Abstract
Objective
To investigate the degree of CHD awareness as well as symptom, risk factor, and treatment knowledge in a broad sample of cardiac inpatients, and to examine its sociodemographic, clinical and psychosocial correlates.
Methods
1308 CHD inpatients (351 [27.0%] female), recruited from 11 acute care sites in Ontario, participated in this cross-sectional study. Participants were provided with a survey which included a knowledge questionnaire among other measures, and clinical data were extracted from medical charts.
Results
855 (68.8%) respondents cited heart disease as the leading cause of death in men, versus only 458 (37.0%) in women. Participants with less than high school education (p<.001), an annual family income less than $50,000CAD (p=.022), low functional capacity (p=.042), who were currently smoking (p=.022), who had no family history of heart disease (p<.001), and who had a perception of low personal control (p=.033) had significantly lower CHD knowledge.
Conclusions
Awareness of CHD is not optimal, especially among women, South Asians, and those of low socioeconomic status. CHD patients have a moderate level of disease knowledge overall, but greater education is needed.
Practice implications
Tailored educational approaches may be necessary for those of low socioeconomic status, particularly with regard to the nature of CHD, tests and treatments.
Keywords: patient knowledge, awareness, heart disease
1. Introduction
Coronary heart disease (CHD) is the leading cause of morbidity and mortality worldwide, accounting for over one-quarter of all deaths in 2001 [1]. Although rates of CHD mortality are declining overall due to early detection strategies, advanced medical treatment, and risk factor reductions [2], this decline is not evident for certain subgroups such as women and those of low socioeconomic status (SES) [3–5]. Significant inequalities exist for these subgroups with respect to their risk factor prevalence, later diagnosis, access to evidence-based therapies, and treatment outcomes. Moreover, it is unknown whether these vulnerable subgroups are less knowledgeable about their disease, which may provide some explanation for their poorer morbidity and mortality outcomes.
Patients’ knowledge about their disease can be comprised of their awareness about the general pathophysiology, risk factors, symptoms, prevention, and treatment associated with their condition. Knowledge of heart disease can strongly influence symptom recognition, advocacy for physician screening, attitudes towards the disease, and provide motivation for individual behaviour changes [6–8]. Likewise, inadequate understanding of the disease may cause unwarranted emotional distress, inappropriate coping behaviour, non-compliance with medical advice, and unnecessary disease progression [9]. For instance, studies have shown significant relationships between general knowledge about CHD risk factors and compliance to lifestyle changes such as weight management, diet, physical activity, attainment of lipid level goals, and medication compliance among CVD patients [10, 11]. As well, illness perceptions and beliefs regarding the causes, symptoms, and treatment of CHD are often influenced by one’s knowledge of the disease. For instance, one study found that misconceived beliefs about angina, such as believing that the cure for angina is rest, were associated with reductions in functional and psychological status [12]. Illness perceptions can also influence one’s willingness to utilize secondary prevention services [13, 14] or to make necessary lifestyle changes following a cardiac event [15, 16]. While knowledge does not necessarily translate into appropriate risk reduction behaviors in the general population or even in patients themselves, a lack of knowledge and awareness regarding one’s disease can hinder possible lifestyle modifications and ultimately cardiac health. Clearly, it is essential to evaluate the level of CHD knowledge among patients with this disease.
Although literature exists on the degree of CHD knowledge and awareness in the general population, there is minimal research examining the level of knowledge among cardiac patients themselves [17–22]. Sociodemographic factors such as female sex, younger age, higher income, greater education, and mainstream ethnocultural background have been found to be significantly related to greater CHD knowledge in the general population [7, 23–26] and in CHD patients [17, 19, 20]. A recent study also found that women who were aware that heart disease was the leading cause of death for women were more likely to increase physical activity and lose weight [27]. This finding is corroborated by previous studies reporting that those who engaged in regular physical activity and who were non-smokers were more knowledgeable about the modifiable risk factors for heart disease [7, 17]. It is also possible that disease severity, or undergoing cardiac procedures such as acute coronary bypass, can influence CHD knowledge, perceived personal risk and disease management behaviors. For example, those who have undergone a percutaneous coronary intervention (PCI) may be less likely to make lifestyle modifications because they feel “cured” from the relatively unintrusive intervention [28], putting them at a higher risk of further CHD progression. However, there are inconsistent findings regarding the degree and correlates of knowledge [17, 19, 20, 29].
The objective of this study was to investigate the degree of CHD knowledge among coronary artery disease (CAD) inpatients with respect to basic pathophysiology, risk factors, symptoms, and treatment, as well as awareness of the leading cause of death. The sociodemographic (e.g., sex, SES, ethnicity) and clinical (e.g., risk factors) correlates of this knowledge were examined to facilitate identification of sociodemographic groups with less knowledge, and to assess the association between knowledge and risk factor status. Considering that knowledge is related to patients’ beliefs and perceptions about their disease, psychosocial correlates (i.e., illness perceptions) were also examined. No study has yet examined such a complete list of knowledge correlates, and very few have assessed level of knowledge in a cardiac inpatient population. Hence, little is known about disease knowledge in this population, and how such knowledge relates to illness perceptions and risk factor status.
2. Methods
2.1. Design and Procedure
This study represents a cross-sectional quantitative component of a larger prospective study (CRCARE [30]). Ethics approval was obtained from all participating institutions, which included 11 acute care hospitals in Ontario, Canada. Consecutive coronary artery disease (CAD) inpatients from each of the sites were approached for informed consent by a site recruiter when medically stable. Medical chart data was extracted, including nature of cardiac event or procedure, comorbid conditions, and risk factors. Patients were then provided with the self-report survey to complete.
2.2. Participants
One thousand three hundred and eight consecutive consenting CAD in-patients (N=351, 27.0% female; 66.0% response rate) were recruited from 11 acute care sites in Ontario. Participating patient characteristics are shown in Table 1. Their age ranged from 34 to 96.
Table 1.
