Abstract
Objectives
The aim of this study was to examine barriers to the use of electronic diaries within the clinic setting and to determine outcome differences between patients who used electronic diaries to monitor their progress with summary data feedback and patients who monitored their progress with paper diaries without summary data feedback.
Methods
One hundred thirty-four (n=134) chronic pain patients were asked to monitor their pain, mood, activity interference, medication use, and pain location on either a paper or electronic diary immediately before each monthly clinic visit for 10 months. Patients and their treating physicians in the electronic diary group (n=67) were able to observe changes in their ratings while patients using the paper diaries (n=67) had no feedback about their data entry.
Results
Most participants believed that completing pain diaries was beneficial, yet only 23% of patients in the experimental condition felt that the data from the electronic diaries improved their care and less than 15% believed that their doctor made a change in their treatment based on the summary diary information.
Conclusion
In general, treating physicians were positive about the use of electronic diaries, although they admitted that they did not regularly incorporate the summary data in their treatment decision-making either because they forgot or they were too busy. Future studies in understanding barriers to physicians’ and patients’ use of diary data to impact treatment outcome are needed in order to improve care for persons with chronic pain.
Keywords: Electronic diaries, PDA, chronic pain, treatment helpfulness, barriers, patient satisfaction
Introduction
While chronic pain is typically not considered “curable,” a main focus in managing chronic pain is to identify and treat the core problems and exacerbating factors to improve quality of life.1 Unfortunately, as pain conditions persist over time, regular clinic visits with a treating physician can become more narrowly focused around specific pain treatments that produce limited improvement. Treatment decisions often have to be made on the basis of everbriefer clinic encounters,2, 3 and patients often feel neglected and misunderstood because no one is closely attending to their conditions.4, 5
In response to these concerns, patients with chronic illnesses are increasingly comfortable with and interested in self-assessment and monitoring activities that allow them to be more actively involved in their care.6, 7 Only recently, with the increased use of electronic data monitoring, has tracking with computers through the Internet, personal digital assistants (PDAs), and cellular phones become an accepted component in the management of chronic diseases. To date, research widely supports the use of electronic data tracking for a variety of medical conditions such as asthma, cancer, back pain, and rheumatoid arthritis.8–13 The benefits of electronic monitoring include instant data access, ease of data sharing, use of summary charts and graphs, portability, real-time sampling, and numerous software applications that include health and self-care information.14–16 There is evidence that tracking progress with an electronic diary increases compliance, allows patients to become more informed about their conditions, and can have a positive impact in changing perceptions of a chronic illness.17 Research has demonstrated that monitoring alone can stimulate behavior change,18, 19 and improve mental health.20, 21 Also, programs designed to track many aspects of the chronic pain condition can supply necessary documentation to track outcomes and reduce variation in care.
Within pain management, many studies have concluded that electronic diaries are reliable and accurate, and improve data quality compared with paper diaries when tracking persons with pain,14,22–26 but few studies have investigated whether electronic tracking can be seamlessly incorporated into the clinic to allow patients and physicians to readily identify factors exacerbating or relieving pain and whether patients and physicians modify treatment accordingly. In a recent crossover pilot study of 36 chronic pain patients,27 subjects reported more treatment changes based on the feedback of electronic diaries than when they monitored their progress with paper diaries. Also, patients using the electronic diaries reported more frequently that a provider suggested medication change based on feedback from the diary and that the diary enabled them and their doctor to make care adjustments according to changes in pain status.27 Despite the growing use of electronic diaries to monitor patient progress, little research attention has been given to how electronic diaries can be incorporated within a busy clinic and whether feedback from the diaries influence perceived treatment helpfulness among patients with chronic pain.
The aim of this study was to examine barriers to the use of electronic diaries within the clinic setting and to determine outcome differences between patients who used electronic diaries to monitor their progress with summary data feedback and patients who monitored their progress with paper diaries without summary data feedback. Data were collected monthly in both groups. We present results from a randomized controlled trial comparing paper and electronic tracking during monthly clinic visits over 10 months, and relate outcome and treatment helpfulness with use of electronic diaries. We decided to collect diary data from monthly visits, since this is a likely interval between visits for persons with chronic pain treated in a pain center. We conducted a qualitative evaluation of patient and physician perceptions of electronic diary use at the end of the study through semi-structured interviews to understand their perspectives. The patient and physician satisfaction questionnaires were selected as the main outcome variables as an index of satisfaction with the electronic diaries and summary data. We hypothesized that physicians would welcome the summarized patient data from electronic diaries and this would, in turn, improve patient outcome and treatment satisfaction.
Methods
Study Patients
This study was part of a larger NIH-sponsored study to compare outcomes and treatment satisfaction of patients who used paper diaries with those assigned to use electronic diaries for use at home and in the clinic each month with monthly feedback summarized electronically over time. Subjects for this study were adults who attended an urban pain management center in an academic teaching hospital. All subjects were 18 years of age or older, English speaking, and experiencing chronic pain for longer than three months. Participants were recruited through flyers placed in the pain clinic or invited to participate by their physician in the pain management center. Exclusion criteria included obvious cognitive impairment, and an inability to speak or read English (all screens were in English). All patients were required to sign an informed consent form prior to participation.
