF, van de Water L. Expression of vascular permeability factor (vascular endothelial growth factor) by epidermal keratinocytes during wound healing. J Exp Med. 1992;176:1375–1379. doi: 10.1084/jem.176.5.1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eming SA, Brachvogel B, Odorisio T, Koch M. Regulation of angiogenesis: wound healing as a model. Prog Histochem Cytochem. 2007;42:115–170. doi: 10.1016/j.proghi.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 64.Li B, Sharpe EE, Maupin AB, Teleron AA, Pyle AL, Carmeliet P, Young PP. VEGF and PlGF promote adult vasculogenesis by enhancing EPC recruitment and vessel formation at the site of tumor neovascularization. FASEB J. 2006;20:1495–1497. doi: 10.1096/fj.05-5137fje. [DOI] [PubMed] [Google Scholar]
- 65.Dvorak HF, Brown LF, Detmar M, Dvorak AM. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol. 1995;146:1029–1039. [PMC free article] [PubMed] [Google Scholar]
- 66.Gerber HP, Dixit V, Ferrara N. Vascular endothelial growth factor induces expression of the antiapoptotic proteins Bcl-2 and A1 in vascular endothelial cells. J Biol Chem. 1998;273:13313–13316. doi: 10.1074/jbc.273.21.13313. [DOI] [PubMed] [Google Scholar]
- 67.Odorisio T, Cianfarani F, Failla CM, Zambruno G. The placenta growth factor in skin angiogenesis. J Dermatol Sci. 2006;41:11–19. doi: 10.1016/j.jdermsci.2005.08.008. [DOI] [PubMed] [Google Scholar]
- 68.Frank S, Hubner G, Breier G, Longaker MT, Greenhalgh DG, Werner S. Regulation of vascular endothelial growth factor expression in cultured keratinocytes. Implications for normal and impaired wound healing. J Biol Chem. 1995;270:12607–12613. doi: 10.1074/jbc.270.21.12607. [DOI] [PubMed] [Google Scholar]
- 69.Babic AM, Chen CC, Lau LF. Fisp12/mouse connective tissue growth factor mediates endothelial cell adhesion and migration through integrin alphavbeta3, promotes endothelial cell survival, and induces angiogenesis in vivo. Mol Cell Biol. 1999;19:2958–2966. doi: 10.1128/mcb.19.4.2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shimo T, Nakanishi T, Nishida T, Asano M, Kanyama M, Kuboki T, Tamatani T, Tezuka K, Takemura M, Matsumura T, Takigawa M. Connective tissue growth factor induces the proliferation, migration, and tube formation of vascular endothelial cells in vitro, and angiogenesis in vivo. J Biochem. 1999;126:137–145. doi: 10.1093/oxfordjournals.jbchem.a022414. [DOI] [PubMed] [Google Scholar]
- 71.Nagy JA, Vasile E, Feng D, Sundberg C, Brown LF, Detmar MJ, Lawitts JA, Benjamin L, Tan X, Manseau EJ, Dvorak AM, Dvorak HF. Vascular permeability factor/vascular endothelial growth factor induces lymphangiogenesis as well as angiogenesis. J Exp Med. 2002;196:1497–1506. doi: 10.1084/jem.20021244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Maruyama K, Asai J, Ii M, Thorne T, Losordo DW, D'Amore PA. Decreased macrophage number and activation lead to reduced lymphatic vessel formation and contribute to impaired diabetic wound healing. Am J Pathol. 2007;170:1178–1191. doi: 10.2353/ajpath.2007.060018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Schledzewski K, Falkowski M, Moldenhauer G, Metharom P, Kzhyshkowska J, Ganss R, Demory A, Falkowska-Hansen B, Kurzen H, Ugurel S, Geginat G, Arnold B, Goerdt S. Lymphatic endothelium-specific hyaluronan receptor LYVE1 is expressed by stabilin-1+, F4/80+, CD11b+ macrophages in malignant tumours and wound healing tissue in vivo and in bone marrow cultures in vitro: implications for the assessment of lymphangiogenesis. J Pathol. 2006;209:67–77. doi: 10.1002/path.1942. [DOI] [PubMed] [Google Scholar]
