Abstract
Objective: We developed clinical practice guidelines for congenital adrenal hyperplasia (CAH).
Participants: The Task Force included a chair, selected by The Endocrine Society Clinical Guidelines Subcommittee (CGS), ten additional clinicians experienced in treating CAH, a methodologist, and a medical writer. Additional experts were also consulted. The authors received no corporate funding or remuneration.
Consensus Process: Consensus was guided by systematic reviews of evidence and discussions. The guidelines were reviewed and approved sequentially by The Endocrine Society’s CGS and Clinical Affairs Core Committee, members responding to a web posting, and The Endocrine Society Council. At each stage, the Task Force incorporated changes in response to written comments.
Conclusions: We recommend universal newborn screening for severe steroid 21-hydroxylase deficiency followed by confirmatory tests. We recommend that prenatal treatment of CAH continue to be regarded as experimental. The diagnosis rests on clinical and hormonal data; genotyping is reserved for equivocal cases and genetic counseling. Glucocorticoid dosage should be minimized to avoid iatrogenic Cushing’s syndrome. Mineralocorticoids and, in infants, supplemental sodium are recommended in classic CAH patients. We recommend against the routine use of experimental therapies to promote growth and delay puberty; we suggest patients avoid adrenalectomy. Surgical guidelines emphasize early single-stage genital repair for severely virilized girls, performed by experienced surgeons. Clinicians should consider patients’ quality of life, consulting mental health professionals as appropriate. At the transition to adulthood, we recommend monitoring for potential complications of CAH. Finally, we recommend judicious use of medication during pregnancy and in symptomatic patients with nonclassic CAH.
Presented is The Endocrine Society Guideline for the evaluation and management of patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency.
Definition, Pathophysiology, and Morbidities of Congenital Adrenal Hyperplasia (CAH)
CAH is a group of autosomal recessive disorders characterized by impaired cortisol synthesis. The incidence ranges from 1:10,000 to 1:20,000 births (1,2,3,4) and is more prevalent in some ethnic groups, particularly in remote geographic regions (e.g. Alaskan Yupiks). The most common form of CAH is caused by mutations in CYP21A2, the gene encoding the adrenal steroid 21-hydroxylase enzyme (P450c21) (5,6). This enzyme converts 17-hydroxyprogesterone (17-OHP) to 11-deoxycortisol and progesterone to deoxycorticosterone, respective precursors for cortisol and aldosterone. Because this enzyme deficiency accounts for approximately 95% of CAH, we will discuss only 21-hydroxylase deficiency here. The cortisol synthetic block leads to corticotropin stimulation of the adrenal cortex, with accumulation of cortisol precursors that are diverted to sex hormone biosynthesis (Fig. 1). A cardinal feature of classic or severe virilizing CAH in newborn females is genital ambiguity. If the disorder is not recognized and treated, both girls and boys undergo rapid postnatal growth and sexual precocity or, in the case of severe enzyme deficiency, neonatal salt loss and death. About 75% of classic CAH cases suffer aldosterone deficiency with salt wasting, failure to thrive, and potentially fatal hypovolemia and shock (9).
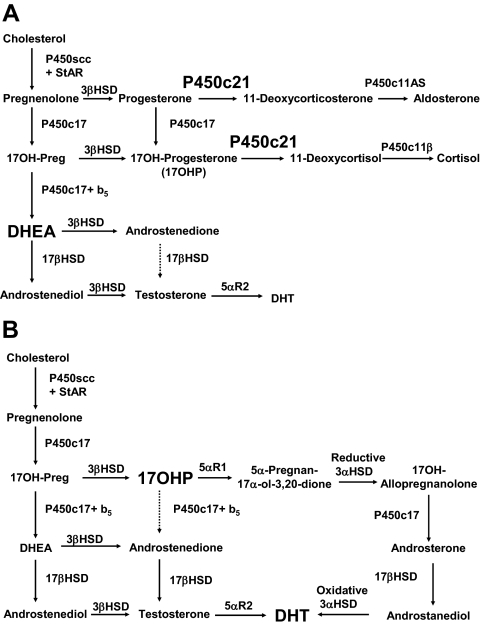
Figure 1.
A, Normal fetal adrenal steroidogenesis. Because the fetal adrenal has low levels of 3β-HSD, most steroidogenesis is directed toward DHEA (and thence to DHEA-sulfate), but small amounts of steroid enter the pathways toward aldosterone and cortisol. The adrenal 21-hydroxylase, P450c21, is essential in both pathways. The adrenal can make small amounts of testosterone via 17β-HSD. B, In the absence of the 21-hydroxylase activity of P450c21, three pathways lead to androgens. First, the pathway from cholesterol to DHEA remains intact. Although much DHEA is inactivated to DHEA-sulfate, the increased production of DHEA will lead to some DHEA being converted to testosterone and dihydrotestosterone (DHT). Second, although minimal amounts of 17-OHP are converted to androstenedione in the normal adrenal, the huge amounts of 17-OHP produced in CAH permit some 17-OHP to be converted to androstenedione and then to testosterone. Third, the proposed backdoor pathway depends on the 5α and 3α reduction of 17-OHP to 17OH-allopregnanolone. This steroid is readily converted to androstanediol, which can then be oxidized to DHT by the reversible 3α-HSD enzyme. Although first discovered in marsupials, mass spectrometric examinations of human urinary steroid metabolites indicate this pathway may also occur in the human adrenal (7,8).
In addition to the so-called classic salt-wasting and simple virilizing forms of CAH, there is also a mild nonclassic form, which may show variable degrees of postnatal androgen excess but is sometimes asymptomatic (10). The mild subclinical impairment of cortisol synthesis in nonclassic CAH (NCCAH) generally does not lead to Addisonian crises.
Nonclassic forms of CAH are more prevalent, occurring in approximately 0.1–0.2% in the general Caucasian population but in up to 1–2% among inbred populations, such as Eastern European (Ashkenazi) Jews (11).
Disease severity correlates with CYP21A2 allelic variation. Genotyping individuals with CAH is fraught with error due to the complexity of gene duplications, deletions, and rearrangements within chromosome 6p21.3 (12). More than 100 CYP21A2 mutations are known (13), but large deletions and a splicing mutation (intron 2, −13 from splice acceptor site, C-G substitution) that ablate enzyme activity comprise about 50% of classic CAH alleles (14,15). A nonconservative amino substitution in exon 4 (Ile172Asn) that preserves approximately 1–2% of enzyme function is associated with simple virilizing classic CAH. A point mutation in exon 7 (Val281Leu) that preserves 20–50% of enzyme function (16) accounts for about 70% of NCCAH alleles (17,18). Because many patients are compound heterozygotes for two or more different mutant CYP21A2 alleles, a wide spectrum of phenotypes may be observed (15).
1.0 Newborn screening
See links to Resources for Newborn Screening in Supplemental Data, Appendix 1, published on The Endocrine Society’s Journals Online web site at http://jcem.endojournals.org.
Recommendation
1.1 We recommend that screening for 21-hydroxylase deficiency be incorporated into all newborn screening programs (1|⊕⊕○○), using a two-tier protocol (initial immunoassay with further evaluation of positive tests by liquid chromatography/tandem mass spectrometry).
1.1 Evidence
CAH is a disease suited to newborn screening because it is common and potentially fatal. Early recognition and treatment can prevent morbidity and mortality. As of 2009, all 50 states in the United States and 12 other countries screen for CAH. Screening markedly reduces the time to diagnosis of infants with CAH (19,20,21,22). Morbidity and mortality are reduced due to early diagnosis and prevention of severe salt wasting. Because undiagnosed infants who die suddenly may not be ascertained, the benefit of screening by direct comparison of death rates from CAH in unscreened and screened populations cannot be readily demonstrated. Indeed, retrospective analysis of sudden infant death in the Czech Republic and Austria identified three genotype-proven cases of classic CAH among 242 samples screened (23). Moreover, males with salt-wasting CAH are more likely than females to suffer from delayed or incorrect diagnosis because there is no genital ambiguity to alert the clinician. Thus, a relative paucity of salt-wasting males is indirect evidence of unreported deaths from salt-wasting crises. In fact, females outnumber males in some (1,24,25) but not all (26) retrospective studies in which CAH was diagnosed clinically. In contrast, salt-wasting CAH patients ascertained through screening programs are equally likely to be male (19,20,22). The death rate in salt-wasting CAH without screening is between 4 and 10% (27,28).
Affected infants ascertained through screening have less severe hyponatremia (mean serum sodium at diagnosis of 134 mm with screening, 124 mm without) (22,29). Learning disabilities have been reported after salt-wasting crises (30); it is not known whether newborn screening reduces the frequency and severity of such abnormalities. Although salt-wasting males would seem to derive the greatest benefit from screening programs, the delay before correct sex assignment of severely virilized females is also markedly reduced (22,31). Moreover, males with simple virilizing disease may otherwise not be diagnosed until rapid growth and accelerated skeletal maturation are detected later in childhood, at which time adult height may already be compromised. Cost-benefit analyses of newborn screening for CAH generally assume that the only adverse outcome of late diagnosis of CAH is death, particularly in males, and thus that the benefit is best quantified in life-years (infants saved by prompt diagnosis, multiplied by life expectancy). Calculations of costs per life-year saved are sensitive to the assumed death rate, and recent estimates have ranged widely from $20,000 (32) to $250,000–300,000 (33). It is conventionally assumed that screening for a particular disease is cost effective at less than $50,000 per life-year (32).
It is difficult to estimate the downstream costs of following up false-positive screens, which may entail a large amount of physician time for evaluation and counseling, plus nursing time and additional laboratory tests if cosyntropin testing is undertaken, Moreover, parents of infants with positive screens may suffer significant psychological distress at the prospect of their children having a potentially life-threatening chronic disease (34). These problems can be ameliorated by adopting screening methods with higher positive predictive values.
1.1 Values and preferences
In making this recommendation, the committee strongly believes that reducing morbidity and mortality from salt-wasting crises is a priority. This recommendation places a lower value in avoiding the incremental expenses of this screening program and subsequent medical care.
Recommendation
1.2 We recommend standardization of first-tier screening tests to a common technology with a single consistent set of norms stratified by gestational age (1|⊕⊕○○).
1.2 Evidence
First-tier screening tests
First-tier screens for CAH employ immunoassays to measure 17-OHP in dried blood spots on the same filter paper (Guthrie) cards as are used for other newborn screening tests (2,3,4). Both RIAs and ELISAs have been almost completely supplanted (9) (in at least 45 states and most European countries) by automated time-resolved dissociation-enhanced lanthanide fluoroimmunoassay (DELFIA) (35).
In interpreting these tests, it must be remembered that 17-OHP levels are normally high at birth and decrease rapidly during the first few postnatal days. In contrast, 17-OHP levels increase with time in infants affected with CAH. Thus, diagnostic accuracy is poor in the first 2 d, which can be problematic if newborns are discharged early. Additionally, premature, sick, or stressed infants typically have higher levels of 17-OHP than term infants and generate many false positives unless higher cutoffs are used. There are no universally accepted standards for stratifying infants, but most U.S. laboratories use a series of birth weight-adjusted cutoffs (9,36,37). Specificity of newborn screening might be improved by using actual gestational age to stratify subjects, rather than birth weight, because 17-OHP levels are much better correlated with gestational age (38). Indeed, in The Netherlands and Switzerland, adopting gestational age criteria improved the positive predictive value of screening (29,39). Finally, antenatal corticosteroid treatment (as used to induce lung maturation in fetuses at risk for premature birth) might reduce 17-OHP levels, but inconsistent effects have been observed in practice (40,41). It is recommended that all such infants be retested after several days of life.
Second-tier screening tests
To obtain adequate sensitivity, the cutoff levels for 17-OHP are typically set low enough that approximately 1% of all tests are reported as positive. Despite the high accuracy of the screening test and given the low prevalence of CAH (about one in 10,000 births), only approximately one in every 100 neonates with a positive screening test will have CAH. Much of the expense of following up positive newborn screening tests could be avoided with a second level of more specific screening. Both biochemical and molecular genetic approaches have been proposed.
Biochemical second screens.
Limitations of immunoassays for 17-OHP include true elevations in levels in premature, sick, or stressed infants and lack of specificity of some antibodies for 17-OHP. Immunoassay specificity can be increased by organic solvent extraction; this is currently mandated as a second screen in four states.
However, liquid chromatography followed by tandem mass spectrometry (LC-MS/MS) more effectively addresses many of these issues (42,43), particularly when steroid ratios are measured. Implementation of this approach improved the positive predictive value of CAH screening in Minnesota from 0.8 to 7.6% during a 3-yr follow-up period (44). In Utah, the positive predictive value improved from 0.4 to 9.3% using similar methodology (45). A modified LC-MS/MS protocol using a ratio of the sum of 17-OHP and 21-deoxycortisol levels, divided by the cortisol level, had a positive predictive value of 100% when this ratio exceeded 0.53 when 1609 samples with a positive primary screen (of 242,500 samples screened by a German program) were tested prospectively (46). If these results can be replicated in other programs, this should become the method of choice for confirming positive screening results. Indeed, if throughput is improved, LC-MS/MS could be used as a primary screen for CAH (47), and problematic immunoassays might be eliminated completely.
Molecular genetic second screens.
CYP21A2 mutations can be detected in DNA extracted from the same dried blood spots that are used for hormonal screening. Because more than 90% of mutant alleles carry one of 10 mutations (deletions or gene conversions), patients carrying none of these mutations are unlikely to be affected. If at least one mutation is detected, the patient is evaluated further. Several studies of genotyping of samples from screening programs have suggested that this is a potentially useful adjunct to hormonal measurements (48,49,50,51), but no large-scale study of efficacy has been reported as a second-tier screen in actual use. Genotyping is more costly than LC-MS/MS on a per-sample basis. Additionally, it is focused on a single gene, i.e. CYP21A2, and will not be helpful in diagnosing other enzyme deficiencies causing CAH, as can be done with LC-MS/MS.
Recommendation
1.3 We recommend that infants with positive newborn screens for CAH be followed up according to specific regional protocols (1|⊕⊕○○).
1.3 Remarks
Cutoff values for screening tests must be empirically derived and vary by laboratory and assay. Whether and when to inform the infant’s physician of record or a pediatric endocrinologist as well depends on the availability of subspecialists. Minimally elevated 17-OHP levels might warrant a second-tier screen from the same blood sample, whereas moderately elevated 17-OHP levels may be followed up with a repeat filter paper specimen. Higher values and signs of impending shock warrant urgent evaluation; in such cases, serum electrolytes and 17-OHP level (LC-MS/MS) are obtained. If the infant manifests clinical signs of adrenal insufficiency and/or abnormal electrolytes, a pediatric endocrinologist should be consulted for appropriate further evaluation and treatment.
The protocol for further evaluation will also depend on local and regional circumstances. Although the gold standard for hormonal diagnosis of CAH is a cosyntropin stimulation test (52), it may be difficult to perform on an urgent basis in many clinical settings. Treatment of infants with positive screens and obvious electrolyte abnormalities or circulatory instability should never be delayed for cosyntropin stimulation testing; in such infants, the adrenal cortex is highly stimulated anyway, and baseline steroids will be markedly elevated.
Extant norms are for tests employing a pharmacological dose of 0.125–0.25 mg cosyntropin (ACTH 1–24). In performing stimulation testing, it should be recognized that 17-OHP may be elevated in other enzymatic defects, particularly 11β-hydroxylase deficiency. One may more fully differentiate the various enzymatic defects potentially causing CAH by measuring 17-OHP, cortisol, deoxycorticosterone, 11-deoxycortisol, 17-OH-pregnenolone, dehydroepiandrosterone (DHEA), and androstenedione after stimulation. Steroid profiling by LC-MS/MS of either serum or urine samples may ultimately supplant stimulation tests (53).
2.0 Prenatal treatment of CAH
Recommendations
2.1 We recommend that prenatal therapy continue to be regarded as experimental. Thus, we do not recommend specific treatment protocols.
2.2 We suggest that prenatal therapy be pursued through protocols approved by Institutional Review Boards at centers capable of collecting outcomes data on a sufficiently large number of patients so that risks and benefits of this treatment can be defined more precisely (2|⊕⊕○○).
2.1–2.2 Evidence
Basic considerations
The mechanism of dexamethasone’s action in the fetus is incompletely understood. Nevertheless, suppression of fetal adrenal androgens in CAH is feasible by administering glucocorticoids (GCs) to the mother (54,55,56). Treatment aims to reduce female genital virilization, the need for reconstructive surgery, and the emotional distress associated with the birth of a child with ambiguous genitalia; prenatal treatment does not change the need for lifelong hormonal replacement therapy, the need for careful medical monitoring, or the risk of life-threatening salt-losing crises if therapy is interrupted. A single approach to prenatal treatment has been studied (57,58), but optimal dosing and duration of treatment have not been determined. Fetal cortisol levels are low in very early gestation, rise during wk 8–12 while the external genitalia are differentiating (59), are only about 10% of maternal levels during midgestation (60,61), and then increase during the third trimester. Thus, the constant dexamethasone dose currently used may result in GC levels that exceed typical midgestation physiological fetal GC levels by about 60-fold (62,63).
CAH is autosomal recessive; if a woman has previously had a child with CAH and again becomes pregnant via the same partner, her fetus will have a one in four chance of having CAH. Because the period during which the genitalia of a female fetus may become virilized begins only 6 wk after conception, treatment must be instituted essentially as soon as the woman knows she is pregnant. Dexamethasone is used because it is not inactivated by placental 11β-hydroxysteroid dehydrogenase type 2 (11β-HSD2) (64). Because treatment must be started at 6–7 wk gestation, and genetic diagnosis by chorionic villous biopsy cannot be done until 10–12 wk, all pregnancies at risk for CAH are treated, even though only one in four is affected. Furthermore, only half of the affected fetuses will be females; hence, treatment is potentially beneficial for only one in eight fetuses.
Obtaining fetal DNA at chorionic villous biopsy reduces the length of time between instituting treatment and obtaining a genetic diagnosis. Knowing the specific mutations carried by each parent substantially increases the efficiency and speed of genetic diagnosis. Fetal sex determination from fetal Y-chromosomal DNA in maternal blood (65,66) has been used in conjunction with prenatal treatment of CAH (67,68). Because early fetal sex determination can improve the probability of treating an affected female fetus from one in eight to one in four, when the technique becomes more consistently accurate in early gestation, it should be a required component of all prenatal treatment research protocols.
At least four factors should be considered in evaluating prenatal treatment of CAH: fetal GC physiology, safety to the mother, safety to the fetus, and efficacy. Because antenatally administered GCs are widely used to induce fetal lung development in the third trimester, many studies have addressed the effects of late-gestation, high-dose, short-term administration, but this may not be germane to prenatal treatment of CAH. Reduced late-term dosing of dexamethasone has been proposed (63,69) and merits further study.
Efficacy
Prenatal administration of dexamethasone has been advocated for the sole purpose of ameliorating or eliminating genital virilization of affected females, reducing the need for genital reconstructive surgery and the psychological impact of virilization. It has been suggested that prenatal dexamethasone may reduce hypothetical androgenization of the fetal female brain, but such effects are difficult to measure and are not the subject of published studies.
