Abstract
Heterosexually transmitted HIV remains of critical concern in the United States and around the world, especially among vulnerable and disadvantaged women, complicated by socioeconomic circumstances, gender power, addiction, and experiences of abuse, among other conditions. Effective woman-initiated HIV prevention options, such as the female condom (FC), are needed that women can use in different sexual relationship contexts. We conducted a behavioral and attitudinal survey with 461 primarily African American and Latina (especially Puerto Rican) women in Hartford, Connecticut, to measure factors on the individual, partner relationship, peer, and community levels influencing their initial and continued use of FC (using the prototype FC1) for disease prevention. We used multivariate analyses and structural equation modeling to assess effects of multiple level factors on FC use and unprotected sex with primary, casual, and paying partners. Initial, recent, and continued FC use was associated with factors on the individual level (education, marital status, drug use, child abuse experiences, HIV status), partner level (number of sex partners, paying sex partner, relationship power), and peer level (more or influential peers saying positive things about FC). Community level factors of availability and support were consistently poor across all sectors, which limited overall FC use. Patterns differed between African American and Latina women in stages and contexts of FC use and unprotected sex. FC can make a valuable contribution to reducing heterosexually transmitted HIV among women in many circumstances. The greatest barrier to increased FC use is the lack of a supportive community environment for its promotion and use.
Introduction
As the third decade of the deadly AIDS pandemic progresses, one of the most tenacious problems for HIV prevention continues to be heterosexual transmission.1,2 Heterosexual contact is by far the primary transmission route in U.S. women of all ethnicities, accounting for 75% of African American, 72% of Hispanic, and 65% of white women living with HIV/AIDS in 2007.3 Numerous interventions for women and couples have been tested to reduce heterosexual transmission, many of which have shown effective results.4–6 Yet the problem remains, and HIV incidence among women continues to increase disproportionately in certain populations, particularly U.S. ethnic minorities, low-income, and impoverished women.2,7
Reducing heterosexual transmission is complicated by the fact that it most often occurs among women and men in their childbearing years, and is exacerbated by the complex intersection of gender roles and power differentials between women and men that limit women's ability or willingness to negotiate male condoms or remain abstinent. It is also complicated by addiction, HIV, and poverty.8–10 In this context, it is essential to ensure that women have available to them more prevention methods that they can initiate and control in order to reduce the risk of HIV transmission among heterosexual couples.11
Women-initiated prevention options that offer the possibility of protection from transmission of HIV and sexually transmitted infections (STI) while at the same time addressing reproductive planning interests have significant potential to enhance women's power to further reduce their risk of infection and/or transmission.12 The most effective woman-initiated barrier method to prevent HIV and other STI as well as pregnancy is the female condom (FC), a vaginally inserted sheath worn during sex.13,14 The FC has become widely used for prevention in several developing countries with high HIV incidence.15–20 Studies around the globe have found positive results from introducing FC to women of all ages, including decreased STI incidence and increased protected sex.21,22
Despite extensive research showing its effectiveness and acceptability with various U.S. populations at highest risk, the FC remains unpopular and underutilized in most communities.11 Cost is a contributing factor. At retail, one FC can cost 2 to 10 times that of a male condom, making it prohibitive for many people at high risk who are also likely to be poor. However, studies indicate that even in resource poor areas, many are willing to purchase effective prevention options even at a notable cost,23,24 and social marketing studies of the FC indicate success at increasing purchases among clientele with more cash resources.25 Awareness and support of the FC is at least as important. Though available for over 15 years, remarkably few people are aware of the FC in the United States, including many service providers, even among those providing HIV prevention or birth planning and reproductive health services.26–28
A deeper and more systematic understanding of the factors on multiple social levels that affect women's initial and continued use of FC for HIV/STI or pregnancy prevention could increase the potential for effective promotion and support of this method in the community. These include individual level characteristics of each woman, such as her sociocultural background, experiences, and personal risk behaviors, as well as relationship level factors like the types of male sex partners and her power in those relationships, peer level influences, and the community context of health resources available to her. Recognizing the multifaceted and layered influences on FC adoption requires analysis of those factors, separately and together, as they create the context of women's understanding and use of the method. We conducted an intensive study of the multi-level factors expected to influence high-risk urban U.S. women's knowledge of, attitudes toward, and initial and continued use of FC with their male partners. This article presents analyses of those multiple factors as they affect FC use among women in Hartford, Connecticut, at risk of HIV exposure, infection, or transmission.
Methods
The Study of Sustained Female Condom Use for HIV/STI Prevention (2004–2008) included a prospective, longitudinal survey of initial and sustained FC use among 461 women recruited from Hartford, a northeastern U.S. city of approximately 119,997 residents who are primarily African American (39.1%) and Puerto Rican and other Hispanic groups (38.8%).29 The survey examined the personal demographic and HIV risk characteristics, sexual partner and gender relationship factors, social network contact and peer influences, and environmental (community) availability of FC as these affect Hartford women's initial and continued use of the FC for HIV or STI prevention. Additionally, we conducted qualitative in-depth interviews with 37 couples who tried FC for 2 weeks to explore the contextual, sexual relationship, gender dynamic, and other factors affecting their use of the method.30 We report here on data from the cross-sectional baseline survey of women as they entered the study, focusing on the multilevel complex of factors defined in our analytical model as expected to contribute to initial and continued FC use among these women. At the time of this study, only the original prototype FC1 was available.
Social ecological theory31 was the basis for the multilevel approach we took to analyze the layered, interactive domains hypothesized to affect women's initial and continued FC use for HIV/STI prevention. Social ecological theory posits that interactive change processes across social levels facilitate or constrain individual and dyadic (partner) or group (network, community) actions and opportunities. Additionally, diffusion theory32 guided our focus on interpersonal social influences affecting adoption of this relatively new prevention method. Diffusion theory postulates that adoption and normalization of a new practice is a process whereby an environment that supports the change, trustworthy change agents or sources of information and pressure for the change, and increasing presence of the practice among peers leads to application of the practice in specific contexts. Moreover, because FC use is a sexual practice that may affect reproduction, gender relations of power, sexuality, and gender roles and definitions affect the context of adopting FC for HIV/STI (or pregnancy) prevention and shape the meaning of FC use with different partners. Thus, gender theory33 framed our recognition of power dynamics between men and women as these affect women's ability to control their own and their partner's HIV risk and prevention.
The sample of women for the study was recruited through a combination of targeted street outreach, referrals from organizations that serve the target populations, and participant referral of others into the study. This adaptive sampling method34 was needed to reach both a convenience sample of women distributed across the city and representing the primary ethnic groups, and to seek hidden subgroups of women at high risk, such as drug users and commercial sex workers, in addition to women whose partners were HIV positive or illicit drug users. Any participant who referred another eligible woman into the survey received a $10 incentive, limited to no more than two referrals per participant. Upon screening for eligibility for the confidential survey (based on proof of age over 16 years old and self-reported sex with a man within the prior 30 days), women were asked to provide signed informed consent to participate in the study. After completion of the 1-hour interviewer administered baseline survey, all women received a brief demonstration of how to use FC correctly, were given four FC1 to try with their partners, were scheduled for follow-up surveys at 1 month and 10 months later, and received a $25 incentive for completing the survey. All recruitment, referral, screening, follow-up, and other study protocols and all research measures received full review and approval by an Institutional Review Board.
Key multilevel variables in the research model that comprised the content of the survey are indicated in Tables 1 and 2 and outcome measures are on Table 3. In our analytical model, we organized these variables into different levels or groupings of factors hypothesized to affect FC initial and continued use. We then conducted a series of analyses to test factors hypothesized to explain the relationships among variation in characteristics of women in the sample and key analytical constructs expected to influence their FC use and adoption.
