Abstract
Although much is known about how TNF-α induces apoptosis in the presence of inhibitors of protein synthesis, little is known about how it induces apoptosis without these inhibitors. In this report we investigated temporal sequence of events induced by TNF-α in the absence of protein synthesis. Regardless of whether we measured the effects by plasma membrane phosphotidylserine accumulation, by DNA strand breaks, or activation of caspases, significant changes were observed only between 12–24 h of TNF-α treatment. One of the earliest changes observed after TNF-α treatment was mitochondrial swelling at 10 min; followed by cytochrome c and Smac release at 10–30 min, and then heterochromatin clumping occurred at 60 min. While genetic deletion of receptor-interaction protein (RIP) had no effect on TNF-α-induced mitochondrial damage, deletion of Fas-associated death domain (FADD) abolished the TNF-induced mitochondrial swelling. Since pan-caspase inhibitor z-VAD-fmk abolished the TNF-α-induced mitochondrial changes, z-DEVD-fmk, an inhibitor of caspase-3 had no effect, suggesting that TNF-α-induced mitochondrial changes or cytochrome c and Smac release requires caspase-8 but not caspase-3 activation. Overall, our results indicated that mitochondrial changes are early events in TNF-α-induced apoptosis and that these mitochondrial changes require recruitment of FADD and caspase-8 activation, but not caspase-3 activation or RIP recruitment. Antioxid. Redox Signal. 13, 821–831.
Introduction
Tumor necrosis factor-α (TNF-α) was initially isolated as a cytokine that specifically kills tumor cells (2, 31). Subsequent work indicated TNF-α-induced cell killing is mediated through specific cell surface receptors (2). Although two different types of transmembrane TNF receptors have been identified, only type I, which is ubiquitously expressed on all eukaryotic cells, is known to mediate apoptosis through its cytoplasmic death domain; this domain sequentially interacts with TNFR1-associated death domain (TRADD), Fas-associated death domain protein (FADD), and FADD-like interleukin-1β-converting enzyme (FLICE) (1). TRADD, however, can also bind to TNFR-associated factor 2 (TRAF2) and receptor-interaction protein (RIP), leading to activation of various transcription factors including NF-κB, which regulates the expression of genes involved in tumor cell survival and inflammation.
Although much is known about the mechanism by which TNF-α mediates apoptosis in different cell types, new information indicates TNF-α induces proliferation as well as cell killing by diverse methods (4, 20, 38, 40). For instance, cell killing by TNF-α through both apoptotic and nonapoptotic mechanisms has been described (30, 45). Nonapoptotic mechanisms usually involve necrosis or autophagy (26, 34, 45). While in most instances TNF-α-induced apoptosis is caspase dependent; recent reports also describe caspase-independent mechanisms for TNF-α-induced apoptosis (26, 45). In a recent report, treatment of a particular cell population with TNF-α produced both apoptosis and necrosis (45). What determines whether cells will die through apoptotic or nonapoptotic mechanisms is not known.
At the subcellular level, extensive research within the last decade has implicated the critical role of mitochondria in TNF-α-induced apoptosis and necrosis (10, 13, 15, 17, 19, 21, 25). The following events have been linked with mitochondrial changes: release of reactive oxygen species, mitochondrial membrane hyperpolarization and depolarization, matrix swelling, activation of Bax/Bak in response to cytosolic truncated Bid, increased permeability of the outer membrane, release of cytochrome c, and Smac, induction of apoptosis-inducing factor (AIF), and the appearance of second mitochondria-derived activator of caspase/direct inhibitor of apoptosis (IAP)-binding protein with low pI (Smac/DIABLO) (37). Additionally a 60-kDa mitochondrial protein has been identified to which TNF can bind directly (24), thus leading to uncoupling of mitochondria (7). Inhibition of electron transport chain (ETS) complex III of mitochondria potentiates TNF-α-induced apoptosis, but inhibition of complex I and II inhibits TNF-α-induced apoptosis (32, 35). Our laboratory has shown that mitochondrial antioxidant enzymes such as superoxide dismutase abolish TNF-α-induced apoptosis (27).
That most cell types are resistant to TNF-α-induced cell-killing when treated with the cytokine alone was reported several years ago by our laboratory (3, 40). When treated with TNF in the presence of a protein synthesis inhibitor such as cycloheximide or actinomycin D, most cells become susceptible to TNF-α-induced cell killing; suggesting a critical role for protein synthesis. It is now clear that TNF-α activates the transcription factor NF-κB, which controls the expression of cell survival proteins such as Bcl-xL, IAP-1, IAP-2, XIAP, and cFLIP, which mediate antiapoptosis (8, 9, 23, 39). The suppression of synthesis of these proteins is needed to sensitize most cells to TNF-α-induced apoptosis (44). Most studies on TNF-α-induced apoptosis have used cells treated with TNF-α in the presence of protein synthesis inhibitors, which do not represent a physiological environment. Which of the various temporal sequences of events that lead to cell killing in the absence of inhibitors of protein synthesis is less well understood. Thus, the aim of this study was to investigate various temporal requirements for TNF-α-induced mitochondrial changes in T cells. We found that mitochondrial changes are early events in TNF-α-induced apoptosis and that it requires FADD and caspase-8 activation, but not caspase-3 or RIP recruitment.
Materials and Methods
Reagents
Monoclonal antibodies against cytochrome c, anti-active caspase-3 (AF835), and TNF were obtained from R&D Systems (Abingdon, UK). Polyclonal antibody against Smac was obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Dihydro-rhodamine 123 was obtained from Sigma (Munich, Germany), and z-VAD-fmk (benzyloxycarbonyl-Val-Ala-Asp-fluoromethylketone) and z-DEVD-fmk were from Biomol (Hamburg, Germany). Secondary antibody GAM (10 nm goat-anti-mouse immunoglobulin conjugated with 10 nm gold particles) was purchased from Amersham (Braunschweig, Germany). LR-White (London Resin) and Epon were purchased from Plano (Marburg, Germany).
Cell lines
Jurkat cells were cultured in growth medium consisting of Ham's F-12/Dulbecco's modified Eagle's medium (1:1) containing 10% fetal calf serum (FCS), 25 μg/ml ascorbic acid, 50 IU/ml streptomycin, 50 IU/ml penicillin, 2.5 μg/ml amphotericin B, essential amino acids, and L-glutamine (Seromed, Munich, Germany).
Isolation of cytosolic fractions
Jurkat cells were trypsinized and washed twice in 1 ml ice cold PBS. The supernatant was carefully removed. Cell pellet was resuspended in 400 μl hypotonic lysis buffer containing protease inhibitors and incubated on ice for 15 min. 12.5 μl of 10% NP-40 were added and the cell suspension vigorously mixed for 15 sec. The extracts were centrifuged for 1.5 min. The supernatants (cytoplasmic extracts) were frozen at −70°C.
Isolation of mitochondrial fractions
Cells were washed in twice in 1 ml ice cold PBS and placed in ice-cold mitochondria isolation buffer (0.25 M sucrose, 0.2 mM EDTA, and 10 mM Tris–HCl, pH 7.8) for 30 min, followed by homogenization using a pre-cooled glass homogenizer. Cell lysates were centrifuged at 1000 g for 15 min at 4°C and the supernatant was centrifuged at 12,000 g for 15 min at 4°C. Pelleted mitochondria were resuspended in ice-cold mitochondria isolation buffer containing protease inhibitors (5 μg/ml leupeptin, 5 μg/ml pepstatin, 10 μg/ml aprotinin, 1 mM PMSF, 1 mM DTT, 100 μM sodium orthovanadate, 10 mM sodium fluoride, and 10 μM phenylarsine oxide).