Limited data are available concerning treatment outcomes. The evidence regarding fetal and maternal sequelae of prenatal dexamethasone treatment for fetuses at risk for CAH is of low or very low quality due to methodological limitations and small sample sizes (70,272). In the largest single series (58), among 532 pregnancies assessed for carrying a fetus with CAH, prenatal treatment was initiated in 281. Among 105 with classic CAH (61 females, 44 males), dexamethasone was given throughout pregnancy to 49. Among 25 CAH-affected females receiving dexamethasone before the ninth week of pregnancy, 11 had normal female genitalia, 11 had minimal virilization (Prader stages 1–2), and three were virilized (Prader stage 3); the mean Prader score for this group was 1.0. Among 24 female fetuses where treatment was begun after wk 9, the genitalia averaged a Prader score of 3.0. Those never treated were most virilized, averaging 3.75. The group first describing prenatal treatment has reported treating 253 pregnancies (71), indicating that “prenatal therapy is effective in significantly reducing or even eliminating virilization in CAH females” and that “the success rate is over 80%.” However, these reports do not provide actual numbers describing their outcomes and did not include control groups of nontreated pregnancies. In a small, carefully done study, three of six female fetuses treated to term were unvirilized, two had mild virilization to Prader stage 2, and a poorly compliant mother had a girl with Prader 2–3 genitalia (72). Thus, the groups advocating and performing prenatal treatment appear to agree that it is effective in reducing and often eliminating virilization of female fetal genitalia and that the success rate is about 80–85%.
Maternal safety
Among 118 women treated to term who responded to a mailed questionnaire, the mean pregnancy-associated weight gain was 7.1 lbs (3.2 kg) greater than that experienced by untreated women (P < 0.005); these women also reported increased striae (P = 0.01) and increased edema (P = 0.02) but no reported increase in hypertension or gestational diabetes (58). A review lacking a control group indicated that 9–30% of treated women complained of mild gastric distress, weight gain, mood swings, pedal edema, and mild hypertension and that only 1.5% of 253 treated women had serious complications including striae, large weight gain, hypertension, preeclampsia, and gestational diabetes (57). A carefully controlled study of 44 women receiving prenatal dexamethasone (only six to term) found increased weight gain in mothers treated during the first trimester, but this difference was absent at term. There were no differences in maternal blood pressure, glycosuria, proteinuria, length of gestation, or placental weight. However, in response to a questionnaire, compared with untreated controls, treated women reported increased appetite (P < 0.01), rapid weight gain (P < 0.02), and edema (P = 0.04), and 30 of the 44 women indicated they would decline prenatal treatment of a subsequent pregnancy (72). Other uncontrolled reports document Cushingoid effects in small numbers of treated women (73). Thus, multiple studies indicate that prenatal treatment is associated with modest but manageable maternal complications that do not appear to pose a major risk to the mother.
Fetal safety
Many reports of teratogenic effects, especially orofacial clefts, produced by high doses of dexamethasone administered to pregnant animals (74,75,76) and in human patients (77,78,79) led the U.S. Food and Drug Administration to classify dexamethasone as a category B drug, whose safety in pregnancy is not established. Prescription of dexamethasone for prenatal treatment of CAH is an off-label use in the United States and European Union. No teratogenic effects have been identified with high-dose GCs administered during gestation; however, these studies concerned steroids that are inactivated by placental 11β-HSD2 and as such do not affect the fetus (80,81). A case-control study of 662 infants with orofacial clefts and 734 controls found higher incidences of isolated cleft lip (odds ratio 4.3) or cleft palate (odds ratio 5.3) among mothers who used GCs “during the 4-month periconceptual period” (82). A multicenter case control study by the same group surveying GC exposure among 1141 cases of cleft lip (with or without cleft palate), 628 with cleft palate, and 4143 controls found a lower risk (odds ratio = 1.7; 95% confidence interval = 1.1–2.6). The data suggested greatest risk for exposure between 1–8 weeks, but the numbers were small (odds ratio = 7.3; 95% confidence interval = 1.8–29.4) (83).
Because newborn birth weight correlates with adult incidences of ischemic heart disease and hypertension (84,85) and because moderately low-dose dexamethasone (100 μg/kg) reduced birth weight and increased blood pressure in rats (86), concern was raised about the effects of prenatal dexamethasone treatment in CAH (87,88,89). Prenatal dexamethasone alters postnatal renal structure and function and produces hypertension in rodents (90,91). One year after prenatal exposure of nonhuman primates to 120 μg/kg dexamethasone, there were reduced pancreatic β-cell numbers, impaired glucose tolerance, increased systolic and diastolic blood pressure, and reduced postnatal growth despite normal birth weight (92). Follow-up reports of prenatally treated children have reported birth weights in the normal range (56,57,71,72) but are nevertheless reduced by about 0.4–0.6 kg in the largest studies (58). The magnitude of this change in birth weight is equivalent to or greater than that seen with maternal cigarette smoking (93). The long-term significance of this reduction in mean birth weight remains of concern.
It is uncertain whether GCs are required for normal human development. A child born with complete generalized GC resistance had no major organ defects (94). Clearly, high doses of GCs exert negative effects in fetal animals (95,96). Dexamethasone administered to pregnant sheep during early gestation in doses similar to those used in CAH prenatal therapy altered fetal adrenal and placental steroidogenesis (97). Betamethasone treatment in mid to late gestation reduced brain weight (98,99) and neuronal myelinization (100) in fetal sheep. High doses of maternally administered dexamethasone also disrupted development of hippocampal neurons in late-term fetal rhesus monkeys (101). Whether these observations are relevant to reports of mild emotional and cognitive disturbances in prenatally treated children is not clear. Questionnaires administered to dexamethasone-treated children showed more shyness and inhibition (102). A questionnaire study of 174 children prenatally treated and 313 untreated control children found no differences between treated and untreated groups with respect to nine social/developmental scales (103). A small but rigorous study, using a standardized treatment protocol, questionnaires, and standardized neuropsychological tests administered by a clinical psychologist, compared prenatally treated children and a control group matched for age and sex. No differences were found in intelligence, handedness, or long-term memory. However, CAH-unaffected children prenatally treated short term had poorer verbal working memory, rated lower on self-perception of scholastic competence (both P = 0.003), and had increased self-rated social anxiety (P = 0.026) (104). The parents of the prenatally treated children described them as being more sociable than controls (P = 0.042); there were no differences in psychopathology, behavioral problems, or adaptive functioning (105). Systematic review and metaanalysis of these publications have not detected significant differences in behavior or temperament (70), and only a single small study indicates a modest but measurable effect of dexamethasone on postnatal cognitive function (104).
Given the small number of potentially affected patients being treated, clinical research of prenatal treatment should be conducted only in centers of excellence coordinating treatment protocols in multicenter studies with standardized registries. Such approaches may provide robust data to guide practice sooner than individual center studies testing idiosyncratic protocols with limited statistical power. Although these will have less protection against bias, centers that have already treated many pregnancies should perform and publish studies of their experience with emphasis on the physical and psychological outcomes in childhood and adolescence, distinguishing between patients treated short term and long term.
2.1–2.2 Values and preferences
The prenatal treatment of CAH remains controversial and poses unresolved ethical questions (62,87,89,106,107,108,109,110,111). The concern is treating seven unaffected and/or male fetuses to treat one affected female in the context of inadequate data regarding the long-term risks of this ther-apy. Prenatal treatment of CAH is directed toward reducing the need for surgery, rather than toward preserving life or intellectual capacity. Therefore, in validating earlier expert opinion, this Task Force placed a higher value on preventing unnecessary prenatal exposure of mother and fetus to dexamethasone and avoiding potential harms associated with this exposure and a relatively lower value on minimizing the emotional toll of ambiguous genitalia on parents and patients.
3.0 Diagnosis of NCCAH/CAH after infancy
Recommendations
3.1 We recommend obtaining an early morning baseline serum 17-OHP in symptomatic individuals (1|⊕⊕○○).
3.2 We recommend obtaining a complete adrenocortical profile after a cosyntropin stimulation test to differentiate 21-hydroxylase deficiency from other enzyme defects and to make the diagnosis in borderline cases (1|⊕⊕○○).
3.3 We suggest genotyping only when results of the adrenocortical profile after a cosyntropin stimulation test are equivocal or for purposes of genetic counseling (2|⊕○○○).
3.1–3.3 Evidence
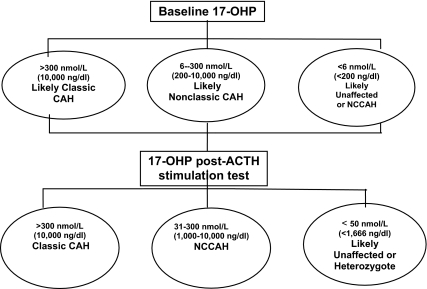
The diagnosis of 21-hydroxylase deficiency is based on measuring 17-OHP, the enzyme’s principal substrate, and excluding 11-hydroxylase and P450 oxidoreductase deficiencies, in which 17-OHP may also be elevated. A sample diagnostic strategy is portrayed in Fig. 2.
Figure 2.
Diagnosis of CAH after infancy. Reference standards for hormonal diagnosis derived from Refs. 115,218,219 and 273. Note that randomly measured 17-OHP levels can be normal in NCCAH; hence, a screening 17-OHP level should be measured in the early morning (before 0800 h). Steroid measurements may differ with the assay employed. Classic CAH includes both salt-wasting and simple virilizing forms of 21-hydroxylase deficiency.
Other steroids whose levels are usually elevated include 21-deoxycortisol, androstenedione, and testosterone. Elevated plasma renin activity (PRA) and a reduced ratio of aldosterone to PRA indicate impaired aldosterone synthesis and can differentiate salt wasters from simple virilizers (112) after the newborn period.
The severity of hormonal abnormalities depends on the degree of the enzymatic impairment, which depends on the genotype. A genetic test cannot detect salt wasting; this requires careful clinical evaluation. For example, genotyping may reveal the IVS2 mutation, which is seen in both salt-wasters and non-salt-wasters (15,113,114). Compound heterozygotes for two different CYP21A2 mutations usually have a phenotype compatible with the milder mutation. Heterozygotes have slightly elevated 17-OHP levels after ACTH stimulation, but there is overlap with unaffected subjects (115). Other analytes have been used as markers of heterozygosity (116,117), but genotyping is a usually superior method of heterozygote detection.
4.0 Medical treatment of CAH in growing patients
Recommendations
Glucocorticoids
4.1 We recommend maintenance therapy with hydrocortisone (HC) tablets in growing patients with classic CAH (1|⊕⊕⊕○).
4.2 We recommend against the use of oral HC suspension and against the chronic use of long-acting potent GCs in growing patients (1|⊕⊕○○).
4.3 We recommend monitoring patients for signs of GC excess as well as for signs of inadequate androgen suppression (1|⊕⊕○○).
Mineralocorticoids (MCs)
4.4 We recommend that all patients with classic CAH be treated with fludrocortisone and sodium chloride supplements in the newborn period and early infancy (1|⊕⊕○○).
4.1–4.4 Evidence
The goal of therapy is to reduce excessive androgen secretion by replacing the deficient hormones. Proper treatment with GCs prevents adrenal crisis and virilization, allowing normal growth and development. Clinical management of classic CAH is a difficult balance between hyperandrogenism and hypercortisolism. Undertreatment carries the risk of adrenal crisis and allows increased adrenal androgen production, with accelerated bone age and loss of growth potential; overtreatment may suppress growth, increase blood pressure, and cause iatrogenic Cushing’s syndrome.
For initial reduction of markedly elevated adrenal hormone levels in infancy, one may exceed the recommended GC doses, but it is important to rapidly reduce the dose when target steroid levels are achieved. Frequent reassessment is needed in infancy. Attempts to completely normalize 17-OHP levels typically result in overtreatment. During childhood, the preferred GC is HC because its short half-life minimizes the adverse side effects of more potent longer-acting GCs, especially growth suppression (118). In one trial, the estimated growth-suppressive effect of prednisolone was about 15-fold more potent than HC (119); dexamethasone is 70- to 80-fold more potent (120). HC suspension and HC tablets are not bioequivalent, and HC oral suspension may be inadequate to control CAH in children (121) due to uneven distribution of the drug in liquid. Good control can be achieved by orally administering crushed HC tablets mixed with a small volume of liquid immediately before administration. Insufficient data exist to recommend higher morning or evening doses (122). When doses exceed 20 mg/m2 · d in infants and 15–17 mg/m2 · d in adolescents, there is loss of height sd score (SDS) and shorter adult height SDS (123,124,125,126,127). Table 1 provides suggested dosing guidelines. Thus, although prednisolone and dexamethasone treatment are effective in suppressing adrenal androgens in children with CAH, these more potent drugs are more likely to impede statural growth and cannot be routinely recommended.
Table 1.
Maintenance therapy in growing CAH patients
| Drugs | Total dose | Daily distribution |
|---|---|---|
| GCs: HC tablets | 10–15 mg/m2 · d | 3 times/d |
| MCs: fludrocortisone tablets | 0.05–0.2 mg/d | 1–2 times/d |
| Sodium chloride supplements | 1–2 g/d (17–34 mEq/d) in infancy | Divided in several feedings |
The doses and schedules are meant as examples and should not be construed as a restrictive menu of choices for the individual patient.
During puberty, despite adequate replacement therapy and compliance, control may be suboptimal because of increased cortisol clearance (128). Adult height of CAH patients correlates negatively with the dose of GC administered in early puberty; patients treated with less than 20 mg HC/m2 · d at start of puberty are significantly taller than those who were given higher HC doses. Therefore, as with younger patients, it is important during puberty to treat with the lowest possible dose (118).
At or near completion of linear growth, long-acting GCs may be used (see Table 2), although HC remains a treatment option. Prednisolone suspension or dexamethasone elixir can be used to titrate the dose more finely than with tablets.
Table 2.
Maintenance therapy suggested in fully grown patients
| Type of long-acting GC | Suggested dose (mg/d) | Daily doses |
|---|---|---|
| HC | 15–25 | 2–3 |
| Prednisone | 5–7.5 | 2 |
| Prednisolonea | 4–6 | 2 |
| Dexamethasonea | 0.25–0.5 | 1 |
| Fludrocortisone | 0.05–0.2 | 1 |
Suspension or elixir may permit better dose titration for these drugs.
Infants with salt-wasting 21-hydroxylase deficiency require MCs in addition to GC treatment as well as supplemental sodium chloride. The requirement for sodium in normally growing infants is approximately 1 mmol/kg · d, the amount provided by human milk. However, in salt-wasting CAH patients, the sodium content of breast milk or infant formulas is insufficient, and sodium chloride supplements are necessary (129).
Although the aldosterone biosynthetic defect is clinically apparent only in the salt-wasting form, subclinical aldosterone deficiency is present in all forms of 21-hydroxylase deficiency (112,130,275) and can be best evaluated by the aldosterone to PRA ratio. The latter decreases with increasing phenotypic severity, clearly demonstrating a spectrum of salt loss in the various forms of 21-hydroxylase deficiency (112). Consequently, all patients with elevated PRA or aldosterone to PRA ratio benefit from fludrocortisone therapy and adequate dietary sodium. Maintenance of sodium balance reduces vasopressin and ACTH levels, contributing to lower GC doses, leading to better auxological outcomes (108,123,131).
Sensitivity to MCs may vary over time, and recovery from salt wasting has been described in some patients, most probably secondary to extraadrenal 21-hydroxylation (132,133). Therefore, the need for continuing MCs should be reassessed periodically based on blood pressure, PRA, and the aldosterone to PRA ratio. It is particularly important to monitor blood pressure in infants who are often initially treated with high doses of MC due to immature renal tubular capacity to reabsorb sodium.
4.1–4.4 Values and preferences
The proposed GC choice places higher value on reducing the negative effects on growing children than on convenience and compliance.
Recommendations
Stress dosing
4.5 We recommend increasing the GC dosage of CAH patients in situations such as febrile illness (>38.5 C), gastroenteritis with dehydration, surgery accompanied by general anesthesia, and major trauma (1|⊕⊕○○).
4.6 We recommend against the use of increased GC doses in mental and emotional stress and minor illness and before physical exercise (1|⊕○○○).
4.7 We recommend against the use of stress doses of GC in patients with NCCAH unless their adrenal function is suboptimal or iatrogenically suppressed (1|⊕○○○).
4.8 We suggest that patients who require treatment always wear or carry medical identification indicating that they have adrenal insufficiency (2|⊕○○○).
4.5–4.8 Evidence
Patients with severe forms of 21-hydroxylase deficiency are unable to produce a sufficient cortisol response to physical stress, such as febrile illness, gastroenteritis with dehydration, surgery, or trauma, and therefore require increased doses of GC during such episodes (Table 3). When pharmacological doses of HC are given, MCs are not needed because HC can activate MC receptors. Maintenance doses should be resumed when the patient is stable. Patients should avoid fasting during acute illnesses; glucose and electrolyte supplementation should be given to young children due to risk of hypoglycemia and electrolyte imbalance.
Table 3.
Suggested stress doses of GC
| Patient age | Initial parenteral HC dose (mg) |
|---|---|
| Infants and preschool children | 25 |
| School-age children | 50 |
| Adults | 100 |
Successive iv HC doses are given as three to four times maintenance doses per day, divided every 6 h.
Exercise and psychological stresses (e.g. anxiety and examinations) (134) do not require increased GC dosing (135).
Recommendations
Monitoring therapy in growing children
4.9 We recommend monitoring treatment by consistently timed hormone measurements (1|⊕○○○).
4.10 We recommend that endogenous adrenal steroid secretion not be completely suppressed to avoid adverse effects of overtreatment (1|⊕⊕○○).
4.11 We suggest regular monitoring of height, weight, and physical examination; annual bone age assessment is suggested after age 2 yr (2|⊕○○○).
4.9–4.11 Evidence
Monitoring treatment is difficult in CAH. Normal growth and growth velocity are important variables in children. Either a reduced or an accelerated height velocity, signs of virilization, and delayed or premature bone maturation usually occur after protracted under- or overtreatment. Laboratory data should indicate the need for dose adjustment before growth and physical changes occur. 17-OHP, androstenedione, and testosterone are the best indicators of the adequacy of GC treatment. Steroid measurements can be performed in blood, saliva (136,137), urine (138), or dried filter paper blood samples (139,140). Assays of sufficient sensitivity such as immunoassays after extraction and chromatography, or LC/MS-MS, should be used in conjunction with appropriate reference data (42,141). Normal levels of 17-OHP and the other steroids are not a treatment goal but instead indicate overtreatment. ACTH measurements are not useful for a diagnostic or therapeutic profile in CAH patients. Acceptably treated CAH patients generally have mildly elevated steroid levels when measured in a consistent manner, and dose adjustments should be made in the context of the overall clinical picture and not solely based on a single 17-OHP measurement.
5.0 Treatment of NCCAH
Recommendations
5.1 We suggest treating NCCAH children with inappropriately early onset and rapid progression of pubarche or bone age, and adolescent patients with overt virilization (2|⊕⊕○○).
5.2 We recommend against treatment in asymptomatic individuals with NCCAH (1|⊕⊕○○).
5.3 We suggest that previously treated NCCAH patients be given the option of discontinuing therapy when symptoms resolve (2|⊕⊕○○).
5.1–5.3 Evidence
Our unsystematic clinical observations suggest that children with inappropriately early onset of body hair and odor should be treated only when bone maturation is sufficiently accelerated to adversely affect height. In the presence of premature pubarche without advanced bone age, treatment can be withheld during careful monitoring. In adolescents with irregular menses and acne, symptoms are usually reversed within 3 months of GC treatment, whereas remission of hirsutism is more difficult to achieve with GC monotherapy. As in other androgenic disorders, treatment of hirsutism may be best served by the addition of an oral contraceptive and/or antiandrogens (142,143).
6.0 Complications of CAH
Recommendations
6.1 We recommend close monitoring for iatrogenic Cushing’s syndrome in all GC-treated patients (1|⊕⊕○○).
6.2 We suggest against the routine evaluation of bone mineral density (BMD) in children (2|⊕○○○).
6.3 We suggest that adrenal imaging be reserved for those patients who have an atypical clinical or biochemical course (2|⊕○○○).
