Abstract
Background
The post mortem external examination is the final service that a physician can render to a patient. Its purpose is not just to establish medical diagnoses, but to provide facts in the service of the judicial process and the public interest. Its main tasks are the definitive ascertainment of death, determination of the cause of death and assessment of the manner of death.
Methods
Selective search and review of relevant literature on cause-of-death statistics, judicial principles, and the performance of the post mortem examination, with emphasis on determination of the cause and manner of death.
Results and discussion
An important duty of the physician performing the post mortem external examination is to know the patient’s history. Thus, in principle, the treating physician is the most suitable person to perform the post mortem examination. In most cases of death (perhaps 60% to 70%), the treating physician will be able to give reliable information on the patient’s underlying illnesses and the cause of death, based on the patient’s history and circumstances at the time of death. Problems arise when death is unexpected and the post mortem external examination alone does not suffice to establish the cause of death. If the cause of death cannot be determined, this fact should be documented, and the manner of death should likewise be documented as undetermined. The autopsy rate in Germany is less than 5% of all deaths, which is very low.
The Royal Bavarian Instructions for Post Mortem Examination of 6 August 1839 are succinct on the objectives of the medical examination after death: “The purpose of the examination after death is, first, to avoid the burial of those who merely appear to be dead, and, next, to prevent the concealment of violent death and medical bungling; and also to give suitable assistance, first, in the discovery of contagious and epidemic diseases and, next, in the production of accurate lists of deaths.” This canon of objectives, fulfilled by determining the occurrence, cause, and time of death, together with an assessment of the manner of death and information as to whether any contagious disease as defined by the Infection Protection Act was present, remains unchanged to this day (1, 2).
In the context of the examination after death, the physician is required to report a death in the presence of any of the following, which are sufficient grounds to break medical confidentiality:
Unnatural or unexplained manner of death
Unknown identity of the body
Any factor or condition requiring reporting under the Infection Protection Act.
The quality of external postmortem examination has been under criticism for decades. The central point of criticism, from the judicial aspect, is incorrect assessment of the manner of death (natural versus unnatural or unexplained), which according to the investigating authorities fails to ensure that unnatural deaths will be identified. There are a multitude of structural problems concerning the post mortem external examination, for example:
In the certification of death, medical confidentiality may be broken when:
The manner of death is unnatural or unexplained
The identity of the deceased is unknown
Conformity with the Infection Protection Act requires it
For certain groups of cases, the certifying physician is objectively inadequate to the task, and is not allowed the flexibility to seek possible solutions.
No pre-training is given in how to handle problem cases.
Coroner’s autopsies are not carried out in cases where the cause of death could not be established at the medical external examination after death.
Medical duties are conflated with criminological duties.
Possible conflicts of interest arise—particularly when physicians in general practice are involved, who also have relatives of the deceased among their patients.
Focusing of reportable cases of death on those where a third party may be guilty.
Systemic failure of the system for determining cause of death, with lack of an intermediate authority between the physician and the investigating authority, analogous to the coroner system in England and Wales (which enables deaths to be investigated irrespective of any suspicion of third-party guilt) (2– 5).
Cause of death statistics.
50% of deaths occur in hospital, around 25% in the home, and about 15% in care homes. The remaining 10% are divided up among transport accidents, work accidents, etc.
Learning goals
This contribution aims to:
Explain, based on the fundamental data on deaths in Germany, the requirements that form the core of the medical external examination for death certification: determination of the cause of death and assessment of the manner of death
Give tips on how to recognize unnatural causes of death
Provide an overview of the legal requirements and duties laid on the physician carrying out a medical examination for the purpose of death certification.
Causes of death as shown by cause of death statistics
In 2007, 818 271 deaths were reported in Germany; according to the Federal Statistical Office, in 784 962 cases the cause of death was natural. Even just for the place where death occurred, there are no uniform data for the whole of Germany; but more than 50% of deaths today occur in hospital (according to own data), about 25% at home, and around 15% in care homes. The remaining 10% are divided up among transport accidents, work accidents, etc.
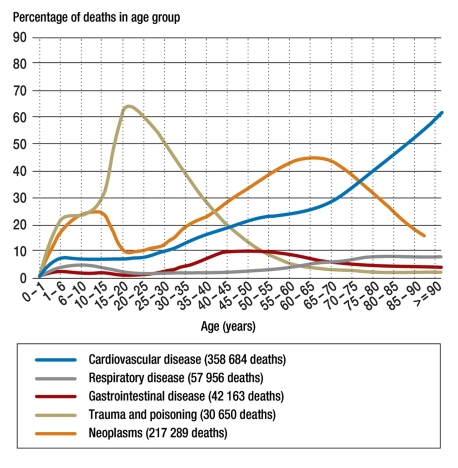
In 2007, of 17 178 573 inpatient admissions, 6 092 198 were cases belonging to the field of internal medicine. The second largest number of admissions—3 592 386 patients—were to departments of surgery. Within internal medical departments, most deaths were in cardiology, followed in order by gastroenterology, hematology, and geriatrics (eTable, eFigure). Out of a total of 818 271 deaths in 2007, 258 684 were due to cardiovascular conditions, the most common of which was ischemic heart disease (148 641 deaths). The second most common group of causes of death is malignant neoplasms, with 211 765 deaths. It should be borne in mind that deaths for the various disease groups vary considerably among age groups.
eTABLE. Admissions and deaths in German hospitals in 2007*1.
| Specialty | Admissions | Deaths |
| Surgery | 3 592 386 | 59 062 |
| Obstetrics and ‧gynecology | 1 730 055 | 4013 |
| Internal medicine | 6 092 198 | 276 890 |
| Endocrinology | 37 304 | 1105 |
| Gastroenterology | 503 033 | 21 618 |
| Hematology | 242 069 | 16 959 |
| Cardiology | 987 266 | 31 419 |
| Pulmonology and bronchology | 246 351 | 8571 |
| Nephrology | 109 841 | 5829 |
| Rheumatology | 57 066 | 197 |
| Geriatrics | 164 192 | 12 686 |
| Neurology | 666 859 | 13 911 |
*1 according to data from the Federal Statistical Office
eFIGURE.
Deaths in the major disease groups in relation to age at death according to cause of death statistics for 2007 (source: German Federal Statistical Office). Other groups, which account for a total of 111 448 deaths, are not shown.
