Abstract
Persistent and intractable hiccups (with respective durations of more than 48 hours and 1 month) can result in depression, fatigue, impaired sleep, dehydration, weight loss, malnutrition, and aspiration syndromes. The conventional treatments for hiccups are either non-pharmacological, pharmacological or a nerve block treatment. Pulsed radiofrequency lesioning (PRFL) has been proposed for the modulation of the excited nervous system pathway of pain as a safe and nondestructive treatment method. As placement of the electrode in close proximity to the targeted nerve is very important for the success of PRFL, ultrasound appears to be well suited for this technique. A 74-year-old man suffering from intractable hiccups that had developed after a coronary artery bypass graft and had continued for 7 years was referred to our pain clinic. He had not been treated with conventional methods or medications. We performed PRFL of the phrenic nerve guided by ultrasound and the hiccups disappeared.
Keywords: hiccup, pulsed radiofrequency, ultrasound
Generally, hiccups resolve itselves. However, if they last longer than usual, this illness can cause dehydration, impaired sleep, depression, gastroenteric disorders, and even death [1]. Usually, hiccups stop within 48 hours. If they continue for more than 48 hours but end within a month, they are known as "persistent hiccups". If they last longer than 1 month, the condition is classified as "intractable hiccups" [2]. Both pharmacological and non-pharmacological treatment can be used to cure the disease, and if these two methods are ineffective, a nerve block can be considered [3]. We, as the authors in this study, applied a phrenic nerve block after the patient did not respond well to a pharmacological treatment. However, the effect of the nerve block was only temporary, and for this reason we performed pulsed radiofrequency lesioning (PRFL) of the phrenic nerve.
PRFL causes less damage to nerves and surrounding structures than heat-based radiofrequency (RF) denervation. Thus, it is becoming more common as a treatment for peripheral nerve disorders [4,5]. If doctors utilize ultrasound as an initial RF treatment, they can assess the anatomical structures as preparation for the treatment of targeted nerves [6]. Herein, as we succeeded in eliminating intractable hiccups through PRFL guided by ultrasound, we report the case with reviewing the related literature.
CASE REPORT
Our patient was a 74-year-old man who had received dialysis for 8 years due to end-stage renal disease. His hiccups started 1 year after the beginning of dialysis and occurred 2-3 times per week, typically lasting 1-2 hours each time. A magnetic resonance image (MRI) scan of his brain did not detect any problems, apart from for a lacunar infarct of the central pontine. He was treated with drugs in the department of internal medicine with no apparent improvement in symptoms. The patient had undergone coronary artery bypass graft surgery 6 years earlier due to myocardial infarction; subsequently, his hiccups worsened, appearing very frequently, especially when he finished eating in the afternoon or tried to sleep at night. He usually suffered 3-4 hours once the hiccups started. To treat his aggravated symptoms, 5 mg of baclofen and 100 mg of gabapentin were given twice a day, making him somewhat better. However, he was not able to increase the dose, as he showed symptoms of drowsiness and ataxia at a higher dose. Eventually, the patient was referred to our pain clinic, complaining of fatigue, insomnia, and weight loss.
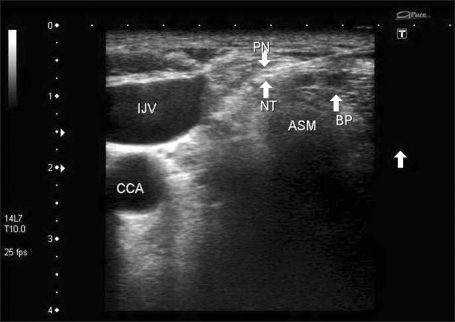
Our first action for the patient was blocking the right phrenic nerve guided by ultrasound using 4 ml of 0.2% ropivacaine and 10 mg of triamcinolone (Fig. 1). This procedure decreased the frequency of the hiccups for about one week, but afterward, his symptoms returned to their previous state. Three weeks later, we attempted to perform the same procedure on the left phrenic nerve, only to have the same outcome: a relapse after approximately 1 week.
Fig. 1.