6.1–6.3 Evidence
Prolonged steroid therapy may reduce BMD. However, in CAH children and adolescents on standard GC therapy (10–20 mg/m2), there is no evidence of decreased BMD assessed by dual-energy x-ray absorptiometry and normalized for height, irrespective of duration of treatment, type of GC used, and 17-OHP or androgen levels (144,145,146,147). Longitudinal follow-up studies of BMD from childhood to adulthood would be useful. At present, the standard of care for good bone health includes age-appropriate vitamin D and calcium intake along with weight-bearing exercise.
Adrenal masses affect 1–4% of normal men and women (148). Their prevalence in autopsy samples increases with age, being 0.2% in young adults and 7% in subjects older than 70 yr (149). A high prevalence of benign adrenal masses has been observed by computed tomography imaging in adults with CAH, especially among those on inadequate GC therapy (150). Adrenal carcinomas have rarely been reported in adults (151) and in only two pediatric patients with CAH (152,153). Insufficient data exist to recommend routine screening for adrenal masses. If an adrenal incidentaloma is discovered in a patient not known to have CAH, the various forms of CAH should be excluded by appropriate testing (152).
The prevalence of testicular adrenal rests in boys with classic CAH aged 2–18 yr varies from 21–28% (154,155,156); there have been no such studies in NCCAH males. These so-called testicular adrenal rest tumors are benign, often related to suboptimal therapy, and usually decrease in size after optimization of GC therapy (157). Testicular masses in boys with classic CAH are usually bilateral and smaller than 2 cm in diameter and therefore not palpable but detectable by ultrasound (US) (154,155,156).
Irregular menstrual cycles are common in females with inadequately treated classic CAH (158,159). However, in a controlled study of 62 adult women with CAH (160), there was no difference in the prevalence of irregular menses between treated CAH and control women. Menstrual irregularity is typically one of the presenting signs (161,162) in NCCAH. A polycystic ovary syndrome type of functional ovarian hyperandrogenism may cause irregular menses in women with well-controlled CAH (163,164); the hyperandrogenism and menstrual irregularity of such individuals benefits from additional therapy with second- or third-generation oral contraceptives. Studies in a limited number of adolescent CAH patients showed a prevalence of polycystic ovaries on US corresponding to that in the general population (165,166). If one examines unselected populations of hyperandrogenic, hirsute women, or patients in fertility clinics, the incidence of NCCAH is 2–4% (167,168,169).
Children with CAH have a higher body mass index than do controls due to increased fat mass (170). Studies in pediatric patients showed that approximately half are overweight, and 16–25% are obese (170,171,172). Hypertension is more prevalent in children with classic CAH than in the general population, and systolic blood pressure was related to body mass index independent of GC or MC therapy (173,174). In a small group of prepubertal children with classic CAH, serum leptin and insulin concentrations were significantly higher than those of healthy counterparts. Whereas subtle insulin resistance can be detected in untreated NCCAH (274), frankly impaired glucose tolerance is uncommon. Oral glucose tolerance was normal in nine of 10 girls with classic CAH aged 8–20 yr (165). Inconsistent data have been reported on triglyceride levels, with one study reporting higher levels in a group of prepubertal patients on GC treatment compared with age-matched controls (175) and another showing a lipid profile in CAH children similar to that of controls (176). These differences probably reflect small sample sizes in both studies.
In view of increased body fat and potential metabolic consequences, we suggest that lifestyle counseling to counteract these trends begin early.
7.0 Feminizing surgery
Recommendation
7.1 We suggest that for severely virilized (Prader stage ≥ 3) females, clitoral and perineal reconstruction be considered in infancy and performed by an experienced surgeon in a center with similarly experienced pediatric endocrinologists, mental health professionals, and social work services (2|⊕⊕○○).
7.1 Evidence
For goals and functional outcomes of genital surgery, see section 10.0, Mental health. There are no randomized controlled studies of either the best age or the best methods for feminizing surgery. The results must be evaluated at adult ages, often 20 yr or more after the initial surgery, and during that time methods may have changed several times.
The timing for vaginoplasty is debated; however, we suggest that in patients with a low vaginal confluence, complete repair including vaginoplasty, perineal reconstruction, and clitoroplasty (if necessary) be done simultaneously at an early age. For individuals with higher vaginal confluence, the timing is less certain. The implied surgical advantage of delayed reconstruction is that the risk of vaginal stenosis and the need for subsequent dilation is diminished. In infants with severe virilization where clitoroplasty is being considered, the advantages of early complete reconstruction are that the phallic skin can also be used as part of the vaginal reconstruction and gives the surgeon much more flexibility. In the neonatal period, the recent exposure to placental estrogens leads to more elastic vaginal tissue, facilitating vaginal reconstruction (177).
If surgery is deferred, vaginoplasty and/or clitoroplasty may be performed in adolescence. Systematic long-term evaluation is lacking for both early and late surgery, for which significant postoperative complications may occur, such as urethra-vaginal fistulae and vaginal stenosis. There are no data comparing psychosexual health in girls and women who have undergone early and late surgery. Parents should be provided with balanced information about timing, risks and benefits of surgery; they should be informed that deferring surgery is an option. It is important that the long-term prognosis for sexual and reproductive function be discussed. There is no evidence at this time that either early or late surgery better preserves sexual function.
7.1 Values and preferences
Presumed values in seeking early surgery are reducing parental anxiety and easing acceptance of the child’s congenital anomaly, avoiding stigmatization of a girl with masculinized genitals, and avoiding the psychological trauma of genital surgery during adolescence. Presumed values of late surgery are patient autonomy regarding surgery that may damage sexual function.
7.1 Remarks
Genital reconstructive surgery requires both surgical experience and the endocrine, anesthesia, nursing, and psychosocial support that is found only in centers that do this procedure regularly.
Recommendation
7.2 We suggest neurovascular-sparing clitoroplasty and vaginoplasty using total or partial urogenital mobilization (2|⊕○○○).
7.2 Evidence
The description of total urogenital mobilization by Peña (178) signaled a significant advance in the surgical management of CAH. The basic technique involves a 360° mobilization of the entire urogenital sinus, which is then brought to the perineum. In partial urogenital mobilization, dissection is avoided superior to the urethra under the pubic bone, a nerve-rich zone that contains the sphincteric musculature necessary for urinary continence. Urinary incontinence and vaginal stenosis requiring dilation or reoperation remain a postoperative concern but have not been reported by either Peña (179) or Rink (180,181,182). Long-term follow-up is necessary to confirm these findings. This recommendation is based on the poor results of other forms of vaginoplasty (147,183), including flap vaginoplasty for severe CAH and vaginal pull-through separating the urethra and vaginal components, and is consistent with the consensus statement on 21-hydroxylase deficiency from the Pediatric Endocrine Society (formerly known as Lawson Wilkins Pediatric Endocrine Society) and the European Society for Pediatric Endocrinology (107).
Recommendation
7.3 We suggest continued long-term outcome studies of early surgery.
7.3 Evidence
In contrast to other significant congenital abnormalities of the genitourinary system (bladder exstrophy, prune belly syndrome, and posterior urethral valves), the incidence of urogenital sinus anomalies associated with CAH has not decreased. Thus, there is a continuing need to derive evidence-based guidelines for surgical treatment of CAH. A metaanalysis and systematic review of the surgical treatment of CAH in 5 yr is a reasonable goal.
7.3 Values and preferences
The majority of women with CAH surveyed favored genital surgery before adolescence (184,185). The Task Force shares the stated preference of the majority of patients and places a high value on the outcomes of early complete repair done by surgeons experienced with either total or partial urogenital mobilization, e.g. reduced need for dilation in adolescence or adulthood and maintaining normal perineal and clitoral sensation.
7.3 Remarks
The decision of whether or when to perform surgery is often difficult. The pediatric endocrinologist, surgeon, social worker, and mental health professionals should meet as a team to discuss various options with the family and continue to provide support. Patient and parent support groups may also be enlisted to provide guidance to the family and relate experiences of those who have recently made such decisions.
8.0 Experimental therapies
Childhood experimental therapies to enhance growth
Recommendations
8.1.1 We suggest that children with CAH who have a predicted height sd of −2.25 or below be considered for experimental treatment in appropriately controlled trials (2|⊕○○○).
8.1.2 We recommend against use of experimental treatment approaches outside of formally approved clinical trials (1|⊕⊕○○).
8.1.3 We suggest further prospective, randomized, and carefully controlled studies to determine whether the use of growth-promoting drugs increases adult height in patients with CAH (2|⊕○○○).
8.1.1–8.1.3 Evidence
The goal of many new treatment approaches is to normalize growth and development in children with CAH. The adult short stature of many CAH patients may be caused by hypercortisolism, hyperandrogenism, or both. Retrospective studies show that adult height is relatively independent of adrenal androgen levels in treated patients (186,187,188). In a study of 341 treated patients with classic CAH, 124 were examined at adult height. Males and females were 10 and 8 cm shorter than expected, respectively (189). A metaanalysis of data from 18 centers worldwide showed that the mean adult height of patients with classic CAH was 1.37 sd (10 cm) below the mean, and patients diagnosed before 1 yr of age had increased adult height outcomes (0.54 sd) (190). In nonsystematic reviews, patients who were diagnosed late or were exposed to GC doses higher than 15 mg/m2 · d had diminished height (191,192). Overtreatment during infancy (126,193) or treatment with long-acting, high-potency GCs may also reduce height (118). The pubertal growth spurt is attenuated in CAH adolescents (118). Despite these concerns, height approximating target height has been reported in patients with strict adherence to thrice-daily medication and monitoring every 3 months (118,194,195). Thus, vigilance during the first 2 yr of life and during puberty is important in optimizing height.
A systematic review and metaanalysis of adult height in patients with classic CAH diagnosed before age 5 yr was prepared in conjunction with these guidelines (131). Of 1016 published reports, only 35 met eligibility criteria for inclusion in the analysis. All were observational studies with methodological limitations, graded very low-quality evidence. Most patients were diagnosed before the era of newborn screening, fewer than half reported a mean age of diagnosis under 1 yr, and most did not give details of GC doses. The pooled data indicated a corrected adult height SDS of −1.05. Subgroup analysis revealed that the addition of MC treatment was associated with increased height outcome. Age at diagnosis, sex, type or dose of steroid, and age of onset of puberty did not significantly influence adult height; however, these subgroup analyses were inconclusive.
Patients with NCCAH can also have compromised adult height, but height deficit is less severe than with classic CAH. However, there is limited evidence that initiation of GC treatment before puberty might improve adult height (187,196). Similarly, there are limited studies evaluating drugs that enhance growth in children with classic CAH.
A four-drug regimen of the antiandrogen flutamide, the aromatase inhibitor testolactone, reduced HC (8 mg/m2 · d), and fludrocortisone decreased growth rate, weight velocity, and bone maturation as compared with conventional treatment with HC and fludrocortisone in a crossover study of 12 children (197). In a 2-yr randomized parallel study of 28 children, patients receiving the experimental four-drug regimen had normal linear growth and bone maturation, despite elevated adrenal androgens (198). Long-term safety data are unknown; blood chemistries and liver function must be carefully monitored during treatment with synthetic antiandrogens.
A 1- to 2-yr nonrandomized study of children with CAH showed improved growth rate and height z score for bone age for GH used alone (n = 12) or in combination with GnRH agonist (GnRHa) (n = 8; P < 0.0001) (199). A combined regimen of GH and GnRHa was administered to 14 patients selected for a predicted height of more than 1 sd below target height. Patients treated with this regimen plus conventional therapy for approximately 4 yr had improved adult height (+1.1 sd) (200). Adult height of the patients treated with this combined regimen for approximately 4 yr was greater than the adult height of matched historical CAH controls treated with conventional therapy alone (sd −0.4 vs. −1.4, P = 0.01). GnRHa treatment increases adult height in CAH children who develop central precocious puberty (201). No randomized study has investigated the effect of GnRHa alone on adult height in children with CAH and normally timed puberty.
Well-designed, large, randomized, controlled studies of experimental drugs aimed at improving adult height of children with CAH are needed. Present evidence is insufficient to warrant recommending use of sex steroid blockade, GH, or GnRHa in children with CAH outside of controlled Institution Review Board-approved trials. Normal adult height can be achieved in CAH with judicious use of standard GC and MC therapies, and height-enhancing drugs are not recommended for individuals whose height is, or is expected to be, more than −2.25 sd.
See links to Resources for Clinical Trials on CAH in Supplemental Material, Appendix 1.
8.1.1–8.1.3 Values and preferences
In recommending further research on experimental therapies in children with low predicted adult height, the Task Force placed high value on reducing potential psychosocial consequences of extreme short stature.
Adrenalectomy
Recommendation
8.2 We suggest that bilateral adrenalectomy be considered only in select cases that have failed medical therapy, especially in rare cases of adult females with salt-wasting CAH and infertility. Risk for noncompliance must be considered before surgery (2|⊕○○○).
8.2 Evidence
Bilateral adrenalectomy for CAH is controversial. Bilateral adrenalectomy reduces the risk of virilization in females and allows for treatment with lower GC doses. Objections to adrenalectomy are based on surgical risk, possible increased risk of adrenal crisis due to loss of protective residual adrenal function, and possible loss of hormones that may have beneficial effects such as epinephrine and DHEA.
Van Wyk and Ritzen (202) reported follow-up of 18 patients with CAH (14 salt-wasting, two simple virilizing, one nonclassic, and two 11-hydroxylase deficiency) from 11 centers who underwent bilateral adrenalectomy (13 laparoscopic and five open flank). Three patients were children (aged 1–8 yr) who had prophylactic adrenalectomy as part of a research protocol, and 15 patients were difficult to manage with conventional therapy. During approximately 5 yr of follow-up, five patients had one or more adrenal crises and two of the younger patients experienced severe hypoglycemia with illness. All patients reported subjective benefits after surgery, including the need for less frequent monitoring, weight loss, and fewer signs and symptoms of androgen excess. Eight patients had elevated steroid precursors postoperatively while on reduced HC dose, presumably from adrenal rest tissue activation, which required increased HC doses. However, GC doses were lower after than before adrenalectomy.
Five adult (aged 21–37 yr) female patients with salt-wasting CAH underwent bilateral adrenalectomy with mean follow-up of 4.2 yr (203). Two patients underwent adrenalectomy for infertility and became pregnant within 2 yr. Three patients underwent adrenalectomy for unsuppressible hyperandrogenism and worsening obesity. Weight loss was achieved; however, all three patients experienced pigmentation and adrenal crises during follow-up.
Laparoscopic bilateral adrenalectomy was performed in two women (aged 22 and 28 yr) with classic salt-wasting CAH for difficult-to-suppress androgens, with amenorrhea, hirsutism, and acne (204). Weight loss and regular menstruation followed in both patients, and one had a successful pregnancy 3 yr postoperatively. One patient had mildly elevated adrenal steroid precursors, likely due to adrenal rest tissue.
Individuals with a history of noncompliance are poor candidates for adrenalectomy because postoperative noncompliance in an adrenalectomized patient could be fatal.
If fertility is desired and adrenalectomy is not an option, hyperandrogenism can be overridden by clomiphene or GnRH ovarian stimulation.
8.2 Remarks
This recommendation requires a surgeon experienced in bilateral adrenalectomy. The lifetime risk of adrenal crisis must be thoroughly evaluated before considering this option.
Physiological cortisol replacement
Recommendation
8.3 We suggest the development of new treatment approaches that minimize daily GC exposure and aim to achieve physiological cortisol replacement.
8.3 Evidence
Existing GC therapy is nonphysiological and may contribute to adverse outcomes. Normal adrenocortical secretion has a circadian rhythm with levels low at onset of sleep, rising between 0200 and 0400 h, peaking in the early morning at approximately 0800 h, and then declining throughout the day (205,206). Programmed infusion of HC delivered in a circadian fashion to poorly controlled CAH patients resulted in nearly normal ACTH and 17-OHP (207,208). A modified-release oral form of HC is being developed (209). Further studies are needed to determine whether more physiological cortisol replacement could improve long-term clinical outcome.
Epinephrine deficiency
Recommendation
8.4 We suggest additional research concerning epinephrine deficiency in the stress response.
8.4 Evidence
Patients with classic CAH have adrenomedullary insufficiency because GCs play essential roles in the development and regulation of the adrenal medulla (198,210). Combined cortisol and epinephrine deficiency results in glucose, insulin, and leptin dysregulation, shown during short-term high-intensity exercise (211,212) and long-term moderate-intensity exercise (213). The clinical implications of epinephrine deficiency are not fully known, but it likely plays a role in the risk for hypoglycemia during febrile illnesses, especially in young children. Chronic adrenomedullary hypofunction also may play a role in the development of insulin resistance (214). Epinephrine replacement or supplementation has not been studied.
Preclinical research
Recommendation
8.5 We suggest continued research concerning novel therapies.
8.5 Evidence
CRH antagonists have been investigated in animals for potential use in psychiatric disorders (215). Increased secretion of hypothalamic CRH is expected in CAH. CRH antagonists may permit lower-dose GC replacement in the treatment of CAH (216). ACTH antagonists could have a similar effect. Drugs that block specific steroidogenic steps might also normalize adrenal androgen production without supraphysiological GC doses.
Gene therapy temporarily restored adrenal steroidogenesis in 21-hydroxylase-deficient mice (217). Patients with CAH have the ability to regulate cortisol normally; thus, altering cells to become cortisol producing represents a potential cure. The ability to correct the genetic mutations causing CAH by applying gene therapy to an individual’s own stem cells would theoretically cure CAH and avoid the need for immune-suppressant therapy. However, in light of the current practical barriers to gene therapy, risks associated with viral gene therapy vectors, the need for high levels of expression of enzyme activity within the adrenal cortex, and the availability of effective medical therapy for this condition, gene therapy is unlikely to be a realistic option for this disorder for decades to come.
Future studies
Recommendation
8.6 We suggest that further study of alternative treatment approaches consider growth, metabolic, reproductive, and neuropsychiatric endpoints.
8.6 Evidence
Current GC therapy for CAH is suboptimal because supraphysiological doses are often needed to suppress adrenal androgens. Excess GC places patients at risk for iatrogenic Cushing’s syndrome, and lower-dose GC leads to inadequately treated androgen excess. Thus, comorbidities associated with both hypercortisolism and hyperandrogenism should be a part of future studies.
9.0 CAH in Adulthood
Diagnosis of NCCAH in adults
Recommendation
9.1. We recommend that NCCAH screening with an early morning serum 17-OHP be confirmed when needed through an ACTH stimulation test (1|⊕⊕○○).
9.1 Evidence
Baseline follicular-phase early-morning 17-OHP levels can be used to detect CAH, but the normal cutoff varies between 200 and 400 ng/dl, depending on the assay (6 and 13 nmol/liter) (167,218,219,220). ACTH stimulation is needed for patients with baseline 17-OHP around the cutoff; NCCAH patients reach higher than 1000 ng/dl (33 nmol/liter). Reference values for the local laboratory should be sought. For occasional patients with nondiagnostic values, genotyping (219,221,222) may confirm the diagnosis.
Treatment of NCCAH
Recommendation
9.2 We suggest treatment of adults with NCCAH with patient-important hyperandrogenism or infertility (2|⊕○○○). We suggest clinicians not prescribe daily GC substitution in adult males with NCCAH (2|⊕○○○).
9.2 Evidence
There are no published randomized and controlled trials of various treatments for NCCAH. However, administration of dexamethasone, 0.25 mg/d, can be effective in reducing acne and irregular menstruations within 3 months and hirsutism within 30 months (223). Although fertility in classic CAH is reduced (147,161), a retrospective multicenter review found that 68% of 203 pregnancies among 101 NCCAH women had occurred before the diagnosis was made, suggesting that GC treatment is not required for fertility. Spontaneous abortions occurred more frequently before treatment in two such studies of referred reproductive endocrinology clinic patients (224,225). Interestingly, this was not observed in a controlled retrospective Swedish study that included 90% classic CAH women (160). It is difficult to draw definitive conclusions about the need for GC therapy in all NCCAH women based on these limited data; however, treatment may benefit infertile NCCAH women or those with a history of miscarriage.
