Abstract
Pigmented Paget’s disease is a rare variant which is often confused clinically and histologically with melanoma in situ. Herein, we describe a case of pigmented extramammary Paget’s disease involving the axilla of a 79 year old white male thought initially to represent malignant melanoma clinically and histologically. Review of the literature reveals that pigmented variant of Paget’s disease, either mammary or extramammary, could be initially misdiagnosed as melanoma unless this entity is considered in the differential diagnosis and additional confirmatory studies are performed.
Paget’s disease was initially reported in 1874 by Sir James Paget 1. He described eczema-like lesions involving the breast of 15 women who subsequently developed breast carcinoma. In 1889, Darier established the link between the intraepidermal Paget cell and the underlying breast adenocarcinoma 2. Paget’s disease of the nipple or mammary Paget’s disease (MPD) occurs in approximately 1–5% of all mammary carcinomas 3, 4 and rarely represents the initial presentation of an underlying breast adenocarcinoma 3–5. MPD occurs from an underlying intraductal breast carcinoma with intraepidermal extension without destruction of the epidermal basement membrane. Epidermotropic metastases of breast carcinoma, in contrast, are characterized by direct infiltration of the epidermis by an underlying breast adenocarcinoma via breaching the basement membrane of the epidermis with colonizing intraepithelial tumor nests. These cases also demonstrate an underlying desmoplastic dermis secondary to infiltrating tumor.
The first case of extramammary Paget’s disease (EMPD) involving the male genitalia was reported by Crocker et al in 1889 6. EMPD is an uncommon entity which may arise as a manifestation of an underlying adnexal apocrine carcinoma 7–9, prostatic carcinoma 10–12, rectal/anal carcinoma 13–15 or as a seemingly primary epidermal neoplasm without an associated carcinoma 16–19.
Pigmented MPD is an uncommon variant described clinically by Cuberson et al. 20. Since then, only 34 cases of this entity have been reported in the literature 21–33. The difficulty in distinguishing this entity both clinically and histopathologically from a melanocytic neoplasm has been first described by Ho et al 21. Pigmented MPD is characterized by Paget cells within the epidermis showing dusty melanin pigment and intervening dendritic melanocytes. Paget cells endocytose melanin pigment 21 making distinction from malignant melanoma in situ very difficult without the aid of immunohistochemistry. Pigmented epidermotropic metastases from a known underlying breast carcinoma may also occur rarely 21, 22, 34–44, however, these cases pose less diagnostic challenges due to previous clinical history. Similar to its mammary counterpart, pigmented EMPD is characterized by intraepidermal Paget cells containing melanin pigment, surrounded by dendritic melanocytes. Pigmented EMPD is an extremely rare neoplasm with only three well documented cases published so far 45, 46.
CASE REPORT
A 79 year old white male presented to the Mohs surgery department for excision of a 6x4 cm pigmented plaque in the right axilla. Clinically the lesion was thought to represent a melanoma. The patient had no clinical evidence of an underlying neoplasm in the axilla or either breasts on palpation and there was no lymphadenopathy. A right axillary excision was undertaken and the specimen measuring 5.3 x 2.6 cm was entirely submitted for histopathological examination. The excision was characterized by a broad intraepidermal proliferation of pagetoid tumor cells with abundant pale cytoplasm and large pleomorphic nuclei (Fig 1). The pale pagetoid cells displayed small amounts of fine melanin granules within the cytoplasm (Fig 2). Interdigitating between the pagetoid cells were numerous benign, dendritic melanocytes (Fig 2). In some areas the epidermis was atrophic and the superficial dermis was remarkable for an increased number of melanophages, fibrosis and a chronic lymphocytic inflammatory infiltrate resembling dermal regression of a melanoma (Fig 3, 4). Based on the histology alone, a diagnosis of melanoma in situ with prominent regression was initially considered. Further immunoperoxidase studies revealed the pagetoid cells to be positive for pancytokeratin, CK7 (Fig 6), CAM 5.2, EMA, and CEA. GCDFP15 and mucicarmine were weakly positive in the pagetoid cells. These cells were negative for CK903 (Fig 5), CK20, S100, MART1, HMB45 (Fig 7), and MITF. The populations of non-neoplastic intraepidermal dendritic melanocytes were highlighted by melanocytic markers (S100, MART1, HMB45 (Fig 7), and MITF). There was no invasive carcinoma identified on multiple levels within the dermis or subcutis and the underlying apocrine sweat glands were normal.