Descriptive characteristics of study sample (N=1308)
| Characteristic | Mean ± SD/n (%)a |
|---|---|
| Sex (% female) | 351 (27.0) |
| Age (mean ± SD) | 65.20 ± 11.07 |
| Education (% <high school) | 323 (26.1) |
| Family income (% <$50,000CAD) | 525 (51.4) |
| Subjective SES (% low SES) | 520 (46.4) |
| Marital status (%married/common law) | 938 (73.5) |
| Ethnocultural background (% white) | 1023 (85.3) |
| Ethnocultural background (% South Asian) | 77 (6.0) |
| Work status (% full-time/part-time) | 443 (36.6) |
| Body Mass Index (mean ± SD) | 29.03 ± 5.59 |
| Previous cardiac event† (%yes) | 667 (56.4) |
| Smoking status† (%current) | 95 (7.8) |
| Current Myocardial Infarction† (%) | 378 (29.4) |
| Current Unstable Angina† (%) | 213 (16.6) |
| Current Percutaneous Coronary Intervention† (%) | 371 (28.8) |
| Current Acute Coronay Bypass† (%) | 552 (43.0) |
| Family history of heart disease (%yes) | 862 (72.0) |
| Duke Activity Status Index (mean ± SD) | 25.59 ± 16.61 |
| Hypertension (%yes) | 708 (58.4) |
| Systolic blood pressure mm Hg† (mean ± SD) | 128.05 ± 20.35 |
| Diastolic blood pressure mm Hg† (mean ± SD) | 70.91 ± 11.96 |
| Dyslipidemia (%yes) | 709 (59.7) |
| Total Cholesterol/HDL Ratio† | 4.41 ± 2.27 |
| HDLb mmol/L† (mean ± SD) | 1.04 ± .37 |
| LDLc mmol/L† (mean ± SD) | 2.45 ± 1.06 |
| Diabetes (%yes) | 393 (31.2) |
| NYHAd Class II-IV † (%) | 95 (32.9) |
| CCSe angina class 2–4 † (%) | 357 (85.8) |
Percentages take into account missing data for some variables.
HDL, high-density lipoprotein.
LDL, low-density lipoprotein.
NYHA, New York Heart Association.
CCS, Canadian Cardiovascular Society.
denotes medical chart data.
CAD diagnosis was confirmed based on indication in patient chart of detailed history, focused physical examination, diagnostic ECG changes (i.e., Q waves, and/or ST-T segment changes), and/or troponin levels above the 99th percentile of normal. Inclusion criteria for the larger trial included confirmed acute coronary syndrome diagnosis or revascularization procedure, eligibility for cardiac rehabilitation based on guidelines [31], and proficiency in English, French, Punjabi, Urdu, or Hindi. Exclusion criteria for the larger study included patients who had life-threatening comorbidities. Participants were more likely to be male, younger, and have at least high school education than non-participants (all ps <.05).
2.3. Measures
2.3.1. Dependent Variable
Since no robust knowledge questionnaire validated in cardiac samples is available, items from existing knowledge questionnaires and investigator-generated questions were integrated to assess CHD knowledge relating to risk factors, symptoms and treatment (see Appendix A – attach knowledge questionnaire).
The first item of the knowledge scale was an investigator-generated question with forced-choice response options assessing respondents’ understanding of the basic pathophysiology of CHD. Two close-ended questions followed assessing awareness of the leading cause of death for both men and women, which paralleled Mosca et al.’s recent national study [27]. Next were a set of twenty true or false questions assessing general knowledge of CHD, including its causes, risk factors, symptoms, and treatment. Eleven of these questions were based on items in the Cardiac Knowledge Questionnaire [32] (Cronbach’s α ranged from 0.69 to 0.86) and the Coronary Heart Disease Knowledge Test [33] (α = 0.84). The remaining nine true or false questions were investigator-generated. An overall knowledge score was computed by totaling the number of correct responses, with a possible range from 0–23, and higher scores indicating greater knowledge.
2.3.2. Sociodemographic Correlates of Knowledge
Self-reported sociodemographic characteristics assessed through forced-choice options included a patient’s ethnocultural background (open and closed-ended), family income, education level, and work status. Subjective SES was assessed using the social status ladder included in the survey, where participants indicate how they would rank their SES relative to others in Canada [34]. Date of birth and sex were obtained from the medical chart.
2.3.3. Clinical Correlates
Cardiac condition and body mass index (BMI; kg/m2) was extracted from patients’ medical charts. From the self-report survey, CHD risk factors, comorbid conditions, functional capacity, and physical activity behavior were assessed. CHD risk factors included smoking status, family history of CHD, hypertension, and dyslipidemia. Participants reported ‘yes’ or ‘no’ if they suffered from any of a list of 13 comorbid conditions including diabetes, mental/emotional problems and muscle, bone, or joint problems. The total number of comorbidities was computed. Participants also self-reported whether or not they have had a previous cardiac event or procedure.
To assess functional capacity (i.e., disease severity), the Duke Activity Status Index (DASI) [35], a brief 12-item self-report instrument, was included in the survey. Participants were asked about their ability to perform common activities of daily living, such as personal care, ambulation, household tasks, sexual function, and recreational activities, which are each associated with specific metabolic equivalents (METs). This valid and common tool correlates with treadmill functional capacity measured in METs [36] and also correlates highly with peak oxygen uptake [37]. The validity of the scale is demonstrated by such strong correlations with peak oxygen uptake.
The Physical Activity Scale for the Elderly (PASE) [38] was also incorporated in the self-report survey to assess physical activity behaviour. The total PASE score was computed by multiplying the amount of time spent in activities of various intensities (hr/week) by item weights and summing over all activities. Higher PASE scores indicate greater physical activity. The PASE has been shown to be highly correlated (r=.58) with energy expenditure using the doubly labelled water method [38].
2.3.4. Psychosocial Correlates
The Illness Perception Questionnaire (IPQ-R [39]) was administered to assess cognitive representations of CHD. Four subscales from the IPQ-R were included in the survey: time course (acute/chronic), perceived personal control, consequences, and treatment cure/controllability. All items are scored on a 5-point Likert-type scale which ranged from ‘strongly disagree’ to ‘strongly agree’. Mean subscale scores were computed, with higher scores denoting greater endorsement of the given construct. Cronbach’s alpha for the subscales were .89, .81, .84, and .80, respectively. The validity and reliability of this questionnaire have also been demonstrated and are quite encouraging [40].
