Abstract
Bacterial cytoskeletal proteins are an emerging set of targets for antibiotic development. This paper describes oligochlorophen analogs based on the monomer 4-chloro-2,6-dimethylphenol as antimicrobial agents against Bacillus anthracis. The most potent analogs have a MIC of 160 to 320 nM against B. anthracis and may target the cytoskeletal protein FtsZ. B. anthracis develops resistance to the oligochlorophens at a rate of 4.34 × 10−10 per generation, which is ∼10-fold lower than that of commercial antibiotics used to treat this human pathogen.
Bacillus anthracis infections typically are treated by long-term exposure to antibiotics, during which resistance to these compounds may emerge (2, 4, 19). The discovery of new cellular targets and the development of inhibitors of these proteins will play a key role in this clinical tug of war. Bacterial cytoskeletal proteins are attractive targets for antibiotic development, as they are conserved, essential, and play a central role in cell physiology in eubacteria (10, 13, 18). The best-characterized protein in this family arguably is FtsZ, which is a GTPase with structural homology to eukaryotic tubulin (7). This protein assembles into the Z ring at the site of cell division, which forms the scaffold for the divisome and directs the remodeling of the cell wall to produce a daughter cell.
A screen for small-molecule inhibitors of FtsZ identified several hits, including 3Z1; we use the nomenclature nZ1, where Z1 corresponds to the zantrin oligomeric structure described by Margalit et al. and n indicates the number of repeating structural units (Fig. 1) (12). 3Z1 inhibits the GTPase activity of recombinant Escherichia coli FtsZ in vitro (12). Several groups previously had described 3Z1 and structurally related compounds as antibiotics (3, 14, 15). Although these compounds have not been explored as clinical therapeutic agents, 2Z1 has been used as a commercial anthelmintic agent, and its 50% lethal dose (LD50) is 1,506 (95% confidence interval [CI], 1,310 to 1,760) and 1,683 (95% CI, 1,402 to 1,986) mg/kg of body weight in male and female rats, respectively (6).
FIG. 1.
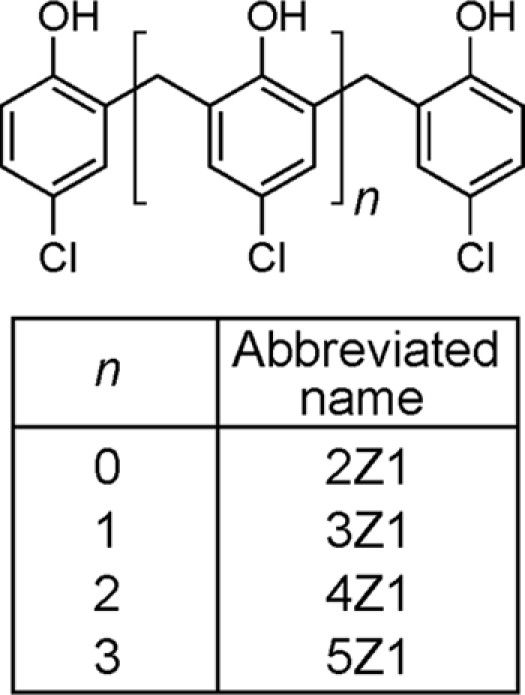
Structure of oligochlorophens. Chemical structures of the compounds studied; n indicates the number of p-chlorophenol units.
Guided by the observation that 3Z1 inhibited Bacillus cereus with a MIC of ∼0.3 μM, we investigated this compound and structurally related oligomers as antibiotics against B. anthracis. Polyphenols have several characteristics that make them attractive as therapeutic agents: (i) they are nontoxic to humans; (ii) they are consumed in large amounts daily via fruits and vegetables; (iii) they are rapidly absorbed by the lumen of the gut; and (iv) they have been implicated in the prevention of diseases (17). We were particularly interested in exploring these compounds as a test bed for determining the resistance profile of bacteria exposed to inhibitors of the bacterial cytoskeleton. While the development of resistance is unlikely to be a problem with an absolute solution, the treatment of cells with antimicrobials that are designed to disrupt the function of cytoskeletal proteins may reduce the rate at which these events occur (1).
MIC determination.
