Abstract
Objective:
There is substantial evidence of a link between parental substance use disorders and antisocial behavior and childhood disruptive disorders in their offspring, but it is unclear whether this transmission is specific to particular disorders, or if a general liability accounts for familial resemblance. The current study examined if the association between parental externalizing disorders and childhood disruptive disorders in their pre-adolescent offspring is due to the transmission of general or disorder-specific liabilities, and estimated the genetic and environmental contributions to variation in these general and specific liability indicators.
Method:
Participants were 1069 families consisting of 11-year-old twins and their biological mother and father. We used structural equation modeling to simultaneously estimate the general and specific transmission effects of four parental externalizing disorders (conduct disorder, adult antisocial behavior, alcohol dependence, and drug dependence) on childhood disruptive disorders (attention deficit/hyperactivity disorder, conduct disorder, and oppositional defiant disorder).
Results:
Parent-child resemblance was accounted for by the transmission of a general liability to externalizing disorders, and this general liability was highly heritable. Specific effects were also detected, but for sibling rather than parental transmission. Specific genetic and nonshared environmental effects were detected for each childhood disruptive disorder, but only conduct disorder exhibited a significant shared environmental effect.
Conclusions:
A highly heritable general liability accounts for the parent-child transmission of externalizing psychopathology from parents to their pre-adolescent offspring. This general liability should be a focus of research for both etiology and intervention.
Numerous studies have demonstrated that parental substance use disorders and antisocial behavior are associated with elevated levels of childhood disruptive disorders in their offspring. For example, investigations using family, twin, and offspring of twin designs have reported that a history of parental alcohol dependence is associated with increased rates of attention deficit/hyperactivity disorder (ADHD) (1) conduct disorder (2, 3), and oppositional defiant disorder (3). A number of other studies have also established a link between parental antisocial behavior and illicit drug abuse with offspring conduct disorder (4-6).
Given the number of parent-child effects, it is reasonable to ask: are there specific associations between parental substance use disorders and antisocial behavior and childhood disruptive disorders, or can a transmission of some type of general liability account for parent-child resemblance? For example, some well-controlled family and adoption studies have reported specific transmission effects (2, 4, 7, 8). On the other hand, a growing body of literature supports the notion of a general transmission effect (4, 9-11).
A conceptual model that can help account for this general transmission effect derives from findings examining the comorbidity among substance use disorders and antisocial behavior. Specifically, twin studies have demonstrated that the comorbidity among substance use disorders and antisocial behavior can best be accounted for by a highly heritable (~.80) general liability dimension, typically referred to as the latent externalizing factor (EXT) (12-18). A similar general factor (albeit somewhat more influenced by shared environmental factors) seems to underlie the comorbidity among childhood disruptive disorders (ADHD, conduct disorder, and oppositional defiant disorder) (19-21). For instance, recent data suggests that symptoms of hyperactivity-impulsivity and oppositionality represent the same underlying liability dimension (22). It may be that EXT is a latent, non-specific liability that accounts for the general transmission effects between parents and children.
One method of disentangling the general and specific effects entails fitting a model that estimates general and specific transmission effects simultaneously. Hicks et al. (13) tested such a model by utilizing a twin-family design to simultaneously estimate the general and specific transmission effects from parents to 17-year old offspring for conduct disorder, adult antisocial behavior (the adult criteria for antisocial personality disorder), alcohol dependence, and drug dependence. Results demonstrated that the transmission of a general EXT liability could account for the parent-child resemblance for the 4 externalizing disorders and that this general liability was highly heritable. Additionally, Hicks et al found evidence for specific transmission for conduct disorder, alcohol dependence, and drug dependence, but across siblings rather than from parents to offspring (i.e., horizontal as opposed to vertical transmission). As such, this study provided a model for examining familial transmission in terms of delineating the relative contributions of general and specific effects.
The current study sought to replicate and extend Hicks et al. by employing a similar family transmission model to clarify the association between substance use disorders and antisocial behavior in parents and childhood disruptive disorders in their pre-adolescent offspring. Specifically, we aimed to determine if the transmission of the general EXT liability alone could account for parent-child resemblance while also estimating the genetic and environmental contributions to variability in the general and specific transmission effects. We again employed a twin-family design such that each family included both biological parents and a twin pair. In contrast to Hicks et al., however, the twins were from a different cohort and approximately 11 years-old. Moreover, we focused on transmission to childhood disruptive disorders, namely, ADHD, oppositional defiant disorder, and conduct disorder; externalizing disorders that were developmentally appropriate to assess at this age. Additionally, a multi-informant approach (child, mother, and teacher) was used to assess the childhood disruptive disorders. Finally the sample size for the current investigation included over 1000 families (roughly twice the size employed by Hicks et al.) providing excellent power to detect effects. In line with the findings from Hicks et al, we hypothesized that most of the parent-child resemblance will be mainly accounted for by the transmission of a highly heritable general liability to externalizing psychopathology.