Transmission electron microscopy
The transmission electron microscopy experiment was performed as described previously (36). Briefly, the Jurkat cells were fixed in 1% glutaraldehyde plus 1% tannic acid in 0.1 M phosphate buffer, pH 7.4, post-fixed in 1% OsO4 in the same buffer, rinsed and dehydrated in ethanol, embedded in Epon, cut with an Ultracut E (Reichert), and stained with 2% uranyl acetate/lead citrate. The specimens were examined with a transmission electron microscope (TEM) (Zeiss EM 10).
Immunoelectron microscopy
The immunoelectron microscopy experiment was performed as described previously (36). Briefly, immediately after fixation (3% paraformaldehyde, 0.25% glutaraldehyde in PBS for 1 h), the Jurkat cells were rinsed with PBS/BSA overnight and gradually dehydrated in ethanol. Subsequently, the cells were embedded in fresh LR-White (London Resin). LR-White sections were cut on an Ultracut E (Reichert) and placed on nickel grids. These grids were placed in a moist chamber on the top of drops of the following solutions: (a) l% bovine serum albumin (BSA) in 0.01 M PBS, pH 7.0 and in 0.5% Tween for 30 min for blocking at room temperature (RT); (b) primary antibody (anti-cytochrome c 1:30 in PBS/BSA/Tween, overnight at 4°C), (c) rinsing in PBS/BSA/Tween at RT; (d) secondary antibody (GAM 10 nm 1:30 in PBS/BSA/Tween) for 60 min at RT; (e) rinsing in PBS/BSA/Tween RT; (f ) fixation (l% glutaraldehyde) for 10 min at RT. Contrasting was carried out with an aqueous saturated solution of 5% uranyl acetate for 20 min, OsO4 for 5 min, and l% tannic acid for 30 min at RT. Examination was performed using a Zeiss TEM.
Toluidine blue staining of Jurkat cells
Semi-thin sections of Jurkat cells embedded in Epon were stained with 0.2 % toluidine blue and rinsed gently 3 × 10 min in aqua bidest. Sections were air dried and covered with gelatin before examination under a Zeiss Axiophot 100 light microscope.
Alkaline phosphatase/anti-alkaline phosphatase method
Pellets of Jurkat cells were immersed in OCT embedding medium and immediately frozen in liquid nitrogen. 5 μm cryosections of cells were fixed with acetone (10 min) and washed twice (5 min) in TBS (0.05 M Tris, 0.15 M NaCl, pH 7.6) at room temperature (RT). Slides were incubated with serum (1:20) in TBS at RT for 10 min and then incubated with primary antibodies 1:30 in TBS in a moist chamber overnight at 4°C. Cells were rinsed as described above and if polyclonal primary antibody was used, additionally incubated with mouse anti-rabbit IgG antibodies (1:50) in TBS for 30 min at RT. They were rinsed again before incubation with dual system bridge antibodies (1:50 in TBS). After rinsing, sections were incubated with dual-system alkaline phosphatase-anti-alkaline-phosphatase (APAAP) complex (1:50) in TBS for 30 min at RT. After thorough rinsing, cells were stained with new fuchsin for 30 min at RT. Cells were washed, air dried, covered with an Kaisers' glycerol gelatin, and examined with a Axiophot 100 light microscope.
Western blot analysis
Jurkat cells were washed three times with Hanks' balanced salt solution and then proteins were extracted with lysis buffer (0.05 M Tris/HCl, pH 7.2, 0.15 M NaCl, l% (v/v) Triton X-100, 1 mM sodium orthovanadate, 50 mM sodium pyrophosphate, 0.1 M sodium fluoride, 0.01% (v/v) aprotinin, 4 μg/ml pepstatin A, 10 μg/ml leupeptin, 1 mM PMSF) on ice for 30 min. Cell debris was removed by centrifugation and supernatants were stored at −70°C until use. Protein determination was performed using the bicinchoninic acid system (Uptima, Interchim, Montlucon, France) and BSA as a standard. Samples of similar total protein concentration were separated by SDS-PAGE under reducing conditions. The separated proteins were transferred onto nitrocellulose membranes. Membranes were pre-incubated in blocking buffer (5% (w/v) skimmed milk powder in PBS/0.1% Tween 20) for 30 min, and incubated with primary antibodies (1 h, RT). Membranes were washed three times with blocking buffer and incubated with alkaline phosphatase-conjugated secondary antibodies for 30 min. They were finally washed three times in 100 mM Tris (pH 9.5) containing 50 mM MgCl2 and 100 mM NaCl. Nitro blue tetrazolium and 5-bromo-4-chloro-3-indoylphosphate (p-toluidine salt; Pierce, Rockford, IL) were used as substrate to reveal alkaline phosphatase-conjugated specific antigen–antibody complexes.
Annexin V assay
One of the early indicators of apoptosis is the rapid translocation and accumulation of the membrane phospholipid phosphatidylserine from the cell's cytoplasmic interface to the extracellular surface. This loss of membrane asymmetry can be detected using the binding properties of annexin V. To detect this, we employed annexin V antibody conjugated with the fluorescent dye FITC. Briefly, 1 × 106 cells were treated with TNF-α for different times, and then subjected to annexin V staining. Cells were washed, stained with FITC-conjugated anti-annexin V antibody, and then analyzed with a flow cytometer (FACSCalibur; BD Biosciences).
Terminal deoxynucleotidyl transferase-mediated deoxyuridine triphosphate nick end-labeling assay
We assayed cytotoxicity by the TUNEL method, which examines DNA strand breaks, using an in situ cell death detection reagent (Roche Molecular Biochemicals, Mannheim, Germany). Briefly, 1 × 106 cells were treated with TNF-α for different times at 37°C. Thereafter, cells were incubated with reaction mixture for 60 min at 37°C. Stained cells were analyzed by flow cytometer (FACSCalibur, BD Biosciences).
Measurement of reactive oxygen intermediate
Jurkat cells were incubated in growth medium and treated with TNF-α (1 nM) for the indicated times. The cells were washed in PBS and incubated with dihydro-rhodamine 123 (DHR-123: 5 mM stock solution in DMSO) at a final concentration of 1 μM for 1 h. The fluorescence intensity resulting from DHR 123 oxidation was measured by a FACScan flow cytometer with excitation at 488 nm and was detected between 515 and 550 nm.
Statistical analysis
Immunoblots were semi-quantitatively analysed using the computer program “Quantity one” (Bio-Rad, Munich, Germany). The results are expressed as the means ± SD of a representative experiment performed in triplicate. The means were compared using Student's t-test assuming equal variances. P < 0.05 was considered statistically significant.
Results
The goal of this study was to investigate temporal sequence of events with relation to mitochondrial changes that occur on TNF-α treatment of cells in the absence of protein synthesis inhibitors. For this, we used human Jurkat T cells, which express both forms of TNF receptors.