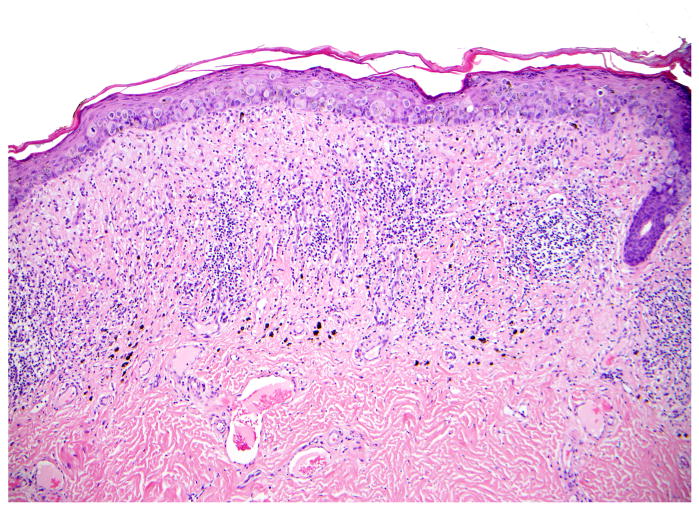
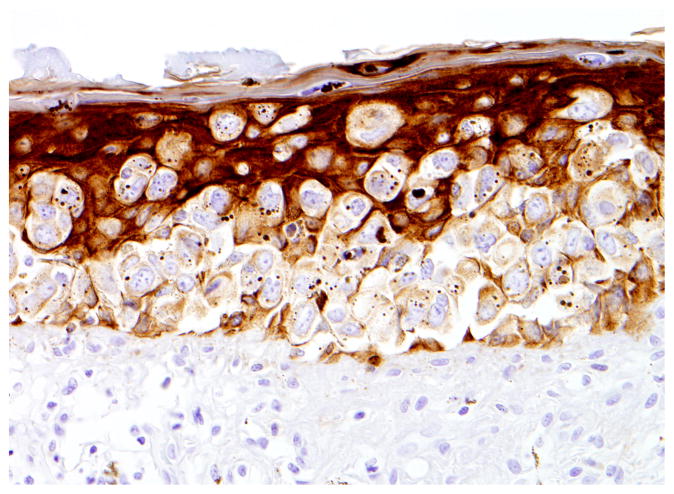
Fig 1.
Extramammary pigmented Paget’s disease (H&E 100X) showing dendritic melanocytes and malignant Paget cells with endocytosed melanin pigment. Note the lymphocytic infiltrate in the papillary dermis simulating regression of a melanoma.
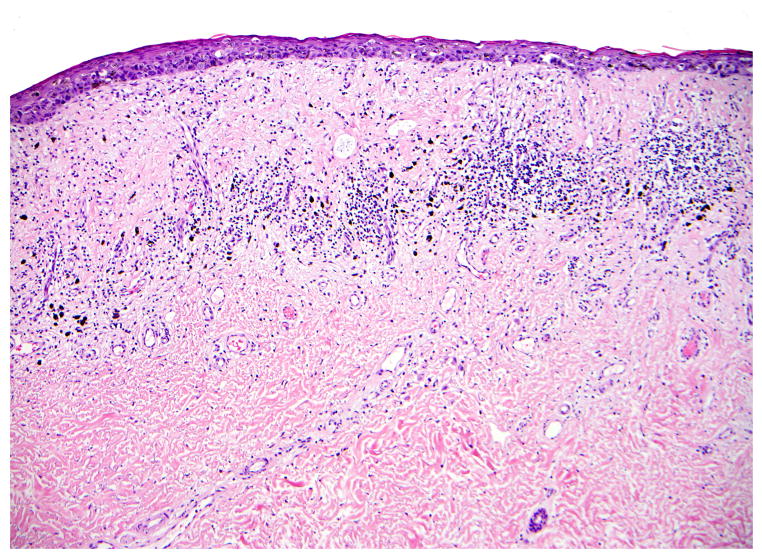
Fig 2.
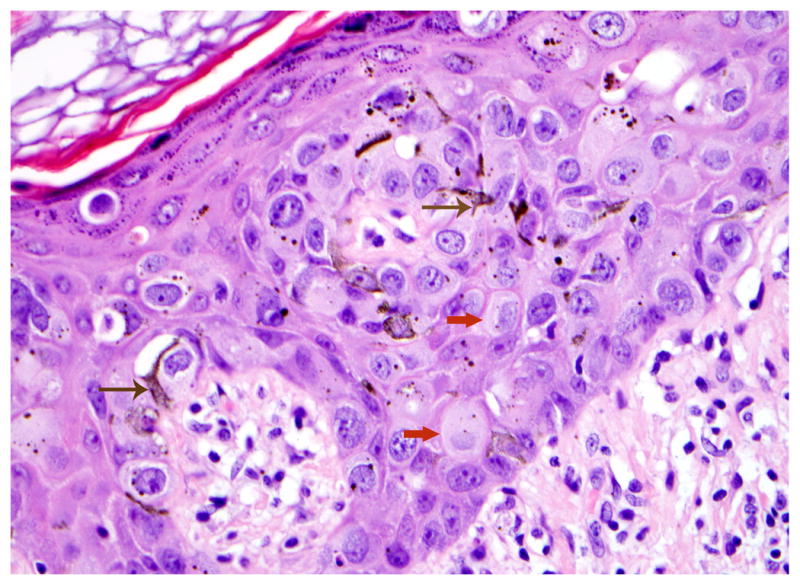
Extramammary pigmented Paget’s disease (H&E 400X) with brown arrows highlighting dendritic melanocytes and red arrows highlighting the malignant Paget adenocarcinoma cells with endocytosed melanin pigment.
