Abstract
Lahey and Waldman (2003; 2005) proposed a developmental propensity model in which three dimensions of children's emotional dispositions are hypothesized to transact with the environment to influence risk for conduct disorder, heterogeneity in conduct disorder, and comorbidity with other disorders. To prepare for future tests of this model, a new measure of these dispositions was tested. Exploratory factor analysis of potential items was conducted in a sample of 1,358 4-17 year olds. Confirmatory factor analyses then confirmed the three dispositional dimensions in a second sample of 2,063 pairs of 6-17 year old twins. Caretaker ratings of the dispositional dimensions were associated as predicted with symptoms of conduct disorder and other psychopathology. In a third sample, caretaker ratings of each disposition correlated uniquely with relevant observational measures of child behavior and unintentional injuries. These findings provide initial support for the new dispositional measure.
Lahey and Waldman (2003, 2005) proposed a developmental propensity model of conduct disorder (CD) in which children's dispositions to respond emotionally to the environment are posited to be key factors in the development of CD. The model states that three relatively enduring emotional dispositions—sympathetic response to other people, negative emotional response to threat and frustration, and positive response to novel and risky situations—influence children's propensity to develop CD through transactions with the environment. These three dispositional dimensions are based conceptually on previously identified dispositional constructs, but the model integrates them in a broad etiologic framework. In particular, the model asserts that the three dispositional dimensions are relatively uncorrelated, but jointly influence risk for CD. The model also offers testable hypotheses regarding the roles of the three dispositions in fostering CD through transactions with the environment and posits that the three dispositions provide an organizing framework for understanding the role of genetic and environmental influences on CD.
The dispositional dimension of prosociality is defined by sympathetic concern for others, helping and sharing, respect for social rules, and guilt over misdeeds. Thus, it is very similar to Goodman's prosocial strengths dimension (Goodman, Ford, Simmons, Gatward, & Meltzer, 2003) and Eisenberg's construct of dispositional sympathy (Eisenberg et al., 1989), which are both inversely related to CD. Some items in the five-factor model construct of agreeableness related to sympathy (Costa & McCrae, 1987) also overlap with prosociality. The difference between prosociality and these constructs is that respect for rules and guilt over misdeeds are not included in these previous constructs, but are hypothesized to be an integral part of prosociality.
In addition, many of the items that define prosociality can be viewed as the opposite of most of the “callousness” items that load consistently on Frick's callous-unemotional trait, which also is correlated with CD (Frick, Bodin, & Barry, 2000; Frick, Stickle, Dandreaux, Farrell, & Kimonis, 2005). Strong support for this view comes from a factor analysis of items on Frick's callous-unemotional trait and Goodman's prosocial strengths dimension (Goodman et al., 2003), which found that both sets of items loaded strongly on the same dimension (Dadds, Fraser, Frost, & Hawes, 2005).
In our proposed developmental propensity model, prosociality is hypothesized to (1) facilitate adaptive social bonding and cooperation, and (2) influence the valence of some key consequences of behavior that create important person-environment interactions. For example, consider a toddler who wins a rough tussle over a toy that gives a bloody nose to the other child. If the aggressor is high in prosociality, seeing the other child cry and bleed would likely be aversive and reduce the likelihood of future aggression. In contrast, if the aggressor is low in prosociality, the seized toy would likely be reinforcing and seeing the bloodied playmate would either be neutral or reinforcing, leading to increased aggression. Furthermore, social praise for appropriate behavior is hypothesized to be less reinforcing to children low in prosociality, and criticism for inappropriate behavior is hypothesized to be less punishing, further increasing risk for CD.
The hypothesized dimension of daring is defined by the descriptors of daring, brave, and adventurous, based on Farrington and West's (1993) observation that parent ratings of the single item of ‘daring’ during childhood was a robust predictor of future criminal offending. Daring is also defined by enjoyment of risky and loud activities and rough games and sports. Thus, daring is also similar to the construct of sensation seeking, which is correlated with CD (Russo et al., 1993). In the current developmental propensity model, daring is hypothesized to influence risk for developing CD through person-environment interactions involving the approach-avoidance valence of high-risk situations and some kinds of consequences of behavior. For example, breaking windows in a school at night might be attractive and the excitement of running from the police might reinforce vandalism in a child who is high in daring, but the same experiences would be aversive and punishing to a child who is low in daring.
Children rated high on negative emotionality are hypothesized to be easily and intensely upset by frustrations, threats, and losses. Therefore, because the rules and restrictions that adults place on children are often frustrating, successfully opposing or circumventing those rules would be strongly reinforcing to children high negative emotionality. When such children experience frustrations or threats during interactions with other children, they react with intense, global negative affect. Such emotional responses can easily be shaped into aggressive behavior by the responses of the children and adults (Lahey & Waldman, 2003). In some ways, negative emotionality is similar to the construct of neuroticism (Costa & McCrae, 1987). It differs from neuroticism primarily by not including items such as fear, anxiety, and depression.
Thus, children who are high in negative emotionality, low in prosociality, and high in daring are hypothesized to be at high risk for the development of ODD behaviors if they become entangled in coercive relationships with adults, siblings, and peers that reinforce oppositional behavior. Similarly, transactions with the environment are hypothesized to lead to the antisocial behaviors that define CD, particularly if disposed children spend significant unsupervised time with deviant peers in childhood and adolescence (Lahey & Waldman, 2003, 2005; Patterson, Reid, & Dishion, 1992). In the absence of such maladaptive environmental influences, the emotional dispositions would rarely lead to ODD or CD, but it is unlikely that predisposed children would not be exposed to maladaptive environments. This is because children high in negative emotionality, low in prosociality, and high in daring are hypothesized to often evoke and select those high risk environments (Lahey & Waldman, 2003, 2005; Waldman, Singh, & Lahey, 2006). The model also proposes that individual differences in cognitive abilities and language development also are related to risk for CD (Lahey & Waldman, 2003). Such abilities are not addressed in the present paper, however, which focuses on the measurement of the emotional dispositions.
Because each dispositional dimension is hypothesized to explain independent variance in the risk for CD, different patterns of variation in the dispositional dimensions may help us understand the heterogeneity of CD. That is, the conduct problems of different youth with CD may be associated with deviance in different emotional dispositions. On the other hand, the developmental propensity model raises the possibility that the three dimensions might influence risk for CD interactively, which could mean that the dispositional dimensions influence risk for CD both independently and jointly.
The developmental propensity model also offers hypotheses regarding comorbidity. CD co-occurs with essentially all common mental disorders at greater than chance levels, but the extent of comorbidity varies considerably by disorder. To consider three examples of such comorbidity, CD is very likely to be comorbid with oppositional defiant disorder (ODD), followed by major depression, followed by anxiety disorders (Angold, Costello, & Erkanli, 1999; Costello, Mustillo, Erkanli, Keeler, & Angold, 2003; Nottelmann & Jensen, 1995). The developmental propensity model proposes that this differential comorbidity with CD is largely the result of different forms of psychopathology sharing more or less similar profiles of emotional dispositions with CD. For example, the hypothesized profile of emotional dispositions of youth with ODD is very similar to that of CD. Both are hypothesized to be high in negative emotionality, but CD is hypothesized to be even lower in prosociality and higher in daring than ODD (Lahey & Waldman, 2003). Depression and anxiety disorders are hypothesized to be comorbid with CD partly because high negative emotionality also is associated with them (Clark, Watson, & Mineka, 1994; Lahey & Waldman, 2005). Depression is hypothesized to be less comorbid with CD than is ODD because depression is unrelated to lower prosociality and higher daring. Anxiety disorders are thought to be least comorbid with CD because, unlike depression, anxiety is inversely associated with daring, whereas CD is positively related to daring (Lahey & Waldman, 2003, 2005).
