Abstract
Background
Complementary and alternative medicine (CAM) use is substantial among African-Americans; however, research on characteristics of African-Americans who use of CAM to treat specific conditions is scarce.
Objective
To determine what predisposing, enabling, need, and disease state factors are related to CAM use for treatment among a nationally representative sample of African-Americans.
Methods
A cross-sectional study design was employed using the 2002 National Health Interview Survey (NHIS). A nationwide representative sample of adult (≥ 18 years) African-Americans who used CAM in the past 12 months (n= 16,113,651 weighted; n=2,952 unweighted) were included. The Andersen Healthcare Utilization Model served the framework with CAM use for treatment as the main outcome measure. Independent variables included: predisposing (e.g., age, gender, education), enabling (e.g., income, employment, access to care); need (e.g., health status, physician visits, prescription medication use); and disease state (i.e., most prevalent conditions among African-Americans) factors. Multivariate logistic regression was used to address the study objective.
Results
Approximately one in five (20.2%) CAM past 12 month users used CAM to treat a specific condition. Ten of the 15 CAM modalities were used primarily for treatment by African-Americans. CAM for treatment was significantly (p<0.05) associated with the following factors: graduate education, smaller family size, higher income, region (northeast, midwest, west more likely than south), depression/anxiety, more physician visits, less likely to engage in preventive care, more frequent exercise behavior, more activities of daily living (ADL) limitations, and neck pain.
Conclusions
Twenty percent of African-Americans who used CAM in the past year were treating a specific condition. Alternative medical systems, manipulative and body-based therapies, as well as folk medicine, prayer, biofeedback, and energy/Reiki were used most often. Health care professionals should routinely ask patients about CAM use, but when encountering African-Americans, there may be a number of factors that may serve as cues for further inquiry.
Keywords: African-American, Andersen Healthcare Utilization Model, CAM, CAM for treatment complementary/alternative medicine
INTRODUCTION
Complementary and alternative medicine (CAM) use is substantial among U.S. adults with estimates ranging from 29 to 68 percent.1–6 The most recent nationally representative estimate of CAM use in the past 12 months (including prayer) was 62.1 percent,7 and even higher prevalence has been reported among African-Americans, with 67.6–71.3 percent using CAM.7,8 Prayer for health reasons, herbals, and deep breathing exercises are the most common CAMs used by the general population,7 and African-Americans have a similar profile with prayer for health reasons, herbals, and relaxation emerging as most prevalent.8 CAM use is common among people with chronic conditions;1,2,7 and African-Americans with chronic conditions are at least 3 times more likely to use CAM than not.8 In the aforementioned studies, CAM use was defined as any use in the past 12 months. However, questions still remain, especially among ethnic minority groups, regarding whether those who have used CAM in the past year were using it for prevention (e.g., taking megavitamins to prevent a cold or anti-oxidants to boost the immune system) or to treat a specific condition (e.g., using acupuncture or chiropractic care for back pain). Understanding more about what factors are associated with individuals who use CAM for treatment may help clinicians improve their quality of care.
Prior research indicates that CAM is used more as a complement versus an alternative to mainstream medicine;1,2,9–11 however, as mentioned previously, little evidence exists regarding use of CAM for treatment. Results from a nationally representative sample showed that CAM use (without prayer) for treatment (African-Americans vs. whites, respectively) was most prevalent with alternative-medical systems (e.g., acupuncture, homeopathy) (75.8% vs. 80.1%) and manipulative and body-based therapies (e.g., chiropractic care, massage) (72.3% vs. 68.6%); while CAM use for prevention was most prevalent with mind-body interventions (e.g., prayer, relaxation) (70.2% vs. 64.4%). In addition, biologically-based therapies (e.g., folk medicine, herbals) were used for treatment (or for both treatment and prevention) more often among whites (56.8%) than African-Americans (49.2%).12 Although use of biologically-based therapies may have beneficial effects,13–14 concerns exist regarding safety due to lack of evidence of efficacy, as well as potential side effects and interactions with prescription and over-the-counter medications.13–20 Among an underserved population, Bazargan et al. found that both CAM users for treatment and CAM users for prevention shared 2 similar characteristics: higher perceived racial discrimination and poor health status. In addition, CAM users for treatment were more likely to experience financial burdens, while CAM users for prevention were likely to have more education.21
Research on African-Americans use of CAM for treatment is scarce. Moreover, most of the studies conducted that included African-Americans may not be generalizable because of focused populations such as women,11 underserved,21 mentally ill, 22–23 and elderly. 24 In addition, most of the studies did not utilize a theoretical model or control for important covariates. What is known based on previous studies is that CAM is substantially used by African-Americans, particularly among those with chronic conditions. African-Americans tend to use CAM for treatment versus prevention. In addition, patients typically do not disclose CAM use to their health care providers, nor do health care providers routinely inquire about CAM use.2,3,10,25,26 Researchers need to address the lack of research in general and use nationally representative findings in particular to provide the most guidance to clinical practitioners.