- 74.Ribatti D. The discovery of the placental growth factor and its role in angiogenesis: a historical review. Angiogenesis. 2008;11:215–221. doi: 10.1007/s10456-008-9114-4. [DOI] [PubMed] [Google Scholar]
- 75.Failla CM, Odorisio T, Cianfarani F, Schietroma C, Puddu P, Zambruno G. Placenta growth factor is induced in human keratinocytes during wound healing. J Invest Dermatol. 2000;115:388–395. doi: 10.1046/j.1523-1747.2000.00085.x. [DOI] [PubMed] [Google Scholar]
- 76.Hattori K, Heissig B, Wu Y, Dias S, Tejada R, Ferris B, Hicklin DJ, Zhu Z, Bohlen P, Witte L, Hendrikx J, Hackett NR, Crystal RG, Moore MA, Werb Z, Lyden D, Rafii S. Placental growth factor reconstitutes hematopoiesis by recruiting VEGFR1(+) stem cells from bone-marrow micro environment. Nat Med. 2002;8:841–849. doi: 10.1038/nm740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Adini A, Kornaga T, Firoozbakht F, Benjamin LE. Placental growth factor is a survival factor for tumor endothelial cells and macrophages. Cancer Res. 2002;62:2749–2752. [PubMed] [Google Scholar]
- 78.Bottomley MJ, Webb NJ, Watson CJ, Holt L, Bukhari M, Denton J, Freemont AJ, Brenchley PE. Placenta growth factor (PlGF) induces vascular endothelial growth factor (VEGF) secretion from mononuclear cells and is co-expressed with VEGF in synovial fluid. Clin Exp Immunol. 2000;119:182–188. doi: 10.1046/j.1365-2249.2000.01097.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Carmeliet P, Moons L, Luttun A, Vincenti V, Compernolle V, De Mol M, Wu Y, Bono F, Devy L, Beck H, Scholz D, Acker T, DiPalma T, Dewerchin M, Noel A, Stalmans I, Barra A, Blacher S, Vandendriessche T, Ponten A, Eriksson U, Plate KH, Foidart JM, Schaper W, Charnock-Jones DS, Hicklin DJ, Herbert JM, Collen D, Persico MG. Synergism between vascular endothelial growth factor and placental growth factor contributes to angiogenesis and plasma extravasation in pathological conditions. Nat Med. 2001;7:575–583. doi: 10.1038/87904. [DOI] [PubMed] [Google Scholar]
- 80.Autiero M, Waltenberger J, Communi D, Kranz A, Moons L, Lambrechts D, Kroll J, Plaisance S, De Mol M, Bono F, Kliche S, Fellbrich G, Ballmer-Hofer K, Maglione D, Mayr-Beyrle U, Dewerchin M, Dombrowski S, Stanimirovic D, Van Hummelen P, Dehio C, Hicklin DJ, Persico G, Herbert JM, Shibuya M, Collen D, Conway EM, Carmeliet P. Role of PlGF in the intra- and intermolecular cross talk between the VEGF receptors Flt1 and Flk1. Nat Med. 2003;9:936–943. doi: 10.1038/nm884. [DOI] [PubMed] [Google Scholar]
- 81.Loots MA, Lamme EN, Zeegelaar J, Mekkes JR, Bos JD, Middelkoop E. Differences in cellular infiltrate and extracellular matrix of chronic diabetic and venous ulcers versus acute wounds. J Invest Dermatol. 1998;111:850–857. doi: 10.1046/j.1523-1747.1998.00381.x. [DOI] [PubMed] [Google Scholar]