Up until the age of 40 years, unnatural death is more frequent than death from disease (internal cause of death); not until after the age of 40 do deaths from malignancy and cardiovascular disease become more numerous than unnatural deaths.
Frequency of causes of death.
Up until the age of 40 years, unnatural death is more frequent than death from disease; not until after the age of 40 do deaths from malignancy and cardiovascular disease predominate.
These data from the German Federal Statistical Office derive from coding of the entries in the death certificate on the underlying disease and immediate cause of death, and only the underlying disease is taken into account in cause of death statistics. In the State (Land) Statistical Offices, by contrast, the statement of underlying disease is not automatically used in the cause of death statistics: the coders examine the entries on each death certificate, determine the underlying disease, and code this underlying disease in accordance with the ICD regulations. Against the background of increasingly multifactorial death processes, however, monocausal representations of deaths only partially fulfill the needs of cause of death statistics and the data derived from them about indicators of health (6, 7).
Agreement between cause of death diagnosis on death certificate and at autopsy
Numerous studies have been published on the validity of clinically determined cause of death as entered on the death certificate in comparison to patho-anatomical findings. The Görlitz study (1986–87), with a nearly 100% rate of autopsy (1060 deaths, in 1023 of which an autopsy was carried out), showed disagreement between certificate and autopsy findings in a total of 45% of male deaths and 48.8% of female deaths. Among hospital deaths, there was disagreement about the underlying disease in 42.9% of men and 44% of women; among deaths in care homes the figures were 63.2% of men and 57.8% of women; and among deaths occurring elsewhere (at home, in public, etc.), 41.3% of men and 50.7% of women (1, 8). Among iatrogenic deaths the rate of disagreement between underlying disease as determined clinically and at autopsy was as high as 72%, and disagreement about the immediate cause of death was 45.8% (5).
A human corpse is constituted by any of the following:
The body of a dead person (bones and tissue)
The body of a dead neonate which showed a sign of life after leaving the womb; a stillbirth (≥ 500 g)
A head or torso found separated from the rest of the body
Numerous studies have differentiated and operationalized the discrepancies between clinically determined cause of death and that determined at autopsy (major mistake, class 1; major mistake, class 2; minor mistake) (box 1). According to various statistics, class 1 major mistakes, which have consequences for treatment and survival of the patient, occur in 11% to 25% of deaths, while class 2 major mistakes, which have no consequences for treatment and survival, occur in 17% to 40% of deaths (9).
Box 1. Discrepancies between causes of death determined clinically and at autopsy*1.
-
Major mistake, class 1
Clinically missed diagnosis that on autopsy proves to have been the underlying cause of death and/or the main immediate cause of the patient’s death. If the diagnosis had been made in time, the patient’s life could have been prolonged, at least for a time.
-
Major mistake, class 2
Clinically missed diagnosis that would not have affected the management and course of the disease had it been made before death.
-
Minor mistake
Diseases or medical facts discovered during autopsy that have no direct causal connection with the underlying or immediate cause of death.
*1 modified from (20)
According to a meta-analysis by Shojania et al., class 1 major mistakes have reduced in the past 40 years but still occur in about 8% to 10% of deaths (10, 11). Here it must be borne in mind, however, that the rate of agreement or disagreement between clinically and autopsy-determined cause of death depends on many variables, such as:
The definition of the cause of death
The evaluated disease class
Age
The patient group under investigation (outpatient, inpatient, specialized hospital)
The duration of the hospital stay
The predictability of the death (expected vs. unexpected)
The following do not constitute a human corpse:
A skeleton or parts of a skeleton
Miscarriages (stillbirths of <500 g birth weight; need not be reported)
When to perform the medical examination for certification of a death.
A medical examination for certification of a death must always be performed when a human corpse is discovered and must be carried out without delay once the report of the death has been received.
No comparison between clinical and autopsy-determined cause of death that takes account of these variables in a differentiated way has yet been carried out, and none is to be expected under the current regulatory framework in Germany for performing clinical autopsies. This is true particularly for outpatient deaths, which are almost never subjected to autopsy except when ordered by the courts.
The concept of diagnostic error would correspond to the class 1 major mistake. A diagnostic error is assumed to have occurred when, at the end of the diagnostic decision process, a disease is definitely presumed to be present in a patient when in fact it later proves not to be so, a treatment is initiated that is not appropriate for the disease recognized at the later date, and the failure to recognize the disease that is actually present has led to a worsening of the patient’s prognosis (1, 3, 12).
Practical procedure
A medical examination for certification of death must always be carried out when a dead human body is found (box 2) and without delay once the report of the death has been received. The general requirements for medical certification of death are summarized in Box 3. Establishing definitively that death has occurred is straightforward. Cessation of vital functions can be diagnosed with certainty by the following:
Box 2. Definition of a human corpse and the deadlines to be observed on the death of a human being.
-
A human corpse is:
The body of a dead person, so long as tissue continuity has not been destroyed by putrefaction
The body of a dead neonate (irrespective of body weight) if it has completely left the womb, and if after leaving the womb it showed one of the three signs of life (heart beat, umbilical pulsation, breathing)
A stillbirth (stillborn baby weighing ≥500 g)
The head or torso separated from a body that cannot be reassembled
-
The following are not corpses:
Skeletons, partial or complete
Miscarriages (stillborn fetuses with a birth weight <500 g; no requirement to report the death)
-
Procedures and deadlines in Germany
The body should be examined without delay once notice of the death has been received.
The body must be delivered to a morgue after no more than 36 hours, but not before it has been examined and the death certificate issued.
The death must be notified to the Register Office no later than one working day after the death occurred.
Interment must take place no earlier than 48 hours and no more than 8 days after the death.
Box 3.
Basic principles and requirements of the medical examination for death certification in Germany*1
-
Law governing certification of death:
Laws of interment and regulations for death certification of the individual states (Länder) of Germany
-
Who may certify a death?
A physician
-
Who may not certify a death?
A physician who is related to the deceased (decree of the Federal Ministry of Health, Work, and Social Affairs, Bundesministerium für Gesundheit, Arbeit und Soziales, 8 June 2009)
-
Who must certify a death?
Every private practice physician in the area covered by his or her practice
In hospital, hospital physicians
-
When?
Without delay
-
How?
