Abstract
Background and Objectives
Tuberculous (TB) pericarditis is a major cause of constrictive pericarditis requiring pericardiectomy. We sought to determine initial prognostic factors in patients with TB pericarditis.
Subjects and Methods
We evaluated initial presentation and clinical outcomes (mean follow-up 32±27 months) in 60 consecutive patients newly diagnosed with TB pericarditis.
Results
Initial presentations were pericardial effusion (PE), effusive-constrictive pericarditis, and constrictive pericarditis in 45 (75%), 9 (15%), and 6 (10%) patients, respectively. Of the 54 patients without initial constrictive pericarditis, 32 (59%) showed echogenic materials in PE, including frond-like exudative coating and fibrinous strands. These patients had a longer disease duration before diagnosis, were initially more symptomatic, in a more advanced state, showed more persistent pericardial constrictions (38% vs. 0%, p<0.001) despite anti-TB medications, and tended to require pericardiectomy more often (19% vs. 0%, p=0.07, p<0.05 by Kaplan-Meier). All patients with effusive-constrictive pericarditis showed echogenic PE. Of the 60 total patients, 10 (17%) underwent pericardiectomies during follow-up. All of these patients showed initial pericardial constrictions, whereas no patient without initial pericardial constriction underwent pericardiectomy (p<0.001). Seven patients showed transient pericardial constrictions that resolved without pericardiectomy.
Conclusion
Initial pericardial constriction and echogenic PE are poor prognostic signs for persistent pericardial constriction and pericardiectomy in patients with newly diagnosed TB pericarditis. These results suggest that early diagnosis and prompt anti-TB medication may be critical.
Keywords: Pericarditis, Tuberculosis, Echocardiography, Prognosis
Introduction
Tuberculosis (TB) continues to be a leading cause of morbidity and mortality from infectious disease worldwide,1) and TB pericarditis is arguably the leading cause of pericarditis in the world, despite a low incidence in developed countries. TB pericarditis patients initially present with diverse features, including pericardial effusion (PE), effusive-constrictive pericarditis, and constrictive pericarditis.2),3) Pericardial constrictive scarring, the most serious complication requiring pericardiectomy, occurs in 18-46% of patients with TB PE despite anti-TB chemotherapy and treatment with corticosteroids.3-5) The predictors of TB constrictive pericarditis have been suggested in several small studies,6-12) but remain to be clearly established.3) Echogenic materials seen in PE on 2-dimensional echocardiography, such as exudative coating and fibrinous strands, can predict pericardial complications irrespective of underlying disease etiologies,13) and are more specific to TB PE.14-18) However, the clinical prognostic value of such echogenic materials in TB PE has not been clearly demonstrated. Therefore, we evaluated clinical outcomes of newly-diagnosed TB pericarditis patients and determined initial prognostic predictors for the development of constrictive pericarditis requiring pericardiectomy.
Subjects and Methods
From 1995 to 2007, 60 consecutive patients (mean age 58±19 years, 30 females) were newly diagnosed with TB pericarditis at the Asan Medical Center, Seoul, Korea, and treated with anti-TB chemotherapy. Sixteen patients were also included in our previous report.13) No patient had any evidence of human immunodeficiency virus infection. For each patient, a complete clinical history was taken, and physical examination, chest X-ray, and 2-dimensional Doppler echocardiography were performed. Symptom onset time could be identified in 54 patients. Of the 60 patients, 47 underwent pericardiocentesis and/or pericardiostomy. Pericardial fluid and biopsy specimens were analyzed for chemistry, cytology, histopathology examination, acid-fast bacilli staining, culture for Mycobacterium tuberculosis, adenosine deaminase (ADA) measurement, and polymerase chain reaction (PCR) detecting M. tuberculosis.19) Diagnosis of TB pericarditis was categorized as definite or probable, as previously reported.3),4) A "definite" diagnosis was made when M. tuberculosis was found in PE fluid or pericardial samples by acid-fast bacilli staining, TB culture, or positive TB-PCR; or when granuloma was seen. All bacteriologically confirmed cases were pan-susceptible to anti-TB drugs. A "probable" diagnosis was made when there was proof of TB elsewhere in a patient with unexplained pericarditis or when PE showed a lymphocyte-dominant exudate with a high ADA (>40 U/L) level.