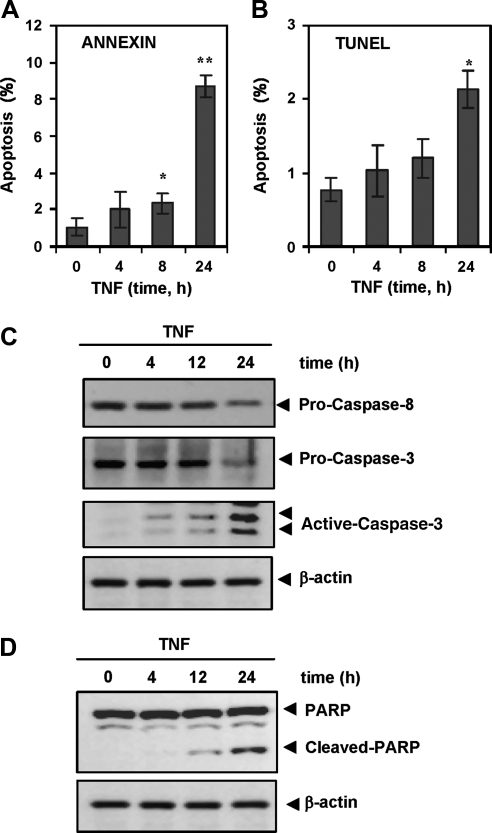
TNF-α-induced plasma membrane phosphotidylserine accumulation and DNA strand breaks, are late event
To determine these, Jurkat cells were treated for 4, 8, and 24 h with TNF-α (1 nM) and then examined for plasma membrane phosphotidylserine accumulation by Annexin staining (Fig. 1A) and for DNA strand breaks by TUNEL assay (Fig. 1B). Results indicated that a significant change occurred only after 24 h of TNF-α treatment. Even after 24 h only 8% of cells were Annexin positive and 2% were TUNEL positive.
FIG. 1.
Effect of TNF-α on different apoptotic parameters. (A) Jurkat cells were treated with 1 nM TNF-α for the indicated times, then incubated with anti-annexin V antibody conjugated with FITC and analyzed with a flow cytometer for apoptotic effects. (B) Cells were incubated with 1 nM TNF-α for indicated times, fixed, stained with TUNEL assay reagent and then analyzed with flow cytometer. Columns, mean from three different experiments with triplicate wells per experiment; bars, SD. *p < 0.05; **p < 0.01, Student's t test. (C) and (D) Jurkat cells were treated with 1 nM TNF-α for 4, 12, and 24 h, prepared the whole-cell extracts and subjected to Western blot analysis using antibodies against PARP, pro-caspase-8, pro-caspase-3, and cleave-caspase-3, as indicated. Blot was reprobed for β-actin to confirm equal loading.
TNF-α activates caspases and induces PARP cleavage
To determine these, Jurkat cells were treated for 4, 8 and 24 h with TNF-α (1 nM) and then examined for caspase-8 and caspase-3 activation (Fig. 1C) and PARP cleavage by Western blot analysis (Fig. 1D). Results indicated that a significant activation of both caspase-8 and caspase-3 and PARP cleavage can be detected only after 24 h of TNF-α treatment.
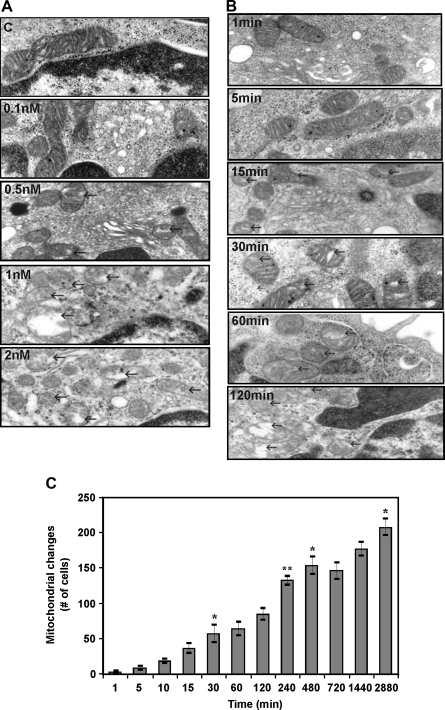
TNF-induced mitochondrial changes is an early event
When cells were examined for TNF-α-induced ultra-structural damage, one of the earliest changes was mitochondrial. This effect was found to be dose- (Fig. 2A) and time-dependent (Fig. 2B). Mitochondrial changes could be seen as early as 5 min and continued to accumulate until 96 h (Fig. 2C).
FIG. 2.
Dose response of TNF-α induced-mitochondrial changes. Transmission electron microscopic investigations of Jurkat cells in monolayer culture (A). The cells were treated with indicated concentrations of TNF-α for 1 h. Degenerative changes in mitochondria (swelling and dilatation) (arrows) increased in Jurkat cells with increasing concentration of TNF-α in the growth medium. Original magnification, × 50,000. (B) Time course of TNF-α-induced mitochondrial changes. Transmission electron microscopic investigations of Jurkat cells in monolayer culture. Jurkat cells were incubated for indicated time intervals with 1 nM TNF-α. Degenerative changes in mitochondria (swelling and dilatation) (arrows) increased in Jurkat cells with increasing time. Original magnification, X 50,000. (C) Effect of TNF-α on mitochondria in Jurkat cells. Jurkat cells were treated with TNF-α (1 nM) for indicated times. The number of cells with mitochondrial changes was determined by scoring 250 cells from 30 different microscopic fields in the electron microscope. The diagram shows the number of pathologically altered cells. Columns, mean from three different experiments; bars, SD. *p < 0.05; **p < 0.01, Student's t test.
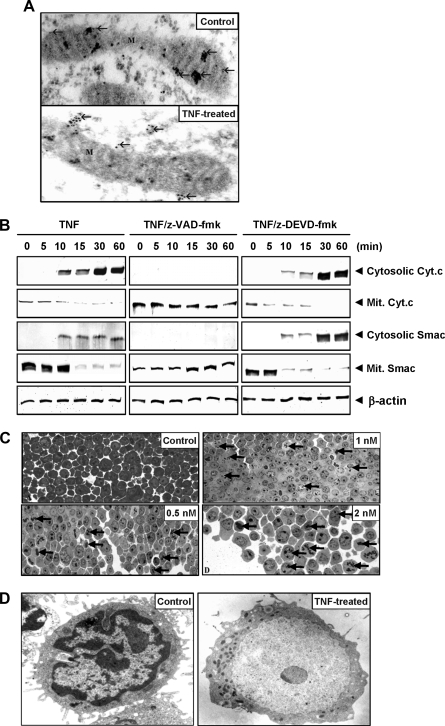
TNF-α-induced mitochondrial cytochrome c and Smac release to cytosol is an early event
We determined whether TNF-α induces mitochondrial cytochrome c and Smac release, a hallmark of apoptosis (12), in the absence of protein synthesis inhibitors in Jurkat cells. Cells were treated with TNF-α for 1 h and then examined for cytochrome c release by using immunogold-labeled with anti-cytochrome c antibodies. In untreated cells, antibody-coupled gold particles were visible within the mitochondrial intermembranal space (Fig. 3A, upper panel). In TNF-α treated cells, however, cytochrome c was found outside the mitochondria in the cytoplasma of Jurkat cells, demonstrating a release of cytochrome c in response to the treatment. Only a few gold particles were still visible in the organelles (Fig. 3A, lower panel).
FIG. 3.