We determined MICs by the macrodilution technique according to the National Committee for Clinical Laboratory Standards criteria for aerobic bacteria (16). The following strains were grown in Luria-Bertani medium using the conditions indicated in parentheses: Escherichia coli strain MC1000 (30°C, shaking at 200 rpm, 14 h), Pseudomonas aeruginosa strain K (37°C, shaking at 200 rpm, 16 h), B. cereus strain UW85 (37°C, shaking at 200 rpm, 16 h), and Staphylococcus aureus strains 100 and 361 (37°C, static conditions, 14 h). We grew Caulobacter crescentus strain CB15N in peptone-yeast extract (5) medium at 30°C with shaking at 200 rpm for 22 h. Enterococcus faecalis strain 1131 and B. anthracis Sterne strain 7702 were grown in brain heart infusion (BHI) medium at 37°C in a static incubator for 14 and 16 h, respectively. We diluted cultures to 5 × 105 cells/ml in growth medium for the starting inoculum. Antibiotics were dissolved in dimethylsulfoxide (DMSO), added to the first tube in a series, and diluted through the set of inoculated tubes to generate a 2-fold dilution series. We prepared control experiments with the same DMSO concentration found in the tubes containing the highest antibiotic concentration. We determined MIC endpoints by finding the lowest concentration of compound that prevented growth in triplicate by visual inspection; to confirm these values, we periodically measured the lowest antibiotic concentration at which there was no detectable absorbance at λ = 600 nm.
Passaging resistant mutants.
We determined initial MICs (passage 0) for B. anthracis Sterne 7702 and passaged cultures of bacteria that survived at the highest concentration of antibiotic into fresh culture media. B. anthracis Sterne 7702 was grown to exponential phase (absorbance, ∼0.8 to 0.9; λ = 600 nm) and used to inoculate the subsequent culture for MIC determination. The process was repeated, and the dilution series was adjusted to include concentrations 128-fold higher and 4-fold lower than the previously determined MIC.
Spontaneous resistant mutant rate determinations.
We performed a Luria-Delbrück fluctuation test (11) to evaluate the spontaneous rate of acquiring antibiotic-resistant variants. We centrifuged fresh, saturated cultures of B. anthracis Sterne 7702 for 5 min at 3,000 × g, removed most of the supernatant, and resuspended the pellet in ∼100 μl of residual supernatant. Resuspended samples were spread on 2% agar BHI medium containing either 80 μM rifampin or 80 μM 3Z1. Cells from 20 parallel cultures (4 ml) were plated for the rifampin experiment. Cells from 10 parallel cultures (8, 12, or 16 ml) were plated for the 3Z1 experiment. Plates were incubated at 37°C in a static incubator for 48 h before resistant colonies were counted. We determined the population size in each experiment by selecting cultures for enumeration experiments. These cultures were diluted with 0.1% phosphate-buffered peptone water in a 10-fold dilution series and spread on nonselective 2% agar BHI plates. We determined the population density after 16 to 24 h by counting plates that had between 20 and 200 colonies. The resistant mutation rate was estimated using the Ma-Sandri-Sarkar maximum likelihood estimator (MSS-MLE) method through the web tool developed by Hall and coworkers (8).
The nZ1 oligomers have MIC values in the low nM to μM range against a variety of eubacteria (Table 1). Notably, 3Z1 and 4Z1 are potent antibiotics against the human pathogens B. anthracis and B. cereus, respectively. We measured the development of the drug resistance of these compounds against B. anthracis Sterne strain 7702 and found that after 18 passages, the bacterium had gained a 2-fold increase in resistance against 3Z1 and no improved resistance against 4Z1 (Fig. 2). The strain developed complete resistance to rifampin and penicillin G after six passages.
TABLE 1.
Antimicrobial activity of nZ1 analogsa
| Species | MIC (μM) of: |
|||
|---|---|---|---|---|
| 2Z1 | 3Z1 | 4Z1 | 5Z1 | |
| E. coli MC1000 | 160 | 5c | >80 | >80 |
| P. aeruginosa K | >320 | 40b,c | >80 | >80 |
| B. cereus UW85 | 10 | 0.3 | 0.08 | 0.3 |
| C. crescentus CB15N | 20 | 2.5 | 0.3 | 5 |
| S. aureus FRI 100 | 20 | 0.08c | 0.16 | 5 |
| S. aureus FRI 361 | 20 | 0.6 | 0.3 | 5 |
| E. faecalis 1131 | 80 | 1.3 | 0.3 | 0.6 |
| B. anthracis Sterne 7702 | 5 | 0.3c | 0.16 | 1.3 |
nZ1 compounds have potent antibacterial activity against both Gram-negative and Gram-positive bacteria.
Confirmed value from reference 5.
Determined using nine replicates by measuring absorbance at λ = 600 nm.