Method
For a full description of sample recruitment, demographic characteristics, measures, and statistical analysis plan, please see the supplemental materials. All parents provided written informed consent for themselves and their offspring, and all twins gave written informed assent. The study protocols were reviewed and approved by an internal review board.
Sample
Participants were members of 1069 families (N = 4276) from the Minnesota Twin Family Study (MTFS). There were 685 monozygotic twin pairs (52% male) and 384 dizygotic twin pairs (49% male). For the twins, the mean age was 11.8 (SD = 0.4); for the mothers, 40.2 (SD = 4.9); and for the fathers, 42.6 (SD = 5.4). Ninety-six percent of the families were Caucasian.
Measures
Parent and child externalizing disorders were assessed via the Substance Abuse Module of the Composite International Diagnostic Interview (23), a slightly modified version of the Structured Clinical Interview for DSM-III-R-II that included additional probes to assess frequency of symptoms for conduct disorder and antisocial personality disorder (24) and the Diagnostic Interview for Children and Adolescents – Revised (DICA-R) (25), respectively. We assessed parental symptoms of lifetime conduct disorder, adult antisocial behavior, alcohol dependence, and drug dependence. We also assessed symptoms of offspring ADHD, conduct disorder, and oppositional defiant disorder using the DICA-R. For the twins, a symptom was considered present if reported by either the mother or twin. Finally, teacher ratings of ADHD, conduct disorder, and oppositional defiant disorder were collected for up to 3 teachers per twin. The mean of the teacher ratings was used for the twin’s teacher rating variable, and a composite of the mother, child, and teacher ratings was made for the indices of childhood disruptive disorders by taking a mean of the three reporters.
Statistical Analysis
We used structural equation modeling to investigate the link between adult externalizing disorders in parents and childhood disruptive disorders in their pre-adolescent offspring as well as the generality versus the specificity of transmission effects. The general liability to externalizing disorders was conceptualized as a latent EXT phenotype (12, 13, 15, 19, 26). For parents, EXT was defined by alcohol dependence, drug dependence, conduct disorder, and adult antisocial behavior, and termed EXT-P (parent). For the twins, EXT was defined by ADHD, conduct disorder, and oppositional defiant disorder, and termed EXT-O (offspring). Symptom counts were used for all disorders. General transmission effects were operationalized as the latent correlations between the EXT-P and EXT-O phenotypes. We estimated the specific transmission effects of a given disorder by allowing the residual variance (i.e., variance unaccounted for by EXT) of the parental symptom count variables to covary with the residuals of the twins' symptom counts.
We also used standard biometric models to examine the influence of additive genetic, shared environmental, and non-shared environmental influences on EXT-O factor as well as on each childhood disruptive disorders. The additive genetic component (a2) refers the effect of individual genes summed over loci on trait variance. Genetic influences are inferred if the monozygotic correlation is greater than the dizygotic correlation for a given trait. Shared environmental (c2) effects refer to environmental influences that increase similarity between members of a twin pair. Shared environmental effects are inferred if the dizygotic correlation is more than ½ the monozygotic correlation. Non-shared environmental (e2) effects refer to environmental factors that contribute to differences between members of a twin pair. Measurement error is also included in the estimate of e2. Also, if the monozygotic correlation is more than ½ the dizygotic correlation, it is common practice to investigate non-additive genetic (dominance, d2) models as an alternative to ACE models. Because c2 and d2 are estimated using the same information, the two parameters cannot be estimated simultaneously. Biometric analyses were conducted using the computer program Mx (27).