Procedures
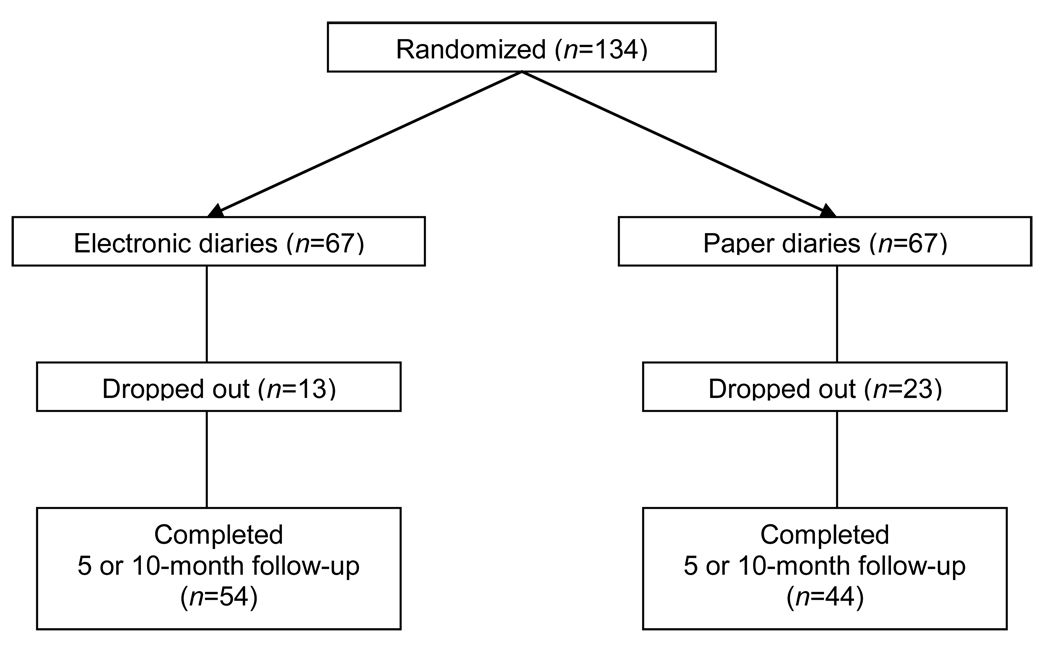
This study was approved by the Brigham and Women’s Hospital Human Subjects Committee and New England Research Institutional Review Board. Participants were randomly assigned to receive one of two conditions: electronic (experimental group) or paper (control group) diaries. Participants were asked to complete either paper or electronic diaries once a month with information about pain status and related factors before their clinic visit. Randomization consisted of assignment to treatment group based on a randomized number list created before the start of the study by independent associates at New England Research Institutes. The researchers involved with recruitment did not have access to the list at the time of each enrollment (Figure 1). Subjects were assigned to their group in the order that they entered into the study prior to conducting any data entry. All subjects completed an evaluation questionnaire at the start of the study (baseline) either on a paper form or the electronic device depending upon their randomization. Baseline measures were repeated again at 5 months (T5), and at the 10-month (T10) completion of the study. After the 10-month trial, participants were also asked to complete satisfaction questionnaires and to report on their experiences. All subjects were given gift cards totaling a maximum of $100 for their monthly participation ($15 first visit, $5 gift cards for visits 2–4, $15 for visits 5 and 10, and $10 gift cards for visits 6–9). The treating physicians were asked to complete satisfaction questionnaires at the start of the study and again at its conclusion, and pain fellows who participated in patient care also were asked to complete an overall satisfaction questionnaire at the conclusion of the study. Treating physicians completed a questionnaire about using the electronic diary on each of their patients who participated in the experimental group and were paid $100 for each of their patients who completed 10 visits and $50 for patients who had 5 visits or fewer. They were not asked to complete questionnaires on patients who dropped out of the study. Pain fellows were paid $100 for completing end-of-study satisfaction questionnaires.
Fig. 1.
Flow diagram of patient inclusion.
Baseline Measures
The Brief Pain Inventory (BPI)28
This self-report questionnaire, formerly the Wisconsin Brief Pain Questionnaire,29 is a well-known measure of clinical pain and has shown sufficient reliability and validity (r=0.77 to 0.9130, 31) and has been translated into 25 different languages. This questionnaire provides information about pain history, intensity, and location as well as the degree to which the pain interferes with daily activities, mood, and enjoyment of life. Scales (rated from 0 to 10) indicate the intensity of pain in general, at its worst, at its least, average pain, and pain “right now.” A figure representing the body is provided for the patient to indicate the area corresponding to his or her pain. Test-retest reliability for the BPI reveals correlations of 0.93 for worst pain, 0.78 for usual pain, and 0.59 for pain now.28
Pain Catastrophizing Scale (PCS)32
The PCS is a 13-item instrument that examines three components of catastrophizing: Rumination, Magnification, and Helplessness. The PCS is found to predict levels of pain and distress among clinical patients and scores have been related to thought intrusions.33 It has good psychometric properties with adequate reliability and validity32 and is associated with levels of pain, depression, and anxiety.
Oswestry Disability Index (ODI)34
The ODI is a 10-item questionnaire rated from 0 to 5 on level of disability of 10 areas of activity interference originally derived from the Oswestry Low Back Pain Disability Questionnaire.35 It has shown to have excellent test-retest reliability and validity 36 and is sensitive to high levels of disability. Although originally created for the assessment of persons with low back pain, it has shown to have adequate reliability (r=0.86) and validity among persons with other types of chronic pain.37
Center for Epidemiologic Studies-Depression Scale (CES-D)38
The CES-D is a self-report measure of depression consisting of 20 items rated on a 0–3 scale reflecting depression symptomatology. The Cronbach’s alpha coefficients range from 0.85 for a general population to 0.90 for a psychiatric population.38 The CES-D is perceived as a useful measure of depression for patients with chronic illnesses because of fewer items with somatic content. The CES-D is found to have good sensitivity and specificity in discriminating between patients with chronic pain who do or do not have major depression.39 The 10-item short-form version of the CES-D was used in this study and is shown to have similar reliability and sensitivity to the original CES-D (sensitivity = 97%; specificity = 84%).40,41
Treatment Helpfulness Questionnaire (THQ)42
This 8-item rating scale was adapted from the original 10-item THQ42 and was completed by the patients at the beginning and end of the study. The items reflecting different aspects of treatment were rated from 0 = extremely harmful to 10 = extremely helpful. It has been shown to have good test-retest reliability (r=0.86) and validity and assesses how helpful overall specific treatments for pain have been.
Follow-up Measures
Patient Satisfaction Questionnaire27
This is a 21-item satisfaction questionnaire, adapted for this study, that was completed by all subjects at the end of the trial. Fourteen of the items were rated on a 5-point Likert scale (1 = strongly disagree; 3 = neither agree nor disagree; 5 = strongly agree). Six items adapted from a previous study27 were answered yes or no. Patients assigned to the electronic diaries were also asked to complete four additional items at the end of the study specific to their use of their diaries.
Physician Satisfaction Questionnaire
The treating physicians (attending) and physicians participating in a 1-year pain fellowship program (fellow) completed an 18-item questionnaire rated from 1 = strongly agree to 5 = strongly disagree about the use of electronic diaries at the end of the study. Information was obtained about their perception of the use of the electronic diaries in the clinic.
Pain Diaries
Paper and electronic diaries consisted of a comprehensive set of 25 items, incorporating questions from the Brief Pain Inventory28 (pain severity, activity interference, function, and mood), medication questions, and a location of pain on a body map. Participants assigned to the electronic diary group were provided with a Hewlett Packard© IPAQ hx2410 Pocket PC personal digital assistant (PDA) to complete one diary entry at each clinic visit. Subjects assigned to the paper diaries group completed identical items matched as closely as possible to those in the electronic diary. All subjects were asked to complete their diaries before meeting with their physician.