Testicular adrenal rest tumors are common in adults with classic CAH but seem to be rare in NCCAH. Thus, prophylactic GCs do not seem warranted in men with NCCAH. There is no evidence of clinically significant cortisol deficiency or adrenal crisis in NCCAH, and we do not suggest that previously untreated adults with NCCAH be given substitution during severe stress, unless they have demonstrated a subnormal cortisol response during cosyntropin stimulation.
GC treatment of adults with CAH or NCCAH
Recommendation
9.3 We suggest that adult patients with classic CAH be treated with HC or long-acting GCs (2|⊕○○○).
9.3 Evidence
Adults with classic CAH are treated to avoid symptoms of adrenocortical deficiency in both sexes; hyperandrogenism, voice changes, and infertility in women; and testicular tumors in men. However, overtreatment with GCs will cause Cushingoid features, and excess MCs will cause hypertension.
There are no randomized controlled studies on long-term follow-up of different modes of treatment of adults with classic CAH, and practice varies. Among European pediatric endocrinologists, 36% said they used HC (mean dose 13.75 mg/m2), 14% used prednisolone (4.75 mg/d), and 33% used dexamethasone (0.5 mg/d) as the primary form of GC for substitution in adults with CAH (226). The longer-acting GCs were more commonly used in adults than in children.
Overtreatment with GCs may lead to osteoporosis, as noted in retrospective studies of 62 adult women with CAH, accompanied by an increased incidence of fractures as compared with healthy controls (227). The occurrence and the severity of osteopenia/osteoporosis was not related to CAH genotype or phenotype but probably was due to overtreatment with GCs. Gestational diabetes was increased among CAH women vs. controls but without other metabolic or cardiovascular abnormalities (228). Control of hyperandrogenic symptoms in young women may require additional treatment such as antiandrogenic oral contraceptives (142).
The optimal dose of fludrocortisone substitution in adults (as in infants and children) has not been critically studied. The need for MCs decreases with age, because serum aldosterone is high and renal MC receptor mRNA is low at birth (229), and the degree of MC and/or salt supplementation must be monitored by blood pressure and renin measurements in blood.
Treatment for hirsutism is beyond the scope of this Guideline and has been discussed separately (142) in another Endocrine Society Guideline.
Monitoring treatment of adults with CAH
Recommendation
9.4 We suggest that monitoring of GC and MC treatment include at least annual physical examination and appropriate hormone measurements.
9.4 Evidence
GC substitution in the adult CAH patient aims to suppress virilization and menstrual disturbance in women, alteration of gonadotropin secretion in both sexes, and testicular adrenal rest tumors in men. Available studies report on small series, and different modes for monitoring treatment have not been studied systematically. Long-term observational studies have been somewhat informative (227,228,230,231). GC overtreatment may cause Cushingoid symptoms, whereas undertreatment may cause Addisonian symptoms. Overtreatment with MCs may cause hypertension; undertreatment may lead to low blood pressure, salt loss, fatigue, and increased requirements for GC replacement.
The principles of monitoring GC treatment in adult CAH patients are similar to those employed in monitoring children. Optimal levels for 17-OHP and androstenedione have not been defined; testosterone levels in men normally reflect gonadal rather than adrenal function and therefore are not useful for monitoring therapy. 17-OHP may be elevated at night, even when morning levels are acceptable. Therefore, home monitoring of salivary 17-OHP may be more informative (232). Men with large testicular adrenal rests may have low morning testosterone indicating poor Leydig cell function (233).
Women with CAH are often overweight, with high blood pressure and hyperinsulinemia, and have risk factors for cardiovascular disease. Although Falhammar et al. (228) found that CAH patients over 30 yr of age had a higher waist to hip ratio than age-matched controls, fat mass was similar, and few CAH patients had hypertension, cardiovascular disease, or diabetes. The most significant metabolic abnormality was a 20% prevalence of gestational diabetes.
Conflicting reports concern BMD and risk of fractures. Reports studying adolescents and young adults differ concerning normal vs. reduced BMD (227). Chakhtoura et al. (234) showed a negative correlation between the accumulated lifetime dose of GC and BMD. All of these factors may reflect the high doses of GCs used to suppress adrenal androgens.
Genetic counseling
Recommendation
9.5 We recommend that genetic counseling be given to parents at birth of a CAH child and to adolescents at the transition to adult care (1|⊕○○○).
9.5 Evidence
CAH is autosomal recessive. The genotype and phenotype correlate well; siblings with CAH generally, but not always, have similar symptoms and degrees of female virilization. There is a 25% probability that siblings of the index case will have CAH and a 50% probability that they are asymptomatic carriers. Based on a classical CAH incidence of 1:10,000–1:20,000 (1,2,3,4), the incidence of carriers in the general population is 1:50–1:71. Using a median value of 1:60, a patient with classic CAH would have a one in 120 probability of having a child with classic CAH. For NCCAH, about two thirds of patients are compound heterozygotes, carrying one allele that causes classic CAH and one that causes NCCAH. The milder mutation will determine the phenotype; hence, the NCCAH parent has a one in 240 risk of having a child with classic CAH. However, in a retrospective analysis of 162 children born to NCCAH women, the risk was 2.5% (225). Bidet et al. (219) found a combined incidence of mild and severe mutations in 8% of partners of French NCCAH patients, suggesting a much higher risk for offspring to have CAH of any form.
9.5 Values and preferences
Genetic counseling is valuable for parents planning for future children. Some adults with CAH may request genotyping for themselves and/or their partner before planning for children. CAH genotyping requires certified laboratories that have adequate quality controls and can sequence the CYP21A2 gene if screening for the most common mutations is not informative.
Transition to adult care
Recommendations
9.6 We suggest that pediatric, reproductive, and adult endocrinologists, gynecologists, and urologists have joint clinics for transferring CAH patients to adult care (2|⊕○○○).
9.7 We suggest a gynecological history and examination under anesthesia in adolescent females with CAH.
9.8 We suggest against the routine use of pelvic US in CAH patients with regular menstrual cycles (2|⊕○○○).
9.9 We suggest that males with classic CAH be periodically screened from adolescence for testicular adrenal rest tumors by US (2|⊕○○○).
9.6–9.9 Evidence
Several reviews, but no controlled studies, describe how to transfer CAH patients from pediatric to adult care. Our suggestions are based on clinical experience (235,236,237,238).
Adult women with CAH often remember childhood visits to their physician as highly intrusive. After follow-up of the initial surgery, gynecological examinations should be minimized until planning for possible additional surgery.
Adolescent girls with virilizing CAH need gynecological consultation before or during puberty. The adolescent gynecological examination should be done under general anesthesia by an experienced gynecologist, ideally together with the pediatric surgeon/urologist. The patient and her family, in consultation with the surgical team, should decide whether additional surgery is needed. Issues of sexual activity and contraception should be discussed by the pediatric endocrinologist, and fertility should be addressed at the appropriate time by a reproductive endocrinologist. Obstetricians should be aware that despite an apparent normal pregnancy rate of about 90%, classic CAH women have low fecundity (0.25 live births per woman vs. 1.8 in the general population) (239).
Pediatric endocrine care is usually transferred to an adult endocrinologist at the end of adolescence, usually coinciding with the completion of secondary school, i.e. typically at age 18. A gradual transition of adolescent to adult care would ideally allow the patient’s relationship with the adult physician to be consolidated before the patient terminates his or her relationship with the pediatric endocrinologist. Males may require consultation with a urologist if testicular adrenal rest tumors are not amenable to medical therapy and/or physical examination and sonogram document incomplete resolution of an adrenal rest leaving a testicular mass suspicious for cancer.
Counseling about fertility
Recommendation
9.10 We suggest that CAH patients with impaired fertility consult a reproductive endocrinologist and/or fertility specialist (2|⊕⊕○○).
9.10 Evidence
Fertility in CAH males is poorly studied (188,240,241,242). One study reported normal fertility (188), but others reported substantially reduced fertility (243).
Testicular adrenal rest tumors increase with age in CAH, impairing fertility. The prevalence of these tumors varies between 0 and 94%, depending on the study population (188,240,243). (See also 6.1–6.3 Evidence regarding testicular adrenal rest tumors in boys aged 2–18 with classic CAH.) Undetected adrenal rest tumors may obstruct the seminiferous tubules, causing secondary gonadal dysfunction and infertility. When tumors are unresponsive to steroid therapy, surgical intervention by a testis-sparing procedure with cryopreservation of the semen may be needed, because fertility is uncertain (154,244). Fertility may be impaired by suppression of gonadotropin secretion by adrenal steroids if adequate doses of GCs are not given (242). Psychosocial factors may also play a role, because fewer men with CAH had steady heterosexual relationships than did age-matched controls (241).
Pregnancy and delivery rates were significantly lower in 62 women with CAH (ages 18–63), despite fertility treatments (160). Only 30% of the women with CAH had ever tried to become pregnant, as compared with 66% of controls. The number of children born to CAH women correlated with CAH genotype; three of six women with NCCAH had children, and nine of 27 women with simple virilizing CAH had children, but only two of 29 women with salt-wasting CAH had children. Hagenfeldt et al. (160) summarized this literature, finding an unexplained 2:1 female to male ratio for offspring of CAH women.
Management of CAH and NCCAH during pregnancy
Recommendations
9.11 We suggest that pregnant women with CAH be followed jointly by endocrinologists and obstetricians.
9.12 We recommend that patients with CAH who become pregnant continue their prepregnancy doses of HC/prednisolone and fludrocortisone therapy (1|⊕⊕○○). GC doses should be adjusted if symptoms and signs of GC insufficiency occur. We recommend against the use of GCs that traverse the placenta, such as dexamethasone, for treatment of pregnant patients with CAH (1|⊕⊕○○). Stress doses of GCs should be used during labor and delivery.
9.11–9.12 Evidence
Androgen and cortisol levels increase gradually during pregnancy (245) due to increases in SHBG and cortisol-binding globulin. Maternal testosterone levels have been used to monitor CAH patients during pregnancy (245). However, higher binding globulins and placental aromatization typically protect the fetus from the potential virilizing effects of maternal androgens. Maternal 17-OHP is elevated in normal pregnancy and hence cannot be used to monitor GC treatment. High progesterone levels during pregnancy might compete for the MC receptor, theoretically requiring increased fludrocortisone doses, but this has not been studied. Dexamethasone and other steroids that are not inactivated by placental 11β-HSD2 should not be used to treat the pregnant woman who is herself affected with CAH. There are scant empiric data and no widely accepted recommendations for the management of GC doses in the pregnant CAH patient. Symptoms of adrenal insufficiency, including postural hypotension, may rarely develop in pregnant women with classic CAH. GC and/or fludrocortisone doses should be increased if such signs and symptoms occur. Consideration may be given to increasing the dose of GC and/or fludrocortisone in advance of the development of clinical evidence of adrenal insufficiency in difficult to manage pregnant salt-wasting CAH patients. During labor and delivery, stress doses of GCs should be given, but there are no controlled studies regarding optimal dosing. CAH women are at increased risk for gestational diabetes (160); thus, glucose tolerance should be monitored throughout pregnancy. Overall, the treatment of the pregnant CAH patient should be individualized.
10.0 Mental health
Recommendation
10.1 We suggest that patients with CAH and psychosocial problems associated with disorders of sexual development be referred to mental health staff with specialized expertise in managing such problems (2|⊕⊕○○).
10.1 Evidence
Existing clinical guidelines (107,246,247,248,249,250) recommend interdisciplinary teams involving mental health staff with expertise in managing psychosocial problems specific to disorders of sexual development (DSD). CAH is one specific subtype under the rubric of DSD (250) but should not be equated with other forms of DSD in which outcomes are less well defined. Patients with CAH may experience psychosocial and psychiatric problems that are not specific to CAH. These can usually be managed by standard mental health clinicians. The 46,XX patients with CAH may also have to cope with problems that are more specific to DSD, such as 1) parent/family medical education, parent/family counseling regarding psychosocial prognosis, and managing parents’ distress; 2) gender assignment at birth in cases of marked genital virilization; 3) decisions on gender-confirming (not medically necessitated) genital surgery in infancy and early childhood; and 4) referral for psychological gender evaluation and counseling regarding potential gender reassignment of 46,XX CAH patients after infancy and at any later age, when patient-motivated gender change, both female to male and male to female, can occur, albeit rarely (251). Physician-recommended reassignment to female during infancy of erroneously male-assigned 46,XX patients does not require a psychological gender evaluation.
Additional DSD-specific items for counseling patient and family include preparation for surgery, gender-atypical behavior, social fit, bisexual and homosexual attractions (which are somewhat increased in 46,XX CAH women but still limited to a minority) (252), sexual functioning, and general quality of life (QoL) as well as concerns about inappropriate curiosity or frank stigmatization by other family, peers, or lovers in reaction to gender-atypical somatic features. Ideally, such DSD-related problems are managed by mental health staff with expertise in DSD, complemented by clinical guidelines (107,246,247,248,249,250,253,254), educational websites (e.g. www.aboutkidshealth.ca/HowTheBodyWorks/Sex-Development-An-Overview.aspx?articleID=7671&categoryID=XS; www.siecus.org), and long-distance consultation with specialists by e-mail or phone. Healthcare providers without such expertise should refer patients to appropriate staff or at least use the resources listed above.
Evaluation of health-related QoL of patients with CAH
Recommendation
10.2 We suggest the development, evaluation, and implementation in long-term clinical trials and in clinical practice of valid and responsive patient-reported assessments of their QoL in response to treatment regimens (2|⊕○○○).
10.2 Evidence
QoL is a broad construct with considerable variability in different settings. Instruments to estimate QoL often cover physical, psychological, and social functioning and ratings of satisfaction. Tools to assess health-related QoL were not designed for issues related to DSD or CAH (255); hence, the results of the few studies of QoL in CAH women are somewhat variable.
A Swedish study of 62 women with CAH noted decreased QoL in the sexuality-related domains (184,256). A Danish study of 70 women with DSD, including some 46,XX CAH women, found impaired QoL and more affective distress in CAH patients (257). In an Australian study, most of the DSD patients including XX women with CAH had positive psychosocial and psychosexual outcomes, although there were some problems with sexual activity (258). An American study that compared 72 females and 42 males with CAH (aged 3–31 yr) and unaffected relatives found no significant differences in psychological adjustment on age-appropriate validated questionnaires (259). A Finnish study found a better health-related QoL in both male and female patients with CAH than in the general Finnish population, despite numerous medical complications; however, 45% of eligible patients did not participate (241). Among 45 German women with CAH (260), the overall QoL of the CAH women did not differ from controls, but significant impairments were found concerning body image and attitudes toward sexuality, and CAH women were more often single and fewer of them had children than did controls.
See links to Resources for Clinical Trials on CAH in Supplemental Material, Appendix 1.
10.1–10.2 Values and preferences
Because patients vary widely in coping with functional impairments, we consider the assessment of QoL of equal importance to the assessment of functional impairment when evaluating the outcome of comprehensive clinical management. Until standard measures that are sensitive to the specific psychosocial issues of patients with DSD and CAH have been developed, clinicians need to adopt existing measures and rating scales from other areas of chronic care.
Relationship between surgical outcome and psychological development
Apart from urinary tract malformations in a minority of CAH girls, genital ambiguity usually does not require urgent surgical intervention. Severely virilized cases may initially be assigned as males, and once such assignment has been made, it may be difficult to reverse, thereby sacrificing fertility. This is especially true in countries where cultural tradition favors males (261). Among 33 46,XX CAH patients raised as males, four identified themselves as female, and three were gender dysphoric (251). In markedly virilized female-raised children, surgical intervention can facilitate heterosexual intercourse and conception, if desired. Fertility and fecundity, although reduced, remain feasible.
Other psychosocial consequences of genital ambiguity have been documented by case reports but not in systematic studies (262). These consequences include perceived incongruence between genital appearance and assigned gender by parents and society, conflicted gender typing by family members, increased curiosity about the patient’s genitals and increased stigmatization by others, impaired genital self-image, and impaired bodily self-image associated with short stature, increased weight, and hirsutism. These factors may lead to social withdrawal, especially from situations involving nudity (team sports or medical examinations), and avoidance of romantic interactions and sexual involvement. Despite the presence of atypical genitalia and anecdotal reports of gender dysphoria and psychosexual dysfunction, core female gender identity is generally preserved among CAH girls (263). Of 250 females with CAH who underwent psychological assessments, 5.2% reported gender problems (251).
To prevent adverse psychosocial consequences, clinical management recommendations have typically included corrective genital surgery (feminizing or masculinizing, depending on the gender assignment of the child in early infancy). This policy of gender-confirming surgery has been questioned by reports of surgical complications, including destruction of the neurovascular bundle during clitoral surgery, especially clitorectomy, clitoral atrophy, vaginal stenosis requiring surgical correction in adolescence, and unsatisfactory cosmetic results after pubertal growth due to misalignment of genital structures. In addition, some patients had problems with sexual function (e.g. decreased arousability and decreased orgasmic capacity). Recent reports of long-term follow-up studies show variable outcomes including impaired cosmesis and sexual functioning (264,265,266,267), and even nonsurgical procedures such as vaginal dilatation can be problematic (268). A patient support group (269) and some ethicists (270) have demanded postponing all such surgery until the patient can give informed consent; some professional activists called for a moratorium on such surgery until better empirical evidence of risks and benefits was available (271). Despite serious deficiencies with the surgical outcome data (small samples, uncertain representativeness, evaluation of cosmesis by the surgeons, inclusion of multiple surgical techniques, and outcome data oriented toward cosmesis rather than sexual function) (262) and the fact that adult women with CAH typically underwent relatively unsophisticated surgical procedures that are no longer used, the outcome is highly variable in terms of cosmesis, function, and patient satisfaction. Even in adult patients, the demand for informed consent appears unrealistic if the patient is sexually inexperienced.
Controlled observational studies are not available to document whether genital surgery prevents adverse psychosocial consequences. The cosmetic results are variably evaluated by patients, who tend to be more critical than their physicians (184,185). Nevertheless, recent surveys of women with CAH showed that most favored genital surgery before adolescence (184,185). We cannot yet know whether improvements in surgical techniques in the last decade will yield improvements in cosmesis and functional outcomes.
Finally, in contemplating the avoidance of early genital surgery, one must also consider that no studies have been conducted to demonstrate that potential adverse psychosocial consequences of gender-incongruent genital appearance can be ameliorated by psychological counseling or psychotherapy. Physicians should inform families of all these concerns and allow them to reach a reasoned decision with input from various sources, including patient and family support groups.
Supplemental Information
A complete description of how the evidence-based recommendations were developed may be found in Supplemental Data, Appendix 2. For a list of all recommendations included in this guideline, see Summary of Recommendations in Supplemental Data, Appendix 3.
Acknowledgments
The authors gratefully acknowledge the assistance of Dr. Patricia Stephens in the preparation of this manuscript. We would like to thank the Clinical Guidelines Subcommittee, the Clinical Affairs Core Committee, the Council of The Endocrine Society, the American Academy of Pediatrics, Androgen Excess and PCOS Society, CARES Foundation, European Society of Endocrinology, European Society for Paediatric Endocrinology, Pediatric Endocrine Society, and the Society of Pediatric Urology for their review and cosponsorship of this guideline.
Footnotes
Cosponsoring associations include the American Academy of Pediatrics, Androgen Excess and PCOS Society, CARES Foundation, European Society of Endocrinology, European Society for Pediatric Endocrinology, Pediatric Endocrine Society, and the Society of Pediatric Urology.