Model fitting for family transmission effects was conducted in Mplus 5 (28) using a robust maximum-likelihood estimator, which is appropriate when analyzing non-normal variables. The non-normality was due to positive skew in the symptom counts variables as is typical for population-based samples. The fit of models was evaluated using the mean-adjusted (Satorra-Bentler) χ2 fit statistic (29), the Bayesian information criterion (BIC) (χ2–df [ln N]) (30), and the root mean-square error of approximation (RMSEA) (31). The mean adjusted χ2 provides an overall estimate of model fit for non-normal data. For nested models, the difference in χ2 can be used to determine if additional parameters significantly improve model fit. Because we conducted 27 tests of specific transmission, we used a Bonferroni corrected α of .0019 (.05/27) when comparing Δχ2 for nested models. The BIC is a function of a model's χ2 value and df, and penalizes the model fit for the retention of unnecessary parameters. This fit index is not interpreted in isolation; rather it is used to compare alternative models such that lower BIC scores are indicative of better fit. When comparing models, a difference in BIC of 0–2 is considered weak evidence in support of the model with the lower BIC value, a difference of 2–6 is considered positive evidence, a difference of 6–10 is considered strong evidence, and a difference over 10 is considered very strong evidence (32). The RMSEA provides an estimate of discrepancy in model fit per df, and with values of .08 indicating a good fit and .05 or less indicating a very good fit to the data (31).
Results
General versus Specific Transmission of Childhood Disruptive Disorders
Results of the model fitting are provided in Table 1. An initial model that allowed for only general transmission of externalizing disorders from parents to offspring provided an adequate fit to the data (χ2 189 = 699.96, BIC = −618.22, RMSEA = 0.071). This model served as the comparison model for all subsequent analyses.
Table 1.
Indexes of Fit for Alternative Models for the Family Transmission of Childhood Disruptive Disorders
| Model | χ 2 | df | RMSEA | BIC | Δχ2, df |
|---|---|---|---|---|---|
| General Transmission Only | 699.96 | 189 | .071 | -618.22 | ---- |
| Specific Transmission Effects | |||||
| Mother Conduct Disorder | |||||
| ADHD | 691.14 | 188 | .071 | −620.06 | 8.82, 1 |
| Conduct Disorder | 699.66 | 188 | .071 | −611.55 | 0.30, 1 |
| Oppositional-Defiant Disorder | 695.05 | 188 | .071 | −616.16 | 4.91, 1 |
| Mother Adult Antisocial Behavior | |||||
| ADHD | 692.31 | 188 | .071 | −618.89 | 7.65, 1 |
| Conduct Disorder | 698.48 | 188 | .071 | −612.72 | 1.48, 1 |
| Oppositional-Defiant Disorder | 699.23 | 188 | .071 | −611.97 | 0.73, 1 |
| Mother Alcohol Dependence | |||||
| ADHD | 698.76 | 188 | .071 | −612.44 | 1.20, 1 |
| Conduct Disorder | 700.71 | 188 | .071 | −610.49 | 0.75, 1 |
| Oppositional-Defiant Disorder | 699.63 | 188 | .071 | −611.58 | 0.33, 1 |
| Mother Drug Dependence | |||||
| ADHD | 698.11 | 188 | .071 | −613.10 | 1.85, 1 |
| Conduct Disorder | 698.76 | 188 | .071 | −612.44 | 1.20, 1 |
| Oppositional Defiant Disorder | 698.85 | 188 | .071 | −612.36 | 1.11, 1 |
| Father Conduct Disorder | |||||
| ADHD | 698.37 | 188 | .071 | −612.83 | 1.59, 1 |
| Conduct Disorder | 699.17 | 188 | .071 | -612.03 | 0.79, 1 |
| Oppositional Defiant Disorder | 698.53 | 188 | .071 | −612.68 | 1.43, 1 |
| Father Adult Antisocial Behavior | |||||
| ADHD | 699.66 | 188 | .071 | −611.54 | 0.30, 1 |
| Conduct Disorder | 695.35 | 188 | .071 | −615.85 | 4.61, 1 |
| Oppositional Defiant Disorder | 698.01 | 188 | .071 | −613.19 | 1.95, 1 |
| Father Alcohol Dependence | |||||
| ADHD | 697.16 | 188 | .071 | −614.04 | 2.80, 1 |
| Conduct Disorder | 696.15 | 188 | .071 | −615.05 | 3.81, 1 |
| Oppositional Defiant Disorder | 698.08 | 188 | .071 | −613.12 | 1.88, 1 |
| Father Drug Dependence | |||||
| ADHD | 699.23 | 188 | .071 | −611.97 | 0.73, 1 |
| Conduct Disorder | 699.05 | 188 | .071 | −612.15 | 0.91, 1 |
| Oppositional Defiant Disorder | 698.80 | 188 | .071 | −612.40 | 1.16, 1 |
| Cross-Twin (Siblings) | |||||
| ADHD | 493.67 | 187 | .055 | −810.35 | 206.29 a, 2 |
| Conduct Disorder | 528.71 | 187 | .058 | −775.52 | 171.25 a, 2 |
| Oppositional Defiant Disorder | 560.99 | 187 | .061 | −743.24 | 138.97 a, 2 |
| Best fitting Model | |||||
| General transmission from parents to offspring with cross-twin specific effects for ADHD, Conduct |
230.97 | 183 | .022 | −1045.36 | 468.99 a, 6 |
| Disorder, Oppositional Defiant | |||||
| Disorder | |||||
| Equate maternal and paternal general transmission | 231.55 | 184 | .022 | −1051.76 | 468.41 a, 5 |
Note. All χ2 change values reflect the difference in χ2 as compared to the first (general transmission only) model. A Bonferroni corrected α of .0019 (.05 divided by 27 tests of specific transmission) was used as the threshold for a significant Δχ2. None of the specific parent to child effects exceeded this threshold (the largest effect had a p = .0029 and accounted for only 0.56% of the variance in the childhood disorder). BIC = Bayesian information criterion; RMSEA = root mean square error of approximation.
