Abstract
Background
Among patients with heart failure, women have worse functional status than do men, but little research has focused on determining factors that influence functional status in either sex.
Objectives
To compare factors that influence functional status in men and women with heart failure and to test whether depressive symptoms mediate the relationship between physical symptoms and functional status.
Methods
A cross-sectional, descriptive study design was used. A total of 231 patients, 133 men and 98 women, were recruited from an inpatient heart failure clinic in South Korea. Functional status (the Korean Activity Scale/Index), physical symptoms (the Symptom Status Questionnaire), depressive symptoms (the Beck Depression Inventory), and situational factors (living status, socioeconomic status) were measured. Hierarchical multiple regression and mediation analysis were used for data analysis.
Results
Women (mean score, 24.5; SD, 17.3) had worse functional status than did men (mean score, 31.9; SD, 20.1; P=.004). Dyspnea on exertion (β = −0.16), ankle swelling (β = −0.19), fatigue (β = −0.20), and depressive symptoms (β = −0.19) were independently associated with functional status in women, whereas only dyspnea on exertion (β = −0.30) influenced functional status of men in hierarchical multiple regression analysis. Mediation analysis indicated that depressive symptoms mediated the relationship between physical symptoms and functional status in women with heart failure, but not in men.
Conclusions
Distinct physical and psychological symptoms influence functional status in women with heart failure. A systematic multidimensional intervention may be required to target depressive symptoms to improve functional status in women with heart failure.
Heart failure is a chronic condition that affects about 5 million patients in the United States.1 In South Korea, heart failure is the most common health problem contributing to hospitalization and readmission of elderly persons.2–4 Among all patients with heart failure, approximately one-half are women,1,5 but women’s specific needs have been underestimated or overlooked in the management of heart failure, and women have been underrepresented in major clinical trials.6–8
Women and men with heart failure differ in demographics, disease-specific characteristics, and outcomes.9–12 Women have a higher prevalence of heart failure at an advanced age than do men, and higher rehospitalization rates, with an increasing annual rehospitalization rate.10,13 In addition, most women with heart failure have worse quality of life (QOL) than do men,14–17 and the lower QOL is influenced by poor functional status.14,18,19
Heart failure is associated with poor QOL, limited social functioning, and lost work capacity.15 These conditions have a strong adverse effect on functional status, and poor functional status has implications for exercise capacity, illness severity, and QOL in patients with heart failure.20–23 Functional status, which is considered an important aspect of illness progression,24 includes 4 dimensions25,26: functional capacity (a person’s maximum potential ability), functional performance (physical daily activities for basic needs), functional reserve, and use of functional capacity. However, researchers14,27 have found that functional capacity and performance were more important to patients with heart failure.
In addition, in most studies28,29 of sex-based differences in patients with heart failure, women had poorer functional status—namely, decreased functional capacity or functional performance—than did men. Most investigators have focused on sex-based differences in functional status, with little attention given to sex-based differences in factors associated with functional status. Because of the importance of functional status in patients with heart failure, factors that influence functional status in men and women with heart failure should be determined and compared.
The purposes of this study were to compare functional status between women and men with heart failure, determine whether sex-based differences exist for factors that influence functional status, and examine whether depressive symptoms mediate the link between physical symptoms and functional status in women and men.
Theoretical Framework
The conceptual framework for this study was the theory of unpleasant symptoms proposed by Lenz et al.30 This middle-range theory was developed to explain the symptom experience from a multidimensional perspective. The theory includes consideration of factors that are influential in explaining the symptom experience and discussion of the consequences of the symptom experience. According to the theory, the symptom experience can be influenced by physiological (eg, existence of any pathological condition), psychological (eg, affective reaction or mood), and situational (eg, social support or physical environment) variables. The major consequence of the symptom experience is a change in performance, conceptualized to include functional status (eg, daily activities or role functioning). In this model, the physiological, psychological, and situational variables as well as the overall symptom experience are directly related to functional status.
Functional status reflects heart failure progression for patients.
Physical and psychological symptoms are common and important problems in patients with heart failure. Up to 91% of patients with heart failure have multiple physical symptoms; the most common are dyspnea and fatigue.31 In addition, ankle edema and elevated jugular venous pressure have been reported more often in women than in men.32,33 Women with heart failure reported different symptoms of heart failure than did men.32,34 Women more often reported sleep difficulties,35 dyspnea, and fatigue. These physical symptoms contribute to limitations of daily activities.
In addition, up to 48% of patients with heart failure experience marked depressive symptoms,31,36,37 and women report a higher prevalence of depressive symptoms than do men.16,36,38 Depressive symptoms differ from depression; depressive symptoms measured by self-report include guilt, hopelessness, low self-esteem, and low energy. Patients may experience important depressive symptoms without a diagnosis of major depression.39 Depressive symptoms influence patients’ perception of their health status, a situation that can lead to lower functional status. Additionally, situational factors such as living alone and low socioeconomic status are associated with worse functional status.40–42
Women with heart failure have higher rehospitalization rates than men.
Thus, on the basis of the theory of unpleasant symptoms, in this study we included symptoms of heart failure (dyspnea on exertion, paroxysmal nocturnal dyspnea, ankle swelling, fatigue, and sleep disturbance) included in the physical symptoms dimension. The psychological symptoms dimension included depressive symptoms, and the situational dimension included living status and socioeconomic status.
Method
A cross-sectional, descriptive study design was used. The study was approved by the appropriate institutional review board. For each patient, before written informed consent was obtained the primary investigator (E. K. S.) explained the purposes of the study and noted that the responses would be kept confidential. When their medical condition was stable, patients received questionnaires to complete, usually within 1 to 2 days before discharge. If requested, a trained research assistant helped patients complete the questionnaires. Each encounter lasted approximately 25 minutes.