Cytochrome c-release from mitochondria in TNF-α treated cells. (A) Immunoelectron microscopic demonstration of cytochrome c release in Jurkat cells treated with 1 nM TNF-α for 30 min. Gold particles are localized (arrows) in untreated cells (top panel) within the mitochondria (M) and in treated cells (bottom panel) outside the mitochondria, demonstrating a release of cytochrome c in response to TNF-α treatment (original magnification, X 50,000). (B) Effect of the caspase inhibitor z-VAD-fmk and z-DEVD-fmk on cytochrome c- and Smac-release from mitochondria in TNF-α-treated cells. Cells were either left untreated or pre-incubated with either z-VAD-fmk (benzyloxycarbonyl-Val-Ala-Asp-fluoromethylketone) (50 μM) or z-DVED-fmk (50 μM) for 1 h and then treated with TNF-α (1 nM) for the indicated times. Cytosolic and mitochondrial fractions were prepared as described in Materials and Methods and were investigated for cytochrome c and Smac using anti-cytochrome c and anti-Smac antibodies by Western blot analysis. Equal amounts (50 μg of protein per lane) of total proteins were separated by 15% SDS-PAGE and analyzed by immunoblotting against cytochrome c and Smac. The results shown are representative of three independent experiments. Equal protein loading was evaluated by β-actin. (C) Toluidine blue staining in Jurkat cells treated with TNF-α. Jurkat cells were treated with increasing concentrations of TNF-α for 1 h, stained with toluidine blue, and then observed under light microscope. The staining intensity decreased with TNF-α dosage and an increasing number of cells showed clumped heterochromatin in their nuclei. More and more cell debris was visible, suggesting an increasing amount of cell death (original magnification, X 160). (D) TNF-α induces apoptosis in Jurkat cells. Electron microscopic demonstration of an untreated and TNF-α-treated (1 nM for 30 min) cells. Untreated cells could be seen as round to oval containing smooth surface, numerous small ridge-like or cusp-like surface processes, a large nucleus with much loosely packed, despiralized, and functionally active euchromatin, and small, increased density, functionally inactive heterochromatin, and numerous cavities of rough endoplasmic reticulum (original magnification, X 10,000). TNF-α treated cell has nuclear changes with peripheral segregation and aggregation of chromatin into dense areas along the nuclear membrane, swellings and dilatations of cell organelles, and bleb formation at the cell membrane.
To further confirm the immunolabelling results, we isolated mitochondrial and cytosolic fractions from normal or TNF-α-treated Jurkat cells and then examined for cytochrome c and Smac release by Western blot analysis. As shown in Figure 3B, left panel, in control (untreated) cells, Smac and cytochrome c were exclusively localized in mitochondrial fractions. 10 min after TNF-α-treatment, cytochrome c and Smac were both observed in the cytosolic fraction. The cytosolic Smac and cytochrome c continued to increase up to 60 min with a corresponding decrease in the mitochondrial compartment.
Pan-caspase inhibitor inhibits TNF-α-induced cytochrome c and Smac release but caspase-3 inhibitor does not
We determined the effect of pan-caspase inhibitor (z-VAD-fmk) on the kinetics of TNF-α-induced mitochondrial cytochrome c and Smac release in Jurkat cells. Cells were treated with TNF for different times in the presence of z-VAD-fmk and then examined for cytochrome c and Smac release by Western blot analysis (Fig. 3B, middle panel). The results show that the z-VAD-fmk completely abolished the TNF-α-induced cytosolic cytochrome c and Smac release with a corresponding amount in the mitochondrial compartment, indicating the critical requirement of caspases for cytochrome c and Smac release.
Since z-VAD-fmk is known to inhibit both caspase-8 and caspase-3 activation, we used z-DEVD-fmk, the caspase-3 inhibitor to distinguish between the two caspases. The results in Figure 3B (right panel) show that caspase-3 inhibitor had no effect on TNF-α-induced cytosolic cytochrome c and Smac release. The cytosolic Smac and cytochrome c continued to increase up to 60 min with a corresponding decrease in the mitochondrial compartment.
Thus, these results suggest that caspase-8 is required for cytochrome c and Smac release but not caspase-3.
TNF-α-induced chromatin condensation is an early event
Whether TNF-α induces chromatin condensation was examined by staining the cells with toluidine blue. Jurkat cells were treated with different concentrations of TNF-α for 1 h and then stained. The staining intensity of cells decreased with the increasing TNF-α concentration. More cells revealed chromatin condensations in their nuclei in response to TNF-α treatment (Fig. 3C), indicating that it is an early event.
Untreated cells had a round to oval shape with a smooth surface, numerous small ridge-like or cusp-like surface processes, a large nucleus with much loosely packed, functionally active euchromatin, functionally inactive heterochromatin, and numerous cavities of rough endoplasmic reticulum (Fig. 3D). Treatment with TNF-α revealed typical features of apoptosis such as nuclear changes with peripheral segregation and aggregation of chromatin into dense areas along the nuclear membrane, swellings, and dilatations of cell organelles, and bleb formation at the cell membrane (Fig. 3D).
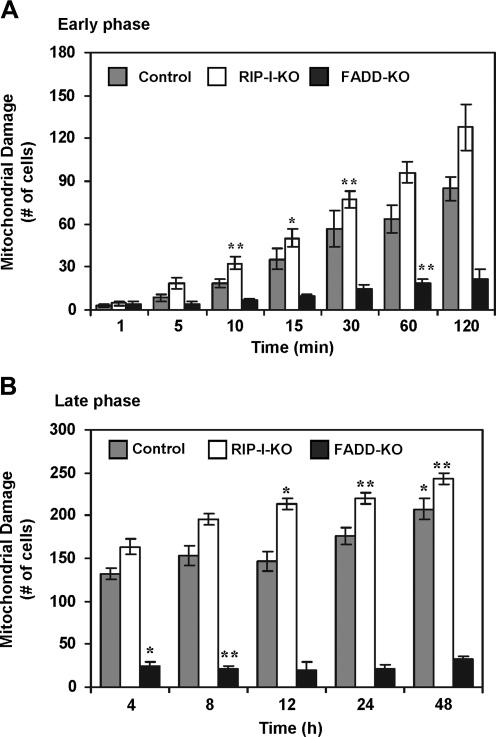
Mitochondrial changes are RIP independent
RIP is a protein that is recruited by the TNFR1 (18); it has been shown to be needed for TNF-α-induced NF-κB activation (22, 42), and in TNF-α-induced cell survival and proliferation (41). Whether it plays any role in TNF-α-induced mitochondrial changes was examined by using RIP-gene-deleted Jurkat cells. Results in Figures 4A and 4B indicate that deletion of RIP had no effect on TNF-induced mitochondrial changes. A slight but significant increase in mitochondrial changes indicates that RIP deletion may enhance the TNF-α-induced mitochondrial damage, thus suggesting a potential role for RIP in cell survival.
FIG. 4.
Effect of TNF-α on mitochondria in control, RIP, and FADD knock out cells. Cells (control, RIP, and FADD knock out cells) were treated with TNF-α (1 nM) for indicated time intervals. The number of cells with mitochondrial damage in early phase (A) and late phase (B) was determined by scoring 250 cells from 30 different microscopic fields in the electron microscope. The diagram shows the number of pathologically altered cells. Columns, mean from three different experiments; bars, SD. *p < 0.05; **p < 0.01, Student's t test.