Need for a New Measure of the Hypothesized Emotional Dispositions
It is necessary to operationalize the three hypothesized dispositional dimensions using psychometrically sound measures before conducting empirical tests of the model. Because the three hypothesized dispositional dimensions are conceptually similar to those identified in previous studies, we considered the option of using existing measures of related constructs, such as neuroticism (Costa & McCrae, 1987), dispositional sympathy (Eisenberg et al., 1989), and sensation seeking (Russo et al., 1993). We rejected this option for four primary reasons, however. First, as noted above, no existing set of scales measures the three hypothesized dimensions of emotional propensity exactly as specified in the model. Second, the existing measures of similar dimensions of emotional propensity each use different response formats, and sometimes different informants, which would seriously compromise integrated tests of the model that used all three dimensions at the same time. Third, the items used by existing measures of the three dispositional dimensions have never been tested together using factor analytic methods to determine if they actually measure three independent dimensions. Fourth, most of the existing relevant scales contain some items that are clear synonyms or antonyms of symptoms of CD and other mental disorders, which could inflate associations of the dispositional constructs with CD and other forms of psychopathology. It would have been possible to remove these confounding items, revise the existing scales to use the same response format, add new items, and conduct new factor analyses and tests of the psychometric properties of the revised scales. That effort would change the existing constructs and be tantamount to developing a new integrated measure of the three dispositional constructs, however. Therefore, we developed the new Child and Adolescent Dispositions Scale (CADS) for the specific purpose of testing the dispositional model of CD in future studies using scales that are completely true to the model.
The goals of the present paper are to describe the development of the CADS and report the results of a series of initial tests of its internal validity, external validity, and test-retest reliability. Our first step was to use exploratory factor analysis (EFA) to select the items that best define each dispositional dimension. Second, we conducted confirmatory factor analyses (CFA) using data from a second sample to confirm the hypothesized factor structure of the CADS. Third, we assessed the test-retest reliability of the CADS. Fourth, we provided initial evidence on its external validity by testing the hypotheses that each dispositional dimension is related to child and adolescent CD and other dimensions of psychopathology as predicted by the model. Fifth, correlations of the CADS dimensions with relevant measures of child behavior coded by independent observers provided additional evidence of the external validity of CADS.
METHODS
In all three studies, the child's parent or guardian signed an informed consent form approved by the University of Chicago Institutional Review Board and the child gave oral assent after hearing an approved assent script.
Participants
Study 1 participants
Participants in the Georgia Health and Behavior Study (GHBS; (Lahey, Applegate et al., 2004) were representative of all 4–17-year-old youth living in the Atlanta metropolitan statistical area in 2000. Interviews of caretakers (82.0% biological mothers, 13.6% biological fathers, 1.2% step-mothers, and 3.2% grandmothers) and 9–17-year-old youth were conducted in the family's home by trained interviewers, with a response rate of 71% for caretakers and 95% for youth whose caretaker was interviewed. After the interviews, 24 youth were excluded because they had been diagnosed by a professional as mentally retarded, psychotic, and/or autistic. As a result, 1,358 caretaker interviews and 832 youth interviews were used in the analyses. The caretaker classified 68.3% of these youth as Non-Hispanic white, 24.1% as African American, 2.9% as Hispanic, and 4.7% as other race-ethnicity. The proportion of females was 51.2%. A randomly selected subsample of 290 caretakers and 196 youth stratified on caretakers' initial ratings of emotional and behavior problems were re-interviewed 7–14 days later to assess test-retest reliability (Lahey, Applegate et al., 2004).
Study 2 participants
The Tennessee Twin Study (TTS) sample was representative of all 6–17-year-old twins who were born in Tennessee and were still living in one of the state's five metropolitan statistical areas (Nashville, Memphis, Knoxville, Chattanooga, and Bristol) in 2001. Addresses of potentially eligible families were provided by the Tennessee Department of Health. A random sample of those families was selected stratified on the age of the twins and 35 geographic subareas. Household interviews were completed with 2,063 adult caretakers (90.8% biological mothers, 7.5% biological fathers, 0.5% step-mothers, and 1.2% grandmothers), with a response rate for caretakers of 69.8% and 97.9% for 9–17-year-old twin pairs who caretaker was interviewed. Twin pairs were excluded if either twin had been diagnosed as psychotic (twin 1 n = 17; twin 2 n = 11), or autistic (twin 1 n = 8; twin 2 n = 5). Only pairs in which both twins were interviewed are included (N = 2,025 pairs). The caretaker classified 71.4% of the twin pairs as Non-Hispanic white, 23.3% as African American, and 5.3 % as members of other race-ethnic groups. The proportion of females was 51.5% (twin 1) and 49.8% (twin 2).
Study 3 participants
Participants were enrolled in a longitudinal study of children who met DSM-IV diagnostic criteria for ADHD and matched comparison children (Lahey, Pelham et al., 2004). Participants were recruited at 4–6 years old at two sites. In Chicago, children presenting to a university child psychiatry clinic with inattention and/or hyperactivity were recruited. In Pittsburgh, 42.4% of the children who met criteria for ADHD were referred to a university child psychiatry clinic and the rest were recruited through advertisements. Comparison children matched on age, sex, and race-ethnicity were recruited from the same schools and neighborhoods. Participants were eligible only if they lived with their biological mother and did not exhibit pervasive developmental disorder, psychosis, or clear neurological disorder. Of the 315 eligible children, 259 participated (82.2%). Four children were excluded because the mean of two Stanford-Binet Short Form (Thorndike, Hagen, & Sattler, 1986) intelligence scores over two years was < 70. In the first assessment, 129 children who met DSM-IV symptom criteria for ADHD and 126 comparison children were assessed. The caretaker classified 63.6% of the probands and 63.5% of the comparison children as Non-Hispanic white, 30.2% of the probands and 31.0% of the comparison children as African American, and 6.2% of the probands and 5.6% of the comparison children as other race-ethnicity. The proportions of female children were 17.0% (proband) and 19.0% (comparison). The children were off medication with physician approval at the time of the initial assessment.
Study 1 and 2 Measures
The same measures were used in Studies 1 and 2. Caretakers were asked to rate each CADS item by thinking about how well it describes the youth's emotional behavior and how often it occurred in the last 12 months using a response scale of: “1. Not at all, 2. Just a little, 3. Pretty much, 4. Very much.” Consistent with Mischel's (2004) definition of the term “disposition,” CADS items refer to consistencies in emotional behavior, both on the whole and in certain situations. Most of the 48 CADS items were written to operationalize the three hypothesized dispositions. In order to determine if other items factored with these dimensions, however, additional items were written on revealing little emotion, being manipulatively charming, and taking pleasure in bothering others. All CADS items were newly written, but two items were loosely based on items used in an earlier measure of sensation seeking (Russo et al., 1993) and the behaviors described in some new items were similar to the behaviors referred to in items used in other measures of prosocial behavior and callousness (Frick et al., 2005; Goodman et al., 2003).
In both Studies 1 and 2, parallel versions of the Child and Adolescent Psychopathology Scale (CAPS) also were completed by adult caretakers for all youth and by 9-17 year old youth themselves. The CAPS (Lahey, Applegate et al., 2004) assesses DSM-IV symptoms of ADHD, ODD, CD, depression, and anxiety disorders. In addition, the CAPS contains items describing emotions and behaviors that are used in delinquency and aggression research, but only DSM-IV symptoms were used in these analyses. Not all kinds of symptoms were measured using both informants in the CAPS. Both respondents are reliable and valid informants on anxiety, depression, and CD, but only caretakers are strong informants on ODD and ADHD (Bird, Gould, & Staghezza, 1992; Hart, Lahey, Loeber, & Hanson, 1994).
CAPS items were rated on the same response scale as CADS items. Both CADS and CAPS items were randomized and administered in counterbalanced order, with random halves of the samples administered the items in forward or reverse order to control order effects. For the CAPS, test-retest intra-class correlations (ICCs) for youth respondents were CD = .78, major depression (MDD) = .68, and all anxiety disorders combined = .75. The CAPS test-retest ICCs for adult caretaker respondents were: CD = .89, ODD = .80, MDD = .80, and anxiety disorders = .86. Strong correlations with relevant measures of functional impairment indicate good external validity for both the caretaker and youth versions of the CAPS (Lahey, Applegate et al., 2004).
