The fourth Millennium Development Goal (MDG) (1) aims to reduce child mortality according to the target: ‘Reduce by two-thirds, between 1990 and 2015, the under-5 mortality rate’ (U5MR). The 2009 MDG report (2) stated ‘Although data on this target are problematic and at times contentious, significant progress in individual African countries has been registered, although the rate of progress at the continental level is poor. The U5MR in Africa dropped from 166 per 1,000 live births in 2005 to 160 per 1,000 live births in 2006’ and later ‘It is clear that the continent as a whole is unlikely to meet this U5MR target, if current trends continue. This calls for renewed and intensified efforts by African governments and their development partners to scale up interventions to reduce the U5MR. Access to and utilisation of basic health services need to be increased and made more equitable. To reduce the wide gap between rural and urban areas, more resources should be allocated to public health interventions, including environmental health, in rural areas.’
One figure in the report cited above shows large variations between African countries in terms of their success in achieving this goal. About one-third of all countries show a decline of 30% or more in U5MR. On the other hand, there are countries that sadly show a considerable increase. Two reviews on that topic have been published recently (3, 4). Rajaratnam et al. (3) found that across 21 regions of the world, rates of neonatal, post-neonatal and childhood mortality are declining. The global decline from 1990 to 2010 is 2.2% per year for childhood mortality. Robust measurement of mortality in children under-5 years of age showed that accelerating declines are occurring in several low-income countries. Bhutta et al. (4) reviewed the progress between 1990 and 2010 in the coverage of 26 key interventions in 68 countdown priority countries, which account for more than 90% of maternal and child deaths worldwide, and found that 19 of the countries studied were on track to meet MDG 4, in 47 countries acceleration was found in the yearly rate of reduction in U5MR, and in 12 countries progress had decelerated since 2000. These are overall positive findings; however, the time trends in mortality at subnational level have not been addressed in these papers. Within less developed countries there are large variations in mortality, often between the capital city, other urban areas, and the countryside, both for young children and the rest of the population. The member health and demographic surveillance systems (HDSSs) within the INDEPTH Network typically cover relatively small areas, either urban or rural, and it is important to investigate whether within such small areas a heterogeneous pattern of mortality also exists. Why is this important? Firstly, it can show whether suspected disparities really exist. Secondly, spatial analysis helps to identify underlying causes, which is the first step in implementing targeted prevention strategies. The INDEPTH Network and its associated HDSS centres play a unique role in these efforts.
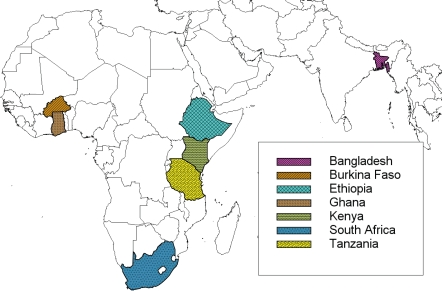
Spatial and spatial–temporal clustering of mortality was investigated at HDSSs in West, East, and South Africa, and in South Asia. Fig. 1 shows the countries that either contributed analyses to this Global Health Action Supplement or that previously published similar analyses. All these countries have their own specific characteristics, and differ substantially from each other. Nevertheless, the analyses presented here show that they have one thing in common: in each of the HDSSs considered, we found evidence of mortality being clustered.
Fig. 1.
Countries with investigations on mortality clustering at INDEPTH HDSS centres.
In this volume, clustering analyses of mortality for nine HDSS members within the INDEPTH Network are presented. Table 1 gives an overview of all the HDSSs, with some of their main characteristics, in which mortality clustering has been investigated, either in this supplement or in previous publications. With one exception, all centres included consideration of the 0–5-year age group. Some did additional analyses for other age groups and one centre combined age groups because of its smaller size.
Table 1.
