Abstract
Purpose: To examine knowledge about hereditary breast and ovarian cancer (HBOC) among Mexican, Puerto Rican, and Cuban women. Methods: Women (age range, 18–65 years) with a personal or family history of breast or ovarian cancer were recruited to a mixed methods study using community-based approaches. Fifty-three women participated in the study: 16 Mexicans, 20 Puerto Ricans, and 17 Cubans. The majority of women (64.2%) were born outside the United States. All questions were interviewer administered in Spanish or English. HBOC knowledge was measured using an 11-item instrument developed by the National Center for Human Genome Research. We evaluated whether differences in knowledge varied as a function of Hispanic subethnicity, demographic characteristics, and medical and acculturation characteristics using a series of one-way analysis of variances. Results: The percentage of correct responses on the knowledge instrument ranged from 9.4% to 73.6% (median number of correct responses = 45%). Knowledge did not significantly differ by Hispanic subethnicity (p = 0.51). Exploratory analysis revealed lower knowledge in women with a personal history of cancer (p = 0.03). Conclusion: Our study provides important information about characteristics associated with lower levels of knowledge and specific areas related to HBOC where additional education may be warranted in the Hispanic community.
Introduction
Approximately 44.3 million Hispanics live in the United States, making them the largest and fastest growing minority group in the United States (U.S. Census Bureau 2006). Hispanics are a diverse population with individuals from multiple origins such as the Caribbean, Central or South America, and Spain (U.S. Census Bureau, 2000). The majority of the U.S. Hispanic population are of Mexican, Puerto Rican, and Cuban origin (Ramirez and de la Cruz, 2003). Among Hispanic women, breast cancer is both the most commonly diagnosed cancer and the leading cause of cancer-related death, with higher rates in Cubans followed by Mexicans (O'Brien et al., 2003; Howe et al., 2006; American Cancer Society I, 2008). Although Hispanic women are less likely to be found to have breast cancer and ovarian cancer than non-Hispanic whites, they are more likely to be found to have nonlocalized disease, resulting in poorer prognosis and survival (O'Brien et al., 2003; Howe et al., 2006). Later stage of diagnosis may be partially associated with less knowledge, access, and utilization of cancer preventive services (Bentley et al., 1998).
An emerging area of disparity that may be associated with later stage of diagnosis within the Hispanic community is in access to and the use of breast cancer genetic counseling and testing services. Women who carry a BRCA1 or BRCA2 (BRCA) mutation have a 43–87% lifetime risk of breast cancer and 27–44% for ovarian cancer (American Medical Association, 2001; Vogel et al., 2007). Breast cancer patients with a BRCA mutation are also at substantially increased risk of contralateral breast cancer and ovarian cancer compared with women without a BRCA mutation (Metcalfe et al., 2004; Brekelmans et al., 2007). Several recent studies have documented the presence of BRCA mutations in Hispanic women (Mullineaux et al., 2003; Weitzel et al., 2005, 2007). Recently, a population-based study from the Northern California Cancer Registry reported that Hispanic breast cancer patients had higher BRCA1 mutation prevalence rates compared with non-Ashkenazi Jewish Whites, African Americans, and Asian Americans (John et al., 2007). Thus, genetic counseling and testing for BRCA mutations is an important way to identify those women most likely to benefit from early detection and prevention strategies to minimize morbidity and mortality from BRCA-associated cancers across the cancer prevention to survivorship continuum.
However, recent data suggest that despite increased risks for carrying BRCA mutations, Hispanics are currently underutilizing cancer genetic services. Leading health organizations have established referral criteria to assess the risk of hereditary breast and ovarian cancer (HBOC) by a cancer genetics professional (American Medical Association, 2002; Hampel et al., 2004; Nelson et al., 2005; Daly et al., 2009). These guidelines recommend referral for women who have bilateral breast cancer, have both breast and ovarian cancer, have a family history that includes a clustering of breast and/or ovarian cancers, have a previously identified mutation in the family, and/or are found to have early-age-onset breast cancer (age ≤50) (Daly et al., 2009). Despite available guidelines and efforts to increase awareness (Ricker et al., 2009), utilization of BRCA counseling and testing among Hispanic women remains low (Chen et al., 2002; Ricker et al., 2006; Hall et al., 2009). In a national study of 46,276 patients who received genetic testing for BRCA1/2 (BRCA) mutations in community-based (nonacademic research) settings between the years of 1996 and 2006, only 4% (n = 1936) were of Hispanic origin (Hall et al., 2009). This low rate of utilization is particularly concerning in light of recent data suggesting that Hispanic women have among the highest prevalence rates of BRCA1 mutations compared with women from other racial ethnic groups (John et al., 2007).