By careful examination of the naked body
-
Sanctions
Careless examination of the body constitutes a regulatory offense; charges may be brought if living people are injured as a consequence of careless medical examination of a dead body (e.g., if CO intoxication is overlooked and other persons suffer by the same cause)
-
Preliminary death certificate
For emergency doctors
-
Manner of death and associated statements
(Reasons to suspect) unnatural death, unexplained manner of death
-
Report to the police
Cases where death is unnatural, manner of death unexplained, or identity of body unknown
-
Report to the Ministry of Health
All cases that fall under the Infection Protection Act
-
Are doctors who have previously treated the deceased required to provide information if asked?
Yes
*1 modified from (1)
Presence of definitive signs of death (livor, rigor, advanced postmortem changes) or
Failure of attempted resuscitation for around 30 minutes, confirmed by about 30 minutes of flatline ECG despite the carrying out of appropriate measures and after ruling out general hypothermia or intoxication by central depressant drugs
Brain death (under clinical conditions can only be determined during assisted ventilation)
Physical trauma that is incompatible with life.
The procedure for ascertaining the time of death depends on the nature of the case (box 4).
Box 4. Ascertaining the time of death.
-
Deaths under medical supervision
Document the time of observed cardiovascular arrest
-
Dead body found
Establish upper and lower time limits by stating the following:
Last seen alive on…
Found dead on… or
Estimate how long the body has been lying on the basis of how far the signs of death have advanced
-
Cases in which death occurred after a brief agony and was observed by witnesses
Time of death as reported by relatives, witnesses, etc.
-
Care must be taken when near-relatives die more or less simultaneously (e.g. childless couple)
Documentation must be good because there may be issues relating to inheritance
Determining the cause of death
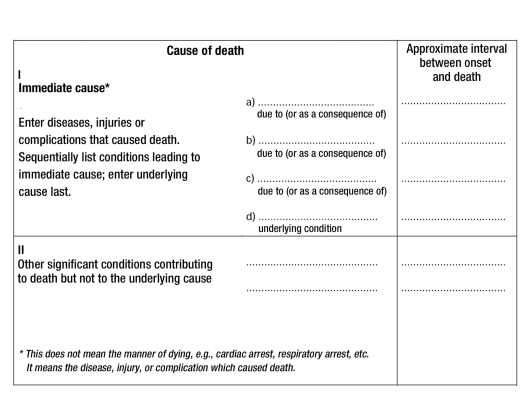
In the confidential part of the death certificate, under the heading “Cause of death,” the disease course is documented in a causal chain (Figure 1).
Figure 1:
International form of medical certificate of cause of death
Confirmation of death.
The death is confirmed by diagnosing irreversible cessation of vital functions.
The immediate cause of death is given in Part Ia and the preceding causes—diseases that caused the immediate cause of death—in Parts Ib and Ic, with the underlying disease coming last. Finally, other important diseases that lead to death but are not connected with the underlying disease are given in Part II.
The chief significance of the cause of death is statistical: how many people die from a given disease. This is as opposed to the final cause of death, which gives information about what people suffering from a particular disease die of (7, 14– 16).
According to Federal Statistical Office recommendations, if nothing precise is known, the entry “cause of death unknown” is preferable to vague speculation. Under no circumstances should constituent elements of every death process, such as “cardiac arrest,” “respiratory arrest,” or “electromechanical decoupling” be included in any part of the cause of death cascade, from underlying disease to the immediate cause of death.
Then, in the righthand column goes the duration (time interval) of the disease, taking as starting point the estimated onset of disease, not the time of diagnosis. The entries on time intervals also function as a plausibility check on the cause of death cascade.
If the cause of death given in Ia is not a consequence of further complications or underlying diseases known from the patient’s history, no further entries are needed, e.g.:
Ia: Cranial gunshot wound
Final indirect causes of death can be divided into the organ-related and those that are not organ-related (17) (table 1).
Table 1. Final indirect causes of death*1.
| Organ-related causes of death | |
| Respiratory organs | Pneumonia, pulmonary gangrene, pleuritis, pleural empyema, pneumothorax, pyopneumothorax, infarction |
| Cardiovascular organs | Coronary thrombosis, pericardial tamponade, coronary insufficiency, myocarditis, myocardial infarction |
| Organic diseases of the heart: e.g., endocarditis, cardiac hypertension, cardiac hypertrophy with mesaortitis, cor pulmonale, calcific constrictive pericarditis (concretio cordis), cardiac insufficiency | |
| Central nervous system: cerebral death | Brain hemorrhage, encephalomalacia, cerebral contusion, cerebral swelling, cerebral edema, encephalitis, status epilepticus, leptomeningitis, pachymeningitis, subdural hematoma, epidural hematoma |
| Gastrointestinal tract | Ileus, peritonitis. In children: gastroenteritis, enterocolitis, poisoning, dyspepsia, dystrophy, atrophy |
| Liver | Hepatic coma |
| Pancreas | Diabetic coma, hypoglycemic coma, hemorrhagic pancreatic necrosis |
| Kidneys | Uremia, urosepsis |
| Non-organ-related causes of death | |
| Fatal embolisms | Thromboembolism, especially pulmonary embolism, fat embolism, air embolism |
| Bleeding, internal and external, e.g.: | Hemoptysis, melena, hemothorax, hemoperitoneum |
| Sepsis | As sequela of phlegmons and the like, pyemia, generalized miliary tuberculosis, urosepsis; see also uremia |
| Tumors | Tumor-associated cachexia, tumor-associated anemia |
| Special last indirect causes of death | |
| Malformations incompatible with life | e.g. cerebral aplasia, anencephaly |
| Special causes of death in fetuses and newborns | Intrauterine asphyxia with/without aspiration of amniotic fluid, chorioamnionitis, dystrophy in the premature newborn |
*1 modified from (17)
In the prestructured entries on underlying disease and cause of death on the death certificate, according to the guidelines of the World Health Organization, physicians should mentally review the entire history of their patient’s illness. In particular, they should ask themselves whether a final morbidity was present that would be expected to lead to the patient’s death at the time given and in the circumstances described. “Hard” and “soft” causes of death should be distinguished: hard causes of death are present when the underlying disease of death and the immediate cause of death are closely related, appear in close sequence in time, and there is a close causal relationship between them, as for example in the case of a clinically diagnosed myocardial infarction that leads to cardiac rupture and thence to pericardial tamponade. Here, the underlying disease and the immediate cause of death are present within one organ system (linear type of death).
Soft diagnoses are present when the patient suffers from more than one underlying disease, none of which suggests itself a priori as the cause of death, and the cause of death remains multifactorial.