Study 3 Measures
In the baseline assessment in this longitudinal study, the mother was asked if the child had “suffered any injury more serious than a scratch, bruise, or bump on the head that was the result of his or her own carelessness, impulsiveness, or poor judgment.” Similar maternal reports of unintentional injuries to children have been found to be reliable and valid when compared with medical records (Stone et al., 2006). This question was used as a criterion variable to test the external validity of daring, which refers to enjoyment of rough-and-tumble and risky activities. In addition, during the baseline assessment, mother-child interactions also were videotaped during a structured protocol for young children (Mariani & Barkley, 1997). This took place in a room equipped with a one-way mirror and a chair for the mother, two child-size chairs, a table with a telephone, shelves containing toys, a dust cloth, a box, a wastebasket, several magazines, a television monitor showing cartoons, and a bookcase. Upon entering the room, the mother played freely with her child. After 10 minutes, the interviewer returned to the room and scattered clothes and trash (e.g., papers, empty containers) around the room. The interviewer then handed the mother a list of instructions, an Etch-a-Sketch, worksheets, a magazine, and a pencil, and quietly reviewed the task instructions. The mother was instructed to complete the following tasks in order during the next 15 minutes: (1) return the toys to the shelf, (2) put the clothes in the box, (3) put the crumpled paper and trash in the wastebasket, (4) sit at the table and count geometric shapes, (5) copy a set of geometric designs on paper, (6) dust the table with the cloth, (7) work cooperatively with their child to draw a diagonal line on the Etch-a-Sketch, and (8) choose one toy and play quietly while the mother reads a magazine and takes a one-minute telephone call from the interviewer. Because tasks were completed in as little as 13 minutes, the first 13 minutes of structured interaction were coded for all dyads. A total of 247 participants completed the mother-child interactions.
Mother-child interactions were coded using the reliable Dyadic Parent-Child Interaction Coding System II (Eyberg et al., 2001), which has been found to discriminate referred young children with conduct problems from comparisons children (Burns & Patterson, 2001). Coders were given no information about the children on the tapes. The primary observer coded all tapes and a second observer independently coded 30% of the tapes. Frequencies of maternal commands and child responses to those commands were coded continuously. To provide a test of the external validity of the prosociality dimension of the CADS, the child's compliance to maternal commands was calculated as the ratio of compliance to direct and indirect maternal commands to the total number of maternal commands (summed across all play and task situations). Inter-rater agreement (agreements/ agreements + disagreements) for total maternal commands was .95 and was .79 for total child compliance. In addition, the child's affective valence was rated once at the end of the play period and once at the end of the task situations and summed to provide a test of the external validity of the negative emotionality dimension. Child affective valence was rated on a scale ranging from 1 (exuberantly positive affect) to 5 (unrestrained negative affect). The Spearman rank correlation for inter-rater agreement on ratings of child negative affect was r (124) = .67, p < .0001.
During the baseline assessment, children also were observed in the “forbidden toy task,” which is part of the Structured Observation of Academic and Play Settings (Mariani & Barkley, 1997; Roberts, 1990), which has been found to reliably distinguish hyperactive from comparison children (Roberts, 1990). An approximately 15 ft x 18 ft room contained two child-size tables and one child-sized chair at each table. The children had been allowed to play with two identical sets of toys placed on both tables (ring toss, Polly Pocket, coloring book with crayons, Magna Doodle, and Tinker Toys) earlier in the day. When brought into the room for the forbidden toy task, novel and attractive toys were on one table (Power Ranger, Gak, toy gun, water toy, Koosh ball, magic wand, and doll), and a chip-sorting task was on the other table. The examiner instructed the child to sit at the table containing the chip-sorting task and instructed the child not to leave the chair and not to play with the toys on the other table. The children were instructed to sort red, blue, and white chips into three slotted containers that were labeled with the same colors. They sorted one chip of each color with the experimenter present, which revealed that all children understood the directions. They were instructed to sort as many chips as they could until the examiner returned. The examiner told the child that he or she would be outside and left the room for 15 minutes.
The child's behavior was later coded from videotapes. Tapes were divided into 40 15-second observe, 5-second record intervals using auditory cues. Observers coded whether the child was engaged in each of the following behaviors during each coding interval: (1) sorted chips, (2) were out of their seat, without continuing to sort chips, (3) made any audible noise, and/or (4) touched a forbidden toy. Interval-by-interval agreement between pairs of coders was computed for 10% of the tapes. Inter-observer agreement for touching toys was kappa = .97. The forbidden toys task provided a second test of the external validity of the prosociality dimension of the CADS. In this longitudinal study, the parent did not complete the CADS on the child until the year 6 assessment.
DATA ANALYSIS
Study 1 Data Analysis
Exploratory factor analysis of CADS
Principal factors analyses of caretaker-rated CADS items from Study 1 were conducted first to identify the items that loaded most strongly and uniquely on each factor. These EFAs were conducted on the product-moment correlation matrix using varimax rotation, defining the communalities as the squared multiple correlation, but results were highly similar using promax rotations. Less than 2% of items had missing data, but to avoid list-wise deletion of all cases with any missing data, we assumed that this small amount of information was missing at random and the correlation matrix was reset to have a pairwise sample size of 1,358 for caretaker ratings. To determine empirically the number of factors to extract in this EFA, we conducted parallel analyses in which eigenvalues were derived from random data matrices with the same numbers of items and participants (Glorfeld, 1995; O'Connor, 2000). We conducted 1,000 random analyses and used the 95th percentile of the distribution of eigenvalues to determine that three factors could be extracted (Glorfeld, 1995). Items with loadings > .40 on each factor, but with no loadings >.30 on another factor will be selected to define each dispositional dimension. Principal components analysis yielded virtually identical results.
Reliability of the CADS
Data from Study 1 also were used to estimate the 7-14 day test-test reliability of the three CADS factor scores as intra-class correlations. Unit-weighted CADS factor scores were computed by taking the mean of all non-missing items with loadings on each factor of ≥ .40 and no secondary loadings of ≥ .30 (see Table 1).
Table 1.
Factor Loadings of Items on the Three Factors Extracted in Exploratory Factor Analyses in Study 1.
| Prosociality Factor | Prosociality | Negative Emotionality |
Daring |
|---|---|---|---|
| Cares about others' feelings | .66 | ||
| Concerned about others when they are hurt | .64 | ||
| Spontaneously helps others | .63 | ||
| Cheers up others | .60 | ||
| Feels sorry for kids who get picked on | .58 | ||
| Concerned about right and wrong | .53 | ||
| Wants everyone to follow the rules | .53 | ||
| Would feel guilty if broke a law | .46 | ||
| Would be upset if saw an animal get hurt | .44 | ||
| Spontaneously shares | .43 | ||
| Enjoys learning interesting things | .43 | ||
| Tries to do excellent work | .43 | ||
| Cautious | .41 | −.34 | |
| Negative Emotionality Factor | |||
| Gets upset easily | .70 | ||
| Reacts intensely | .61 | ||
| Moods change unpredictably | .56 | ||
| Emotional | .56 | ||
| Blows things out of proportion | .52 | ||
| Enjoys disobeying adults | −.32 | .47 | |
| Selfish | −.32 | .44 | |
| Jealous | .44 | ||
| Gets bored easily | .44 | ||
| Easily embarrassed | .42 | ||
| Calm and easy-going (inverse) | −.43 | ||
| Daring Factor | |||
| Daring and adventurous | .66 | ||
| Enjoys risky and dangerous things | .57 | ||
| Likes rough games and sports | .51 | ||
| Likes things that are exciting and loud | .43 | ||
| Brave | .40 |
Note: All items with factor loadings of ≥.40 on at least one factor are shown. Items with no loadings ≥.40: friendly; afraid of children who like to fight; enjoys other people saying did a good job; reacts with little or no emotion to both positive and negative things; keeps true feelings to self; likes to scare other children; thinks it would be fun to watch dogs fight; thinks it's funny when other children are upset; likes TV, movies, comics, or electronic games with a lot of violence in them; enjoys bothering or hurting other children; likes for things to stay the same, smooth and charming when trying to get own way, more interested in sex than other children of same age, would be bothered if had no close friend, likes meeting new children, curious, enjoys being with other children of same age, and avoids situations where might get hurt.
