Abstract
Objective
To report diagnostic, clinical, and histopathologic features of a patient with coccidioidomycosis endophthalmitis without concomitant systemic involvement diagnosed by vitreous biopsy.
Design
Interventional case report
Participants
One patient
Intervention
Diagnostic pars plana vitrectomy, systemic and intravitreal antifungal treatment, and enucleation.
Main Outcome Measures
Diagnostic, clinical, and histopathologic features of chronic coccidioidomycosis endophthalmitis.
Results
A 64-year-old Caucasian male from Southern California presented with chronic intraocular inflammation in the right eye for 18 months. He had been unsuccessfully treated with topical and subtenon steroids. At presentation, best-corrected visual acuity (BCVA) was 20/400 in the right eye and 20/20 in the left eye. Ophthalmoscopy of the right eye revealed significant vitritis and multiple yellowish chorioretinal lesions. Evaluation by an internist had shown no underlying inflammatory, infectious, or neoplastic systemic illnesses. A vitreous biopsy followed by histopathologic examination showed the presence of multiple Coccidioides sp. microrganisms. The patient was then treated with intravitreal amphotericin B and oral fluconazole. BCVA initially improved to 20/80, but inflammation progressed and did not respond to two subsequent injections of antifungals, two additional pars plana vitrectomies, and oral fluconazole. The eye eventually became blind and painful and was enucleated. Histopathologic examination disclosed intraocular granulomas displaying multiple Coccidioides sp. microrganisms.
Conclusions
Coccidioides sp. endophthalmitis may present with no concomitant systemic involvement. Histopathologic examination of the vitreous is helpful in the diagnosis. A high index of suspicion is important, especially in areas where the incidence of coccidioidomycosis is rising.
Coccidioidomycosis is primarily a pulmonary disease1, 2 and may rarely lead to ocular involvement.3, 4 In highly endemic areas of the United States, such as California and Arizona, there has been a steep rise in the number of reported cases of coccidioidomycosis over the current decade.2, 5 Ocular disease is rare and may be underrecognized because the diagnosis is challenging, especially in the absence of extraocular involvement.4, 6
We report a patient with intraocular coccidioidomycosis that presented as a chronic posterior uveitis progressing to endophthalmitis in the absence of systemic manifestations.
CASE REPORT
A 64-year-old nondiabetic Caucasian male from Southern California presented with progressively decreasing vision and floaters in the right eye for 18 months. He had been diagnosed with uveitis of undetermined etiology and unsuccessfully treated with topical and subtenon steroids. An extensive physical examination and laboratory work-up by his internist had been negative for infectious, inflammatory, or neoplastic disease. Testing included a chest x-ray and serologic tests for syphilis, Lyme disease, and Valley fever. His past medical history was significant for two cardiac angioplasties, as well as a thyroidectomy for a benign tumor.
At presentation, best-corrected visual acuity (BCVA) was 20/400 in the right eye and 20/20 in the left eye. The anterior segment was unremarkable except for the presence of whitish keratic precipitates and 1+ flare in the right eye. The vitreous in the right eye revealed 2+ cells and 2–3+ haze. Multiple grey-yellowish retinal infiltrates could also be observed in the right eye, mostly located inferiorly, around an area of chorioretinal scarring (Fig 1A–B). Fluorescein angiography disclosed disc leakage, diffuse venular staining, and hypofluorescence of the chorioretinal lesions (Fig 1C–D). A diagnostic 25-gauge pars plana vitrectomy was performed, and specimens were sent for culture and histopathologic examination. Cell-block preparation of the vitreous specimen showed chronic granulomatous vitritis and the presence of multiple Coccidioides sp. spherules (Fig 2A). One intact mature spherule could also be identified in a section of an epiretinal membrane (Fig 2B). Cultures were negative for bacteria and fungi. On further questioning the patient acknowledged that he had been hunting in the high desert and had undergone previous treatment for pulmonary Valley fever with oral fluconazole 8 years before.
Figure 1.