Ultrasound image of needle tip which is adjacent to phrenic nerve for nerve block.
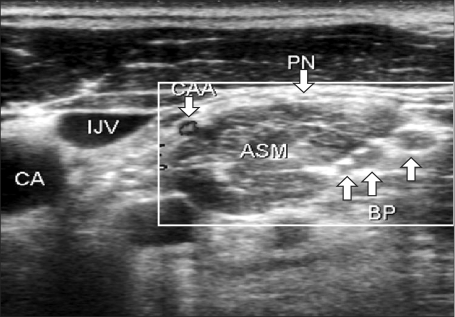
Consequently, we decided to perform PRFL, targeting both phrenic nerves with the use of ultrasound. After explaining the procedure, efficacy and possible side effects of the pulsed RF treatment, we put the patient in a supine position and turned his face to the left in order to perform the procedure, aiming at the right phrenic nerve. We prepped the skin above with betadine and aseptically draped and placed a 10 MHz, linear probe at a position 2 cm cephalad from the top of the clavicle to observe the anatomical structures of his neck through ultrasound (Xario, Toshiba, USA). After discovering the phrenic nerves situated in the middle, anterior margin of anterior scalene (Fig. 2), the 10 cm RF electrode (Neurotherm, Medipoint, Germany) with a 5 mm active tip was advanced as close as possible to the nerves by using the ultrasound. Nerve stimulation using the RF lesion generator (Neurotherm, Morgan Automation LTD, UK) showed concordant movement of 120 times per minutes in upper abdomen at 2 Hz and 0.5 mA which confirmed proper localization of the RF electrode. After clarifying the location of the target nerves once again, we performed PRFL twice for a total of 120 seconds at 42℃ and at stimulation intervals of 20 ms/sec. Following this procedure, the same method was applied to the left phrenic nerve.
Fig. 2.
Ultrasound image of patient's phrenic nerve and related structures for pulsed radiofrequency lesioning.
Throughout the treatment, the patient did not show any problem; he went back home after taking a rest for 1 hour. The frequency of his hiccups gradually decreased; they were at half of the previous level 1 month after the treatment, when he visited our hospital as an outpatient. In addition, the number of days he was completely free from hiccups were increased. To improve the effectiveness, we repeated the same treatment after 2 and 4 months and confirmed that he was completely healed from hiccups according to the follow up by asking the patient by telephone call 1 month after he received the last treatment.
DISCUSSION
A hiccup is a sudden, involuntary and spasmodic contraction of the diaphragm and external intercostal muscles. In humans, the abrupt termination of inspiration causes the epiglottis to close, creating a "hic" sound [7]. There are more than one hundred reasons for this phenomenon [8], and among the common causes are irritation inflicted by esophageal and gastric distension or regurgitation; disorders of the central nervous system; and metabolic disorders such as uremia [9].
The treatments for the hiccups include pharmacological, non-pharmacological therapy and nerve block. In addition, etiologies of underlying disorders should be evaluated and corresponding treatment should follow [3]. Non-pharmacological therapy is method to inhibit afferent pathway of vagus nerve, for example, holding a breath, drinking cold water, and inserting a nasogastric tube. If non-pharmacological therapy is ineffective, drugs such as metoclopramide, chlorpromazine, amitriptyline, phenytoin, valproic acid can be used [1]. Recently, baclofen and gabapentin have been selected for monotherapy or combination therapy. Lee et al. [10] reported a case that the intractable hiccups that had lasted for five years completely disappeared by using monotherapy of baclofen. Also, Tegeler and Baumrucker [11] reported that under treatment with gabapentin showed satisfactory clinical results. As for nerve blocks, Babacan et al. [12] reported a case that the frequency of hiccups decreased by blocking of the glossopharyngeal nerve. Calvo et al. [13] reported a case that five cancer patients, who suffered from hiccups not responsive to drugs, benefited from the cervical phrenic nerve block using 4 ml of 1% lidocaine and 40 mg of triamcinolone.