Table 1.
Female Condom Survey Sample Characteristics of Women by Ethnic Groups (Percentages Except where Indicated Means [SD])a
| African/Black Americans (n = 256) | Puerto Ricans/other Latinos (n = 140) | Whites/other groupsb (n = 65) | Total sample (n = 461) | |
|---|---|---|---|---|
| Total sample | 55.4 | 30.4 | 14.1 | |
| Level 1a: Individual Demographic | ||||
| Mean age** | M = 40.8 (9.38) | M = 36.9 (9.27) | M = 37.4 (9.62) | M = 39.2 (9.55) |
| High school graduate** | 52.7 | 33.6 | 73.8 | 49.9 |
| >Marital status:** | ||||
| Single | 65.6 | 45.7 | 43.1 | 56.4 |
| Married/living together | 17.2 | 37.1 | 30.8 | 25.2 |
| Divorced/widowed/separated | 16.4 | 15.7 | 26.2 | 17.6 |
| Homeless (currently) | 25.0 | 31.4 | 38.5 | 28.9 |
| Level 1b: Individual HIV/STI Risk | ||||
| Substance use in last 30 days: | ||||
| Any illicit drug use | 54.3 | 62.9 | 55.4 | 57.0 |
| Alcohol use to intoxication** | 36.7 | 21.4 | 29.2 | 31.0 |
| Injection drug use** | 1.2 | 14.3 | 16.9 | 7.4 |
| Crack use | 35.5 | 32.9 | 26.1 | 33.4 |
| Polydrug use** | 15.2 | 32.9 | 24.6 | 21.9 |
| STIs: | ||||
| Past infection | 69.9 | 57.9 | 67.7 | 65.9 |
| Current symptoms | 8.1 | 12.9 | 16.9 | 10.8 |
| HIV-positive (self report) | 12.8 | 11.1 | 9.5 | 11.8 |
| Sexual/physical abuse experiences: | ||||
| Any abuse history*** | 54.7 | 76.4 | 90.8 | 66.4 |
| Childhood abuse** | 36.6 | 57.1 | 55.4 | 45.5 |
| Adulthood abuse** | 36.2 | 57.1 | 78.5 | 48.6 |
| Level 2: Partner | ||||
| Multiple sex partners (2 or more in last 30 days) | 12.9 | 9.3 | 18.5 | 12.6 |
| Sex partner types (last 30 days): | ||||
| Primary male partner | 89.5 | 92.9 | 87.7 | 90.2 |
| Casual male partner(s)* | 18.8 | 10.7 | 23.1 | 16.9 |
| Paying male partner(s) | 6.3 | 6.4 | 6.2 | 6.3 |
| Multiple partner types | 12.1 | 8.6 | 13.8 | 11.3 |
| Pregnant or trying* | 2.0 | 8.6 | 4.6 | 4.3 |
| Contraception in use (last 30 days)c | ||||
| Nothing | 36.3 | 39.3 | 43.1 | 38.2 |
| Sterilization | 22.7 | 29.3 | 18.5 | 24.1 |
| Hormones (pill/shot/patch/subdermal) | 7.0 | 5.0 | 3.1 | 5.9 |
| Condoms (male or female) | 32.0 | 24.3 | 33.8 | 29.9 |
| Current partner abuse** | 2.8 | 10.0 | 13.8 | 6.5 |
| Primary partner FC refusal (last 30d) | 1.3 | 2.3 | 0 | 1.5 |
| Level 3: Peer/Network | ||||
| # in network who talked about FC | M = 1.16 (1.24) | M = 1.60 (1.56) | M = 0.94 (1.04) | M = 1.26 (1.34) |
| Influential person said + about FC | 53.9 [n = 89] | 57.0 [n = 53] | 52.6 [n = 20] | 54.7 [n = 162] |
| Influential person said − about FC | 0.6 [n = 1] | 10.8 [n = 10] | 0 | 3.7 [n = 11] |
| Perceived FC peer norms (scale)d | M = 0.95 | M = 1.01 | M = 0.77 | M = 0.95 |
| Level 4: Environment | ||||
| FC users who got all FC free | 96.0 [n = 25] | 87.5 [n = 16] | 66.7 [n = 3] | 90.9 [n = 44] |
p Values refer to differences by ethnicity.
Other ethnic groups included 0.4% Native American (n = 2), 0.2% Asian (n = 1), 1.5% mixed/other (n = 7).
Thirteen sterilized women also reported using MC or FC for contraception, as did 6 women using hormonal contraception. Condom users for contraception included 119 who used only MC, 5 who used only FC, and 16 who used both FC and MC.
Three-item scale: 0 = very unlikely; 1 = somewhat likely; 2 = somewhat unlikely; 3 = very unlikely; higher score indicates more positive peer norms regarding FC.
p < 0.05.
p < 0.01.
p < 0.001.
FC, female condom; MC, male condom; SD, standard deviation.
Table 2.
Gender Power Attitudes and Female Condom Knowledge and Attitudes in the Survey Sample of Women by Ethnic Groups: Means (SD)a
| African/Black Americans (n = 256) | Puerto Ricans/other Latinos (n = 140) | Whites/other groups (n = 65) | Total sample (n = 461) | |
|---|---|---|---|---|
| Partner relationship scalesb | ||||
| Decision-making dominance** | 1.20 (0.41) | 1.10 (0.35) | 1.05 (0.42) | 1.15 (0.40) |
| Relationship power | 2.90 (0.36) | 2.89 (0.48) | 2.92 (0.52) | 2.90 (0.42) |
| Female condom knowledge (score)c** | .80 (0.21) | 0.68 (0.21) | 0.73 (0.73) | 0.75 (0.22) |
| Female condom beliefs/attitudes:d | ||||
| All scale items | 2.80 (0.29) | 2.80 (0.31) | 2.78 (0.25) | 2.80 (0.29) |
| Subscale: HIV/STI prevention* | 3.26 (0.42) | 3.35 (0.44) | 3.39 (0.45) | 3.31 (0.43) |
| Subscale: Compared to MC | 2.80 (0.52) | 2.89 (0.50) | 2.72 (0.53) | 2.81 (0.52) |
| Subscale: FC insertion | 2.80 (0.46) | 2.76 (0.52) | 2.78 (0.50) | 2.78 (0.48) |
| Subscale: effects on sexual pleasure | 2.76 (0.33) | 2.77 (0.38) | 2.74 (0.30) | 2.76 (0.35) |
| Subscale: FC appearance | 2.57 (0.42) | 2.49 (0.46) | 2.50 (0.42) | 2.53 (0.43) |
| Item: FC puts woman in charge** | 2.89 (0.74) | 2.65 (0.71) | 2.82 (0.66) | 2.80 (0.73) |
| FC self-efficacy:e | ||||
| With primary partner | 2.11 (0.72) [n = 248] | 2.17 (0.76) [n = 137] | 2.16 (0.72) [n = 64] | 2.14 (0.73) [n = 449] |
| With casual partner | 2.37 (0.73) [n = 72] | 2.17 (0.89) [n = 44] | 2.44 (0.51) [n = 20] | 2.31 (0.76) [n = 136] |
| With paying partner | 2.30 (0.92) [n = 32] | 1.98 (0.98) [n = 21] | 2.19 (0.71) [n = 7] | 2.18 (0.92) [n = 60] |
| Internal STI locus of controlf | 3.09 (0.77) | 3.15 (0.87) | 3.11 (0.81) | 3.11 (0.81) |
| Perceived HIV riskg* | 0.45 (0.80) [n = 226] | 0.74 (1.0) [n = 125] | 0.61 (0.83) [n = 59] | 0.56 (0.88) [n = 410] |
p Values refer to differences by ethnicity.