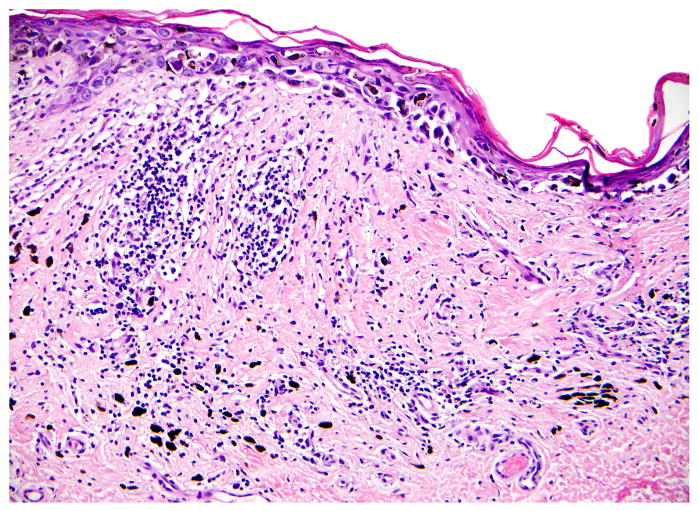
Fig 3.
Extramammary pigmented Paget’s disease (H&E 100X) showing epidermal atrophy, dermal fibrosis, inflammation and melanophages resembling regression of a melanoma.
Fig 4.
Extramammary pigmented Paget’s disease (H&E 200X) showing epidermal atrophy, intraepidermal apoptotic cells, dermal fibrosis, inflammation and melanophages resembling regression of a melanoma.
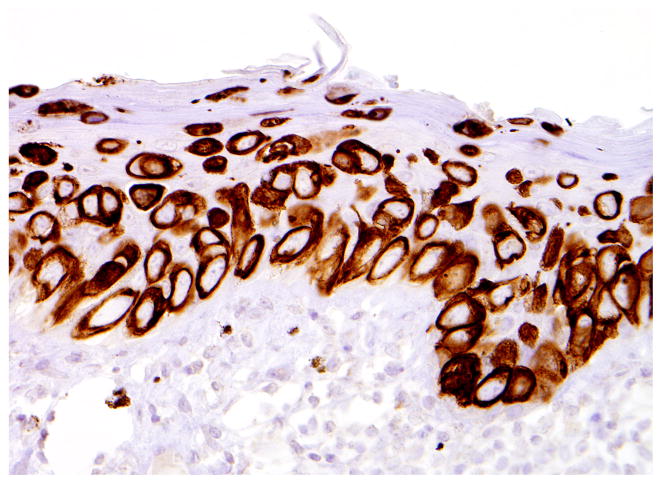
Fig 6.
Immunoperoxidase staining (cytokeratin CK7, a low molecular weight keratin; 400X) which highlights the malignant Paget adenocarcinoma cells.
Fig 5.
Immunoperoxidase staining (cytokeratin CK903 (34βE12), a high molecular weight keratin; 400X), which highlights normal keratinocytes and produces a negative image of the Paget’s disease.
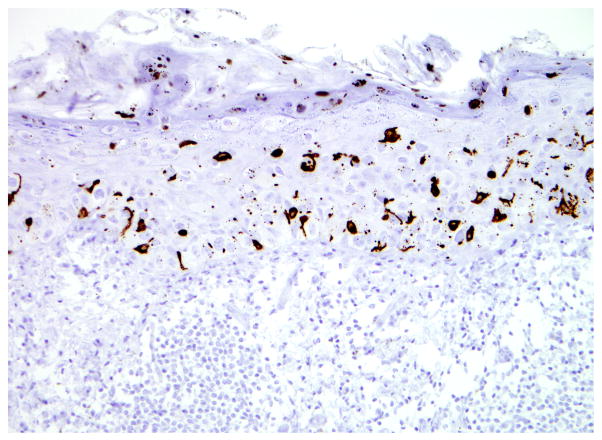
Fig 7.
Immunoperoxidase staining (HMB45, a melanocytic marker; 200X) which highlights the dendritic melanocytes. Note the melanin pigment within Paget adenocarcinoma cells forming a granular cytoplasmic blush.
Integrating the histological findings and immunohistochemical profile, the diagnosis of pigmented EMPD was rendered. Based on clinical and histopathological examination, which failed to detect invasive carcinoma, this case, most likely represents an example of primary EMPD. No further treatment was given post excision with negative margins. The patient was alive and free of disease 9 months after the primary excision.
DISCUSSION
Compared to the MPD, EMPD is relatively uncommon with most cases occurring in the genital or perianal region 47. Axillary location of EMPD is very rare. A review of the literature revealed only 23 cases reported so far, the majority in Japanese population 48–64 (Table 1). Out of these, 10 cases had isolated axillary involvement while 13 demonstrated simultaneous axillary and genital disease (so called triple EMPD). An additional number of 22 cases of triple EMPD were described exclusively in the Japanese literature for a total of 45 cases of reported axillary EMPD 54, 55. The cases of triple EMPD show a striking male predominance (94.3% of cases) in contrast to the cases with isolated axillary involvement which are more prevalent in females (70% of cases). Presence of an underlying carcinoma in axillary EMPD has been reported in 8 of the 23 cases (35%).
Table 1.