While review papers and reports emphasize the need for and use of genetic counseling and testing services in the Hispanic community (Penchaszadeh, 2001; Ramirez, 2003; Doksum et al., 2004), there is less empirical data about factors that may contribute to utilization of these services. An underlying factor that may contribute to low utilization of breast cancer genetic counseling and testing services among Hispanic women may be knowledge. Without knowledge about basic concepts related to HBOC such as the prevalence, patterns of inheritance, associated cancer risks, and risk management options, it would be difficult for women to make informed choices about whether to seek cancer genetics services (Schwartz et al., 2001). Previous studies have examined awareness about availability of or interest in genetic testing for BRCA mutations among Hispanic women (Ramirez et al., 2006; Lacour et al., 2008). Some studies also indicate that awareness of genetic testing varies by Hispanic subethnicities (Vadaparampil et al., 2006; Heck et al., 2008). Therefore, it is also possible that knowledge about HBOC will also vary among Hispanic subethnic groups. A limited number of studies have addressed knowledge about basic concepts related to HBOC (e.g., pattern of inheritance pattern, cancer risks, and mutation prevalence) (Strecker et al., 2002; Katapodi and Aouizerat, 2005). However, none have examined knowledge in a multiethnic group of Hispanic women with a personal or family history of cancer suggestive of HBOC. The purpose of this exploratory study was to examine knowledge about HBOC among Mexican, Puerto Rican, and Cuban women with a personal or family history of breast cancer before the age of 50 or ovarian cancer at any age.
Materials and Methods
Design and setting
A cross-sectional design using mixed qualitative and quantitative research methods was employed. Eligible consenting subjects participated in a semistructured in-depth qualitative interview followed by a brief battery of structured quantitative survey items for descriptive and exploratory purposes. Therefore, the sample size was based on estimates of the number needed for qualitative saturation (Kvale, 1996; Guest et al., 2006), rather than on statistical power calculations. Participants were recruited after the project received appropriate Institutional Review Board approvals, and each participant provided written informed consent before participation. This article focuses on the results from the quantitative survey.
Participant recruitment and data collection
Eligible participants were Hispanic women who (a) were between 18 and 65 years of age; (b) self-identified as Mexican, Puerto Rican, or Cuban; (c) had a personal diagnosis of breast cancer before age 50 or ovarian cancer at any age or had at least one first-degree relative (mother, sister, daughter) found to have breast cancer before age 50 or at least one first-degree relative ovarian cancer at any age; and (d) had not previously had genetic counseling and/or genetic test for hereditary cancer. Participants were recruited from the Tampa Bay area between May 2006 and September 2008 through various community-based approaches, including (1) local health department clinics serving a large Hispanic population; (2) posting and in person distribution of flyers at Hispanic-owned businesses and organizations; (3) attending Hispanic health fairs and food pantries; (4) attendance at a local Hispanic breast cancer support group meeting; (5) attendance at local medical clinics affiliated with the cancer center; and (6) press releases to local English and Spanish media outlets. Active recruitment efforts were facilitated by a team of three bilingual–bicultural trained research assistants. For the health department, local medical clinics, Hispanic health fairs, and Hispanic food pantries, these active recruitment methods involved at least two research assistants setting up a table at the particular venue (e.g., waiting room of the health department), passing out flyers and promotional items (e.g., sun screen, lip balm, and snacks), and answering questions for and prescreening potential participants. For the most part, the research assistants had to take a proactive role to create rapport with the participants (e.g., smiling, making eye contact with participants, and verbally encouraging participants to come to the table). For some of the health fairs, food pantries, and all of the support groups, the research assistants were provided a brief time slot during a scheduled group meeting or event to present the study. Before the recruitment day, arrangements were made with the contact person at each location for a private room in which to consent patients and conduct on-site interviews. If a woman stated that she was unable to complete the interview at that time, the research assistants obtained their name and contact information and followed up to schedule an interview at convenient time and location. Passive recruitment efforts generally involved posting of a flyer or providing a press release with a brief description and purpose of the study, basic eligibility criteria, and a telephone number for prospective participants to call with questions or to express interest in the study. Eligible, consenting individuals were interviewed in-person at a location selected by the participant. All questions were interviewer administered in Spanish or English based on the participant's language preference. The research assistant read all study materials aloud to the respondents to minimize literacy issues. The interview (both the qualitative and quantitative portions) required approximately 1 h in total to complete. At the end of the interview, participants received a $40 honorarium.
Translation of study materials
The primary instrument for the proposed study was an 11-item knowledge scale developed by the National Center for Human Genome Research (NCHGR) Cancer Genetic Studies Consortium (Lerman et al., 1997). The NCHGR scale is not available in Spanish. Therefore, a multistep approach was used to develop Spanish translations. First, the instrument was forward translated and back translated by two bilingual–bicultural members of the study team. Any back-translated issues were discussed and resolved by a certified Spanish language translator. Once the Spanish language instrument was developed, it was reviewed by a national panel of 10 fully bilingual–bicultural experts representing several Hispanic ethnicities. The panel had extensive experience in the areas of cancer genetics outreach and education (n = 2), medical genetics (n = 2), and cancer genetic counseling (n = 3). In addition, Hispanic consumer reviewers who had previously undergone genetic counseling for HBOC were included (n = 3). Four panel members were mailed the NCHGR scale and asked to rate the instructions and items for content, clarity, and acceptability to Hispanic women. All panel and study team members then participated in a conference call to discuss results. Each suggestion was discussed until consensus (greater than 50% of panelists agreed) was reached. Table 1 summarizes the words that were discussed, the alternative suggestions, and the final decision by the panel. Interestingly, although there was much discussion regarding several of the words used, ultimately, the original words identified during the initial translation process were the ones used in the final version of the instrument. The final version of the instrument was then pilot tested with five additional women meeting study criteria.