Theoretical Framework
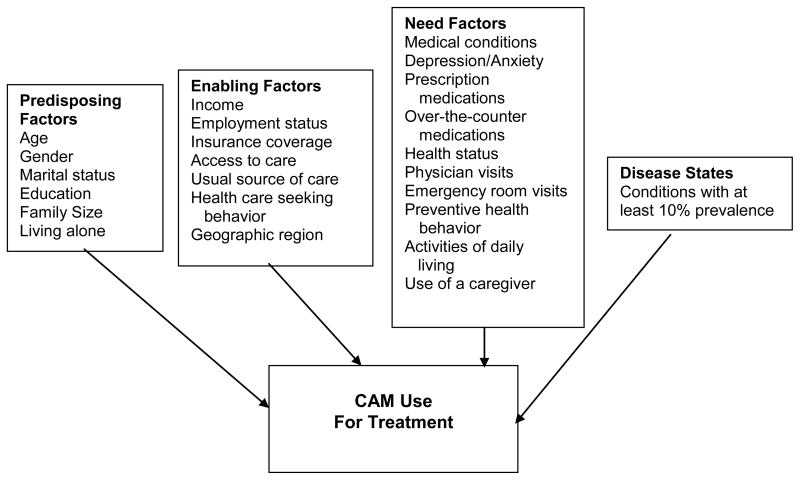
The Andersen Healthcare Utilization Model was used to assess relationships between predisposing (individuals propensity to use services), enabling (individual’s ability to access services), and need (illness level) factors and CAM use for treatment.27 Overall, the literature shows that several predisposing variables have been consistently related to CAM use including older age, 1,2,4–7,9 female gender, 2,6,7,28–30 white race, 1,2,9,30–32 higher education, 5–7,28–30,32–36 and unmarried. 28,34,37 In studies that focused specifically on African-Americans, the primary predictors of CAM use were similar regarding age and gender, however, African-Americans with lower education were more likely to use CAM. 38–40 Of note, these studies utilized convenience samples. Once individuals are predisposed to utilize services, a mechanism to access the services must be available. These mechanisms, categorized as enabling factors, have been examined in CAM studies. CAM users typically have higher income, 1,2,33 poor access (financial or distance) to conventional services, 9,37,38 live in western regions of the US, 1,2,30,33 have insurance, 9,36,37 have a usual source of care,5,34 and are employed.33–34 Regarding African-Americans, lower income, urbanicity, living with a grandparent as a child, comorbidities, influence of family/friends, influence of social groups, lower access to care, and community group involvement have predicted CAM use.32,36,38,40 Again, most of these factors have been identified in convenience samples. The most immediate cause of health services use is the patients illness level or their perceived need for care. Overall, need factors are the strongest predictors of health care utilization.41 Higher use of conventional services and several disease related variables have been associated with CAM use. They include chronic and/or multiple health conditions, 3,9,32,35,37,42 lower depression/depressive symptoms, 31,33 higher prescription medication use,28,43 poorer health status, 5,10,34,37 higher number of physician visits, 5,9,34,37,42 higher emergency department visits, 5,44 more preventative health behaviors (e.g., no cigarette use, exercise behaviors), 32–34,36 higher disease severity,35,44 and higher OTC use.28,37 Among African-Americans, need for care predictors included higher number of prescription medications, use of a caregiver and current cigarette smoker.32,45
In addition to these standard Andersen model variables, prior research on CAM use in African-Americans has shown that including specific disease states adds unique increased explanatory power.8 This study utilizes a theoretical framework and multivariate model to determine what predisposing, enabling, need, and disease state factors are related to CAM use for treatment among a nationally representative sample of African-Americans. The operationalization of the Andersen conceptual framework for this study is shown in Figure 1.
Figure 1.
Study Model
METHODS
Data Source
The 2002 National Health Interview Survey (NHIS) served as the data source. The NHIS used complex sampling design and person weights that resulted in a nationally representative database of all civilian, non-institutionalized persons who resided in the 50 states and the District of Columbia in 2002, with oversampling for black non-Hispanic participants.46 The study sample included adult African-Americans who used CAM in the past 12 months. The following NHIS files were used: Family Core, Sample Adult Core, and the Alternative Health/Complementary and Alternative Medicine supplement. The University of Texas at Austin Institutional Review Board approved this study.
Variables
CAM for treatment
The dependent variable in this study was “CAM for Treatment.” The 2002 NHIS participants were asked whether they used 17 different CAM modalities (see Table 1) in the past 12 months. Participants who indicated they had used the CAM modality in the past 12 months were asked if they had used it to treat a specific health problem or condition. If the respondent indicated “yes” to this question, the response was coded as CAM for Treatment. For those that indicated “no” to this question, CAM may have been used for prevention of health problems,12 health promotion, health maintenance, or other reasons. However, the survey question did not provide any specifics for the “no” response. For the purposes of this study, we used the term “prevention” for these “no” responses. For the prayer modality, participants who indicated they had a healing ritual or sacrament performed for their own health in the past 12 months were asked if this was for a specific problem or condition, but using prayer itself to treat a specific condition was not asked. Only 15 CAM modalities were included (chelation and hypnosis were excluded) in the analyses because none of the respondents used chelation in the past 12 months and respondents were not asked if hypnosis was used to treat a specific problem or condition. As indicated by the theoretical model, a number of factors were utilized to profile characteristics of African- Americans who use of CAM for treatment. The following describes the predisposing, enabling, need, and disease state factors.
Table 1.
Number (weighted) and percent of CAM use for treatment and prevention among African-Americans who used CAM in the past 12 months, U.S., 2002.
| CAM past 12 months | CAM for treatment | CAM for prevention | |||||
|---|---|---|---|---|---|---|---|
| CAM | Number | Number | %a | SE | Number | %a | SE |
| Overall CAM Use | 16,113,651 | 3,261,809 | 20.2 | (0.7) | 12,851,842 | 79.8 | (0.7) |
| Alternative-medical systems | |||||||
| Total | 326,079 | 251,367 | 77.1 | (3.8) | 74,712 | 22.9 | (3.8) |
| Acupuncture | 169,596 | 127,244 | 75.0 | (0.3) | 39,373 | 23.2 | (1.9) |
| Ayurveda | 15,388 | 15,388 | 100.0 | (----) | 0 | n/a | n/a |
| Homeopathic | 138,217 | 106,384 | 77.0 | (7.7) | 31,833 | 23.0 | (7.7) |
| Naturopathy | 32,768 | 28,772 | 87.8 | (15.0) | 3996 | 12.2 | (15.0) |
| Biologically-based therapies | |||||||
| Total | 3,868,605 | 1,890,543 | 48.9 | (1.8) | 1,978,062 | 51.1 | (1.8) |
| Chelation | 0 | 0 | n/a | 0 | n/a | ||
| Folk medicine | 27,141 | 21,259 | 78.3 | (----)b | 5,882 | 21.7 | (----)b |
| Herbal | 3,394,228 | 1,660,353 | 48.9 | (2.1) | 1,709,464 | 50.4 | (2.1) |
| Special diets | 519,904 | 210,011 | 40.4 | (2.7) | 309,893 | 59.6 | (2.7) |
| Megavitamins | 534,355 | 210,890 | 39.5 | (2.9) | 323,465 | 60.5 | (2.9) |
| Manipulative/body-based therapies | |||||||
| Total | 1,084,453 | 846,573 | 78.1 | (2.2) | 237,880 | 21.9 | (2.2) |
| Chiropractic | 662,284 | 624,498 | 94.3 | (0.7) | 37,786 | 5.7 | (0.7) |
| Massage | 570,894 | 303,875 | 53.2 | (3.1) | 267,019 | 46.8 | (3.1) |
| Mind-body therapy | |||||||
| Total | 15,378,457 | 1,212,532 | 7.9 | (0.5) | 14,165,925 | 92.1 | (0.5) |
| Biofeedback | 22,615 | 18,522 | 81.9 | (16.9) | 4093 | 18.1 | (16.9) |
| Relaxation | 3,239,705 | 752,095 | 23.2 | (1.4) | 2,470,666 | 76.3 | (1.4) |
| Hypnosisc | 40,097 | - | - | - | - | ||
| YTQd | 758,666 | 125,887 | 16.6 | (3.1) | 632,779 | 83.4 | (3.1) |
| Prayere | 635,210 | 421,165 | 66.3 | (2.6) | 211,838 | 33.3 | (2.6) |
| Energyf | 87,570 | 51,314 | 58.6 | (----)b | 36,256 | 41.4 | (----)b |
CAM- complementary and alternative medicine SE- standard error n/a- not applicable
Percent calculated from those who used CAM in the past 12 months
Standard error could not be calculated due to small sample size.