Financial Disclosure of Task Force
Phyllis W. Speiser, M.D. (chair) – Financial or Business/Organizational Interests: Pediatric Endocrine Society, Society for Pediatric Research, and American Association of Clinical Endocrinologists; Significant Financial Interest or Leadership Position: Medical Advisory Board, CARES Foundation, and National Adrenal Diseases Foundation; Ricardo Azziz, M.B.A., M.D., M.P.H. – Financial or Business/Organizational Interests: none declared; Significant Financial Interest or Leadership Position: none declared; Laurence S. Baskin, M.D. – Financial or Business/Organizational Interests: none declared; Significant Financial Interest or Leadership Position: none declared; Lucia Ghizzoni, M.D., Ph.D. – Financial or Business/Organizational Interests: none declared; Significant Financial Interest or Leadership Position: none declared; Terry W. Hensle, M.D. – Financial or Business/Organizational Interests: none declared; Significant Financial Interest or Leadership Position: none declared;a Deborah P. Merke, MS, M.D. – Financial of Business/Organizational Interests: Phoqus Pharmaceuticals and CARES Foundation; Significant Financial Interest or Leadership Position: none declared; Heino F. L. Meyer-Bahlburg, Dr. rer. Nat. – Financial of Business/Organizational Interests: Pediatric Endocrine Society, World Professional Association of Transgender Health, and Gender Identity Disorders for DSM-V of the American Psychiatric Association; Significant Financial Interest or Leadership Position: none declared; Walter L. Miller, M.D. – Financial or Business/Organizational Interests: CARES Foundation and Pediatric Endocrine Society; Significant Financial Interest or Leadership Position: Medical Advisory Board and CARES Foundation;b Victor M. Montori, M.D.- Financial or Business/Organizational Interests: KER Unit (Mayo Clinic); Significant Financial Interest or Leadership Position: none declared; Sharon E. Oberfield, M.D. – Financial or Business/Organizational Interests: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Significant Financial Interest or Leadership Position: Pediatric Endocrine Society, Medical Advisory Board, and CARES Foundation; Martin Ritzen, M.D. – Financial or Business/Organizational Interests: Biopartners AG and Acta Paediatrica; Significant Financial Interest or Leadership Position: none declared; Perrin C. White, M.D. – Financial or Business/Organizational Interests: none declared; Significant Financial Interest or Leadership Position: none declared.
* This work was supported by the Intramural Research Program of the National Institutes of Health.
† Evidence-based reviews for this guideline were prepared under contract with The Endocrine Society.
Abbreviations: BMD, Bone mineral density; CAH, congenital adrenal hyperplasia; DHEA, dehydroepiandrosterone; DSD, disorders of sexual development; GC, glucocorticoid; GnRHa, GnRH agonist; HC, hydrocortisone; 11β-HSD2, 11β-hydroxysteroid dehydrogenase type 2; LC-MS/MS, liquid chromatography followed by tandem mass spectrometry; MC, mineralocorticoid; NCCAH, nonclassic CAH; 17-OHP, 17-hydroxyprogesterone; PRA, plasma renin activity; QoL, quality of life; SDS, sd score; US, ultrasound.
References
- Nordenström A, Ahmed S, Jones J, Coleman M, Price DA, Clayton PE, Hall CM 2005 Female preponderance in congenital adrenal hyperplasia due to CYP21 deficiency in England: implications for neonatal screening. Horm Res 63:22–28 [DOI] [PubMed] [Google Scholar]
- Pang S, Shook MK 1997 Current status of neonatal screening for congenital adrenal hyperplasia. Curr Opin Pediatr 9:419–423 [DOI] [PubMed] [Google Scholar]
- Therrell BL 2001 Newborn screening for congenital adrenal hyperplasia. Endocrinol Metab Clin North Am 30:15–30 [DOI] [PubMed] [Google Scholar]
- van der Kamp HJ, Wit JM 2004 Neonatal screening for congenital adrenal hyperplasia. Eur J Endocrinol 151(Suppl 3):U71–U75 [DOI] [PubMed] [Google Scholar]
- Krone N, Dhir V, Ivison HE, Arlt W 2007 Congenital adrenal hyperplasia and P450 oxidoreductase deficiency. Clin Endocrinol (Oxf) 66:162–172 [DOI] [PubMed] [Google Scholar]
- White PC, Speiser PW 2000 Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr Rev 21:245–291 [DOI] [PubMed] [Google Scholar]
- Homma K, Hasegawa T, Nagai T, Adachi M, Horikawa R, Fujiwara I, Tajima T, Takeda R, Fukami M, Ogata T 2006 Urine steroid hormone profile analysis in cytochrome P450 oxidoreductase deficiency: implication for the backdoor pathway to dihydrotestosterone. J Clin Endocrinol Metab 91:2643–2649 [DOI] [PubMed] [Google Scholar]
- Leihy MW, Shaw G, Renfree MB, Wilson JD 2002 Administration of 5α-androstane-3α,17β-diol to female tammar wallaby pouch young causes development of a mature prostate and male urethra. Endocrinology 143:2643–2651 [DOI] [PubMed] [Google Scholar]
- NNSIS 2009 National Newborn Screening Information System. Available at http://www2.uthscsa.edu/nnsis [Google Scholar]
- Kohn B, Levine LS, Pollack MS, Pang S, Lorenzen F, Levy D, Lerner AJ, Rondanini GF, Dupont B, New MI 1982 Late-onset steroid 21-hydroxylase deficiency: a variant of classical congenital adrenal hyperplasia. J Clin Endocrinol Metab 55:817–827 [DOI] [PubMed] [Google Scholar]
- Speiser PW, Dupont B, Rubinstein P, Piazza A, Kastelan A, New MI 1985 High frequency of nonclassical steroid 21-hydroxylase deficiency. Am J Hum Genet 37:650–667 [PMC free article] [PubMed] [Google Scholar]
- Yang Z, Mendoza AR, Welch TR, Zipf WB, Yu CY 1999 Modular variations of the human major histocompatibility complex class III genes for serine/threonine kinase RP, complement component C4, steroid 21-hydroxylase CYP21, and tenascin TNX (the RCCX module). A mechanism for gene deletions and disease associations. J Biol Chem 274:12147–12156 [DOI] [PubMed] [Google Scholar]
- 2008 The Human Gene Mutation Database at the Institute of Medical Genetics in Cardiff. Available at http://www.hgmd.cf.ac.uk/ac/gene.php?gene=CYP21A2. [Google Scholar]
- Krone N, Braun A, Roscher AA, Knorr D, Schwarz HP 2000 Predicting phenotype in steroid 21-hydroxylase deficiency? Comprehensive genotyping in 155 unrelated, well defined patients from southern Germany. J Clin Endocrinol Metab 85:1059–1065 [DOI] [PubMed] [Google Scholar]
- Speiser PW, Dupont J, Zhu D, Serrat J, Buegeleisen M, Tusie-Luna MT, Lesser M, New MI, White PC 1992 Disease expression and molecular genotype in congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Invest 90:584–595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tusie-Luna MT, Traktman P, White PC 1990 Determination of functional effects of mutations in the steroid 21-hydroxylase gene (CYP21) using recombinant vaccinia virus. J Biol Chem 265:20916–20922 [PubMed] [Google Scholar]
- Blanché H, Vexiau P, Clauin S, Le Gall I, Fiet J, Mornet E, Dausset J, Bellanné-Chantelot C) 1997 Exhaustive screening of the 21-hydroxylase gene in a population of hyperandrogenic women. Hum Genet 101:56–60 [DOI] [PubMed] [Google Scholar]
- Deneux C, Tardy V, Dib A, Mornet E, Billaud L, Charron D, Morel Y, Kuttenn F 2001 Phenotype-genotype correlation in 56 women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 86:207–213 [DOI] [PubMed] [Google Scholar]
- Balsamo A, Cacciari E, Piazzi S, Cassio A, Bozza D, Pirazzoli P, Zappulla F 1996 Congenital adrenal hyperplasia: neonatal mass screening compared with clinical diagnosis only in the Emilia-Romagna region of Italy, 1980–1995. Pediatrics 98:362–367 [PubMed] [Google Scholar]
- Brosnan PG, Brosnan CA, Kemp SF, Domek DB, Jelley DH, Blackett PR, Riley WJ 1999 Effect of newborn screening for congenital adrenal hyperplasia. Arch Pediatr Adolesc Med 153:1272–1278 [DOI] [PubMed] [Google Scholar]
- Therrell Jr BL, Berenbaum SA, Manter-Kapanke V, Simmank J, Korman K, Prentice L, Gonzalez J, Gunn S 1998 Results of screening 1.9 million Texas newborns for 21-hydroxylase-deficient congenital adrenal hyperplasia. Pediatrics 101:583–590 [DOI] [PubMed] [Google Scholar]
- Thil'en A, Nordenström A, Hagenfeldt L, von Döbeln U, Guthenberg C, Larsson A 1998 Benefits of neonatal screening for congenital adrenal hyperplasia (21-hydroxylase deficiency) in Sweden. Pediatrics 101:E11 [DOI] [PubMed] [Google Scholar]
- Strnadová KA, Votava F, Lebl J, Mühl A, Item C, Bodamer OA, Torresani T, Bouska I, Waldhauser F, Sperl W 2007 Prevalence of congenital adrenal hyperplasia among sudden infant death in the Czech Republic and Austria. Eur J Pediatr 166:1–4 [DOI] [PubMed] [Google Scholar]
- Lebovitz RM, Pauli RM, Laxova R 1984 Delayed diagnosis in congenital adrenal hyperplasia. Need for newborn screening. Am J Dis Child 138:571–573 [DOI] [PubMed] [Google Scholar]
- Thompson R, Seargeant L, Winter JS 1989 Screening for congenital adrenal hyperplasia: distribution of 17 α-hydroxyprogesterone concentrations in neonatal blood spot specimens. J Pediatr 114:400–404 [DOI] [PubMed] [Google Scholar]
- Thilén A, Larsson A 1990 Congenital adrenal hyperplasia in Sweden 1969–1986. Prevalence, symptoms and age at diagnosis. Acta Paediatr Scand 79:168–175 [DOI] [PubMed] [Google Scholar]
- Grosse SD, Van Vliet G 2007 How many deaths can be prevented by newborn screening for congenital adrenal hyperplasia? Horm Res 67:284–291 [DOI] [PubMed] [Google Scholar]
- Watson MS, Lloyd-Puryear MA, Mann MY, Rinaldo P, Howell RR 2006 Newborn screening: toward a uniform screening panel and system. Available at http://www.acmg.net/resources/policies/NBS/NBS-sections.htm [Google Scholar]
- Van der Kamp HJ, Noordam K, Elvers B, Van Baarle M, Otten BJ, Verkerk PH 2001 Newborn screening for congenital adrenal hyperplasia in the Netherlands. Pediatrics 108:1320–1324 [DOI] [PubMed] [Google Scholar]
- Nass R, Baker S 1991 Learning disabilities in children with congenital adrenal hyperplasia. J Child Neurol 6:306–312 [DOI] [PubMed] [Google Scholar]
- Pang SY, Wallace MA, Hofman L, Thuline HC, Dorche C, Lyon IC, Dobbins RH, Kling S, Fujieda K, Suwa S 1988 Worldwide experience in newborn screening for classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Pediatrics 81:866–874 [PubMed] [Google Scholar]
- Carroll AE, Downs SM 2006 Comprehensive cost-utility analysis of newborn screening strategies. Pediatrics 117:S287–295 [DOI] [PubMed] [Google Scholar]
- Yoo BK, Grosse SD 2009 The cost effectiveness of screening newborns for congenital adrenal hyperplasia. Public Health Genomics 12:67–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurian EA, Kinnamon DD, Henry JJ, Waisbren SE 2006 Expanded newborn screening for biochemical disorders: the effect of a false-positive result. Pediatrics 117:1915–1921 [DOI] [PubMed] [Google Scholar]
- Gonzalez RR, Mäentausta O, Solyom J, Vihko R 1990 Direct solid-phase time-resolved fluoroimmunoassay of 17 α-hydroxyprogesterone in serum and dried blood spots on filter paper. Clin Chem 36:1667–1672 [PubMed] [Google Scholar]
- Allen DB, Hoffman GL, Fitzpatrick P, Laessig R, Maby S, Slyper A 1997 Improved precision of newborn screening for congenital adrenal hyperplasia using weight-adjusted criteria for 17-hydroxyprogesterone levels. J Pediatr 130:128–133 [DOI] [PubMed] [Google Scholar]
- Olgemoller B, Roscher AA, Liebl B, Fingerhut R 2003 Screening for congenital adrenal hyperplasia: adjustment of 17-hydroxyprogesterone cut-off values to both age and birth weight markedly improves the predictive value. J Clin Endocrinol Metab 88:5790–5794 [DOI] [PubMed] [Google Scholar]
- van der Kamp HJ, Oudshoorn CG, Elvers BH, van Baarle M, Otten BJ, Wit JM, Verkerk PH 2005 Cutoff levels of 17-α-hydroxyprogesterone in neonatal screening for congenital adrenal hyperplasia should be based on gestational age rather than on birth weight. J Clin Endocrinol Metab 90:3904–3907 [DOI] [PubMed] [Google Scholar]
- Steigert M, Schoenle EJ, Biason-Lauber A, Torresani T 2002 High reliability of neonatal screening for congenital adrenal hyperplasia in Switzerland. J Clin Endocrinol Metab 87:4106–4110 [DOI] [PubMed] [Google Scholar]
- Gatelais F, Berthelot J, Beringue F, Descamps P, Bonneau D, Limal JM, Coutant R 2004 Effect of single and multiple courses of prenatal corticosteroids on 17-hydroxyprogesterone levels: implication for neonatal screening of congenital adrenal hyperplasia. Pediatr Res 56:701–705 [DOI] [PubMed] [Google Scholar]
- King JL, Naber JM, Hopkin RJ, Repaske DR, Bailey L, Leslie ND 2001 Antenatal corticosteroids and newborn screening for congenital adrenal hyperplasia. Arch Pediatr Adolesc Med 155:1038–1042 [DOI] [PubMed] [Google Scholar]
- Lacey JM, Minutti CZ, Magera MJ, Tauscher AL, Casetta B, McCann M, Lymp J, Hahn SH, Rinaldo P, Matern D 2004 Improved specificity of newborn screening for congenital adrenal hyperplasia by second-tier steroid profiling using tandem mass spectrometry. Clin Chem 50:621–625 [DOI] [PubMed] [Google Scholar]
- Rauh M, Gröschl M, Rascher W, Dörr HG 2006 Automated, fast and sensitive quantification of 17 α-hydroxy-progesterone, androstenedione and testosterone by tandem mass spectrometry with on-line extraction. Steroids 71:450–458 [DOI] [PubMed] [Google Scholar]
- Matern D, Tortorelli S, Oglesbee D, Gavrilov D, Rinaldo P 2007 Reduction of the false-positive rate in newborn screening by implementation of MS/MS-based second-tier tests: the Mayo Clinic experience (2004–2007). J Inherit Metab Dis 30:585–592 [DOI] [PubMed] [Google Scholar]
- Schwarz E, Liu A, Randall H, Haslip C, Keune F, Murray M, Longo N, Pasquali M 2009 Use of steroid profiling by UPLC-MS/MS as a second tier test in newborn screening for congenital adrenal hyperplasia: the Utah experience. Pediatr Res 66:230–235 [DOI] [PubMed] [Google Scholar]
- Janzen N, Peter M, Sander S, Steuerwald U, Terhardt M, Holtkamp U, Sander J 2007 Newborn screening for congenital adrenal hyperplasia: additional steroid profile using liquid chromatography-tandem mass spectrometry. J Clin Endocrinol Metab 92:2581–2589 [DOI] [PubMed] [Google Scholar]
- Janzen N, Sander S, Terhardt M, Peter M, Sander J 2008 Fast and direct quantification of adrenal steroids by tandem mass spectrometry in serum and dried blood spots. J Chromatogr B Analyt Technol Biomed Life Sci 861:117–122 [DOI] [PubMed] [Google Scholar]
- Fitness J, Dixit N, Webster D, Torresani T, Pergolizzi R, Speiser PW, Day DJ 1999 Genotyping of CYP21, linked chromosome 6p markers, and a sex-specific gene in neonatal screening for congenital adrenal hyperplasia. J Clin Endocrinol Metab 84:960–966 [DOI] [PubMed] [Google Scholar]
- Kösel S, Burggraf S, Fingerhut R, Dörr HG, Roscher AA, Olgemöller B 2005 Rapid second-tier molecular genetic analysis for congenital adrenal hyperplasia attributable to steroid 21-hydroxylase deficiency. Clin Chem 51:298–304 [DOI] [PubMed] [Google Scholar]
- Nordenström A, Thilén A, Hagenfeldt L, Larsson A, Wedell A 1999 Genotyping is a valuable diagnostic complement to neonatal screening for congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency. J Clin Endocrinol Metab 84:1505–1509 [DOI] [PubMed] [Google Scholar]
- Yang YP, Corley N, Garcia-Heras J 2001 Reverse dot-blot hybridization as an improved tool for the molecular diagnosis of point mutations in congenital adrenal hyperplasia caused by 21-hydroxylase deficiency. Mol Diagn 6:193–199 [DOI] [PubMed] [Google Scholar]
- New MI, Lorenzen F, Lerner AJ, Kohn B, Oberfield SE, Pollack MS, Dupont B, Stoner E, Levy DJ, Pang S, Levine LS 1983 Genotyping steroid 21-hydroxylase deficiency: hormonal reference data. J Clin Endocrinol Metab 57:320–326 [DOI] [PubMed] [Google Scholar]
- Caulfield MP, Lynn T, Gottschalk ME, Jones KL, Taylor NF, Malunowicz EM, Shackleton CH, Reitz RE, Fisher DA 2002 The diagnosis of congenital adrenal hyperplasia in the newborn by gas chromatography/mass spectrometry analysis of random urine specimens. J Clin Endocrinol Metab 87:3682–3690 [DOI] [PubMed] [Google Scholar]
- David M, Forest MG 1984 Prenatal treatment of congenital adrenal hyperplasia resulting from 21-hydroxylase deficiency. J Pediatr 105:799–803 [DOI] [PubMed] [Google Scholar]
- Evans MI, Chrousos GP, Mann DW, Larsen Jr JW, Green I, McCluskey J, Loriaux DL, Fletcher JC, Koons G, Overpeck J, Schulman JD 1985 Pharmacologic suppression of the fetal adrenal gland in utero. Attempted prevention of abnormal external genital masculinization in suspected congenital adrenal hyperplasia. JAMA 253:1015–1020 [PubMed] [Google Scholar]
- Forest MG, David M, Morel Y 1993 Prenatal diagnosis and treatment of 21-hydroxylase deficiency. J Steroid Biochem Mol Biol 45:75–82 [DOI] [PubMed] [Google Scholar]
- Forest MG, Morel Y, David M 1998 Prenatal treatment of congenital adrenal hyperplasia. Trends Endocrinol Metab 9:284–289 [DOI] [PubMed] [Google Scholar]
- New MI, Carlson A, Obeid J, Marshall I, Cabrera MS, Goseco A, Lin-Su K, Putnam AS, Wei JQ, Wilson RC 2001 Prenatal diagnosis for congenital adrenal hyperplasia in 532 pregnancies. J Clin Endocrinol Metab 86:5651–5657 [DOI] [PubMed] [Google Scholar]