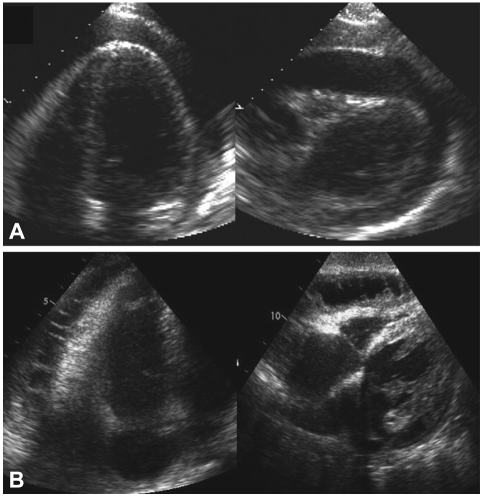
All patients underwent transthoracic 2-dimensional echocardiography (Sonos 7500, Philips Medical Systems, Andover, MA; Vivid 7, General Electric, Waukesha, WI; Acuson Sequoia, Mountain View, CA, USA), and all data were analyzed by a single expert. Patients with PE were divided into two groups by differences in initial echocardiographic characteristics of PE and pericardium. Echo-free PE was defined as PE without any echogenic materials (Fig. 1A),20) whereas echogenic PE was defined as PE showing echogenic materials in PE or on the pericardium (Fig. 1B).15),17),20)
Fig. 1.
Representative examples of echo-free pericardial effusion (PE) (A) and echogenic PE (B). PE: pericardial effusion.
Effusive-constrictive pericarditis was diagnosed when constrictive physiology was not resolved by PE removal, or when constrictive physiology was observed together with only a mild to moderate amount of PE. Constrictive physiology was defined as a significant respiratory variation in mitral inflow E wave velocity (≥25%) and a prominent increase in diastolic flow reversal with expiration in the hepatic vein on 2-dimensional Doppler echocardiography.21),22) Chest contrast-enhanced computed tomography (CT) was performed in 39 patients.
Clinical and echocardiographic observations were conducted for 32±27 months (median: 25 months) on patients taking adequate anti-TB medications for at least 6 months. Pericardial constriction was diagnosed when constrictive physiology (as described above) and diffuse pericardial thickening without PE were found on 2-dimensional Doppler echocardiography.21),23) Referral for pericardiectomy was determined by attending physicians' discretion.
Numeric variables are expressed as means±SD. Statistical analysis of between-groups differences was performed using Student's unpaired t-test. The χ2 test and Fisher's exact test were used to compare frequency ratios between groups. A Kaplan-Meier analysis and the log rank test were employed to compare event-free survival rates. A p of <0.05 was considered significant.
Results
Initial presentations were PE, effusive-constrictive pericarditis, and constrictive pericarditis in 45 (75%), 9 (15%), and 6 (10%) patients, respectively. Of the 45 patients who presented with PE, 9 patients (15%) showed initial cardiac tamponade defined as a large amount of PE, significant respiratory variations in mitral inflow E velocity, and diastolic collapse of the right atrium or ventricle. Of the 9 patients with effusive-constrictive pericarditis, constrictive physiology was not resolved by PE removal in 4 patients and constrictive physiology was observed together with only mild to moderate PE in 5 patients. Of the 54 patients without initial constrictive pericarditis, 32 (59%) showed echogenic PE, whereas 22 showed echo-free PE. Clinical features of both groups are summarized in Table 1. Weight loss was more prevalent in patients with echogenic PE than in those with echo-free PE, and the former patients presented with a greater number of symptoms, of longer duration, than did the latter cohort. All nine patients with effusive-constrictive pericarditis showed echogenic PE.
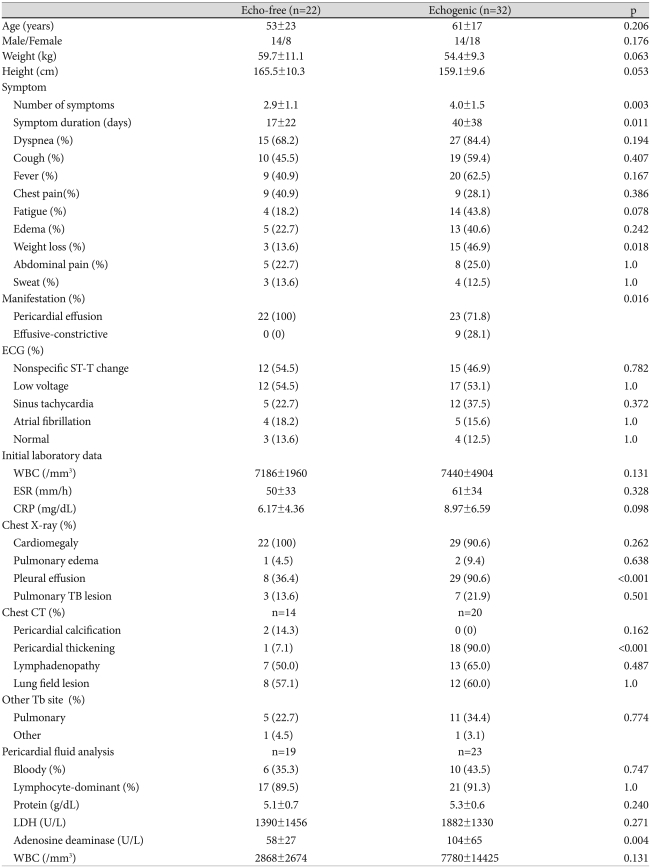
Table 1.