Extramammary Paget’s Disease of the axilla
| Study | Year | No of cases | Age | Sex | Site | Pigmented | Underlying carcinoma | Follow up (months) |
|---|---|---|---|---|---|---|---|---|
| Kawatsu et al.62 | 1971 | 1 | 77 | M | A+G | No | No | NED (12) |
| Ueki et al.64 | 1979 | 1 | 60 | M | A+G | No | No | NED (6) |
| Miki et al.63 | 1979 | 1 | 61 | M | A+G | No | Yes (groin) | NED (14) |
| Imai et al.50 | 1981 | 1 | 63 | F | A | No | Yes | NED (12) |
| Gibson et al.48 | 1983 | 1 | 78 | M | A+G | No | Yes (groin) | NED (6) |
| Hashimoto et al.49 | 1986 | 1 | 75 | M | A+G | No | No | NED (12) |
| Urabe et al.53 | 1990 | 4 | 77 85 61 79 |
F M M M |
A A+G A+G A+G |
No No No No |
No No Yes No |
N/A Local recurrence (72) NED (72) N/A |
| Coppens et al.51 | 1994 | 1 | 84 | F | A | No | No | NED (24) |
| Morgan et al.52 | 1996 | 1 | 71 | M | A | No | Yes | N/A* |
| Koseki et al.55 | 1997 | 1 | 74 | M | A+G | No | No | NED (12) |
| Kitajima et al.54 | 1997 | 2 | 86 82 |
M M |
A+G A+G |
No No |
Yes (groin) Yes (groin) |
N/A Lung met (7) |
| Ohno et al.56 | 1998 | 2 | 84 72 |
F F |
A A |
No** No** |
No No |
NED (36) NED (36) |
| Katagiri et al.58 | 1999 | 1 | 64 | M | A | No | Yes | NED (24) |
| Inui et al.57 | 2000 | 1 | 82 | M | A+G | No | No | N/A |
| Van Hamme et al.59 | 2002 | 1 | 79 | M | A+G | No | No | NED (6) |
| Castelli et al.60 | 2002 | 1 | 63 | F | A | No | Yes | Local recurrence (8) |
| Chagpar et al.61 | 2007 | 1 | 63 | F | A | No | No | NED (22) |
| Present study | 2008 | 1 | 79 | M | A | Yes | No | NED (9) |
Abbreviations: A – axilla, G – groin, NED – no evidence of disease, N/A – not available.
The patient died shortly after EMPD diagnosis of an exacerbation of his respiratory condition.
Brownish pigmentation is noted clinically however, no histologic description of pigmented Paget cells or melanocytes is given.
Pigmented variant of mammary or extramammary Paget’s disease is very uncommon 20–33, 45, 46, 65. Out of the 34 cases reported of pigmented MPD, 5 cases (15%) were males which is unusual considering the overwhelming predominance of MPD in females (95–99%) 66, 67. The pigmented variant of EMPD is an extremely rare entity with only 3 well documented cases previously reported in the literature (Table 2) 45, 46. The 3 cases of pigmented EMPD have all occurred in females with an average age of 62 years (range 52–70 years), and have involved the vulvar or perineal region (Table 2). We present here the first, to our knowledge, histologically confirmed case of a pigmented EMPD occurring in a male patient and in an axillary location. Only one previous report by Ohno et al. describes 2 cases of axillary EMPD which had a brownish appearance on clinical examination however, there is no histologic description of pigmented Paget cells or increased number of intraepidermal dendritic melanocytes 56. All cases (including the current one) demonstrated intraepidermal Paget cells with abundant cytoplasm containing conspicuous melanin pigment. In addition, a reactive population of dendritic melanocytes was also noted in the epidermis, enveloping the tumor cells. One explanation for the pigmentation of Paget cells could be the transfer of melanin pigment from the surrounding melanocytes. Interestingly, increased uptake of melanin pigment was not observed in to the surrounding epidermal keratinocytes. In pigmented epidermotropic breast carcinoma it has been shown that basic fibroblastic growth factor (bFGF) and other chemotactic factors may aid in the transfer of pigment to the carcinoma cells from the surrounding dendritic melanocytes 38, 42. It is possible that these factors could play a role in pigmented Paget’s disease as well.
Table 2.
Pigmented Extramammary Paget’s Disease in the Literature
| Study | Year | No of Cases | Age | Sex | Site | Underlying carcinoma | Follow up |
|---|---|---|---|---|---|---|---|
| Chiba et al.45 | 2000 | 2 | 52 70 |
F F |
Vulva Vulva |
No No |
N/A N/A |
| Gumurdula et al.46 | 2004 | 1 | 63 | F | Perineum | No | N/A |
Abbreviations: N/A – not available.
The clinical relevance of this variant of EMPD (or MPD) resides in its potential to be misdiagnosed as malignant melanoma. The clinical differential diagnosis often includes an atypical melanocytic neoplasm or a pigmented Bowen’s disease. In this context, the presence of intraepidermal pagetoid cells containing cytoplasmic melanin pigment, in the absence of an underlying carcinoma may prompt the histological diagnosis of melanoma unless pigmented variant of Paget’s disease is considered in the differential diagnosis and additional confirmatory studies are performed. Adding to the confusion is the presence of increased number of bonafide intraepidermal melanocytes associated with the Paget cells and of dermal melanophages, inflammation and fibrosis mimicking regression of a dermal melanocytic component. With the advent of immunohistochemical studies, pigmented variant of Paget’s disease is easily diagnosed. Similar to non-pigmented counterparts, Paget cells in the pigmented variant stain positively for CK7, CAM 5.2, EMA, CEA, Her2neu, BCA-225 (BRST1), mammoglobin, and variably with GCDFP15 (BRST2) and mucicarmine. They are almost uniformly negative for melanocytic markers: S100, HMB45, MART1, and MITF.