- Goto M, Piper Hanley K, Marcos J, Wood PJ, Wright S, Postle AD, Cameron IT, Mason JI, Wilson DI, Hanley NA 2006 In humans, early cortisol biosynthesis provides a mechanism to safeguard female sexual development. J Clin Invest 116:953–960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kari MA, Raivio KO, Stenman UH, Voutilainen R 1996 Serum cortisol, dehydroepiandrosterone sulfate, and steroid-binding globulins in preterm neonates: effect of gestational age and dexamethasone therapy. Pediatr Res 40:319–324 [DOI] [PubMed] [Google Scholar]
- Partsch CJ, Sippell WG, MacKenzie IZ, Aynsley-Green A 1991 The steroid hormonal milieu of the undisturbed human fetus and mother at 16–20 weeks gestation. J Clin Endocrinol Metab 73:969–974 [DOI] [PubMed] [Google Scholar]
- Speiser PW, Miller WL 2008 Prenatal treatment of classic CAH: Pro vs. Con. Endocr News 33:14–18; available in 2 parts at http://www.endo-society.org/endo_news/2008/upload/14_15.pdf. and http://www.endo-society.org/endo_news/2008/upload/16_20.pdf [Google Scholar]
- White PC 2006 Ontogeny of adrenal steroid biosynthesis: why girls will be girls. J Clin Invest 116:872–874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White PC, Mune T, Agarwal AK 1997 11β-Hydroxysteroid dehydrogenase and the syndrome of apparent mineralocorticoid excess. Endocr Rev 18:135–156 [DOI] [PubMed] [Google Scholar]
- Lo YM, Corbetta N, Chamberlain PF, Rai V, Sargent IL, Redman CW, Wainscoat JS 1997 Presence of fetal DNA in maternal plasma and serum. Lancet 350:485–487 [DOI] [PubMed] [Google Scholar]
- Lo YM, Tein MS, Lau TK, Haines CJ, Leung TN, Poon PM, Wainscoat JS, Johnson PJ, Chang AM, Hjelm NM 1998 Quantitative analysis of fetal DNA in maternal plasma and serum: implications for noninvasive prenatal diagnosis. Am J Hum Genet 62:768–775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartha JL, Finning K, Soothill PW 2003 Fetal sex determination from maternal blood at 6 weeks of gestation when at risk for 21-hydroxylase deficiency. Obstet Gynecol 101:1135–1136 [DOI] [PubMed] [Google Scholar]
- Rijnders RJ, van der Schoot CE, Bossers B, de Vroede MA, Christiaens GC 2001 Fetal sex determination from maternal plasma in pregnancies at risk for congenital adrenal hyperplasia. Obstet Gynecol 98:374–378 [DOI] [PubMed] [Google Scholar]
- Coleman MA, Honour JW 2004 Reduced maternal dexamethasone dosage for the prenatal treatment of congenital adrenal hyperplasia. BJOG 111:176–178 [DOI] [PubMed] [Google Scholar]
- Fernandez-Balsells MM, Muthusamy K, Murad MH, Smushkin G, Lampropulos JF, Elamin MB, Abu Elnour NO, Elamin KB, Agrwal N, Gallegos-Orozco JF, Erwin PJ, Montori VM 9 June 2010 Prenatal dexamethasone use for the prevention of virilization in pregnancies at risk for classical congenital adrenal hyperplasia due to 21 hydroxylase (CYP21A2) deficiency: a systematic review and meta-analyses. Clin Endocrinol (Oxf) 10.1111/j.1365-2265.2010.03826.x [DOI] [PubMed] [Google Scholar]
- Forest MG 2004 Recent advances in the diagnosis and management of congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Reprod Update 10:469–485 [DOI] [PubMed] [Google Scholar]
- Lajic S, Wedell A, Bui TH, Ritzén EM, Holst M 1998 Long-term somatic follow-up of prenatally treated children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 83:3872–3880 [DOI] [PubMed] [Google Scholar]
- Pang S, Clark AT, Freeman LC, Dolan LM, Immken L, Mueller OT, Stiff D, Shulman DI 1992 Maternal side effects of prenatal dexamethasone therapy for fetal congenital adrenal hyperplasia. J Clin Endocrinol Metab 75:249–253 [DOI] [PubMed] [Google Scholar]
- Fraser FC, Fainstat TD 1951 Production of congenital defects in the off-spring of pregnant mice treated with cortisone; progress report. Pediatrics 8:527–533 [PubMed] [Google Scholar]
- Goldman AS, Sharpior BH, Katsumata M 1978 Human foetal palatal corticoid receptors and teratogens for cleft palate. Nature 272:464–466 [DOI] [PubMed] [Google Scholar]
- Rowland JM, Hendrickx AG 1983 Corticosteroid teratogenicity. Adv Vet Sci Comp Med 27:99–128 [PubMed] [Google Scholar]
- Czeizel AE, Rockenbauer M 1997 Population-based case-control study of teratogenic potential of corticosteroids. Teratology 56:335–340 [DOI] [PubMed] [Google Scholar]
- Robert E, Vollset SE, Botto L, Lancaster PA, Merlob P, Mastroiacovo P, Cocchi G, Ashizawa M, Sakamoto S, Orioli I 1994 Malformation surveillance and maternal drug exposure: the MADRE project. Int J Risk Safety Med 6:78–118 [DOI] [PubMed] [Google Scholar]
- Rodríguez-Pinilla E, Martínez-Frías ML 1998 Corticosteroids during pregnancy and oral clefts: a case-control study. Teratology 58:2–5 [DOI] [PubMed] [Google Scholar]
- Fraser FC, Sajoo A 1995 Teratogenic potential of corticosteroids in humans. Teratology 51:45–46 [DOI] [PubMed] [Google Scholar]
- Safari HR, Fassett MJ, Souter IC, Alsulyman OM, Goodwin TM 1998 The efficacy of methylprednisolone in the treatment of hyperemesis gravidarum: a randomized, double-blind, controlled study. Am J Obstet Gynecol 179:921–924 [DOI] [PubMed] [Google Scholar]
- Carmichael SL, Shaw GM 1999 Maternal corticosteroid use and risk of selected congenital anomalies. Am J Med Genet 86:242–244 [DOI] [PubMed] [Google Scholar]
- Carmichael SL, Shaw GM, Ma C, Werler MM, Rasmussen SA, Lammer EJ 2007 Maternal corticosteroid use and orofacial clefts. Am J Obstet Gynecol 197:585.e1–e7; discussion 683–684.e1–e7 [DOI] [PubMed] [Google Scholar]
- Barker DJ, Bull AR, Osmond C, Simmonds SJ 1990 Fetal and placental size and risk of hypertension in adult life. BMJ 301:259–262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barker DJ, Winter PD, Osmond C, Margetts B, Simmonds SJ 1989 Weight in infancy and death from ischaemic heart disease. Lancet 2:577–580 [DOI] [PubMed] [Google Scholar]
- Benediktsson R, Lindsay RS, Noble J, Seckl JR, Edwards CR 1993 Glucocorticoid exposure in utero: new model for adult hypertension. Lancet 341:339–341 [DOI] [PubMed] [Google Scholar]
- Miller WL 1999 Dexamethasone treatment of congenital adrenal hyperplasia in utero: an experimental therapy of unproven safety. J Urol 162:537–540 [PubMed] [Google Scholar]
- Seckl JR 2004 Prenatal glucocorticoids and long-term programming. Eur J Endocrinol 151(Suppl 3):U49–U62 [DOI] [PubMed] [Google Scholar]
- Seckl JR, Miller WL 1997 How safe is long-term prenatal glucocorticoid treatment? JAMA 277:1077–1079 [PubMed] [Google Scholar]
- Celsi G, Kistner A, Aizman R, Eklöf AC, Ceccatelli S, de Santiago A, Jacobson SH 1998 Prenatal dexamethasone causes oligonephronia, sodium retention, and higher blood pressure in the offspring. Pediatr Res 44:317–322 [DOI] [PubMed] [Google Scholar]
- Dickinson H, Walker DW, Wintour EM, Moritz K 2007 Maternal dexamethasone treatment at midgestation reduces nephron number and alters renal gene expression in the fetal spiny mouse. Am J Physiol Regul Integr Comp Physiol 292:R453–R461 [DOI] [PubMed] [Google Scholar]
- de Vries A, Holmes MC, Heijnis A, Seier JV, Heerden J, Louw J, Wolfe-Coote S, Meaney MJ, Levitt NS, Seckl JR 2007 Prenatal dexamethasone exposure induces changes in nonhuman primate offspring cardiometabolic and hypothalamic-pituitary-adrenal axis function. J Clin Invest 117:1058–1067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang X, Zuckerman B, Pearson C, Kaufman G, Chen C, Wang G, Niu T, Wise PH, Bauchner H, Xu X 2002 Maternal cigarette smoking, metabolic gene polymorphism, and infant birth weight. JAMA 287:195–202 [DOI] [PubMed] [Google Scholar]
- McMahon SK, Pretorius CJ, Ungerer JP, Salmon NJ, Conwell LS, Pearen MA, Batch JA 2010 Neonatal complete generalized glucocorticoid resistance and growth hormone deficiency caused by a novel homozygous mutation in helix 12 of the ligand binding domain of the glucocorticoid receptor gene (NR3C1). J Clin Endocrinol Metab 95:297–302 [DOI] [PubMed] [Google Scholar]
- Matthews SG 2001 Antenatal glucocorticoids and the developing brain: mechanisms of action. Semin Neonatol 6:309–317 [DOI] [PubMed] [Google Scholar]
- Sloboda DM, Challis JR, Moss TJ, Newnham JP 2005 Synthetic glucocorticoids: antenatal administration and long-term implications. Curr Pharm Des 11:1459–1472 [DOI] [PubMed] [Google Scholar]
- Braun T, Li S, Sloboda DM, Li W, Audette MC, Moss TJ, Matthews SG, Polglase G, Nitsos I, Newnham JP, Challis JR 2009 Effects of maternal dexamethasone treatment in early pregnancy on pituitary-adrenal axis in fetal sheep. Endocrinology 150:5466–5477 [DOI] [PubMed] [Google Scholar]
- Huang WL, Beazley LD, Quinlivan JA, Evans SF, Newnham JP, Dunlop SA 1999 Effect of corticosteroids on brain growth in fetal sheep. Obstet Gynecol 94:213–218 [DOI] [PubMed] [Google Scholar]
- Moss TJ, Doherty DA, Nitsos I, Sloboda DM, Harding R, Newnham JP 2005 Effects into adulthood of single or repeated antenatal corticosteroids in sheep. Am J Obstet Gynecol 192:146–152 [DOI] [PubMed] [Google Scholar]
- Quinlivan JA, Dunlop SA, Newnham JP, Evans SF, Beazley LD 1999 Repeated, but not single, maternal administration of corticosteroids delays myelination in the brain of fetal sheep. Prenat Neonat Med 4:47–55 [Google Scholar]
- Uno H, Lohmiller L, Thieme C, Kemnitz JW, Engle MJ, Roecker EB, Farrell PM 1990 Brain damage induced by prenatal exposure to dexamethasone in fetal rhesus macaques. I. Hippocampus. Brain Res Dev Brain Res 53:157–167 [DOI] [PubMed] [Google Scholar]
- Trautman PD, Meyer-Bahlburg HF, Postelnek J, New MI 1995 Effects of early prenatal dexamethasone on the cognitive and behavioral development of young children: results of a pilot study. Psychoneuroendocrinology 20:439–449 [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg HF, Dolezal C, Baker SW, Carlson AD, Obeid JS, New MI 2004 Cognitive and motor development of children with and without congenital adrenal hyperplasia after early-prenatal dexamethasone. J Clin Endocrinol Metab 89:610–614 [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Nordenström A, Lindholm T, Lindblad F, Ritzén EM, Wedell A, Lajic S 2007 Cognitive functions in children at risk for congenital adrenal hyperplasia treated prenatally with dexamethasone. J Clin Endocrinol Metab 92:542–548 [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Nordenström A, Lindholm T, Lindblad F, Ritzén EM, Lajic S 2008 Long-term follow-up of prenatally treated children at risk for congenital adrenal hyperplasia: does dexamethasone cause behavioural problems? Eur J Endocrinol 159:309–316 [DOI] [PubMed] [Google Scholar]
- 2000 Technical report: congenital adrenal hyperplasia. Section on Endocrinology and Committee on Genetics. Pediatrics 106:1511–1518 [PubMed] [Google Scholar]
- Clayton PE, Miller WL, Oberfield SE, Ritzen EM, Sippell WG, Speiser PW 2002 Consensus statement on 21-hydroxylase deficiency from the Lawson Wilkins Pediatric Endocrine Society and the European Society for Paediatric Endocrinology. J Clin Endocrinol Metab 87:4048–4053 [DOI] [PubMed] [Google Scholar]
- Miller WL 1994 Genetics, diagnosis, and management of 21-hydroxylase deficiency. J Clin Endocrinol Metab 78:241–246 [DOI] [PubMed] [Google Scholar]
- Riepe FG, Sippell WG 2007 Recent advances in diagnosis, treatment, and outcome of congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Rev Endocr Metab Disord 8:349–363 [DOI] [PubMed] [Google Scholar]
- Ritzén EM 1998 Prenatal treatment of congenital adrenal hyperplasia: a commentary. Trends Endocrinol Metab 9:293–295 [DOI] [PubMed] [Google Scholar]
- Tajima T, Fujieda K 2008 Prenatal diagnosis and treatment of steroid 21-hydroxylase deficiency. Clin Pediatr Endocrinol 17:95–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nimkarn S, Lin-Su K, Berglind N, Wilson RC, New MI 2007 Aldosterone-to-renin ratio as a marker for disease severity in 21-hydroxylase deficiency congenital adrenal hyperplasia. J Clin Endocrinol Metab 92:137–142 [DOI] [PubMed] [Google Scholar]
- Balsamo A, Cacciari E, Baldazzi L, Tartaglia L, Cassio A, Mantovani V, Piazzi S, Cicognani A, Pirazzoli P, Mainetti B, Zappulla F 2000 CYP21 analysis and phenotype/genotype relationship in the screened population of the Italian Emilia-Romagna region. Clin Endocrinol (Oxf) 53:117–125 [DOI] [PubMed] [Google Scholar]
- Wedell A, Ritzén EM, Haglund-Stengler B, Luthman H 1992 Steroid 21-hydroxylase deficiency: three additional mutated alleles and establishment of phenotype-genotype relationships of common mutations. Proc Natl Acad Sci USA 89:7232–7236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson RC, Mercado AB, Cheng KC, New MI 1995 Steroid 21-hydroxylase deficiency: genotype may not predict phenotype. J Clin Endocrinol Metab 80:2322–2329 [DOI] [PubMed] [Google Scholar]
- Fiet J, Gueux B, Gourmelen M, Kuttenn F, Vexiau P, Couillin P, Pham-Huu-Trung MT, Villette JM, Raux-Demay MC, Galons H, Julien R 1988 Comparison of basal and adrenocorticotropin-stimulated plasma 21-deoxycortisol and 17-hydroxyprogesterone values as biological markers of late-onset adrenal hyperplasia. J Clin Endocrinol Metab 66:659–667 [DOI] [PubMed] [Google Scholar]
- Peter M, Sippell WG, Lorenzen F, Willig RP, Westphal E, Grosse-Wilde H 1990 Improved test to identify heterozygotes for congenital adrenal hyperplasia without index case examination. Lancet 335:1296–1299 [DOI] [PubMed] [Google Scholar]
- Bonfig W, Bechtold S, Schmidt H, Knorr D, Schwarz HP 2007 Reduced final height outcome in congenital adrenal hyperplasia under prednisone treatment: deceleration of growth velocity during puberty. J Clin Endocrinol Metab 92:1635–1639 [DOI] [PubMed] [Google Scholar]
- Punthakee Z, Legault L, Polychronakos C 2003 Prednisolone in the treatment of adrenal insufficiency: a re-evaluation of relative potency. J Pediatr 143:402–405 [DOI] [PubMed] [Google Scholar]
- Rivkees SA, Crawford JD 2000 Dexamethasone treatment of virilizing congenital adrenal hyperplasia: the ability to achieve normal growth. Pediatrics 106:767–773 [DOI] [PubMed] [Google Scholar]
- Merke DP, Cho D, Calis KA, Keil MF, Chrousos GP 2001 Hydrocortisone suspension and hydrocortisone tablets are not bioequivalent in the treatment of children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 86:441–445 [DOI] [PubMed] [Google Scholar]
- German A, Suraiya S, Tenenbaum-Rakover Y, Koren I, Pillar G, Hochberg Z 2008 Control of childhood congenital adrenal hyperplasia and sleep activity and quality with morning or evening glucocorticoid therapy. J Clin Endocrinol Metab 93:4707–4710 [DOI] [PubMed] [Google Scholar]
- Balsamo A, Cicognani A, Baldazzi L, Barbaro M, Baronio F, Gennari M, Bal M, Cassio A, Kontaxaki K, Cacciari E 2003 CYP21 genotype, adult height, and pubertal development in 55 patients treated for 21-hydroxylase deficiency. J Clin Endocrinol Metab 88:5680–5688 [DOI] [PubMed] [Google Scholar]
- Bonfig W, Pozza SB, Schmidt H, Pagel P, Knorr D, Schwarz HP 2009 Hydrocortisone dosing during puberty in patients with classical congenital adrenal hyperplasia: an evidence based recommendation. J Clin Endocrinol Metab 94:3882–3888 [DOI] [PubMed] [Google Scholar]
- Grigorescu-Sido A, Bettendorf M, Schulze E, Duncea I, Heinrich U 2003 Growth analysis in patients with 21-hydroxylase deficiency influence of glucocorticoid dosage, age at diagnosis, phenotype and genotype on growth and height outcome. Horm Res 60:84–90 [DOI] [PubMed] [Google Scholar]
- Manoli I, Kanaka-Gantenbein C, Voutetakis A, Maniati-Christidi M, Dacou-Voutetakis C 2002 Early growth, pubertal development, body mass index and final height of patients with congenital adrenal hyperplasia: factors influencing the outcome. Clin Endocrinol (Oxf) 57:669–676 [DOI] [PubMed] [Google Scholar]
- Van der Kamp HJ, Otten BJ, Buitenweg N, De Muinck Keizer-Schrama SM, Oostdijk W, Jansen M, Delemarre-de Waal HA, Vulsma T, Wit JM 2002 Longitudinal analysis of growth and puberty in 21-hydroxylase deficiency patients. Arch Dis Child 87:139–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmandari E, Hindmarsh PC, Johnston A, Brook CG 2001 Congenital adrenal hyperplasia due to 21-hydroxylase deficiency: alterations in cortisol pharmacokinetics at puberty. J Clin Endocrinol Metab 86:2701–2708 [DOI] [PubMed] [Google Scholar]
- Mullis PE, Hindmarsh PC, Brook CG 1990 Sodium chloride supplement at diagnosis and during infancy in children with salt-losing 21-hydroxylase deficiency. Eur J Pediatr 150:22–25 [DOI] [PubMed] [Google Scholar]
- Frisch H, Battelino T, Schober E, Baumgartner-Parzer S, Nowotny P, Vierhapper H 2001 Salt wasting in simple virilizing congenital adrenal hyperplasia. J Pediatr Endocrinol Metab 14:1649–1655 [DOI] [PubMed] [Google Scholar]
- Muthusamy K, Elamin MB, Smushkin G, Murad MH, Lampropulos JF, Elamin KB, Elnour NOA, Gallegos-Orozco JF, Fatourechi MM, Agrwal N, Lane MA, Albuquerque FN, Erwin PJ, Montori VM 2010 Adult height outcomes in patients with congenital adrenal hyperplasia: a systematic review and metaanalysis. J Clin Endocrinol Metab 95:4161–4172 [DOI] [PubMed] [Google Scholar]
- Gomes LG, Huang N, Agrawal V, Mendonça BB, Bachega TA, Miller WL 2009 Extraadrenal 21-hydroxylation by CYP2C19 and CYP3A4: effect on 21-hydroxylase deficiency. J Clin Endocrinol Metab 94:89–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speiser PW, Agdere L, Ueshiba H, White PC, New MI 1991 Aldosterone synthesis in salt-wasting congenital adrenal hyperplasia with complete absence of adrenal 21-hydroxylase. N Engl J Med 324:145–149 [DOI] [PubMed] [Google Scholar]