Comparison of clinical characteristics of echo-free and echogenic pericardial effusion patients
ECG: electrocardiogram, WBC: white blood cell, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, TB: tuberculosis, LDH: lactate dehydrogenase
Pleural effusion on initial chest X-ray and pericardial thickening on chest CT were significantly more prevalent in patients with echogenic PE than in those with echo-free PE. ADA activity in pericardial fluid was higher in the former patients than in the latter group. Definite diagnoses were more often possible in patients with echogenic PE than in those with echo-free PE (Table 2), and TB-specific pericardial pathology results, such as stained acid-fast bacilli and granuloma, were more frequently positive in echogenic patients. TB-PCR on PE fluid was more often positive in echogenic PE patients than in echo-free PE patients. Durations of anti-TB chemotherapy and proportions of patients treated with adjunctive corticosteroids did not differ between the two groups (Table 3).
Table 2.
Comparison of diagnostic criteria of tuberculous pericarditis between echo-free and echogenic pericardial effusion patients
*Echo-free: TB (0), Granuloma (4); Echogenic: TB (2), Granuloma (15). TB: tuberculosis, PCR: polymerase chain reaction, ADA: adenosine deaminase
Table 3.
Treatments and clinical events in patients with echo-free and echogenic pericardial effusion
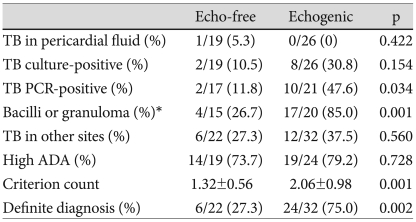
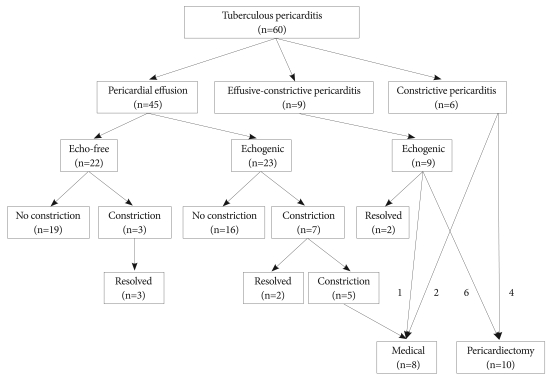
During follow-up, new pericardial constrictions developed in 10 patients, of whom 7 had shown echogenic PE on initial echocardiography (Fig. 2). Of these 10 patients, 100% (3/3) of echo-free PE patients and 29% (2/7) of those with initial echogenic PE showed transient pericardial constrictions that resolved during longer follow-up. No patient with initial echo-free PE but 5 patients (22%) with initial echogenic PE without initial pericardial constrictions, developed unresolved pericardial constrictions. In nine patients with initial effusive-constrictive pericarditis, two (22%) showed transient constrictions that resolved during anti-TB therapy, whereas six (67%) required pericardiectomies. The overall incidence of pericardial constriction on both initial and follow-up echocardiographic evaluations was higher in patients with initial echogenic PE than in those with initial echo-free PE (50.0% vs. 13.6%, p<0.01). During follow-up, pericardiectomies were performed on six patients with initial echogenic PE, but in no patient with initial echo-free PE. Of six patients who presented with initial constrictive pericarditis, four (67%) underwent pericardiectomies. None of these 6 patients showed pericardial constriction resolution despite the use of anti-TB medications.
Fig. 2.
Clinical outcomes of tuberculous pericarditis patients according to clinical and echocardiographic classifications.