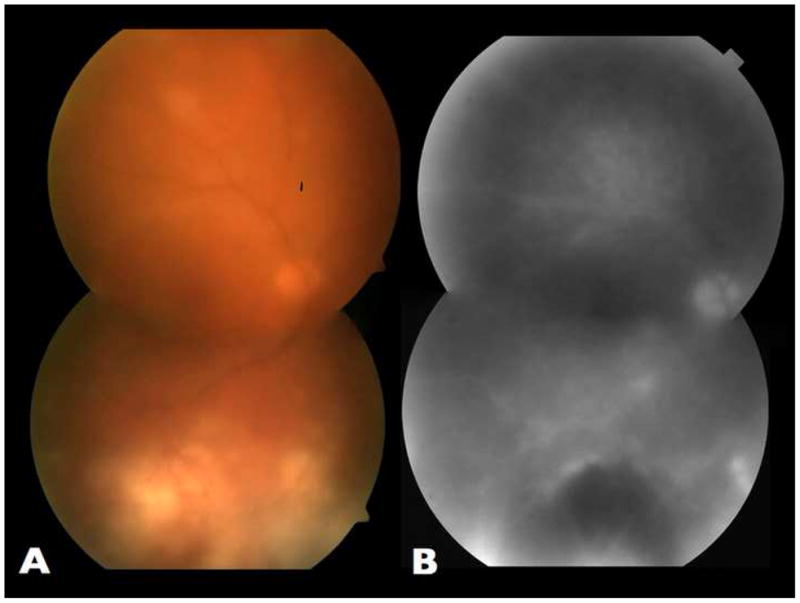
Fundus aspect of the right eye at presentation. A. Montage color fundus photograph showing significant vitreous haze and multiple grey-yellowish chorioretinal lesions. Note that inferiorly these lesions are distributed around an area of chorioretinal scarring. B. Montage of late phase fluorescein angiogram frame, showing disc leakage, diffuse venular staining and hypofluorescence of the large lesion inferiorly.
Figure 2.
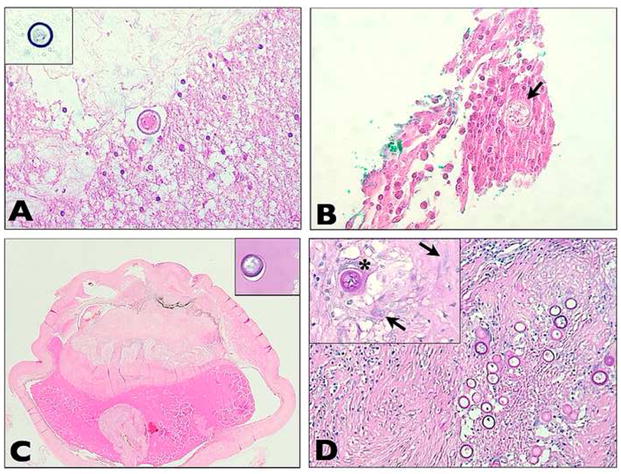
Histopathologic aspects. A. Cell block preparation of undiluted vitreous specimen, showing the presence of lymphocytes. A mature spherule of Coccidioides sp. is seen (hematoxylin-eosin, original magnification ×400). The spherule stains with Gomori methenamine silver (inset, ×400). B. Section of epiretinal membrane specimen obtained during diagnostic vitrectomy, revealing infiltration of lymphocytes and plasma cells. Epithelioid cells are also seen. A mature spherule of Coccidioides sp. full of endospores (arrow) can be identified. (hematoxylin-eosin, original magnification ×400). C. Section of the globe after enucleation, with retinal detachment and disorganization of intraocular contents (hematoxylin-eosin, original magnification ×1). A Coccidioides sp. spherule can be seen within subretinal fluid (inset, top right, Periodic acid Schiff [PAS], original magnification ×400). D. Detail of vitreous cavity, showing a granuloma with multiple PAS positive Coccidioides sp. organisms (PAS, original magnification ×100). Epitheliod cells can be seen (arrows), as well as a PAS positive Coccidioides sp. spherule within a multinucleate giant cell (asterisk) (inset, top left, original magnification ×400).