Table 1.
Results of Translation/Back Translation and Expert Panel Review of National Center for Human Genome Research Knowledge Scale Items
| Question no. | Original English word | Translation by study team | Back translation by study team and medical translator | Words/phrases discussed by expert panel |
|---|---|---|---|---|
| Introduction | Chance | Riesgo | Risk | Probabilidad (Probability) Chance (Chance) Posibilidad (Possibility) Riesgo (Risk) |
| 1 | Altered | Alterado (modificado) | Changed (Modified) | Cambiado (Changed) Alterado (Altered) Modificado (Modified) |
| 4 | Removed | Remover | Removing | Quitar (Take Off ) Extirpar (Extract) Remover (Remove) |
| 7 | Spreads | Regado | Spreads | Esparcido (Scattered) Extendido (Extended) Ha ido a otra parte (Has gone to another part) Regado (Spread) |
| 11 | Breasts removed | Una mujer que se ha removido los senos | Breasts removed | Extirpado (Eradicate) Se le han quitado (She had taken off ) Una mujer que se ha removido los senos (A woman who has had her breasts removed) |
Boldface words indicate final Spanish words used.
Measures
Sociodemographic and medical characteristics
The following sociodemographic and medical characteristics were assessed via a self-report questionnaire: age (<24, 25–34, 35–50, 51–65); ethnicity (Cuban, Mexican, Puerto Rican), marital status (currently married/living with someone/never married/separated/divorced/widowed); have children (yes, no); education (<high school, high school, some college, college graduate, or beyond); employment status (full time/part time or retired/disabled/unemployed); insurance status (public insurance, no insurance, other), religion (Catholic, Christian, other); income (<$20,000; $20,001–$40,000, >$40,000); personal history of breast below the age of 50 (yes, no); personal history of ovarian cancer (yes, no); first-degree relative (i.e., mother, sister, or daughter) with of breast cancer below the age of 50 (yes, no); and first-degree relative (i.e., mother, sister, or daughter) with of ovarian cancer (yes, no).
Acculturation characteristics
Acculturation characteristics included having been born in the United States (yes, no), time in the United States (<1, 1–5, 6–10, ≥11 years), and English language preference. English language preference was assessed using an eight-item scale of language preference from the Year 2000 National Health Interview Survey. The entire National Health Interview Survey was translated and back translated in a multistep process and is described in detail elsewhere (Vadaparampil et al., 2006). English language preference (low, medium, high) was quantified based on responses to eight questions concerning language. These questions were phrased in the form, “(In) Which language”: (1) “do you speak?” (2) “did you use as a child?” (3) “do you read better?” (4) “do you usually speak at home?” (5) “do you usually speak with your friends?” (6) “do you usually think?” (7) “are the T.V. programs you usually watch?” (8) “are the radio programs you usually listen to?” Responses were reported on a Likert (1–5) scale with categories “Only Spanish,” “More Spanish than English,” “Spanish and English about the same,” “More English than Spanish,” and “Only English.” Similar to previous studies using these items (Berrigan et al., 2006; Vadaparampil et al., 2006), respondents were classified by language preference tertile. Summed scores of 8–13 were classified as low English language preference, scores of 14–27 as medium English language preference, and scores of 28–40 as high English language preference (Cronbach's α = 0.95).
Knowledge
Knowledge is the primary outcome variable of the study and was measured with an 11-item instrument developed by the NCHGR Cancer Genetic Studies Consortium, to measure knowledge in studies of women at risk for HBOC (Lerman et al., 1996, 1997; Hopwood et al., 2001). The NCHGR scale measures four aspects of HBOC genetics knowledge: (1) prevalence of the BRCA gene mutations; (2) patterns of inheritance; (3) cancer risks associated with BRCA mutations; and (4) risk management options for women with a BRCA mutation. All items were scored as 1 if the respondent provided the correct answer and 0 if they gave an incorrect or don't know response. This allowed for the calculation of an overall knowledge score that could range from 0 to 11.
Data analysis
In this descriptive study, we first examined the distribution of correct responses on the knowledge questionnaire and evaluated whether differences in knowledge varied as a function of demographic, medical, and cultural characteristics using a series of one-way analysis of variance with knowledge as the outcome variable. All tests were two-sided and declared significant at the 5% level. No multiple comparisons adjustment were considered due to the exploratory nature of this study.