External validity of the CADS: Relations to psychopathology
We conducted initial tests of the external validity of the CADS using data from Study 1 to determine if unit-weighted CADS factor scores exhibit: (1) the specific pattern of associations with CD, and (2) the different patterns of correlations with other dimensions of DSM-IV psychopathology predicted by the model (Lahey & Waldman, 2003, 2005). The criterion variables were mean ratings on DSM-IV symptoms of DSM-IV CD, ODD, major depression, and all anxiety disorders. Counts of caretaker and youth reports of symptoms of psychopathology were analyzed separately to test associations with CADS dimensions both within and between informants. Because the counts of symptoms were highly skewed and kurtotic, log-linear regression models that used robust standard errors were used. In these models, the three unit-weighted CADS factor scores, age, sex, total family income, and race-ethnicity were entered as simultaneous predictors. The developmental propensity model allows for the possibility of interactions among the dispositional dimensions. For this reason, the 3-way interaction among the dispositions will be tested for CD while testing all 2-way interactions.
Because log-linear regression does not provide an estimate of the amount of variance explained by the predictors, a pseudo-R2 was calculated by taking the square of the Pearson correlations between the predicted and observed values in each model using only the three CADS dimensions as the predictors. For this purpose only, psychopathology scores were first residualized on age, sex, age-squared, and the interaction of sex with age and age-squared. Differences in the magnitudes of associations of each CADS dimension with each pair of psychopathology dimensions were tested by simultaneously fitting separate log-linear models for each pair of psychopathology dimensions as the response variable, using the three dispositions, age, and sex as the predictor variables in general estimating equations (Zeger & Liang, 1986) to allow for the correlation between the psychopathology dimensions in the same participants.
Study 2 Data Analysis
CFAs were next conducted using data from Study 2 to confirm the three hypothesized CADS dimensions, which were defined by the items that loaded most strongly and uniquely on each of the three factors identified in the EFA of data from Study 1 (Table 1). CFA was used to compare the fit of the hypothesized 3-factor CADS model to a 1-factor model, in which one dimension was assumed to underlie all CADS items. CFA was conducted on the variance-covariance matrices for CADS items using maximum likelihood (ML) estimation, which assumes multivariate normality. Given the untenability of this assumption for these data, we also estimated the asymptotic covariance matrix. This allows estimation of appropriate standard errors and use of the Satorra-Bentler scaled χ2, which does not assume multivariate normality and scales the χ2 test to take into account the non-normality of the data. Alternative models were compared using the scaled difference (δ) χ2 test, which is appropriate for non-normal data (Satorra & Bentler, 2001). More than 97% of both twins having valid caretaker ratings for all items and >99.9% of both twins had complete caretaker ratings for > 90% of CADS items. ML estimation requires list-wise deletion of cases with missing data on one or more items. This resulted in effective sample size of 6- through 17-year-old youth of 1,799 for twin 1 and 1,804 for twin 2. The last step was to choose between orthogonal and correlated (oblique) factor versions of the hypothesized 3-factor model.
Study 3 Data Analysis
Data from Study 3 were used to provide initial evidence on the external validity of the three CADS dimensions. In these analyses, existing variables thought to be related to the CADS dimensions were used as criterion variables and the three CADS dimensions were entered simultaneously with age, sex, total family income, and race-ethnicity. First, using continuous observational data from the dyadic parent-child interaction, linear regression analyses were used to test predicted associations between CADS negative emotionality and the child's negative affective valence and between CADS prosociality and the child's compliance with parental commands. Second, logistic regression analysis was used to test the predicted association between daring and the child's unintentional injuries. Third, longitudinal binomial regression analyses were conducted to test associations between CADS dispositional scores and the proportion of children observed to touch forbidden toys over each of 40 observation intervals in the forbidden toy task. Children high in prosociality were predicted not to touch the toys both because the construct of prosociality is theoretically linked to social cooperation and because the CADS items on respect for rules and capacity for guilt loaded most strongly on this dimension. It is also possible, however, that children high in daring would be more attracted to both the toys and the risk of apprehension. Because the goal of these analyses was to test the external validity of each CADS dimension, interactions among CADS dimensions were not tested.
RESULTS
Study 1 Results: Exploratory Factor Analysis
The results of the initial EFA of the full CADS item pool shown in Table 1 were consistent with the dispositional model (Lahey & Waldman, 2003, 2005; Waldman et al., 2006), with items referring to sympathetic concern for others, helping, sharing, respect for rules, and capacity for guilt loading uniquely at ≥ .40 on the prosociality factor. Similarly, the items loading uniquely on the negative emotionality factor described getting upset easily, intensely, unpredictably, and out of proportion to the provocation. The items with unique loadings on the daring factor described youth who enjoy rough games and sports, like loud and exciting things, and are daring, adventurous, and brave. The EFA was repeated for CADS caretaker ratings for girls and boys separately and for younger (4- through 10-year-olds) and older (11- through 17-year-olds) youth separately. Congruence coefficients (Rummel, 1970) for the three factors were very high at .93–.97 between the sexes and .96–.98 between the age groups.
Study 2 Results: Confirming the Factor Structure of the CADS
CFA was used to compare the fit of the hypothesized 3-factor CADS model to a 1-factor model using data from a different sample than the one used in the EFA. Each of the three factors was defined by the items identified in Study 1 as loading >.40 on a dispositional dimension, but with no loading >.30 on another dimension. The correlated 3-factor model fit significantly better than the 1-factor model, as indicated by the scaled δχ2 (Satorra & Bentler, 2001). The superior fit of the correlated 3-factor model is also seen in the normed fit index (NFI), Akaike's Information Criterion (AIC), the root mean square residual (RMR), and the root mean square error of approximation (RMSEA). The NFI for the correlated 3-factor model was ≥ the .90 threshold for an adequate fit for each twin (Hu & Bentler, 1995). Similarly, the RMSEA for the correlated 3-factor model was in the “good fit” range of < .08 (Brown & Cudeck, 1993). The correlated 3-factor model fit significantly better than the orthogonal 3-factor model. This reflects modest correlations among the latent factors (all p < .0001) of negative emotionality and prosociality (r = −.32), negative emotionality and daring (r = .22), and prosociality and daring (r = −.23).
Study 1 Results: Reliability, Sex and Age Differences, and External Validity of the CADS
Reliability of the CADS
Test-retest intra-class correlations over 7-14 days were high for prosociality (ICC = .84), negative emotionality (ICC = .80), and daring (ICC = .80).
Sex and age differences in means
Simultaneous log-linear regression analyses revealed that mean prosociality scores were lower in males on average, β = −0.08, χ2 = 80.15, p < .0001, but there were not significant age differences at p < .05. Mean daring scores were higher in males on average, β = 0.18, χ2 = 71.26, p < .0001, and declined somewhat with increasing age, β = −0.01, χ2 = 8.73, p < .0001. There were neither sex nor age differences in mean negative emotionality scores at p < .05. Sex-by-age interactions were tested for each dimension, but were never significant at p < .05.
External validity of the CADS: Relations to psychopathology
Mean ratings on DSM-IV symptoms of CD, ODD, major depression, and all anxiety disorders were used as criterion variables in separate analyses. Caretaker and youth reports of symptoms from the CAPS were analyzed separately. As predicted by the developmental propensity model, CADS caretaker ratings of negative emotionality, prosociality, and daring each accounted for unique variance in both caretaker- and youth-reported CD symptoms (Table 3). The 3-way interaction among the dispositional dimensions was significant for both caretaker (β = −0.35, χ2 = 4.04, p < .05) and youth reports (β = −0.45, χ2 = 4.34, p < .05) of CD symptoms.
Table 3.