Cause of death unknown.
The statement “cause of death unknown” is preferable to vague speculation.
In evaluating disease conditions with regard to their potential to cause death, it is helpful to be guided by a classification of findings that has been usual in forensic medicine for over 90 years:
Group 1: Findings that, because of their severity and localization, are sufficient in themselves to explain the death of a person without further qualification; e.g., ruptured basilar artery aneurysm with fatal subarachnoid hemorrhage.
Group 2: Organ changes that explain the death but not the acuity with which it occurred. One example would be acute coronary insufficiency. The morphological substrate, severe atherosclerosis, undoubtedly existed on the previous day, but an external stress such as physical labor in sultry weather was the added external event that led to the onset of death at the given time.
Group 3: Deaths for which no explanation is found despite the most careful examination.
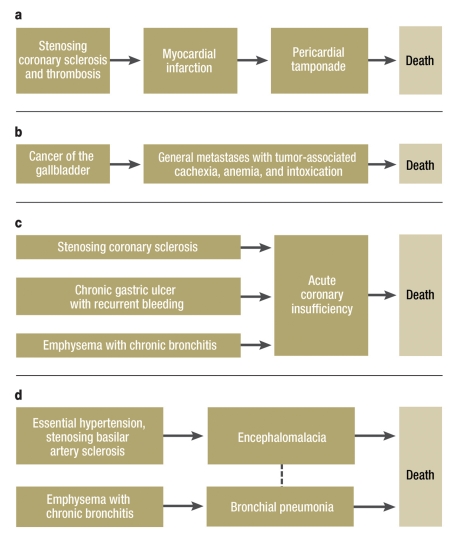
In addition, one may be guided by “death types” that have been described as a “thanatological bridge” between the underlying disease and the immediate cause of death (18, 19) (figure 2):
Figure 2.
Types of death according to Leis (9). Examples are shown for: (a) linear type of death (75-year-old man with cardiovascular disease and cardiac cause of death), (b) diverging type of death (45-year-old woman with metastatic cancer and non-organ-specific cause of death), (c) converging type of death (79-year-old man with cardiovascular, gastric, and lung disease and cardiac cause of death), and (d) complex type of death (63-year-old man with cardiovascular and pulmonary disease and with cerebral and pulmonary causes of death)
Entering the cause of death.
When entering the cause of death, the physician should review the entire history of the patient’s disease and ask him- or herself whether a morbidity was present that led to death.
Linear type of death: Underlying disease and immediate cause are within one organ system
Diverging type of death: Organ-specific underlying cause, but non-organ-specific immediate cause
Converging type of death: Underlying diseases in various organ systems lead to death via a final pathogenetic phase common to all of them
Complex type of death: Underlying diseases in various organ systems with more than one non-organ-specific immediate cause of death.
If the cause of death remains unclear in a case of unexpected death of a healthy person, this should be noted on the death certificate. Federal Statistical Office recommendations on entering the cause of death and important terms are given in Table 2 (20).
Soft diagnoses.
Soft diagnoses are present when the patient had been suffering from several underlying diseases, none of which suggests itself a priori as the cause of death.
Finally, particular problems arise with deaths in old age or in connection with medical procedures. “Senility” or “old age” is not a cause of death. Retrospective examinations of deaths of over-85-year-olds and over-100-year-olds have shown that in each case morphologically ascertainable underlying diseases and immediate causes of death were present (6). If appropriate, the diagnosed diseases that contributed to the occurrence of death may be descriptively listed as a multifactorial converging type of death, in order to avoid “makeshift” diagnoses.
As regards deaths attributable to medical procedures, the first notable point is the considerable discrepancy between the deaths recorded in the federal statistics as due to complications of medical and surgical treatment and the data derived from epidemiological research on deaths due to treatment errors.
How to proceed in the case of soft diagnoses.
It can be helpful to take account of the type of death. “Death types” are described as the thanatological bridge between the underlying disease and the immediate cause of death.
In epidemiological research, for Germany 17 500 deaths per year are suspected as a result of treatment errors (21)—these figures accord with international data—whereas the Federal Statistical Office gives only 399 deaths as complications of medical and surgical treatment in 2007 (4, 22). Here there are clearly a considerable number of unrecorded cases. This raises the question of whether in relevant circumstances the attending physician should issue the death certificate or whether, irrespective of the existence or otherwise of suspicion, such cases should always be subject to official investigation.
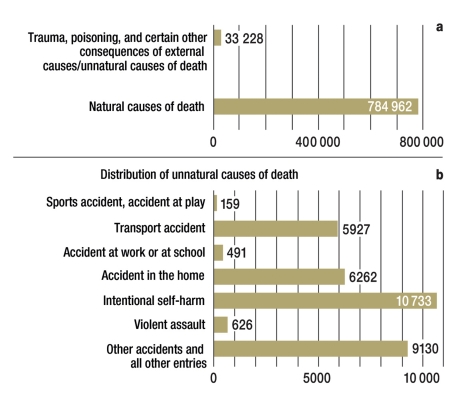
Manner of death
According to cause of death statistics, around 4% of deaths in Germany are due to unnatural causes (figure 3) (20). Around 10 000 a year are due to suicide, 6000 to accidents in the home, just under 6000 to transport accidents, and 526 deaths to physical assault.
Figure 3.
Proportion of unnatural causes of death among deaths in Germany in 2007 (source: Federal Statistical Office [20])
Retrospective analyses of death certificates for which the manner and cause of death have been checked at autopsy suggest that unnatural deaths are around 33% to 50% more frequent than is reflected in the federal statistics, and that it should be assumed that there are around 81 000 unnatural deaths every year (1, 23, e2). From the judicial point of view, a particular concern must be the number of homicides that remain undiscovered by the medical death certification; a multicenter study suggests that every year around 1200 homicides remain unidentified on death certificates in Germany (23). This large number of unrecorded cases is repeatedly confirmed by incidental findings of homicide or even serial murders (including in care homes and hospitals). Six percent of hospital physicians regularly attest exclusively to a natural death; 30% check the box for natural death even in cases of violence, poisoning, suicide, or medical intervention (e3). In assessing the manner of death, the certifying physician decides whether a death will come to the notice of the investigative authorities at all. Assessing the manner of death is thus an extremely responsible task not only from the judicial point of view (detection of homicide), but also in terms of the interests of the bereaved (for example, compensation claims after a fatal accident). “Natural” is a death from an internal cause (disease), where the deceased person has suffered from a disease that can be precisely characterized and from which death was anticipated; the death occurred entirely independently of any external factors of legal significance. The prerequisite for attesting a natural death is thus the existence of an underlying disease of death known from the patient’s medical history with a poor prognosis as to survival.