Results
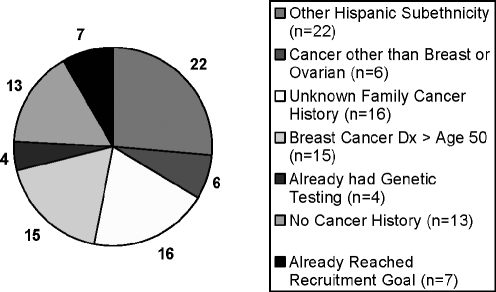
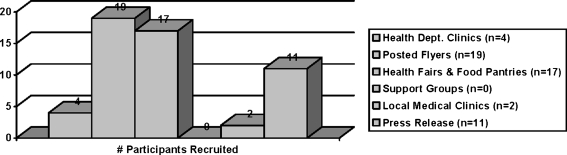
One hundred forty-three women were prescreened for participation in the parent research study in a period of 8 months. Eighty-three women were ineligible to participate in the study. As shown in Figure 1, the most common reasons for ineligibility included being of another Hispanic subethnicity, not knowing the personal or family cancer history type, and being found to have breast cancer after the age of 50. Of the 60 eligible women, 7 women scheduled an interview, but did not attend, resulting in a total of 53 study participants. As shown in Figure 2, the majority of participants were recruited through flyers posted at local Hispanic businesses (n = 19) and by attending community events, including health fairs and food pantries (n = 17).
FIG. 1.
Reasons for ineligibility among prescreened women (n = 83).
FIG. 2.
Sources for participant recruitment (n = 53).
Demographic, medical, and cultural characteristics of the sample are shown in Table 2. The sample was approximately equally distributed across the age categories; the majority of respondents were married or living as married and had children. Educational attainment was split with one-third having not completed high school and one-third having a college degree. Approximately half of the sample was employed at least part time, one-third had no health insurance and endorsed the Catholic faith as their religion, and half of the sample had an income of at least $20,000 a year. In terms of medical characteristics, the majority of women had no personal history of breast or ovarian cancer, but had a first-degree relative with at least one of these cancers. Approximately two-thirds of the sample was not born in the United States, but approximately the same proportion of respondents had lived in the United States for at least 10 years. Approximately two-thirds of the sample had low to medium English language preference.
Table 2.
Sociodemographic, Medical, and Cultural Characteristics of Study Participants (n = 53)
| n (%) | |
|---|---|
| Sociodemographic characteristics | |
| Age | |
| <34 | 12 (23.5) |
| 35–44 | 17 (32.1) |
| 45–50 | 12 (22.6) |
| 51–65 | 11 (20.8) |
| Ethnicity | |
| Cuban | 17 (32.1) |
| Mexican | 16 (30.2) |
| Puerto Rican | 20 (37.7) |
| Marital status | |
| Married/living as married | 33 (62.3) |
| Single/never married/separated/divorced/widowed | 20 (37.7) |
| Have children | |
| Yes | 47 (88.7) |
| No | 6 (11.3) |
| Education | |
| <High school | 19 (35.8) |
| High school | 5 (9.4) |
| Some college | 11 (20.8) |
| College | 17 (32.1) |
| Employment status | |
| Full or part time | 29 (54.7) |
| Retired/disabled/unemployed | 23 (43.4) |
| Health insurance | |
| Public | 11 (21.2) |
| Other | 19 (35.8) |
| No insurance | 20 (37.7) |
| Religion | |
| Catholic | 24 (51.1) |
| Christian | 10 (21.3) |
| Other | 13 (27.7) |
| Income | |
| ≤$20,000 | 19 (35.8) |
| >$20,000–$40,000 | 13 (24.5) |
| >$40,000 | 15 (28.3) |
| Medical characteristics | |
| Personal history of breast cancer <age 50 | |
| Yes | 11 (21.2) |
| No | 41 (78.8) |
| Personal history of ovarian cancer | |
| Yes | 2 (3.8) |
| No | 50 (96.2) |
| FDR had breast cancer <age 50 | |
| Yes | 31 (64.6) |
| No | 17 (35.4) |
| FDR had ovarian cancer | |
| Yes | 25 (56.8) |
| No | 19 (43.2) |
| Acculturation characteristics | |
| Born in the United States | |
| Yes | 19 (35.8) |
| No | 34 (64.2) |
| Time in the United States | |
| <1 year | 3 (5.7) |
| 1–10 years | 15 (28.8) |
| ≥11 years | 34 (64.1) |
| English language preference (α = 0.95) | |
| Low | 15 (28.3) |
| Medium | 22 (41.5) |
| High | 16 (30.2) |
n for each variable may not equal 53 due to missing data; percentages may not add up to 100% due to rounding error.
FDR, first degree relative.
Table 3 shows the frequency of correct responses across the 11 items of the knowledge questionnaire. On average, respondents answered almost half of the items correctly (mean ± standard deviation, 5.15 ± 1.65). However, as shown in Table 4, there was considerable variability in the specific questions that were answered correctly. Women had the lowest levels of knowledge related to the prevalence of BRCA mutations. With respect to patterns of inheritance, the majority of women appeared to recognize paternal inheritance of and risks of inheriting a BRCA mutation among first-degree relatives. Similarly, the majority of women appeared to differentiate cancer risks for sporadic versus suspected hereditary cancer based on the presence of a mutation and age of onset. However, slightly less than half the respondents correctly answered the question related to penetrance of BRCA mutations. Finally, the majority of women appeared to recognize the residual risk of breast cancer after prophylactic surgery. Far fewer correctly answered questions related to risk management of ovarian cancer.