Mitochondrial changes require the presence of FADD
TNFR1 binds to TRADD which then recruits FADD (18), but whether FADD is needed for TNF-α-induced mitochondrial changes is not known. We used FADD gene-deleted Jurkat cells to determine its role in TNF-α induced mitochondrial changes. TNF-α induced mitochondrial changes in the control cells in a time-dependent manner but no mitochondrial change was observed in FADD-deleted cells, even when treated for 48 h (Fig. 4). Thus, the presence of the FADD gene was essential for the effect of TNF-α on mitochondria.
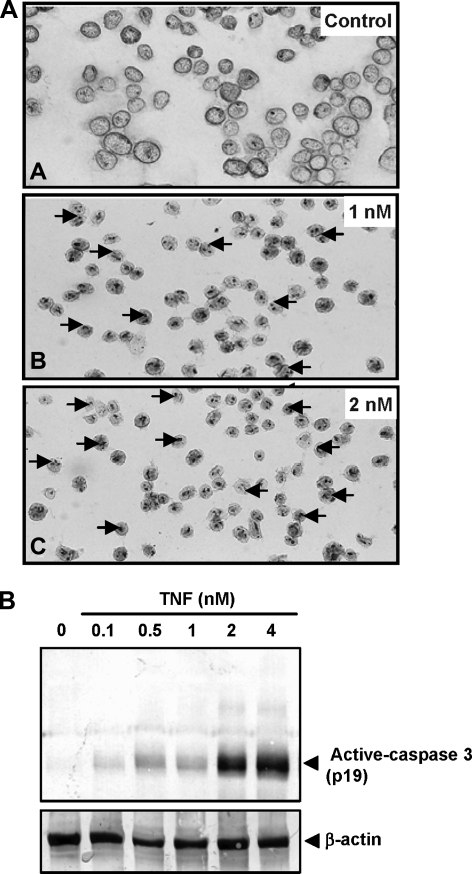
TNF-α-induced caspase-3 activation is an early event
Caspase-3 is a downstream protease that has been shown to be needed for TNF-α-induced apoptosis. How early this caspase activated in response to TNF-α, without protein synthesis inhibitors, was examined. Cells untreated or those treated with indicated concentrations of TNF-α for 60 min were labeled with anti-caspase-3 antibodies by APAAP technique. Untreated cells showed no caspase-3 activation (Fig. 5A). Activated caspase-3 was observed in the nuclei of cells in response to TNF-α treatment in a dose-dependent manner.
FIG. 5.
Dose-dependent activation of caspase-3 in TNF-α-treated Jurkat cells. (A) Cells were treated with indicated concentrations of TNF for 1 h and labeled with anti-caspase-3 antibodies by alkaline phosphatase-anti-alkaline-phosphatase (APAAP) technique. Treated cells showed activated caspase-3 in their nuclei in response to TNF-α treatment. Untreated cells revealed no caspase-3 activation (original magnification, X 160). (B) Cells were treated with indicated concentrations of TNF-α for 1 h and cell lysates were investigated for activated caspase-3 using anti-caspase-3 antibodies by Western blot analysis.
Caspase-3 activation examined by Western blot analysis using anti-active caspase-3 antibodies also indicated a dose-dependent increase (Fig. 5B).
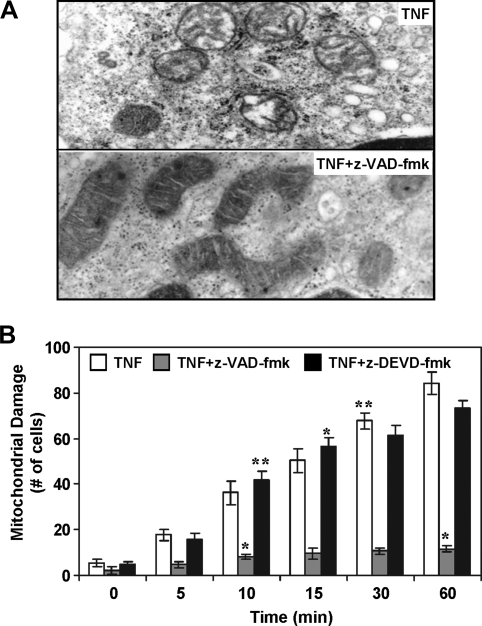
Caspase inhibitor z-VAD-fmk prevents mitochondrial damage and apoptosis in Jurkat cells
So far our results have indicated that TNF-α induces mitochondrial damage and activates caspases. Whether caspase activation is needed for mitochondrial damage induced by TNF-α was investigated by using broad-spectrum caspase inhibitor z-VAD-fmk. Cells were either left untreated or pre-incubated with the inhibitor for 1 h, and then treated with TNF-α. Changes of mitochondria (swelling and dilatation) were observed in TNF-α-treated cells (Fig. 6A, upper panel) but these changes were totally blocked in the presence of z-VAD-fmk in Jurkat cells (Fig. 6A, lower panel). z-VAD-fmk alone did not induce any pathological features in Jurkat cells (data not shown).
FIG. 6.
Effect of the caspase inhibitor on TNF-α-treated Jurkat cells. (A) Cells were either left untreated or pre-incubated with z-VAD-fmk (50 μM) for 1 h. Thereafter the cells were treated with TNF-α (1nM) for 1 h and observed under transmission electron microscopy for mitochondrial change (original magnification, X 50,000). (B) Cells were either left untreated or pre-incubated with either the z-VAD-fmk (50 μM) or z-DVED-fmk (50 μM) for 1 h before incubation with TNF-α (1nM) for 1h. The number of cells with mitochondrial changes was determined in the electron microscope by scoring 100 cells from 20 different microscopic fields. The figure shows the number of pathologically altered cells. Columns, mean from three different experiments; bars, SD. *p < 0.05; **p < 0.01, Student's t test.
The number of cells with TNF-α-induced mitochondrial damage of z-VAD-fmk was determined by scoring 100 cells from 20 different microscopic fields; the number of damaged was found to be time-dependent (Fig. 6B). In contrast, caspase-3 inhibitor had no effect on mitochondrial change (Fig. 6B).
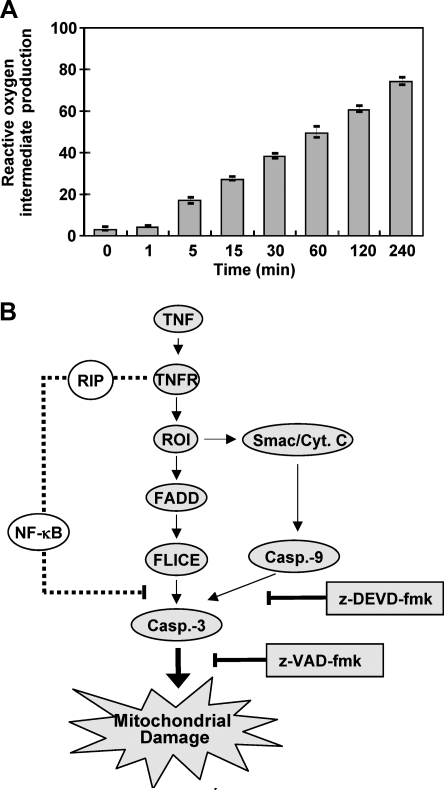
TNF-α-treated cells release reactive oxygen intermediates in a time-dependent manner
Mitochondrial changes have been linked with the release of reactive oxygen intermediates (ROI). Whether TNF-α-induces release of ROI under these conditions was examined. As measured by the flow cytometry method, we found that cells treated with TNF-α produced ROI in a time-dependent manner (Fig. 7A). Production of ROI could be seen as early as 5 min.