Tests of the External Validity of the Three Dimensions of the Child and Adolescent Dispositions Scale (CADS) by Assessing Associations with Four dimensions of Psychopathology in Simultaneous Regression Analyses in Study 1.
| Conduct Disorder | Oppositional- Defiant Disorder |
Major Depression | Anxiety Disorders | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Caretaker Ratings of Psychopathology | ||||||||||||
| Caretaker CADS Ratings | β | χ2 | R2 | β | χ2 | R2 | β | χ2 | R2 | β | χ2 | R2 |
| Prosociality | −0.86 | 138.74*** | .34 | −0.40 | 117.99*** | .39 | −0.11 | 5.53* | .33 | 0.07 | 2.91 | .25 |
| Negative Emotionality | 1.30 | 190.59*** | 0.77 | 602.66*** | 0.84 | 516.16*** | 0.70 | 433.42*** | ||||
| Daring | 0.44 | 41.27*** | 0.14 | 26.47*** | 0.00 | 0.00 | −.13 | 18.71*** | ||||
| Youth Ratings of Psychopathology | ||||||||||||
| Caretaker CADS Ratings | ||||||||||||
| Prosociality | −0.56 | 32.92*** | .26 | −0.02 | 0.09 | .12 | 0.05 | 0.74 | .11 | |||
| Negative Emotionality | 0.74 | 54.64*** | 0.45 | 105.95*** | 0.39 | 80.46*** | ||||||
| Daring | 0.22 | 6.14* | −0.09 | 5.56* | −0.18 | 19.38*** | ||||||
p < .05
p < .01
p < .0001
Note: Only tests of main effects are tabled; interactions among the dispositions in their associations with CD are reported in the text. All models simultaneously controlled for the two other dispositional dimensions, age, sex, total family income, and race-ethnicity. R2 = model pseudo-R2.
The three CADS dimensions also each accounted for unique variance in caretaker-reported ODD symptoms. This similarity in findings is consistent with hypothesis that ODD is the primary developmental precursor to childhood-onset CD and is frequently comorbid with CD because both disorders share very similar dispositional profiles (Lahey & Waldman, 2003). As predicted by the model, however, prosociality and daring were more strongly related with CD than with ODD and with any other dimension of psychopathology (all p < .0001). The association of the three CADS dimensions with parent-reported ODD also was tested with parent-reported CD included as an additional simultaneous predictor to attempt to control for comorbidity with CD. ODD symptoms were still significantly predicted by negative emotionality (β = 0.75, χ2 = 549.71, p < .0001), prosociality (β = −0.33, χ2 = 66.03, p < .0001), and daring (β = 0.12, χ2 = 20.03, p < .0001).
As predicted by the model, depression and anxiety symptoms were both significantly related to negative emotionality. Furthermore, anxiety was inversely related to daring, as predicted. Findings that were not predicted by the model included small but significant inverse associations between prosociality and major depression (for the caretaker informant) and between daring and major depression (for the youth informant). Consistent with the model, however, the association between prosociality and depression was significantly less strong than for both ODD and CD (both p < .0001). Similarly, the inverse association between daring and depression was significantly less strong than for the anxiety disorders, p < .001.
The association of the three CADS dimensions with depression also was tested with CD included as an additional simultaneous predictor. Parent-reported depression symptoms were still significantly predicted by negative emotionality (β = 0.81, χ2 = 457.94, p < .0001), but not prosociality (β = −0.02, χ2 = 0.24, p = .62) or daring (β = −0.02, χ2 = 0. 40, p = .52), controlling parent-reported CD. Youth-reported depression symptoms were still significantly predicted by negative emotionality (β = 0.38, χ2 = 75.73, p < .0001), prosociality (β = 0.11, χ2 = 3.94, p < .05), and daring (β = −0.13, χ2 = 11.46, p < .001), controlling youth-reported CD. The association of the three CADS dimensions with anxiety also was tested with CD included as an additional simultaneous predictor. Parent-reported anxiety symptoms were significantly predicted by negative emotionality (β = 0.67, χ2 = 374.07, p < .0001), prosociality (β = 0.14, χ2 = 10.34, p < .005), and daring (β = −0.15, χ2 = 25.55, p < .0001), controlling parent-reported CD. Youth-reported anxiety symptoms were still significantly predicted by negative emotionality (β = 0.32, χ2 = 55.03, p < .0001), prosociality (β = 0.16, χ2 = 8.06, p < .005), and daring (β = −0.22, χ2 = 29.89, p < .0001), controlling youth-reported CD. Thus, for depression and anxiety disorders, the significant associations with daring and prosociality were in the opposite direction as the significant associations of these dispositions with conduct disorder, supporting their discriminant validity. This was not found for negative emotionality, but it was predicted to be associated with each of these forms of psychopathology in the same direction.
The proportion of variance in each dimension of psychopathology accounted for by the three CADS dimensions alone (i.e., not including CD or the demographic covariates) was estimated using pseudo-R2 (Table 3). For example, the correlation between observed scores on the caretaker-rated CD dimension and scores predicted by the model for caretaker ratings on the three CADS dimensions was r = .58 (pseudo-R2 = .34).
Study 3 Results
Parent-child interactions
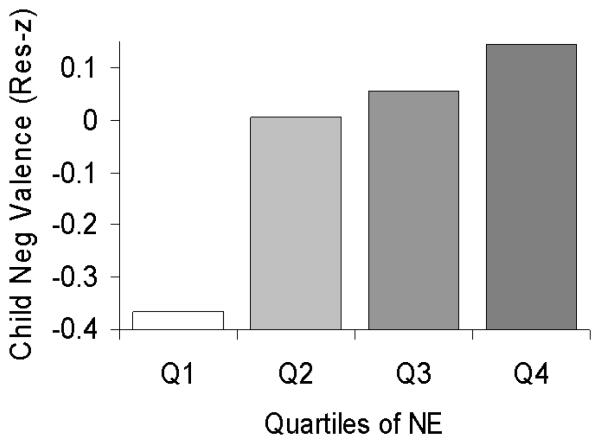
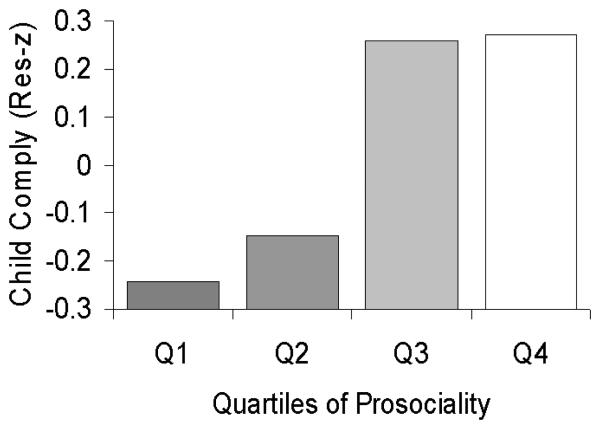
As reported in Table 4 and Figure 1, blind observer ratings of child negative affective valence during the parent-child interactions in Year 1 were significantly related to adult caretaker ratings of negative emotionality obtained five years later, but not with the other dispositional dimensions. Similarly, as reported in Table 4 and Figure 2, children who received higher caretaker ratings on prosociality were more compliant with parental commands during the parent-child interactions, but compliance was not associated with the other dispositional dimensions.
Table 4.
Tests of the External Validity of the Three Dispositional Dimensions of the Child and Adolescent Dispositions Scale (CADS) by Assessing Associations with Behavior Coded by Independent Observers in Study 3.
| Child Valence in Parent-child Interactions | ||
| Prosociality | β = −0.12 | χ2 = 0.89 |
| Negative Emotionality | β = 0.24 | χ2 = 4.75* |
| Daring | /5 = 0.01 | χ2 = 0.02 |
| Child Compliance in Parent-child Interactions | ||
| Prosociality | β = 0.04 | χ2 = 7.19** |
| Negative Emotionality | β = −0.02 | χ2 = 1.61 |
| Daring | β = −0.00 | χ2 = 0.04 |
| Touching Toys in Forbidden Toys Task | ||
| Prosociality | β = −0.93 | z = −2.56* |
| Negative Emotionality | β = 0.28 | z = 0.97 |
| Daring | /5 = 0.38 | z= 1.59 |
| Unintentional Injuries | ||
| Prosociality | O.R. = 0.6 (95% CI = 0.2 - 1. 4) | |
| Negative Emotionality | O.R. = 1.6 (95% CI = 0.7 – 3.6) | |
| Daring | O.R. = 2.8 (95% C.I. = 1.5-5.2)** | |
Note: All models simultaneously controlled for the other two dispositional dimensions, age, sex, total family income, intelligence, and race-ethnicity.
p < .05
p < .01
Figure 1.