Table 3.
Frequency and Percentage of Women with Correct Responses on the Knowledge Scale
| Number of items correct | n | Sample (%) |
|---|---|---|
| 0–1 | 0 | 0 |
| 2 | 5 | 9.4 |
| 3 | 2 | 3.8 |
| 4 | 13 | 24.5 |
| 5 | 8 | 15.1 |
| 6 | 14 | 26.4 |
| 7 | 7 | 13.2 |
| 8 | 4 | 7.5 |
| 9–11 | 0 | 0 |
Percentages may not add up to 100% due to rounding error.
Table 4.
Percent Correct for Items from the National Center for Human Genome Research Cancer Genetics Studies Consortium Knowledge Scale
| Item | % correct |
|---|---|
| Prevalence | |
| 1 in 10 women has an altered breast cancer gene. (False) | 11.3 |
| One half of all breast cancer cases occur in women who have an altered breast cancer gene. (False) | 9.4 |
| Patterns of inheritance | |
| A father can pass down an altered breast cancer gene to his children. (True) | 66.0 |
| The sister of a woman with an altered breast cancer gene has a 50% risk of having the altered gene. (True) | 60.4 |
| Cancer risks | |
| A woman who does not have an altered breast cancer gene can still get breast or ovarian cancer. (True) | 73.6 |
| Early onset breast cancer is more likely due to an altered breast cancer gene than is late onset breast cancer. (True) | 64.2 |
| A woman who has an altered breast cancer gene has a higher ovarian cancer risk. (True) | 62.3 |
| All women who have an altered breast cancer gene get cancer. (False) | 49.1 |
| Risk management options | |
| A woman who has her breasts removed can still get breast cancer. (True) | 58.5 |
| Ovarian cancer screening tests often do not detect cancer until after it spreads. (True) | 35.8 |
| Having ovaries removed will definitely prevent ovarian cancer. (False) | 24.5 |
To examine whether overall knowledge varied as a function of the demographic, medical, and cultural characteristics listed in Table 2, we performed a series of one-way analysis of variances with knowledge as the outcome variable. Respondents with a personal history of breast cancer had significantly lower levels of overall knowledge compared to individuals with no personal history of breast cancer (mean ± standard deviation, 4.27 ± 1.62 vs. 5.46 ± 1.54, respectively; F[1, 50] = 5.11, p = 0.03).
Discussion
This is among the first studies to examine knowledge of specific aspects of HBOC among a multiethnic group of Hispanic women. Although no differences were found by ethnic subgroup, overall knowledge levels appear to be low with approximately half of respondents correctly answering at least 50% of the questions correctly. Our findings indicate no differences in overall knowledge by Hispanic subethnicity or by any sociodemographic, medical, or acculturation factors, with the exception of personal history of breast cancer diagnosed before the age of 50. While previous studies have documented the relationship of acculturation to awareness and familiarity with genetic testing (Vadaparampil et al., 2006; Sussner et al., 2009), fewer have conducted in depth evaluations of HBOC knowledge. Knowledge about risk factors for hereditary breast cancer in the general population of women, regardless of race or ethnicity, appear to be low (Katapodi and Aouizerat, 2005). While education has been found to be significantly associated with knowledge (Katapodi and Aouizerat, 2005), it is possible that our sample sizes in the various educational categories were too small to detect an association between education and HBOC knowledge.
Those women with a personal history of breast cancer had lower levels of overall knowledge about HBOC compared to those without such a history. While this issue has not been specifically examined among Hispanic women, previous studies suggest that women may not regard personal cancer history as a risk factor for HBOC. In a study of 95 African American breast cancer survivors at increased risk for HBOC, most women reported that they had the same or lower risk of developing breast cancer again compared with other women (53%) (Brewster et al., 2007). In a qualitative study of patients recently diagnosed with breast cancer referred for genetic counseling and testing, several women questioned why they received the referral given the lack of a family history of breast cancer (Vadaparampil et al., 2009). Yet, these women were appropriately referred based on their personal history of cancer based on established clinical guidelines (e.g., early age of onset and bilateral cancer) (Daly et al., 2009). It is important for women with a personal history of breast cancer, particularly like those women in our study with early onset breast cancer (i.e., diagnosed <age 50), to recognize the possibility of HBOC. Recognition of this risk may provide an important opportunity to self-identify and seek appropriate genetic counseling and testing services given that breast cancer patients with a BRCA1 or BRCA2 (BRCA) mutation are at substantially increased risk of contralateral breast cancer and ovarian cancer (∼30%; 10 years postdiagnosis) compared to women without a BRCA mutation (∼10%; 10 years postdiagnosis) (Metcalfe et al., 2004; Brekelmans et al., 2007). Patients with a BRCA mutation also have a 7–13% chance of developing ovarian cancer in the 10 years after diagnosis (Metcalfe et al., 2005). In addition, it is possible that for women who recently immigrate from other countries, it may be even more challenging to identify and document a complete family cancer history, given limited accesses to medical records and/or communication with family members. Thus, personal history may provide the only information upon which to base decisions related to genetic counseling and testing for HBOC.