The problem of “death in old age”.
“Old age” or “senility” is not a cause of death. Underlying diseases and immediate causes of death with a morphology that can be described are always present.
Unnatural deaths.
In Germany, about 4% of all deaths have an unnatural cause.
“Unnatural,” by contrast, is a death attributable to an event caused, triggered, or influenced from outside, irrespective of whether due to the fault of the patient him- or herself or of a third party. Unnatural deaths, therefore, are those due to:
Physical assault
Accident (irrespective of whose fault)
Homicide
Poisoning
Suicide
Treatment errors
Fatal consequences of any of the first six points.
High number of unreported homicides.
According to a multicenter study, it must be assumed that in Germany around 1200 homicides a year go undetected in the medical examination for death certification.
The interval between an external event at the beginning of the causal chain that leads to death and the occurrence of that death can thus be indefinitely long (it may be years). If the cause of death cannot be ascertained when the death certificate is issued, the manner of death will therefore also remain unclear.
Various regulations relating to the certification of death in different states (Länder) in Germany, and a draft outline for a federal-wide death certification process from the German Medical Association, envisage explicitly that attestation of a natural death requires examination of the naked body (e4). Section 3 of the Bavarian Interment Regulations, for example, says, “[…] determination of a natural death requires in every case that the medical external examination on which the death certificate is based be carried out with the body of the deceased completely undressed. This examination of the completely undressed body shall include all regions of the body including all body orifices, the back, and the scalp.”
Sensible though this requirement is, there is no doubt that it is almost regularly disregarded. If the physician fails to meet the required standard of thoroughness, however, he or she has committed a regulatory offence. On the other hand, it must be recognized that completely undressing a dead body in cases of expected death in hospital will not lead to any gain of further information and can face the certifying physician with objective problems (e.g., when complete rigor mortis is established and no support personnel are available to help). Furthermore, this requirement fails to take into account the difference between expected and unexpected deaths. The manner of death remains undetermined if the cause of death cannot be identified on examination even with the help of the medical history. The attestation of natural death always assumes that a clear cause of death can be given. In this connection, it is disturbing that around 50% to 70% of physicians certify a “natural” death for death following femoral neck fracture, 20% for deaths during injections, and 30% to 40% for intraoperative deaths (24).
Definition of “natural cause of death”.
Death from internal morbidity, where the deceased suffered from a disease from which death was expected; the death occurred entirely independently of any external factors of legal significance.
If on the one hand unnatural deaths are considerably under-represented in official statistics, on the other hand both physicians in private practice and those working in emergency departments report attempts by the police to influence them to certify a death as natural although no cause of death is apparent and hence the death ought to be certified as at least unexplained. In an anonymous survey of randomly selected physicians from the area of the Westfalen-Lippe Medical Association, 41% of physicians in private practice and 47% of emergency room physicians reported such attempts to influence death certification (24). The background to these attempts is that investigative authorities have a teleologically narrowed understanding of the term “unnatural death” as meaning “death in which there is a possibility of third-party guilt.” If a natural death is attested, no investigation is necessary. Indicators that a death may be unnatural may arise from the case history and findings: for example, sudden death without a known previous illness, “prima facie” accidents and suicides, farewell letters, etc. Findings that tend to indicate unnatural death are conjunctival hemorrhage, unusual color of livor, remains of tablets in the oral area, and signs of injury.
Unsuitable criteria for indications of natural death are age, especially when no pre-existing life-threatening diseases are known, and the absence of visible trauma.
As regards deaths in hospital, especially when the patient was under medical treatment for a long enough period, the mistake rate should also be relatively low; problem areas here are failure to recognize causal connections to traumas at the beginning of the fatal causal chain, and deaths related to medical procedures. In the inpatient setting, there are occasional reports of initially unrecognized series of killings by physicians or nursing personnel.
The danger of errors and scope for deception are no doubt greatest when the death is certified by private practice physicians in the home; typical mistakes and sources of error, in order of frequency, are:
Inexperience
Carelessness
Careless examination of the body
Consideration of the feelings of relatives.
Added to these, however, are sometimes also unfavorable external conditions, poor lighting, and simply not being adequate to the job, and there are no flexible solutions such as calling in qualified certifying physician. Physicians in private practice especially can find themselves with a collision of interests, since when they are also physician to the relatives of the deceased, attesting an unexplained death puts them at risk of triggering investigations that could lose them the relatives as patients. Compared to a physician in private practice, the hospital physician is in a more protected position (death in the medically dominated environment of a hospital rather than in the private area).
Manner of death “unexplained”.
The manner of death is unexplained when the cause of death cannot be determined at the time of death certification even when the history is taken into account.
Problem areas
Problems that repeatedly arise in the hospital context are:
Deaths in connection with medical interventions, and
Deaths following injury from a fall or other vio–lent events, in which the causal connection with violence from another person or other external event is not recognized and the death is wrongly certified as natural
For deaths that occur unexpectedly in the context of medical interventions, the manner of death should always be given as unexplained, so that an official autopsy can be carried out to investigate the underlying and immediate causes of death objectively. Only on this basis can an opinion be formed on any question of treatment error. Designating the manner of death as -unexplained or unnatural does not signify an admission of treatment error.
For physicians in private practice, the main problems arise when bodies are found at home, patients die unexpectedly, and deaths occur in old age.
Indicators of an unnatural death:
Conjunctival hemorrhages
Color of livor
Remains of tablets in the oral area
Signs of injury
If the cause of death cannot be established from external examination of the corpse or from interviewing any doctors previously involved in treatment, this should be recorded and the manner of death entered as unexplained. With old people, the question is always whether the history and severity of the diagnosed disease explain why death occurred here and at this particular moment. Mistakes and risks in medical examination of the body are summarized in Box 5.
Box 5. Errors and risks in the medical examination for death certification*1.
Beware:
Never certify a death in the absence of definitive sign(s) of death.
Examine the naked body carefully.
-
Review the patient’s medical history:
What was the diagnosis?
What was the sequence of events leading to death?
Can the manner and circumstances in which death occurred be explained by the confirmed diagnosis?
How certain are the diagnoses of the underlying and immediate causes of death?