Decision-making dominance is a 7-item scale (responses: 0 = your partner; 1 = both of you equally; 2 = you; α = 0.765). Relationship power is a 15-item scale (range 1–4, higher is more power; inverted questions were reverse coded; α = .887).43,44
Percent correct of 6 items.45
FC attitudes were measured using a 26-item scale (range 1 = strongly unfavorable to 4 = strongly favorable; α = 0.849); subscales include: effects on sexual pleasure [8 items, α = 0.70], FC appearance [4 items, α = 0.568], value of FC for STI/HIV prevention [3 items, α = 0.742], FC insertion [4 items, α = 0.751], and FC in comparison with MC [5 items, α = 0.814]; item 14 [FC puts women in charge]).46
FC efficacy (perceived ability to use) was measured with a 6-item scale (range 0 = very unsure to 3 = very sure: with primary partner [α = 0.737], with casual partners [α = 0.852], with paying partners [α = 0.912]).
We report here on a single item: “It is my own behavior that determines if I will get an STI” (range 1 = strongly disagree to 4 = strongly agree).
Perceived risk of HIV infection was a single item (range 0 = very unlikely to 3 = very likely; HIV-positive participants were excluded).
p < 0.05.
p < 0.01.
FC, female condom; STI, sexually transmitted infection; SD, standard deviation.
Table 3.
Initial and Recent Female Condom Use and Stages of Female Condom Adoption in the Survey Sample of Women by Ethnic Groups (percentages)a
| African/Black Americans (n = 256) | Puerto Ricans/other Latinos (n = 140) | Whites/other groups (n = 65) | Total sample (n = 461) | |
|---|---|---|---|---|
| Ever seen FC before today* | 79.3 | 72.1 | 66.2 | 75.3 |
| Ever used FC during sex | 30.1 | 29.3 | 21.5 | 28.6 |
| Use FC during sex in last 30 days | 8.2 | 10.0 | 3.1 | 8.0 |
| Stage of FC Use (last 6 months)b: | ||||
| FC nonusers: | 88.7 (n = 227) | 82.6 (n = 114) | 89.2 (n = 58) | 86.9 (n = 399) |
| 0—Never thought about it | 66.4 | 56.5 | 69.2 | 63.8 |
| 1—Thought about but didn't use it | 18.8 | 18.8 | 20.0 | 19.0 |
| 2—Used it once then never again | 3.5 | 7.2 | 0 | 4.1 |
| FC users: | 11.3 (n = 29) | 17.4 (n = 24) | 10.8 (n = 7) | 13.1 (n = 60) |
| 3—Use it occasionally | 5.5 | 8.7 | 6.2 | 6.5 |
| 4—Use regularly | 2.3 | 4.3 | 1.5 | 2.8 |
| 5—Use as a primary method | 3.5 | 4.3 | 3.1 | 3.7 |
| Any unprotected sex in last 30 daysc: | 60.5 | 65.7 | 70.8 | 63.6 |
| With primary partner | 64.2 (of 229) | 65.4 (of 130) | 78.6 (of 57) | 66.5 (of 416) |
| With casual partner(s) | 33.3 (of 48) | 26.7 (of 15) | 26.7 (of 15) | 30.8 (of 78) |
| With paying partners | 12.5 (of 16) | 66.7 (of 9) | 50.0 (of 4) | 34.5 (of 29) |
| Use MC during sex in last 30 days | 54.3 | 57.1 | 47.7 | 54.2 |
p Values refer to differences by ethnicity.
Two cases were missing. Percents at each stage are of the total reported in that column.
Numbers in parentheses indicate those who reported having that type of partner.
p < 0.05.
FC, female condom; MC, male condom.
In this article, we first describe the total sample and the two primary ethnic subpopulations (African Americans and Latinas), and their responses regarding each of the sets of variables in the model. Ethnic identity often reflects significant cultural beliefs and deep meaning around issues of sexuality and gender roles, which in turn affect sexual practices in heterosexual relationships.10,35 We expected that these differences would result in significant variation in personal and social contexts in which FC would be accepted and used.
Following this descriptive comparison, we report on associations among key variables in the model for the total sample, and explore specific differences among the ethnic subgroups. We then report on multiple regression analysis conducted to look at relationships within and between “levels” of the significant factors identified in correlational analyses in order to refine the model. Finally, we explore more deeply the relationships among multilevel factors using structural equation modeling (SEM) to further refine the model and identify pathways to initial and continued FC use. SEM simultaneously tests specified causal paths between variables,36 while allowing flexible modeling of the unexplained covariances between variables in the model. Our outcomes of interest in the correlations tests and analyses of variance included initial, current, and stage of FC use, and in the multiple regression and SEM analyses, included only stage of FC use, ranging from nonuse (pre-contemplation), to initial trial use, to continued intermittent or regular use.
Results
Descriptive characteristics of the study sample and FC users
Table 1 describes the general sample characteristics, specified by the three primary ethnic groups and their responses on key variables in the multi-level model. Most of the women in the study were African American or Latino (primarily Puerto Rican). Demographically (Level 1a), participants differed significantly by ethnicity in age, educational attainment and marital status, with African American women on average being older and more likely to be single and Latinas most likely to be married and least likely to have a high-school degree.
Most women in the study indicated generally high potential risk for exposure to HIV related to drug use or health history (Level 1b). The majority reported illicit drug use within the prior thirty days, including crack use, injected drugs, or multiple illicit drugs, as well as alcohol to the point of getting drunk. Differences by ethnicity were significant for alcohol intoxication, injected drug use, and polydrug use. A history of STI was also extremely high, and nearly 12% of all women reported current STI or HIV infection. Also notable were the extremely high reported rates of a history of physical or sexual abuse, either as children (below age 16) or as adults, especially among whites and Latinas.
Variation in types of sex partners and male partner relationships (Level 2) also indicated potential risk for some women, including having multiple or paying partners in the prior month. Few women indicated interest in getting pregnant (more Latinas than others), yet few used dual protection via male condoms (MC) (29.3%) or FC (4.6%). Many reported using either no contraception or nonbarrier methods such as hormones or sterilization. In this study, we did not ask about FC use during anal sex. Few women in the study reported anal sex in the prior 30 days with any type of sex partner, including 36 (8.7%) of the 416 women with primary partners, 7 (9.0%) of the 78 women with casual partners, and 2 (6.9%) of the 29 women with paying partners. However, MC use during anal sex was inconsistent, particularly with primary partners. A small but notable proportion reported currently being in an abusive relationship (more Whites and Latinas). Also at the partner level, decision-making dominance in women's relationships with male partners (reported in Table 2) varied significantly by ethnicity (African Americans scoring highest), but differences by ethnicity in relationship power were not significant.
Level 3 measures of peer effects indicated that most study participants have at least one person in their network (including friends, partners, family members, acquaintances, medical or social service providers, or others) who had spoken to them previously about FC, either positively or negatively. More than half indicated that the person had said positive things about FC and was someone they considered to influence them. Notably, of the 296 women who had a network member talk to them about FC, 93.6% reported that the person had said something positive; of those 75% had said only positive things, and another 18.6% had said both positive and negative things about FC. Also importantly, 80% of FC users (defined as having used FC at least occasionally in the last 6 months) reported that they had an influential network member say positive things to them about the FC.