Presence of reactive melanocytes within an epithelial neoplasm has been described in other cutaneous tumors. Melanoacanthomas represent rare benign tumors of the skin characterized by an epithelial component with the resemblance of seborrheic keratosis populated by numerous dendritic melanocytes 68, 69. Similarly, basal cell carcinomas are commonly colonized by benign reactive melanocytes 70 and rarely a bonafide melanoma is found within a basal cell carcinoma 71, 72. Melanocytic matricoma is another example of a benign adnexal neoplasm with pilar differentiation and prominent dendritic melanocytes 73.
In summary, we described the first case of pigmented extramammary Paget’s disease in a male patient and axillary location and the fourth patient in the literature with this uncommon neoplasm. We also intended to raise awareness to the potential pitfall of misdiagnosing pigmented Paget’s disease both clinically and histologically as melanoma unless this variant of Paget’s disease is considered in the differential diagnosis.
References
- 1.Paget J. On disease of the mammary areola preceding cancer of the mammary gland. St Bartholomew Hosp Rep. 1874;10:87–89. [Google Scholar]
- 2.Darier MJ. Sur un nouvelle forme de psorrospermose cutanee: la maladie de Paget du reammelon. C R Soc Biol. 1889;41:294–98. [Google Scholar]
- 3.Caliskan M, Gatti G, Sosnovskikh I, Rotmensz N, Botteri E, Musmeci S, Rosali Dos Santos G, Viale G, Luini A. Paget's disease of the breast: the experience of the European institute of oncology and review of the literature. Breast Cancer Res Treat. 2008 doi: 10.1007/s10549-007-9880-5. [DOI] [PubMed] [Google Scholar]
- 4.Dalberg K, Hellborg H, Warnberg F. Paget's disease of the nipple in a population based cohort. Breast Cancer Res Treat. 2007 doi: 10.1007/s10549-007-9783-5. [DOI] [PubMed] [Google Scholar]
- 5.Ashikari R, Park K, Huvos AG, Urban JA. Paget's disease of the breast. Cancer. 1970;26:680–5. doi: 10.1002/1097-0142(197009)26:3<680::aid-cncr2820260329>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 6.Crocker HR. Paget's disease affecting the scrotum and penis. Trans Pathol Soc London. 1889;40:187–91. [Google Scholar]
- 7.Merot Y, Mazoujian G, Pinkus G, Momtaz TK, Murphy GF. Extramammary Paget's disease of the perianal and perineal regions. Evidence of apocrine derivation. Arch Dermatol. 1985;121:750–2. [PubMed] [Google Scholar]
- 8.Hernandez JM, Copeland EM., 3rd Infiltrating apocrine adenocarcinoma with extramammary pagetoid spread. Am Surg. 2007;73:307–9. [PubMed] [Google Scholar]
- 9.Regauer S. Extramammary Paget's disease--a proliferation of adnexal origin? Histopathology. 2006;48:723–9. doi: 10.1111/j.1365-2559.2006.02405.x. [DOI] [PubMed] [Google Scholar]
- 10.Allan SJ, McLaren K, Aldridge RD. Paget's disease of the scrotum: a case exhibiting positive prostate-specific antigen staining and associated prostatic adenocarcinoma. Br J Dermatol. 1998;138:689–91. doi: 10.1046/j.1365-2133.1998.02187.x. [DOI] [PubMed] [Google Scholar]
- 11.Hammer A, Hager H, Steiniche T. Prostate-specific antigen-positive extramammary Paget's disease--association with prostate cancer. Apmis. 2008;116:81–8. doi: 10.1111/j.1600-0463.2008.00816.x. [DOI] [PubMed] [Google Scholar]
- 12.Sleater JP, Ford MJ, Beers BB. Extramammary Paget's disease associated with prostate adenocarcinoma. Hum Pathol. 1994;25:615–7. doi: 10.1016/0046-8177(94)90229-1. [DOI] [PubMed] [Google Scholar]
- 13.Gunn A, Fox H. Perianal Paget's disease. Br J Dermatol. 1971;85:476–80. doi: 10.1111/j.1365-2133.1971.tb14057.x. [DOI] [PubMed] [Google Scholar]
- 14.Kuan SF, Montag AG, Hart J, Krausz T, Recant W. Differential expression of mucin genes in mammary and extramammary Paget's disease. Am J Surg Pathol. 2001;25:1469–77. doi: 10.1097/00000478-200112000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Redondo P, Idoate M, Espana A, Quintanilla E. Pruritus ani in an elderly man. Extramammary Paget's disease. Arch Dermatol. 1995;131:952–3. 55–6. doi: 10.1001/archderm.131.8.952. [DOI] [PubMed] [Google Scholar]
- 16.Battles OE, Page DL, Johnson JE. Cytokeratins, CEA, and mucin histochemistry in the diagnosis and characterization of extramammary Paget's disease. Am J Clin Pathol. 1997;108:6–12. [PubMed] [Google Scholar]