FIG. 7.
Release of reactive oxygen intermediates by TNF-α treated cells. (A) Jurkat cells were treated with TNF-α (1 nM) for indicated times. Release of reactive oxygen intermediates (ROI) was measured for the time intervals as indicated by the flow cytometry method. Columns, mean from three different experiments; bars, SD. *p < 0.05; **p < 0.01, Student's t test. (B) A working model for the TNF-α-induced early changes in mitochondrial morphology leading to apoptosis in Jurkat cells.
Discussion
Although TNF-α was discovered more than 2 decades ago, the mechanism by which TNF-α induces proliferation, survival, and apoptosis is still incompletely understood. Further, even though almost all eukaryotic cells are known to express type I TNF receptors with the death domain, not all cells are sensitive to TNF-α-induced growth-modulatory effects. Why some cells are sensitive while others are resistant to TNF is less clear. TNF-α can activate NF-κB, which mediates cell survival role (5, 29, 43). In most cell types, TNF would activate NF-κB and this may mediate survival role in some cells but not others. Thus, TNF-α can activate simultaneously both survival and apoptotic signals and the balance between the two determines the ultimate response of the cell to TNF-α (1).
That mitochondria play a critical role in TNF-α-induced apoptosis has been documented (11). Whether mitochondria have any role in TNF-α-induced survival or proliferation of cells, however, is not understood. The goal of the current study was to investigate the temporal sequence of events that relate to TNF-α-induced mitochondrial changes in the absence of protein synthesis inhibitors. We found that TNF-α induced plasma membrane phosphotidylserine accumulation, DNA strand breaks, and caspase-3 activation, but these events were late and occurred minimally even after 24 h of TNF-α treatment of Jurkat cells. The earliest change observed after treatment of cells with TNF-α was ROI production at 5 min, mitochondrial swelling at 10 min, cytochrome c and Smac release at 30 min, and heterochromatin clumping at 60 min (Fig. 7B). The deletion of RIP had no effect on TNF-α-induced mitochondrial damage; but deletion of FADD abolished the TNF-α-mitochondrial swelling. FADD is needed for the activation of caspase -8. The latter was a critical event, as its inhibition abolished the TNF-α-induced mitochondrial changes, whereas inhibition of caspase-3 had no effect.
Our results clearly show that the activation of the executioner caspase-8 by TNF-α is needed for changes in the mitochondria. However, no caspase-3 activation as monitored by PARP cleavage could be detected until late. It is possible that activation of caspase-8 mediates mitochondrial changes. Smac, a protein that is released from the mitochondria when cells undergo apoptosis, reverses the inhibition of caspase-8 activation induced by IAP-1, IAP-2, and XIAP (33). Thus, it is possible that mitochondrial changes are early events in TNF-α-induced apoptosis that are initiated by the release of Smac and the activation of caspase-8, which in turn leads to further alterations in mitochondria. Indeed, the results of this study show clearly the presence of Smac in the cytosolic fraction after 10 min with TNF-α treatment.
Our results also indicate that FADD, which interacts with TNFR1 through TRADD, is needed for TNF-α-induced mitochondrial damage. FADD is known to interact with caspase-8, which can mediate mitochondrial changes. Whether superoxide generation, mitochondrial membrane potential, or change in ATP levels are involved in TNF-induced mitochondrial damage, is not clear at present. Since TNF induces ROS production, it is possible that ROS is involved in mitochondrial swelling.
Our results also indicate that RIP is not needed for TNF-α-induced mitochondrial damage. In fact, mitochondrial changes were enhanced by deletion of RIP. RIP contains a kinase domain and a death domain. Through the death domain, RIP interacts with TNFR1. The role of RIP in TNF-α-induced NF-κB activation is well established (22, 42) and thus NF-κB activation may play the pro-survival signal (44). Our results are consistent with this hypothesis. The kinase domain of RIP (RIPK1), although not needed for NF-κB activation (22, 42), has been linked with activation of caspase-8, thus leading to apoptosis (33). Our results are consistent with these studies. Thus the role of RIP, Smac, IAP-1, IAP-2, and XIAP; and their sequential involvement in activation of NF-κB and apoptosis is highly complex.
We also observed that TNF-α induced cytochrome c and Smac release, even in the absence of protein synthesis inhibitors. Surprisingly, this TNF-α-induced cytochrome c and Smac release was unaffected by inhibition of caspase-3 but was prevented by inhibition of caspase-8. The caspase inhibitor z-VAD-fmk used in the present study inhibits the apoptosis-inducing factor (AIF), which is responsible for caspase activation (16), but also partly blocks the insertion of Bax a pro-apoptotic protein of the Bcl-2 superfamily in the outer mitochondrial membrane (14). Bax and Bak induce mitochondrial changes such as cytochrome c and Smac release and loss of transmembrane electric potential in mitochondria (12, 46). Mitochondrial cytochrome c release has been shown to be directly regulated by caspase-8 activation. Caspase-8 and −3 cleave the pro-apoptotic Bid protein that belongs also to the Bcl-2 superfamily, and the cleavage product of Bid promotes cytochrome c release from mitochondria (6). Furthermore, cytochrome c release leads to caspase activation.
Beside caspase-3 activation, Jurkat cells showed production of ROI in a time-dependent manner. ROI production is an early feature of apoptosis. Mitochondria are the major source of cellular ROI involved in TNF-α-induced apoptosis. TNF has been reported to alter the cellular redox state, reduce the expression of four complex I subunits by increasing mitochondrial superoxide production, depleting ATP synthesis, thereby resulting in mitochondrial damage (28). These results are consistent with ours showing that treatment of cells with TNF-α induces mitochondrial swelling that may lead to cytochrome c and Smac release. Overall, our results demonstrate that mitochondrial changes are early events in TNF-α-induced apoptosis and require FADD and caspase-8 activation, but not RIP (Fig 7B).
