Abstract
Synovial sarcomas are most commonly localized in the extermities, especially the lower thigh and knee areas. Retroperitoneal synovial sarcoma is very rare. We decribe the radiological findings of an adult retroperitoneal synovial sarcoma.
Keywords: Synovial sarcoma, retroperitoneal, CT, MRI
INTRODUCTION
Soft tissue sarcomas (STS) are rare tumors that comprise only 1% of all malignancies. The retroperitoneum is an uncommon site of origin for them, accounting for 10% of all STS. Because of its anatomic peculiarities (lack of boundaries to allow true compartmental surgical resection and asymptomatic growth of huge masses), the presentation of STS remains challenging. The prognosis of patients with STS generally is poor, especially when they are assessed over the long term.[1]
Only 10–20% of sarcomas are retroperitoneal sarcomas, and the overall incidence is 0.3–0.4% per 100 000 of the population. The peak incidence is in the fifth decade of life, although they can occur in any age group. The most common types of retroperitoneal STS in adults vary from study to study. However, in most studies, the most frequently encountered cell types are liposarcomas, leiomyosarcomas and malignant fibrous histiocytomas (MFH). Recently, the frequent diagnosis of MFH in the retroperitoneum has been disputed. With the use of immunohistochemistry, many of these fibrous tumors have now been shown to represent other sarcoma types such as leiomyosarcomas or dedifferentiated liposarcomas. For this reason, it is anticipated that the number of these neoplasms that will be considered as MFH will be dramatically reduced in the future. Patients with sarcomas present late, because these tumors arise in the large potential spaces of the retroperitoneum and can grow very large without producing symptoms. Moreover, when symptoms do occur, they are nonspecific, such as abdominal pain and fullness, and are easily dismissed as being caused by other less serious processes. Retroperitoneal sarcomas, therefore, are usually very large at the time of presentation.[2]
Synovial sarcoma constitutes 8–10% of all sarcomas and most commonly affects adults in the third to fifth decades of life. This malignancy usually involves the extremities, especially the lower extremities around the knees. Synovial sarcoma is frequently misdiagnosed as a benign condition because of its often small size, slow growth and well-defined appearance.[3,4]
The term synovial sarcoma refers to the morphology that resembles developing synovium. Eighty five to 95% of synovial sarcomas occur in the extremities near the large joints. Only 5–15% of synovial sarcomas affect the head and neck, mediastinum, abdominal wall and retroperitoneum .Primary retroperitoneal synovial sarcoma is extremely rare and has poor prognosis.[5] They have no specific imaging features differentiating it from other mesenchymal tumors. Despite the rarity of mesenchymal tumors of the retroperitoneum, synovial sarcoma should be included in the differential diagnosis of a retroperitoneal soft tissue mass detected in adults.[6]
CASE REPORT
A 37-year-old woman was admitted to King Khaled University Hospital, in Riyadh with a history of left loin pain and swelling, weight loss and hematuria. Physical examination revealed a palpable left side abdominal mass.
CT pre-and post-IV contrast was done for the abdomen and it showed a lobular soft tissue mass in retroperitoneal space on the left side, also. It showed heterogeneous contrast enhancement with peripheral hypervascularity and central area of breakdown. Bowel loops also are seen displaced with no sign of invasion. However, it was difficult to differentiate renal mass from extra renal mass by CT, hence MRI was done [Figure 1].
Figure 1.
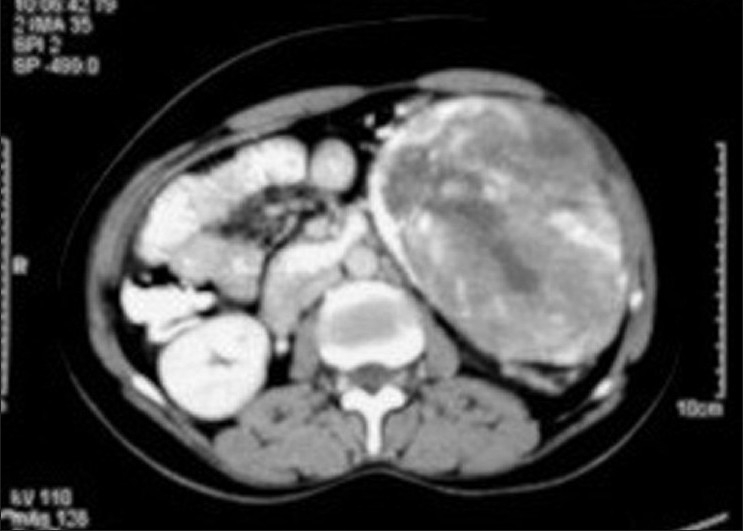
Post contrast CT showing retroperitoneal soft tissue mass with peripheral hypervascularity and central area of breakdown
Multiplanar MRI of the abdomen and pelvis was done and it demonstrated a large well-defined lobulated mass noted occupying left lumbar region. It displaced left kidney upward and bowel loop medially to the contralateral. It abuts left psoas muscle in its posteromedial aspect as well as anterior abdominal wall anteriorly. It exhibits iso-to low-signal intensity in T1WI with multiple areas of low signals of necrosis and showing area of high signal in its caudal portion. In T2WI, it exhibits mixed high and low signal and it takes mild contrast enhancement after contrast administration. It measures about 14 × 10 cm [Figure 2].