- Merke DP, Bornstein SR 2005 Congenital adrenal hyperplasia. Lancet 365:2125–2136 [DOI] [PubMed] [Google Scholar]
- Weise M, Drinkard B, Mehlinger SL, Holzer SM, Eisenhofer G, Charmandari E, Chrousos GP, Merke DP 2004 Stress dose of hydrocortisone is not beneficial in patients with classic congenital adrenal hyperplasia undergoing short-term, high-intensity exercise. J Clin Endocrinol Metab 89:3679–3684 [DOI] [PubMed] [Google Scholar]
- Shibayama Y, Higashi T, Shimada K, Kashimada K, Onishi T, Ono M, Miyai K, Mizutani S 2008 Liquid chromatography-tandem mass spectrometric method for determination of salivary 17α-hydroxyprogesterone: a noninvasive tool for evaluating efficacy of hormone replacement therapy in congenital adrenal hyperplasia. J Chromatogr B Analyt Technol Biomed Life Sci 867:49–56 [DOI] [PubMed] [Google Scholar]
- Zerah M, Ueshiba H, Wood E, Speiser PW, Crawford C, McDonald T, Pareira J, Gruen D, New MI 1990 Prevalence of nonclassical steroid 21-hydroxylase deficiency based on a morning salivary 17-hydroxyprogesterone screening test: a small sample study. J Clin Endocrinol Metab 70:1662–1667 [DOI] [PubMed] [Google Scholar]
- Erhardt E, Sólyom J, Homoki J, Juricskay S, Soltész G 2000 Correlation of blood-spot 17-hydroxyprogesterone daily profiles and urinary steroid profiles in congenital adrenal hyperplasia. J Pediatr Endocrinol Metab 13:205–210 [DOI] [PubMed] [Google Scholar]
- Bode HH, Rivkees SA, Cowley DM, Pardy K, Johnson S 1999 Home monitoring of 17 hydroxyprogesterone levels in congenital adrenal hyperplasia with filter paper blood samples. J Pediatr 134:185–189 [DOI] [PubMed] [Google Scholar]
- Shimon I, Kaiserman I, Sack J 1995 Home monitoring of 17α-hydroxyprogesterone levels by filter paper blood spots in patients with 21-hydroxylase deficiency. Horm Res 44:247–252 [DOI] [PubMed] [Google Scholar]
- Kushnir MM, Rockwood AL, Roberts WL, Pattison EG, Owen WE, Bunker AM, Meikle AW 2006 Development and performance evaluation of a tandem mass spectrometry assay for 4 adrenal steroids. Clin Chem 52:1559–1567 [DOI] [PubMed] [Google Scholar]
- Martin KA, Chang RJ, Ehrmann DA, Ibanez L, Lobo RA, Rosenfield RL, Shapiro J, Montori VM, Swiglo BA 2008 Evaluation and treatment of hirsutism in premenopausal women: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 93:1105–1120 [DOI] [PubMed] [Google Scholar]
- Spritzer P, Billaud L, Thalabard JC, Birman P, Mowszowicz I, Raux-Demay MC, Clair F, Kuttenn F, Mauvais-Jarvis P 1990 Cyproterone acetate versus hydrocortisone treatment in late-onset adrenal hyperplasia. J Clin Endocrinol Metab 70:642–646 [DOI] [PubMed] [Google Scholar]
- Girgis R, Winter JS 1997 The effects of glucocorticoid replacement therapy on growth, bone mineral density, and bone turnover markers in children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 82:3926–3929 [DOI] [PubMed] [Google Scholar]
- Gussinyé M, Carrascosa A, Potau N, Enrubia M, Vicens-Calvet E, Ibáñez L, Yeste D 1997 Bone mineral density in prepubertal and in adolescent and young adult patients with the salt-wasting form of congenital adrenal hyperplasia. Pediatrics 100:671–674 [DOI] [PubMed] [Google Scholar]
- Mora S, Saggion F, Russo G, Weber G, Bellini A, Prinster C, Chiumello G 1996 Bone density in young patients with congenital adrenal hyperplasia. Bone 18:337–340 [DOI] [PubMed] [Google Scholar]
- Stikkelbroeck NM, Beerendonk CC, Willemsen WN, Schreuders-Bais CA, Feitz WF, Rieu PN, Hermus AR, Otten BJ 2003 The long term outcome of feminizing genital surgery for congenital adrenal hyperplasia: anatomical, functional and cosmetic outcomes, psychosexual development, and satisfaction in adult female patients. J Pediatr Adolesc Gynecol 16:289–296 [DOI] [PubMed] [Google Scholar]
- Barzon L, Sonino N, Fallo F, Palu G, Boscaro M 2003 Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol 149:273–285 [DOI] [PubMed] [Google Scholar]
- Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B 1995 Incidentally discovered adrenal masses. Endocr Rev 16:460–484 [DOI] [PubMed] [Google Scholar]
- Jaresch S, Kornely E, Kley HK, Schlaghecke R 1992 Adrenal incidentaloma and patients with homozygous or heterozygous congenital adrenal hyperplasia. J Clin Endocrinol Metab 74:685–689 [DOI] [PubMed] [Google Scholar]
- Barzon L, Maffei P, Sonino N, Pilon C, Baldazzi L, Balsamo A, Del Maschio O, Masi G, Trevisan M, Pacenti M, Fallo F 2007 The role of 21-hydroxylase in the pathogenesis of adrenal masses: review of the literature and focus on our own experience. J Endocrinol Invest 30:615–623 [DOI] [PubMed] [Google Scholar]
- Lightner ES, Levine LS 1993 The adrenal incidentaloma. A pediatric perspective. Am J Dis Child 147:1274–1276 [DOI] [PubMed] [Google Scholar]
- Varan A, Unal S, Ruacan S, Vidinlisan S 2000 Adrenocortical carcinoma associated with adrenogenital syndrome in a child. Med Pediatr Oncol 35:88–90 [DOI] [PubMed] [Google Scholar]
- Claahsen-van der Grinten HL, Stikkelbroeck NM, Sweep CG, Hermus AR, Otten BJ 2006 Fertility in patients with congenital adrenal hyperplasia. J Pediatr Endocrinol Metab 19:677–685 [DOI] [PubMed] [Google Scholar]
- Claahsen-van der Grinten HL, Sweep FC, Blickman JG, Hermus AR, Otten BJ 2007 Prevalence of testicular adrenal rest tumours in male children with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Eur J Endocrinol 157:339–344 [DOI] [PubMed] [Google Scholar]
- Martinez-Aguayo A, Rocha A, Rojas N, García C, Parra R, Lagos M, Valdivia L, Poggi H, Cattani A 2007 Testicular adrenal rest tumors and Leydig and Sertoli cell function in boys with classical congenital adrenal hyperplasia. J Clin Endocrinol Metab 92:4583–4589 [DOI] [PubMed] [Google Scholar]
- Stikkelbroeck NM, Hermus AR, Suliman HM, Jager GJ, Otten BJ 2004 Asymptomatic testicular adrenal rest tumours in adolescent and adult males with congenital adrenal hyperplasia: basal and follow-up investigation after 2.6 years. J Pediatr Endocrinol Metab 17:645–653 [DOI] [PubMed] [Google Scholar]
- Helleday J, Siwers B, Ritzén EM, Carlström K 1993 Subnormal androgen and elevated progesterone levels in women treated for congenital virilizing 21-hydroxylase deficiency. J Clin Endocrinol Metab 76:933–936 [DOI] [PubMed] [Google Scholar]
- Holmes-Walker DJ, Conway GS, Honour JW, Rumsby G, Jacobs HS 1995 Menstrual disturbance and hypersecretion of progesterone in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Clin Endocrinol (Oxf) 43:291–296 [DOI] [PubMed] [Google Scholar]
- Hagenfeldt K, Janson PO, Holmdahl G, Falhammar H, Filipsson H, Frisén L, Thorén M, Nordenskjöld A 2008 Fertility and pregnancy outcome in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Reprod 23:1607–1613 [DOI] [PubMed] [Google Scholar]
- Azziz R, Dewailly D, Owerbach D 1994 Nonclassic adrenal hyperplasia: current concepts. J Clin Endocrinol Metab 78:810–815 [DOI] [PubMed] [Google Scholar]
- Moran C, Azziz R, Carmina E, Dewailly D, Fruzzetti F, Ibañez L, Knochenhauer ES, Marcondes JA, Mendonca BB, Pignatelli D, Pugeat M, Rohmer V, Speiser PW, Witchel SF 2000 21-Hydroxylase-deficient nonclassic adrenal hyperplasia is a progressive disorder: a multicenter study. Am J Obstet Gynecol 183:1468–1474 [DOI] [PubMed] [Google Scholar]
- Barnes RB, Rosenfield RL, Ehrmann DA, Cara JF, Cuttler L, Levitsky LL, Rosenthal IM 1994 Ovarian hyperandrogynism as a result of congenital adrenal virilizing disorders: evidence for perinatal masculinization of neuroendocrine function in women. J Clin Endocrinol Metab 79:1328–1333 [DOI] [PubMed] [Google Scholar]
- Ghizzoni L, Virdis R, Vottero A, Cappa M, Street ME, Zampolli M, Ibañez L, Bernasconi S 1996 Pituitary-ovarian responses to leuprolide acetate testing in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 81:601–606 [DOI] [PubMed] [Google Scholar]
- Fleischman A, Paltiel H, Chow J, Ringelheim J, Gordon CM 2007 Normal ovarian structure and function with normal glucose tolerance in girls with early treatment of classic congenital adrenal hyperplasia. J Pediatr Adolesc Gynecol 20:67–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stikkelbroeck NM, Hermus AR, Schouten D, Suliman HM, Jager GJ, Braat DD, Otten BJ 2004 Prevalence of ovarian adrenal rest tumours and polycystic ovaries in females with congenital adrenal hyperplasia: results of ultrasonography and MR imaging. Eur Radiol 14:1802–1806 [DOI] [PubMed] [Google Scholar]
- Azziz R, Hincapie LA, Knochenhauer ES, Dewailly D, Fox L, Boots LR 1999 Screening for 21-hydroxylase-deficient nonclassic adrenal hyperplasia among hyperandrogenic women: a prospective study. Fertil Steril 72:915–925 [DOI] [PubMed] [Google Scholar]
- Carmina E, Rosato F, Janni A, Rizzo M, Longo RA 2006 Extensive clinical experience: relative prevalence of different androgen excess disorders in 950 women referred because of clinical hyperandrogenism. J Clin Endocrinol Metab 91:2–6 [DOI] [PubMed] [Google Scholar]
- Escobar-Morreale HF, Sanchón R, San Millán JL 2008 A prospective study of the prevalence of nonclassical congenital adrenal hyperplasia among women presenting with hyperandrogenic symptoms and signs. J Clin Endocrinol Metab 93:527–533 [DOI] [PubMed] [Google Scholar]
- Völkl TM, Simm D, Körner A, Rascher W, Kiess W, Kratzsch J, Dörr HG 2009 Does an altered leptin axis play a role in obesity among children and adolescents with classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency? Eur J Endocrinol 160:239–247 [DOI] [PubMed] [Google Scholar]
- Cornean RE, Hindmarsh PC, Brook CG 1998 Obesity in 21-hydroxylase deficient patients. Arch Dis Child 78:261–263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Völkl TM, Simm D, Beier C, Dörr HG 2006 Obesity among children and adolescents with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Pediatrics 117:e98–e105 [DOI] [PubMed] [Google Scholar]
- Roche EF, Charmandari E, Dattani MT, Hindmarsh PC 2003 Blood pressure in children and adolescents with congenital adrenal hyperplasia (21-hydroxylase deficiency): a preliminary report. Clin Endocrinol (Oxf) 58:589–596 [DOI] [PubMed] [Google Scholar]
- Völkl TM, Simm D, Dötsch J, Rascher W, Dörr HG 2006 Altered 24-hour blood pressure profiles in children and adolescents with classical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 91:4888–4895 [DOI] [PubMed] [Google Scholar]
- Botero D, Arango A, Danon M, Lifshitz F 2000 Lipid profile in congenital adrenal hyperplasia. Metabolism 49:790–793 [DOI] [PubMed] [Google Scholar]
- Isguven P, Arslanoglu I, Mesutoglu N, Yildiz M, Erguven M 2008 Bioelectrical impedance analysis of body fatness in childhood congenital adrenal hyperplasia and its metabolic correlates. Eur J Pediatr 167:1263–1268 [DOI] [PubMed] [Google Scholar]
- Bernbaum JC, Umbach DM, Ragan NB, Ballard JL, Archer JI, Schmidt-Davis H, Rogan WJ 2008 Pilot studies of estrogen-related physical findings in infants. Environ Health Perspect 116:416–420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peña A 1997 Total urogenital mobilization–an easier way to repair cloacas. J Pediatr Surg 32:263–267; discussion 267–268 [DOI] [PubMed] [Google Scholar]
- Peña A 1989 The surgical management of persistent cloaca: results in 54 patients treated with a posterior sagittal approach. J Pediatr Surg 24:590–598 [DOI] [PubMed] [Google Scholar]
- Rink RC, Adams MC 1998 Feminizing genitoplasty: state of the art. World J Urol 16:212–218 [DOI] [PubMed] [Google Scholar]
- Rink RC, Herndon CD, Cain MP, Kaefer M, Dussinger AM, King SJ, Casale AJ 2005 Upper and lower urinary tract outcome after surgical repair of cloacal malformations: a three-decade experience. BJU Int 96:131–134 [DOI] [PubMed] [Google Scholar]
- Rink RC, Metcalfe PD, Cain MP, Meldrum KK, Kaefer MA, Casale AJ 2006 Use of the mobilized sinus with total urogenital mobilization. J Urol 176:2205–2211 [DOI] [PubMed] [Google Scholar]
- Burgu B, Duffy PG, Cuckow P, Ransley P, Wilcox DT 2007 Long-term outcome of vaginal reconstruction: comparing techniques and timing. J Pediatr Urol 3:316–320 [DOI] [PubMed] [Google Scholar]
- Nordenskjöld A, Holmdahl G, Frisén L, Falhammar H, Filipsson H, Thorén M, Janson PO, Hagenfeldt K 2008 Type of mutation and surgical procedure affect long-term quality of life for women with congenital adrenal hyperplasia. J Clin Endocrinol Metab 93:380–386 [DOI] [PubMed] [Google Scholar]
- Wisniewski AB, Migeon CJ, Malouf MA, Gearhart JP 2004 Psychosexual outcome in women affected by congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Urol 171:2497–2501 [DOI] [PubMed] [Google Scholar]
- DiMartino-Nardi J, Stoner E, O'Connell A, New MI 1986 The effect of treatment of final height in classical congenital adrenal hyperplasia (CAH). Acta Endocrinol Suppl (Copenh) 279:305–314 [DOI] [PubMed] [Google Scholar]
- New MI, Gertner JM, Speiser PW, Del Balzo P 1989 Growth and final height in classical and nonclassical 21-hydroxylase deficiency. J Endocrinol Invest 12:91–95 [PubMed] [Google Scholar]
- Urban MD, Lee PA, Migeon CJ 1978 Adult height and fertility in men with congenital virilizing adrenal hyperplasia. N Engl J Med 299:1392–1396 [DOI] [PubMed] [Google Scholar]
- Hargitai G, Sólyom J, Battelino T, Lebl J, Pribilincová Z, Hauspie R, Kovács J, Waldhauser F, Frisch H 2001 Growth patterns and final height in congenital adrenal hyperplasia due to classical 21-hydroxylase deficiency. Results of a multicenter study. Horm Res 55:161–171 [DOI] [PubMed] [Google Scholar]
- Eugster EA, Dimeglio LA, Wright JC, Freidenberg GR, Seshadri R, Pescovitz OH 2001 Height outcome in congenital adrenal hyperplasia caused by 21-hydroxylase deficiency: a meta-analysis. J Pediatr 138:26–32 [DOI] [PubMed] [Google Scholar]
- Jääskeläinen J, Voutilainen R 1997 Growth of patients with 21-hydroxylase deficiency: an analysis of the factors influencing adult height. Pediatr Res 41:30–33 [DOI] [PubMed] [Google Scholar]
- Silva IN, Kater CE, Cunha CF, Viana MB 1997 Randomised controlled trial of growth effect of hydrocortisone in congenital adrenal hyperplasia. Arch Dis Child 77:214–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasat R, Espiner EA, Abbott GD 1995 Growth patterns and outcomes in congenital adrenal hyperplasia: effect of chronic treatment regimens. NZ Med J 108:311–314 [PubMed] [Google Scholar]
- Dorr HG 2007 Growth in patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Horm Res 68(Suppl 5):93–99 [DOI] [PubMed] [Google Scholar]
- Hoepffner W, Kaufhold A, Willgerodt H, Keller E 2008 Patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency can achieve their target height: the Leipzig experience. Horm Res 70:42–50 [DOI] [PubMed] [Google Scholar]
- Weintrob N, Dickerman Z, Sprecher E, Galatzer A, Pertzelan A 1997 Non-classical 21-hydroxylase deficiency in infancy and childhood: the effect of time of initiation of therapy on puberty and final height. Eur J Endocrinol 136:188–195 [DOI] [PubMed] [Google Scholar]
- Laue L, Merke DP, Jones JV, Barnes KM, Hill S, Cutler Jr GB 1996 A preliminary study of flutamide, testolactone, and reduced hydrocortisone dose in the treatment of congenital adrenal hyperplasia. J Clin Endocrinol Metab 81:3535–3539 [DOI] [PubMed] [Google Scholar]
- Merke DP, Keil MF, Jones JV, Fields J, Hill S, Cutler Jr GB 2000 Flutamide, testolactone, and reduced hydrocortisone dose maintain normal growth velocity and bone maturation despite elevated androgen levels in children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 85:1114–1120 [DOI] [PubMed] [Google Scholar]
- Quintos JB, Vogiatzi MG, Harbison MD, New MI 2001 Growth hormone therapy alone or in combination with gonadotropin-releasing hormone analog therapy to improve the height deficit in children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 86:1511–1517 [DOI] [PubMed] [Google Scholar]
- Lin-Su K, Vogiatzi MG, Marshall I, Harbison MD, Macapagal MC, Betensky B, Tansil S, New MI 2005 Treatment with growth hormone and luteinizing hormone releasing hormone analog improves final adult height in children with congenital adrenal hyperplasia. J Clin Endocrinol Metab 90:3318–3325 [DOI] [PubMed] [Google Scholar]
- Dacou-Voutetakis C, Karidis N 1993 Congenital adrenal hyperplasia complicated by central precocious puberty: treatment with LHRH-agonist analogue. Ann NY Acad Sci 687:250–254 [DOI] [PubMed] [Google Scholar]
- Van Wyk JJ, Ritzen EM 2003 The role of bilateral adrenalectomy in the treatment of congenital adrenal hyperplasia. J Clin Endocrinol Metab 88:2993–2998 [DOI] [PubMed] [Google Scholar]
- Ogilvie CM, Rumsby G, Kurzawinski T, Conway GS 2006 Outcome of bilateral adrenalectomy in congenital adrenal hyperplasia: one unit’s experience. Eur J Endocrinol 154:405–408 [DOI] [PubMed] [Google Scholar]
- Gmyrek GA, New MI, Sosa RE, Poppas DP 2002 Bilateral laparoscopic adrenalectomy as a treatment for classic congenital adrenal hyperplasia attributable to 21-hydroxylase deficiency. Pediatrics 109:E28 [DOI] [PubMed] [Google Scholar]