Setting and Participants
Participants for the study were recruited from 3 cardiology units at Yonsei University Medical Center, Severance Hospital in Seoul, South Korea. The hospital is a tertiary referral medical center with a heart failure clinic. Patients were eligible if they were 20 years or older, had heart failure diagnosed by 2 cardiologists and confirmed by using the Framingham criteria,43,44 and had American Heart Association stage C (current or previous symptoms of heart failure associated with underlying structural myocardial change) or stage D (symptomatic at rest or with minimal activity despite optimal medical therapies) heart failure.45 Patients recruited for the study had impaired left ventricular systolic function (left ventricular ejection fraction ≤40% at admission) or preserved systolic function (left ventricular ejection fraction >40%). Patients were recruited during an exacerbation of chronic heart failure. Patients were excluded from the study if they had a history of neurological disease (eg, stroke, head injury, or encephalopathy), cancer, current acute psychiatric problems, or end-stage renal disease or were homeless. A total of 244 patients were eligible. Of these, 8 patients refused to participate and 5 withdrew because of worsening health status. The final sample therefore consisted of 231 patients.
Women with heart failure have worse quality of life than men.
Variables
Functional Status
Functional status was measured by using the Korean Activity Scale/Index, a self-administrated tool for evaluating functional capacity in patients with cardiac diseases.46 Patients were asked to rate their ability during the past 1 month to perform daily activities such as carrying heavy things, doing housework, going upstairs, and walking rapidly. Respondents score each of 15 items as 0 (cannot perform the activity) or 1 (can perform the activity). The total score is calculated by adding the scores for all items multiplied by a weight given to each item that reflects the difficulty of performing the activity. The total score ranges from 0 to 77. A higher score indicates better functional status. The Cronbach α for the total 15-item scale was 0.89. All patients were categorized into 1 of 4 groups of functional status on the basis of standard clinical categories for the scale. A score of 0 to 3.9 was categorized as class I (low functional status), 4.0 to 23.9 as class II, 24 to 45.9 as class III, and 46 to 77.0 as class IV (high functional status).46
Symptoms of Heart Failure
The following 5 symptoms of heart failure were assessed by using the modified Symptom Status Questionnaire: dyspnea on exertion, paroxysmal nocturnal dyspnea, ankle swelling, fatigue, and sleep disturbance. Symptom distress was measured by the question, “For the past 1 month, how bothered or distressed were you by each of the following heart failure symptoms?” Patients responded on a scale ranging from 1 (not at all distressed) to 4 (extremely distressed) for each symptom. Thus, the score for each symptom ranged from 1 to 4, with higher scores indicating higher distress. The content validity of the instrument was established by 2 cardiologists and 3 nurse experts in management of heart failure. The Cronbach α in this study for the 5 items was 0.76.
Depressive Symptoms
Depressive symptoms were measured by using the Beck Depression Inventory,47,48 a widely used self-report, 21-item instrument that consists of statements reflecting symptoms of and attitudes about depression. Response statements are rated on a 4-point scale ranging from 0 (not at all) to 3 (very much so) in terms of severity. The total score range is 0 to 63, and higher scores indicate more severe depressive symptoms. The initial Cronbach α for the total 21 items of the Korean version of the Beck Depression Inventory was 0.86.49 In this study, the α was 0.87. All patients were categorized into 4 groups of depressive symptoms on the basis of standard clinical categories for the inventory. A score of 0 to 9 was categorized as no depressive symptoms, 10 to 16 as mild symptoms, 17 to 29 as moderate symptoms, and 30 to 63 as severe symptoms.47
Living Status
Living alone or not (cohabitation with spouse, children, or other persons) was assessed by using a single-item question: “Do you live alone?”
Socioeconomic Status
Socioeconomic status was classified into 3 groups on the basis of the following considerations: educational level, occupational status (unskilled or semiskilled workers, skilled workers, foremen in industry, employed and self-employed professionals, higher civil servants, and executives), and household income. These characteristics were determined by chart review and by self-reporting at admission.
Clinical Characteristics
Age, sex, ischemic vs nonischemic heart disease as the cause of heart failure, and left ventricular ejection fraction were collected from patients’ medical records.
Statistical Analysis
The data were analyzed by using SPSS for Windows 12.0 (SPSS Inc, Chicago, Illinois). Descriptive statistics (frequencies and percentages, means and standard deviations) were used for reporting the clinical, physical, psychological and situational variables, and functional status. An independent t test or χ2 test was performed to examine sex-based differences for all study variables, depending on level of measurement.
Hierarchical multiple regression analysis was used to determine which factors influenced functional status in women and men. Variables were entered as follows: In the first step, clinical (ie, age, cause of heart failure, type of heart failure [preserved vs non-preserved systolic function]), and situational (ie, living alone, socioeconomic status) factors were entered. In the second step, physical symptoms (ie, dyspnea on exertion, paroxysmal nocturnal dyspnea, ankle swelling, fatigue, sleep disturbance) and the psychological factors (depressive symptoms) were entered.
Separate mediation analyses were used to examine whether depressive symptoms mediated the association between physical symptoms and functional status in men and in women.50 In the first step, the relationship between physical symptoms and depressive symptoms was tested after other clinical and situational factors were controlled for. In the second step, the relationship between physical symptoms and functional status was tested after adjusting for the same clinical and situational factors. In the third step, both depressive symptoms and physical symptoms were entered as independent variables, and their relationship to functional status was tested. Depressive symptoms were considered to mediate the impact of physical symptoms on functional status if the percentage of variance in functional status explained by physical symptoms in the third model was significantly less than that in the second model. Multi-collinearity was not a problem. The significance level for all statistical analyses was set a priori at P < .05.