Respondents were not asked about use for a specific condition
Yoga/Tai Chi/Qi Gong
Question referred to healing ritual or sacrament
Energy Healing/Reiki
Note: When CAM for treatment and prevention do not add to 100 percent, the remaining respondents indicated “don’t know” or “refused. Reprinted with permission from Journal of Alternative and Complementary Medicine
Predisposing factors
Age was assessed using the following six categories: 18–24 (reference), 25–34, 35–44, 45–54, 55–64, and ≥65 years of age. For gender, males were the reference category and marital status was dichotomized as married or not married (reference). The following five education categories were used: less than 12 years (reference), 12 years (high school degree), 13–15 years (some college), bachelors degree, and advanced degree. Two variables were used to capture the number of individuals in the family: family size (total number of individuals in the household) and living alone dichotomized as yes or no (reference).
Enabling factors
Income was measured using 11 ordinal categories: 0–4,999 (reference) to 75,000 or greater. Employment status was categorized as not working (reference), working, and retired. Based on responses to nine types of insurance, insurance coverage was dichotomized as uninsured (reference) or insured. Access to care was operationalized using two variables: delay care and unable to afford care. Delay care was dichotomized as no (reference) or yes based on any positive response to the following reasons: couldn’t get through on the phone; couldn’t get appointment soon enough; have to wait too long; not open when you could get there; and no transportation. Unable to afford care was dichotomized as yes or no (reference). Similarly, usual source of care was dichotomized as yes or no (reference). Health care seeking behavior was operationalized using responses regarding the last time the respondent sought care: never, less than one year, or greater than or equal to one year (reference). Geographic region was comprised of four categories: south (reference), northeast, midwest, and west.
Need factors
The medical conditions variable, which served as a proxy for disease burden, was the total count of “yes” responses to the question, “During the past 12 months have you had…” or “have you been told that you have…” for 37 different conditions provided in the NHIS.46 Depression/anxiety, prescription medication use, and over the counter (OTC) medication use were all dichotomized as yes or no (reference). Health status change over the past 12 months was categorized as better, worse, or about the same (reference). Medical visits to a doctor or other health professional and emergency room visits were both categorized using an eight-point scale (0=none, 8= greater than or equal to 16). Preventive health behavior was operationalized using three measures: prevention care, current smoking status, and exercise frequency. Prevention care was measured as yes or no (reference) based on respondents indicating whether they had received prevention care or used one of six places (clinic, physician, HMO, emergency department, outpatient department, other place) for prevention care. Current smoking status was dichotomized as yes or no (referent). Exercise frequency was assessed by how often the respondents engaged in at least ten minutes of vigorous activity using the following three categories: “never/unable” (referent), “zero, one, or two times per week,” and “greater than three times a week.” The same categorization scheme was used for engaging in a moderate or strength exercise activity for ten minutes. Activities of daily living (ADL) limitations were categorized as no (referent) or yes if respondents indicated that they had experienced any degree of limitation for 12 activities. Use of a caregiver at home by the respondent was dichotomized as yes or no (referent).
Disease state factors
Although total number of medical conditions was included among the need factors, as mentioned previously, prior research on CAM use in African-Americans showed that including specific disease states to the Andersen model added unique increased explanatory power.8 Disease state factors in this study were derived by using the NHIS database to determine the most prevalent (at least 10% prevalence) disease states (or medical conditions) among African Americans. The following 13 disease states were included as factors in the model: anxiety/depression, arthritis, diabetes, fatigue, high cholesterol, hypertension, insomnia, lower back pain, neck pain, pain/aching joints, recurring pain, severe/migraine headache, and sinusitis.
Data Analysis
Logistic regression was employed and the analysis was conducted using Proc Surveylogistic in SAS 9.1.3 SP4, which accounts for the NHIS complex sampling design. Individual sample weights were also used to represent US civilian non-institutionalized adults.46 The Wald chi-square test was used to control for the simultaneous effects of all of the variables included in the model in order to determine individual net effect and utilize adjusted odds ratios for each predictor variable to interpret study results. An a priori p-value of 0.05 was chosen. To address missing data, multiple imputation using SAS Proc MI and Proc MIanalyze were used. Specifically, 10 datasets with different imputed missing values were created using Proc MI and, using the survey weights, logistic regression was employed with the 10 imputed datasets. Proc MIanalyze was used to calculate 10 estimates for each parameter and then computes an adjusted t-test statistic. An additional joint test of the 12 coefficients being zero was also performed to test whether the disease states added additional explanation to the standard Andersen model.
RESULTS
Individual Modalities
Of the 4,256 total NHIS CAM survey respondents, 2,952 (69.4%) used CAM in the past 12 months. Of these (n= 2,952 unweighted; n=16,113,651 weighted) individuals, 610 (20.2%) (n=3,261,809 weighted) used CAM to treat a specific condition. The study sample and CAM modalities used for treatment have been described in a previous paper.8 In brief, of the 15 CAM modalities that inquired about treatment, 10 were used primarily (≥50%) for treatment, while the remaining 5 were used for prevention (See Table 1). Thus, the majority of individual CAM modalities were used to treat a specific condition. Alternative-medical systems (i.e., acupuncture, ayurveda, homeopathic treatment, and naturopathy) and manipulative and body-based therapies (i.e., chiropractic care and massage) were used for treatment by at least 75 percent of those who used the respective CAM therapies in the past 12 months. Less than 50 percent of African-American CAM (past 12 month) users used biologically-based therapies (i.e., herbals, special diets, megavitamins) for treatment, with the exception of folk medicine, which was used for treatment by >75 percent (78.3%) of African-Americans who used this modality in the past 12 months. Some mind-body therapies [i.e., relaxation (76.3%), yoga/tai chi/qi gong (83.4%)] were used primarily for prevention, while other mind-body therapies [i.e., biofeedback (81.9%), prayer (66.3%), and energy healing/Reiki (58.6%)] were primarily used for treatment.