- 17.Park S, Grossfeld GD, McAninch JW, Santucci R. Extramammary Paget's disease of the penis and scrotum: excision, reconstruction and evaluation of occult malignancy. J Urol. 2001;166:2112–6. doi: 10.1016/s0022-5347(05)65516-4. discussion 17. [DOI] [PubMed] [Google Scholar]
- 18.Goldblum JR, Hart WR. Vulvar Paget's disease: a clinicopathologic and immunohistochemical study of 19 cases. Am J Surg Pathol. 1997;21:1178–87. doi: 10.1097/00000478-199710000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Goldblum JR, Hart WR. Perianal Paget's disease: a histologic and immunohistochemical study of 11 cases with and without associated rectal adenocarcinoma. Am J Surg Pathol. 1998;22:170–9. doi: 10.1097/00000478-199802000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Cuberson JD, Horn RC. Paget's disease of the nipple: review of 25 cases with special references to melanin pigmentation of “Paget cells”. Arch Surg. 1956;72:224–31. [PubMed] [Google Scholar]
- 21.Ho TC, St Jacques M, Schopflocher P. Pigmented Paget's disease of the male breast. J Am Acad Dermatol. 1990;23:338–41. doi: 10.1016/0190-9622(90)70217-6. [DOI] [PubMed] [Google Scholar]
- 22.Requena L, Sangueza M, Sangueza OP, Kutzner H. Pigmented mammary Paget disease and pigmented epidermotropic metastases from breast carcinoma. Am J Dermatopathol. 2002;24:189–98. doi: 10.1097/00000372-200206000-00001. [DOI] [PubMed] [Google Scholar]
- 23.del Boz J, Sanz A, Martin T, Martinez S, Sanchez V, Samaniego E, Ojeda A, Vera A, Crespo V. Pigmented mammary Paget's disease. J Eur Acad Dermatol Venereol. 2007;21:844–6. doi: 10.1111/j.1468-3083.2006.02046.x. [DOI] [PubMed] [Google Scholar]
- 24.Fujisawa Y, Yamamoto A, Machida H, Yamazaki N. Cytokeratin 7 staining was useful in a case of pigmented mammary Paget's disease resembling malignant melanoma. Int J Dermatol. 2006;45:1257–8. doi: 10.1111/j.1365-4632.2006.03015.x. [DOI] [PubMed] [Google Scholar]
- 25.Kutzner H, Hugel H, Embacher G. Pigmented Paget's disease and pigmented breast cancer metastasis. Clinical and histologic simulation of malignant melanoma of the breast. Hautarzt. 1992;43:28–31. [PubMed] [Google Scholar]
- 26.Menet E, Vabres P, Brecheteau P, Bonneau-Herve F, Duport G, Levillain P, Larregue M, Babin P. Pigmented Paget's disease of the male nipple. Ann Dermatol Venereol. 2001;128:649–52. [PubMed] [Google Scholar]
- 27.Mitchell S, Lachica R, Randall MB, Beech DJ. Paget's disease of the breast areola mimicking cutaneous melanoma. Breast J. 2006;12:233–6. doi: 10.1111/j.1075-122X.2006.00247.x. [DOI] [PubMed] [Google Scholar]
- 28.Nakamura S, Ishida-Yamamoto A, Takahashi H, Hashimoto Y, Yokoo H, Iizuka H. Pigmented Paget's disease of the male breast: report of a case. Dermatology. 2001;202:134–7. doi: 10.1159/000051614. [DOI] [PubMed] [Google Scholar]
- 29.Neubecker RD, Bradshaw RP. Mucin, melanin, and glycogen in Paget's disease of the breast. Am J Clin Pathol. 1961;36:49–53. doi: 10.1093/ajcp/36.1.49. [DOI] [PubMed] [Google Scholar]
- 30.Peison B, Benisch B. Paget's disease of the nipple simulating malignant melanoma in a black woman. Am J Dermatopathol. 1985;7 (Suppl):165–9. doi: 10.1097/00000372-198501001-00031. [DOI] [PubMed] [Google Scholar]
- 31.Pimentel CL, Barnadas MA, Dalmau J, Puig L, Sancho F, Alonso C, Alomar A. Pigmented Paget's disease in a man previously treated with mammaplasty reduction for gynecomastia. J Am Acad Dermatol. 2006;55:S62–3. doi: 10.1016/j.jaad.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 32.Pizzichetta MA, Canzonieri V, Massarut S, Gloghini A, Trevisan G, Veronesi A, Soyer HP. Pigmented mammary Paget's disease mimicking melanoma. Melanoma Res. 2004;14:S13–5. doi: 10.1097/00008390-200404000-00017. [DOI] [PubMed] [Google Scholar]
- 33.Stretch JR, Denton KJ, Millard PR, Horak E. Paget's disease of the male breast clinically and histopathologically mimicking melanoma. Histopathology. 1991;19:470–2. doi: 10.1111/j.1365-2559.1991.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 34.Azzopardi JG, Eusebi V. Melanocyte colonization and pigmentation of breast carcinoma. Histopathology. 1977;1:21–30. doi: 10.1111/j.1365-2559.1977.tb01641.x. [DOI] [PubMed] [Google Scholar]