We initially included community environment variables of FC sources and availability as Level 4 factors affecting women's initial and continued FC use. However, we dropped these factors from our bivariate and multivariate analyses because we found virtually no variation in these measures within the sample. Community assessments we conducted every 6 months as part of this study to document locations where FC could be purchased or acquired for free indicated little availability across the city, virtually no promotion by clinics or pharmacies, and very little promotion by social and health service organizations. This universal condition across the city may explain the difficulty of finding any variability in the Level 4 factors, such as sources of FC and use of free FC. However, among the women who reported ever getting FC (n = 236), 48.3% indicated clinics were the most common source, followed by community outreach workers (32.6%), “other places” (22.5%), drug treatment programs (15.3%), and AIDS service organizations (11.9%). A number of women who indicated “other places” reported that FC were included in a package upon their release from jail or prison. Notably, nearly all of the women who had used FC in the prior 30 days (97.3%) got all of their FC for free. It is important to note that 83.9% of these FC users also got all of their MC for free, and 77.5% of MC users got all of their MC for free. Although we did not ask specifically about access to free FC, users appeared to have access to and use health and social services where free FC were provided.
Some differences by ethnicity were evident in the hypothesized cognitive influences on potential FC use and adoption, including FC knowledge and attitudes and other health related attitudes (Table 2). Scores showed that women's knowledge about FC was modest, with Latinas scoring lowest. Few differences were evident in FC attitudes by ethnic groups, averaging generally favorably in all groups. Among the subscales of FC attitudes, women felt most positively about the FC as an HIV/STI or pregnancy prevention method, and also in comparison to MC. The average response was somewhat less positive with regard to effects of the FC on sexual pleasure, and many did not like the appearance of the FC. Notably, on the responses to a single item in the scale regarding the value of FC for women's HIV prevention empowerment (“female condoms put the woman in charge”), over two thirds responded that they agreed (53.9%) or agreed strongly (15.0%), with significantly more African American women agreeing than Whites or Latinas. Regarding FC self-efficacy with specific types of sex partners, women generally felt somewhat sure of their ability to negotiate and use FC with their primary, casual, and/or paying male partners, though overall less so with primary partners than casual. Most women in all ethnic groups (85.2%) felt strongly that they control whether or not they will get an STI (high internal locus of control). Latinas were significantly more likely to perceive themselves at risk for HIV infection than the other groups.
Regarding the outcome variables of FC exposure, initial use and adoption (Table 3), the majority of women said they had seen the FC before entering this study, though significantly fewer whites reported this. However, less than a third of all women said they had ever used it, and only 37 women had used it in the 30 days prior to this survey. In the stages of FC adoption, the majority said they had never thought about using it, possibly because of lack of exposure (34.6% were not familiar with FC and 24.7% said they had never seen it), and nearly one fifth reported having thought about using it or gotten it, but had not used it. Latinas were more likely to have tried the FC and then never used it again, but were also more likely than others to have used it occasionally, regularly, or as their primary prevention method. However, of the 60 women who reported having used the FC at all in the prior 6 months (13.1% of the total sample), half of them use it either regularly (21.7%) or as their primary HIV/STI prevention method (28.3%; not shown on the table). Although differences by ethnicity were not significant, African American FC users were most likely to use FC as the primary method (31.0% of users), followed by white women (28.6% of users), then Latinas (25.0% of users). We also looked at MC use and overall unprotected sex in the prior 30 days and found high rates of unprotected sex across all ethnic groups and with all types of partners, and only modest use of MC.
We compared the group of FC users (i.e., women who reported using FC occasionally, regularly or as a primary method) with nonusers (those who had never thought about using it, thought about or got it but didn't use it, or used it once but never again; Table 4). Demographically (Level 1a) FC users were significantly more likely than nonusers to be high school graduates, less likely to be single or married, and more likely to be separated, divorced, or widowed. However, differences in use by age groups were not significant. In terms of health risks (Level 1b), more non-FC users had used drugs or alcohol in the prior 30 days. The two groups were not different in terms of STI history or HIV serostatus, but more FC users reported a history of childhood physical or sexual abuse. In relationship and partner characteristics (Level 2), FC users differed from nonusers only in their scores on relationship power. However, differences in peer influences (Level 3) were more notable, with FC users reporting more people in their networks who talked to them about FC, higher reported rates of having at least one influential peer who talked to them positively about FC, and more positive peer FC norms. All cognitive measures also differed significantly between FC users and nonusers. Furthermore, we found that FC users were less likely than nonusers to have had any unprotected sex in the prior 30 days and particularly with primary partners, although differences were not significant in unprotected sex with casual or paying partners. FC users were also more likely than non-FC users to have used MC in the prior 30 days, suggesting that they are better condom users overall.
Table 4.
Multilevel Differences Between Female Condom Users and Female Condom Nonusers (Percentages except where indicated Mean [SD])a
| FC Usersb(n = 60) | FC Nonusersb(n = 399) | |
|---|---|---|
| Total Sample | 13.1 | 86.9 |
| Level 1a: Individual Demographic | ||
| Age group | ||
| 16–24 (n = 50) | 12.1 | 3.3 |
| 25–44 (n = 277) | 60.1 | 63.3 |
| 45+ (n = 131) | 27.9 | 33.3 |
| High school graduate** | 65.0 | 47.6 |
| Marital status*: | ||
| Single | 50.0 | 57.6 |
| Married/living together | 18.3 | 26.1 |
| Divorced/widowed/separated | 31.7 | 15.3 |
| Level 1b: Individual HIV/STI Risk | ||
| Any substance use in last 30 days* | 51.7 | 63.7 |
| STI history (ever diagnosed) | 61.7 | 63.2 |
| HIV-positive (self report) | 16.7 | 10.0 |
| Physical/sexual abuse history: | ||
| Ever experienced abuse* | 76.7 | 64.7 |
| Childhood abuse*** | 65.0 | 42.3 |
| Level 2: Partner | ||
| Multiple sex partners ≥2 in last 30 days | 20.0 | 11.5 |
| Relationship power (scale)* | M = 3.04 (0.46) | M = 2.88 (0.41) |
| Level 3: Peer/Network | ||
| # in network who talked about FC (avg.)*** | M = 1.88 (1.33) | M = 1.17 (1.32) |
| Influential person said + about FC** | 79.6 | 49.2 |
| Perceived FC peer norms (scale)*** | M = 1.44 (1.08) | M = 0.87 (0.88) |
| Cognitive Influences | ||
| FC knowledge (score)** | M = 0.78 (0.18) | M = 0.75 (0.23) |
| FC beliefs/attitudes (scale)*** | M = 2.95 (0.31) | M = 2.77 (0.28) |
| FC self-efficacy: primary partner (scale)** | M = 2.39 (0.66) | M = 2.10 (0.73) |
| Internal STI locus of control (scale)*** | M = 3.43 (0.77) | M = 3.06 (0.80) |
| Unprotected Sex (last 30 days)*** | 31.7 | 68.2 |
| With primary partners*** | 30.4 | 72.0 |
| With casual partners | 33.3 | 30.4 |
| With paying partners | 28.6 | 36.4 |
| MC use in last 30 days*** | 85.0 | 49.6 |
p Values refer to differences by FC use/nonuse.
FC users include those who reported using FC occasionally, regularly, or as their primary prevention method; FC nonusers include those who never thought about using it, thought about it but did not use it, or used it once and then never again.
p < 0.05.
p < 0.01.
p < 0.001.
FC, female condom; MC, male condom; STI, sexually transmitted infection; SD, standard deviation.