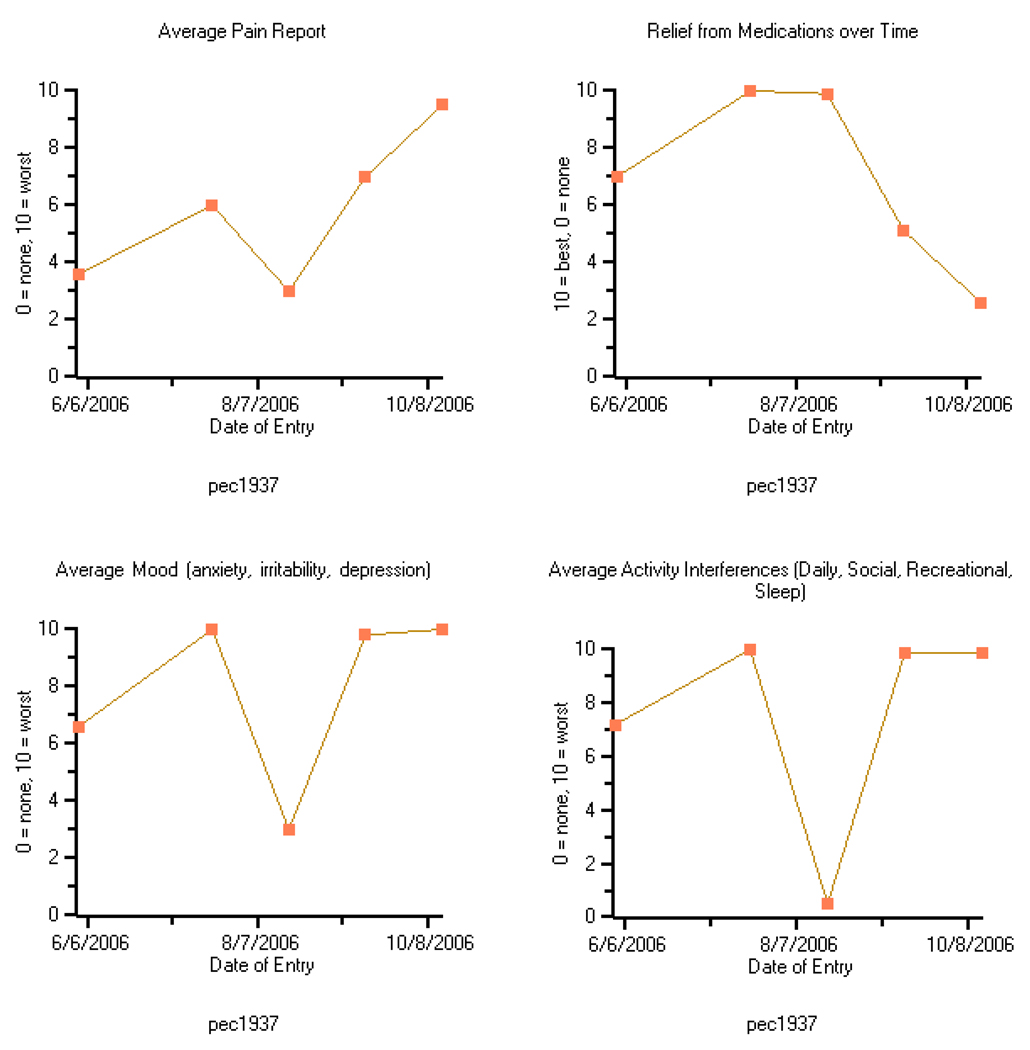
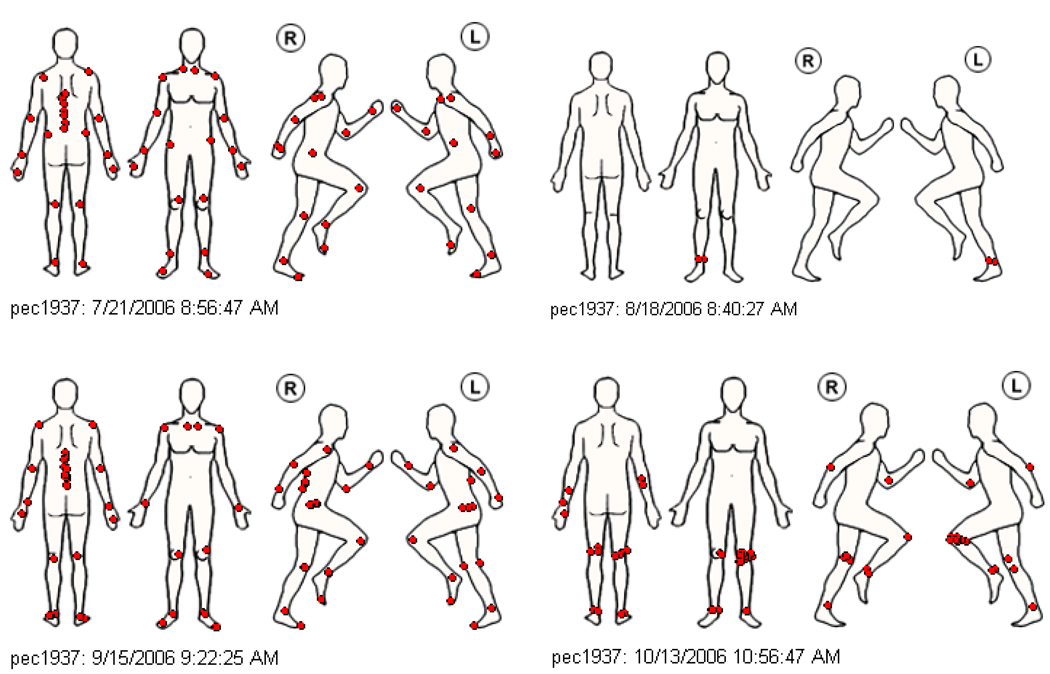
After the participants in the electronic diary group completed their data entry, the PDA was placed in a docking station and the data were saved to a computer in the front desk of the waiting room. Four summary graphs (average pain, average relief from pain, average mood, and average activity interference) were saved and printed and study research assistants provided them to the patients prior to their visit with their physician. The graphs were updated upon each visit. Examples of a summary graph and body map are presented in Figures 2 and 3. Information from the summary graphs and pain drawings were also stored as an electronic file within the electronic medical record of each patient marked as “electronic diaries.” The treating physicians were informed that this file was available to them for those subjects who were assigned to the electronic diary group. At the end of the trial, participants were asked to complete a brief survey of their experiences with the diaries (either paper or electronic). A qualitative evaluation was also conducted at the end of data collection with a subset of patients and physicians.
Fig. 2.
Sample of the graphs and pain sites generated by the monthly electronic diary data – Pain and Activity Charts
Fig. 3.
Sample of the graphs and pain sites generated by the monthly electronic diary data - Body Map Data.
Semi-Structured Interviews
Two trained interviewers conducted semi-structured telephone interviews with the attending physicians and a subgroup of patients who completed the study selected at random. The interviews were digitally recorded and transcribed. Patients and physicians were consented and the corresponding treating physician was supplied the paper chart of one of their patients who participated in the study prior to the interview. Physicians were asked to review the patient’s electronic and paper chart before being interviewed and to answer the questions with the specific patient in mind. The physician and patient semi-structured interviews included 15 questions on the nature of the patient’s pain, use of the diary, changes in treatment related to the diary, perceptions regarding doctor-patient communication, and recommendations for future assessment programs. The physicians were also asked about the utility of incorporating the diary into clinic practice.
A trained qualitative analyst first read and coded the interview transcripts using the question topics from the discussion guide to organize the coding scheme. Second, the analyst identified themes emerging under each set of questions for the physicians and patients separately and responses were summarized by groups (physicians and patients). The analyst assigned a unique study identification number to protect confidentiality in the summary reports. To further protect confidentiality, we amended the content to mask the gender of the participants.