Means of z-scores of the sum of independent observer ratings of child negative affective valence during the structured task and the play parent-child interactions (residualized for age and sex) in the Year 1 assessment among children in the four quartiles of the distribution of negative emotionality as rated by adult caretakers during the Year 6 assessment in Study 3.
Figure 2.
Means of z-scores of the proportion of caretaker commands to which the child complied coded by independent raters during the structured task and the play parent-child interactions (residualized for age and sex) in the Year 1 assessment among children in the four quartiles of the distribution of prosociality as rated by adult caretakers during the Year 6 assessment in Study 3.
Forbidden toy task
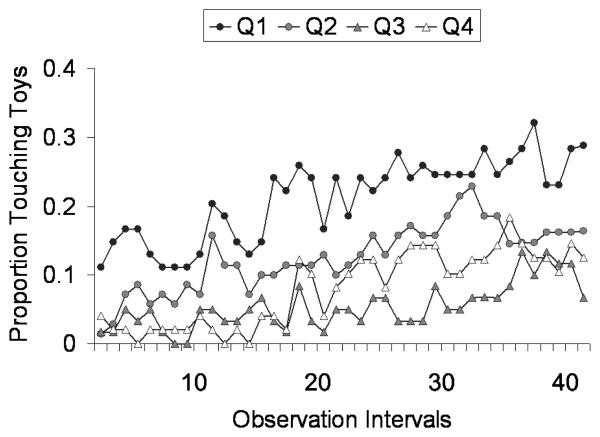
As reported in Table 4 and Figure 3, children who received lower caretaker ratings on prosociality were observed to touch the forbidden toys more often over time, but the other dispositional dimensions were not significantly related to this form of noncompliance.
Figure 3.
The proportion of children touching the forbidden toys during each interval in the Forbidden Toy Task coded by independent observers among children in four groups in Study 3. The four groups were based on quartiles of the sample distribution of caretaker ratings of prosociality during Year 6.
Unintentional injuries
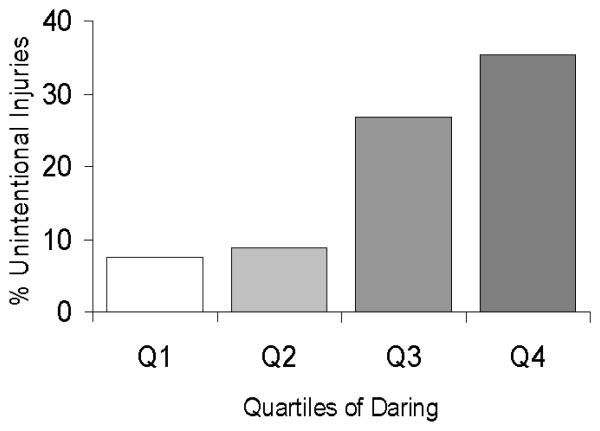
As reported in Table 4 and Figure 4, there was a significant relation between caretaker ratings of daring and the caretaker's report of unintentional injuries five years earlier, but the other dispositional dimensions were not significantly related to injuries.
Figure 4.
Percent of children reported by adult caretakers during the Year 1 assessment to have ever experienced a nontrivial unintentional injury attributed to the child's behavior among children in the four quartiles of the distribution of daring as rated by adult caretakers during the Year 6 assessment in Study 3.
DISCUSSION
The results of the EFA and CFA of the CADS using data from separate studies provided strong support for the internal validity of the CADS. That is, they support the hypothesis that the three CADS dispositions are defined by the items specified in the model and are sufficiently independent to be considered separate dimensions. Furthermore, the test-retest reliability of each CADS dimension was consistently high, indicating that each disposition can be measured reliably using adult caretaker respondents. Before the CADS dimensions can be said to measure the theoretical constructs they were developed to operationalize, however, it is necessary to test their external validity. This will require many studies using a variety of criterion variables, but a number of measures obtained in Studies 1 and 3 provided useful initial tests of the external validity of the CADS. As predicted by the model, each dispositional dimension accounted for unique variance in CD, when controlling for the other dispositional dimensions and demographic covariates. This both provides initial support for the validity of the CADS and constitutes a crucial first test of the model. That is, the developmental propensity model would have been disconfirmed had the three dispositions not been significantly associated with CD as predicted.
The significant 3-way interactions among the dispositional dimensions in their associations with both caretaker and youth ratings of CD symptoms are important for further articulation of the model. Not only was the level of CD symptoms reported by each informant highest in those youth who were simultaneously high in negative emotionality, low in prosociality, and high in daring, the degree to which this was the case exceeded the additive combination of the separate associations of each dispositional dimension with CD. This indicates that a complete model of the role of emotional dispositions in CD must consider the possibility that the three emotional dispositions work together interactively to influence risk for CD, rather than simply being three separate dispositional constructs that are each related to CD. This is one important reason why it is very important to include all three dispositional dimensions in an integrated developmental propensity model, such as the one that we have proposed.
The developmental propensity model also offers hypotheses regarding the comorbidity of CD with other forms of psychopathology. In particular, the model hypothesizes that CD tends to co-occur with other disruptive behavior disorders and with emotional disorders partly because they are all etiologically related to negative emotionality. Consistent with this hypothesis, caretaker ratings of negative emotionality were found to be robustly associated with ODD, depression, and anxiety symptoms according to both caretaker and youth reports of symptoms.
The model also predicts differences in associations between dispositions and each form of psychopathology that limit comorbidity. For example, as predicted by the model, prosociality was found to be more strongly associated with CD than with ODD, depression, or anxiety. Importantly, when CD was controlled to reduce concerns about comorbidity, prosociality was found to be significantly related to depression and anxiety in the opposite direction as prosociality was significantly related to CD. Furthermore, as predicted, daring was positively related to CD and ODD, but inversely related to anxiety. These significant differences in the magnitudes of associations of the CADS dimensions with different forms of psychopathology provide evidence for the discriminant validity of the CADS dimensions.
Although the present findings are consistent with the model's predictions regarding comorbidity, it should be noted that the hypotheses regarding comorbidity were not formally tested in the present paper. For example, in the future, it will be important to test the hypothesis that youth with CD who are higher in negative emotionality will be more likely also to meet criteria for comorbid mental disorders. Similarly, it would be useful to test the hypothesis that youth with CD who are higher in daring will be less likely also to meet criteria for an anxiety disorder.
Other initial tests of the external validity of the CADS dispositional dimensions were conducted using measures available in Study 3 as criterion variables. Each CADS dimension was found to be uniquely related to at least one relevant measure of affect or behavior coded by observers who were unaware of the caretaker's dispositional ratings of the child. Caretaker ratings of negative emotionality, but not the other CADS dimensions, were significantly related to observer ratings of child negative affective valence during parent-child interactions. Similarly, only the CADS dimension of prosociality was positively related to child compliance with adult commands during the mother-child interaction task and inversely to not complying with the prohibition against touching the forbidden toys.
These initial findings on the external validity of the CADS in Study 3 are encouraging partly because common method variance is a key threat to the external validity of studies of relations between dispositions and psychopathology when ratings of both constructs are completed by the same informant. Consider a parent who is asked if her daughter “gets upset easily,” “cares about the feelings of others,” and “likes things that may be dangerous.” The mother may answer these questions by thinking about her daughter's frequent fighting. Even if there is evidence to the contrary in the girl's behavior, the salience of her fighting could lead the mother to infer that her daughter is easily upset, unconcerned about others, and likes dangerous situations—based on the mother's implicit theory of the characteristics of girls who fight. Fortunately, the independent direct observations of child behavior used in Study 3 were not subject to such potential biases. Similarly, it is helpful that the associations between caretaker ratings of the dispositions and youth reports of CD and other forms of psychopathology were not subject to this bias.