FIG. 2.
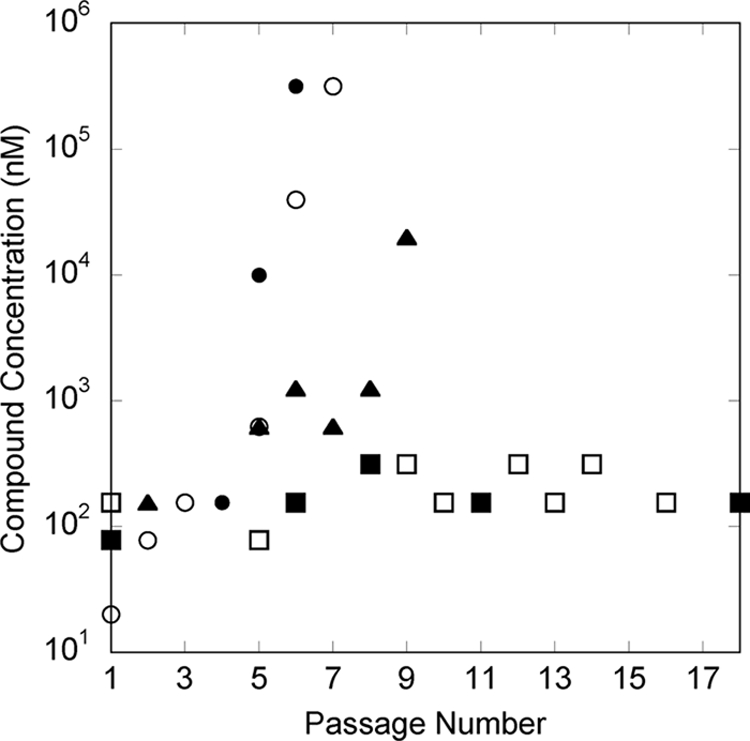
Emergence of resistant mutants in Bacillus anthracis. B. anthracis Sterne strain 7702 was cultured in the presence of different concentrations of antibiotics. The compound concentrations represent the MIC value (nM), and the passage number represents the number of consecutive cultivations performed previously against the antibiotic for resistance. Data for rifampin (•), penicillin G (○), tetracycline (▴), 3Z1 (▪), and 4Z1 (□) are shown. Data points show the initial MIC, changes in MIC during passaging, and the final MIC. Rifampin, tetracycline, and 3Z1 overlap at passage 1, and the symbols for the first two antibiotics are obscured by the symbol for 3Z1.
The rate at which B. anthracis Sterne strain 7702 becomes resistant to rifampin and 3Z1 was 2.65 × 10−9 (95% confidence interval, 4.11, 1.44) and 4.34 × 10−10 (95% confidence interval, 7.26, 2.03) per generation, respectively. This result indicates that mutants resistant to 3Z1 are less likely to occur than those resistant to rifampin. The small-molecule inhibitor of FtsZ developed by Haydon and coworkers (e.g., PC190723) was tested against Staphylococcus aureus ATCC 29213, which acquired resistance at a rate of 2 × 10−8 (9).
Tetracycline (MIC, ∼70 nM) and penicillin G (MIC, ∼20 nM) are antibiotics commonly used to treat B. anthracis infections (19). 3Z1 has a MIC of ∼320 nM against B. anthracis, which is comparable to those of these commercial antibiotics. This class of polyphenols has a range of properties, including a scaffold amenable to functionalization with a variety of substituents, that make it a reasonable starting point for antibiotic development. The further characterization of the properties of this class of compounds may lead to new pharmaceuticals for the treatment of bacterial infections.
Acknowledgments
We acknowledge funding from the Human Frontiers Science Program (RGY0069/2008-C), DARPA, USDA (WIS00974), and a Searle Scholar Award.
We thank Kathleen A. Glass for B. anthracis Sterne strain 7702.
Footnotes
Published ahead of print on 21 June 2010.