- 82.Wetzler C, Kampfer H, Stallmeyer B, Pfeilschifter J, Frank S. Large and sustained induction of chemokines during impaired wound healing in the genetically diabetic mouse: prolonged persistence of neutrophils and macrophages during the late phase of repair. J Invest Dermatol. 2000;115:245–253. doi: 10.1046/j.1523-1747.2000.00029.x. [DOI] [PubMed] [Google Scholar]
- 83.Tchaikovski V, Olieslagers S, Bohmer FD, Waltenberger J. Diabetes mellitus activates signal transduction pathways resulting in vascular endothelial growth factor resistance of human monocytes. Circulation. 2009;120:150–159. doi: 10.1161/CIRCULATIONAHA.108.817528. [DOI] [PubMed] [Google Scholar]
- 84.Goren I, Muller E, Pfeilschifter J, Frank S. Severely impaired insulin signaling in chronic wounds of diabetic ob/ob mice: a potential role of tumor necrosis factor-alpha. Am J Pathol. 2006;168:765–777. doi: 10.2353/ajpath.2006.050293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Zykova SN, Jenssen TG, Berdal M, Olsen R, Myklebust R, Seljelid R. Altered cytokine and nitric oxide secretion in vitro by macrophages from diabetic type II-like db/db mice. Diabetes. 2000;49:1451–1458. doi: 10.2337/diabetes.49.9.1451. [DOI] [PubMed] [Google Scholar]
- 86.Fang Y, Shen J, Yao M, Beagley KW, Hambly BD, Bao S. Granulocyte-macrophage colony-stimulating factor enhances wound healing in diabetes via upregulation of proinflammatory cytokines. Br J Dermatol. 2009 doi: 10.1111/j.1365-2133.2009.09528.x. [DOI] [PubMed] [Google Scholar]
- 87.Ure I, Partsch B, Wolff K, Petzelbauer P. Granulocyte/macrophage colony-stimulating factor increases wound-fluid interleukin 8 in normal subjects but does not accelerate wound healing. Br J Dermatol. 1998;138:277–282. doi: 10.1046/j.1365-2133.1998.02074.x. [DOI] [PubMed] [Google Scholar]
- 88.Cianfarani F, Tommasi R, Failla CM, Viviano MT, Annessi G, Papi M, Zambruno G, Odorisio T. Granulocyte/macrophage colony-stimulating factor treatment of human chronic ulcers promotes angiogenesis associated with de novo vascular endothelial growth factor transcription in the ulcer bed. Br J Dermatol. 2006;154:34–41. doi: 10.1111/j.1365-2133.2005.06925.x. [DOI] [PubMed] [Google Scholar]
- 89.Deiters U, Barsig J, Tawil B, Muhlradt PF. The macrophage-activating lipopeptide-2 accelerates wound healing in diabetic mice. Exp Dermatol. 2004;13:731–739. doi: 10.1111/j.0906-6705.2004.00233.x. [DOI] [PubMed] [Google Scholar]
- 90.Goren I, Muller E, Schiefelbein D, Christen U, Pfeilschifter J, Muhl H, Frank S. Systemic anti -TNFalpha treatment restores diabetes-impaired skin repair in ob/ob mice by inactivation of macrophages. J Invest Dermatol. 2007;127:2259–2267. doi: 10.1038/sj.jid.5700842. [DOI] [PubMed] [Google Scholar]
- 91.Nahrendorf M, Swirski FK, Aikawa E, Stangenberg L, Wurdinger T, Figueiredo JL, Libby P, Weissleder R, Pittet MJ. The healing myocardium sequentially mobilizes two monocyte subsets with divergent and complementary functions. J Exp Med. 2007;204:3037–3047. doi: 10.1084/jem.20070885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cochain C, Rodero MP, Vilar J, Recalde A, Richart A, Loinard C, Zouggari Y, Guerin C, Duriez M, Combadiere B, Poupel L, Levy BI, Mallat Z, Combadiere C, Silvestre JS. Regulation of monocyte subsets systemic levels by distinct chemokine receptors controls postischemic neovascularization. Cardiovasc Res. 2010 doi: 10.1093/cvr/cvq153. in press. [DOI] [PubMed] [Google Scholar]