- Debono M, Ghobadi C, Rostami-Hodjegan A, Huatan H, Campbell MJ, Newell-Price J, Darzy K, Merke DP, Arlt W, Ross RJ 2009 Modified-release hydrocortisone to provide circadian cortisol profiles. J Clin Endocrinol Metab 94:1548–1554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman ED, Fukushima D, Nogeire C, Roffwarg H, Gallagher TF, Hellman L 1971 Twenty-four hour pattern of the episodic secretion of cortisol in normal subjects. J Clin Endocrinol Metab 33:14–22 [DOI] [PubMed] [Google Scholar]
- Bryan SM, Honour JW, Hindmarsh PC 2009 Management of altered hydrocortisone pharmacokinetics in a boy with congenital adrenal hyperplasia using a continuous subcutaneous hydrocortisone infusion. J Clin Endocrinol Metab 94:3477–3480 [DOI] [PubMed] [Google Scholar]
- Merza Z, Rostami-Hodjegan A, Memmott A, Doane A, Ibbotson V, Newell-Price J, Tucker GT, Ross RJ 2006 Circadian hydrocortisone infusions in patients with adrenal insufficiency and congenital adrenal hyperplasia. Clin Endocrinol (Oxf) 65:45–50 [DOI] [PubMed] [Google Scholar]
- Verma S, Sinaii N, Kim MS, Nieman LK, Ravindran S, Calis KA, Arlt W, Ross RJ, Merke DP 2010 A pharmacokinetic and pharmacodynamic study of delayed- and extended-release hydrocortisone (Chronocort™) versus conventional hydrocortisone (Cortef™) in the treatment of congenital adrenal hyperplasia. Clin Endocrinol (Oxf)72:441–447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merke DP, Chrousos GP, Eisenhofer G, Weise M, Keil MF, Rogol AD, Van Wyk JJ, Bornstein SR 2000 Adrenomedullary dysplasia and hypofunction in patients with classic 21-hydroxylase deficiency. N Engl J Med 343:1362–1368 [DOI] [PubMed] [Google Scholar]
- Riepe FG, Krone N, Krüger SN, Sweep FC, Lenders JW, Dötsch J, Mönig H, Sippell WG, Partsch CJ 2006 Absence of exercise-induced leptin suppression associated with insufficient epinephrine reserve in patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Exp Clin Endocrinol Diabetes 114:105–110 [DOI] [PubMed] [Google Scholar]
- Weise M, Mehlinger SL, Drinkard B, Rawson E, Charmandari E, Hiroi M, Eisenhofer G, Yanovski JA, Chrousos GP, Merke DP 2004 Patients with classic congenital adrenal hyperplasia have decreased epinephrine reserve and defective glucose elevation in response to high-intensity exercise. J Clin Endocrinol Metab 89:591–597 [DOI] [PubMed] [Google Scholar]
- Green-Golan L, Yates C, Drinkard B, VanRyzin C, Eisenhofer G, Weise M, Merke DP 2007 Patients with classic congenital adrenal hyperplasia have decreased epinephrine reserve and defective glycemic control during prolonged moderate-intensity exercise. J Clin Endocrinol Metab 92:3019–3024 [DOI] [PubMed] [Google Scholar]
- Charmandari E, Brook CG, Hindmarsh PC 2002 Why is management of patients with classical congenital adrenal hyperplasia more difficult at puberty? Arch Dis Child 86:266–269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willenberg HS, Bornstein SR, Hiroi N, Päth G, Goretzki PE, Scherbaum WA, Chrousos GP 2000 Effects of a novel corticotropin-releasing-hormone receptor type I antagonist on human adrenal function. Mol Psychiatry 5:137–141 [DOI] [PubMed] [Google Scholar]
- Webster EL, Lewis DB, Torpy DJ, Zachman EK, Rice KC, Chrousos GP 1996 In vivo and in vitro characterization of antalarmin, a nonpeptide corticotropin-releasing hormone (CRH) receptor antagonist: suppression of pituitary ACTH release and peripheral inflammation. Endocrinology 137:5747–5750 [DOI] [PubMed] [Google Scholar]
- Tajima T, Okada T, Ma XM, Ramsey W, Bornstein S, Aguilera G 1999 Restoration of adrenal steroidogenesis by adenovirus-mediated transfer of human cytochromeP450 21-hydroxylase into the adrenal gland of21-hydroxylase-deficient mice. Gene Ther 6:1898–1903 [DOI] [PubMed] [Google Scholar]
- Armengaud JB, Charkaluk ML, Trivin C, Tardy V, Bréart G, Brauner R, Chalumeau M 2009 Precocious pubarche: distinguishing late-onset congenital adrenal hyperplasia from premature adrenarche. J Clin Endocrinol Metab 94:2835–2840 [DOI] [PubMed] [Google Scholar]
- Bidet M, Bellanné-Chantelot C, Galand-Portier MB, Tardy V, Billaud L, Laborde K, Coussieu C, Morel Y, Vaury C, Golmard JL, Claustre A, Mornet E, Chakhtoura Z, Mowszowicz I, Bachelot A, Touraine P, Kuttenn F 2009 Clinical and molecular characterization of a cohort of 161 unrelated women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency and 330 family members. J Clin Endocrinol Metab 94:1570–1578 [DOI] [PubMed] [Google Scholar]
- Török D, Halász Z, Garami M, Homoki J, Fekete G, Sólyom J 2003 Limited value of serum steroid measurements in identification of mild form of 21-hydroxylase deficiency. Exp Clin Endocrinol Diabetes 111:27–32 [DOI] [PubMed] [Google Scholar]
- Speiser PW, White PC 1998 Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency. Clin Endocrinol (Oxf) 49:411–417 [DOI] [PubMed] [Google Scholar]
- Wedell A, Thilén A, Ritzén EM, Stengler B, Luthman H 1994 Mutational spectrum of the steroid 21-hydroxylase gene in Sweden: implications for genetic diagnosis and association with disease manifestation. J Clin Endocrinol Metab 78:1145–1152 [DOI] [PubMed] [Google Scholar]
- New MI 2006 Extensive clinical experience: nonclassical 21-hydroxylase deficiency. J Clin Endocrinol Metab 91:4205–4214 [DOI] [PubMed] [Google Scholar]
- Bidet M, Bellanné-Chantelot C, Galand-Portier MB, Golmard JL, Tardy V, Morel Y, Clauin S, Coussieu C, Boudou P, Mowzowicz I, Bachelot A, Touraine P, Kuttenn F 2010 Fertility in women with nonclassical congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 95:1182–1190 [DOI] [PubMed] [Google Scholar]
- Moran C, Azziz R, Weintrob N, Witchel SF, Rohmer V, Dewailly D, Marcondes JA, Pugeat M, Speiser PW, Pignatelli D, Mendonca BB, Bachega TA, Escobar-Morreale HF, Carmina E, Fruzzetti F, Kelestimur F 2006 Reproductive outcome of women with 21-hydroxylase-deficient nonclassic adrenal hyperplasia. J Clin Endocrinol Metab 91:3451–3456 [DOI] [PubMed] [Google Scholar]
- Riepe FG, Krone N, Viemann M, Partsch CJ, Sippell WG 2002 Management of congenital adrenal hyperplasia: results of the ESPE questionnaire. Horm Res 58:196–205 [DOI] [PubMed] [Google Scholar]
- Falhammar H, Filipsson H, Holmdahl G, Janson PO, Nordenskjöld A, Hagenfeldt K, Thorén M 2007 Fractures and bone mineral density in adult women with 21-hydroxylase deficiency. J Clin Endocrinol Metab 92:4643–4649 [DOI] [PubMed] [Google Scholar]
- Falhammar H, Filipsson H, Holmdahl G, Janson PO, Nordenskjöld A, Hagenfeldt K, Thorén M 2007 Metabolic profile and body composition in adult women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 92:110–116 [DOI] [PubMed] [Google Scholar]
- Martinerie L, Viengchareun S, Delezoide AL, Jaubert F, Sinico M, Prevot S, Boileau P, Meduri G, Lombès M 2009 Low renal mineralocorticoid receptor expression at birth contributes to partial aldosterone resistance in neonates. Endocrinology 150:4414–4424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arlt W, Krone N 2007 Adult consequences of congenital adrenal hyperplasia. Horm Res 68(Suppl 5):158–164 [DOI] [PubMed] [Google Scholar]
- Premawardhana LD, Hughes IA, Read GF, Scanlon MF 1997 Longer term outcome in females with congenital adrenal hyperplasia (CAH): the Cardiff experience. Clin Endocrinol (Oxf) 46:327–332 [DOI] [PubMed] [Google Scholar]
- Young MC, Robinson JA, Read GF, Riad-Fahmy D, Hughes IA 1988 170H-progesterone rhythms in congenital adrenal hyperplasia. Arch Dis Child 63:617–623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claahsen-van der Grinten HL, Otten BJ, Takahashi S, Meuleman EJ, Hulsbergen-van de Kaa C, Sweep FC, Hermus AR 2007 Testicular adrenal rest tumors in adult males with congenital adrenal hyperplasia: evaluation of pituitary-gonadal function before and after successful testis-sparing surgery in eight patients. J Clin Endocrinol Metab 92:612–615 [DOI] [PubMed] [Google Scholar]
- Chakhtoura Z, Bachelot A, Samara-Boustani D, Ruiz JC, Donadille B, Dulon J, Christin-Maître S, Bouvattier C, Raux-Demay MC, Bouchard P, Carel JC, Leger J, Kuttenn F, Polak M, Touraine P 2008 Impact of total cumulative glucocorticoid dose on bone mineral density in patients with 21-hydroxylase deficiency. Eur J Endocrinol 158:879–887 [DOI] [PubMed] [Google Scholar]
- Conway GS 2007 Congenital adrenal hyperplasia: adolescence and transition. Horm Res 68(Suppl 5):155–157 [DOI] [PubMed] [Google Scholar]
- Hughes IA 2004 Congenital adrenal hyperplasia: transitional care. Growth Horm IGF Res 14(Suppl A):S60–S66 [DOI] [PubMed] [Google Scholar]
- Kruse B, Riepe FG, Krone N, Bosinski HA, Kloehn S, Partsch CJ, Sippell WG, Mönig H 2004 Congenital adrenal hyperplasia: how to improve the transition from adolescence to adult life. Exp Clin Endocrinol Diabetes 112:343–355 [DOI] [PubMed] [Google Scholar]
- Speiser PW, White PC 2003 Congenital adrenal hyperplasia. N Engl J Med 349:776–788 [DOI] [PubMed] [Google Scholar]
- Casteras A, De Silva P, Rumsby G, Conway GS 2009 Reassessing fecundity in women with classical congenital adrenal hyperplasia (CAH): normal pregnancy rate but reduced fertility rate. Clin Endocrinol (Oxf) 70:833–837 [DOI] [PubMed] [Google Scholar]
- Cabrera MS, Vogiatzi MG, New MI 2001 Long term outcome in adult males with classic congenital adrenal hyperplasia. J Clin Endocrinol Metab 86:3070–3078 [DOI] [PubMed] [Google Scholar]
- Jääskeläinen J, Voutilainen R 2000 Long-term outcome of classical 21-hydroxylase deficiency: diagnosis, complications and quality of life. Acta Paediatr 89:183–187 [DOI] [PubMed] [Google Scholar]
- Reisch N, Flade L, Scherr M, Rottenkolber M, Pedrosa Gil F, Bidlingmaier M, Wolff H, Schwarz HP, Quinkler M, Beuschlein F, Reincke M 2009 High prevalence of reduced fecundity in men with congenital adrenal hyperplasia. J Clin Endocrinol Metab 94:1665–1670 [DOI] [PubMed] [Google Scholar]
- Jääskeläinen J, Kiekara O, Hippeläinen M, Voutilainen R 2000 Pituitary gonadal axis and child rate in males with classical 21-hydroxylase deficiency. J Endocrinol Invest 23:23–27 [DOI] [PubMed] [Google Scholar]
- Claahsen-van der Grinten HL, Otten BJ, Hermus AR, Sweep FC, Hulsbergen-van de Kaa CA 2008 Testicular adrenal rest tumors in patients with congenital adrenal hyperplasia can cause severe testicular damage. Fertil Steril 89:597–601 [DOI] [PubMed] [Google Scholar]
- Lo JC, Schwitzgebel VM, Tyrrell JB, Fitzgerald PA, Kaplan SL, Conte FA, Grumbach MM 1999 Normal female infants born of mothers with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab 84:930–936 [DOI] [PubMed] [Google Scholar]
- Carmichael P, Ransley P 2002 Telling children about a physical intersex condition. Dialogues Pediatr Urol 25:7–8 [Google Scholar]
- Cohen-Kettenis PT, Pfäfflin F (eds) 2003 Transgenderism and intersexuality in childhood and adolescence. Making choices. Thousand Oaks, CA: Sage [Google Scholar]
- Consortium on the management of disorders of sex differentiation 2006 Clinical guidelines for the management of disorders of sex differentiation in childhood. Intersex Society of North American. available at www.dsdguidelines.org [Google Scholar]
- Consortium on the management of disorders of sex differentiation 2006 Handbook for parents. Intersex Society of North America. Available at www.dsdguidelines.org [Google Scholar]
- Hughes IA, Houk C, Ahmed SF, Lee PA 2006 Consensus statement on management of intersex disorders. Arch Dis Child 91:554–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dessens AB, Slijper FM, Drop SL 2005 Gender dysphoria and gender change in chromosomal females with congenital adrenal hyperplasia. Arch Sex Behav 34:389–397 [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg HF, Dolezal C, Baker SW, New MI 2008 Sexual orientation in women with classical or non-classical congenital adrenal hyperplasia as a function of degree of prenatal androgen excess. Arch Sex Behav 37:85–99 [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg HF 2008 Treatment guidelines for children with disorders of sex development. Neuropsychiatr Enfance Adolesc 56:345–349 [Google Scholar]
- Money J 1994 Sex errors of the body and related syndromes: a guide to counseling children, adolescents, and their families. 2nd ed. Baltimore: Paul H. Brookes [Google Scholar]
- Meyer-Bahlburg HF 1999 Health-related quality of life in intersexuality. Acta Paediatr Suppl 88:114–115 [DOI] [PubMed] [Google Scholar]
- Frisén L, Nordenström A, Falhammar H, Filipsson H, Holmdahl G, Janson PO, Thorén M, Hagenfeldt K, Möller A, Nordenskjöld A 2009 Gender role behavior, sexuality, and psychosocial adaptation in women with congenital adrenal hyperplasia due to CYP21A2 deficiency. J Clin Endocrinol Metab 94:3432–3439 [DOI] [PubMed] [Google Scholar]
- Johannsen TH, Ripa CP, Mortensen EL, Main KM 2006 Quality of life in 70 women with disorders of sex development. Eur J Endocrinol 155:877–885 [DOI] [PubMed] [Google Scholar]
- Warne G, Grover S, Hutson J, Sinclair A, Metcalfe S, Northam E, Freeman J 2005 A long-term outcome study of intersex conditions. J Pediatr Endocrinol Metab 18:555–567 [DOI] [PubMed] [Google Scholar]
- Berenbaum SA, Korman Bryk K, Duck SC, Resnick SM 2004 Psychological adjustment in children and adults with congenital adrenal hyperplasia. J Pediatr 144:741–746 [DOI] [PubMed] [Google Scholar]
- Kuhnle U, Bullinger M 1997 Outcome of congenital adrenal hyperplasia. Pediatr Surg Int 12:511–515 [DOI] [PubMed] [Google Scholar]
- Al-Maghribi H 2007 Congenital adrenal hyperplasia: problems with developmental anomalies of the external genitalia and sex assignment. Saudi J Kidney Dis Transpl 18:405–413 [PubMed] [Google Scholar]
- Meyer-Bahlburg HF 2002 Gender assignment and reassignment in intersexuality: controversies, data, and guidelines for research. Adv Exp Med Biol 511:199–223 [DOI] [PubMed] [Google Scholar]
- Berenbaum SA, Bailey JM 2003 Effects on gender identity of prenatal androgens and genital appearance: evidence from girls with congenital adrenal hyperplasia. J Clin Endocrinol Metab 88:1102–1106 [DOI] [PubMed] [Google Scholar]
- Crouch NS, Liao LM, Woodhouse CR, Conway GS, Creighton SM 2008 Sexual function and genital sensitivity following feminizing genitoplasty for congenital adrenal hyperplasia. J Urol 179:634–638 [DOI] [PubMed] [Google Scholar]
- Minto CL, Liao LM, Woodhouse CR, Ransley PG, Creighton SM 2003 The effect of clitoral surgery on sexual outcome in individuals who have intersex conditions with ambiguous genitalia: a cross-sectional study. Lancet 361:1252–1257 [DOI] [PubMed] [Google Scholar]
- Ogilvie CM, Crouch NS, Rumsby G, Creighton SM, Liao LM, Conway GS 2006 Congenital adrenal hyperplasia in adults: a review of medical, surgical and psychological issues. Clin Endocrinol (Oxf) 64:2–11 [DOI] [PubMed] [Google Scholar]
- Sircili MH, de Mendonca BB, Denes FT, Madureira G, Bachega TA, e Silva FA 2006 Anatomical and functional outcomes of feminizing genitoplasty for ambiguous genitalia in patients with virilizing congenital adrenal hyperplasia. Clinics (Sao Paulo) 61:209–214 [DOI] [PubMed] [Google Scholar]
- Liao L, Doyle J, Crouch NS, Creighton SM 2006 Dilation as treatment for vaginal agenesis and hypoplasia: a pilot exploration of benefits and barriers as perceived by patients. J Obstet Gynaecol 26:144–148 [DOI] [PubMed] [Google Scholar]
- Intersex Society of North America 1995 Recommendations for treatment: intersex infants and children (pamphlet). San Francisco: Intersex Society of North America [Google Scholar]
- Sytsma SE 2006 Ethics and intersex. Dordrecht, The Netherlands: Springer [Google Scholar]
- Diamond M, Sigmundson HK 1997 Management of intersexuality. Guidelines for dealing with persons with ambiguous genitalia. Arch Pediatr Adolesc Med 151:1046–1050 [DOI] [PubMed] [Google Scholar]
- Swiglo BA, Murad MH, Schünemann HJ, Kunz R, Vigersky RA, Guyatt GH, Montori VM 2008 A case for clarity, consistency, and helpfulness: state-of-the-art clinical practice guidelines in endocrinology using the grading of recommendations, assessment, development, and evaluation system. J Clin Endocrinol Metab 93:666–673 [DOI] [PubMed] [Google Scholar]
- Bachega TA, Billerbeck AE, Marcondes JA, Madureira G, Arnhold IJ, Mendonca BB 2000 Influence of different genotypes on 17-hydroxyprogesterone levels in patients with nonclassical congenital adrenal hyperplasia due to 21-hydorxylase deficiency. Clin Endocrinol (Oxf) 52:601–607 [DOI] [PubMed] [Google Scholar]
- Speiser PW, Serrat J, New MI, Gertner JM 1992 Insulin insensitivity in adrenal hyperplasia due to nonclassical steroid 21-hydroxylase deficiency. J Clin Endocrinol Metab 75:1421–1424 [DOI] [PubMed] [Google Scholar]
- Fiet J, Gueux B, Rauxdemay MC, Kuttenn F, Vexiau P, Brerault J, Couillin P, Galons H, Villette J, Julien R, Dreux C 1989 Increased plasma 21-deoxycorticosterone (21-DB) levels in late-onset adrenal 21-hydroxylase deficiency suggest a mild defect of the mineralocorticoid pathway. J Clin Endocrinol Metab 68:542–547 [DOI] [PubMed] [Google Scholar]