Abbreviations Used
- AIF
apoptosis-inducing factor
- FADD
Fas-associated death domain protein
- FLICE
FADD-like interleukin-1β-converting enzyme
- IAP
inhibitor-of-apoptosis protein
- NF-κB
nuclear factor-kappa B
- PARP
poly (ADP-ribose) polymerase;
- RIP
receptor-interacting protein
- ROI
reactive oxygen intermediate
- TNF-α
tumor necrosis factor alpha
- TNFR1
TNF receptor type 1
- TRADD
TNFR1-associated death domain
- TRAF2
TNFR-associated factor 2
- XIAP
X-linked IAP
Acknowledgments
The authors are grateful to Ms. Karoline Fischer and Ms. Ursula Schwikowski for their excellent technical assistance. Dr. Aggarwal is the Ransom Horne, Jr., Professor of Cancer Research. This work was supported by a grant from the Clayton Foundation for Research (BBA), a core grant from the National Institutes of Health (CA-16 672), a program project grant from National Institutes of Health (NIH CA-124787-01A2), and grant from Center for Targeted Therapy of M.D. Anderson Cancer Center.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Aggarwal BB. Signalling pathways of the TNF superfamily: A double-edged sword. Nat Rev Immunol. 2003;3:745–756. doi: 10.1038/nri1184. [DOI] [PubMed] [Google Scholar]
- 2.Aggarwal BB. Eessalu TE. Hass PE. Characterization of receptors for human tumour necrosis factor and their regulation by gamma-interferon. Nature. 1985;318:665–667. doi: 10.1038/318665a0. [DOI] [PubMed] [Google Scholar]
- 3.Aggarwal BB. Moffat B. Harkins RN. Human lymphotoxin. Production by a lymphoblastoid cell line, purification, and initial characterization. J Biol Chem. 1984;259:686–691. [PubMed] [Google Scholar]
- 4.Aggarwal BB. Schwarz L. Hogan ME. Rando RF. Triple helix-forming oligodeoxyribonucleotides targeted to the human tumor necrosis factor (TNF) gene inhibit TNF production and block the TNF-dependent growth of human glioblastoma tumor cells. Cancer Res. 1996;56:5156–5164. [PubMed] [Google Scholar]
- 5.Beg AA. Baltimore D. An essential role for NF-kappaB in preventing TNF-alpha-induced cell death. Science. 1996;274:782–784. doi: 10.1126/science.274.5288.782. [DOI] [PubMed] [Google Scholar]
- 6.Bossy–Wetzel E. Green DR. Caspases induce cytochrome c release from mitochondria by activating cytosolic factors. J Biol Chem. 1999;274:17484–17490. doi: 10.1074/jbc.274.25.17484. [DOI] [PubMed] [Google Scholar]
- 7.Busquets S. Aranda X. Ribas–Carbo M. Azcon–Bieto J. Lopez–Soriano FJ. Argiles JM. Tumour necrosis factor-alpha uncouples respiration in isolated rat mitochondria. Cytokine. 2003;22:1–4. doi: 10.1016/s1043-4666(03)00098-x. [DOI] [PubMed] [Google Scholar]
- 8.Chen C. Edelstein LC. Gelinas C. The Rel/NF-kappaB family directly activates expression of the apoptosis inhibitor Bcl-x(L) Mol Cell Biol. 2000;20:2687–2695. doi: 10.1128/mcb.20.8.2687-2695.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu ZL. McKinsey TA. Liu L. Gentry JJ. Malim MH. Ballard DW. Suppression of tumor necrosis factor-induced cell death by inhibitor of apoptosis c-IAP2 is under NF-kappaB control. Proc Natl Acad Sci USA. 1997;94:10057–10062. doi: 10.1073/pnas.94.19.10057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clohessy JG. Zhuang J. de Boer J. Gil–Gomez G. Brady HJ. Mcl-1 interacts with truncated Bid and inhibits its induction of cytochrome c release and its role in receptor-mediated apoptosis. J Biol Chem. 2006;281:5750–5759. doi: 10.1074/jbc.M505688200. [DOI] [PubMed] [Google Scholar]
- 11.Cossarizza A. Franceschi C. Monti D. Salvioli S. Bellesia E. Rivabene R. Biondo L. Rainaldi G. Tinari A. Malorni W. Protective effect of N-acetylcysteine in tumor necrosis factor-alpha-induced apoptosis in U937 cells: The role of mitochondria. Exp Cell Res. 1995;220:232–240. doi: 10.1006/excr.1995.1311. [DOI] [PubMed] [Google Scholar]
- 12.Du C. Fang M. Li Y. Li L. Wang X. Smac, a mitochondrial protein that promotes cytochrome c-dependent caspase activation by eliminating IAP inhibition. Cell. 2000;102:33–42. doi: 10.1016/s0092-8674(00)00008-8. [DOI] [PubMed] [Google Scholar]
- 13.Gao W. Pu Y. Luo KQ. Chang DC. Temporal relationship between cytochrome c release and mitochondrial swelling during UV-induced apoptosis in living HeLa cells. J Cell Sci. 2001;114:2855–2862. doi: 10.1242/jcs.114.15.2855. [DOI] [PubMed] [Google Scholar]
- 14.Goping IS. Gross A. Lavoie JN. Nguyen M. Jemmerson R. Roth K. Korsmeyer SJ. Shore GC. Regulated targeting of BAX to mitochondria. J Cell Biol. 1998;143:207–215. doi: 10.1083/jcb.143.1.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gottlieb E. Vander Heiden MG. Thompson CB. Bcl-x(L) prevents the initial decrease in mitochondrial membrane potential and subsequent reactive oxygen species production during tumor necrosis factor alpha-induced apoptosis. Mol Cell Biol. 2000;20:5680–5689. doi: 10.1128/mcb.20.15.5680-5689.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Green DR. Reed JC. Mitochondria and apoptosis. Science. 1998;281:1309–1312. doi: 10.1126/science.281.5381.1309. [DOI] [PubMed] [Google Scholar]
- 17.Hansen JM. Zhang H. Jones DP. Mitochondrial thioredoxin-2 has a key role in determining tumor necrosis factor-alpha-induced reactive oxygen species generation, NF-kappaB activation, and apoptosis. Toxicol Sci. 2006;91:643–650. doi: 10.1093/toxsci/kfj175. [DOI] [PubMed] [Google Scholar]
- 18.Hsu H. Huang J. Shu HB. Baichwal V. Goeddel DV. TNF-dependent recruitment of the protein kinase RIP to the TNF receptor-1 signaling complex. Immunity. 1996;4:387–396. doi: 10.1016/s1074-7613(00)80252-6. [DOI] [PubMed] [Google Scholar]
- 19.Hughes G. Murphy MP. Ledgerwood EC. Mitochondrial reactive oxygen species regulate the temporal activation of nuclear factor kappaB to modulate tumour necrosis factor-induced apoptosis: Evidence from mitochondria-targeted antioxidants. Biochem J. 2005;389:83–89. doi: 10.1042/BJ20050078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jackson–Bernitsas DG. Ichikawa H. Takada Y. Myers JN. Lin XL. Darnay BG. Chaturvedi MM. Aggarwal BB. Evidence that TNF-TNFR1-TRADD-TRAF2-RIP-TAK1-IKK pathway mediates constitutive NF-kappaB activation and proliferation in human head and neck squamous cell carcinoma. Oncogene. 2007;26:1385–1397. doi: 10.1038/sj.onc.1209945. [DOI] [PubMed] [Google Scholar]
- 21.Jia L. Dourmashkin RR. Newland AC. Kelsey SM. Mitochondrial ultracondensation, but not swelling, is involved in TNF alpha-induced apoptosis in human T-lymphoblastic leukaemic cells. Leuk Res. 1997;21:973–983. doi: 10.1016/s0145-2126(97)00078-7. [DOI] [PubMed] [Google Scholar]