Women had worse functional status than men with heart failure.
Results
Characteristics of the Patients
The mean age of the patients in the sample was 63 years (SD, 13; range, 20–92); 58% were men. Almost half of the sample had ischemic heart disease as the underlying cause of heart failure. The sample was distributed evenly among patients with preserved and nonpreserved systolic function. More than one-third of the patients had hypertension and diabetes. Common medications were β-blockers, angiotensin-converting enzyme inhibitors, and diuretics. Only 26% of the patients took antidepressants. A total of 56% of the patients had moderately limited to very poor functional status. Symptoms were common; fatigue and dyspnea on exertion were the most troubling ones, although all symptoms were associated with substantial distress. Only 18% of the patients had no depressive symptoms, and nearly half of the patients had moderate to severe depressive symptoms. Most patients lived with family members and had a low socioeconomic status.
Women had higher levels of depressive symptoms than men.
Sex-Based Differences
On bivariate analyses, women had worse functional status as assessed by the Korean Activities Scale/Index than did men and greater distress from dyspnea on exertion, fatigue, sleep disturbance, and depressive symptoms (Table 1). Among the clinical variables, women were older than men. The prevalence of heart failure with preserved systolic function was higher in women, and the prevalence of diabetes was higher in men. There were no sex-based differences for any other variables (Table 1).
Table 1.
Comparison of factors related to functional status in men and women with heart failure
| Valuea |
Significance |
||||
|---|---|---|---|---|---|
| Variable | Men (n = 133) | Women (n = 98) | t or χ2 | P | |
| Functional status, mean (SD), scoreb | 31.9 (20.1) | 24.5 (17.3) | 8.49 | .004 | |
| Clinical factors | |||||
| Age, mean (SD), y | 61 (12) | 65 | (13) | 5.32 | .02 |
| Ischemic heart disease | 66 (50) | 48 | (49) | 0.01 | .92 |
| Heart failure with preserved systolic function | 56 (42) | 61 | (62) | 9.16 | .002 |
| Comorbid diseases | |||||
| Hypertension | 52 (39) | 41 | (42) | 0.18 | .68 |
| Diabetes | 55 (41) | 28 | (29) | 4.00 | .04 |
| Medications | |||||
| Angiotensin-converting enzyme inhibitors | 109 (82) | 72 | (73) | 6.56 | .12 |
| Digoxin | 41 (31) | 21 | (21) | 3.15 | .08 |
| Diuretics | 100 (75) | 81 | (83) | 1.85 | .17 |
| β-Blockers | 119 (89) | 88 | (90) | 0.01 | .94 |
| Calcium blockers | 18 (14) | 14 | (14) | 0.03 | .87 |
| Aldosterone antagonist | 41 (31) | 24 | (24) | 1.12 | .29 |
| Antidepressants | 30 (23) | 30 | (31) | 1.90 | .17 |
| Situational factors | |||||
| Living status | 0.35 | .55 | |||
| Living alone | 7 (5) | 7 | (7) | ||
| Living with family | 126 (95) | 91 | (93) | ||
| Socioeconomic status | 3.07 | .22 | |||
| Low | 66 (50) | 60 | (61) | ||
| Middle | 31 (23) | 18 | (18) | ||
| High | 36 (27) | 20 | (20) | ||
| Physical symptoms, mean (SD) | |||||
| Dyspnea on exertion | 2.8 (0.9) | 3.1 | (0.9) | 4.49 | .03 |
| Paroxysmal nocturnal dyspnea | 2.1 (1.0) | 2.2 | (1.1) | 1.06 | .30 |
| Ankle swelling | 2.1 (1.0) | 2.2 | (1.0) | 0.16 | .69 |
| Fatigue | 2.8 (1.0) | 3.2 | (0.9) | 13.36 | <.001 |
| Sleep disturbance | 2.4 (1.1) | 2.8 | (1.1) | 8.04 | .005 |
| Psychological symptoms, mean (SD) | 17.0 (9.5) | 19.8 | (9.9) | 4.77 | .03 |
| Depressive symptoms, No. (%) of patientsc | |||||
| None | 27 (20) | 15 | (15) | ||
| Mild | 55 (41) | 31 | (32) | ||
| Moderate | 38 (29) | 36 | (37) | ||
| Severe | 13 (10) | 16 | (16) | ||
Values are expressed as number (%) of patients unless otherwise indicated. Because of rounding, percentages may not total 100.
Score on Korean Activity Scale/Index.
Score on Beck Depression Inventory: 0–9, no symptoms; 10–16, mild symptoms; 17–29, moderate symptoms; 30–63, severe symptoms.
Differences in Factors Influencing Functional Status in Men and Women
In hierarchical multiple regression analysis (Table 2), severe dyspnea on exertion, ankle swelling, fatigue, and depressive symptoms were independently associated with worse functional status in women. In contrast, severe dyspnea on exertion was independently associated with worse functional status in men. In both men and women, older age and low socioeconomic status were associated with worse functional status.
Table 2.