Statistical Analysis
Analyses were conducted using SAS version 9.1.3. For the baseline scales (PCS, ODI, and CES-D) an average score of the available items was computed, which was then transformed to sum scores. Wilcoxon nonparametric two-sample tests were used to compare results from the electronic and paper diary groups. For categorical variables, Chi-square or Fisher exact tests were used to compare groups. Multivariate analyses of variance (MANOVA) analyses were run on the repeated measures. A completer was defined as a person who completed an evaluation at time T5 or T10. Follow-up data are given for the last (T5 or T10) time point available. The primary variables used to address the study hypotheses were the patient and physician satisfaction questionnaires with support from the qualitative interviews.
Results
One hundred thirty-four (n=134) patients with chronic pain were recruited for this study; 67 were randomized to the paper diaries group and 67 randomized to the electronic diaries group. Demographic information of the participants is presented in Table 1. The subjects averaged 49.5 years of age, half were female, and subjects had pain for an average of 10.5 years. Although we did not collect primary pain site information as part of the demographic data from the participants, we examined the pain sites reported on the pain drawings. Seventy four percent experienced low back pain and 72.7% reported multiple pain sites. Most subjects were taking pain medication (96.2%), and reported significant interference with activities (average interference with activities scores greater than 5). About half described their health as fair or poor (49.2%). Mean baseline scores of the BPI-interference, PCS, ODI, and CES-D between groups are presented in Table 2 and are representative of other subpopulations of chronic noncancer pain patients.30, 31, 37, 40 Thirteen subjects in the electronic diaries group (19.4%) and 23 subjects from the paper diaries group (34.3%) did not complete any follow-up information (T5 or T10) and were considered dropouts. Analyses showed that those in the paper group were more likely to drop out than those in the electronic diary group (X2=3.80; P=0.05). Dropouts from the paper group were less likely to find their drug prescriptions to be helpful (6.8 vs. 8.1, P<0.01) and had less interference with relations with other people (4.1 vs. 5.6, P<0.05) on baseline measures compared with completers. Dropouts from the electronic group had less pain (least pain 2.8 vs. 4.4, P<0.05; average pain 4.8 vs. 6.1, P<0.05; pain now 4.2 vs. 6.0, P<0.05) on baseline measures compared with completers. No significant differences were found between groups on the baseline measures (Tables 1 and 2) and no consistent groups differences were found at post-treatment on the BPI, PCS, ODI, and CES-D. MANOVA results were nonsignificant between groups for the seven items of the BPI (P=0.974) and for the PCS, ODI, and CES-D at baseline (P=0.773) and follow-up (P=0.745).
Table 1.
Comparison of Patient Demographic and Descriptive Characteristics Between Electronic (n= 67) and Paper Groups (n=67)
| Overall | Electronic | Paper | |||||
|---|---|---|---|---|---|---|---|
| Variable | Mean | Standard Deviation |
Mean | Standard Deviation |
Mean | Standard Deviation |
P- value |
| Age (years) | 49.5 | 11.3 | 48.5 | 11.6 | 50.5 | 11.0 | 0.312 |
| Gender (% male) | 50.0 | 52.2 | 47.8 | 0.604 | |||
| Duration of pain (years) | 10.5 | 9.5 | 9.1 | 6.1 | 11.8 | 11.9 | 0.099 |
| Average paina in 24 hours (0–10) | 5.9 | 1.9 | 5.8 | 1.9 | 5.9 | 1.9 | 0.789 |
| Currently taking pain meds (%) | 96.2 | 94.0 | 98.5 | 0.366 | |||
| Pain medication relief (0–100%) | 52.6 | 24.7 | 51.6 | 21.3 | 53.7 | 27.8 | 0.633 |
| Pain interferesb with (1–10): | |||||||
| General activities | 6.5 | 2.4 | 6.4 | 2.5 | 6.6 | 2.3 | 0.802 |
| Mood | 5.9 | 2.6 | 5.9 | 2.7 | 6.0 | 2.5 | 0.790 |
| Walking | 5.9 | 2.8 | 5.8 | 2.9 | 5.9 | 2.8 | 0.787 |
| Sleep | 6.5 | 2.9 | 6.4 | 3.0 | 6.5 | 2.8 | 0.942 |
| Relations | 5.0 | 2.5 | 5.0 | 2.4 | 5.1 | 2.5 | 0.863 |
| Enjoyment | 6.7 | 2.5 | 6.7 | 2.6 | 6.7 | 2.4 | 0.890 |
| Normal work | 6.8 | 2.4 | 6.7 | 2.7 | 7.0 | 2.1 | 0.499 |
| General Health fair-poor (%) | 49.2 | 52.2 | 46.2 | 0.490 | |||
| Health over 1 yr (% worse) | 41.8 | 43.2 | 40.3 | 0.726 | |||
0=no pain; 10=pain as bad as you can imagine
1=does not interfere; 10=completely interferes
Table 2.
Comparison of Patient Descriptive Characteristics on Baseline and Post-Study Measures Between Electronic and Paper Groups (Including Only Those With Pre-Post Values)
| Electronic | Paper | Difference | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable a | Pre | Post | Pre | Post | Pre | Post | Change | ||||||||
| n | Mean | SD | Mean | SD | Pb | n | Mean | SD | Mean | SD | Pb | Pc | Pd | Pe | |
| Brief Pain Inventory (BPI) Interferencea |
54 | 6.2 | 2.2 | 5.9 | 2.1 | 0.457 | 44 | 6.5 | 2.1 | 6.3 | 2.1 | 0.637 | 0.492 | 0.377 | 0.860 |
| Pain Catastrophizing Scale (PCS) |
54 | 1.9 | 0.8 | 1.7 | 0.9 | 0.030 | 44 | 1.9 | 1.0 | 1.8 | 1.0 | 0.358 | 0.932 | 0.529 | 0.413 |
| Helplessness | 54 | 1.9 | 0.9 | 1.6 | 0.9 | 0.047 | 44 | 1.9 | 1.1 | 1.8 | 1.0 | 0.436 | 0.806 | 0.309 | 0.399 |
| Magnification | 54 | 1.5 | 0.9 | 1.3 | 1.0 | 0.134 | 44 | 1.5 | 1.1 | 1.4 | 1.1 | 0.442 | 0.983 | 0.706 | 0.646 |
| Rumination | 54 | 2.3 | 1.0 | 2.0 | 1.1 | 0.066 | 44 | 2.1 | 1.1 | 2.0 | 1.1 | 0.410 | 0.578 | 0.879 | 0.490 |
| Oswestry Disability Index (ODI) |
54 | 3.2 | 0.8 | 3.2 | 0.9 | 0.802 | 44 | 3.5 | 0.8 | 3.4 | 0.8 | 0.643 | 0.170 | 0.226 | 0.920 |
| CES-D Depression | 54 | 2.5 | 0.6 | 2.3 | 0.6 | 0.003 | 44 | 2.5 | 0.5 | 2.4 | 0.7 | 0.489 | 0.673 | 0.508 | 0.198 |
SD = standard deviation; CES-D = Center for Epidemiologic Studies-Depression Scale.
These are average scores. To obtain total scores, multiply by 7 for the BPI Interference, by 13 for the PCS, by 6 for Helplessness, by 3 for Magnification, by 4 for Rumination, by 10 for the CES-D Depression Scale. For the ODI, percent disability is (x-1)*20 where x is the average score.