The external validity of daring was further supported by the finding that caretaker reports of unintentional injuries to the child that were attributed to the child's behavior were independently related to caretaker ratings on daring obtained five years later. This criterion variable has the advantage of good face validity, but was measured by questioning the same informant that later rated the child's dispositions.
Limitations
Although these initial tests of the internal and external validity of the CADS are encouraging, some important limitations in the present tests of external validity should guide future research. Although it is informative to demonstrate that the three CADS dispositional dimensions are each independently associated with CD and other forms of psychopathology in cross-sectional analyses, the most important predictions of the developmental propensity model require prospective tests. This is because a key goal of the model is to identify young children who are at very high risk for CD and comorbid disorders before they exhibit serious CD behaviors. Therefore, longitudinal studies beginning in the preschool years will provide rigorous tests of the hypotheses that (1) young children who are high in negative emotionality, low in prosociality, and high daring are at increased risk for developing CD across childhood and adolescence, (2) the development of comorbid disorders over time also will be predicted by the dispositional measures in early childhood as specified in the model, and (3) environmental factors during the course of development, such as coercive parent-child relationships, low levels of supervision, and deviant peer associations, will interact with the child's emotional dispositions to determine which predisposed young children will develop CD.
Although the developmental propensity model includes hypotheses regarding the comorbidity of CD with emotional disorders, the CADS is not intended to provide a complete measure of all dispositions related to emotional disorders. The CADS was developed to understand CD and the dispositional dimensions may be defined in ways that are less relevant to depression and anxiety. In addition, other dispositional constructs also may be relevant to depression and anxiety that are not related to CD (Clark et al., 1994). It should be noted that the CADS dispositions are almost certainly not the only source of comorbidity between CD and emotional disorders. For example, there is emerging evidence that CD may be comorbid with depression partly through environmental processes. For example, youth who engage in high levels of CD behaviors tend to generate negative life events such as peer rejection and incarceration, which increase their risk for future depression (Burke, Loeber, Lahey, & Rathouz, 2005; Capaldi, 1992). Thus, a complete account of comorbidity between CD and depression will need to incorporate shared emotional dispositions, linked environmental influences, and other factors.
The initial tests of external validity that were conducted in Study 3 were encouraging, but limited in two ways. First, although the existing measures used in Study 3 that were selected as external criterion variables were appropriate for that purpose, additional tests will be needed that use observational measures specifically developed or selected for that purpose. For example, observational measures of sympathetic response to distress and cooperative sharing would provide strong tests of the external validity of prosociality. Other predictions could be directly tested in studies that could determine if individual differences in prosociality are related to variations in the strength of social reinforcers. Second, because Study 3 was designed to test the validity of ADHD in young children, that sample could be biased in ways that threaten the tests of validity of the CADS. Third, Study 3 was not ideal because the criterion measures were obtained during the initial assessment, but the dispositions were not measured until 6 years later. In some ways, the association between the CADS dimensions and the criterion measures over 5 years is impressive, but a prospective study in which dispositional measures were obtained at the youngest age would provide a stronger test. This is partly because caretaker ratings of dispositions are likely influenced by their observations of their child's behavior at younger ages. The congruence analyses in Study 1 suggest that the three emotional dispositions measured by the CADS are invariant in factor structure across sex and age, even though there are mean sex differences in prosociality and sex and age differences in daring. It will be important for future studies to continue to evaluate the validity and usefulness of the CADS across these and other demographic groups, however.
It should be noted that the developmental propensity model is intended to be integrative, but is not necessarily a complete model of CD. For example, although much of what is meant by the construct of “impulse control” may be captured by the three dispositions and measures of cognitive ability, it is possible that impulse control constitutes yet another independent dimension of antisocial propensity that would be needed in a truly comprehensive model of CD. The same holds for other dispositional constructs not addressed in this paper.
Implications for Future Research, Policy, and Practice
The CADS will allow empirical tests of a new psychological model of conduct disorder (Lahey & Waldman, 2003). If prospective longitudinal studies support the model, that would suggest that interventions designed to modify the three dispositions should be tested to reduce rates of CD. Alternatively, it could be more fruitful to test interventions designed to reduce the frequency with which predisposed young children develop or persist in CD.
The CADS model may also help clinicians understand the heterogeneity of CD. Future studies should examine two key aspects of the hypotheses regarding the heterogeneity of CD. First, because the three dispositions are only modestly correlated, one implication is that groups of youth who are deviant only in negative emotionality, only in prosociality, and only in daring would each be at risk for CD, but for different reasons. It will be important, therefore, to determine if such groups differ in their specific antisocial behaviors, comorbid conditions, and other characteristics. These possibilities would need to be addressed using analyses of profiles of dispositions that are beyond the scope of this paper, however. Such future tests would be important because the significant 3-way interaction among the dispositions in their association with CD could mean that the model will not facilitate understanding heterogeneity in CD. This is because the 3-way interaction raises the possibility that only youth who are deviant on all three dispositions are at increased for CD.
Future studies also could test the hypothesis that the three dispositional dimensions might help understand the rather different form of heterogeneity revealed in developmental trajectories. The model hypothesizes that the three dispositions are far more strongly associated with childhood-onset than adolescent-onset antisocial behavior. Nonetheless, the three childhood dispositions are hypothesized to inversely predict to some extent which well-behaved children will not engage in adolescent-onset antisocial behavior. Again, these hypotheses can only be tested prospectively.
It also should be noted that the other dispositional models may prove to be as useful or more useful than the CADS model in understanding CD. For example, several traits in the five-factor model of adult personality have been found to be correlated with adult antisocial personality disorder and psychopathy (Lynam, 2002). Only direct empirical tests can determine if a downward extension of the five-factor model would be more useful than the CADS in research on CD, but three potentially important limitations of the five-factor approach for this purpose should be noted. First, the items used to measure the five-factor model dimensions in the NEO (Costa & McCrae, 1987) include synonyms and antonyms of symptoms of psychopathology, which could contaminate tests of associations with CD. Second, a number of studies have shown that, unlike the CADS, the supposed factor structure of the NEO in adults is not supported by confirmatory factor analysis (Gignac, Bates, & Jang, 2007). The same lack of support using confirmatory factor analysis has been found for a five-factor model measure developed for children and adolescents (Barbaranelli, Caprara, Rabasca, & Pastorelli, 2003). Third, only some groups of items (facets) among the five-factor model items are strongly related to antisocial behavior (Lynam, 2002).
Table 2.
Fit Statistics and Comparisons of Alternative Models of the Latent Structure of the Investigational Child and Adolescent Dispositions Scale Using Confirmatory Factor Analysis for Each Member of 6- through 17-Year-Old twin Pairs, Randomly Designated as “Twin 1” or “Twin 2” in Study 2.
| Alternative models | Twin | d.f. |
Satorra- Bentler χ2 |
NFI | RMR | AIC | RMSEA (90% C.I.) |
Scaled Δ χ2a |
d.f. |
|---|---|---|---|---|---|---|---|---|---|
| One factor | 1 | 299 | 8801 | .80 | .11 | 8905 | .13 (.12 - .13) | 4804* | 3 |
| 2 | 299 | 9206 | .76 | .089 | 9310 | .13 (.13 - .13) | 6836* | 3 | |
| Three factors (orthogonal) | 1 | 299 | 3104 | .91 | .077 | 3208 | .072 (.070-.075) | 278* | 3 |
| 2 | 299 | 3128 | .89 | .069 | 3232 | .072 (.070-.075) | 220* | 3 | |
| Three factors (correlated) | 1 | 296 | 2825 | .91 | .056 | 2935 | .069 (.067 - .071) | Reference model | |
| 2 | 296 | 2894 | .90 | .052 | 3004 | .070 (.068 - .072) | Reference model |
All model Satorra-Bentler χ2 tests significant at p < .0001.
p < .0001.
Compared to the correlated 3-factor structure for the same twin.
Note: NFI = normed fit index; RMR = root mean square residual; AIC = Akaike's Information Criterion; RMSEA = root mean square error of approximation. After deletion of participants with missing data on any caretaker-rated CADS items, N = 1,799 for “twin 1” and N = 1,804 for “twin 2.”