Differences between factors influencing functional status in men and women with heart failure
| Men (n = 133) | Women (n = 98) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Step 1 | Step 2 | Step 1 | Step 2 | |||||||||
| Variable | β | t | P | β | t | P | β | t | P | β | t | P |
| Clinical factors | ||||||||||||
| Age, y | −0.42 | −4.32 | <.001 | −0.29 | −3.11 | .003 | −0.31 | −3.78 | <.001 | −0.15 | −2.12 | .03 |
| Ischemic heart disease | 0.20 | 2.02 | .04 | 0.12 | 1.36 | .18 | 0.16 | 1.82 | .07 | 0.03 | 0.44 | .66 |
| Heart failure with preserved systolic function | −0.08 | −0.82 | .41 | −0.15 | −1.79 | .08 | 0.12 | 1.38 | .17 | 0.05 | 0.72 | .48 |
| Comorbid diseases | ||||||||||||
| Hypertension | −0.14 | −1.39 | .17 | −0.03 | −0.38 | .70 | −0.15 | −1.84 | .07 | −0.13 | −1.91 | .06 |
| Diabetes | −0.00 | −0.01 | .99 | −0.05 | −0.60 | .55 | −0.08 | −0.87 | .38 | −0.04 | −0.46 | .65 |
| Situational factors | ||||||||||||
| Living alone | −0.05 | −0.51 | .61 | −0.13 | −1.48 | .14 | 0.06 | 0.72 | .47 | 0.08 | 1.24 | .22 |
| Middle socioeconomic status | −0.13 | −1.16 | .25 | −0.13 | −1.25 | .23 | 0.02 | 0.19 | .85 | 0.01 | 0.11 | .91 |
| Low socioeconomic status | −0.17 | −1.43 | .16 | −0.21 | −1.99 | .04 | −0.29 | −2.98 | .004 | −0.23 | −2.81 | .006 |
| Physical symptoms | ||||||||||||
| Dyspnea on exertion | −0.30 | −2.71 | .008 | −0.16 | −2.02 | .04 | ||||||
| Paroxysmal nocturnal dyspnea | −0.20 | −1.95 | .06 | −0.02 | −0.28 | .78 | ||||||
| Ankle swelling | −0.09 | −0.90 | .37 | −0.19 | −2.49 | .01 | ||||||
| Fatigue | −0.01 | −0.06 | .95 | −0.20 | −2.53 | .01 | ||||||
| Sleep disturbance | −0.01 | −0.12 | .91 | −0.09 | −1.07 | .29 | ||||||
| Psychological symptoms | ||||||||||||
| Depressive symptoms | −0.03 | −0.28 | .78 | −0.19 | −2.57 | .01 | ||||||
| Overall |
R2 = 0.38, ΔR2 = 0.38 P < .01 |
R2 = 0.56, ΔR2= 0.18 P < .01 |
R2 = 0.30, ΔR2 = 0.30 P < .01 |
R2 = 0.56, ΔR2 = 0.26 P < .01 |
||||||||
Effect of Depressive Symptoms on the Link Between Physical Symptoms and Functional Status
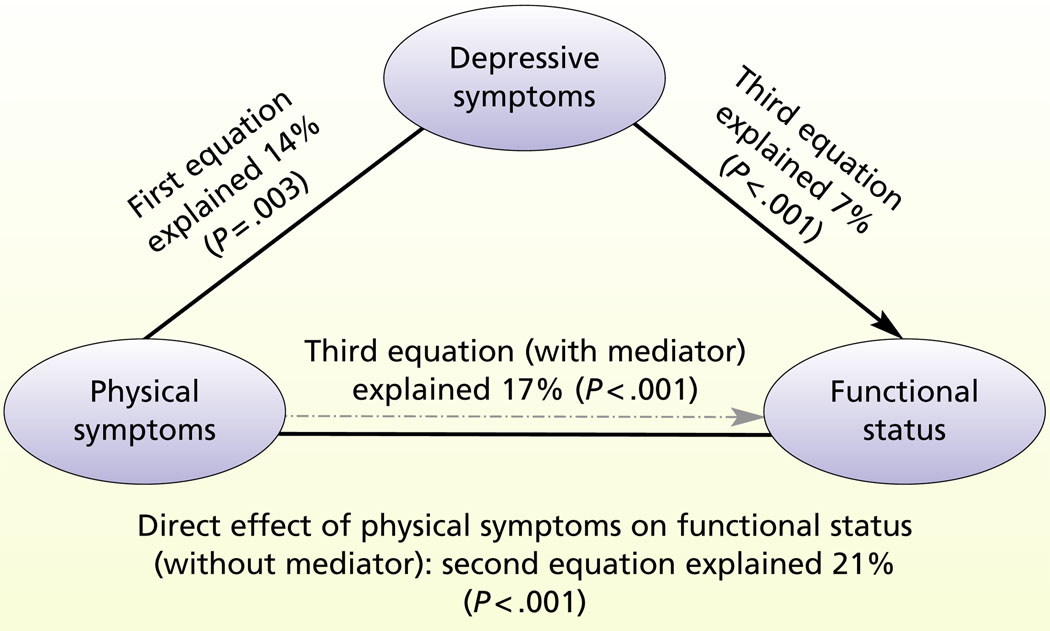
Women With Heart Failure
The first equation regressed depressive symptoms on physical symptoms (β = 0.22; P = .003) after controlling for other clinical and situational factors. Physical symptoms explained 11% of the variance in depressive symptoms. The second equation regressed functional status on physical symptoms in women with heart failure (β = −0.50; P < .001) after adjusting for the same clinical and situational factors. Physical symptoms explained 22% of the variance in functional status. When both depressive symptoms and physical symptoms were entered as independent variables in the third equation, the relationship between depressive symptoms and functional status was significant (β = −0.22; P < .001). Depressive symptoms explained 9% of the variance in functional status of women. The percentage of variance in functional status explained by physical symptoms was reduced from 22% in the second equation to 17% in the final equation (β = −0.45; P < .001). Thus, mediation analysis indicated depressive symptoms mediated the impact of physical symptoms on functional status in women with heart failure (Figure 1).
Figure 1.