P-value from paired t-test that the pre-post difference is zero.
P-value from two sample t-test that electronic and paper means are the same at pre-test.
P-value from two sample t-test that electronic and paper means are the same at post-test.
P-value from two sample t-test that the pre-post electronic and paper means are the same.
No unexpected or technical difficulties were encountered with the PDA technology or in transferring the data to the patients’ medical records. As expected from previous PDA studies, users experienced some initial questions about using the devices, which were generally resolved after successfully completing the diary entry the first time. At no time did any of the patients report an inability to complete the diaries.
End-of-study survey responses of many of the participants using the electronic diaries reported that the charts were very helpful to them (44%) and to their doctors (47%). However, only 23% from this group reported that the charts resulted in changes to the care they received from their doctor and less than 15% of these patients believed that their doctor used the diary information to make a change in their daily routine or medication (Table 3).
Table 3.
Group Differences in Electronic Versus Paper Diary on Items from the Patient Satisfaction Questionnaire (% Agree)
| Variable a | Electronic (n=43) |
Paper (n=35) |
P- value |
|---|---|---|---|
| I thought the diary was easy to use and understand. | 67.4 | 91.4 | 0.013 |
| I found the body map useful. | 76.7 | 69.7 | 0.489 |
| The diary helpful to me in understanding my pain and its symptoms. | 53.4 | 68.6 | 0.176 |
| The pain charts were very helpful to my doctor. | 46.5 | --- | --- |
| The pain charts with my results were very helpful to me. | 44.2 | --- | --- |
| Tracking helps me to understand my pain | 42.9 | 44.1 | 0.912 |
| I think the charts helped improve the care I received from my doctor. My doctor suggested a change in daily routine |
23.3 14.3 |
--- 32.3 |
--- 0.067 |
| My doctor suggested a change in my medication | 11.9 | 36.7 | 0.013 |
NS = nonsignificant.
Each variable rated as “strongly disagree,” “disagree,” “neither,” “agree,” “strongly agree.” Percentages in the table are combined “strongly agree” and “agree” scores.
Thirteen physicians (seven attendings and six pain fellows) agreed to complete the Physician Satisfaction Questionnaire at the end of the trial. All of the physicians had access to the electronic diary data and were familiar with the study protocol. No differences were found between the attending physicians and pain fellows, except that the pain fellows were less likely to believe that the electronic diaries would positively change the patients’ lives (P<0.05). The majority of both groups was satisfied with the electronic diaries and believed that they were clinically useful (Table 4).
Table 4.
Physician End-of-Study Evaluations (n = 14; percent agree)
| Questionnaire Itema | Pain Physicians (n=14) |
|---|---|
| Patient diary data is a waste of time. (disagree) b |
92.9 |
| If I had a printout of patient diary data, I would use the information. | 92.9 |
| I am satisfied with the way the electronic diaries identifies pain on the body map. |
92.9 |
| I am satisfied with the way the electronic diary can be used in the clinic. | 92.9 |
| I think that using electronic diaries in the clinic will improve our overall practice. |
92.9 |
| I believe that feedback from electronic diaries will not improve patient outcome. (disagree) b |
85.7 |
| Reviewing diary data with patient present is important. | 85.7 |
| I believe that the electronic diaries were an added burden to the clinic. (disagree) b |
85.7 |
| Diary data would help identify and prevent future patient problems. | 78.6 |
| I have time to examine individual patient diary data during clinic hours. | 71.4 |
| I am dissatisfied with the pain graphs. (disagree) b | 71.4 |
| Electronic diaries are far more beneficial than paper diaries. | 64.3 |
| I am satisfied with the way the electronic diaries help patients understand their pain. |
64.3 |
| I am satisfied with the way electronic diaries track medication use. | 61.5 |
| I believe that the electronic diaries positively changed my patients’ lives. |
57.1 |
| I believe that the regular use of electronic diaries will reduce healthcare costs |
51.1 |
Responses were: “strongly agree,” “agree,” “neither agree nor disagree,” “disagree,” “strongly disagree.” Responses in this table are percent of combined “strongly agree” and “agree.”
Reverse scoring
Semi-structured telephone interviews were performed on all of the attending physicians (n=7) and a representative group of study patients (n=6 patients) selected at random to determine how they felt about the pain diaries and if they had recommendations for improvement. The interviews, digitally recorded and transcribed, ranged between 30 to 60 minutes in length. No patients declined to be interviewed once they were contacted. The patients reported that they had a better understanding of their pain and a greater ability to cope as a result of completing the monthly diaries. They further reported that the act of completing the monthly diaries helped them to become aware of how pain impacted their lives. Two patients (PT2, 4) reported positive experiences in which the details of the diary and their specific pain diary tracking information were discussed during their appointment. PT2 described how discussing the level of pain was helpful in determining medication dosages and resulting self-management stating “…I woke up at night trying to mark [the levels of pain] down and trying to decide do I really need medication or is it bad enough that I do need to take a medication? Is the level above a 5? Do I really need it or can I get away with focusing on something else and not taking medication? And using it that way to help me judge. You know. And that was what the diaries have helped.” PT4 described how specific questions in the diary related to depression and anxiety helped to facilitate a conversation with the treating physician. As a result of discussing the diary, modified approaches to reduce depression and anxious symptoms were discussed (such as breathing). In particular, one patient (PT5) commented that electronic tracking facilitated new items to discuss during his/her appointments stating “They have been very willing to incorporate me into the conversation and also into the matter of what they’re going to do or considering doing, and what did I think about it.”
The physicians reported in the semi-structured interviews that the diaries would conceivably be useful in a clinic setting, but noted that they were not inclined to consult the data regularly, either because they forgot or were too busy. When asked specifically about whether they used the diary in discussion with their patient, two physicians reported limited use of the diary. DR 1 said, “… I didn’t really use it [diary] to make judgments too much about their care. Just kind of a general gestalt of how they’re doing.” DR 4 expressed regret for not utilizing the diary more in practice. “I didn’t use it…I didn’t rely on it as much as if it was a regular part of my assessment…I should have…I saw it more as an experimental thing…and retrospectively…I could have probably picked up some of his symptoms…I don’t think it would have changed his outcome, but it just might‥‥” Another physician (DR 3) reviewed the diary to assess “changes in the various metrics that were tracked.” The physicians as a group also held mixed opinions about the body maps and graphs of the diary data. Four felt the information they offered was not useful, especially when a patient is stable, while two reported that the diary data was useful. DR 2 said, “…unless it’s a rare situation where it’s [pain] moving or it’s changing…” the body graphs are not as helpful. DR5 captured the essence of how the body map was most useful in assessing pain status (DR1 and DR7 reflected similar feedback): “I don’t know that I found the body map that helpful‥‥for instance, take [name] case. I mean [patient] has pain in his shoulder‥‥and it doesn’t really change, so I mean it’s been that way for 15 years. It’s kind of additional information that doesn’t really add much to what I already know…maybe I can envision some patients whose pain location changes in some way that that might be helpful, but not in his case.” The physicians all believed that the diary data would have been consulted more often if all patients in the clinic were required to complete it. They also shared their belief that they did not anticipate much change in the pain graphs over the course of the 10-month study and they did not believe that dramatic changes in treatment were indicated.