Figure 2.
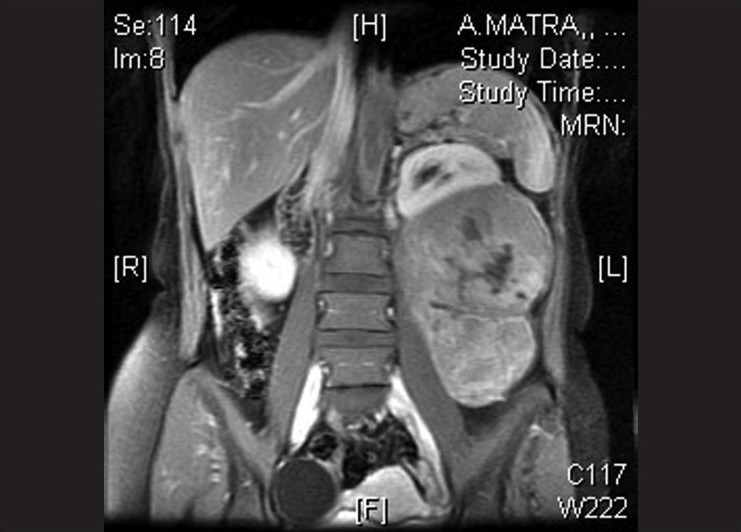
Coronal T1WI, post Gadolinium showing lobulated retroperitonea mass with heterogenous enhancment and renal displacement
The initial differential diagnosis of this case was:
-
-
Lymphoma
Other primary retroperitoneal sarcoma such as:
-
-
Leiomyosarcoma
-
-
Synovial sarcoma
-
-
Rhabdomyosarcoma
The patient underwent excisional biopsy and the histopathology report showed synovial sarcoma.
DISCUSSION
Primary retroperitoneal STS group is a rare, but diverse group of neoplasms. This group is characterized by late clinical presentation and high rate of recurrence. Hence, cross-sectional imaging particularly CT and MRI play an important role in their diagnosis. Synovial sarcoma is a rare subtype of this group,[4] they have poor prognosis.[5] Still its early diagnosis is important for less morbidity and mortality.
Although the diagnosis of a retroperitoneal synovial sarcoma is based on the pathological characteristics of the specimen obtained by needle or surgical resection, radiographic studies suggest preoperative diagnosis of synovial sarcoma. CT may identify soft tissue calcifications, especially those that are subtle or are located in areas where the anatomy is complex. It may also show areas of hemorrhage, necrosis or cyst formation within the tumor. CT defines the mass, and readily confirms bone involvement. Intravenous contrast may help in differentiating the mass from the adjacent muscle and neurovascular complex. On MRI, the findings are of a lesion that is usually a nonspecific heterogeneous mass with signal intensity approximately equal to that of skeletal muscle on T1WI and higher than that of subcutaneous fat on T2WI MRI. Signal intensity changes compatibility with previous hemorrhage and fluid–fluid levels have been reported. The soft tissue calcifications frequently seen on radiographs and CT may not be detected on MRI, although larger calcifications may be identified as areas of decreased signal intensity on all pulse sequences.[6]
Therefore CT and MRI can allow proper identification of the primary retroperitoneal origin of the tumor and differentiating it from tumor originating from retroperitoneal structures, which will clearly have different management plan and have different prognosis.
Footnotes
Source of Support:Nil
Conflict of Interest: None.
REFERENCES
- 1.Gronchi A, Casali PG, Fiore M, Mariani L, Vullo SL, Bertulli R, et al. Retroperitoneal Soft Tissue Sarcomas. Cancer. 2004;100:2448–55. doi: 10.1002/cncr.20269. [DOI] [PubMed] [Google Scholar]
- 2.Francis IR, Cohan RH, Varma DG, Sondak VK. Retroperitoneal sarcomas. Cancer Imaging. 2005;5:89–94. doi: 10.1102/1470-7330.2005.0019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphey MD, Gibson MS, Jennings BT, et al. From the archives of the AFIP: Imaging of synovial sarcoma with radiologic-pathologic correlation. Radiographics. 2006;26:1543–65. doi: 10.1148/rg.265065084. [DOI] [PubMed] [Google Scholar]
- 4.Nakajima H, Matsushita K, Shimizu H, et al. Synovial sarcoma of the hand. Skeletal Radiol. 1997;26:674–6. doi: 10.1007/s002560050310. Nov. [DOI] [PubMed] [Google Scholar]
- 5.Song H, Koh BH, Cho OK, Rhim H, Kim Y, Hong EK, Park YW. Primary Retroperitoneal Synovial Sarcoma. J Korean Med Sci. 2002;17:419–22. doi: 10.3346/jkms.2002.17.3.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ulusan S, Kizilkilic O, Yildirim T, Hurcan C, Bal N, Nursal TZ. Radiological findings of primary retroperitoneal synovial Sarcoma. The British Journal of Radiology. 2005;78:166–9. doi: 10.1259/bjr/67990800. [DOI] [PubMed] [Google Scholar]