Mediator effect of depressive symptoms on the link between physical symptoms and functional status in women.
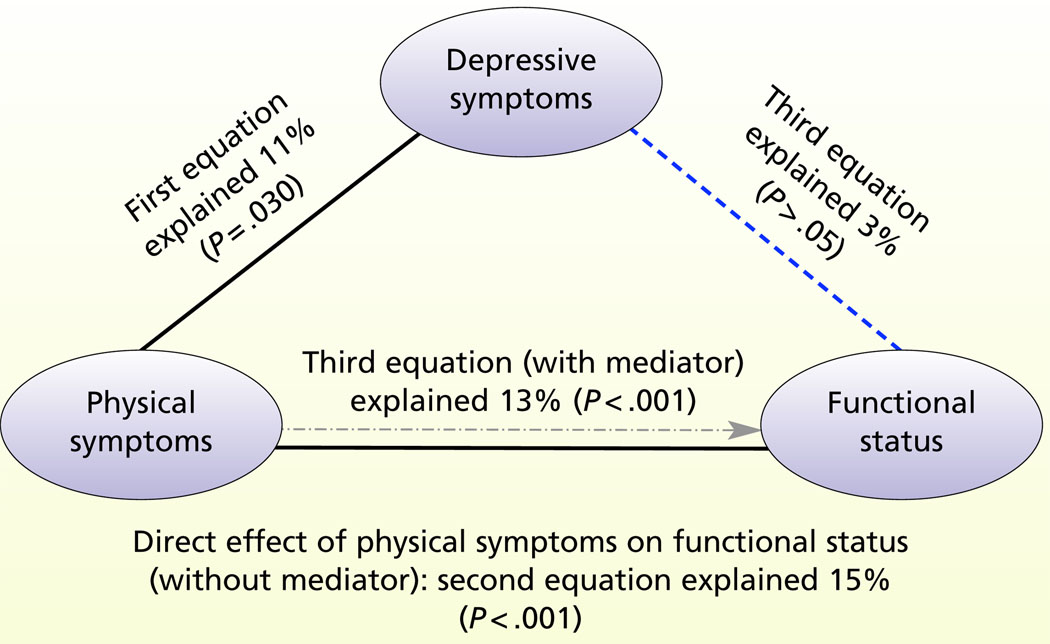
Men With Heart Failure
The first equation regressed depressive symptoms on physical symptoms (β = 0.33; P = .03) after other clinical and situational factors were controlled for. Physical symptoms explained 15% of the variance in depressive symptoms. The second equation regressed functional status on physical symptoms in men with heart failure (β = −0.42; P < .001) after the same clinical and situational factors were adjusted for. Physical symptoms explained 16% of the variance in functional status. When both depressive symptoms and physical symptoms were entered as independent variables in the third equation, the relationship between depressive symptoms and functional status was not significant (β = −0.01; P = .78). The percentage of variance in functional status explained by physical symptoms was reduced from 16% in the second equation to 13% in the final equation (β = −0.40; P < .001). Thus, mediation analysis indicated that depressive symptoms did not mediate the impact of physical symptoms on functional status in men with heart failure (Figure 2).
Figure 2.
Mediator effect of depressive symptoms on the link between physical symptoms and functional status in men.
Discussion
Functional status is a fundamental construct relevant to patients with heart failure and to the nurses who care for these patients because functional status reflects how much patients are able to perform physical activities without limitations due to physical symptoms.19,29 Functional status affects satisfaction with work, domestic, and social roles, and good functional status is associated with better QOL among all patients with heart failure. Functional status has particular meaning for women with heart failure,51 who have worse functional status and worse QOL than do men, and in whom functional status is a particularly strong predictor of QOL.
Severe depressive symptoms are associated with worse functional status in women, but not men.
In our study, and consistent with the findings of previous investigations28,29,52 of patients with heart failure, women had worse functional status than did men. We expanded previous research by identifying factors that influence functional status in both women and men. The major findings of our study are that severe depressive symptoms are independently associated with worse functional status in women, but not in men, and that only in women do depressive symptoms mediate the link between physical symptoms and functional status. We found a significant difference between men and women in the mean level of depressive symptoms: women had higher levels. In several previous studies16,36,38 of patients with heart failure, women had more depressive symptoms than men did, and women experienced crying, tearfulness, and sadness more often.53 Apparently the effect of psychological symptoms on functional status in women with heart failure is greater than the effect of physical symptoms.
Consistent with the theory of unpleasant symptoms, the influences on functional status were multidimensional and included psychological, physical, and situational factors. From a situational perspective, older age and low socioeconomic status were independently associated with worse functional status, regardless of sex. Because most of the patients in our sample were older than 65 years and most were retired, the effect of age and socioeconomic status might be overestimated. Because age still remained a significant predictor of functional status after other clinical and situational factors are con-rolled for, studies to compare predictors of functional status among older and younger patients with heart failure are needed. Additionally, results of previous studies54,55 suggest that patients with lower socioeconomic status, regardless of age, are increasingly vulnerable and have increased morbidity and mortality. Because the importance of socioeconomic status has been overlooked among women in South Korea, socioeconomic status should be assessed and considered in both men and women with heart failure.
In our sample, the number of physical symptoms that influenced functional status was greater in women than in men. Physical symptoms also influenced functional status, although differently, in both men and women. In women, dyspnea on exertion, ankle swelling, and fatigue were independently associated with functional status, whereas only dyspnea on exertion was associated with functional status in men. This difference may be the result of the influence of depressive symptoms. Compared with men, women reported more distress from depressive symptoms, and depressive symptoms influence the experience and recognition of physical symptoms such as fatigue and dyspnea on exertion. Recurrent symptoms of fatigue and dyspnea leave women with insufficient energy to perform daily activities and to fulfill family and domestic roles at home and in other social settings.14,27,51,56 Accordingly, the effect of a greater variety of physical symptoms on functional status in women may have occurred because depressive symptoms amplified the perception of physical symptoms.