- 35.Bourlond A. Pigmented epidermotropic metastasis of a breast carcinoma. Dermatology. 1994;189 (Suppl 2):46–9. doi: 10.1159/000246990. [DOI] [PubMed] [Google Scholar]
- 36.Fernandez-Figueras MT, Puig L, Casanova JM, Musulen E, Matias-Guiu X, Navas-Palacios JJ. Pigmented epidermotropic ductal carcinoma of the breast in a male. Ultrastructural evidence of melanocytic colonization and melanin transfer to the tumor. J Cutan Pathol. 1995;22:276–80. doi: 10.1111/j.1600-0560.1995.tb00750.x. [DOI] [PubMed] [Google Scholar]
- 37.Jacobi R, Roses DF, Valense Q. Carcinoma of the breast metastatic to the skin simulating malignant melanoma. In: Ackerman AB, editor. Pathology of malignant melanoma. New York: Masson Publishing; 1981. pp. 263–67. [Google Scholar]
- 38.Konomi K, Imayama S, Nagae S, Terasaka R, Chijiiwa K, Yashima Y. Melanocyte chemotactic factor produced by skin metastases of a breast carcinoma. J Surg Oncol. 1992;50:62–6. doi: 10.1002/jso.2930500117. [DOI] [PubMed] [Google Scholar]
- 39.Poiares-Baptista A, De Vasconcelos AA. Cutaneous pigmented metastasis from breast carcinoma simulating malignant melanoma. Int J Dermatol. 1988;27:124–5. doi: 10.1111/j.1365-4362.1988.tb01291.x. [DOI] [PubMed] [Google Scholar]
- 40.Requena L, Sanchez Yus E, Nunez C, White CR, Jr, Sangueza OP. Epidermotropically metastatic breast carcinomas. Rare histopathologic variants mimicking melanoma and Paget's disease. Am J Dermatopathol. 1996;18:385–95. doi: 10.1097/00000372-199608000-00010. [DOI] [PubMed] [Google Scholar]
- 41.Romanelli R, Toncini C. Pigmented papillary carcinoma of the male breast. Tumori. 1986;72:105–8. doi: 10.1177/030089168607200116. [DOI] [PubMed] [Google Scholar]
- 42.Saitoh K, Saga K, Okazaki M, Maeda K. Pigmented primary carcinoma of the breast: a clinical mimic of malignant melanoma. Br J Dermatol. 1998;139:287–90. doi: 10.1046/j.1365-2133.1998.02368.x. [DOI] [PubMed] [Google Scholar]
- 43.Sau P, Solis J, Lupton GP, James WD. Pigmented breast carcinoma. A clinical and histopathologic simulator of malignant melanoma. Arch Dermatol. 1989;125:536–9. doi: 10.1001/archderm.125.4.536. [DOI] [PubMed] [Google Scholar]
- 44.Shamai-Lubovitz O, Rothem A, Ben-David E, Sandbank M, Hauben D. Cutaneous metastatic carcinoma of the breast mimicking malignant melanoma, clinically and histologically. J Am Acad Dermatol. 1994;31:1058–60. doi: 10.1016/s0190-9622(09)80086-8. [DOI] [PubMed] [Google Scholar]
- 45.Chiba H, Kazama T, Takenouchi T, Nomoto S, Yamada S, Tago O, Ito M. Two cases of vulval pigmented extramammary Paget's disease: histochemical and immunohistochemical studies. Br J Dermatol. 2000;142:1190–4. doi: 10.1046/j.1365-2133.2000.03547.x. [DOI] [PubMed] [Google Scholar]
- 46.Gumurdula D, Sung CJ, Lawrence WD. Pathologic quiz case: a 63-year-old woman with a pigmented perineal lesion. Extramammary Paget disease. Arch Pathol Lab Med. 2004;128:e23–4. doi: 10.5858/2004-128-e23-PQC. [DOI] [PubMed] [Google Scholar]
- 47.Kanitakis J. Mammary and extramammary Paget's disease. J Eur Acad Dermatol Venereol. 2007;21:581–90. doi: 10.1111/j.1468-3083.2007.02154.x. [DOI] [PubMed] [Google Scholar]
- 48.Gibson JR, Pequm JS, Baker H, Pollock DJ. Multifocal extramammary Paget's disease. J R Soc Med. 1983;76:426–7. doi: 10.1177/014107688307600520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hashimoto T, Inamoto N, Nakamura K. Triple extramammary Paget's disease. Immunohistochemical studies. Dermatologica. 1986;173:174–9. [PubMed] [Google Scholar]
- 50.Imai S, Nitto H, Imai R. Axillary Paget's disease. J Dermatol. 1981;8:245–52. doi: 10.1111/j.1346-8138.1981.tb02541.x. [DOI] [PubMed] [Google Scholar]
- 51.Coppens M, Colpaert C, Van Dam P, Van Marck E, Buytaert P. Extramammary Paget's disease of the axilla. Eur J Obstet Gynecol Reprod Biol. 1994;54:140–2. doi: 10.1016/0028-2243(94)90254-2. [DOI] [PubMed] [Google Scholar]
- 52.Morgan JM, Carmichael AJ, Ritchie C. Extramammary Paget's disease of the axilla with an underlying apocrine carcinoma. Acta Derm Venereol. 1996;76:173–4. doi: 10.2340/0001555576173174. [DOI] [PubMed] [Google Scholar]
- 53.Urabe A, Matsukuma A, Shimizu N, Nishimura M, Wada H, Hori Y. Extramammary Paget's disease: comparative histopathologic studies of intraductal carcinoma of the breast and apocrine adenocarcinoma. J Cutan Pathol. 1990;17:257–65. doi: 10.1111/j.1600-0560.1990.tb00099.x. [DOI] [PubMed] [Google Scholar]