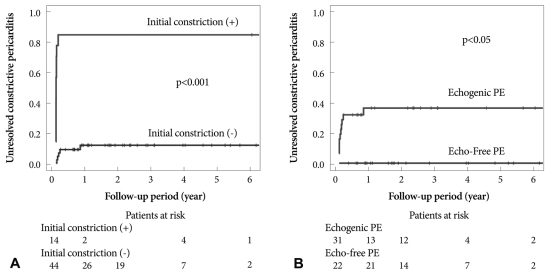
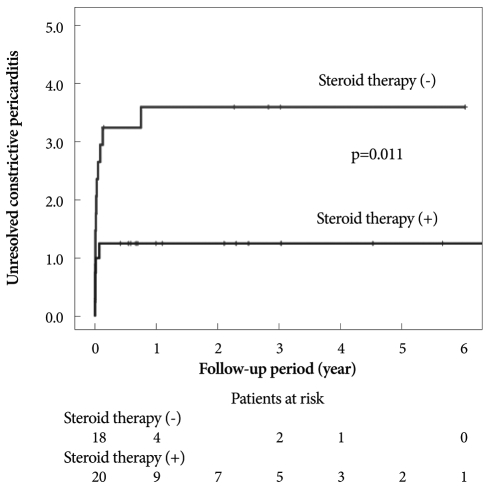
Of the 60 patients, 18 (30%) showed persistent constrictive pericarditis during follow-up. The incidence of unresolved pericardial constriction was higher in patients with initial constrictions than in those without, and was greater in patients with echogenic PE than in those with echo-free PE, as shown by Kaplan-Meier analyses of the unresolved constrictive pericarditis development rate (Fig. 3). Unresolved constrictive pericarditis developed in about 38% of patients who presented with echogenic PE, and in no patient with initial echo-free PE. Of 18 patients with persistent constrictive pericarditis, 8 patients were followed-up medically because their symptoms were tolerable with medications, including diuretics.
Fig. 3.
Kaplan-Meier analyses of developing persistent constrictive pericarditis in patients with or without initial pericardial constriction (A), and in patients with echogenic pericardial effusion (PE) or echo-free PE (B). PE: pericardial effusion.
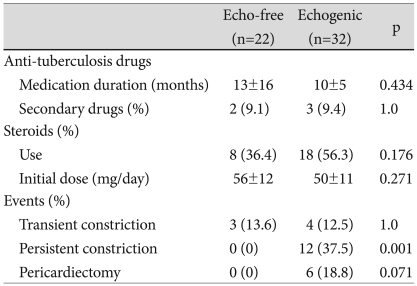
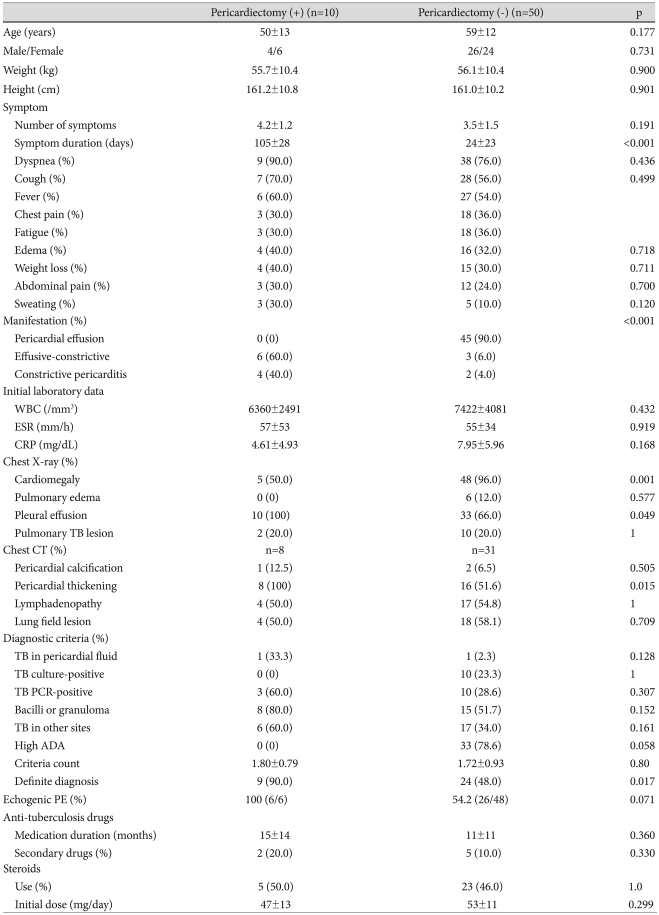
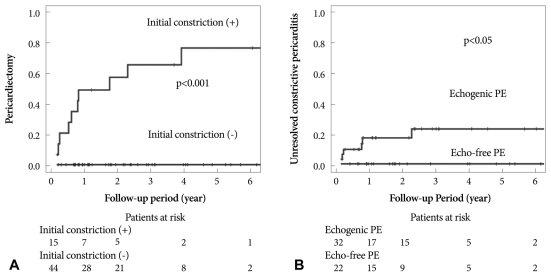
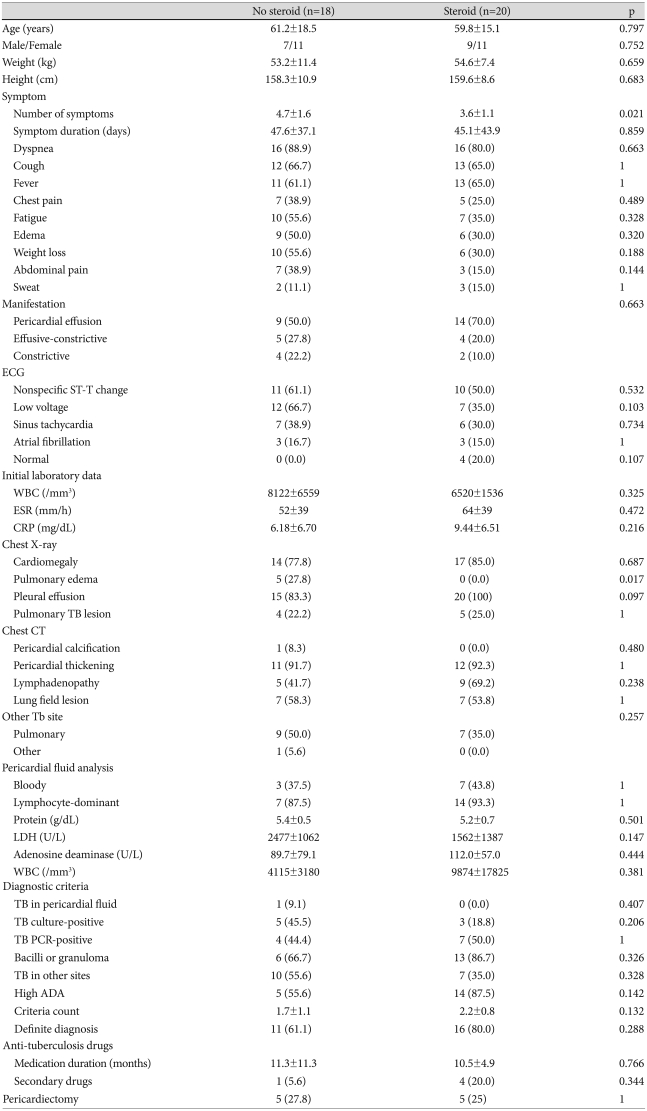
Of 60 patients, 10 (17%) underwent pericardiectomies during follow-up. On initial echocardiography, these patients showed a higher prevalence of pericardial constriction, thickening, and calcification, than did patients who did not require pericardiectomy (Table 4). The former patients showed