Therefore, the impact of depressive symptoms on functional status in women with heart failure warrants further research. It is also important to determine whether depressive symptoms alter the effect of functional status on adverse outcomes in women with heart failure. Additionally, sex-specific, interventions or interventions tailored for each sex should be developed to improve functional status.
Limitations
Our findings must be considered within the limitations of the study. In this study, each symptom of heart failure was measured by using a single item. Single-item indicators may not fully reflect the multidimensional nature of a symptom. In further studies, researchers might use a multidimensional instrument to determine the effect of these variables on functional status. We measured functional status once during hospitalization, so potential changes in functional status after discharge from the hospital could not be considered. Additionally, functional status rating for the preceding month before hospitalization may not reflect patients’ functional status, when their medical condition is more stable. Repeated measurements of functional status with long-term follow-up are needed in future studies.
Conclusion
Women with heart failure have worse functional status than men do. Depressive symptoms were the most influential factor associated with functional status in women, and depressive symptoms mediated the relationship between physical symptoms and functional status. Furthermore, the number of physical symptoms that influenced functional status was greater in women than in men. This finding may have occurred because depressive symptoms amplified the perception of physical symptoms in women. Therefore, any multidimensional intervention to improve functional status should address depressive symptoms, particularly in women.
Footnotes
FINANCIAL DISCLOSURES
This project was supported by grant 1P20NR010679 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
SEE ALSO
For more about heart failure and depression, visit the Critical Care NurseWeb site, www.ccnonline.org, and read the article by Thomas and colleagues, “Depression in Patients With Heart Failure: Prevalence, Pathophysiological Mechanisms, and Treatment” (April 2008).
To purchase electronic or print reprints, contact The InnoVision Group, 101 Columbia, Aliso Viejo, CA 92656. Phone, (800) 899-1712 or (949) 362-2050 (ext 532); fax, (949) 362-2049; reprints@aacn.org.
REFERENCES
- 1.Thom T, Haase N, Rosamond W, et al. American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics — 2006 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee [published corrections in Circulation. 2006;113(14):e696 and 2006;114(23):e630] Circulation. 2006;113(6):e85–e151. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Ha JW. Diastolic dysfunction and heart failure: a new paradigm [in Korean] Korean J Med. 2003;65(6):631–637. [Google Scholar]
- 3.Han SW, Ryu KH, Chae SC, et al. Multicenter analysis of clinical characteristics and prognostic factors of patients with congestive heart failure in Korea [in Korean] Korean Circ J. 2005;35:357–361. [Google Scholar]
- 4.Lee MM, Oh BH, Park HS, et al. Multicenter analysis of clinical characteristics of the patients with congestive heart failure in Korea [in Korean] Korean Circ J. 2003;33(6):533–541. [Google Scholar]
- 5.Richardson LG, Rocks M. Women and heart failure. Heart Lung. 2001;30(2):87–97. doi: 10.1067/mhl.2001.114191. [DOI] [PubMed] [Google Scholar]
- 6.Wenger NK. Women, heart failure, and heart failure therapies. Circulation. 2002;105(13):1526–1528. doi: 10.1161/01.cir.0000014121.94868.81. [DOI] [PubMed] [Google Scholar]
- 7.Meinert CL, Gilpin AK, Unalp A, Dawson C. Gender representation in trials. Control Clin Trials. 2000;21(5):462–475. doi: 10.1016/s0197-2456(00)00086-6. [DOI] [PubMed] [Google Scholar]
- 8.Paton B, Backlund J, Barnes M, Thirsk L. Recalibrating time and space: women’s challenges of living with heart failure. Can J Cardiovasc Nurs. 2007;17(1):7–14. [PubMed] [Google Scholar]
- 9.Adams KF, Jr, Sueta CA, Gheorghiade M, et al. Gender differences in survival in advanced heart failure: insights from the FIRST study. Circulation. 1999;99(14):1816–1821. doi: 10.1161/01.cir.99.14.1816. [DOI] [PubMed] [Google Scholar]
- 10.Deswal A, Bozkurt B. Comparison of morbidity in women versus men with heart failure and preserved ejection fraction. Am J Cardiol. 2006;97(8):1228–1231. doi: 10.1016/j.amjcard.2005.11.042. [DOI] [PubMed] [Google Scholar]
- 11.Friedman MM. Gender differences in the health related quality of life of older adults with heart failure. Heart Lung. 2003;32(5):320–327. doi: 10.1016/s0147-9563(03)00098-0. [DOI] [PubMed] [Google Scholar]
- 12.Ng AC, Wong HS, Yong AS, Sindone AP. Impact of gender on outcomes in chronic systolic heart failure. Int J Cardiol. 2007;117(2):214–221. doi: 10.1016/j.ijcard.2006.04.079. [DOI] [PubMed] [Google Scholar]
- 13.Koelling TM, Chen RS, Lubwama RN, L’Italien GJ, Eagle KA. The expanding national burden of heart failure in the United States: the influence of heart failure in women. Am Heart J. 2004;147(1):74–78. doi: 10.1016/j.ahj.2003.07.021. [DOI] [PubMed] [Google Scholar]