- 54.Kitajima S, Yamamoto K, Tsuji T, Schwartz RA. Triple extramammary Paget's disease. Dermatol Surg. 1997;23:1035–8. [PubMed] [Google Scholar]
- 55.Koseki S, Mitsuhashi Y, Yoshikawa K, Kondo S. A case of triple extramammary Paget's disease. J Dermatol. 1997;24:535–8. doi: 10.1111/j.1346-8138.1997.tb02835.x. [DOI] [PubMed] [Google Scholar]
- 56.Ohno H, Hatoko M, Kuwahara M, Ohnuma Y, Iida T, Muramatsu T, Shirai T. Two cases of unilateral axillary Paget's disease. J Dermatol. 1998;25:260–3. doi: 10.1111/j.1346-8138.1998.tb02393.x. [DOI] [PubMed] [Google Scholar]
- 57.Inui S, Fukuhara S, Asada H, Tadokoro T, Yoshikawa K, Itami S. Double involvement of extramammary Paget's disease in the genitalia and axilla. J Dermatol. 2000;27:409–12. doi: 10.1111/j.1346-8138.2000.tb02194.x. [DOI] [PubMed] [Google Scholar]
- 58.Katagiri Y, Ansai S. Two cases of cutaneous apocrine ductal carcinoma of the axilla. Case report and review of the literature. Dermatology. 1999;199:332–7. doi: 10.1159/000018285. [DOI] [PubMed] [Google Scholar]
- 59.Van Hamme C, Marot L, Dachelet C, Dumont M, Salamon E, Lachapelle JM. Paget's extramammary disease of the axillae and perineum. Ann Dermatol Venereol. 2002;129:717–9. [PubMed] [Google Scholar]
- 60.Castelli E, Wollina U, Anzarone A, Morello V, Tomasino RM. Extramammary Paget Disease of the Axilla Associated With Comedo-like Apocrine Carcinoma In Situ. Am J Dermatopathol. 2002;24:351–7. doi: 10.1097/00000372-200208000-00013. [DOI] [PubMed] [Google Scholar]
- 61.Chagpar AB, Heim K, Carron KR, Sewell C. Extramammary Paget's disease of the axilla: an unusual case. Breast J. 2007;13:291–3. doi: 10.1111/j.1524-4741.2007.00424.x. [DOI] [PubMed] [Google Scholar]
- 62.Kawatsu T, Miki Y. Triple extramammary Paget's disease. Arch Dermatol. 1971;104:316–9. [PubMed] [Google Scholar]
- 63.Miki Y, Kawatsu T, Kawatsu T, Yamada T, Okada T. Axillary involvements in genital Paget's disease. J Dermatol. 1979;6:25–9. doi: 10.1111/j.1346-8138.1979.tb01876.x. [DOI] [PubMed] [Google Scholar]
- 64.Ueki H, Kohda M. Multilocular extramammary Paget's disease. Hautarzt. 1979;30:267–70. [PubMed] [Google Scholar]
- 65.Longo C, Fantini F, Cesinaro AM, Bassoli S, Seidenari S, Pellacani G. Pigmented mammary Paget disease: dermoscopic, in vivo reflectance-mode confocal microscopic, and immunohistochemical study of a case. Arch Dermatol. 2007;143:752–4. doi: 10.1001/archderm.143.6.752. [DOI] [PubMed] [Google Scholar]
- 66.Satiani B, Powell RW, Mathews WH. Paget disease of the male breast. Arch Surg. 1977;112:587–92. doi: 10.1001/archsurg.1977.01370050047007. [DOI] [PubMed] [Google Scholar]
- 67.Bodnar M, Miller OF, 3rd, Tyler W. Paget's disease of the male breast associated with intraductal carcinoma. J Am Acad Dermatol. 1999;40:829–31. [PubMed] [Google Scholar]
- 68.Prince C, Mehregan AH, Hashimoto K, Plotnick H. Large melanoacanthomas: a report of five cases. J Cutan Pathol. 1984;11:309–17. doi: 10.1111/j.1600-0560.1984.tb00383.x. [DOI] [PubMed] [Google Scholar]
- 69.Schlappner OL, Rowden G, Philips TM, Rahim Z. Melanoacanthoma. Ultrastructural and immunological studies. J Cutan Pathol. 1978;5:127–41. doi: 10.1111/j.1600-0560.1978.tb00949.x. [DOI] [PubMed] [Google Scholar]
- 70.Florell SR, Zone JJ, Gerwels JW. Basal cell carcinomas are populated by melanocytes and Langerhans [correction of Langerhan's] cells. Am J Dermatopathol. 2001;23:24–8. doi: 10.1097/00000372-200102000-00004. [DOI] [PubMed] [Google Scholar]
- 71.Burkhalter A, White WL. Malignant melanoma in situ colonizing basal cell carcinoma. A simulator of invasive melanoma. Am J Dermatopathol. 1997;19:303–7. doi: 10.1097/00000372-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 72.Wang H, Benda PM, Piepkorn MW. Parasitism of basal cell carcinoma by lentigo maligna melanoma. J Am Acad Dermatol. 2003;48:S92–4. doi: 10.1067/mjd.2003.237. [DOI] [PubMed] [Google Scholar]
- 73.Williams CM, Bozner P, Oliveri CV, Horenstein MG. Melanocytic matricoma: case confirmation of a recently described entity. J Cutan Pathol. 2003;30:275–8. doi: 10.1046/j.0303-6987.2003.042.x. [DOI] [PubMed] [Google Scholar]