Basic characteristics of the HDSS centres undertaking mortality clustering analyses
| HDSS centre | Average overall population (approx.) | Period of observation | Age groups (years) | Reference number |
|---|---|---|---|---|
| West Africa | ||||
| Dodowa, Ghana | 90,000 | 2005–2006 | <5 | 11 |
| Kintampo, Ghana | 126,000 | 2005–2007 | <5 | 12 |
| Navrongo, Ghana | 140,000 | 1997–2006 | <5 | 13 |
| Nouna, Burkina Faso | 30,000 | 1993–1998 | <5 | 8 |
| East Africa | ||||
| Butajira, Ethiopia | 43,000 | 1987–2008 | <5, 5–14, 15–49, 50–64, 65+ | 14 |
| Ifakara, Tanzania | 85,000 | 1997–2006 | <5 | 15 |
| Kisumu, Kenya | 135,000 | 2002–2005 | <5 | 10 |
| Rufiji, Tanzania | 13,000 | 1999–2008 | <5 | 16 |
| South Africa | ||||
| Agincourt, South Africa | 70,000 | 1992–2007 | <5, 5–14, 15–49, 50–64, 65+ | 17 |
| Dikgale, South Africa | 8,000 | 1996–2007 | <15, 15–49, 50 + | 18 |
| South Asia | ||||
| Chakaria, Bangladesh | 416,000 | 2005–2008 | <5 | 20 |
| Matlab, Bangladesh | 224,000 | 1998–2007 | <5 | 19 |
There are different statistical methods available to investigate mortality clustering (5). The method developed by Kulldorff (6) proved to be effective for analysing clustering of mortality in settings such as an HDSS. All papers in this volume and the previous studies listed in Table 1 have used the same statistical method to identify mortality clusters. SaTScan™ software was then used for analyses (7). It employs Kulldorff's spatial scan statistic to identify and test clusters of mortality. A brief review of the method is appropriate here. A scan statistic or test statistic is the maximum likelihood ratio over all possible circles (c) that identify the most likely (unusual) cluster. In mathematical notation,
where S is a scan statistic, L(c) is the likelihood under the alternative hypothesis that there exists a cluster (circle c) at a given location in which there is a higher rate than that expected by chance, and L 0 is the likelihood under the null hypothesis. The ratio is defined as:
where N is the total number of death cases in the study area, n c is the observed number of death cases inside the circle c and µc is the number of expected cases in the same circle. Death events are usually assumed to be Poisson distributed. Thus, a Poisson model within SaTScan™ was used during the analysis. Mortality clustering analyses were performed for purely spatial, temporal and spatial–temporal scenarios separately. During purely spatial analysis, SaTScan™ imposes a circular window on a map. This window is centred on each of several possible geographical coordinates throughout the region of study. For each coordinate, the radius of the window is varied from zero to some upper limit. The method creates an infinite number of distinct geographical circles with different sets of neighbouring locations within them. Each circle is a possible potential cluster of mortality. During purely spatial adjustments, a time interval – often one calendar year – is chosen. A similar approach is applied during purely temporal and spatial–temporal analysis. With temporal clustering, time is variable and space is held constant while for spatial–temporal clustering, both time and space are variable. Instead of a circular window, space–time scan statistic uses a cylindrical window with a circular geographic base and with height corresponding to time. The base is defined exactly as for the purely spatial scan statistic, while the height reflects the time period of potential mortality clusters. Purely temporal moves windows in one dimension with time defined in the same way as the height of the cylinder used by the space–time scan statistic. For each method of analysis, identified mortality clusters are tested as to whether they are randomly distributed over space, over time or over space and time, and evaluated with statistical significance tests.
A central assumption in the method is the circular shape of the cluster. This has been motivated by a common situation that there is a (unknown) point source of exposure, which has an effect on the mortality. This may also be appropriate in the present situation if, for example, the fertility of the soil as a potential source of morbidity is best or worst at a particular location. A circular shape may be less appropriate if, for example, a river or a coastline is related to factors that are the underlying cause for mortality differences. Therefore, the result of the clustering analysis must be discussed carefully in relation to the local conditions. Taken together, the findings presented may contribute substantially to new recommendations for public health initiatives.
The first publication analysing HDSS data with this method was Sankoh et al. (8), for the Nouna HDSS in Burkina Faso. They found strong clustering in the north-east region of the HDSS, including one particular village with strikingly high mortality. This finding gave rise to further investigations and searches for causes, and particular efforts have been made to reduce the prevalence of risk factors in this region. Recent analysis has shown (9) that the overall mortality has decreased in the HDSS, and a stronger decrease was found in the previously high mortality region. The earlier finding, which was unexpected and purely descriptive, gave rise to public health actions such as providing a better drinking water supply. It is a matter of speculation whether these particular efforts led to the stronger overall decrease in mortality; however, it must also be considered as a success in that the overall disparity in mortality has decreased.
Two other HDSS centres also published results on mortality clustering earlier this year. These are the sites in Kisumu, Kenya (10) and Dodowa, Ghana (11). In the Kenyan HDSS, living in areas of lower population density and with less direct access to health care was associated with observed clusters of childhood mortality and considered as likely causal factors. In the Ghanaian HDSS, less clustering was found; however, some of the clusters identified were associated with poorer socioeconomic status. The underlying causes for mortality were less clear.