Factors Related to CAM Use for Treatment
The purpose of this study was to determine what predisposing, enabling, need for care, and disease state factors are related to CAM use for treatment among a nationally representative sample of African-Americans who used any one of 15 CAMs in the past 12 months (see Table 2). Of the 6 predisposing factors from Andersen’s model, the 2 factors significantly (p<0.05) related to CAM for treatment were education and family size. African-Americans who were college-educated [Advanced degree (OR=1.98, p=0.008)] and had smaller family sizes (OR=0.86, p=0.003) were more likely to use CAM for treatment. Of the 8 enabling factors, 2 had a significant relationship to CAM for treatment: income and region. Individuals with higher incomes (OR=1.07, p=0.016) were more likely to use CAM for treatment. Compared to the south, respondents in other regions were more likely to use CAM for treatment: northeast (OR=1.82, p<0.0001); midwest (OR=1.45, p=0.004); west (OR=1.88, p<0.0001). Of the 12 need factors, 6 were significantly related to CAM for treatment. While respondents who engaged in preventative care were less likely to use CAM for treatment (OR=0.58, p=0.039), respondents more likely to use CAM for treatment: had depression/anxiety (OR=1.93, p<0.0001); had more physician visits (OR=1.08, p=0.016); were engaged in vigorous exercise 0–2 times per week (OR=1.46, p=0.027), vigorous exercise ≥3 times per week (OR=1.67, p=0.001) (compared to never/unable); had at least one ADL limitation (OR=1.46, p=0.015); and had neck pain (OR=1.68, p=0.002). Additionally, as was shown in a previous study, 8 an F-test of the joint hypothesis that adding disease states to the model was significant.
Table 2.
Logistic Regression of Factors related to CAM use for Treatment
| Multivariate Conditional Estimates | Unconditional Univariate Estimates | ||||
|---|---|---|---|---|---|
| Factors | Odds Ratio | Confidence Intervals | P-value | Odds Ratio | Confidence Intervals |
| Predisposing Factors | |||||
| Agea | |||||
| 25 to 34 | 1.16 | (.74,1.83) | 0.514 | 0.91 | (.72,1.15) |
| 35 to 44 | 1.25 | (.81,1.94) | 0.312 | 1.07 | (.85,1.36) |
| 45 to 54 | 1.22 | (.78,1.91) | 0.383 | 1.33 | (1.04,1.68) |
| 55 to 64 | 1.12 | (.60,2.06) | 0.725 | 1.29 | (.94,1.78) |
| 65 or older | 0.74 | (.40,1.37) | 0.343 | 0.57 | (.41,.79) |
| Femaleb | 1.11 | (.85,1.45) | 0.449 | 1.22 | (.99,1.51) |
| Marital statusc | |||||
| Married or living with partner | 0.81 | (.59,1.11) | 0.192 | 0.84 | (.68,1.03) |
| Educationd | |||||
| High school degree | 1.08 | (.78,1.50) | 0.649 | 0.78 | (.62,.98) |
| Some college or associate’s degree | 1.22 | (.86,1.72) | 0.266 | 1.22 | (.96,1.54) |
| Bachelors degree | 1.33 | (.87,2.04) | 0.184 | 1.29 | (1.00,1.66) |
| Advanced degree | 1.98 | (1.20,3.27) | 0.008 | 1.8 | (1.28,2.53) |
| Family size | 0.86 | (.78,.95) | 0.003 | 0.91 | (.85,.98) |
| Live alonee | 0.83 | (.59,1.18) | 0.310 | 1.13 | (.91,1.39) |
| Enabling Factors | |||||
| Income | 1.07 | (1.01,1.13) | 0.016 | 1.04 | (1.00,1.07) |
| Employment statusf | |||||
| Currently working | 0.83 | (.61,1.13) | 0.231 | 0.91 | (.74,1.12) |
| Retired | 0.79 | (.47,1.31) | 0.364 | 0.58 | (.39,.84) |
| Insuredg | 1.1 | (.66,1.83) | 0.709 | 1.15 | (.79,1.69) |
| Delayed careh | 1.14 | (.83,1.55) | 0.417 | 2 | (1.57,2.56) |
| Able to afford carei | 1.33 | (.95,1.86) | 0.094 | 2.09 | (1.60,2.73) |
| Usual source of carej | 1.23 | (.74,2.07) | 0.422 | 1.24 | (.90,1.72) |
| Health care seeking behaviork | |||||
| Last sought care <1 year | 0.97 | (.56,1.69) | 0.914 | 1.73 | (1.15,2.60) |
| Last sought care = never | 0.25 | (.03,2.08) | 0.202 | 0.12 | (.02,.92) |
| Regionl | |||||
| Northeast | 1.82 | (1.41,2.35) | <0.0001 | 1.56 | (1.28,1.92) |
| Midwest | 1.45 | (1.12,1.87) | 0.004 | 1.42 | (1.15,1.76) |
| West | 1.88 | (1.41,2.51) | <0.0001 | 1.68 | (1.36,2.08) |
| Need for Care Factors | |||||
| Total medical conditions | 1.05 | (.97,1.14) | 0.207 | 1.13 | (1.11,1.15) |
| Depression/Anxietym | 1.93 | (1.45,2.56) | <0.0001 | 2.88 | (2.32,3.56) |
| Change in health statusn | |||||
| Better | 1.2 | (.93,1.54) | 0.161 | 1.43 | (1.14,1.80) |
| Worse | 0.8 | (.56,1.15) | 0.231 | 1.44 | (1.08,1.93) |
| Number of MD visits | 1.08 | (1.01,1.14) | 0.016 | 1.16 | (1.12,1.21) |
| Number of ER visits | 1.09 | (.98,1.20) | 0.119 | 1.25 | (1.15,1.36) |
| Prescription medication useo | 1.22 | (.87,1.70) | 0.254 | 1.74 | (1.41,2.16) |
| Over-the-counter medication usep | 0.97 | (.74,1.26) | 0.806 | 1.22 | (.99,1.51) |
| Prevention careq | 0.58 | (.34,.97) | 0.039 | 1.05 | (.75,1.46) |
| Current Smokerr | 0.98 | (.76,1.28) | 0.907 | 1.18 | (.94,1.48) |
| Vigorous Activitys | |||||
| <3 times per week | 1.46 | (1.04,2.05) | 0.027 | 1.23 | (.96,1.59) |
| ≥3 times per week | 1.67 | (1.23,2.28) | 0.001 | 1.5 | (1.19,1.88) |
| Moderate Activitys | |||||
| <3 times per week | 1.22 | (.85,1.76) | 0.276 | 1.16 | (.88,1.52) |
| ≥3 times per week | 1.3 | (.99,1.72) | 0.061 | 1.42 | (1.13,1.80) |
| Strength Activitys | |||||
| <3 times per week | 1.21 | (.81,1.80) | 0.356 | 1.37 | (1.01,1.87) |
| ≥3 times per week | 1.25 | (.88,1.77) | 0.208 | 1.41 | (1.08,1.84) |
| Activities of daily living (ADL) limitationst | 1.46 | (1.08,1.98) | 0.015 | 2 | (1.64,2.43) |
| Use of a caregiveru | 0.69 | (.35,1.38) | 0.297 | 1.08 | (.64,1.83) |
| Disease Statesv | |||||
| Pain/aching joints | 1.16 | (.86,1.56) | 0.334 | 1.98 | (1.63,2.40) |
| Hypertension | 0.86 | (.65,1.15) | 0.304 | 1.04 | (.86,1.26) |
| Lower back pain | 1.27 | (.94,1.72) | 0.121 | 2.34 | (1.89,2.89) |
| Arthritis | 0.83 | (.61,1.11) | 0.208 | 1.61 | (1.32,1.96) |
| Recurring pain | 1.15 | (.78,1.70) | 0.479 | 2.43 | (1.86,3.17) |
| Insomnia | 0.96 | (.71,1.30) | 0.791 | 2.29 | (1.89,2.77) |
| Severe headache | 0.82 | (.60,1.12) | 0.217 | 1.83 | (1.46,2.30) |
| Sinusitis | 1.13 | (.75,1.69) | 0.567 | 1.71 | (1.30,2.24) |
| High cholesterol | 1.16 | (.87,1.55) | 0.298 | 1.43 | (1.14,1.79) |
| Neck pain | 1.68 | (1.20,2.36) | 0.002 | 3.05 | (2.34,3.97) |
| Diabetes | 0.77 | (.53,1.11) | 0.159 | 0.97 | (.70,1.34) |
| Fatigue | 0.77 | (.52,1.14) | 0.196 | 1.77 | (1.36,2.31) |
CAM Use for Treatment-Any CAM use in past 12 months to treat a specific condition
UCL-Upper confidence limit; LCL-Lower confidence limit