Was there any external event at the beginning of the causal chain that led to death? If yes, the death should be certified as unnatural.
If the death occurred in the context of medical interventions, the manner of death is unexplained or unnatural.
If the cause of death cannot be established even after interviewing doctors who previously treated the patient, it remains unclear, and so does the manner of death.
Resist attempts to influence how you fill out the death certificate.
Mistakes
Giving the functional end status as cause of death without relating it to an underlying cause
Incorrect sequence from the final cause of death to the underlying cause
Time intervals not stated
Overlooking a causal connection with an external event (e.g., trauma) at the beginning of the causal chain that led to death
*1 modified from (1)
Collision of interests.
General physicians who are also the doctor of relatives of the deceased run the risk of losing those relatives as patients if they certify the death as unexplained.
Whenever the cause of death cannot be established by external examination, an autopsy should be carried out, as is still usual in many of our neighboring countries in Europe. In Germany, the present autopsy rate is less than 5% of all deaths; the rate of hospital autopsies in particular has been dropping sharply in recent years, while judicial autopsies have remained relatively stable at 2% of deaths (compare autopsy rates of 20% to 30% in England and Wales, Sweden, and Finland) (25, e5).
Problems arising in hospital.
Deaths occurring in connection with medical interventions
Deaths occurring after a fall or other violence
These autopsies, which are necessary for valid cause of death statistics and for the planned National Mortality Register, would however have to be adequately remunerated, which at present unfortunately they are not.
A complete (German-language) checklist for certification of death is given at www.aerzteblatt.de/v4/archiv/artikel.asp?src=suche&p=%C4rztliche+Leichen schau&id=39572 and in (e6).
Death in connection with medical intervention.
For these deaths the manner of death should always be given as unexplained, so that an official autopsy can be carried out to investigate the underlying and immediate causes of death objectively.
Certification of death in old age.
When old people die, the question to ask is always whether the history and severity of the diagnosed disease explain why death occurred here and now.
Table 2. Causes of death: examples and important aspects*1.
| Pneumonia |
|
| Infection |
|
| Urinary infection |
|
| Renal failure |
|
| Hepatitis |
|
| Infarction |
|
| Thrombosis |
|
| Pulmonary embolism |
|
| Leukemia |
|
| Alcohol/medical drugs/narcotics |
|
| Complication of surgery |
|
| Dementia |
|
| Accidental death |
|
| Tumor |
|
*1 modified from (25); Federal Statistical Office recommendations on stating cause of death
Further Information On Cme. This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education.
Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire within 6 weeks of publication of the article. See the following website: cme.aerzteblatt.de
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
The solutions to the following questions will be published in issue 41/2010
The CME unit “The Treatment of Patients with HIV” (issue 28–29/2010) can be accessed until 30 August 2010.
For issue 37/2010 we plan to offer the topic “Drug Therapy in Patients With Chronic Renal Failure.”
Solutions to the CME questionnaire in issue 25/2010:
Halis G, et al.: The Diagnosis and Treatment of Deep Infiltrating Endometriosis.
Solutions: 1d, 2e, 3c, 4a, 5d, 6c, 7b, 8d, 9b, 10a
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
A medical examination to certify the cause of death should always be carried out when a human corpse is found. What, in this context, is a human corpse?
A complete leg
A skeleton (at least torso and skull)
A head with only slight signs of decomposition
A stillborn baby with a birth weight of 250 g
A decomposed corpse lacking soft tissue continuity
Question 2
What is a definitive sign of death, signifying that even resuscitation procedures are no longer indicated?
Rigor mortis
Respiratory arrest
Asystole
Areflexia
Hypothermia
Question 3
Which of these is one of the so-called hard causes of death?
Heart failure in a patient with enterocolitis with altered electrolyte balance
Failure of central regulation in a patient with chronic pulmonary emphysema
Uremia in a patient with cardiomyopathy and type 1 diabetes mellitus
Intracerebral hemorrhage in a patient with a ruptured basilar artery aneurysm
Cardiovascular failure in a patient with bacteremia and a sacral grade 3 pressure ulcer
Question 4
A 54-year-old bedridden patient with spastic paralysis and dysphagia following severe craniocerebral trauma, sustained during a robbery 7 years previously, dies as a consequence of aspiration pneumonia.
How long an interval can there be between an external event (in this case craniocerebral trauma) at the beginning of a causal sequence leading to death and the eventual occurrence of death (in this case from aspiration pneumonia) for a death to be certified as unnatural?
One month
One year
Five years
Ten years
Indefinitely long
Question 5
A 42-year-old man on foot under the influence of alcohol is run over by a car. At the hospital, a tibial fracture and multiple abrasions caused by the accident are diagnosed. After conservative treatment of the fracture he is transferred to the internal medicine ward because of his liver cirrhosis, pancreatic fibrosis, and generally poor condition of health with known alcoholism, pre-existing icterus, and diabetic metabolism. Four weeks later he dies in the medical intensive care ward, showing the signs of hepatic coma.
What is the correct causal chain to enter on the death certificate? (1 = immediate cause of death, 2 = due to, 3 = underlying cause)
1) Hepatic coma, 2) tibial fracture, 3) liver cirrhosis
1) Hepatic coma, 2) liver cirrhosis, 3) alcoholism
1) Metabolic decompensation, 2) hepatic coma, 3) tibial fracture
1) Metabolic decompensation, 2) tibial fracture, 3) alcoholism
1) Metabolic decompensation, 2) alcoholism, 3) liver cirrhosis
Question 6
A 58-year-old man is admitted to hospital with symptoms typical of myocardial infarction. Myocardial infarction is confirmed by ECG and laboratory tests. On the way to the cardiac catheterization room the patient suddenly loses consciousness. Subsequent examination suggests that pericardial tamponade has occurred. The patient is asystolic within a few minutes, and as part of the resuscitation measures a great deal of blood is aspirated from the pericardium. Despite attempts at resuscitation, the patient dies. The patient’s history, which is known to the hospital, includes nicotine abuse, arterial hypertension, stenosing coronary sclerosis (patient had had two stents implanted, the most recent 2 years previously), cardiac hypertrophy, and fatty liver.