The majority of women (i.e., ≥60%) correctly answered questions about specific features of HBOC, including the pattern of inheritance and associated cancer risks. In contrast, less than 40% of women correctly answered questions related to the prevalence of BRCA mutations and risk reduction options related to ovarian cancer. In a study of 103 Hispanic patients enrolled in one of five primary clinics in a Texas-based study, less than one quarter of respondents was able to identify the amount of breast cancer due to hereditary predisposition (Strecker et al., 2002). Similarly, in our study, only 9% of women selected false to a question about whether half of all cases of breast cancer are attributed to a BRCA mutation. The other general area where knowledge was low was among the questions about ovarian cancer risk management.
While this study represents an important first step in understanding baseline levels of knowledge among Hispanic women with risk factors for HBOC, there are certain limitations that must be considered. First, our sample was recruited from the Tampa Bay area and may not be representative of Hispanics from other regions of the United States. However, we did find many parallels between knowledge in our study population and that of studies of other Hispanic groups in Texas and New York (Strecker et al., 2002; Sussner et al., 2009). Second, there is currently controversy about if or how acculturation should be measured in the context of health research (Hunt et al., 2004). Some argue that there has been a lack of underlying conceptualization of the definition of acculturation that precludes accurate measurement of this construct; however, most agree that language use is a central issue in assessing acculturation (Hunt et al., 2004). One of the three measures of acculturation we used related to language use. Additionally, there is concern that studies that measure acculturation fail to consider other important variables such as Hispanic subethnicity and socioeconomic status (Hunt et al., 2004). In our study, we have attempted to address this issue by evaluating each of these factors in relation to knowledge. Finally, our sample size of 53 participants is considered sufficient for the qualitative aspects of the project, but does limit our ability to interpret and generalize the quantitative data presented in this analysis.
Recent data that suggest the important role of BRCA mutations in breast cancer risk among Hispanic women (John et al., 2007), coupled with the identification of founder mutations in this group (Weitzel et al., 2005, 2007), make it imperative to provide Hispanic women with information related to HBOC to promote risk-appropriate access to and use of genetic counseling and testing services. Our study provides important preliminary information about characteristics associated with lower levels of knowledge (e.g., personal history of breast cancer) and specific areas related to HBOC where additional research and education may be warranted in the Hispanic community.
Acknowledgments
Funding for this project was provided by Grant 1 R03 HG003887 from the National Human Genome Research Institute. The work contained within this publication was supported in part by the Survey Methods Core Facility at the H. Lee Moffitt Cancer Center and Research Institute.
Disclosure Statement
No competing financial interests exist.
References
- American Cancer Society I. Cancer Facts & Figures for Hispanics/Latinos. 2008. www.cancer.org/downloads/STT/CAFF2006HispPWSecured.pdf. [Oct 22;2009 ]. www.cancer.org/downloads/STT/CAFF2006HispPWSecured.pdf
- American Medical Association. Identifying and Managing Hereditary Risk for Breast and Ovarian Cancer. Chicago: 2001. [Google Scholar]
- American Medical Association. An AMA Continuing Medical Education Program. Chicago: 2002. Identifying and Managing Hereditary Risk for Breast and Ovarian Cancer: Case Studies in Genetic Testing. [Google Scholar]
- Bentley JR. Delfino RJ. Taylor TH, et al. Differences in breast cancer stage at diagnosis between non-Hispanic white and Hispanic populations, San Diego County 1988–1993. Breast Cancer Res Treat. 1998;50:1–9. doi: 10.1023/a:1006097601517. [DOI] [PubMed] [Google Scholar]
- Berrigan D. Dodd K. Troiano RP, et al. Physical activity and acculturation among adult Hispanics in the United States. Res Q Exerc Sport. 2006;77:147–157. doi: 10.1080/02701367.2006.10599349. [DOI] [PubMed] [Google Scholar]
- Brekelmans CT. Tilanus-Linthorst MM. Seynaeve C, et al. Tumour characteristics, survival and prognostic factors of hereditary breast cancer from BRCA2-, BRCA1- and non-BRCA1/2 families as compared to sporadic breast cancer cases. Eur J Cancer. 2007;43:867–876. doi: 10.1016/j.ejca.2006.12.009. [DOI] [PubMed] [Google Scholar]
- Brewster K. Wileyto EP. Kessler L, et al. Sociocultural predictors of breast cancer risk perceptions in African American breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2007;16:244–248. doi: 10.1158/1055-9965.EPI-06-0481. [DOI] [PubMed] [Google Scholar]
- Chen WY. Garber JE. Higham S, et al. BRCA1/2 genetic testing in the community setting. J Clin Oncol. 2002;20:4485–4492. doi: 10.1200/JCO.2002.08.147. [DOI] [PubMed] [Google Scholar]
- Daly M. Axilbund JE. Bryant E, et al. The NCCN Genetic/Familial High-Risk Assessment: Breast and Ovarian Clinical Practice Guideline, version 1.2009. 2009. www.nccn.org/professionals/physician_gls/PDF/genetics_screening.pdf. www.nccn.org. [Oct 22;2009 ]. www.nccn.org/professionals/physician_gls/PDF/genetics_screening.pdfwww.nccn.org To view the most recent and complete version of guideline, go to.