REFERENCES
- 1.American Academy of Microbiology. 2009. Antibiotic resistance: an ecological perspective on an old problem. American Society for Microbiology, Washington, DC. [PubMed]
- 2.Athamna, A., M. Athamna, N. Abu-Rashed, B. Medlej, D. J. Bast, and E. Rubinstein. 2004. Selection of Bacillus anthracis isolates resistant to antibiotics. J. Antimicrob. Chemother. 54:424-428. [DOI] [PubMed] [Google Scholar]
- 3.Beaver, D. J., R. S. Shumard, and P. J. Stoffel. 1953. Preparation and bacteriostatic properties of substituted trisphenols. J. Am. Chem. Soc. 75:5579-5581. [Google Scholar]
- 4.Choe, C. H., S. S. Bouhaouala, I. Brook, T. B. Elliott, and G. B. Knudson. 2000. In vitro development of resistance to ofloxacin and doxycycline in Bacillus anthracis Sterne. Antimicrob. Agents Chemother. 44:1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ely, B. 1991. Genetics of Caulobacter crescentus. Methods Enzymol. 204:372-384. [DOI] [PubMed] [Google Scholar]
- 6.Gaines, T. B., and R. E. Linder. 1986. Acute toxicity of pesticides in adult and weanling rats. Fund. Appl. Toxicol. 7:299-308. [DOI] [PubMed] [Google Scholar]
- 7.Graumann, P. L. 2007. Cytoskeletal elements in bacteria. Annu. Rev. Microbiol. 61:589-618. [DOI] [PubMed] [Google Scholar]
- 8.Hall, B. M., C.-X. Ma, P. Liang, and K. K. Singh. 2009. Fluctuation AnaLysis CalculatOR: a web tool for the determination of mutation rate using Luria-Delbruck fluctuation analysis. Bioinformatics 25:1564-1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haydon, D. J., N. R. Stokes, R. Ure, G. Galbraith, J. M. Bennett, D. R. Brown, P. J. Baker, V. V. Barynin, D. W. Rice, S. E. Sedelnikoca, J. R. Heal, J. M. Sheridan, S. T. Aiwale, P. K. Chauhan, A. Srivastava, A. Taneja, I. Collins, J. Errington, and L. G. Czaplewski. 2008. An inhibitor of FtsZ with potent and selective anti-staphylococcal activity. Science 321:1673-1675. [DOI] [PubMed] [Google Scholar]
- 10.Lock, R. L., and E. J. Harry. 2008. Cell-division inhibitors: new insights for future antibiotics. Nat. Rev. 7:324-338. [DOI] [PubMed] [Google Scholar]
- 11.Luria, S. E., and M. Delbruck. 1943. Mutations of bacteria from virus sensitivity to virus resistance. Genetics 28:491-511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Margalit, D. N., L. Romberg, R. B. Mets, A. M. Hebert, T. J. Mitchison, M. W. Kirschner, and D. RayChaudhuri. 2004. Targeting cell division: Small-molecule inhibitors of FtsZ GTPase perturb cytokinetic ring assembly and induce bacterial lethality. Proc. Natl. Acad. Sci. U. S. A. 101:11821-11826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Michie, K. A., and J. Lowe. 2006. Dynamic filaments of the bacterial cytoskeleton. Annu. Rev. Biochem. 75:467-492. [DOI] [PubMed] [Google Scholar]
- 14.Moshfegh, A. A., R. Badri, M. Hojjatie, M. Kaviani, B. Naderi, A. H. Nazmi, M. Ramezanian, B. Roozpeikar, and G. H. Hakimelahi. 1982. The synthesis of 4,11,18,25-tetrachloro[14]metacyclophane-7,14,21,28-tetrol. Structural analogues of phloroglucides. Helvetica Chim. Acta 65:1221-1228. [Google Scholar]
- 15.Moshfegh, A. A., B. Mazandarani, A. Nahid, and G. H. Hakimelahi. 1982. The synthesis of hetero-halogenated derivative of phloroglucide analogues. Helvetica Chim. Acta 65:1229-1232. [Google Scholar]
- 16.NCCLS. 1997. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. Approved standard, 5th ed. National Committee for Clinical Laboratory Standards, Wayne, PA.
- 17.Scalbert, A., and G. Williamson. 2000. Dietary intake and bioavailability of polyphenols. J. Nutr. 130:2073S-2085S. [DOI] [PubMed] [Google Scholar]
- 18.Shih, Y.-L., and L. Rothfield. 2006. The bacterial cytoskeleton. Microbiology 70:729-754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Turnbull, P. C. B., N. M. Sirianni, C. I. LeBron, M. N. Samaan, F. N. Sutton, A. E. Reyes, and L. F. Peruski, Jr. 2004. MICs of selected antibiotics for Bacillus anthracis, Bacillus cereus, Bacillus thuringiensis, and Bacillus mycoides from a range of clinical and environmental sources as determined by the Etest. J. Clin. Microbiol. 42:3626-3634. [DOI] [PMC free article] [PubMed] [Google Scholar]