What is the correct causal chain to enter on the death certificate? (1 = immediate cause of death, 2 = due to, 3 = underlying cause)
1) Pericardial tamponade, 2) coronary heart disease, 3) myocardial infarction
1) Pericardial tamponade, 2) myocardial infarction, 3) coronary heart disease
1) Heart failure, 2) myocardial infarction, 3) coronary heart disease
1) Heart failure, 2) pericardial tamponade, 3) myocardial infarction
1) Heart failure, 2) myocardial infarction, 3) nicotine abuse, arterial hypertension
Question 7
You are called as an emergency doctor to the home of a 5-month-old infant whose father says that the infant suddenly collapsed during feeding. On your arrival, the infant is asystolic and limp, and you start resuscitation measures which continue until the child reaches hospital. After admission, signs of brain death are seen, but no external injuries. CT shows a thin collection of blood in the subdural space.
What do you enter as the immediate cause of death (CD), and what manner of death (MD) do you attest?
CD: Failure of central regulation, MD: natural death
CD: Failure of central regulation, MD: unnatural death
CD: Failure of central regulation, MD: unexplained
CD: Subdural hematoma, MD: natural death
CD: Subdural hematoma, MD: unnatural death
Question 8
A 60-year-old patient is admitted as an inpatient because of severe angina pectoris. Three days later cardiogenic shock occurs, followed by death. Laboratory tests and ECG show signs of fresh myocardial infarction. From the patient’s history it is known that about a year previously the patient sustained thoracic bruising with the fracture of several ribs in a road traffic accident in which he was a passenger, but was discharged apparently in normal condition after a few days. According to relatives, he had had no complaints from that time until the day of his recent admission.
What do you enter as the immediate cause of death (CD), and what manner of death (MD) do you attest?
CD: Myocardial infarction, MD: natural death
CD: Myocardial infarction, MD: unnatural death
CD: Coronary stenosis, MD: natural death
CD: Coronary stenosis, MD: unnatural death
CD: Heart failure, MD: unexplained
Question 9
A 68-year-old woman is found dead in her bed by relatives. They tell you, the out-of-hours doctor on call, who did not know the deceased, that her general condition of health had been sharply deteriorating over the past two weeks due to severe pneumonia. She had absolutely refused to go into hospital. You telephone the patient’s primary care physician from her home and he confirms what the relatives have said; he says that he last visited the patient at home 2 days previously and found her still to have a very high temperature, so he changed her antibiotic. He makes it clear that he assumes the death to have been due to pneumonia from an internal cause. Apart from some small hematomas of variable age on the front of both lower legs, your examination of the body reveals nothing abnormal.
What do you enter as the immediate cause of death (CD), and what manner of death (MD) do you attest?
CD: Respiratory failure, MD: natural death
CD: Respiratory failure, MD: unexplained
CD: Sepsis, MD: unnatural death
CD: Pneumonia, MD: natural death
CD: Pneumonia, MD: unnatural death
Question 10
As emergency doctor, you are called to the body of a 4-month-old male infant at home. The parents say that he had had a cold for 3 days, and on the day before he died they had taken him to the pediatrician, but the pediatrician had judged that there was no cause to worry. The following morning the child was dead in his bed. Your examination shows a normally developed infant with no externally visible injuries or signs of neglect.
What do you enter as the immediate cause of death (CD), and what manner of death (MD) do you attest?
CD: Sudden infant death syndrome, MD: natural death
CD: Respiratory failure, MD: natural death
CD: Unexplained, MD: unexplained
CD: Cerebral hemorrhage, MD: unexplained
CD: Cerebral hemorrhage, MD: unnatural death
Case Illustration. Case illustration showing types of mistake in stating the cause of death—case scenario adapted from (16).
A 75-year-old male smoker with a 5-year history of pulmonary emphysema is admitted to hospital because of an exacerbation of his lung disease. In hospital, Haemophilus influenzae pneumonia is diagnosed. Independently of this, he has a 10-year history of coronary heart disease. While in hospital his condition worsens, but he does not wish to be intubated and artificially ventilated. One week after admission he is found dead in his bed. Four alternative ways of stating the cause of death on the death certificate are shown (A–D).
In this case only alternative D is correct.
Table. Types of mistake in stating cause of death.
| Disease leading to death | Finding | Approximate time interval from onset of disease to death | Mistake type |
| A | |||
| Part 1 | |||
| (a) | Respiratory arrest | – | Functional end status given, time interval from onset of disease to death omitted |
| (b) | – | – | – |
| (c) | – | – | – |
| Part 2 | Coronary heart disease | – | – |
| B | |||
| Part 1 | |||
| (a) | Emphysema | – | Incorrect sequencing of underlying cause and immediate cause of death, time intervals absent |
| (b) | Pneumonia | – | – |
| (c) | – | – | – |
| Part 2 | Coronary heart disease | – | – |
| C | |||
| Part 1 | – | – | – |
| (a) | Emphysema | 5 years | Competing causes of death that have no causal connection |
| (b) | Coronary heart | 10 years | – |
| disease | |||
| Part 2 | – | – | – |
| D | |||
| Part 1 | – | – | |
| (a) | Haemophilus influenzae pneumonia | 1 week | – |
| (b) Emphysema | – | 5 years | – |
| (c) – | – | – | – |
| Part 2 | Coronary heart disease | 10 years | – |
Acknowledgments
Translated from the original German by Kersti Wagstaff MA
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists according to the guidelines of the International Committee of Medical Journal Editors.