- 14.Riedinger MS, Dracup KA, Brecht ML, Padilla G, Sarna L, Ganz PA. Quality of life in patients with heart failure: do gender differences exist? Heart Lung. 2001;30(2):105–116. doi: 10.1067/mhl.2001.114140. [DOI] [PubMed] [Google Scholar]
- 15.Chin MH, Goldman L. Gender differences in 1-year survival and quality of life among patients admitted with congestive heart failure. Med Care. 1998;36(7):1033–1046. doi: 10.1097/00005650-199807000-00010. [DOI] [PubMed] [Google Scholar]
- 16.Hou N, Chui MA, Eckert GJ, Oldridge NB, Murray MD, Bennett SJ. Relationship of age and sex to health-related quality of life in patients with heart failure. Am J Crit Care. 2004;13(2):153–161. [PubMed] [Google Scholar]
- 17.Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY. Health-related quality of life in elderly patients with heart failure. Scand Cardiovasc J. 1999;33(5):278–285. doi: 10.1080/14017439950141524. [DOI] [PubMed] [Google Scholar]
- 18.Riedinger MS, Dracup KA, Brecht ML. Predictors of quality of life in women with heart failure. SOLVD Investigators. Studies of Left Ventricular Dysfunction. J Heart Lung Transplant. 2000;19(6):598–608. doi: 10.1016/s1053-2498(00)00117-0. [DOI] [PubMed] [Google Scholar]
- 19.Heo S, Moser DK, Widener J. Gender differences in the effects of physical and emotional symptoms on health-related quality of life in patients with heart failure. Eur J Cardiovasc Nurs. 2007;6(2):146–152. doi: 10.1016/j.ejcnurse.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Yeh GY, Wood MJ, Lorell BH, et al. Effects of tai chi mind-body movement therapy on functional status and exercise capacity in patients with chronic heart failure: a randomized controlled trial. Am J Med. 2004;117(8):541–548. doi: 10.1016/j.amjmed.2004.04.016. [DOI] [PubMed] [Google Scholar]
- 21.Carels RA. The association between disease severity, functional status, depression and daily quality of life in congestive heart failure patients. Qual Life Res. 2004;13(1):63–72. doi: 10.1023/B:QURE.0000015301.58054.51. [DOI] [PubMed] [Google Scholar]
- 22.Marwick TH, Zuchowski C, Lauer MS, Secknus MA, Williams J, Lytle BW. Functional status and quality of life in patients with heart failure undergoing coronary bypass surgery after assessment of myocardial viability. J Am Coll Cardiol. 1999;33(3):750–758. doi: 10.1016/s0735-1097(98)00642-1. [DOI] [PubMed] [Google Scholar]
- 23.Hawthorne MH, Hixon ME. Functional status, mood disturbance and quality of life in patients with heart failure. Prog Cardiovasc Nurs. 1994;9(1):22–32. [PubMed] [Google Scholar]
- 24.van den Broek SA, van Veldhuisen DJ, de Graeff PA, Landsman ML, Hillege H, Lie KI. Comparison between New York Heart Association classification and peak oxygen consumption in the assessment of functional status and prognosis in patients with mild to moderate chronic congestive heart failure secondary to either ischemic or idiopathic dilated cardiomyopathy. Am J Cardiol. 1992;70(3):359–363. doi: 10.1016/0002-9149(92)90619-a. [DOI] [PubMed] [Google Scholar]
- 25.Coyne KS, Allen JK. Assessment of functional status in patients with cardiac disease. Heart Lung. 1998;27(4):263–273. doi: 10.1016/s0147-9563(98)90038-3. [DOI] [PubMed] [Google Scholar]
- 26.Leidy NK. Functional status and the forward progress of merry-go-rounds: toward a coherent analytical framework. Nurs Res. 1994;43(4):196–202. [PubMed] [Google Scholar]
- 27.Rao A, Asadi-Lari M, Walsh J, Wilcox R, Gray D. Quality of life in patients with signs and symptoms of heart failure — does systolic function matter? J Card Fail. 2006;12(9):677–683. doi: 10.1016/j.cardfail.2006.08.004. [DOI] [PubMed] [Google Scholar]
- 28.Martensson J, Stromberg A, Dahlstrom U, Karlsson JE, Fridlund B. Patients with heart failure in primary health care: effects of a nurse-led intervention on health-related quality of life and depression. Eur J Heart Fail. 2005;7(3):393–403. doi: 10.1016/j.ejheart.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 29.Franzen K, Saveman BI, Blomqvist K. Predictors for health related quality of life in persons 65 years or older with chronic heart failure. Eur J Cardiovasc Nurs. 2007;6(2):112–120. doi: 10.1016/j.ejcnurse.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Lenz ER, Suppe F, Gift AG, Pugh LC, Milligan RA. Collaborative development of middle-range nursing theories: toward a theory of unpleasant symptoms. ANS Adv Nurs Sci. 1995;17(3):1–13. doi: 10.1097/00012272-199503000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Carlson B, Riegel B, Moser DK. Self-care abilities of patients with heart failure. Heart Lung. 2001;30(5):351–359. doi: 10.1067/mhl.2001.118611. [DOI] [PubMed] [Google Scholar]
- 32.Johnson MR. Heart failure in women: a special approach? J Heart Lung Transplant. 1994;13(4):S130–S134. [PubMed] [Google Scholar]
- 33.Johnstone D, Limacher M, Rousseau M, et al. Clinical characteristics of patients in Studies of Left Ventricular Dysfunction (SOLVD) Am J Cardiol. 1992;70(9):894–900. doi: 10.1016/0002-9149(92)90734-g. [DOI] [PubMed] [Google Scholar]
- 34.Costello JA, Boblin S. What is the experience of men and women with congestive heart failure? Can J Cardiovasc Nurs. 2004;14(3):9–20. [PubMed] [Google Scholar]