Discussion
This study examined differences in treatment helpfulness and outcome between patients with chronic pain who used monthly electronic diaries with feedback of their progress and patients using paper diaries and no summary feedback over 10 months. No pre-post differences in pain, mood, function, medication use, or perceived treatment helpfulness were found between groups. No differences were also found in treatment helpfulness between those using electronic diaries and those using paper diaries, however, electronic diary users were more likely to remain in the study and complete their monthly sessions. Most patients felt that both diaries were easy to use and improved their understanding of their conditions, and most treating physicians expressed a strong preference for electronic diaries over paper diaries, indicating that they would agree to adopt them in the clinic setting. However, patients in the electronic diary group overwhelmingly reported that their providers did not suggest a change in their routine or medication and the diary feedback did not change the care they received by their doctor. Thus, while physicians reported that they felt that electronic tracking was important, they did not regularly view the charts provided or incorporate this information in their treatment decisions.
Support can be found in the literature that monitoring alone can offer information that can impact learning and change behavior. According to learning theory proposed by Bandura,43 and as discussed by Carter et al.,44 data collection with diaries, in particular with hand-held or computerized devices, can enhance learning and behavior change. This was found to be true of the participants of this study. Interestingly, the physicians reported in the semi-structured interview results that the diaries would conceivably be useful in a clinic setting, but noted that they were not inclined to consult the data regularly, either because they forgot or were too busy. It is relevant to note that information on usefulness of the electronic diary was obtained through the end-of-study evaluation forms. On these forms the physicians conceptually reported that electronic diaries in the clinic would improve the practice (93% agree), that reviewing the diary data with the patient present was important (86% agree), and that the data would help to identify future problems (79% agree). The physician interviews revealed that they unanimously believed that the diary data would be consulted if all patients were required to complete it. They also shared their belief that because the pain patients in this study had pain for many years (average 10.5 years) and their treatment regimens were generally stable, they did not anticipate much change in the pain graphs over the course of the 10-month study and they did not believe that dramatic changes in treatment were indicated. This finding may suggest that changes in management (as reported by paper diary patients) may not be equal to better pain control. Additional exploration would be important to understand whether having access to the graphs from the electronic diary may lead to fewer changes in management based on the length and stability of the pain conditions in this population. Another conclusion from this study is that regular monitoring may not be required or be beneficial among persons with chronic pain who are stabilized over many years.
Enabling pain practitioners to identify historical trends in symptom reporting and changes in pain, mood, or activity fluctuations has potential to provide a more accurate indication of patient status within a busy clinic practice beyond asking, “How has your pain been?” One would think that electronic data capture and up-dated summary of progress with the use of electronic data capture could also potentially improve patient satisfaction with the care that they are given. It was anticipated that the attention from the physicians when examining the summary graphs of the patients in the electronic diaries group would improve patient satisfaction. However, a significant effect was not found. In a study in which guidelines and algorithms for the treatment of chronic pain were disseminated within primary care physician clinics,45 many physicians showed reluctance to regularly consult the algorithms and to change their practice behavior, despite initially welcoming input about managing difficult pain patients. Similarly, there may have been some reluctance by the physicians over the 10-month study period to modify practice behavior, despite their interest in using the diary technology. When introducing new technology and a change of practice within each medical visit, it is important to provide additional support for the patients and providers in order to successfully change the required behavior. It is possible that incorporating the pain diary more seamlessly into practice (such as linking directly to an electronic medical record) would encourage physicians to adopt the new technology and diary feedback as part of each patient visit and improve the use of the pain summary data. A further benefit of having instant access to electronic diary data is cumulative analyses of the patients served in the clinic to assess overall trends in outcome.
Although there was not a strong preference for electronic over paper diaries, patients assigned to the electronic diaries were more likely to complete the study and to comply with the monthly monitoring than those assigned to the paper diaries, in keeping with past research.14, 17, 46 The treating physicians, while not found to make major changes in patient care in the 10-month period, also reported interest in the potential benefits of adopting this technology in everyday clinical practice. These findings support results from our pilot study of 36 patients using a crossover design, which reported a trend toward patients saying that they would continue to use the electronic diary (61%) compared to a paper diary (47%) if it were provided.
One possible conclusion drawn from this study could be that because the study population had an average of 10 years since onset of pain and did not show wide fluctuations in their pain status or related activities (e.g., many returned to the pain center on stable doses of their medications and often reported that their pain and symptoms are unchanged), this may have limited how much change in medication or treatment was required. Future investigations might consider enrolling subacute pain patients who have a greater likelihood of need for change in their medical treatment. In addition, the importance of a pain-tracking diary in a pain management clinic might have an influence on psychosocial aspects of pain (coping, understanding, learning to live with pain) rather than impacting changes in medical treatment. This explanation is supported by the semi-structured interviews.
The results of the qualitative interviews offered additional information about the study and, overall, indicated that the physicians and the patients felt that the diaries were beneficial. Patients felt that understanding their pain condition impacted how they perceived their use of medications and behaviors and that better awareness of their condition led to improved self-management of their pain, including empowering to them to “face” their pain, focus on improvements rather than limitations to daily life, and feel like their pain was more manageable. Importantly, reports from the qualitative interviews indicated that the electronic tracking also helped patients to track aspects of their pain not previously considered, such as changes in the pattern of their pain levels, which encouraged changes in daily activities and medication usage. The physicians felt that the diary was particularly useful for patients with fluctuating patterns of pain as opposed to those with stable pain patterns. They commented on the potential utility of the diary as a regular part of the pain clinic. Two main themes which arose from the physician interviews on future use of clinic-based electronic diaries were (1) attention to the time and effort required to institute the use of electronic diaries, and (2) the potential of the electronic diary data to capture subjective quality-of-life information. One doctor voiced concern about the potential demand required to teach patients how to use the diary and the decreasing amount of time that doctors have with each patient. If in-clinic electronic diary tracking is found to have added value for patient self management, further understanding of how this technology can be effectively integrated into a clinic with limited added burden placed on the staff will be important to understand.
The results of this study could be explained in part with the use of Normalization Process Theory.47,48 Normalization Process Theory is an explanatory model that helps managers, clinicians, and researchers understand the dynamic processes that occur when people put new technologies and complex interventions into practice. Innovation in healthcare promises better ways of organizing and delivering treatment by incorporating improvements in the clinical setting with the goals of implementing cost-effective services specifically designed to reduce the treatment burdens of chronic illness. Most research on healthcare innovation focuses on the outcomes of innovations, measuring their impact and exploring their effects. However, outcomes evaluations alone are often not sufficient to help understand how these effects come about. Rather, efforts are needed to understand the dynamics of the implementation process of new innovative technology into existing clinical settings. This requires an understanding of the integration of these changes and to focus on the processes that lead to innovations as they become embedded in everyday work. Normalization Process Theory suggests that the identification of those factors that promote or inhibit the incorporation of heathcare technologies is most important. Even though no differences were found on outcome measures between groups, the qualitative feedback from the physicians and patients in this study was helpful in understanding these outcomes.