a higher prevalence of pleural effusion and pericardial thickening by chest X-ray and CT, and had longer symptom duration, than did patients who did not require pericardiectomy. The durations of anti-TB medication and proportions of patients treated with steroids did not differ significantly between the two groups. Patients with pericardial constrictions on initial echocardiography showed a higher pericardiectomy rate than did those without constriction, by Kaplan-Meier analysis (p<0.001) (Fig. 4A). Similarly, patients with initial echogenic PE showed a higher pericardiectomy rate than did those with echo-free PE (p<0.05) (Fig. 4B). No mortality from pericarditis or surgery was observed in our study population. For 38 patients with initial constrictive physiology or echogenic PE (Table 5), Kaplan Meier analysis revealed that rate of persistent constriction during follow-up was lower in patients with than without steroid therapy (p=0.011) (Fig. 5).
Table 4.
Comparison of initial clinical and echocardiographic characteristics between patients who required pericardiectomies and those who did not
WBC: white blood cell, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, TB: tuberculosis, PCR: polymerase chain reaction, ADA: adenosine deaminase, PE: pericardial effusion
Fig. 4.
Kaplan-Meier analyses of pericardiectomy in patients with or without initial pericardial constriction (A), and in patients with echogenic pericardial effusion (PE) or echo-free PE (B). PE: pericardial effusion.
Table 5.