McFadden’s pseudo-R2 =0.14. Nagelkerke’s pseudo-R2 =1.0
Referent categories:
18 to 24;
Male;
Not married;
Less than high school;
Not living alone;
Not currently working;
Uninsured;
Did not delay care;
Unable to afford care;
No usual source of care;
Last sought care >1 year;
South region;
No Depression/Anxiety;
About the same;
No prescription medication use;
No over-the-counter medication use;
No prevention care;
Not current smoker;
Never/unable;
No activities of daily living limitations;
No use of a caregiver;
Disease state not present.
CAM for Treatment Without Prayer
Because of its prevalence in CAM use among African-Americans and the general population, additional analyses were conducted excluding prayer. Results indicate that characteristics of African-American CAM users were very similar to those who used prayer, with 4 factors changing their significance status: prevention care (OR=0.62, p=0.074) and ADL limitations (OR=1.31, p=0.55) were no longer significant, whereas moderate activity ≥3 times per week (OR=1.40, p=0.024) emerged as significant. Lastly, in addition to neck pain, lower back pain (OR=1.39, p=0.036), emerged as significant when prayer was excluded.
DISCUSSION
Individual Modalities
The majority of CAM modalities (10 out of 15) were used by African-American CAM users (past 12 months) primarily for treatment. All 4 of the alternative-medical systems modalities (i.e., acupuncture, ayurveda, homeopathic, and naturopathy) were used for treatment by at least 75 percent of African-Americans who used these in the past 12 months. Not surprisingly, both of the manipulative and body-based therapies [i.e., chiropractic (94.3%) and massage 53.2%)] were used by the majority of African-Americans for treatment purposes as well. Our findings are congruent with previous studies that show that most African-American users of alternative-medical systems (e.g., acupuncture)12,47 and chiropractic care and massage12 employ these modalities for treatment purposes. Thus, health care providers, when treating African-Americans using alternative-medical systems, should suspect other mainstream therapies are also being used to treat the condition. Of the 5 mind-body therapies, 3 [biofeedback (81.9%), prayer (66.3%), and energy healing/Reiki (58.6%)] were used primarily for treatment. However, another study, which also used the same NHIS data source, found that, among the general population and African-Americans, mind-body therapies were primarily used for prevention (72% vs. 73%, respectively).12 Even though the data source was the same, this discrepancy may be attributed to different methodologies: our study included prayer, whereas theirs did not. The role of prayer is discussed in the next section. Although, overall, the biologically-based therapies were used primarily for prevention, folk medicine (78.3%) was most often used for treatment, followed by herbals (48.9%). The literature supports a higher prevalence of folk medicine (sometimes referred to as “home remedies,” or “traditional medicine”) in ethnic minority populations.40 In one multivariate study investigating older adults, African-Americans were almost 3 times more likely to use home remedies for health reasons when compared to whites. Although the study did not specifically indicate home remedy use for prevention or treatment, the multivariate model indicated that increased home remedy use was significantly associated with more chronic conditions and higher pain severity,24 supporting the speculation that home remedies were likely used for treatment. Another multivariate study assessed home remedy use among older adults with diabetes and found that African-Americans were significantly more likely than whites to use non-food home remedies for health self-management.48 Additionally, Xu et al. revealed that African-Americans were more likely to use traditional medicine (e.g., folk medicine, home remedies) as an alternative to mainstream medicine.47 Because of the widespread use of home remedies among African-Americans and the possibility that they are being used as an alternative, health care providers should inquire about home remedies and how these modalities are incorporated into their health care practices.
Prevalent Modalities
Although some of the CAM modalities were used by the vast majority of African-American users for treatment [e.g., ayurveda (100%), naturopathy (87.8%)], these modalities were used by a very small percentage of African-Americans overall. It is important to focus on the most prevalent CAM modalities (i.e., prayer, herbals, relaxation) used by African-Americans8 since clinicians are more likely to encounter these patients. These prevalent modalities fall into 3 use categories: primarily treatment (prayer 66.3%), both treatment and prevention (herbals 48.9% vs. 51.1%), and primarily prevention (relaxation 76.3%). Religion and spirituality are predominant in African-American culture and have been influential in guiding healthcare decisions and behaviors, 49,50 with one study documenting prayer as the most prevalent form of self-help therapy Among African-Americans 51 Another study reported that African-American women who used religion/spirituality (e.g., prayer) for health reasons were more likely to see a physician for their health problems, implying complementary behaviors; and they also tended to use religion/spirituality to treat serious conditions such as cancer, heart disease, osteoporosis, and depression.52 In this same study, African-American women were more likely to turn to religion/spirituality when consistent with their beliefs, if they were inclined to more natural approaches to health, if they experienced medication-related problems, as well as if they had childhood influences.52 Questions still remain regarding how African-Americans use prayer for treatment. For example it is not known whether prayer is used as a complement or an alternative and whether the use of prayer results in a delay in treatment seeking? Since prayer was one of the predominant forms of CAM used for treatment by African-Americans, it is important for health care providers to engage patients in a dialogue regarding use of prayer to treat specific conditions so that they may be better informed about how to incorporate spirituality into their self-care practices.