2.4. Statistical Analyses
SPSS Version 14.0 [41] was used for all analyses. Sociodemographic variables with more than two response options were dichotomized using a median split where possible. The forced-choice ethnicity variable on the survey was dichotomized to distinguish between white (i.e., North American, French, British Isles, and European descent) and non-white (all other responses) participants. Also, given that South Asians represented the second largest ethnocultural group in this sample (6.0%), and have been identified as a high risk population [42], a dichotomous variable was created comparing South Asians to non-South Asians. Response rate was computed, and differences between participating and non-participating patients were tested by Pearson’s chi-square and analyses of variance as appropriate. Characteristics of participants were described. A descriptive examination of awareness and CHD knowledge was performed.
The composite knowledge score was analyzed by the correlates under study using Pearson’s Correlation, one-way ANOVA, or Student’s t-test as appropriate. A multivariate analysis using linear regression was then conducted to identify which sociodemographic, clinical and psychosocial correlates were independently associated with the CHD knowledge composite score. To minimize multicollinearity, only significant variables in bivariate screening were included in the multivariate model.
3. Results
Eight hundred and fifty-five respondents (68.8%) cited CHD as the leading cause of death for men, versus 458 respondents (37.0%) who cited CHD as the leading cause of death for women. Eighty-seven (26.4%) females believed that breast cancer was their leading cause of death, versus 140 (42.4%) citing CHD. Men were significantly less aware than women of CHD as the leading cause of death for women (p=.029), and similarly women were significantly less aware than men of CHD as the leading cause of death for men (p<.001). South Asian participants were significantly less likely than non-South Asians to identify heart attack as the leading cause of death for men (p=.010) and women (p=.045). White participants were significantly less aware regarding CHD as the leading cause of death for men than non-white participants (p=.018). Those who self-reported low SES were significantly less likely than their high SES counterparts to cite CHD as the leading cause of death for both men (p=.028) and women (p=.034).
3.1 CHD Knowledge among Cardiac Inpatients
The mean composite knowledge score was 16.67 ± 2.59, ranging from 7 to 22. This mean corresponds to an average of approximately 72% correct responses. Over half (54.0%) of respondents correctly identified CHD as reduced blood flow to the heart. The four questions most often answered correctly (true/false) were as follows: daily aspirin is recommended to reduce heart disease risk (98.8% correct), lifestyle changes can reduce chances of dying from heart disease (98.6% correct), a heart attack is caused by blocking blood flow to part of the heart (97.4% correct), and the hardening of arteries begins with accumulation of fat deposits in the arterial wall (97.1% correct). The four questions most often answered incorrectly (true/false) were as follows: nitroglycerine is not of great help in a heart attack (89.7% incorrect), PCI is not used to diagnose CHD (69.2% incorrect), an angiogram cannot improve blood flow through narrow or blocked arteries (37.8% incorrect) and that coronary bypass surgery can improve blood flow through blocked arteries (33.7% incorrect).
3.2 Correlates of Composite Knowledge Score
Bivariate analyses of sociodemographic, clinical and psychosocial correlates of the composite knowledge score are shown in Table 2. Female sex, low subjective SES, white ethnicity, less than high school education, a family income of less than $50,000 CAD, and not engaging in full-time/part-time work were significant sociodemographic correlates of a lower knowledge score. Those who reported greater functional capacity, greater physical activity, not currently smoking, family history of heart disease and no diabetes also had significantly higher knowledge scores. Interestingly, with regard to psychosocial correlates, results revealed a significant correlation between higher knowledge scores and perception of greater negative illness consequences, greater personal control, and perception of CHD as a chronic condition.
Table 2.
Results of bivariate analyses of correlates associated with composite knowledge score, N=1253
| Type of Correlate | Correlate | Mean ± SD/r | p | |
|---|---|---|---|---|
| Sociodemographic | Sex | Female | 16.27 ± 2.71 | .001 |
| Male | 16.82 ± 2.53 | |||
| Subjective SESa | Low SES | 16.50 ± 2.55 | <.001 | |
| High SES | 17.13 ± 2.40 | |||
| White | Yes | 16.82 ± 2.49 | .043 | |
| No | 16.40 ± 2.88 | |||
| South Asian | Yes | 16.61 ± 2.89 | .822 | |
| No | 16.68 ± 2.57 | |||
| Age | −.046 | .107 | ||
| Marital status | Married/Common law | 16.75 ± 2.58 | .057 | |
| Other | 16.43 ± 2.63 | |||
| Education | < High school | 15.80 ± 2.62 | <.001 | |
| ≥ High school | 16.97 ± 2.53 | |||
| Family income | <$50,000 CAD | 16.20 ± 2.64 | <.001 | |
| >= $50,000 CAD | 17.50 ± 2.20 | |||
| Work status | Full-time/part-time | 17.17 ± 2.43 | <.001 | |
| Other | 16.50 ± 2.57 | |||
| Clinical | DASIb | .140 | <.001 | |
| # comorbid conditions | −.032 | .264 | ||
| PASEc | .063 | .040 | ||
| Smoking status | Current | 15.98 ± 2.71 | <.001 | |
| Past | 16.94 ± 2.38 | |||
| Never | 16.52 ± 2.79 | |||
| Hypertension | Yes | 16.69 ± 2.52 | .514 | |
| No | 16.79 ± 2.61 | |||
| Dyslipidemia | Yes | 16.78 ± 2.55 | .846 | |
| No | 16.75 ± 2.53 | |||
| Family history of CHD | Yes | 16.89 ± 2.50 | <.001 | |
| No | 16.25 ± 2.68 | |||
| Previous cardiac event | Yes | 16.80 ± 2.59 | .139 | |
| No | 16.57 ± 2.64 | |||
| BMId | −.009 | .815 | ||
| Cardiac condition† | PCIe | 16.84 ± 2.49 | .161 | |
| Other | 16.61 ± 2.64 | |||
| Diabetes† | Yes | 16.47 ± 2.65 | .046 | |
| No | 16.79 ± 2.55 | |||
| Psychosocial | IPQf –timeline | .127 | <.001 | |
| IPQf –consequences | .105 | <.001 | ||
| IPQf –personal control | .187 | <.001 | ||
| IPQf –treatment control | .050 | .083 | ||
SES, Socioeconomic status.