Our patient slightly responded to baclofen and gabapentin, but all other drugs were not effective. The authors reported previously that baclofen could cause neurotoxicity to renal disease patients even with a small amount [14]. For this reason, we were not able to increase the dose of baclofen because the patient had uremia developed in the end-stage renal disease. Also, in the case of gabapentin, he showed the symptoms of drowsiness and ataxia, which made it hard for him to lead a normal life, so that he had to stop taking the drug. Furthermore, the effect of phrenic nerve block using local anesthetics remained only for a week. After all, we decided to perform PRFL.
The phrenic nerve commands the movement of a diaphragm and provides the sensory innervation of the middle of a diaphragm, some parts of the pleura and pericardium. The phrenic nerve originates mainly from the 4th cervical nerve, but also receives contributions from the 3rd and 5th cervical nerves (C3-C5) in humans. Those three nerves join at the upper, lateral portion of the anterior scalene, forming phrenic nerves. The nerve descends obliquely across the anterior scalene, through the gap between sternocleidomastoid and omohyoid muscles, and deep into the thorax. According to the recent anatomical study of the phrenic nerve by using ultrasound, it is oval and its average diameter is 0.6 × 1.0 mm (ranging from 0.3 × 0.6 to 0.8 × 1.7) whether left or right side. Moreover, there is no significant difference in this nerve between among genders and ages [15].
Nerve block guided by ultrasound is known to be safer than the one solely depending on surface anatomy. The reason is that operators can identify the anatomical structures of nerves, muscles and blood vessels in real time while approaching a needle to target nerves. In other words, operators don't have to depend only on surface anatomy anymore and nerve or blood vessel damage can be prevented [6]. We thought that ultrasound was necessary not only for nerve block but also for PRFL since a RF catheter should be placed as close as possible to target nerves. In our case, we found his phrenic nerve so easily by moving the probe in a cephalo-caudal direction that we were able to situate the needle exactly in front of the target nerve without injury to any other structure.
The mechanism of PRFL is based to inhibit evoked synaptic activity of excitatory C-fiber in response to repetitive, burst-like stimulation of A δ-fiber and to change structure of nerve tissue [16]. The conventional heat-based RF is programmed to remove pain-causing nerve with heat as high as 60-80℃. Accordingly, it inevitably gives damage to surrounding nerve tissues although it can relieve pain in the long time. However, PRFL can minimize nerve damage since mechanism of PRFL is neuromodulation of electromagnetic fields generated by electric current [4]. Amidst recently-growing use of PRFL in peripheral nerve disorders, Philip et al. [17] reported a case that a patient with meralgia paraesthetica was completely cured after receiving a round of PRFL at his lateral femoral cutaneous nerve without any side effect accompanied. Also, Liliang et al. [18] reported a case of PRFL applied for 11 patients who suffer from chronic shoulder pain, targeting their suprascapular nerves, and confirmed that the effect of pain relief lasted longer than 6 months.
In conclusion, through this case report, we illustrated our experience of performing PRFL of phrenic nerve, which is safer and more accurate treatment, with the guidance of ultrasound. We attempted to present the possible effectiveness of PRFL against the intractable hiccups that are not responsive to other types of treatments including pharmacological treatment. Last but not least, we believe that, for PRFL to be used widely in this way, further studies will be needed to prove the safety and efficacy of the treatment, getting more patients involved.