- 22.Kelliher MA. Grimm S. Ishida Y. Kuo F. Stanger BZ. Leder P. The death domain kinase RIP mediates the TNF-induced NF-kappaB signal. Immunity. 1998;8:297–303. doi: 10.1016/s1074-7613(00)80535-x. [DOI] [PubMed] [Google Scholar]
- 23.Kreuz S. Siegmund D. Scheurich P. Wajant H. NF-kappaB inducers upregulate cFLIP, a cycloheximide-sensitive inhibitor of death receptor signaling. Mol Cell Biol. 2001;21:3964–3973. doi: 10.1128/MCB.21.12.3964-3973.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ledgerwood EC. Prins JB. Bright NA. Johnson DR. Wolfreys K. Pober JS. O'Rahilly S. Bradley JR. Tumor necrosis factor is delivered to mitochondria where a tumor necrosis factor-binding protein is localized. Lab Invest. 1998;78:1583–1589. [PubMed] [Google Scholar]
- 25.Liu H. Ma Y. Pagliari LJ. Perlman H. Yu C. Lin A. Pope RM. TNF-alpha-induced apoptosis of macrophages following inhibition of NF-kappa B: A central role for disruption of mitochondria. J Immunol. 2004;172:1907–1915. doi: 10.4049/jimmunol.172.3.1907. [DOI] [PubMed] [Google Scholar]
- 26.Maianski NA. Roos D. Kuijpers TW. Tumor necrosis factor alpha induces a caspase-independent death pathway in human neutrophils. Blood. 2003;101:1987–1995. doi: 10.1182/blood-2002-02-0522. [DOI] [PubMed] [Google Scholar]
- 27.Manna SK. Zhang HJ. Yan T. Oberley LW. Aggarwal BB. Overexpression of manganese superoxide dismutase suppresses tumor necrosis factor-induced apoptosis and activation of nuclear transcription factor-kappaB and activated protein-1. J Biol Chem. 1998;273:13245–13254. doi: 10.1074/jbc.273.21.13245. [DOI] [PubMed] [Google Scholar]
- 28.Mariappan N. Elks CM. Fink B. Francis J. TNF-induced mitochondrial damage: a link between mitochondrial complex I activity and left ventricular dysfunction. Free Radic Biol Med. 2009;46:462–470. doi: 10.1016/j.freeradbiomed.2008.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mayo MW. Wang CY. Cogswell PC. Rogers–Graham KS. Lowe SW. Der CJ. Baldwin AS., Jr Requirement of NF-kappaB activation to suppress p53-independent apoptosis induced by oncogenic Ras. Science. 1997;278:1812–1815. doi: 10.1126/science.278.5344.1812. [DOI] [PubMed] [Google Scholar]
- 30.Munker R. Greither L. Darsow M. Ellwart JW. Mailhammer R. Wilmanns W. Effects of tumor necrosis-factor on primary human leukemia cells: Ultrastructural changes. Acta Haematol. 1993;90:77–83. doi: 10.1159/000204380. [DOI] [PubMed] [Google Scholar]
- 31.Pennica D. Nedwin GE. Hayflick JS. Seeburg PH. Derynck R. Palladino MA. Kohr WJ. Aggarwal BB. Goeddel DV. Human tumour necrosis factor: Precursor structure, expression and homology to lymphotoxin. Nature. 1984;312:724–729. doi: 10.1038/312724a0. [DOI] [PubMed] [Google Scholar]
- 32.Pessayre D. Fromenty B. Mansouri A. Mitochondrial injury in steatohepatitis. Eur J Gastroenterol Hepatol. 2004;16:1095–1105. doi: 10.1097/00042737-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Petersen SL. Wang L. Yalcin–Chin A. Li L. Peyton M. Minna J. Harran P. Wang X. Autocrine TNFalpha signaling renders human cancer cells susceptible to Smac-mimetic-induced apoptosis. Cancer Cell. 2007;12:445–456. doi: 10.1016/j.ccr.2007.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prins JB. Ledgerwood EC. Ameloot P. Vandenabeele P. Faraco PR. Bright NA. O'Rahilly S. Bradley JR. Tumor necrosis factor-induced cytotoxicity is not related to rates of mitochondrial morphological abnormalities or autophagy-changes that can be mediated by TNFR-I or TNFR-II. Biosci Rep. 1998;18:329–340. doi: 10.1023/a:1020261316486. [DOI] [PubMed] [Google Scholar]
- 35.Schulze-Osthoff K. Bakker AC. Vanhaesebroeck B. Beyaert R. Jacob WA. Fiers W. Cytotoxic activity of tumor necrosis factor is mediated by early damage of mitochondrial functions. Evidence for the involvement of mitochondrial radical generation. J Biol Chem. 1992;267:5317–5323. [PubMed] [Google Scholar]
- 36.Shakibaei M. Zimmermann B. Merker HJ. Changes in integrin expression during chondrogenesis in vitro: An immunomorphological study. J Histochem Cytochem. 1995;43:1061–1069. doi: 10.1177/43.10.7560884. [DOI] [PubMed] [Google Scholar]
- 37.Shi Y. A structural view of mitochondria-mediated apoptosis. Nat Struct Biol. 2001;8:394–401. doi: 10.1038/87548. [DOI] [PubMed] [Google Scholar]
- 38.Shishodia S. Amin HM. Lai R. Aggarwal BB. Curcumin (diferuloylmethane) inhibits constitutive NF-kappaB activation, induces G1/S arrest, suppresses proliferation, and induces apoptosis in mantle cell lymphoma. Biochem Pharmacol. 2005;70:700–713. doi: 10.1016/j.bcp.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 39.Stehlik C. de Martin R. Kumabashiri I. Schmid JA. Binder BR. Lipp J. Nuclear factor (NF)-kappaB-regulated X-chromosome-linked iap gene expression protects endothelial cells from tumor necrosis factor alpha-induced apoptosis. J Exp Med. 1998;188:211–216. doi: 10.1084/jem.188.1.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sugarman BJ. Aggarwal BB. Hass PE. Figari IS. Palladino MA., Jr. Shepard HM. Recombinant human tumor necrosis factor-alpha: Effects on proliferation of normal and transformed cells in vitro. Science. 1985;230:943–945. doi: 10.1126/science.3933111. [DOI] [PubMed] [Google Scholar]
- 41.Thakar J. Schleinkofer K. Borner C. Dandekar T. RIP death domain structural interactions implicated in TNF-mediated proliferation and survival. Proteins. 2006;63:413–423. doi: 10.1002/prot.20895. [DOI] [PubMed] [Google Scholar]
- 42.Ting AT. Pimentel-Muinos FX. Seed B. RIP mediates tumor necrosis factor receptor 1 activation of NF-kappaB but not Fas/APO-1-initiated apoptosis. EMBO J. 1996;15:6189–6196. [PMC free article] [PubMed] [Google Scholar]
- 43.Van Antwerp DJ. Martin SJ. Kafri T. Green DR. Verma IM. Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science. 1996;274:787–789. doi: 10.1126/science.274.5288.787. [DOI] [PubMed] [Google Scholar]
- 44.Wang CY. Mayo MW. Korneluk RG. Goeddel DV. Baldwin AS., Jr. NF-kappaB antiapoptosis: Induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science. 1998;281:1680–1683. doi: 10.1126/science.281.5383.1680. [DOI] [PubMed] [Google Scholar]
- 45.Wilson CA. Browning JL. Death of HT29 adenocarcinoma cells induced by TNF family receptor activation is caspase-independent and displays features of both apoptosis and necrosis. Cell Death Differ. 2002;9:1321–1333. doi: 10.1038/sj.cdd.4401107. [DOI] [PubMed] [Google Scholar]
- 46.Zhai D. Huang X. Han X. Yang F. Characterization of tBid-induced cytochrome c release from mitochondria and liposomes. FEBS Lett. 2000;472:293–296. doi: 10.1016/s0014-5793(00)01471-x. [DOI] [PubMed] [Google Scholar]