Comparisions of clinical characteristics for treatment with or without steroids in patients with echogenic pericardial effusion or constrictive physiology
ECG: electrocardiogram, WBC: white blood cell, ESR: erythrocyte sedimentation rate, CRP: C-reactive protein, LDH: lactate dehydrogenase, TB: tuberculosis, ADA: adenosine deaminase
Fig. 5.
Kaplan-Meier analyses of persistent constrictive pericarditis in patients with or without steroid therapy in patients with initial echogenic pericardial effusion or constrictive physiology (n=38).
Discussion
Predictors of constrictive pericarditis and pericardiectomy
Echogenic substances in PE are suggestive of TB pericarditis and signs of pericardial inflammation and a hypersensitivity reaction.14-17) However, echogenic substances are also found in the PE of other etiologies as risk factors for the development of constrictive pericarditis, irrespective of cause, in patients with PE.13),24),25) We previously reported on 178 consecutive patients with moderate to severe PE of any etiology, including 16 patients with TB PE.13) This study of 60 patients diagnosed with TB pericarditis was designed to evaluate the clinical outcome of TB pericarditis, and identify poor prognostic indicators for permanent constriction and pericardiectomy. Initial constrictive physiology was the major poor prognostic factor in TB pericarditis, which we did not find in our previous study as we only included PE patients. In this study, 59% of patients with TB pericarditis accompanied by PE showed echogenic PE, consistent with previous reports.15),17) In PE patients, intrapericardial echogenic materials were associated with a greater level of symptomatic presentation and a more advanced disease state. All patients who presented with effusive-constrictive pericarditis showed echogenic PE. Patients with initial echogenic PE developed more unresolved pericardial constrictions and required pericardiectomy despite the use of anti-TB medications, than did those with echo-free PE. In previous studies, echogenic PE was regarded as specific for TB PE,14-18) but the high prevalence of echogenic PE makes its value in TB PE patients unclear. Here we have demonstrated that echogenic PE is a predictor of constrictive pericarditis in patients with TB pericarditis.
Only some patients who initially presented with effusive-constrictive pericarditis or constrictive pericarditis required pericardiectomy during follow-up, whereas no patient without initial pericardial constriction underwent pericardiectomy. Some patients with pericardial thickening by initial CT needed pericardiectomy. Patients who present with pericardial thickening and constriction and/or echogenic PE have poor prognoses and may develop persistent constrictive pericarditis requiring pericardiectomy. TB pericarditis patients initially presenting without constriction and with echo-free PE may not develop permanent pericardial constriction nor require pericardiectomy, provided anti-TB medication is adequate.
Initial pericardial constriction and echogenic PE may reflect a more advanced disease state and a higher degree of pericardial inflammation. Symptom duration before diagnosis was greater in echocardiographically advanced patients, defined as those showing fibrinous strands and thickened pericardia,18) in agreement with our present data showing that patients with echogenic PE had been symptomatic for longer than echo-free PE patients. Patients who presented with constrictive pericarditis showed an even greater symptom duration (average 83±35 days) than did those who presented with PE. These results demonstrate that initial echocardiographic characteristics are informative with respect to both disease duration and inflammation severity. The fact that patients initially diagnosed with advanced disease are more likely to require pericardiectomy than patients with less severe illness emphasizes that TB pericarditis needs to be detected early. Timely diagnosis, followed by appropriate treatment, is essential to prevent constrictive pericarditis and pericardiectomy. We observed a beneficial effect of steroid therapy on preventing persistent pericardial constriction in patients with initial echogenic PE or constrictive physiology in the present study. However, randomized controlled study will be needed to verigy this finding, because more patients with PE were included in the steroid therapy group, whereas more patients with constrictive physiology were in the non-steroid group.
Transient pericardial constriction
We also found that 7 patients (11.7% of the total) developed transient pericardial constrictions that resolved during longer follow-up (6.3±6.3 months, range 1-18 months) with use of anti-TB medications. Data from the Mayo Clinic showed that about 17% of constrictive pericarditis patients developed transient constrictions, the common etiology being prior cardiovascular surgery, whereas only 1 case of TB pericarditis was transient.26) However, TB pericarditis seems to be a primary etiology of transient constrictive pericarditis in Korea, where TB is more prevalent than in the United States.27) The relatively high incidence of transient pericardial constrictions in TB pericarditis patients suggests observation for 6 months with adequate anti-TB medication and echocardiography follow-up, especially in patients initially presenting without overt constrictive pericarditis.