There are limitations of this study. First, while eligible pain patients were scheduled for monthly follow-up, more patients than expected cancelled or changed their appointments resulting in fewer data points. We anticipated monthly data points over 10 months, but the subjects averaged only five data points over the course of the study. This average includes all participants with visits ranging from 1–11. Second, the dropout rate in both groups was higher than anticipated, which might have influenced the outcome. Further investigations of the factors contributing to compliance are needed. A third possible limitation is that only a select number of subjects participated out of a busy clinic of over 7,000 annual visits and identification of the study subjects among the other patients was not always clear. Improvements in how charts are integrated into the electronic medical record prior to office visits and how they can be readily accessed would allow for better use of the tracking features. Fourth, the participants represented a heterogeneous group of chronic noncancer pain patients. This study collected data on pain region but did not specifically request information regarding diagnosis or primary type of pain. Certain subgroups of pain patients, including patients with cancer pain, may result in different experiences with diary use. Finally, a cluster randomized trial design in which the clinic was the unit of randomization rather than the patients may have provided information about how the diary can be implemented at the clinic level.
Conclusions
These results move beyond previous studies to lend insight about how patients perceive the use of in-clinic electronic and paper diaries and how providers may or may not adapt their practice to use feedback from computer technology. Initial findings suggest that the use of electronic diaries with summary data is perceived to be helpful, but this perception does not necessarily result in changes in treatment practice or outcome. A better understanding of the psychosocial contributions of electronic tracking and investigating differences between daily inhome versus less frequent in-clinic monitoring and the role of body map data in predicting changes in pain management is needed. Future studies are also needed to investigate whether electronic documentation of pain status would lead to improved standardization of care. Continuing research in this area will also inform how information technology can be better integrated into a treatment center to improve patient management and clinic efficiency.
Acknowledgments
The authors would like to thank the staff and patients at Brigham and Women’s Hospital for their assistance. Special thanks are also extended to Li Chen, David Janfaza, Edward Michna, Sanjeet Narang, Srdjan Nedeljkovic, Sarah O’Shea, Loc Pham, Edgar Ross, Sharonah Soumekh, Ajay Wasan, and Christina Yantsides for their invaluable contribution to this study.
This work was supported by a grant from the National Institutes of Health, National Institute of Dental and Craniofacial Research (1R43 DE014797-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Maniadakis N, Gray A. The economic burden of back pain in the UK. Pain. 2002;84:95–103. doi: 10.1016/S0304-3959(99)00187-6. [DOI] [PubMed] [Google Scholar]
- 2.Elliott TE, Murray DM, Elliot BA, et al. Physician knowledge and attitudes about cancer pain management: a survey from the Minnesota Cancer Pain Project. J Pain Symptom Manage. 1995;10:494–504. doi: 10.1016/0885-3924(95)00100-d. [DOI] [PubMed] [Google Scholar]
- 3.Simoens S, Scott A, Sibbald B. Job satisfaction, work-related stress and intentions to quit of Scottish GPS. Scot Med J. 2002;47:80–86. doi: 10.1177/003693300204700403. [DOI] [PubMed] [Google Scholar]
- 4.Marwick C. New advocates of adequate treatment say have no fear of pain or prosecution. JAMA. 1999;281:406–407. [PubMed] [Google Scholar]
- 5.Joranson DE, Gilson AM, Dahl JL, Haddox JD. Pain management, controlled substances, and state medical board policy: a decade of change. J Pain Symptom Manage. 2002;23:138–147. doi: 10.1016/s0885-3924(01)00403-1. [DOI] [PubMed] [Google Scholar]
- 6.Jamison RN, Fanciullo G, Baird JC. Introduction: special series on computer and information technology in the assessment and management of patients with pain. Pain Med. 2002;S3:83–84. [Google Scholar]
- 7.Wire B. What Americans really want from their doctor: Roper Starch survey results reveals what patients want and how they feel about whey they're getting. [Accessed May 5, 2008]; Available from: Business Services Industry, http://findarticles.com/p/articles/mi_m0EIN/is_1996_July_19/ai_18496582.
- 8.Aiello EJ, Taplin S, Reid R, et al. In a randomized controlled trial, patients preferred electronic data collection of breast cancer risk-factor information in a mammography setting. J Clin Epidem. 2002;59:77–81. doi: 10.1016/j.jclinepi.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Bushnell DM, Martin ML, Parasuraman B. Electronic versus paper questionnaires: a further comparison in persons with asthma. J Asthma. 2002;40:751–762. doi: 10.1081/jas-120023501. [DOI] [PubMed] [Google Scholar]
- 10.Cook AJ, Roberts DA, Henderson MD, et al. Electronic pain questionnaires: A randomized crossover comparison with paper questionnaires for chronic pain assessment. Pain. 2004;110:310–317. doi: 10.1016/j.pain.2004.04.012. [DOI] [PubMed] [Google Scholar]
- 11.Jamison RN, Raymond SA, Slawsby EA, McHugo GJ, Baird JC. Pain assessment in patients with low back pain: comparison of weekly recall and momentary electronic data. J Pain. 2006;7:192–199. doi: 10.1016/j.jpain.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Johannes C, Woods J, Crawford S, et al. Electronic versus paper instruments for daily data collection. Ann Epidemiol. 2000;10:457. doi: 10.1016/s1047-2797(00)00141-1. AU: PLS PROVIDE FULL PAGE RANGE. [DOI] [PubMed] [Google Scholar]
- 13.Kvien TK, Mowinckle P, Heiberg T, et al. Performance of health status measures with a pen based personal digital assistant. Ann Rheum Dis. 2005;64:1480–1484. doi: 10.1136/ard.2004.030437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jamison RN, Raymond SA, Levine JG, et al. Electronic diaries for monitoring chronic pain: 1-year validation study. Pain. 2001;91:277–285. doi: 10.1016/S0304-3959(00)00450-4. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen HQ, Carrieri-Kohlman V, Rankin SH, Slaughter R, Stulbarg MS. Internet-based patient education and support interventions: a review of evaluation studies and directions for future research. Computers Biol Med. 2004;34:95–112. doi: 10.1016/S0010-4825(03)00046-5. [DOI] [PubMed] [Google Scholar]
- 16.Raymond SA, Ross RN. Electronic subject diaries in clinical trials. Appl Clin Trials. 2000;9:48–58. [Google Scholar]