We examined reasons for FC nonuse by asking women if they had had sex without an FC in the prior 30 days with each type of partner (primary, casual, paying) because: (1) that partner had refused, (2) she was uncomfortable asking that partner to use it, or (3) she did not want to use it herself. Very few women indicated partner refusal, whether with primary partners (n = 6; 1.5%), casual partners (n = 1; 1.3%), or paying partners (n = 0), or her own discomfort with asking her primary partner (n = 6; 1.5%), casual partner (n = 3; 3.8%), or paying partners (n = 4; 13.8%). Thus, although partner FC refusal may be important, small numbers of active FC users who reported it in this study precluded our inclusion of this factor in subsequent analyses. More women indicated they had had sex without FC in the prior month because of their own preference not to use one with primary partners (n = 143 [34.6%]), with casual partners (n = 28 [35.9%]) and with paying partners (n = 4 [13.8%]). Reported preference not to use FC with primary partners in the prior month varied by ethnicity (p = 0.001); African Americans were more likely to report this (n = 95; 41.7%) than whites (n = 19; 33.3%) or Latinas (n = 29; 22.7%).
Associations among variables in the analytical model
We obtained Pearson correlations (for continuous measures) and Spearman's ρ (for ordinal measures) to test associations between each of the predictors (Levels 1–3), hypothesized mediators (cognitive measures), and the behavioral outcomes of ever used FC, current (past 30 day) use of FC, and the 5-category stages of FC use (nonuse to regular use; Table 5). Additionally, we evaluated these associations separately for African Americans and Latinas to determine whether the patterns were different in these subgroups.
Table 5.
Associations between Female Condom Use and Multilevel Influences (n = 461)a
| Ever used FC (132 = yes; 28.6%) | Used FC in the last 30 days (37 = yes; 8.0%) | Stage of FC useb | |
|---|---|---|---|
| Level 1a Predictors: Demographic | |||
| Homeless | −0.054 | −0.065 | −0.037 |
| Being African American | 0.036 | 0.007 | −0.068 |
| Being Latina | 0.010 | 0.048 | 0.115* |
| Education level | 0.111* | 0.024 | 0.115* |
| Being single | 0.015 | −0.014 | −0.014 |
| Being married/living as married | −0.102* | −0.079 | −0.083 |
| Being separated/divorced/widowed | 0.111* | 0.115* | 0.112* |
| Level 1b Predictors: HIV Risk | |||
| Any illicit drug use in last 30 days | −0.042 | −0.066 | −0.004 |
| Injection drug use in last 30 days | −0.087 | −0.083 | −0.017 |
| Crack use in last 30 days | 0.009 | −0.006 | −0.006 |
| Ever experienced any abuse | 0.061 | 0.041 | 0.121** |
| Ever experienced child abuse | 0.081 | 0.051 | 0.159** |
| Level 2 Predictors: Partners | |||
| Had multiple sex partners in last 30 days | 0.078 | −0.064 | 0.121** |
| Had primary male partner in last 30 days | −0.002 | 0.016 | 0.084 |
| Had casual male partner in last 30 days | 0.034 | −0.069 | −0.019 |
| Had paying male partner in last 30 days | 0.053 | −0.044 | 0.095* |
| Had multiple partner types in last 30 days | 0.078 | −0.080 | 0.108* |
| Relationship power | 0.073 | 0.143** | 0.123** |
| Decision-making dominance | 0.037 | 0.054 | 0.038 |
| Level 3 Predictors: Peers/Network | |||
| Number of people talking about FC ever | 0.220** | 0.141** | 0.261** |
| Influence of 1st person mentioned who talked to them about FC | −0.167** | −0.221** | −0.214** |
| Influence of 2nd person mentioned who talked to them about FC | −0.129 | −0.317** | −0.213* |
| Perceived peer norms about FC | 0.158** | 0.231** | 0.218** |
| Cognitive Factors | |||
| FC knowledge | 0.190** | 0.122** | 0.018 |
| FC beliefs | −0.094* | −0.218** | −0.216** |
| Self efficacy w/primary partner | 0.105* | 0.122** | 0.154** |
| Self efficacy w/casual partner | 0.072 | 0.134 | 0.061 |
| Self efficacy w/paying partner | 0.117 | 0.126 | 0.006 |
| Internal locus of control | 0.101* | 0.090 | 0.152** |
| Perceived HIV risk | −0.064 | −0.077 | 0.007 |
| Behavioral Outcomes | |||
| Used FC in last 30 days | 0.466** | ||
| Stage of FC use [5 items] | 0.545** | 0.474** | |
| Any unprotected sex in last 30 days | −0.228** | −0.224** | −0.223** |
| Unprotected sex: Primary partner last 30 daysc | −0.232** | −0.253** | −0.276** |
| Unprotected sex: Paying partner last 30 daysd | −0.268 | −0.137 | −0.093 |
| Used MC in last 30 | 0.254** | 0.175** | 0.265** |
Pearson's r is shown, except for associations with ordinal variables, where Spearman's ρ is reported, including for ever used FC and used FC in the last 30 days.
Stages of FC use (prior 6 months) in these analyses included: 0 = never thought about it; 1 = thought about or got it but didn't use it; 2 = tried it once but decided not to use it again; 3 = use it occasionally; 4 = use it regularly or as primary prevention method.
Includes only participants who reported having primary partners (n = 416).
Includes only participants who reported having paying partners (n = 29).
p < 0.05.
p < 0.01.
FC, female condom; MC, male condom.
Boldface values are significant at p < 0.05 or less.
Investigating associations between FC outcomes and demographic characteristics (Level 1a) showed that marital status (i.e., ever having been married) and education were associated with past FC use, but only being separated, divorced, or widowed was associated with current FC use. However, education level and being Latina were associated with stage of FC use. Differences in these associations between the two primary ethnic groups were also notable (not shown in Table 5). While high school attainment among African Americans was positively associated with initial FC use (r = 0.177, p < 0.01) and stage of FC use (r = 0.139, p < 0.01), it was not associated with these measures among Latinas. Also, being single was associated with recent FC use and stage of FC use only among African Americans (r = −0.143, p < 0.05 and r = −0.130, p < 0.05, respectively). Even more notable ethnic differences were evident in the association between marital status and ever having used FC, which was highest among single Latinas (r = 0.229, p < 0.01) and lowest among single African Americans (r = −0.153, p < 0.05).
Correlating FC initial, current, and stage of use with personal risk factors (Level 1b) indicated few significant associations (Table 5). Only a history of abuse and particularly having experienced childhood sexual or physical abuse were correlated with higher stage of FC use. When tested separately, this pattern was evident among African American women (r = 0.148, p < 0.05 for history of abuse, and r = 0.204, p < 0.01 for childhood abuse), but not among Latinas.
Several partner relationship (Level 2) variables were associated with stage of FC use, including having multiple sex partners, paying partners, multiple types of sex partners, and high relationships power. Having a paying male partner was also positively associated with higher stage of FC use among African American women (r = 0.133, p < 0.05) but not among Latinas. Similarly, having more sex partners was positively associated with higher stage of FC use among Latinas (r = 0.179, p < 0.05), but not among African American women. Further, while relationship power was associated with last 30 day FC use in the total sample, this was only evident among African American women (r = 0.147, p < 0.05), not Latinas, when analyzed separately. Notably, decision-making dominance was not associated with any FC outcome variables.
Peer factors (Level 3) were also highly correlated with FC use. Both the number of people in their networks talking about FC and having an influential peer talking positively or negatively about FC were associated with ever having used FC, current FC use, and stage of FC use. (As indicated above and in Table 1, the majority of peers talking about FC were saying positive things.) Latinas also demonstrated this pattern, but not African American women when analyzed separately. Positive FC peer norms were also associated with all FC use measures in the total sample; this association was not significant among Latinas, but was significant among African American women (r = 0.212, p < 0.01) when analyzed separately.