References
- 1.Madea B. 2nd edition. Berlin Heidelberg New York: Springer; 2006. Die ärztliche Leichenschau. Rechtsgrundlagen - Praktische Durchführung - Problemlösungen. [Google Scholar]
- 2.Madea B, Dettmeyer R. Ärztliche Leichenschau und Todesbescheinigung. Dtsch Arztebl. 2003;100(48):A 3161–A 3179. [Google Scholar]
- 3.Gross R, Löffler M. Berlin Heidelberg New York: Springer; 1998. Prinzipien der Medizin. Eine Übersicht ihrer Grundlagen und Methoden. [Google Scholar]
- 4.Madea B. Strukturelle Probleme bei der Leichenschau. Rechtsmedizin. 2009;19:399–406. [Google Scholar]
- 5.Madea B, Dammeyer Wiehe de Gomez B, Dettmeyer R. Zur Reliabilität von Leichenschaudiagnosen bei fraglich iatrogenen Todesfällen. Kriminalistik. 2007;12:767–773. [Google Scholar]
- 6.Berzlanovic A, Keil W, Waldhoer T, Sim E, Fasching P, Fazeny-Dörner B. Do centenarians die healthy? An autopsy study. J Gerontol. 2005;60:862–865. doi: 10.1093/gerona/60.7.862. [DOI] [PubMed] [Google Scholar]
- 7.Schelhase T, Weber S. Die Todesursachenstatistik in Deutschland. Probleme und Perspektiven. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2007;50:969–976. doi: 10.1007/s00103-007-0287-6. [DOI] [PubMed] [Google Scholar]
- 8.Modelmog D, Goertchen R. Der Stellenwert von Obduktionsergebnissen. Dtsch Arztebl. 1992;89(42) [Google Scholar]
- 9.Bundesärztekammer. Stellungnahme zur Autopsie. Langfassung. 2005 [Google Scholar]
- 10.Shojania KG, Burton EC, McDonald KM, Goldman L. Changes in rates of autopsy. Detected diagnostic errors over time. A systematic review. JAMA. 2003;289:2849–2856. doi: 10.1001/jama.289.21.2849. [DOI] [PubMed] [Google Scholar]
- 11.Shojania K, Burton E, McDonald K, et al. The autopsy as an outcome and performance measure. Evidence report/technology assessment number 58 (prepared by the University of California at San Francisco-Standford, Evidence-based practice centre under contract no. 290-97-0013) AHRQ Publication for health care research and quality. 2002 Oct; [PMC free article] [PubMed] [Google Scholar]
- 12.Kirch W. Fehldiagnosen und Diagnosefehler in der Inneren Medizin. In: Madea B, Schwonzen M, Winter UJ, Radermacher D, editors. Innere Medizin und Recht. Konfrontation - Kommunikation - Kooperation. Berlin, Wien: Blackwell; 1996. pp. 65–71. [Google Scholar]
- 13.Schwarze EW, Pawlitschko J. Autopsie in Deutschland: Derzeitiger Stand, Gründe für den Rückgang der Obduktionszahlen und deren Folgen. Dtsch Arztebl. 2003;100(43):A 2802–2808. [Google Scholar]
- 14.Magrane BP, Gilliland GF, King DA. Certification of death by family physicians. American Family Physician. 1997;56:1433–1438. [PubMed] [Google Scholar]
- 15.Maudsley G, Williams EN. Inaccuarcy in death certification—where are we now? Journal of Public Health Medicine. 1996;18:59–66. doi: 10.1093/oxfordjournals.pubmed.a024463. [DOI] [PubMed] [Google Scholar]
- 16.Myers K, Farquhar DRE. Improving the accuracy of death certification. CMAJ. 1998;158:1317–1323. [PMC free article] [PubMed] [Google Scholar]
- 17.Feyrter F. Über den ärztlichen Begriff der Todesursache (mit besonderer Berücksichtigung der Todesursache im Sektionsprotokoll des pathologischen Anatomen) Wiener Zeitschrift Innere Medizin und Grenzgebiete. 1946;27:438–456. [Google Scholar]
- 18.Leis J. Die Todesursache unter individual-pathologischen Gesichtspunkten. Deutsche Medizinische Wochenschrift. 1982;107:1069–1072. doi: 10.1055/s-0029-1236771. [DOI] [PubMed] [Google Scholar]
- 19.Thieke Ch, Nitze H. Sterbenstypen: Thanatologische Brücke zwischen Grundleiden und Todesursache. Pathologe. 1988;9:240–244. [PubMed] [Google Scholar]
- 20.Statistisches Bundesamt. Empfehlungen zur Angabe der Todesursache. www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Content/Statistiken/Gesundheit/Todesursachen/Aktuell,templateId= renderPrint.psmle.
- 21.Schrappe M, Lessing C, Conen D, et al. Agenda Patientensicherheit 2008. www.aktionsbuendnis-patientensicherheit.de/apsside/Agenda_2008.pdf.
- 22.Madea B. Autoptisch bestätigte Behandlungsfehler. Zeitschrift für Evidenz, Fortbildung, Qualität im Gesundheitswesen. (ZEFQ) 2008;102:535–541. doi: 10.1016/j.zefq.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 23.Brinkmann B. Fehlleistungen bei der Leichenschau in der Bundesrepublik Deutschland. Ergebnisse einer multizentrischen Studie (I) und (II) Arch Kriminol. 1997;199(2 12):65–74. [PubMed] [Google Scholar]
- 24.Vennemann B, Du Chesne A, Brinkmann B. Die Praxis der ärztlichen Leichenschau. DMW. 2001;126:712–716. doi: 10.1055/s-2001-15033. [DOI] [PubMed] [Google Scholar]
- 25.Brinkmann B, Du Chesne A, Vennemann B. Aktuelle Daten zur Obduktionsfrequenz in Deutschland. DMW. 2002;127:791–795. doi: 10.1055/s-2002-25021. [DOI] [PubMed] [Google Scholar]
- e1.Modelmog D. Deutsche Hochschulschriften 491. Engelsbach: Hänsel-Hohenhausen; 1993. (1993) Todesursachen sowie Häufigkeit pathologisch-anatomischer Befundkomplexe und Diagnosen in einer mittelgroßen Stadt bei fast 100%iger Obduktionsquote. [Google Scholar]
- e2.Eckstein P, Schyma C, Madea B. Rechtsmedizinische Erfahrungen bei der Kremationsleichenschau - eine retorspektive Analyse der letzten 11 Jahre. Arch Kriminol in press. 2010 [PubMed] [Google Scholar]
- e3.Berg S, Ditt J. Probleme der Ärztlichen Leichenschau im Krankenhausbereich. Niedersächsisches Ärztebl. 1984;8:332–336. [Google Scholar]
- e4.Bundesärztekammer 2002. 2nd edition. Berlin Heidelberg New York: Springer; 2006. Entwurf einer Gesetzgebung zur ärztlichen Leichenschau und Todesbescheinigung. In: Madea B (2006) Die Ärztliche Leichenschau Rechtsgrundlagen, Praktische Durchführung, Problemlösung; pp. 213–216. [Google Scholar]
- e5.Doberentz E, Madea B, Böhm U, Lessig R. Zur Relialibität von Leichenschaudiagnosen von nichtnatürlichen Todesfällen - vor und nach der Wende. Archiv für Kriminologie. 2009;225:1–17. [PubMed] [Google Scholar]
- e6.AWMF-Leitlinien Register Nr. 054/002 Regeln zur Durchführung der Ärztlichen Leichenschau. [Google Scholar]