- 17.Stone AA, Broderick JE, Schwartz JE, et al. Intensive momentary reporting of pain with an electronic diary: reactivity, compliance, and patient satisfaction. Pain. 2003;104:343–351. doi: 10.1016/s0304-3959(03)00040-x. [DOI] [PubMed] [Google Scholar]
- 18.Shiffman S, Swaltney CJ, Balabanis MH, et al. Immediate antecedents of cigarette smoking: an analysis from ecological momentary assessment. J Abnorm Psychol. 2002;111:531–545. doi: 10.1037//0021-843x.111.4.531. [DOI] [PubMed] [Google Scholar]
- 19.Sieck WA, McFall RM. Some determinants of self-monitoring effects. J Consult Clin Psychol. 1976;44:958–965. doi: 10.1037//0022-006x.44.6.958. [DOI] [PubMed] [Google Scholar]
- 20.Kenardy JA, Dow MGT, Johnston DW, et al. A comparison of delivery methods of cognitive behavioral therapy for panic disorder: an international multicenter trial. J Consult Clin Psychol. 2003;71:1068–1075. doi: 10.1037/0022-006X.71.6.1068. [DOI] [PubMed] [Google Scholar]
- 21.Newman MG, Consoli AJ, Taylor CB. A palmtop computer program for the treatment of generalized anxiety disorder. Behav Mod. 199;23:597–619. doi: 10.1177/0145445599234005. [DOI] [PubMed] [Google Scholar]
- 22.Jamison RN, Gracely RH, Raymond SA, et al. Comparative study of electronic vs. paper VAS ratings: a randomized, crossover trial using healthy volunteers. Pain. 2002;99:341–347. doi: 10.1016/s0304-3959(02)00178-1. [DOI] [PubMed] [Google Scholar]
- 23.Peters ML, Sorbi MJ, Kruise DA, et al. Electronic diary assessment of pain, disability and psychological adaptation in patients differing in duration of pain. Pain. 2000;84:181–192. doi: 10.1016/s0304-3959(99)00206-7. [DOI] [PubMed] [Google Scholar]
- 24.Tseng HM, Macleod HA, Wright P. Computer anxiety and measurement mood change. Comp Hum Behav. 1997;13:305–316. [Google Scholar]
- 25.VanDenKerkhof EG, Goldstein DH, Lane J, Rimmer MJ, Van Dijk JP. Using a personal digital assistant enhances gathering of patient data on an acute pain management service: a pilot study. Can J Anaesth. 2003;50:368–375. doi: 10.1007/BF03021034. [DOI] [PubMed] [Google Scholar]
- 26.Wilkie DJ, Judge MKM, Berry DL, et al. Usability of a Computerized PAINReportIt in the general public with pain and people with cancer pain. J Pain Symptom Manage. 2003;25:213–224. doi: 10.1016/s0885-3924(02)00638-3. [DOI] [PubMed] [Google Scholar]
- 27.Marceau LD, Link C, Jamison RN, Carolan S. Electronic diaries as a tool to improve pain management: is there any evidence? Pain Med. 2007;S3:S101–S109. doi: 10.1111/j.1526-4637.2007.00374.x. [DOI] [PubMed] [Google Scholar]
- 28.Cleeland CS, Ryan KM. Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore. 1994;23:129–138. [PubMed] [Google Scholar]
- 29.Daut RL, Cleeland CS, Flanery RC. Development of the Wisconsin Brief Pain Questionnaire to assess pain in cancer and other diseases. Pain. 1983;17:197–210. doi: 10.1016/0304-3959(83)90143-4. [DOI] [PubMed] [Google Scholar]
- 30.Keller S, Bann CM, Dodd SL, et al. Validity of the Brief Pain Inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain. 2004;20:309–318. doi: 10.1097/00002508-200409000-00005. [DOI] [PubMed] [Google Scholar]
- 31.Mendoza TR, Mayne T, Rublee D, Cleeland CS. Reliability and validity of a modified Brief Pain Inventory short form in patients with osteoarthritis. Eur J Pain. 2006;10:353–361. doi: 10.1016/j.ejpain.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan MJL, Bishop S, Pivik J. The Pain Catastrophizing Scale: development and validation. Psychol Assess. 1995;7:524–532. [Google Scholar]
- 33.Sullivan MJL, Neish N. Psychological predictors of pain during dental hygiene treatment. Probe. 1997;31:123–127. [PubMed] [Google Scholar]
- 34.Fairback JCT, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 35.Fairback J, Davies K, Couper J, Obrien J. The Oswestry Low Back Pain Disability Questionnaire. Physiother. 1980;66:271–273. [PubMed] [Google Scholar]
- 36.Grönblad M, Hupli M, Wennerstrand P, et al. Intercorrelation and test-retest reliability of the Pain Disability Index (PDI) and the Oswestry Disability Questionnaire (ODQ) and their correlation with pain intensity in low back pain patients. Clin J Pain. 1993;9:189–195. doi: 10.1097/00002508-199309000-00006. [DOI] [PubMed] [Google Scholar]
- 37.Wittink J, Turk D, Carr DB, Sukiennik A, William R. Comparison of the redundancy, reliability, and responsiveness of change among SF-36, Oswestry Disability Index, and Multidimensional Pain Inventory. Clin J Pain. 2004;20:133–142. doi: 10.1097/00002508-200405000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measure. 1977;1:385–401. [Google Scholar]
- 39.Santor DA, Zuroff DC, Ramsey JO, Cervantes P, Palacios J. Examining scale disciminability in the BDI and CES-D as a function of depressive severity. Psychol Assess. 1995;7:131–139. [Google Scholar]
- 40.Irwin M, Artin KH, Oxman MN. Screening for depression in older adults: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Arch Intern Med. 1999;159:1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- 41.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D. Amer J Prevent Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 42.Chapman SL, Jamison RN, Sanders SH. Treatment helpfulness questionnaire: a measure of patient satisfaction with treatment modalities provided in chronic pain management programs. Pain. 1996;68:349–361. doi: 10.1016/s0304-3959(96)03217-4. [DOI] [PubMed] [Google Scholar]
- 43.Bandura A. Behavior therapy and models of man. Amer Psychol. 1974;29:859–869. [Google Scholar]
- 44.Carter BL, Day SX, Cinciripini PM, Wetter DW. Momentary health interventions: where are we and where are we going? In: Stone AA, Shiffman S, Atienza AA, Nebeling L, editors. The science of real-time data capture. New York: Oxford University Press; 2007. pp. 289–307. [Google Scholar]
- 45.Jamison RN, Gintner L, Rogers JF, Fairchild DG. Disease management for chronic pain: barriers of program implementation with primary care physicians. Pain Med. 2002;3:92–101. doi: 10.1046/j.1526-4637.2002.02022.x. [DOI] [PubMed] [Google Scholar]
- 46.Stone AA, Shiffman S, Schwartz JE, Broderick JE, Hufford MR. Patient compliance with paper and electronic diaries. Control Clin Trials. 2003;24:182–199. doi: 10.1016/s0197-2456(02)00320-3. [DOI] [PubMed] [Google Scholar]
- 47.May C, Finch T. Implementation, embedding, and integration: an outline of Normalization Process Theory. Sociology. 2009;43:535–554. [Google Scholar]
- 48.May C, Mair FS, Finch T, et al. Development of a theory of implementation and integration: Normalization Process Theory. Implement Sci. 2009;4 doi: 10.1186/1748-5908-4-29. article 29. Available from: http://www.implementationscience.com/content/4/1/29. [DOI] [PMC free article] [PubMed]