Cognitive factors in our model also correlated with FC use. In particular, greater FC knowledge, more positive FC attitudes, greater efficacy with primary partners, and greater internal STI locus of control were associated with FC use, particularly with primary sex partners. Several of these measures varied by ethnicity. For example, FC knowledge was positively correlated with current FC use among African Americans (r = 0.147, p < 0.05), but not among Latinas. Efficacy to use FC with primary partners correlated with all FC use measures among African American women (r = 0.212, p < 0.01 for ever used; r = 0.190, p < 0.01 for past 30 day use; r = 0.229, p < 0.01 for stage of FC use), but not for any of these measures among Latinas.
We also found that FC use measures correlated with unprotected sex, particularly showing less unprotected sex in the last 30 days in association with FC use, especially with primary partners. However, FC use measures were not associated with unprotected sex with paying or casual partners. Notably, when analyzed separately by ethnicity, this association was only evident for African Americans, though among Latinas ever having used FC and stage of FC use were associated with unprotected sex with paying partners (r = −0.791, p < 0.05 and r = −0.688, p < 0.05, respectively).
To further refine our analyses of these multilevel factors, we explored the explanatory power of variables on each of the analytical levels, both grouped and as key individual factors in a causal model. We conducted multiple regression with four stepwise blocks reflecting the four levels of predictors to examine the differential percentage of variance accounted for by groups of variables from the personal (Levels 1a and 1b), partner (Level 2), peer (Level 3), and cognitive domains as they explain the dependent variable stage of FC use (Table 6). After controlling for the Level 1a and 1b effects (block 1 in the regression analyses), FC stage of use scores indicated a weak potential association (p = 0.10) with having a paying male partner and relationship power with primary partners; having a paying partner became significant (p < 0.01) when nonsignificant factors were removed in subsequent regressions (block 2). Further, peer factors were also significant in predicting FC stage of use (block 3). Likewise, FC attitudes and internal locus of control were significant in predicting stage of FC use (block 4). The changes in explained variance (R2) between each model and the subsequent model with an additional predictive block entered were all significant at p < 0.001. The percentage of variance accounted for by this model was 25.8%, and the overall model significantly predicts stage of FC use (F13,280 = 8.84, p < 0.001).
Table 6.
Summary of Multiple Regression Analyses for Variables Predicting Stage of Female Condom Use (n = 461)a,b
| B | Sig. | |
|---|---|---|
| Block 1 | ||
| Ethnicity (Whites/others, reference group) | ||
| Latina | 0.15 | 0.09 |
| African American | 0.05 | 0.58 |
| Graduated from high school | 0.14 | 0.01* |
| Marital status (married/living as married, reference group) | ||
| Single | 0.07 | 0.27 |
| Separated, divorced or widowed | 0.16 | 0.02* |
| No drugs or alcohol abuse in the last 30 days | 0.04 | 0.50 |
| Crack use in last 30 days | 0.03 | 0.60 |
| Ever had an STI (excluding Hepatitis) | 0.09 | 0.12 |
| HIV positive | 0.20 | 0.01* |
| Experienced childhood sexual or physical abuse | 0.17 | 0.00* |
| Block 2 | ||
| Had a paying male partner in last 30 daysc | 0.14 | 0.09 |
| Relationship power | 0.10 | 0.09 |
| Primary partner FC refusal in last 30 days | 0.03 | 0.66 |
| Had multiple sex partners in last 30 days | 0.04 | 0.60 |
| Block 3 | ||
| Number of people in network talking about FC | 0.11 | 0.08 |
| Has influential peer talking positively about FC | 0.15 | 0.01* |
| FC peer norms | 0.14 | 0.02* |
| Block 4 | ||
| FC knowledge | 0.05 | 0.42 |
| FC beliefs/attitudes | 0.16 | 0.01* |
| FC self-efficacy with primary partner | 0.06 | 0.35 |
| Internal STI locus of control | 0.12 | 0.04* |
| Perceived HIV risk | −0.13 | 0.13 |
R2 = 0.128 for Block 1; R2 = 0.195 for Block 2; R2 = 0.278 for Block 3; R2 = 0.327 for Block 4.
Change in R2 was significant from each block to the next (p < 0.001 for Blocks 1 to 2, Blocks 2 to 3, and Blocks 3 to 4).
Having a paying male partner became significant (p < 0.01) after non-significant items in the table were removed for final regression.
p < 0.05.
Boldface values are significant at p < 0.05 or less.
Italicized values are significant at p < 0.10 but p > 0.05.
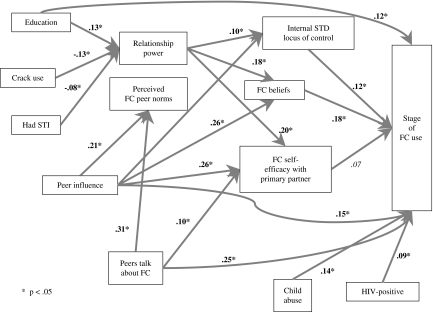
These analyses highlight the primary factors at each level that suggest multiple influences on initial and continued FC use among women in the study. However, this complex picture is better understood using a method to identify which factors combine to produce greater or lesser FC use and under which circumstances different women are likely to want or use FC for HIV/STI prevention. Figure 1 illustrates findings of structural equation modeling (SEM) analyses we conducted with the variables identified in our model as significant for FC initial and continued use, using the total sample. We report here only the structural part of SEM single occasion models,37 i.e., the results of path analyses performed in AMOS 16 38 for models with total scores as observed variables. The initial model of the hypothesized theoretical relations has been re-specified after exclusion of non-significant paths and variables not contributing to explaining variance in the main outcome, and inclusion of covariances between exogenous variables that were suggested by modification indices.
FIG. 1.
Structural equation model of multilevel influences on stage of female condom use.
Model fit for the final model reported was very good, according to main fit statistic, χ2 (nonsignificant), as well as other fit indices that can be considered in evaluating fit (e.g., comparative fit index [CFI] and root mean square error of approximation [RMSEA]).39 We report here the standardized β coefficients. We found significant direct effects on FC use from education, childhood abuse, HIV-positive status, peer influence, peers talking about FC, sexually transmitted disease (STD) locus of control, FC beliefs, and FC self-efficacy (Fig. 1).
Discussion
The question of who uses FC and under what circumstances is complex and shaped by multiple individual, relationship, peer, and community factors. Women's social contexts, cultural and personal beliefs, life cycle stage, personal history, and immediate social influences, as well as environmental context of risk or support for prevention, all contribute to the likelihood that women and their male partners will consider, try, and adopt FC as a viable prevention method.
In our study of multilevel factors influencing initial and continued FC use, we found conditions on each of the levels that contributed to women's use of FC with their male partners. Our analyses revealed that characteristics of women associated with FC use included being HIV positive, having more education, and having a greater sense of power in heterosexual relationships. By contrast, age did not appear to have any significant bearing on FC use; women of any age group were as likely (or unlikely) to use FC as any other. Other context factors associated with FC use included being separated, widowed, or divorced (but not single or married), having multiple or paying sex partners, and having positive peer or network influences supporting FC use. Though it appears counterintuitive, a history of abuse, especially childhood abuse, was also associated with FC use; however, this may reflect the significance of prior physical and sexual abuse among women with substance abuse problems. These women are also the primary target populations of services and programs that provide free FC to their clientele, thereby reducing barriers to access. Positive attitudes toward FC were expectedly associated with greater use; however, many FC users indicated dislike for the product, but willingness to use it for desired prevention. Few women reported partner resistance as a reason for nonuse; more expressed their own reluctance to use the product, though women who overcame the challenge of initial use of the product appeared willing to encourage their partners to use it.