The remaining HDSS analyses investigating clustering of mortality are published in this supplement to Global Health Action. These were located in Ghana, Ethiopia, Tanzania, South Africa and Bangladesh. In both Ghanaian HDSSs (Kintampo and Navrongo) clear spatial clustering was observed (12, 13). Although in Kintampo the observation period was too short to consider temporal trends, the 10-year period in the Navrongo HDSS showed persistent clustering of mortality in the north-east region, in parallel with a clear overall decline in mortality.
The analysis from Butajira, Ethiopia, considered all age groups, and all of them showed clustering, but at varying locations and times (14). As in many other centres, the main town had considerably lower mortality, expressed in this analysis as a cluster with a significantly lower rate. Interestingly, the mortality differences within this HDSS seemed to become smaller over time. The authors also attributed some of the clusters to particular infectious causes.
Similarly, in the Ifakara HDSS, Tanzania, strong clustering of mortality was only found in the early years of observation, with a spatial–temporal analysis identifying a cluster for 1997 and 1998 (15). Overall mortality declined strongly, with a reduction of about one-third within 10 years. A similar observation was found in the other HDSS in Tanzania, Rufiji (16). The mortality decline was even stronger here, and again the clusters associated with significantly higher mortality were found in the early years of observation.
Two HDSSs from South Africa conclude the African centres undertaking clustering analyses. A long period of observation was provided by Agincourt HDSS (17). In contrast to the sites described above, mortality increased here for all age groups (except 65 years and over), and clusters with highly significantly increased mortality were identified for all years. These probably corresponded to areas with high prevalences of HIV and other communicable diseases. The HDSS in Dikgale (18) in the north of South Africa is relatively small, and a separate analysis for children under five was therefore not possible. In the age group 0–15 years, no clustering was found. As in Agincourt, mortality increased over time.
The series is completed by two HDSSs in Bangladesh. Both HDSSs are very large. In Matlab HDSS (19), results were very much in line with those from Tanzania. There was a strong decline in mortality, and two highly significant clusters of increased mortality were found for the first 5 years, 1998–2002, in the south-east and in the north of the study area. In the Chakaria HDSS (20) a significant cluster was found in the south-west, which is a low-lying delta area. Here, the period of observation was only 4 years, thus not allowing a clear temporal analysis.
Overall, the results presented in this supplement show that there are not only wide gaps in mortality between the less developed countries, and between rural and urban areas within a country, but also within rural areas. Table 2 summarises these results. The magnitude of the observed effects, expressed as relative risks, were often between 1.5 and 2 and sometimes larger. In absolute numbers, this represents a considerable difference in mortality. It may be argued that particular efforts to reduce mortality in the high-risk areas are not appropriate since they might disadvantage other areas; however, the data presented here support the opposite. At some centres disparities decreased over the years, and those centres were also particularly successful in reducing overall mortality. This shows that both of these effects go hand in hand. In my view, within a less developed country, particular attention should be paid to more remote or disadvantaged areas, and as a result the whole country might be expected to benefit. These investigations on spatial clustering in several HDSSs within the INDEPTH Network represent an important contribution in that respect.
Table 2.
Summary results for spatial-temporal mortality clustering at HDSS centres
| HDSS centre | Clustering detected | Comments | Reference number |
|---|---|---|---|
| West Africa | |||
| Dodowa, Ghana | Yes | Clustering analysis performed within area councils, some clustering found | 11 |
| Kintampo, Ghana | Yes | Clustering found in remote areas with high poverty levels | 12 |
| Navrongo, Ghana | Yes | Strong spatial clustering found consistently over total observation period, overall mortality decline | 13 |
| Nouna, Burkina Faso | Yes | Strong spatial clustering over the whole observation period | 8 |
| East Africa | |||
| Butajira, Ethiopia | Yes | Clustering observed at various times and places, decreasing disparity of mortality | 14 |
| Ifakara, Tanzania | Yes | Clustering observed in early years only, overall mortality decline | 15 |
| Kisumu, Kenya | Yes | Strong clustering found, related to suspected risk factors | 10 |