Consultation with an infectious disease specialist failed to reveal any systemic (including pulmonary) coccidioidomycosis. The patient was treated with intravitreal amphotericin B (5 g) and oral fluconazole (400 mg PO daily). BCVA initially improved to 20/80 over the next 3 weeks, but soon afterwards intraocular inflammation dramatically progressed and vision decreased, despite two subsequent injections of antifungals, two additional pars plana vitrectomies, and oral fluconazole. One of the two vitreous specimens revealed structures consistent with the fungal capsule, but cultures were invariably negative. The eye eventually became blind and painful and was enucleated.
Gross pathologic examination of the right eye revealed a hazy cornea and a collapsed anterior chamber filled with a fibrotic mass encompassing uveal tissue. The vitreous was replaced by a yellowish-white mass, and the retina was totally detached. Microscopic examination disclosed chronic granulomatous endophthalmitis and disorganization of the intraocular contents. There were multiple sarcoidal-type granulomas located on the posterior surface of the iris, in the vitreous cavity, and on the anterior surface of the detached retina (Fig 2C). A large number of Coccidioides sp. microrganisms were seen, especially within these granulomas, but also in the subretinal space (Fig 2C–D). The choroid revealed only mild lymphocytic infiltration in the sections studied.
DISCUSSION
We describe a patient with Coccidioides sp. endophthalmitis presenting several years after successful treatment of pulmonary infection. Coccidioidomycosis is subclinical in most individuals, with ocular involvement being regarded as rare and usually associated with disseminated disease.3, 4, 7 However, the incidence of coccidioidomycosis in California and Arizona has risen significantly, with the incidence now three times that of the previous decade.2, 5 The rate of hospitalizations associated with the disease has similarly increased.2, 5
The diagnosis of intraocular coccidioidomycosis is difficult and may often rely on direct examination of ocular fluids/specimens.4, 6 Serological tests may be negative,2, 4, 8 as in our patient, and fungal cultures are frequently negative for growth.8 In the setting of concomitant systemic involvement, biopsy of nonocular tissues may also help in the diagnosis.9
Coccidioidomycosis uveitis is classically reported to involve separately either the anterior or the posterior segment of the eye, with only a few cases involving both.3, 4 Histopathologic examination characteristically demonstrates intraocular granulomas, often containing the fungal organisms (Fig 2D).4, 6 Mature fungal spherules may rupture, releasing endospores and leading to suppurative inflammation.4, 6 Persistent inflammation may lead to severe tissue damage, as observed in our patient (Fig 2C). Endophthalmitis caused by Coccidioides sp., as seen in our patient, is exceedingly rare, and most cases reported as such have actually consisted of chorioretinitis without vitreal involvement, 3, 4, 7, 10 although retinal seeding in anterior uveitis following pars plana vitrectomy has been recently described.11 As the choroid was relatively spared in our patient, it is possible that the infection may have arisen from the retina, although this could not be proven.
Interestingly, our patient developed ocular disease several years after he had been treated for pulmonary coccidioidomycosis. Extensive systemic investigations failed to reveal any concomitant extraocular involvement; in particular, there was no evidence of pulmonary changes. As acquired immunity to coccidioidomycosis protects from reinfection,1, 4 it is likely that the ocular disease in our patient resulted from reactivation of a latent infection, as has been observed in posttransplantation coccidioidomycosis.12 However, posttransplantation coccidioidomycosis often presents with disseminated disease associated with immunosuppression. In our patient reactivation was confined to the right eye and he was apparently immunocompetent.
The best treatment for coccidioidomycosis uveitis is unclear. Systemic antifungals are usually recommended, but the exact role of intraocular antifungals is currently unknown.4, 6 In severe cases, such as in our patient, as well as in those in which penetration of antifungals may be of concern, intraocular therapy may be indicated. Azole antifungals, especially fluconazole, are now the standard therapy for extrapulmonary coccidioidomycosis, including meningitis.13 Newer antifungals, such as voriconazole, posaconazole, and caspofungin, may also be promising.2 An infectious disease specialist should be involved in the care of these patients.