- Doksum T. Joseph C. Watson M, et al. Genetics Education and Underserved Populations: Summary of the Literature. Abt Associates Inc.; Cambridge, MA: 2004. [Google Scholar]
- Guest G. Bunce A. Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- Hall MJ. Reid JE. Burbidge LA, et al. BRCA1 and BRCA2 mutations in women of different ethnicities undergoing testing for hereditary breast-ovarian cancer. Cancer. 2009;115:2222–2233. doi: 10.1002/cncr.24200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampel H. Sweet K. Westman JA, et al. Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. J Med Genet. 2004;41:81–91. doi: 10.1136/jmg.2003.010918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck JE. Franco R. Jurkowski JM. Sheinfeld Gorin S. Awareness of genetic testing for cancer among United States Hispanics: the role of acculturation. Community Genet. 2008;11:36–42. doi: 10.1159/000111638. [DOI] [PubMed] [Google Scholar]
- Hopwood P. Shenton A. Lalloo F, et al. Risk perception and cancer worry: an exploratory study of the impact of genetic risk counselling in women with a family history of breast cancer. J Med Genet. 2001;38:139–142. doi: 10.1136/jmg.38.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe HL. Wu X. Ries LA, et al. Annual report to the nation on the status of cancer, 1975–2003, featuring cancer among U.S. Hispanic/Latino populations. Cancer. 2006;107:1711–1742. doi: 10.1002/cncr.22193. [DOI] [PubMed] [Google Scholar]
- Hunt LM. Schneider S. Comer B. Should “acculturation” be a variable in health research? A critical review of research on US Hispanics. Soc Sci Med. 2004;59:973–986. doi: 10.1016/j.socscimed.2003.12.009. [DOI] [PubMed] [Google Scholar]
- John EM. Miron A. Gong G, et al. Prevalence of pathogenic BRCA1 mutation carriers in 5 US racial/ethnic groups. JAMA. 2007;298:2869–2876. doi: 10.1001/jama.298.24.2869. [DOI] [PubMed] [Google Scholar]
- Katapodi MC. Aouizerat BE. Do women in the community recognize hereditary and sporadic breast cancer risk factors? Oncol Nurs Forum. 2005;32:617–623. doi: 10.1188/05.ONF.617-623. [DOI] [PubMed] [Google Scholar]
- Kvale S. Interviews: An Introduction to Qualitative and Research Interviewing. Sage; London: 1996. [Google Scholar]
- Lacour RA. Daniels MS. Westin SN, et al. What women with ovarian cancer think and know about genetic testing. Gynecol Oncol. 2008;111:132–136. doi: 10.1016/j.ygyno.2008.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman C. Biesecker B. Benkendorf JL, et al. Controlled trial of pretest education approaches to enhance informed decision-making for BRCA1 gene testing. J Natl Cancer Inst. 1997;89:148–157. doi: 10.1093/jnci/89.2.148. [DOI] [PubMed] [Google Scholar]
- Lerman C. Narod S. Schulman K, et al. BRCA1 testing in families with hereditary breast-ovarian cancer. A prospective study of patient decision making and outcomes. JAMA. 1996;275:1885–1892. [PubMed] [Google Scholar]
- Lerman C. Schwartz MD. Lin TH, et al. The influence of psychological distress on use of genetic testing for cancer risk. J Consult Clin Psychol. 1997;65:414–420. doi: 10.1037//0022-006x.65.3.414. [DOI] [PubMed] [Google Scholar]
- Metcalfe K. Lynch HT. Ghadirian P, et al. Contralateral breast cancer in BRCA1 and BRCA2 mutation carriers. J Clin Oncol. 2004;22:2328–2335. doi: 10.1200/JCO.2004.04.033. [DOI] [PubMed] [Google Scholar]
- Metcalfe KA. Lynch HT. Ghadirian P, et al. The risk of ovarian cancer after breast cancer in BRCA1 and BRCA2 carriers. Gynecol Oncol. 2005;96:222–226. doi: 10.1016/j.ygyno.2004.09.039. [DOI] [PubMed] [Google Scholar]
- Mullineaux LG. Castellano TM. Shaw J, et al. Identification of germline 185delAG BRCA1 mutations in non-Jewish Americans of Spanish ancestry from the San Luis Valley, Colorado. Cancer. 2003;98:597–602. doi: 10.1002/cncr.11533. [DOI] [PubMed] [Google Scholar]
- Nelson HD. Huffman LH. Fu R. Harris EL. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: systematic evidence review for the U.S. Preventive Services Task Force. Ann Intern Med. 2005;143:362–379. doi: 10.7326/0003-4819-143-5-200509060-00012. [DOI] [PubMed] [Google Scholar]