DASI, Duke Activity Status Index.
PASE, Physical Activity Scale for the Elderly.
BMI, body mass index.
PCI, Percutaneous Coronary Intervention.
IPQ, Illness Perceptions Questionnaire.
Chart reported data
Table 3 displays the results from the multivariate analysis using linear regression represented by the adjusted β coefficients (F=6.52, p<.001). No variables identified through bivariate screening were omitted from the model as multicollinearity was not evident. In this adjusted analysis, less than high school education, less than $50,000CAD family income, lower functional status, smoking, lack of a family history of heart disease, and perception of low personal control were significantly associated with a lower composite knowledge score.
Table 3.
Linear regression analysis of correlates associated with composite knowledge score
| Adjusted β (95% CI) | p value | |
|---|---|---|
| Female sex | −.04 (−.46, .38) | .845 |
| Low Subjective SESa | −.07 (−.44, .31) | .723 |
| White ethnicity | −.04 (−.54, .47) | .883 |
| Less than High School Education | −.85 (−1.28, −.42) | <.001 |
| < $50,000 CAD Family income | −.63 (−1.03, −.24) | .002 |
| Full-time/part-time Work status | .09 (−.29, .47) | .636 |
| DASIb | .01 (.00, .02) | .042 |
| PASEc | .00 (−.003, .002) | .863 |
| Smoking status | ||
| Current Smoker vs. non-smoker | −.83 (−1.54, −.12) | .022 |
| Former Smoker vs. non-smoker | .10 (−.27, .48) | .587 |
| No Family History of CHD | −.68 (−1.06, −.30) | <.001 |
| Diabetes | .02 (−.36, .40) | .917 |
| IPQd – timeline | .03 (−.01, .06) | .161 |
| IPQd - consequences | .03 (−.02, .07) | .203 |
| IPQd – personal control | .06 (.01, .11) | .033 |
SES, Socioeconomic status.
DASI, Duke Activity Status Index.
PASE, Physical Activity Scale for the Elderly.
IPQ, Illness Perceptions Questionnaire.
4. Discussion and conclusion
4.1 Discussion
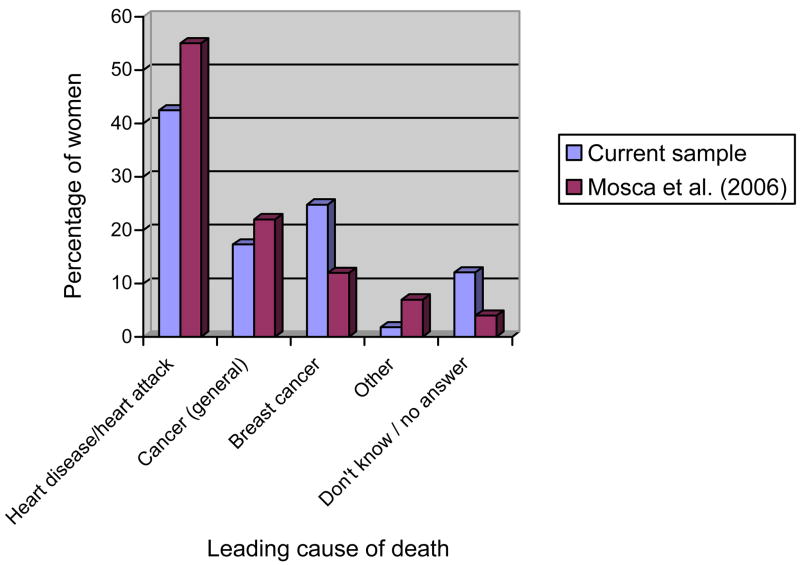
This study investigated awareness and degree of CHD knowledge, including an extensive list of potential correlates of such knowledge, in a broad sample of CHD inpatients. Results showed that even CHD patients themselves continue to perceive CHD as a man’s disease, as demonstrated by the differences in awareness of the leading cause of death for men and women. This is disappointing given that CHD is also the leading cause of mortality in women [43, 44]. In fact, female inpatients in the current study had a lower level of awareness (42.4%) of CHD as women’s leading cause of death than previously reported in a U.S. sample [27] wherein 55% of women from the general population correctly identified women’s leading cause of death. See Figure 1 for a comparison between the current findings (females only shown, Canadian inpatient cardiac sample) and those reported by Mosca et al. (2006) in an American non-patient female population.
Figure 1.
A comparison between current study and Mosca et al.’s study (2006) examining women’s awareness of their leading cause of death.
The South Asian inpatients in this study also demonstrated significantly poorer awareness about CHD as the leading cause of death for both men and women. This is novel, as no other study has assessed sex differences in awareness among the South Asian population to our knowledge. This finding is surprising, given increasing evidence of the greater burden of CHD in the South Asian population [42], particularly among women, [44, 45] and their poorer prognosis [46, 47].
To our knowledge, researchers have not examined SES differences in awareness. This study found that those who self reported low SES were significantly less aware of CHD as the leading cause of death for men and women. These findings may suggest the need for increased public health initiatives among areas of low SES to increase awareness, as low SES is associated with greater CHD morbidity and mortality [48, 49].
4.1.1. Degree of CHD Knowledge
The CAD inpatients in this study demonstrated a moderate level of CHD knowledge. One other Canadian study assessing risk factor knowledge among a small sample (N=71) of cardiac in-patients [19] reported a mean knowledge score of 85% correct, compared to the 72% broader knowledge score in our patient sample. Other studies have suggested a significant lack of CHD knowledge among the general population [50] and in patients themselves [17, 20, 29]. Our results suggest that cardiac inpatients do have general knowledge regarding their condition, but that continued efforts are necessary to fully educate patients, particularly with regard to diagnostic tests, treatment of symptoms and interventional procedures such as PCI and coronary bypass surgery.