χ2 change significantly different at p < 0.001
To test for disorder-specific effects, we allowed the residual variances of parental disorders to covary with the residual variances of offspring disorders (e.g., mother conduct disorder and twin conduct disorder; father alcohol dependence and twin ADHD). If model fit improved, this indicated that parents and offspring were more similar than would be expected given only general transmission. To maximize power to detect specific effects, we conducted 1df tests separately for each paternal and maternal disorder (see Table 1 under “Specific Transmission Effects”), which are differentiated from the general transmission-only model by a reduction of 1df and subsequent changes in model fit indexes. We conducted 24 tests to determine if a specific effect model supporting parent-offspring transmission fit better than the general transmission model. None of the specific transmission effects resulted in a significant reduction in χ2 (Bonferroni corrected α < .0019), a drop in BIC of at least 2 (rather, almost all specific effects resulted in higher BIC values), or a lower RMSEA value. Therefore, the results show that a general transmission only model can account for familial resemblance on adult externalizing disorders in parents and childhood disruptive disorders in their offspring.
Next, we examined specific cross-twin (sibling) effects for ADHD, conduct disorder, and oppositional defiant disorder by allowing the residual variance of each disorder to correlate across members of the twin pair. We allowed the paths to vary by zygosity, therefore, these were 2df tests for each disorder. Cross-twin specific effects were detected for each childhood disorder (Table 1, bottom), indicating familial liability factors to these disorders that are independent of the general liability, but that do not stem from parental externalizing disorders.
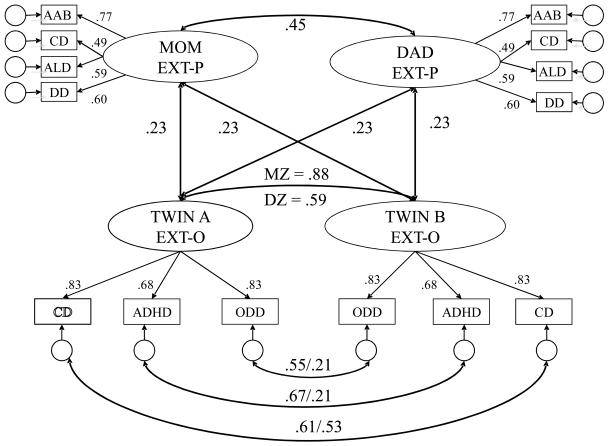
Maternal and paternal general transmission effects were estimated as the latent correlation between EXT-P and EXT-O. The latent correlations between mother and father EXT-P and EXT-O were r = 0.26 (95% confidence interval [CI], 0.13-0.38) and r = 0.20 (95% CI, 0.12-0.29), respectively. As such, in the next model, we equated the effects of EXT-P on EXT-O. Equating the parental effects yielded a lower BIC value, indicating the strength of maternal and paternal transmission was not significantly different. The resulting latent correlation between EXT-P and EXT-O (r = 0.23; 95% CI, 0.14-0.31) was moderate and represents the effect of the general transmission of parental externalizing disorders on offspring childhood disruptive disorders (Figure 1).
Figure 1. Final Model for General and Specific Transmission Effects.