While ethnicity did not appear as a strong predictor of FC use taken alone, comparison of African American and Latina women in Hartford suggested that different patterns of personal, relationship, and peer dynamics influence their FC attitudes, decision making, and practices. This may be explained by cultural beliefs and gender relationship expectations of women and men in these groups, or other within group conditions that affect these women. These patterned differences suggest the need to tailor or specify messages in FC promotion and support among different ethnic groups.
Other factors in women's past and current circumstances besides ethnicity, such as those indicated above, appeared to have had more significant influence on their views of FC and their preferences and sense of ability to use it than their ethnicity. These influences cannot be assumed a priori. Each person's constellation of personal characteristics (current drug and alcohol use, physical or sexual abuse history, education level, age), relationship context (partner influences, power), and partner types (e.g., spouse, noncommitted, or commercial) shape the specific encounters in which she or her partner might attempt to use and succeed in using FC. This suggests the need to make FC as readily available and commonly known as MC, so that when it is needed or desired, both women and men can access and incorporate it into their sexual practices and their risk prevention routines. The potential value, and apparent acceptability, of FC for women who have experienced abuse especially as a child is noteworthy. Greater availability and support for this effective woman-initiated prevention option may be particularly important for this highly vulnerable group.
As a relatively new product (approximately 15 years on the market), and like many innovations not broadly promoted nor well known, FC are slow to move into the public consciousness and become a standard recognized prevention option.28 Also like other innovations, the degree to which FC is increasingly adopted is affected by the presence of influential advocates for its use and peer encouragement to adopt it. From this perspective, it is not surprising that perceived positive FC peer norms and presence of an influential peer talking positively about FC appeared to be strong determinants of initial and long-term use.
While relatively few women in this study reported anal sex with any type of partner, those who did were inconsistent in their use of MC on these occasions. Some preliminary research has been conducted on FC use during anal sex among men who have sex with men (MSM).40 Although users reported several problems with FC use during anal sex, including pain, discomfort, and even rectal bleeding, men in some contexts, especially those with HIV-positive sex partners, reported more protected sex than those using MC alone. Further research is warranted on the safety, benefits, and acceptability of FC use during anal sex to increase protected encounters among both MSM and heterosexual couples.
An important consideration is the implications of these findings for application to understanding the potential for other woman-initiated HIV/STI prevention options, like vaginal microbicides. Lessons learned from a deeper understanding of the complex interaction of multilevel influences on women's initial and continued use of the FC could inform the targeting of efforts to test and roll out other new products currently in clinical trials. Thus, attention to these multilevel influences may be additionally beneficial for further expanding the array of options from which women and men can choose for prevention that suit their preferences and particular circumstances.
In this single-city study design, there was little variation in community level factors that might differentially influence women's use of FC; we therefore had limited ability to include community level factors in our analyses. Clearly, community context, particularly the almost universal lack of support, availability, and promotion of FC, was a contributor to nonuse. This was suggested by overall low levels of FC knowledge and awareness in the study population, and the clear association between FC use and availability of free FC. Thus, although women have found FC from a few sources, uptake remains low. Even those who have gained access to FC do not necessarily receive the training and support needed for its proper use. One woman in our study summarized the problem well when she said, “I tried to use it a few times and it didn't work so I didn't use it no more … but if I ever figured out how to use it, that would be good.”
One of the greatest continuing barriers to FC uptake results from negative provider reactions to it and their own lack of familiarity or comfort with explaining its proper use.11,24,26,27 The initial responses of many health and service providers, including primary care physicians, pharmacists, clinicians and even HIV counselors, tend to be dismissive and denigrating of FC.41 Reasons for this include commonly expressed beliefs, often with no knowledge or evidence, that no one will use them, no one likes them, no one will purchase them, and difficulties with insertion and negotiation present insurmountable barriers to adoption of the method.24,41
Availability of FC compared to MC is drastically limited by inadequate stock at pharmacies and unsupportive attitudes of pharmacists and large chain pharmacy distribution centers, as well as severe rationing by public health authorities, ostensibly because of cost. MC remain the standard for prevention with millions distributed annually for free; yet, many providers still fail to recognize that most women are not able to control MC use. Nevertheless, it is notable that FC users in the study had access to free FC and made use of those resources. Increasing availability of free FC has also been shown to increase use among paying customers,23,24 thereby encouraging uptake and promotion by broader providers in the community such as pharmacies and other retailers.
Recent calls for increased availability of FC on a national and global level highlight the need to integrate FC promotion and accessibility into general health systems, both in high-income and low-income settings.24,42 Until a broad-based and comprehensive change in community access and support for FC takes place, including in community health clinics, private physicians' clinics and pharmacies, the most likely FC users will be those reached by community outreach workers and those who seek services where free FC are made available to all clientele. Promotion and widespread use of FC is likely to further reduce heterosexually transmitted HIV significantly. The ethics of the epidemic demand that every effective HIV prevention option for women be made available and supported in the community, including FC, so that it can be truly integrated into the prevention toolkit for women and men in widely varying personal, social, and partner relationship circumstances.
Acknowledgments
This project was funded by the National Institute of Mental Health (R01 MH069088). We wish to acknowledge the contributions of the field research team to this study and this paper, including Evelyn Baez, Michelle Garner, Mary Prince, and Jennifer Salonia.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.UNAIDS/WHO. AIDS epidemic update: December 2006. Geneva: 2006. [Google Scholar]
- 2.Wingood GM. Feminization of the HIV epidemic in the United States: Major research findings and future research needs. J Urban Health. 2003;80(4 Suppl 3):iii67–76. doi: 10.1093/jurban/jtg084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control & Prevention. Cases of HIV infection and AIDS in the United States and dependent areas, by race/ethnicity, 2003–2007. HIV AIDS Surveill Suppl Rep. 2009;14:1–43. [Google Scholar]
- 4.Barnett B. Scientists examine how and why couples use barrier methods, and what they like or do not like about them. Network 2000, vol. 20, no. 2. http://www.fhi.org/en/RH/Pubs/Network/v20_2/NWvol2000-2barmethpref.htm http://www.fhi.org/en/RH/Pubs/Network/v20_2/NWvol2000-2barmethpref.htm