| Rufiji, Tanzania | Yes | Clustering observed in early years only, overall mortality decline | 16 |
| South Africa | |||
| Agincourt, South Africa | Yes | Clustering observed, overall mortality increase | 17 |
| Dikgale, South Africa | Yes | Small study size, some clustering in adults, overall mortality increase | 18 |
| South Asia | |||
| Chakaria, Bangladesh | Yes | Clustering observed in early years only, overall mortality decline | 20 |
| Matlab, Bangladesh | Yes | Clustering observed in low-lying delta area | 19 |
References
- 1.United Nations, New York: Millennium Campaign Offices; Available from: http://www.endpoverty2015.org/ [cited 12 July 2010] [Google Scholar]
- 2.African Development Bank Group. Assessing progress in Africa toward the millennium development goals. MDG Report 2009. Available from: http://www.afdb.org/fileadmin/uploads/afdb/Documents/Publications/Full%20Report-MDG-WEB.pdf [cited 12 July 2010]
- 3.Rajaratnam JK, Marcus JR, Flaxman AD, Wang H, Levin-Rector A, Dwyer L, et al. Neonatal, postneonatal, childhood, and under-5 mortality for 187 countries, 1970–2010: a systematic analysis of progress towards millennium development goal 4. Lancet. 2010;375:1988–2008. doi: 10.1016/S0140-6736(10)60703-9. [DOI] [PubMed] [Google Scholar]
- 4.Bhutta ZA, Chopra M, Axelson H, Berman P, Boerma T, Bryce J, et al. Countdown to 2015 decade report (2000–10): taking stock of maternal, newborn, and child survival. Lancet. 2010;375:2032–44. doi: 10.1016/S0140-6736(10)60678-2. [DOI] [PubMed] [Google Scholar]
- 5.Sankoh OA, Becher H. Disease cluster methods in epidemiology: application to data on childhood mortality in rural Burkina Faso, West Africa. Informatik. Biometrie und Epidemiologie in Medizin und Biologie. 2002;33:460–72. [Google Scholar]
- 6.Kulldorff M. A spatial scan statistic. Commun Stat Theory Methods. 1997;26:1481–96. [Google Scholar]
- 7.SatScan™. Software for the spatial, temporal, and space–time scan statistics. Available from: http://www.satscan.org/ [cited 10 July 2010]
- 8.Sankoh OA, Yé Y, Sauerborn R, Müller O, Becher H. Clustering of childhood mortality in rural Burkina Faso. Int J Epidemiol. 2001;30:485–92. doi: 10.1093/ije/30.3.485. [DOI] [PubMed] [Google Scholar]
- 9.Sié A, Louis VR, Gbangou A, Müller O, Niamba L, Stieglbauer G. The health and demographic surveillance system (HDSS) in Nouna, Burkina Faso, 1993–2007. Global Health Action (in review) doi: 10.3402/gha.v3i0.5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ombok M, Adazu K, Odhiambo F, Bayoh N, Kiriinya R, Slutsker L, et al. Geospatial distribution and determinants of child mortality in rural western Kenya 2002–2005. Trop Med Int Health. 2010;15:423–33. doi: 10.1111/j.1365-3156.2010.02467.x. [DOI] [PubMed] [Google Scholar]
- 11.Awini E, Mattah P, Sankoh O, Gyapong M. Spatial variations in childhood mortalities at the Dodowa Health and Demographic Surveillance System site of the INDEPTH Network in Ghana. Trop Med Int Health. 2010;15:520–28. doi: 10.1111/j.1365-3156.2010.02492.x. [DOI] [PubMed] [Google Scholar]
- 12.Nettey OEA, Zandoh C, Sulemana A, Adda R, Owusu-Agyei S. Clustering of childhood mortality in the Kintampo Health and Demographic Surveillance System in Ghana. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adjuik M, Kanyomse E, Kondayire F, Wak G, Hodgson A. Clustering of under-five mortality in the Navrongo HDSS in the Kassena-Nankana District of northern Ghana. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Byass P, Fantahun M, Emmelin A, Molla M, Berhane Y. Spatio-temporal clustering of mortality in Butajira, Ethiopia, from 1987 to 2008. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lutambi AM, Alexander M, Charles J, Mahutanga C, Nathan R. Under-five mortality: spatial–temporal clusters in Ifakara HDSS in South-eastern Tanzania. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shabani J, Lutambi AM, Mwakalinga V, Masanja H. Clustering of under-five mortality in Rufiji Health and Demographic Surveillance System in rural Tanzania. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sartorius B, Kahn K, Vounatsou P, Collinson MA, Tollman SM. Space and time clustering of mortality in rural South Africa (Agincourt HDSS), 1992–2007. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanjala C, Alberts M, Byass P, Burger S. Spatial and temporal clustering of mortality in Digkale HDSS in rural northern South Africa. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alam N, Zahirul Haq M, Streatfield PK. Spatio-temporal patterns of under-five mortality in Matlab HDSS rural Bangladesh. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hanifi SMA, Haq MZ, Aziz RR, Bhuiya A. High concentration of childhood deaths in the low-lying areas of Chakaria HDSS, Bangladesh: findings from a spatial analysis. Global Health Action. 2010;(Supplement 1) doi: 10.3402/gha.v3i0.5274. [DOI] [PMC free article] [PubMed] [Google Scholar]