Study limitations
This study was a retrospective observational study, and hence has the limitations inherent to such studies. Not all patients met definitive TB PE diagnosis criteria. Steroid treatment was not controlled, being at the discretion of attending physicians, and this may affect the incidence of pericardial constriction and pericardiectomy. However, neither the proportions of steroid-treated patients, nor initial steroid therapy doses, differed between patient groups (Table 3 and 4). The lack of invasive catheterization data for understanding the hemodynamic aspects of disease evolution, particularly in patients with constrictive pericarditis, was another limitation of this study. Constrictive physiology determined by a significant respiratory variation in mitral inflow E wave velocity (≥25%) could have lead to false negative in diagnosing constriction, especially in patients with increased preload.28) The clinical outcomes and predictors for constriction demonstrated in this study were limited to TB pericarditis. We could not demonstrate independent determinants of outcomes using multivariate regression analysis, because no variable with statistical significance was identified, probably due to relatively small number of patients and large number of variables. Although the incidence of constrictive pericarditis in TB pericarditis was higher than in other types of pericarditis such as malignant or idiopathic pericarditis,13) further studies would be necessary to evaluate clinical outcomes and poor prognostic predictors in these specific categories.
Conclusions
In conclusion, initial echocardiographic and clinical presentations are of substantial prognostic value in patients with newly diagnosed TB pericarditis, and initial pericardial constriction and echogenic PE seem to be poor prognostic signs for persistent constrictive pericarditis and pericardiectomy. These results suggest that early TB diagnosis and prompt anti-TB therapy may be critical.
References
- 1.Zumla A, Mwaba P, Huggett J, Kapata N, Chanda D, Grange J. Reflections on the white plague. Lancet Infect Dis. 2009;9:197–202. doi: 10.1016/S1473-3099(09)70045-3. [DOI] [PubMed] [Google Scholar]
- 2.Mayosi BM, Wiysonge CS, Ntsekhe M, et al. Clinical characteristics and initial management of patients with tuberculous pericarditis in the HIV era: the Investigation of the Management of Pericarditis in Africa (IMPI Africa) registry. BMC Infect Dis. 2006;6:2. doi: 10.1186/1471-2334-6-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Syed FF, Mayosi BM. A modern approach to tuberculous pericarditis. Prog Cardiovasc Dis. 2007;50:218–236. doi: 10.1016/j.pcad.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Mayosi BM, Burgess LJ, Doubell AF. Tuberculous pericarditis. Circulation. 2005;112:3608–3616. doi: 10.1161/CIRCULATIONAHA.105.543066. [DOI] [PubMed] [Google Scholar]
- 5.Mayosi BM, Volmink JA, Commerford PJ. Pericardial Disease: an Evidence-Based Approach to Diagnosis and Treatment. 2nd ed. London: BMJ Books; 2003. [Google Scholar]
- 6.Suwan PK, Potjalongsilp S. Predictors of constrictive pericarditis after tuberculous pericarditis. Br Heart J. 1995;73:187–189. doi: 10.1136/hrt.73.2.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hageman JH, D Esopo ND, Glenn WW. Tuberculosis of the pericardium: a long-term analysis of forty-four proved cases. N Engl J Med. 1964;270:327–332. doi: 10.1056/NEJM196402132700702. [DOI] [PubMed] [Google Scholar]
- 8.Williams IP, Hetzel MR. Tuberculous pericarditis in south-west London: an increasing problem. Thorax. 1978;33:816–817. doi: 10.1136/thx.33.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Komsuoglu B, Goldeli O, Kulan K, Gedik Y. Tuberculous pericarditis in north-east Turkey: an echocardiographic study. Acta Cardiol. 1994;49:157–163. [PubMed] [Google Scholar]
- 10.Long R, Younes M, Patton N, Hershfield E. Tuberculous pericarditis: long-term outcome in patients who received medical therapy alone. Am Heart J. 1989;117:1133–1139. doi: 10.1016/0002-8703(89)90873-9. [DOI] [PubMed] [Google Scholar]