4.1.2. Correlates of CHD Knowledge
Although some studies have reported significantly less knowledge among men [19, 23], in the current study there were no sex differences in knowledge after adjusting for covariates. As well, contrary to previous studies which found that South Asians are significantly lacking in CHD knowledge [17, 29, 50], we were unable to find a difference between South Asians and non-South Asians. The lack of a significant effect may have been due to insufficient power considering the small number of South Asian patients in this study, or due to the fact that other studies examined South Asians alone and did not make comparisons to other ethnic groups. Another possible explanation for this could be that the South Asian participants were significantly more likely to have greater than high school education than non South Asians (p<.001). Therefore, the greater level of education seen among the South Asian participants in this study may have contributed to their higher level of CHD knowledge. However, examining the level of knowledge among South Asians is of particular importance given that they are the fastest growing visible minority in Canada [51] and also have one of the highest risks of CHD in the world [17, 52]. Further, we did not find any other significant ethnic differences in CHD knowledge. While we found no sex or ethnic differences in overall CHD knowledge, it is interesting to note that female and South Asian inpatients incorrectly perceive other conditions as the leading cause of death.
This study incorporated several indicators of SES, namely subjective SES, education, income, and work status. Results showed that those with less than high school education and with an annual income of less than $50,000 CAD had significantly lower CHD knowledge. This is consistent with what has been reported in the literature [7, 17, 19, 23, 26, 29], whereby those with advanced education and income were more knowledgeable about CHD. These findings are problematic because low SES is strongly associated with an increased prevalence of CHD risk factors [4, 53, 54] and with greater morbidity and mortality among CHD patients [48, 49, 55, 56]. It is likely that those with less education have inadequate health literacy, as measured by their reading fluency. Baker et al. (2007) found that subjects who were older, non-white, with a lower annual income and lower education level had poor health literacy which resulted in less health knowledge, worse disease management, and lower use of preventive services. Baker et al. also found that inadequate health literacy increased the risk of cardiovascular mortality [57]. Given that the majority of Canadian adults do not have the skills to understand information about their own health or make daily decisions about their health [58], this highlights the urgent need for improvements in health care communication and education to reduce the association between SES and poorer cardiovascular outcomes. Although health literacy itself was not addressed in this current study, future studies should include a measure of this key variable to examine its relationship with CHD knowledge.
As expected, having a family history of heart disease was significantly associated with greater CHD knowledge. It is likely that these individuals have had greater exposure to CHD information and education than those with no family history of the disease. However, having a previous cardiac event was not significantly associated with CHD knowledge. Other studies have failed to report consistent findings regarding this association [19, 24]. Although it is somewhat expected that patients who have had a previous cardiac event would have greater knowledge about their disease, our results may suggest that patients are being provided with insufficient information at the time of their event. However, it may also indicate that health care providers are not doing an adequate job educating patients throughout their continuum of care. Clearly, additional efforts to improve the quantity and quality of patient education are essential.
Contrary to previous studies which found that those with greater CHD knowledge had better risk factor profiles and engaged in physical activity [7, 10, 11, 17], we did not find an association between knowledge and risk factor status, such as increased physical activity, lower blood pressure, lower cholesterol, or lower BMI. However, similar to our findings, Khan et al. (2006) also found that non-smokers had significantly greater CHD knowledge, possibly because they are more aware of the consequences of unhealthy habits and risk factors. In addition, we found that those with greater functional capacity (i.e., less disease severity) had greater CHD knowledge. This is in contrast to a study by Zerwic et al. (1997), which found that angiography patients were more likely to be unsure of the causes of their disease than MI patients. Numerous studies have also found that patients with less disease severity, such as those who undergo a PCI, do not perceive a need to make behavioural changes following their procedure [28, 59, 60]. These patients may feel that the relatively simple and non-invasive procedure ‘fixed’ or ‘cured’ their condition [28]. Knowledge regarding diagnostic tests and interventional procedures can allow patients to clearly understand their condition and will enable them to make educated decisions regarding their health and healthcare. Therefore, adequate and comprehensive patient education, including the nature of tests and procedures, during the rehabilitative phase is essential to ensure that patients are aware of the need for lifelong lifestyle modifications to minimize disease progression and improve quality of life.
This study is novel in approach by also examining illness perceptions and its relation to knowledge. The results demonstrated that more knowledgeable patients feel more in control regarding disease management, symptom recognition and lifestyle modifications, or alternatively that they seek out CHD information to better manage their illness. Identifying specific illness perceptions which may influence the effectiveness of patient education is essential. Future studies should assess the efficacy of interventions which modify patients’ illness perceptions, particularly perceptions of personal control, on CHD knowledge. For instance, education regarding modifiable risk factors for CHD and tools to modify them may promulgate improved perceptions of control. At the same time, the effect of improved CHD knowledge in altering patients’ illness perceptions should also be examined.
4.1.2. Strengths and Limitations
Some major strengths of this study are the large sample size and participation rate, as well as the thorough list of correlates examined. However, caution is warranted when interpreting the results. A key limitation of this study is that knowledge was not measured using a validated questionnaire. Existing questionnaires in the literature have rarely been tested on patients with established heart disease [32, 33, 61–63], and only two of these studies examined the psychometric properties of their instrument [33, 62]. Therefore, we were unable to adequately compare our results with findings from other studies investigating knowledge. An attempt was made, however, to incorporate items from previously tested knowledge questionnaires, and therefore some degree of confidence can be made in the results. Finally, due to the cross-sectional design, no causal conclusions can be drawn.
4.2. Conclusion
CHD patients, in particular women and South Asians, still do not have optimal awareness regarding CHD as their leading cause of death. Although CHD patients do have a moderate level of disease knowledge overall, greater education regarding CHD pathophysiology and treatments is needed. Cardiac patients with lower socioeconomic status, lower functional status, who were current smokers, who did not have a family history of CHD and who perceived less personal control over their disease had lower overall CHD knowledge. Given the established benefits of secondary prevention, clearly improving health knowledge among CHD patients may have beneficial effects on their cardiac prognosis.