The prognosis of anterior segment disease is regarded as worse than that of posterior segment disease.3, 4 However, our case illustrates that disease arising from the posterior segment may progress to endophthalmitis, with a dreadful prognosis in spite of intravitreal and systemic therapy, even in an apparently immunocompetent patient.6
The incidence of coccidioidomycosis is rising in the United States, and a high index of suspicion is required in the setting of granulomatous uveitis in patients traveling or living in highly endemic areas. The diagnosis of intraocular coccidioidomycosis may be delayed and examination of ocular fluids/specimens is helpful. Unfortunately, despite aggressive treatment, the prognosis may be poor.
Acknowledgments
Financial support: NEI grants EY03040 and EY001792 and an unrestricted grant from Research to Prevent Blindness, Inc., New York, NY.
Footnotes
There is no conflict of interest for any author.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chiller TM, Galgiani JN, Stevens DA. Coccidioidomycosis. Infect Dis Clin North Am. 2003;17:41–57. viii. doi: 10.1016/s0891-5520(02)00040-5. [DOI] [PubMed] [Google Scholar]
- 2.Ampel NM. Coccidioidomycosis: a review of recent advances. Clin Chest Med. 2009;30:241–51. v. doi: 10.1016/j.ccm.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Rodenbiker HT, Ganley JP. Ocular coccidioidomycosis. Surv Ophthalmol. 1980;24:263–90. doi: 10.1016/0039-6257(80)90056-9. [DOI] [PubMed] [Google Scholar]
- 4.Foos RY, Zakka KA. Coccidioidomycosis. In: Pepose JS, Holland GN, Wilhelmus KR, editors. Ocular Infection and Immunity. St. Louis, MO: Mosby; 1996. pp. 1430–6. [Google Scholar]
- 5.Increase in coccidioidomycosis - California, 2000–2007. MMWR Morb Mortal Wkly Rep. 2009;58:105–9. [PubMed] [Google Scholar]
- 6.Moorthy RS, Rao NA, Sidikaro Y, Foos RY. Coccidioidomycosis iridocyclitis. Ophthalmology. 1994;101:1923–8. doi: 10.1016/s0161-6420(94)31082-7. [DOI] [PubMed] [Google Scholar]
- 7.Blumenkranz MS, Stevens DA. Endogenous coccidioidal endophthalmitis. Ophthalmology. 1980;87:974–84. doi: 10.1016/s0161-6420(80)35137-3. [DOI] [PubMed] [Google Scholar]
- 8.Saubolle MA. Laboratory aspects in the diagnosis of coccidioidomycosis. Ann N Y Acad Sci. 2007;1111:301–14. doi: 10.1196/annals.1406.049. [DOI] [PubMed] [Google Scholar]
- 9.Cunningham ET, Jr, Seiff SR, Berger TG, et al. Intraocular coccidioidomycosis diagnosed by skin biopsy. Arch Ophthalmol. 1998;116:674–7. doi: 10.1001/archopht.116.5.674. [DOI] [PubMed] [Google Scholar]
- 10.Hagele AJ, Evans DJ, Larwood TR. Primary endophthalmic coccidioidomycosis: report of a case of exogenous primary coccidioidomycosis of the eye diagnosed prior to enucleation. In: Ajello L, editor. Coccidioidomycosis: Papers from the Second Symposium. Tucson, AZ: University of Arizona Press; 1967. pp. 37–9. [Google Scholar]
- 11.Mondino KM, Holland GN, Glasgow BJ. Retinal seeding from anterior segment coccidioidomycosis after vitrectomy [letter] Br J Ophthalmol. 2007;91:837–8. doi: 10.1136/bjo.2006.106195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blair JE. Approach to the solid organ transplant patient with latent infection and disease caused by Coccidioides species. Curr Opin Infect Dis. 2008;21:415–20. doi: 10.1097/QCO.0b013e3283073828. [DOI] [PubMed] [Google Scholar]
- 13.Galgiani JN, Ampel NM, Blair JE, et al. Coccidioidomycosis. Clin Infect Dis. 2005;41:1217–23. doi: 10.1086/496991. [DOI] [PubMed] [Google Scholar]