- 11.Ng TT, Strang JI, Wilkins EG. Serodiagnosis of pericardial tuberculosis. QJM. 1995;88:317–320. [PubMed] [Google Scholar]
- 12.Komsuoglu B, Goldeli O, Kulan K, Komsuoglu SS. The diagnostic and prognostic value of adenosine deaminase in tuberculous pericarditis. Eur Heart J. 1995;16:1126–1130. doi: 10.1093/oxfordjournals.eurheartj.a061057. [DOI] [PubMed] [Google Scholar]
- 13.Kim SH, Song JM, Jung IH, Kim MJ, Kang DH, Song JK. Initial echocardiographic characteristics of pericardial effusion determine the pericardial complications. Int J Cardiol. 2009;136:151–155. doi: 10.1016/j.ijcard.2008.04.033. [DOI] [PubMed] [Google Scholar]
- 14.Chia BL, Choo M, Tan A, Ee B. Echocardiographic abnormalities in tuberculous pericardial effusion. Am Heart J. 1984;107:1034–1035. doi: 10.1016/0002-8703(84)90850-0. [DOI] [PubMed] [Google Scholar]
- 15.George S, Salama AL, Uthaman B, Cherian G. Echocardiography in differentiating tuberculous from chronic idiopathic pericardial effusion. Heart. 2004;90:1338–1339. doi: 10.1136/hrt.2003.020081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ku CS, Chiou KR, Lin SL, Liu CP, Chaing HT. Echocardiographic features of tuberculous pericarditis. J Chin Med Assoc. 2003;66:613–616. [PubMed] [Google Scholar]
- 17.Liu PY, Li YH, Tsai WC, et al. Usefulness of echocardiographic intrapericardial abnormalities in the diagnosis of tuberculous pericardial effusion. Am J Cardiol. 2001;87:1133–1135. doi: 10.1016/s0002-9149(01)01481-3. [DOI] [PubMed] [Google Scholar]
- 18.Yang CC, Lee MH, Liu JW, Leu HS. Diagnosis of tuberculous pericarditis and treatment without corticosteroids at a tertiary teaching hospital in Taiwan: a 14-year experience. J Microbiol Immunol Infect. 2005;38:47–52. [PubMed] [Google Scholar]
- 19.Park SY. The usefulness of pericardial biopsy to evaluate the causes of pericardial disease. Korean Circ J. 1999;29:517–522. [Google Scholar]
- 20.Hinds SW, Reisner SA, Amico AF, Meltzer RS. Diagnosis of pericardial abnormalities by 2D-echo: a pathology-echocardiography correlation in 85 patients. Am Heart J. 1992;123:143–150. doi: 10.1016/0002-8703(92)90758-n. [DOI] [PubMed] [Google Scholar]
- 21.Oh JK, Hatle LK, Seward JB, et al. Diagnostic role of Doppler echocardiography in constrictive pericarditis. J Am Coll Cardiol. 1994;23:154–162. doi: 10.1016/0735-1097(94)90514-2. [DOI] [PubMed] [Google Scholar]
- 22.Jung HG. Respiratory variations of Doppler echocardiographic parameters in cardiac tamponade. Korean Circ J. 1998;28:412–424. [Google Scholar]
- 23.Dal-Bianco JP, Sengupta PP, Mookadam F, Chandrasekaran K, Tajik AJ, Khandheria BK. Role of echocardiography in the diagnosis of constrictive pericarditis. J Am Soc Echocardiogr. 2009;22:24–33. doi: 10.1016/j.echo.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 24.Come PC, Miklozek CL, Riley MF, Carl LV, Morgan JP. Echocardiographic changes in rapidly developing pericardial constriction. Am Heart J. 1985;109:1385–1387. doi: 10.1016/0002-8703(85)90369-2. [DOI] [PubMed] [Google Scholar]
- 25.Sinha PR, Singh BP, Jaipuria N, Rao KD, Shetty GG, Avasthey P. Intrapericardial echogenic images and development of constrictive pericarditis in patients with pericardial effusion. Am Heart J. 1996;132:1268–1272. doi: 10.1016/s0002-8703(96)90473-1. [DOI] [PubMed] [Google Scholar]
- 26.Haley JH, Tajik AJ, Danielson GK, Schaff HV, Mulvagh SL, Oh JK. Transient constrictive pericarditis: causes and natural history. J Am Coll Cardiol. 2004;43:271–275. doi: 10.1016/j.jacc.2003.08.032. [DOI] [PubMed] [Google Scholar]
- 27.Yang HS, Song JK, Song JM, et al. Clinical characteristics of constrictive pericarditis diagnosed by echo-Doppler technique in Korea. J Korean Med Sci. 2001;16:558–566. doi: 10.3346/jkms.2001.16.5.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oh JK, Tajik AJ, Appleton CP, Hatle LK, Nishimura RA, Seward JB. Preload reduction to unmask the characteristic Doppler features of constrictive pericarditis: a new observation. Circulation. 1997;95:796–799. doi: 10.1161/01.cir.95.4.796. [DOI] [PubMed] [Google Scholar]