4.3. Practice Implications
This current study suggests that although CHD patients have a moderate level of knowledge regarding their condition, there are disparities in knowledge among certain vulnerable groups. Tailored educational approaches may be necessary for those of low socioeconomic status, particularly with regard to CHD pathophysiology, tests and treatments. Possible formal testing for inadequate health literacy may be necessary, as it impacts adherence to diet, exercise, and medication instructions [64]. In addition, cardiac knowledge interventions must ensure that they are sensitive to the perceptions and capabilities of targeted individuals. It is also necessary to consider developing culturally appropriate interventions for those in different ethnic groups. Future studies should determine where in the continuum of care CHD education is most effective (i.e. community level, physician level, pre-event rehab level or post-event rehab level). Essentially, educational initiatives at any level need to be continually evaluated to ensure that they minimize disparities between vulnerable groups and that they truly do impact a patient’s ability to improve their cardiac health.
Acknowledgments
This study was funded by CIHR grant # HOA-80676. Dr. Grace is supported by CIHR MSH-80489 and Ms. Kayaniyil is supported by the Heart and Stroke Foundation of Ontario.
Contributor Information
Sheena Kayaniyil, York University.
Chris Ardern, York University.
Jane Winstanley, York Central Hospital.
Cynthia Parsons, York Central Hospital.
Stephanie Brister, University Health Network.
Paul Oh, Sunnybrook Health Sciences Centre and Toronto Rehabilitation Institute.
Donna E. Stewart, University Health Network and University of Toronto
Sherry L. Grace, York University and University Health Network, 4700 Keele St., Bethune 368, Toronto, ON M3J 1P3, Tel: 416-736-2100 x.22364, Fax: 416-736-5774
References
- 1.World Health Organization. Measuring the global burden of disease and risk factors, 1990—2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global burden of disease and risk factors. New York: Oxford University Press; 2006. [Google Scholar]
- 2.Grace SL, Fry R, Cheung A, Stewart DE. Cardiovascular disease. BMC Womens Health. 2004;4:S15. doi: 10.1186/1472-6874-4-S1-S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–41. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 4.Salomaa V, Miettinen H, Niemela M, Ketonen M, Mahonen M, Immonen-Raiha P, et al. Relation of socioeconomic position to the case fatality, prognosis and treatment of myocardial infarction events; the FINMONICA MI register study. J Epidemiol Community Health. 2001;55:475–82. doi: 10.1136/jech.55.7.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vaccarino V, Rathore SS, Wenger NK, Frederick PD, Abramson JL, Barron HV, et al. Sex and racial differences in the management of acute myocardial infarction, 1994 through 2002. N Engl J Med. 2005;353:671–82. doi: 10.1056/NEJMsa032214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Becker MH, Maiman LA, Kirscht JP, Haefner DP, Drachman RH. The health belief model and prediction of dietary compliance: A field experiment. J Health Soc Behav. 1977;18:348–66. [PubMed] [Google Scholar]
- 7.Ford ES, Jones DH. Cardiovascular health knowledge in the United States: Findings from the national health interview survey, 1985. Prev Med. 1991;20:725–36. doi: 10.1016/0091-7435(91)90067-e. [DOI] [PubMed] [Google Scholar]
- 8.Stewart DE, Abbey SE, Shnek ZM, Irvine J, Grace SL. Gender differences in health information needs and decisional preferences in patients recovering from an acute ischemic coronary event. Psychosom Med. 2004;66:42–8. doi: 10.1097/01.psy.0000107006.83260.12. [DOI] [PubMed] [Google Scholar]
- 9.Wenger NK. Patient and family education after myocardial infarction. Postgrad Med. 1975;57:129–34. doi: 10.1080/00325481.1975.11714080. [DOI] [PubMed] [Google Scholar]
- 10.Alm-Roijer C, Fridlund B, Stagmo M, Erhardt L. Knowing your risk factors for coronary heart disease improves adherence to advice on lifestyle changes and medication. J Cardiovasc Nurs. 2006;21:E24–31. doi: 10.1097/00005082-200609000-00015. [DOI] [PubMed] [Google Scholar]
- 11.Alm-Roijer C, Stagmo M, Uden G, Erhardt L. Better knowledge improves adherence to lifestyle changes and medication in patients with coronary heart disease. Eur J Cardiovasc Nurs. 2004;3:321–30. doi: 10.1016/j.ejcnurse.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 12.Furze G, Lewin RJ, Murberg T, Bull P, Thompson DR. Does it matter what patients think? The relationship between changes in patients’ beliefs about angina and their psychological and functional status. J Psychosom Res. 2005;59:323–9. doi: 10.1016/j.jpsychores.2005.06.071. [DOI] [PubMed] [Google Scholar]
- 13.Cooper A, Lloyd G, Weinman J, Jackson G. Why patients do not attend cardiac rehabilitation: Role of intentions and illness beliefs. Heart. 1999;82:234–6. doi: 10.1136/hrt.82.2.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Petrie KJ, Weinman J, Sharpe N, Buckley J. Role of patients’ view of their illness in predicting return to work and functioning after myocardial infarction: Longitudinal study. Brit Med J. 1996;312:1191–4. doi: 10.1136/bmj.312.7040.1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gump BB, Matthews KA, Scheier MF, Schulz R, Bridges MW, Magovern GJS. Illness representations according to age and effects on health behaviors following coronary artery bypass graft surgery. J Am Geriatr Soc. 2001;49:284–9. doi: 10.1046/j.1532-5415.2001.4930284.x. [DOI] [PubMed] [Google Scholar]