Almost half of African-Americans who used CAM in the past 12 months used herbals for treatment. Kennedy found a positive relationship between prescription and over-the-counter medication use and herbals, which suggests complementary behaviors. However, herbal users were also more likely to delay or avoid care due to lack of monetary resources, which suggests a substitutive pattern.53 More research is needed to determine how specific herbals are being used by African-Americans and the extent to which they result in substitutive practices. In this study, relaxation was used primarily for prevention. The paucity of studies on relaxation and African Americans makes it difficult to put these findings into context. Perhaps, African Americans use of relaxation for prevention was for reducing stress, a known cause of illness. Thus, the role of relaxation for prevention among African-Americans also warrants further investigation.
Factors Related to CAM Use for Treatment
This study’s multivariate analyses, using the Andersen model framework, revealed several characteristics of African-Americans who used CAM for treatment. Although previous convenience sample studies including only African-Americans showed that lower education was significantly related to CAM use,38–40 this study revealed that African-Americans who were educated with an advanced degree were predisposed to using CAM to treat a specific condition. These results are congruent with other CAM use studies that were large and included various population groups.1–3,5,7,39,48 This also shows that African-Americans are more similar to the general population in this respect. African-Americans with advanced degrees may be more aware of and more likely to investigate alternative therapies such as acupuncture, ayurveda, naturopathy, and biofeedback, which were shown in this study to be used primarily for treatment. African-Americans who had fewer family members were more predisposed to use CAM for treatment, which reflects findings from other studies where being unmarried was associated with CAM use.28,34,37
Regarding enabling factors, higher income and living in regions outside of the south were significant. It is likely that higher income was associated with higher education levels, both of which lead to increased access to care. Since a number of alternative therapies are not covered by insurance, individuals may need more disposable income to cover expenditures for these services. As shown in other studies, areas outside of the south (primarily the west)1,2,30,33 were more likely to use CAM. Perhaps ethnic cultural influences (e.g., Asian, European) in these areas of the US were more likely to be diffused into the African-American culture.
As is typical with the Andersen model, need factors are the main impetus for seeking care and this held true for our study. While other studies of the general population showed CAM use was associated with lower depressive symptoms, 31,33 African-Americans who suffer from anxiety and depression were almost twice as likely to use CAM for treatment. According to Unutzer et al. and Kessler et al., nonelderly adults with anxiety and depression tend to use spiritual practices, relaxation, and herbs to treat mental health conditions22,23 (which coincides with the most prevalent CAMs used by African-Americans in the past 12 months). This is an important observation since minorities, in particular African-Americans, are less likely to seek primary care or specialists to address mental health issues.55 Additionally, African-American women who used religion/spirituality were more likely to use it as a treatment for depression compared to those who did not use religion/spirituality for health reasons.52
Consistent with other studies, 5,9,34,37,42 the results of this study also showed that African-Americans who used CAM for treatment may have poorer health status as they were more likely to have physician visits and ADL limitations. However, the temporal order of this relationship is unclear. CAM use may have resulted in disability either because of substitutive behaviors or adverse reactions. It is also possible that “sicker” African-Americans were more likely to use CAM: because of failed treatment from mainstream medicine; or to “enhance” or complement mainstream medicine. While our sample was less likely to engage in preventive care activities, they were more likely to engage in exercise behaviors. Other studies have shown CAM users are typically non-smokers and exercisers. 32–34,36 The positive relationship between exercise behavior and CAM suggests that although African-Americans who use CAM for treatment may be sicker, they are also more likely to engage in health conscience behaviors such as exercise. This “health conscious” attitude was also reflected in a study of African-American women.52 Regarding disease states, CAM users (with prayer) were more likely to have neck pain, and when prayer was excluded from CAM use, lower back pain emerged as an additional significant predictor. Other studies also support the correlation between CAM use and having chronic conditions related to pain.24,52,54 When encountering patients who suffer from chronic pain, health care providers should suspect and therefore ask the patient if any type of CAM is being used to treat their condition. The addition of disease states to the Andersen model resulted in a unique and significant explanation. It is important to note that African-Americans were not likely to use CAM to treat chronic disease states that are highly prevalent (and have effective traditional medical treatments) such as hypertension, dyslipidemia, and diabetes.
African-Americans are not only substantial users of CAM, they also use the majority of modalities for treatment. Although a number of clinical trials using CAM are underway, questions still remain regarding the risks/benefits of CAM use for treating various conditions. Health care professionals should routinely ask about CAM use, but when encountering African-Americans, several characteristics may serve as cues for further inquiry. “Health conscious,” educated and higher income individuals, as well as those who have frequent physician visits are more likely to use CAM for treatment. In addition, African-Americans who suffer from anxiety and depression will more likely use prayer, herbals, and relaxation to treat their condition.22.23 Since prayer and spirituality are commonly used by African-Americans as a form of treatment, health care professionals should engage patients to understand what role they play in their health care management. Establishing a partnership built on understanding of and respect for their beliefs may lead to more information sharing between patients and providers. With knowledge of CAM use, providers are better able to monitor conditions for both positive and negative outcomes, as well as share clinical evidence regarding CAM use.
Limitations
Although the main strengths of this study were the use of a nationally representative sample of African-Americans and a theoretical model, several limitations still exist. As mentioned previously, CAM for treatment “no” responders used CAM in the past 12 months, but it is unknown whether they were using it for prevention or for other reasons. Prayer as a form of CAM treatment may have been underestimated in this study because the question regarding treatment was only asked of participants who indicated they had a healing ritual or sacrament performed for their own health in the past 12 months (weighted n=635,210) as compared to all African-Americans who used prayer in the past 12 months (weighted n=14,471,491). Additionally, use of CAM may have been underestimated because terms such as “home remedies” and culturally sensitive examples familiar to African-Americans were not used. Secondary database analyses are limited to available information. Thus, other variables such as acculturation, urbanicity, living with a grandparent as a child, and influence of family/friends, that have been associated with CAM use among African-Americans were not available in this study.32,36,38,40 As with any survey, respondents may not have interpreted questions as intended, however, NHIS has a history of surveying individuals using reliable and valid methodology.