- 35.Brostrom A, Stromberg A, Dahlstrom U, Fridlund B. Sleep difficulties, daytime sleepiness, and health-related quality of life in patients with chronic heart failure. J Cardiovasc Nurs. 2004;19(4):234–242. doi: 10.1097/00005082-200407000-00003. [DOI] [PubMed] [Google Scholar]
- 36.Gottlieb SS, Khatta M, Friedmann E, et al. The influence of age, gender, and race on the prevalence of depression in heart failure patients. J Am Coll Cardiol. 2004;43(9):1542–1549. doi: 10.1016/j.jacc.2003.10.064. [DOI] [PubMed] [Google Scholar]
- 37.Rutledge T, Reis SE, Olson MB, et al. Depression symptom severity and reported treatment history in the prediction of cardiac risk in women with suspected myocardial ischemia: the NHLBI-sponsored WISE study. Arch Gen Psychiatry. 2006;63(8):874–880. doi: 10.1001/archpsyc.63.8.874. [DOI] [PubMed] [Google Scholar]
- 38.Broström A, Johansson P, Kihl J, et al. Depressive symptoms in men and women with chronic heart failure — effects on sleep, daytime sleepiness and health-related quality of life. Eur J Cardiovasc Nurs. 2006;5 suppl 1:S14–S15. [Google Scholar]
- 39.Judd LL, Akiskal HS, Zeller PJ, et al. Psychosocial disability during the long-term course of unipolar major depressive disorder. Arch Gen Psychiatry. 2000;57(4):375–380. doi: 10.1001/archpsyc.57.4.375. [DOI] [PubMed] [Google Scholar]
- 40.Luttik ML, Jaarsma T, Veeger N, van Veldhuisen DJ. Marital status, quality of life, and clinical outcome in patients with heart failure. Heart Lung. 2006;35(1):3–8. doi: 10.1016/j.hrtlng.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 41.Gott M, Barnes S, Payne S, et al. Patient views of social service provision for older people with advanced heart failure. Health Soc Care Community. 2007;15(4):333–342. doi: 10.1111/j.1365-2524.2007.00689.x. [DOI] [PubMed] [Google Scholar]
- 42.Gott M, Barnes S, Parker C, et al. Predictors of the quality of life of older people with heart failure recruited from primary care. Age Ageing. 2006;35(2):172–177. doi: 10.1093/ageing/afj040. [DOI] [PubMed] [Google Scholar]
- 43.McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285(26):1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- 44.Solomon SD, Dobson J, Pocock S, et al. Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation. 2007;116(13):1482–1487. doi: 10.1161/CIRCULATIONAHA.107.696906. [DOI] [PubMed] [Google Scholar]
- 45.Hunt SA, Abraham WT, Chin MH, et al. American College of Cardiology; American Heart Association Task Force on Practice Guidelines; American College of Chest Physicians; International Society for Heart and Lung Transplantation; Heart Rhythm Society. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: endorsed by the Heart Rhythm Society. Circulation. 2005;112(12):e154–e235. doi: 10.1161/CIRCULATIONAHA.105.167586. [DOI] [PubMed] [Google Scholar]
- 46.Sung J, On YK, Kim HS, et al. Development of Korean Activity Scale/Index (KASI) Korean Circ J. 2000;30(8):1004–1009. [Google Scholar]
- 47.Beck AT. Depression: Causes and Treatments. Philadelphia, PA: University of Pennsylvania Press; 1967. [Google Scholar]
- 48.Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive Therapy of Depression. New York, NY: Guilford Press; 1979. [Google Scholar]
- 49.Rhee MK, Lee YH, Park SH, et al. A standardization study of Beck Depression Inventory 1-Korean version (K-BDI): reliability and factor analysis. Korean J Psychopathol. 1995;4(1):77–95. [Google Scholar]
- 50.Bennett JA. Mediator and moderator variables in nursing research: conceptual and statistical differences. Res Nurs Health. 2000;23(5):415–420. doi: 10.1002/1098-240x(200010)23:5<415::aid-nur8>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 51.Plach SK. Psychological well-being in women with heart failure: can social roles make a difference? Health Care Women Int. 2008;29(1):54–75. doi: 10.1080/07399330701723830. [DOI] [PubMed] [Google Scholar]
- 52.Howie-Esquivel J, Dracup K. Effect of gender, ethnicity, pulmonary disease, and symptom stability on rehospitalization in patients with heart failure. Am J Cardiol. 2007;100(7):1139–1144. doi: 10.1016/j.amjcard.2007.04.061. [DOI] [PubMed] [Google Scholar]
- 53.Bennett SJ, Cordes DK, Westmoreland G, Castro R, Donnelly E. Self-care strategies for symptom management in patients with chronic heart failure. Nurs Res. 2000;49(3):139–145. doi: 10.1097/00006199-200005000-00004. [DOI] [PubMed] [Google Scholar]
- 54.Struthers AD, Anderson G, Donnan PT, MacDonald T. Social deprivation increases cardiac hospitalisations in chronic heart failure independent of disease severity and diuretic non-adherence. Heart. 2000;83(1):12–16. doi: 10.1136/heart.83.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rathore SS, Masoudi FA, Wang Y, et al. Socioeconomic status, treatment, and outcomes among elderly patients hospitalized with heart failure: findings from the National Heart Failure Project. Am Heart J. 2006;152(2):371–378. doi: 10.1016/j.ahj.2005.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dunbar SB, Clark PC, Deaton C, Smith AL, De AK, O’Brien MC. Family education and support interventions in heart failure: a pilot study. Nurs Res. 2005;54(3):158–166. doi: 10.1097/00006199-200505000-00003. [DOI] [PubMed] [Google Scholar]