- 16.Weinman J, Petrie KJ, Sharpe N, Walker S. Causal attributions in patients and spouses following first-time myocardial infarction and subsequent lifestyle changes. Br J Health Psychol. 2000;5:263–73. [Google Scholar]
- 17.Khan MS, Jafary FH, Jafar TH, Faruqui AM, Rasool SI, Hatcher J, et al. Knowledge of modifiable risk factors of heart disease among patients with acute myocardial infarction in Karachi, Pakistan: A cross sectional study. BMC Cardiovasc Disord. 2006;6:18. doi: 10.1186/1471-2261-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marcuccio E, Loving N, Bennett SK, Hayes SN. A survey of attitudes and experiences of women with heart disease. Women’s Health Issues. 2003;13:23–31. doi: 10.1016/s1049-3867(02)00193-7. [DOI] [PubMed] [Google Scholar]
- 19.Momtahan K, Berkman J, Sellick J, Kearns SA, Lauzon N. Patients’ understanding of cardiac risk factors: A point-prevalence study. J Cardiovasc Nurs. 2004;19:13–20. doi: 10.1097/00005082-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 20.Oliver-Mcneil S, Artinian NT. Women’s perceptions of personal cardiovascular risk and their risk-reducing behaviors. Am J Crit Care. 2002 May;11(3):221–7. [PubMed] [Google Scholar]
- 21.Redfern J, Ellis ER, Briffa T, Freedman SB. High risk-factor level and low risk-factor knowledge in patients not accessing cardiac rehabilitation after acute coronary syndrome. Medical Journal of Australia. 2007;186:21–5. doi: 10.5694/j.1326-5377.2007.tb00783.x. [DOI] [PubMed] [Google Scholar]
- 22.Zerwic JJ, King KB, Wlasowicz GS. Perceptions of patients with cardiovascular disease about the causes of coronary artery disease. Heart Lung. 1997;26:92–8. doi: 10.1016/s0147-9563(97)90068-6. [DOI] [PubMed] [Google Scholar]
- 23.Andersson P, Leppert J. Men of low socio-economic and educational level possess pronounced deficient knowledge about the risk factors related to coronary heart disease. J Cardiovasc Risk. 2001;8:371–7. doi: 10.1177/174182670100800606. [DOI] [PubMed] [Google Scholar]
- 24.Kirkland SA, MacLean DR, Langille DB, Joffres MR, MacPherson KM, Andreou P. Knowledge and awareness of risk factors for cardiovascular disease among Canadians 55 to 74 years of age: Results from the Canadian heart health surveys, 1986–1992. CMAJ. 1999;161:S10–6. [PMC free article] [PubMed] [Google Scholar]
- 25.Liew H, Taylor DM, Tjipto A, Bailey M. Investigation of the variables that impact upon the knowledge of cardiac risk factors. Emerg Med Australas. 2006;18:252–8. doi: 10.1111/j.1742-6723.2006.00848.x. [DOI] [PubMed] [Google Scholar]
- 26.Potvin L, Richard L, Edwards AC. Knowledge of cardiovascular disease risk factors among the Canadian population: Relationships with indicators of socioeconomic status. CMAJ. 2000;162:S5–11. [PMC free article] [PubMed] [Google Scholar]
- 27.Mosca L, Mochari H, Christian A, Berra K, Taubert K, Mills T, et al. National study of women’s awareness, preventive action, and barriers to cardiovascular health. Circulation. 2006;113:525–34. doi: 10.1161/CIRCULATIONAHA.105.588103. [DOI] [PubMed] [Google Scholar]
- 28.Cronin SN, Freeman LH, Ryan G, Drake DM. Recovery after percutaneous transluminal coronary angioplasty: Assessment after discharge. Crit Care Nurse. 2000;20:70–3. [PubMed] [Google Scholar]
- 29.Jafary FH, Aslam F, Mahmud H, Waheed A, Shakir M, Afzal A, et al. Cardiovascular health knowledge and behavior in patient attendants at four tertiary care hospitals in Pakistan--a cause for concern. BMC Public Health. 2005;5:124. doi: 10.1186/1471-2458-5-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Link I, Stewart DE, Williamson KM, Rush JW, Reid RD, Anand SS, et al. The cardiac rehabilitation care continuity through automatic referral evaluation (CRCARE) study: Design and methods. Presented at the Heart & Stroke/Richard Lewar Centre of Excellence in Cardiovascular Research Annual Scientific Day; 2007 May. [Google Scholar]
- 31.Canadian Association of Cardiac Rehabilitation. Canadian guidelines for cardiac rehabilitation and cardiovascular disease prevention: Enhancing the science, refining the art. Winnipeg, MB: CACR; 2004. [Google Scholar]
- 32.Maeland JG, Havik OE. Measuring cardiac health knowledge. Scand J Caring Sci. 1987;1:23–31. doi: 10.1111/j.1471-6712.1987.tb00296.x. [DOI] [PubMed] [Google Scholar]
- 33.Smith MM, Hicks VL, Heyward VH. Coronary heart disease knowledge test: Developing a valid and reliable tool. Nurse Pract. 1991;16:28, 31, 35–8. [PubMed] [Google Scholar]
- 34.MacArthur scale of subjective social status [homepage on the Internet] University of California; San Francisco: Mar 17, 2001. Available from: http://www.macses.ucsf.edu/Research/Psychosocial/notebook/usladder.html. [Google Scholar]
- 35.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, et al. A brief self-administered questionnaire to determine functional capacity (the duke activity status index) Am J Cardiol. 1989;64:651–4. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 36.Bairey Merz CN, Olson M, McGorray S, Pakstis DL, Zell K, Rickens CR, et al. Physical activity and functional capacity measurement in women: A report from the NHLBI-sponsored WISE study. J Womens Health Gend Based Med. 2000;9:769–77. doi: 10.1089/15246090050147745. [DOI] [PubMed] [Google Scholar]
- 37.Nelson CL, Herndon JE, Mark DB, Pryor DB, Califf RM, Hlatky MA. Relation of clinical and angiographic factors to functional capacity as measured by the duke activity status index. Am J Cardiol. 1991;68:973–5. doi: 10.1016/0002-9149(91)90423-i. [DOI] [PubMed] [Google Scholar]
- 38.Schuit AJ, Schouten EG, Westerterp KR, Saris WH. Validity of the physical activity scale for the elderly (PASE): According to energy expenditure assessed by the doubly labeled water method. J Clin Epidemiol. 1997;50:541–6. doi: 10.1016/s0895-4356(97)00010-3. [DOI] [PubMed] [Google Scholar]