Conclusions
African-Americans use the majority of CAM modalities to treat a specific condition, in particular alternative-medical systems and manipulative and body-based therapies, as well as folk medicine, prayer, biofeedback, and energy/Reiki. Multivariate analyses revealed a number of factors (e.g., educated, higher income, anxiety/depression, physician visits) related to CAM for treatment that health care professionals might consider using as cues for further inquiry.
Acknowledgments
The authors would like to acknowledge the National Institutes of Health/National Center for Complementary and Alternative Medicine for supporting this research (Grant 1 R21 AT002858-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Eisenberg DM, Kessler RC, Foster C, et al. Unconventional medicine in the United States: prevalence, costs, and patterns of use. NEJM. 1993;328:246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 2.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 3.Astin JA, Shapiro SK, Eisenberg DM, Forys KL. Mind-body medicine: state of the science, implications for practice. J Am Board Fam Pract. 2003;16:131–147. doi: 10.3122/jabfm.16.2.131. [DOI] [PubMed] [Google Scholar]
- 4.Kessler RC, Davis RB, Foster DF, et al. Long-term trends in the use of complementary and alternative-medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 5.Ni H, Simile C, Hardy AM. Utilization of complementary and alternative medicine by United States adults. Med Care. 2002;40:353–358. doi: 10.1097/00005650-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 6.Mackenzie ER, Taylor L, Bloom BS, et al. Ethnic minority use of complementary and alternative medicine (CAM): a national probability survey of CAM utilizers. Altern Therapies. 2003;9:50–56. [PubMed] [Google Scholar]
- 7.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Advance data from vital and health statistics. 343. Hyattsville, Maryland: National Center for Health Statistics; 2004. Complementary and alternative medicine use among adults: United States, 2002. [PubMed] [Google Scholar]
- 8.Brown CM, Barner JC, Richards KM, Bohman TM. Patterns of complementary and alternative Medicine use in African-Americans. J Altern Complement Med. 2007;13:751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]
- 9.Paramore LC. Use of alternative therapies: estimates from the 1994 Robert Wood Johnson Foundation National Access to Care Survey. J Pain Symptom Management. 1997;13:83–89. doi: 10.1016/s0885-3924(96)00299-0. [DOI] [PubMed] [Google Scholar]
- 10.Astin JA. Why patients use alternative medicine: results of a national study. JAMA. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 11.Kronenberg F, Cushman LF, Wade CM, Kalmuss D, Chao MT. Race/ethnicity and women’s use of complementary and alternative medicine in the United States: results of a national survey. Am J Public Health. 2006;96(7):1239–1242. doi: 10.2105/AJPH.2004.047688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grzywacz JG, Lang W, Suerken C, et al. Age, race, and ethnicity in the use of complementary and alternative medicine for health self-management: evidence from the 2002 National Health Interview Survey. J Aging Health. 2005;17:547–572. doi: 10.1177/0898264305279821. [DOI] [PubMed] [Google Scholar]
- 13.Ernst E, Pittler MH. Herbal medicine. Med Clin North Am. 2002;86:149–161. doi: 10.1016/s0025-7125(03)00077-4. [DOI] [PubMed] [Google Scholar]
- 14.Tyler VE. Herbal medicine: From the past to the future. Public Health Nutr. 2000;3:447–452. doi: 10.1017/s1368980000000525. [DOI] [PubMed] [Google Scholar]
- 15.Barrett B, Kiefer D, Rabago D. Assessing the risks and benefits of herbal medicine: An overview of scientific evidence. Altern Ther Health Med. 1999;5:40–49. [PubMed] [Google Scholar]
- 16.Cupp MJ. Herbal remedies: Adverse effects and drug interactions. Am Fam Physician. 1999;59:1239–1245. [PubMed] [Google Scholar]
- 17.Abebe W. Herbal medication. Potential for adverse reactions with analgesic drugs. J Clin Pharm Ther. 2002;27:391–401. doi: 10.1046/j.1365-2710.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 18.Awang DV, Fugh-Berman A. Herbal interactions with cardiovascular drugs. J Cardiovasc Nurs. 2002;22:22–28. doi: 10.1097/00005082-200207000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Ernst E. Use of herbal medications before surgery. JAMA. 2001;286:2542–2544. [PubMed] [Google Scholar]
- 20.Williamson EM. Drug interactions between herbal and prescription medicines. Drug Saf. 2003;26:1075–1092. doi: 10.2165/00002018-200326150-00002. [DOI] [PubMed] [Google Scholar]
- 21.Bazargan M, Norris K, Bazargan-Hejazi S, Akhanjee L, Calderon JL, Safvati SD, Baker RS. Alternative healthcare use in the under-served population. Ethn Dis. 2005;15:531–539. [PubMed] [Google Scholar]
- 22.Unutzer J, Klap R, Sturm R, et al. Mental disorders and the use of alternative medicine. Results from a national survey. Am J Psychiatry. 2000;157:1851–1857. doi: 10.1176/appi.ajp.157.11.1851. [DOI] [PubMed] [Google Scholar]
- 23.Kessler RC, Soukup J, Davis RB, et al. The use of complementary and alternative therapies to treat anxiety and depression in the United States. Am J Psychiatry. 2001;158:289–294. doi: 10.1176/appi.ajp.158.2.289. [DOI] [PubMed] [Google Scholar]
- 24.Grzywacz JG, Arcury TA, Bell RA, et al. Ethnic differences in elders home remedy use: sociostructural explanations. Am J Health Behav. 2006;30(1):39–50. doi: 10.5555/ajhb.2006.30.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shah S, Brown CM, Barner JC. Actions of Community Pharmacists in Response to Concurrent Use of Prescribed Medicines with Complementary and Alternative Medicine. J Am Pharm Asso. 2005;45(1):41–47. doi: 10.1331/1544345052843011. [DOI] [PubMed] [Google Scholar]
- 26.Kemper KJ. Taking on the herbal education challenge: Commentary on increasing physician awareness of the common uses and contraindications of herbal medicines. Utility of a case-based tutorial for residents. J Altern Complement Med. 2003;9:577–579. doi: 10.1089/107555303322284875. [DOI] [PubMed] [Google Scholar]
- 27.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? J Health Sci Soc Behav. 1995;36(1):1–10. [PubMed] [Google Scholar]