Acknowledgements
The present studies and analyses were supported by National Institute of Mental Health grants U01-MH54281, R01-MH59111, and R01-MH53554 to Benjamin B. Lahey and K01-MH01818 to Irwin D. Waldman. The senior author is grateful to Jon Shaw for engendering an interest in the key role played by empathy in the development of child and adolescent conduct disorder and to Nancy Eisenberg for our discussions of the importance of sympathy.
References
- Angold A, Costello EJ, Erkanli A. Comorbidity. Journal of Child Psychology and Psychiatry. 1999;40:57–87. [PubMed] [Google Scholar]
- Barbaranelli C, Caprara GV, Rabasca A, Pastorelli C. A questionnaire for measuring the Big Five in late childhood. Personality and Individual Differences. 2003;34:645–664. [Google Scholar]
- Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- Brown MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Burns GL, Patterson DR. Normative data on the Eyberg Child Behavior Inventory and Sutter-Eyberg Student Behavior Inventory Parent and Teacher Rating Scales of disruptive behavior problems in children and adolescents. 2001;23:15–28. [Google Scholar]
- Capaldi DM. Co-occurrence of conduct problems and depressive symptoms in early adolescent boys: II. A 2-year follow-up at grade 8. Development and Psychopathology. 1992;4:125–144. doi: 10.1017/s0954579499001959. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D, Mineka S. Temperament, personality, and the mood and anxiety disorders. Journal of Abnormal Psychology. 1994;103:103–116. [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO. Psychological Assessment Resources; Odessa, FL: 1987. [Google Scholar]
- Costello EJ, Mustillo S, Erkanli A, Keeler G, Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Archives of General Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Dadds MR, Fraser J, Frost A, Hawes DJ. Disentangling the underlying dimensions of psychopathy and conduct problems in childhood: A community study. Journal of Consulting and Clinical Psychology. 2005;73:400–410. doi: 10.1037/0022-006X.73.3.400. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Miller PA, Schaller M, Fabes RA, Fultz J, Shell R, et al. The role of sympathy and altruistic personality traits in helping: A reexamination. Journal of Personality. 1989;57:41–67. doi: 10.1111/j.1467-6494.1989.tb00760.x. [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Funderburk BW, Hernbree-Kigin TL, McNeil CB, Querido JG, Hood KK. Parent-child interaction therapy with behavior problem children: One and two year maintenance of treatment effects in the family. Child and Family Behavior Therapy. 2001;23:1–20. [Google Scholar]
- Farrington DP, West DJ. Criminal, penal and life histories of chronic offenders: Risk and protective factors and early identification. Criminal Behaviour and Mental Health. 1993;3:492–523. [Google Scholar]
- Frick PJ, Bodin SD, Barry CT. Psychopathic traits and conduct problems in community and clinic-referred samples of children: Further development of the Psychopathy Screening Device. Psychological Assessment. 2000;12:382–393. [PubMed] [Google Scholar]
- Frick PJ, Stickle TR, Dandreaux DM, Farrell JM, Kimonis ER. Callous-unemotional traits in predicting the severity and stability of conduct problems and delinquency. Journal of Abnormal Child Psychology. 2005;33:471–487. doi: 10.1007/s10648-005-5728-9. [DOI] [PubMed] [Google Scholar]
- Gignac GE, Bates TC, Jang KL. Implications relevant to CFA model misfit, reliability, and the five-factor model as measured by the NEO-FFI. Personality and Individual Differences. 2007;43:1051–1062. [Google Scholar]
- Glorfeld LW. An improvement on Horn's parallel analysis methodology for selecting the correct number of factors to retain. Educational and Psychological Measurement. 1995;55:377–393. [Google Scholar]
- Goodman R, Ford T, Simmons H, Gatward R, Meltzer H. Using the Strengths and Difficulties Questionnaire (SDQ) to screen for child psychiatric disorders in a community sample. International Review of Psychiatry. 2003;15:166–172. doi: 10.1080/0954026021000046128. [DOI] [PubMed] [Google Scholar]
- Hart EL, Lahey BB, Loeber R, Hanson KS. Criterion validity of informants in the diagnosis of disruptive behavior disorders in children: A preliminary study. Journal of Consulting and Clinical Psychology. 1994;62:410–414. doi: 10.1037/0022-006X.62.2.410. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Evaluating model fit. In: Hoyle RH, editor. Structural equation modeling: Concepts, issues and applications. Sage; Newbury Park, CA: 1995. [Google Scholar]
- Lahey BB, Applegate B, Waldman ID, Loft JD, Hankin BL, Rick J. The structure of child and adolescent psychopathology: Generating new hypotheses. Journal of Abnormal Psychology. 2004;113:358–385. doi: 10.1037/0021-843X.113.3.358. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS, et al. Three-year predictive validity of DSM-IV attention deficit/hyperactivity disorder in children diagnosed at 4-6 years of age. American Journal of Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- Lahey BB, Waldman ID. A developmental propensity model of the origins of conduct problems during childhood and adolescence. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. Guilford Press; New York: 2003. pp. 76–117. [Google Scholar]
- Lahey BB, Waldman ID. A developmental model of the propensity to offend during childhood and adolescence. In: Farrington DP, editor. Advances in criminological theory. Vol. 13. Transaction Publishers; Piscataway, N. J.: 2005. pp. 15–50. [Google Scholar]
- Lynam DR. Psychopathy from the perspective of the five-factor model of personality. In: Costa PT, Widiger TA, editors. Personality disorders and the five-factor model of personality. 2 ed. American Psychological Association; Washington, DC: 2002. pp. 325–348. [Google Scholar]
- Mariani MA, Barkley RA. Neuropsychological and academic functioning in preschool boys with attention deficit hyperactivity disorder. Developmental Neuropsychology. 1997;13:111–129. [Google Scholar]
- Mischel W. Toward an integrative science of the person. Annual Review of Psychology. 2004;215:1–22. doi: 10.1146/annurev.psych.55.042902.130709. [DOI] [PubMed] [Google Scholar]
- Nottelmann ED, Jensen PS. Comorbidity of disorders in children and adolescents: Developmental perspectives. In: Ollendick TH, Prinz RJ, editors. Advances in Clinical Child Psychology. Vol. 17. Plenum; New York: 1995. pp. 109–155. [Google Scholar]
- O'Connor BP. SPSS, SAS, and MATLAB programs for determining the number of components using parallel analysis and Velicer's MAP test. Behavior Research Methods, Instruments, and Computers. 2000;32:396–402. doi: 10.3758/bf03200807. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Reid JB, Dishion TJ. Antisocial boys. Castalia; Eugene, OR: 1992. [Google Scholar]
- Roberts MA. A behavior observation method for differentiating hyperactive and aggressive boys. Journal of Abnormal Child Psychology. 1990;18:131–142. doi: 10.1007/BF00910726. [DOI] [PubMed] [Google Scholar]
- Rummel RJ. Applied factor analysis. Northwestern University Press; Evanston: 1970. [Google Scholar]
- Russo MF, Stokes GS, Lahey BB, Christ MAG, McBurnett K, Loeber R, et al. A sensation seeking scale for children: Further refinement and psychometric development. Journal of Psychopathology and Behavioral Assessment. 1993;15:69–86. [Google Scholar]
- Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone KE, Burrell L, Higman SM, McFarlane E, Fuddy L, Sia C, et al. Agreement of injury reporting between primary care medical record and maternal interview for children aged 0-3 years: Implications for research and clinical care. Ambulatory Pediatrics. 2006;6:91–95. doi: 10.1016/j.ambp.2005.10.003. [DOI] [PubMed] [Google Scholar]
- Thorndike RL, Hagen EP, Sattler JM. Stanford-Binet intelligence scale. fourth ed. Riverside; Chicago: 1986. [Google Scholar]
- Waldman ID, Singh AL, Lahey BB. Dispositional dimensions and the causal structure of child and adolescent conduct problems. In: Krueger RF, Tackett JL, editors. Personality and psychopathology. Guilford Press; New York: 2006. pp. 112–152. [Google Scholar]
- Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]