- 39.Moss-Morris R, Weinman J, Petrie KJ, Horne R, Cameron LD, Buick D. The revised illness perception questionnaire (IPQ-R) Psychol Health. 2002;17:1–16. [Google Scholar]
- 40.Weinman J, Petrie KJ, Moss-Morris R, Horne R. The illness perception questionnaire: A new method for assessing the cognitive representation of illness. Psychology and Health. 1996;11:431–45. [Google Scholar]
- 41.SPSS Inc. SPSS for windows. 2006. p. 15.0. [Google Scholar]
- 42.Anand SS, Yusuf S. Risk factors for cardiovascular disease in Canadians of South Asian and European origin: A pilot study of the study of heart assessment and risk in ethnic groups (SHARE) Clin Invest Med. 1997;20:204–10. [PubMed] [Google Scholar]
- 43.Pilote L, Dasgupta K, Guru V, Humphries KH, McGrath J, Norris C, et al. A comprehensive view of sex-specific issues related to cardiovascular disease. CMAJ. 2007;176:S1–44. doi: 10.1503/cmaj.051455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rosenfeld JA. Heart disease in women. Gender-specific statistics and prevention strategies for a population at risk. Postgrad Med. 2000;107(6):111, 6. doi: 10.3810/pgm.2000.5.15.1094. quiz 156. [DOI] [PubMed] [Google Scholar]
- 45.McPherson R. Coronary artery disease and women: Applying the guidelines for risk factor management. Can J Cardiol. 2000;16:5A–10A. [PubMed] [Google Scholar]
- 46.Brister SJ, Hamdulay Z, Verma S, Maganti M, Buchanan MR. Ethnic diversity: South Asian ethnicity is associated with increased coronary artery bypass grafting mortality. J Thorac Cardiovasc Surg. 2007;133:150–4. doi: 10.1016/j.jtcvs.2006.05.068. [DOI] [PubMed] [Google Scholar]
- 47.Gupta M, Singh N, Warsi M, Reiter M, Ali K. Canadian South Asians have more severe angiographic coronary disease than European Canadians despite having fewer risk factors. Can J Cardiol. 2001;17:226C. [Google Scholar]
- 48.Alboni P, Amadei A, Scarfo S, Bettiol K, Ippolito F, Baggioni G. In industrialized nations, a low socioeconomic status represents an independent predictor of mortality in patients with acute myocardial infarction. Ital Heart J. 2003;4:551–8. [PubMed] [Google Scholar]
- 49.Horne BD, Muhlestein JB, Lappe DL, Renlund DG, Bair TL, Bunch TJ, et al. Less affluent area of residence and lesser-insured status predict an increased risk of death or myocardial infarction after angiographic diagnosis of coronary disease. Ann Epidemiol. 2004;14:143–50. doi: 10.1016/S1047-2797(03)00125-X. [DOI] [PubMed] [Google Scholar]
- 50.Rankin J, Bhopal R. Understanding of heart disease and diabetes in a South Asian community: Cross-sectional study testing the ‘snowball’ sample method. Public Health. 2001;115:253–60. doi: 10.1038/sj.ph.1900777. [DOI] [PubMed] [Google Scholar]
- 51.2001 census: Visible minority population, by age group. [homepage on the Internet] 2005. Available from: http://www40.statcan.ca/l01/cst01/demo50a.htm?sdi=census.
- 52.McKeigue PM, Miller GJ, Marmot MG. Coronary heart disease in South Asians overseas: A review. J Clin Epidemiol. 1989;42:597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 53.Capewell S, MacIntyre K, Stewart S, Chalmers JW, Boyd J, Finlayson A, et al. Age, sex, and social trends in out-of-hospital cardiac deaths in Scotland 1986–95: A retrospective cohort study. Lancet. 2001;358:1213–7. doi: 10.1016/S0140-6736(01)06343-7. [DOI] [PubMed] [Google Scholar]
- 54.Morrison C, Woodward M, Leslie W, Tunstall-Pedoe H. Effect of socioeconomic group on incidence of, management of, and survival after myocardial infarction and coronary death: Analysis of community coronary event register. Brit Med J. 1997;314:541–6. doi: 10.1136/bmj.314.7080.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Salomaa V, Niemela M, Miettinen H, Ketonen M, Immonen-Raiha P, Koskinen S, et al. Relationship of socioeconomic status to the incidence and prehospital, 28-day, and 1-year mortality rates of acute coronary events in the FINMONICA myocardial infarction register study. Circulation. 2000;101:1913–8. doi: 10.1161/01.cir.101.16.1913. [DOI] [PubMed] [Google Scholar]
- 56.Smith GD, Hart C, Blane D, Gillis C, Hawthorne V. Lifetime socioeconomic position and mortality: Prospective observational study. Brit Med J. 1997;314:547–52. doi: 10.1136/bmj.314.7080.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. 2007;167:1503–9. doi: 10.1001/archinte.167.14.1503. [DOI] [PubMed] [Google Scholar]
- 58.Rootman I, Gordon-El-Bihbety D. A vision for a health literate Canada: Report of the expert panel on health literacy. Ottawa, ON: Canadian Public Health Association; 2008. [Google Scholar]
- 59.Gaw BL. Motivation to change life-style following PTCA. Dimens Crit Care Nurs. 1992;11:68–74. doi: 10.1097/00003465-199203000-00005. [DOI] [PubMed] [Google Scholar]
- 60.Gulanick M, Naito A. Patients’ reactions to angioplasty: Realistic or not? Am J Crit Care. 1994;3:368–73. [PubMed] [Google Scholar]
- 61.Rahe RH, Ward HW, Hayes V. Brief group therapy in myocardial infarction rehabilitation: Three- to four-year follow-up of a controlled trial. Psychosom Med. 1979;41:229–42. doi: 10.1097/00006842-197905000-00006. [DOI] [PubMed] [Google Scholar]
- 62.Rahe RH, Scalzi C, Shine K. A teaching evaluation questionnaire for postmyocardial infarction patients. Heart Lung. 1975;4:759–66. [PubMed] [Google Scholar]
- 63.Scalzi CC, Burke LE, Greenland S. Evaluation of an inpatient educational program for coronary patients and families. Heart Lung. 1980;9:846–53. [PubMed] [Google Scholar]
- 64.Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998;158:166–72. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]