- 28.Burge SK, Albright TL. Use of complementary and alternative medicine use among family practice patients in south Texas. Am J Public Health. 2002;92:1614–1615. doi: 10.2105/ajph.92.10.1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arcury TA, Quandt SA, Bell RA, Vitolins MZ. Complementary and alternative medicine use among rural older adults. Complementary Health Pract Review. 2002;7:167–186. doi: 10.1177/1533210106292461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Druss BG, Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;282:651–656. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- 31.Gore-Felton C, Vosvick M, Power R, et al. Alternative therapies: a common practice among men and women living with HIV. JANAC. 2003;14:17–27. doi: 10.1177/1055329003014003002. [DOI] [PubMed] [Google Scholar]
- 32.Lee MM, Chang JS, Jacobs B, Wrensch MR. Complementary and alternative medicine use among men with prostate cancer in 4 ethnic populations. Am J Public Health. 2002;92:1606–1607. doi: 10.2105/ajph.92.10.1606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bair YA, Gold EB, Greendale GA, et al. Ethnic differences in use of complementary and alternative medicine at midlife: longitudinal results from SWAN participants. Am J Public Health. 2002;92:1832–1840. doi: 10.2105/ajph.92.11.1832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gray CM, Tan AW, Pronk NP, OConnor PJ. Complementary and alternative medicine use among health plan members: a cross-sectional survey. Effective Clin Pract. 2002 Jan/Feb;:1–7. [PubMed] [Google Scholar]
- 35.Shumay DM, Maskarinec G, Gotay CC, et al. Determinants of the degree of complementary and alternative medicine use among patients with cancer. J Altern Complementary Med. 2002;8:661–671. doi: 10.1089/107555302320825183. [DOI] [PubMed] [Google Scholar]
- 36.Lee MM, Lin SS, Wrensch MR, et al. Alternative therapies used by women with breast cancer in four ethnic populations. J Natl Cancer Inst. 2000;92:42–47. doi: 10.1093/jnci/92.1.42. [DOI] [PubMed] [Google Scholar]
- 37.Loera JA, Black SA, Markides KS, et al. The use of herbal medicine by older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2001;56A:M714–M718. doi: 10.1093/gerona/56.11.m714. [DOI] [PubMed] [Google Scholar]
- 38.Barnett MC, Cotroneo M, Purnell J, et al. Use of CAM in local African-American communities: community-partnered research. J Natl Med Assoc. 2003;95:943–950. [PMC free article] [PubMed] [Google Scholar]
- 39.Cuellar N, Aycock T, Cahill B, Ford J. Complementary and alternative medicine (CAM) use by African American (AA) and Caucasian American (CA) older adults in a rural setting: a descriptive, comparative study. BMC Complementary and Alternative Med. 2003;3:8. doi: 10.1186/1472-6882-3-8. Available: http://www.biomedcentral.com/1472-6882/3/8. [DOI] [PMC free article] [PubMed]
- 40.Boyd EL, Taylor SD, Shimp LA, Semler CR. An assessment of home remedy use by African-Americans. J Natl Med Assoc. 2000;92:341–353. [PMC free article] [PubMed] [Google Scholar]
- 41.de Boer A, Wijker W, de Haes H. Predictors of health care utilization in the chronically ill: a review of the literature. Health Policy. 1997;42:101–115. doi: 10.1016/s0168-8510(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 42.Najm W, Reinsch S, Hoehler F, Tobis J. Use of complementary and alternative medicine among the ethnic elderly. Altern Ther Health Med. 2003;9(3):50–57. [PubMed] [Google Scholar]
- 43.Poss JE, Jezewski MA, Stuart AG. Home remedies for type 2 diabetes used by Mexican Americans in El Paso, Texas. Clin Nurs Res. 2003;12:304–323. doi: 10.1177/1054773803256872. [DOI] [PubMed] [Google Scholar]
- 44.Ng TP, Wong ML, Hong CY, et al. The use of complementary and alternative medicine by asthma patients. Q J Med. 2003;96:747–754. doi: 10.1093/qjmed/hcg121. [DOI] [PubMed] [Google Scholar]
- 45.Sternberg SA, Chandran A, Sikka M. Alternative therapy use by elderly African Americans attending a community clinic. JAGS. 2003;51:1768–1772. doi: 10.1046/j.1532-5415.2003.51562.x. [DOI] [PubMed] [Google Scholar]
- 46.Anonymous . National Health Interview Survey description. National Center for Health Statistics, Centers for Disease Control and Prevention; [Accessed May 30, 2006]. Available at: http://www.cdc.gov/nchs/about/major/nhis/hisdesc.htm. [Google Scholar]
- 47.Xu KT, Farrell TW. Determinants of utilization: the complementary and substitution between unconventional and mainstream medicine among racial and ethnic groups. Health Serv Res. 2007;42:811–826. doi: 10.1111/j.1475-6773.2006.00628.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Arcury TA, Bell RA, Snively BM, et al. Complementary and alternative medicine use as health self-management: rural older adults with diabetes. J Gerontol: Social Sciences. 2006;61B:S62–S70. doi: 10.1093/geronb/61.2.s62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Roberson MH. The influence of religious beliefs on health choices of Afro-Americans. Top Clin Nurs. 1985;7(3):57–63. [PubMed] [Google Scholar]
- 50.Newlin K, Knafl K, Melkus GD. African-American spirituality: concept analysis. Adv Nurs Sci. 2002;25(2):57–70. doi: 10.1097/00012272-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 51.Silverman M, Musa D, Kirsch B, Siminoff LA. Self care for chronic illness: older African- Americans and Whites. J Cross-Cult Gerontol. 1999;14:169–189. doi: 10.1023/a:1006676416452. [DOI] [PubMed] [Google Scholar]
- 52.Dessio W, Wade C, Chao M, Kronenberg F, Cushman LF, Kalmuss D. Religion, spirituality and healthcare choices of African-American women: results of a national survey. Ethn Dis. 2004;14:189–196. [PubMed] [Google Scholar]
- 53.Kennedy J. Herb and supplement use in the US adult population. Clin Ther. 2005;27:1847–1858. doi: 10.1016/j.clinthera.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 54.Cherniak EP, Senzel RS, Pan CX. Correlates of use of alternative medicine by the elderly in an urban population. J Altern Complement Med. 2001;7:277–280. doi: 10.1089/107555301300328160. [DOI] [PubMed] [Google Scholar]
- 55.Neighbors HW, Caldwell C, Williams DR, Nesse R, Taylor RJ, Bullard KM, Torres M, Jackson JS. Race, ethnicity and the use of services for mental disorders. Arch Gen Psychiatry. 2007;64:485–494. doi: 10.1001/archpsyc.64.4.485. [DOI] [PubMed] [Google Scholar]