- O'Brien K. Cokkinides V. Jemal A, et al. Cancer statistics for Hispanics, 2003. CA Cancer J Clin. 2003;53:208–226. doi: 10.3322/canjclin.53.4.208. [DOI] [PubMed] [Google Scholar]
- Penchaszadeh VB. Genetic counseling issues in Latinos. Genet Test. 2001;5:193–200. doi: 10.1089/10906570152742236. [DOI] [PubMed] [Google Scholar]
- Ramirez AG. Hispanic/Latino Genetics Community Consultation Network (HLGCCN) Summitt Report 2003. Redes En Accion; San Antonio, TX: 2003. [Oct 22;2009 ]. [Google Scholar]
- Ramirez AG. Aparicio-Ting FE. de Majors SS. Miller AR. Interest, awareness, and perceptions of genetic testing among Hispanic family members of breast cancer survivors. Ethn Dis Spring. 2006;16:398–403. [PubMed] [Google Scholar]
- Ramirez RR. de la Cruz PG. The Hispanic Population in the United States: March 2002. U.S. Census Bureau, United States Department of Commerce; Washington, DC: 2003. [Google Scholar]
- Ricker C. Lagos V. Feldman N, et al. If we build it … will they come?—establishing a cancer genetics services clinic for an underserved predominantly Latina cohort. J Genet Couns. 2006;15:505–514. doi: 10.1007/s10897-006-9052-5. [DOI] [PubMed] [Google Scholar]
- Schwartz MD. Benkendorf J. Lerman C, et al. Impact of educational print materials on knowledge, attitudes, and interest in BRCA1/BRCA2: testing among Ashkenazi Jewish women. Cancer. 2001;92:932–940. doi: 10.1002/1097-0142(20010815)92:4<932::aid-cncr1403>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Strecker MN. Williams AJ. Bondy M, et al. Knowledge and attitudes of Hispanic women and their health care providers about breast cancer risk factors and screening. Community Genet. 2002;5:222–231. doi: 10.1159/000066685. [DOI] [PubMed] [Google Scholar]
- Sussner KM. Thompson HS. Valdimarsdottir HB, et al. Acculturation and familiarity with, attitudes towards and beliefs about genetic testing for cancer risk within Latinas in East Harlem, New York City. J Genet Couns. 2009;18:60–71. doi: 10.1007/s10897-008-9182-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau. Population Projection Program. Population Division (NP-D1-A); Washington, DC: 2000. Projections of the Resident Population by Age, Sex, Race, and Hispanic Origin: 1999 to 2100. [Google Scholar]
- U.S. Census Bureau. Hispanic Population of the United States. 2006. www.census.gov/population/www/socdemo/hispanic/hispanic.html. [Oct 22;2009 ]. www.census.gov/population/www/socdemo/hispanic/hispanic.html
- Vadaparampil S. Quinn G. Miree CA, et al. Recall of and reactions to a surgeon referral letter for BRCA genetic counseling among high risk breast cancer patients. Ann Surg Oncol. 2009;16:1973–1981. doi: 10.1245/s10434-009-0479-4. [DOI] [PubMed] [Google Scholar]
- Vadaparampil ST. Wideroff L. Breen N. Trapido E. The impact of acculturation on awareness of genetic testing for increased cancer risk among Hispanics in the year 2000 National Health Interview Survey. Cancer Epidemiol Biomarkers Prev. 2006;15:618–623. doi: 10.1158/1055-9965.EPI-05-0378. [DOI] [PubMed] [Google Scholar]
- Vogel KJ. Atchley DP. Erlichman J, et al. BRCA1 and BRCA2 genetic testing in Hispanic patients: mutation prevalence and evaluation of the BRCAPRO risk assessment model. J Clin Oncol. 2007;25:4635–4641. doi: 10.1200/JCO.2006.10.4703. [DOI] [PubMed] [Google Scholar]
- Weitzel JN. Lagos V. Blazer KR, et al. Prevalence of BRCA mutations and founder effect in high-risk Hispanic families. Cancer Epidemiol Biomarkers Prev. 2005;14:1666–1671. doi: 10.1158/1055-9965.EPI-05-0072. [DOI] [PubMed] [Google Scholar]
- Weitzel JN. Lagos VI. Herzog JS, et al. Evidence for common ancestral origin of a recurring BRCA1 genomic rearrangement identified in high-risk Hispanic families. Cancer Epidemiol Biomarkers Prev. 2007;16:1615–1620. doi: 10.1158/1055-9965.EPI-07-0198. [DOI] [PubMed] [Google Scholar]