- 5.El-Bassel N. Witte SS. Gilbert L, et al. The efficacy of a relationship-based HIV/STD prevention program for heterosexual couples. Am J Public Health. 2003;93:963–969. doi: 10.2105/ajph.93.6.963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Logan TK. Cole J. Leukefeld C. Women, sex, and HIV: Social and contextual factors, meta-analysis of published interventions, and implications for practice and research. Psychol Bull. 2002;128:851–885. doi: 10.1037/0033-2909.128.6.851. [DOI] [PubMed] [Google Scholar]
- 7.CDC. HIV/AIDS among Women (CDC HIV/AIDS Fact Sheet) Atlanta, GA: 2007. [Google Scholar]
- 8.El-Bassel N. Witte SS. Wada T. Gilbert L. Wallace J. Correlates of partner violence among female street-based sex workers: Substance abuse, history of childhood buse, and HIV risks. AIDS Patient Care STDs. 2001;15:41–51. doi: 10.1089/108729101460092. [DOI] [PubMed] [Google Scholar]
- 9.Dworkin SL. Ehrhardt AA. Going beyond “ABC” to include “GEM”: Critical reflections on progress in the HIV/AIDS epidemic. Am J Public Health. 2007;97:13–18. doi: 10.2105/AJPH.2005.074591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weeks MR. Grier M. Radda K. McKinley D. AIDS and social relations of power: Urban African American women's discourse on the contexts of risk and prevention. In: Elwood WN, editor. Power in the Blood: AIDS, Politics, and Communication. Mahwah, NJ; Lawrence Erlbaum Press: 1999. pp. 181–197. [Google Scholar]
- 11.Mantell JE. Dworkin SL. Exner TM. Hoffman S. Smit JA. Susser I. The promises and limitations of female-initiated methods of HIV/STI protection. Soc Sci Med. 2006;63:1998–2009. doi: 10.1016/j.socscimed.2006.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Askew I. Berer M. The contribution of sexual and reproductive health services to the fight against HIV/AIDS: A review. Reprod Health Matters. 2003;11:51–73. doi: 10.1016/s0968-8080(03)22101-7. [DOI] [PubMed] [Google Scholar]
- 13.French PP. Latka M. Gollub EL. Rogers C. Hoover DR. Stein ZA. Use-effectiveness of the female versus male condom in preventing sexually transmitted disease in women. Sex Transm Dis. 2003;30:433–439. doi: 10.1097/00007435-200305000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Galvao LW. Oliveira LC. Diaz J, et al. Effectiveness of female and male condoms in preventing exposure to semen during vaginal intercourse: A randomized trial. Contraception. 2005;71:130–136. doi: 10.1016/j.contraception.2004.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Jivasak-Apimas S. Saba J. Chandeying V, et al. Acceptability of the female condom among sex workers in Thailand: Results from a prospective study. Sex Transm Dis. 2001;28:648–654. doi: 10.1097/00007435-200111000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Adeokun L. Mantell JE. Weiss E. Delano GE. Promoting dual protection in family planning clinics in Ibadan, Nigeria. Int Family Planning Perspect. 2002;28:87–95. [Google Scholar]
- 17.Agha S. Intention to use the female condom following a mass-marketing campaign in Lusaka, Zambia. Am J Public Health. 2001;91:307–310. doi: 10.2105/ajph.91.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beksinska ME. Rees VH. McIntyre JA. Wilkinson D. Acceptability of the female condom in different groups of women in South Africa: A multicentred study to inform the national female condom introductory strategy. S Afr Med J. 2001:91672–678. [PubMed] [Google Scholar]
- 19.Napierala S. Kang MS. Chipato T. Padian N. Van der Straten A. Female condom uptake and acceptability in Zimbabwe. AIDS Educ Prev. 2008;20:121–134. doi: 10.1521/aeap.2008.20.2.121. [DOI] [PubMed] [Google Scholar]
- 20.Wadhams N. Uganda to reintroduce female condoms. Lancet. 2009;374:190. doi: 10.1016/s0140-6736(09)61315-5. [DOI] [PubMed] [Google Scholar]
- 21.Choi KH. Gregorich SE. Anderson K. Grinstead O. Gomez CA. Patterns and predictors of female condom use among ethnically diverse women attending family planning clinics. Sex Transm Dis. 2003;30:91–98. doi: 10.1097/00007435-200301000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Thomsen SC. Ombidi W. Toroitich-Ruto C, et al. A prospective study assessing the effects of introducing the female condom in a sex worker population in Mombasa, Kenya. Sexually Transm Infect. 2006;82:397–402. doi: 10.1136/sti.2006.019992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Price N. The performance of social marketing in reaching the poor and vulnerable in AIDS control programmes. Health Policy Plan. 2001;16:231–239. doi: 10.1093/heapol/16.3.231. [DOI] [PubMed] [Google Scholar]
- 24.Warren M. Philpott A. Expanding safer sex options: Introducing the female condom into national programmes. Reprod Health Matters. 2003;11:130–139. doi: 10.1016/s0968-8080(03)02178-5. [DOI] [PubMed] [Google Scholar]
- 25.Female Health Company. Working with the Female Condom. 2008. www.femalehealth.com/images/miniguide.pdf. [Mar 15;2010 ]. www.femalehealth.com/images/miniguide.pdf
- 26.Kaler A. The future of female-controlled barrier methods for HIV prevention: Female condoms and lessons learned. Cult Health Sex. 2004;6:501–516. [Google Scholar]
- 27.Mantell JE. Hoffman S. Exner TM. Stein ZA. Atkins K. Family planning providers' perspectives on dual protection. Perspect Sex Reprod Health. 2003;35:71–78. doi: 10.1363/3507103. [DOI] [PubMed] [Google Scholar]
- 28.Vijayakumar G. Mabude Z. Smit J. Beksinska M. Lurie M. A review of female-condom effectiveness: Patterns of use and impact on protected sex acts and STI incidence. Int J STD AIDS. 2006;17:652–659. doi: 10.1258/095646206780071036. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Census Bureau. American Community Survey. 2006.
- 30.Corbett M. Dickson-Gomez J. Hilario H. Weeks MR. A little thing called love: Condom use among high-risk primary heterosexual couples. Perspect Sex Reprod Health. 2009;41:218–224. doi: 10.1363/4121809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McLeroy KR. Bibeau D. Steckler A. Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 32.Rogers EM. Diffusion of Innovations. 4th. New York: The Free Press; 1995. [Google Scholar]
- 33.Connell RW. Gender and Power: Society, the Person and Sexual Politics. Stanford, CA: Stanford University Press; 1987. [Google Scholar]
- 34.Thompson SK. Adaptive sampling in behavioral surveys. NIDA Res Monogr. 1997;167:296–319. [PubMed] [Google Scholar]
- 35.Weeks MR. Schensul JJ. Williams SS. Singer M. Grier M. AIDS prevention for African-American and Latina women: Building culturally and gender-appropriate intervention. AIDS Educ Prev. 1995;7:251–264. [PubMed] [Google Scholar]
- 36.Kline R. Principles and Practice of Structural Equation Modeling. New York: The Guilford Press; 2005. [Google Scholar]
- 37.Loehlin J. Latent Variable Models: An Introduction to Factor, Path, and Structural Analysis. 4th. Hillsdale: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 38.Amos 16 User's Guide [computer program] Version 16. Chicago, IL: Marketing Department, SPSS Inc.; 2007. [Google Scholar]
- 39.Kim K. The Relation Among Fit Indexes, Power, and Sample Size in Structural Equation Modeling. Struct Equ Modeling. 2005;12:368–390. [Google Scholar]
- 40.Gross M. Buchbinder SP. Holte S. Celum CL. Kobin BA. Douglas JM. Use of Reality “Female Condoms” for anal sex by U.S. men who have sex with men. Am J Public Health. 1999;89:1739–1741. doi: 10.2105/ajph.89.11.1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mantell JE. Hoffman JA. Weiss E, et al. The acceptability of the female condom: Perspective of family planning providers in New York City, South Africa, and Nigeria. J Urban Health. 2001;78:658–668. doi: 10.1093/jurban/78.4.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoffman S. Smit JA. Adams-Skinner J. Exner T. Mandel J. Stein Z. Female condom promotion needed. Lancet. 2008;8:348. doi: 10.1016/S1473-3099(08)70109-9. [DOI] [PubMed] [Google Scholar]
- 43.Pulerwitz J. Gortmaker SL. DeJong W. The Sexual Relationship Power Scale: Development and Future Applications. Microbicides 2000 Conference; Washington, D.C.. Mar, 2000. [Google Scholar]
- 44.Pulerwitz J. Gortmaker SL. DeJong W. Measuring sexual relationship power in HIV/STD research. Sex Roles. 2000;42:637–660. [Google Scholar]
- 45.Raphan G. Cohen S. Boyer AM. The female condom, a tool for empowering sexually active urban adolescent women. J Urban Health. 2001;78:605–613. doi: 10.1093/jurban/78.4.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neilands TB. Choi K. A validation and reduced form of the female condom attitudes scale. AIDS Educ Prev. 2002;14:158–171. doi: 10.1521/aeap.14.2.158.23903. [DOI] [PubMed] [Google Scholar]