References
- 1.Homer JR, Davies JM, Amundsen LB. Persistent hiccups after attempted interscalene brachial plexus block. Reg Anesth Pain Med. 2005;30:574–576. doi: 10.1016/j.rapm.2005.07.187. [DOI] [PubMed] [Google Scholar]
- 2.Cymet TC. Retrospective analysis of hiccups in patients at a community hospital from 1995-2000. J Natl Med Assoc. 2002;94:480–483. [PMC free article] [PubMed] [Google Scholar]
- 3.Pooran N, Lee D, Sideridis K. Protracted hiccups due to severe erosive esophagitis: a case series. J Clin Gastroenterol. 2006;40:183–185. doi: 10.1097/00004836-200603000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Cosman ER, Jr, Cosman ER., Sr Electric and thermal field effects in tissue around radiofrequency electrodes. Pain Med. 2005;6:405–424. doi: 10.1111/j.1526-4637.2005.00076.x. [DOI] [PubMed] [Google Scholar]
- 5.Nguyen M, Wilkes D. Pulsed radiofrequency V2 treatment and intranasal sphenopalatine ganglion block: a combination therapy for atypical trigeminal neuralgia. Pain Pract. 2010;10:370–374. doi: 10.1111/j.1533-2500.2010.00382.x. [DOI] [PubMed] [Google Scholar]
- 6.Brull R, Perlas A, Cheng PH, Chan VW. Minimizing the risk of intravascular injection during ultrasound-guided peripheral nerve blockade. Anesthesiology. 2008;109:1142. doi: 10.1097/ALN.0b013e31818dd8aa. [DOI] [PubMed] [Google Scholar]
- 7.McFarling DA, Susac JO. Hoquet diabolique: intractable hiccups as a manifestation of multiple sclerosis. Neurology. 1979;29:797–801. doi: 10.1212/wnl.29.6.797. [DOI] [PubMed] [Google Scholar]
- 8.Marshall JB, Landreneau RJ, Beyer KL. Hiccups: esophageal manometric features and relationship to gastroesophageal reflux. Am J Gastroenterol. 1990;85:1172–1175. [PubMed] [Google Scholar]
- 9.Kahrilas PJ, Shi G. Why do we hiccup? Gut. 1997;41:712–713. doi: 10.1136/gut.41.5.712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee JH, Kim TY, Lee HW, Choi YS, Moon SY, Cheong YK. Treatment of intractable hiccups with an oral agent monotherapy of baclofen: a case report. Korean J Pain. 2010;23:42–45. doi: 10.3344/kjp.2010.23.1.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tegeler ML, Baumrucker SJ. Gabapentin for intractable hiccups in palliative care. Am J Hosp Palliat Care. 2008;25:52–54. doi: 10.1177/1049909107305657. [DOI] [PubMed] [Google Scholar]
- 12.Babacan A, Oztürk E, Kaya K. Relief of chronic refractory hiccups with glossopharyngeal nerve block. Anesth Analg. 1998;87:980. doi: 10.1097/00000539-199810000-00052. [DOI] [PubMed] [Google Scholar]
- 13.Calvo E, Fernández-La Torre F, Brugarolas A. Cervical phrenic nerve block for intractable hiccups in cancer patients. J Natl Cancer Inst. 2002;94:1175–1176. doi: 10.1093/jnci/94.15.1175. [DOI] [PubMed] [Google Scholar]
- 14.Chou CL, Chen CA, Lin SH, Huang HH. Baclofen-induced neurotoxicity in chronic renal failure patients with intractable hiccups. South Med J. 2006;99:1308–1309. doi: 10.1097/01.smj.0000247632.84949.27. [DOI] [PubMed] [Google Scholar]
- 15.Canella C, Demondion X, Delebarre A, Moraux A, Cotten H, Cotton A. Anatomical study of phrenic nerve using ultrasound. Eur Radiol. 2010;20:659–665. doi: 10.1007/s00330-009-1579-z. [DOI] [PubMed] [Google Scholar]
- 16.Cahana A, Vutskits L, Muller D. Acute differential modulation of synaptic transmission and cell survival during exposure to pulsed and continuous radiofrequency energy. J Pain. 2003;4:197–202. doi: 10.1016/s1526-5900(03)00554-6. [DOI] [PubMed] [Google Scholar]
- 17.Philip CN, Candido KD, Joseph NJ, Crystal GJ. Successful treatment of meralgia paresthetica with pulsed radiofrequency of the lateral femoral cutaneous nerve. Pain Physician. 2009;12:881–885. [PubMed] [Google Scholar]
- 18.Liliang PC, Lu K, Liang CL, Tsai YD, Hsieh CH, Chen HJ. Pulsed radiofrequency lesioning of the suprascapular nerve for chronic shoulder pain: a preliminary report. Pain Med. 2009;10:70–75. doi: 10.1111/j.1526-4637.2008.00543.x. [DOI] [PubMed] [Google Scholar]