Note: All path coefficients in the figure are standardized. All paths presented in the figure are significant, p < .01. The latent externalizing (EXT) variables represent the general liability factors common among the 4 diagnoses for parents and 3 disorders for offspring. The circular blank latent variables associated with each disorder are the residual variances and represent liability factors that are specific to the disorder or unaccounted for by the general EXT liability factor. Double-headed arrows linking mother and father EXT to twin A and twin B EXT represent the general transmission effect for the 4 disorders. All parent-to-offspring effects were constrained to be equal, as model-fitting results indicated that there was not a statistically significant difference in the strength of maternal and paternal transmission. The double-headed arrow that links twin A and twin B EXT indexes monozygotic/dizygotic twin similarity for the general liability to the 3 disorders. The double-headed arrows linking the residual variances of ADHD, conduct disorder, and oppositional defiant disorder across members of the twin pair represent disorder-specific liabilities that increase sibling similarity but that are independent of the general EXT liability. AAB = Adult Antisocial Behavior; CD = Conduct disorder; ALD = Alcohol Dependence; DD = Drug Dependence; ADHD = Attention-Deficit Hyperactive Disorder; ODD = Oppositional Defiant Disorder; EXT-P = Externalizing factor for parents; EXT-O = Externalizing factor for offspring.
To ensure that the parental transmission effects did not differ by the gender of the offspring, we conducted the same tests of specific and general transmission effects (i.e., following the procedure and models outlined above) separately for male and female twins. The general transmission effects could be equated for male and female twins without a loss in model fit. Moreover, we did not detect any specific transmission from parents to offspring for either male or female twins. To ascertain that these results did not differ by informant, we fit separate models using parent, child, and teacher reports for offspring disorders. The results were consistent with those in Figure 1.
Genetic and Environmental Contributions to Variation in EXT and Disorder-Specific Liabilities
In testing the magnitude of genetic influences on cross-twin effects, we first examined the latent correlation between mother and father EXT-P. The correlation between parents sometimes increases the similarity of dizygotic twins in twin studies, thereby decreasing the study heritability (33). There was a significant correlation between maternal and paternal EXT (r = 0.45; 95% CI, 0.31-0.60). Despite this finding, the cross-twin correlations for EXT-O differed strongly across zygosity indicating a strong genetic influence (Figure 1). The dizygotic correlation, however, was greater than ½ the monozygotic correlation suggesting shared environmental effects on the general EXT-O factor. For the disorder-specific effects (Figure 1, bottom), the monozygotic correlations for ADHD and oppositional defiant disorder were larger than the dizygotic twin correlations, indicting specific genetic effects. In contrast, the monozygotic and dizygotic correlations were quite similar for conduct disorder, indicating a shared environmental effect.
Next, we fit biometric models to decompose the variance of each disorder into its additive genetic (a2), shared environmental (c2), and non-shared environmental (e2) factors (see Table 2). Genetic effects were large for ADHD and oppositional defiant disorder, and moderate for conduct disorder. Notably, because the monozygotic correlation for ADHD was more than ½ the dizygotic correlation, we also investigated a non-additive genetic model, with dominance (d2) replacing the c2 effect. This model did not fit significantly better than the ACE model (change in BIC was only −1.62), and d2 was not significant (d2 = .27; CI = 0.00-.60). Thus, an ACE model was fit for each disorder. Only conduct disorder evidenced a notable shared environmental component. Small non-shared environmental effects were detected for each disorder.
Table 2.
Twin correlations, univariate parameter estimates (95% confidence intervals) for additive genetic effects (A), shared environmental effects (C), and nonshared environmental effects (E) contributing to childhood disruptive disorders.
| Variable | Monozygotic Pairs |
Dizygotic Pairs |
A | C | E |
|---|---|---|---|---|---|
| ADHD | |||||
| Boys | .74 | .30 | .74 (.62, .78) | .00 (.00, .11) | .26 (.22, .31) |
| Girls | .71 | .26 | .73 (.65, .77) | .00 (.00, .06) | .27 (.23, .32) |
| Total | .72 | .28 | .73 (.68, .76) | .00 (.00, .05) | .27 (.24, .30) |
| Conduct Disorder | |||||
| Boys | .84 | .56 | .52 (.37, .70) | .32 (.13, .46) | .16 (.14, .20) |
| Girls | .72 | .48 | .50 (.33, .70) | .22 (.03, .38) | .28 (.24, .33) |
| Total | .81 | .54 | .51 (.39, .63) | .30 (.18, .41) | .19 (.17, .22) |
| Oppositional | |||||
| Defiant Disorder | |||||
| Boys | .78 | .39 | .78 (.58, .81) | .00 (.00, .19) | .22 (.19, .26) |
| Girls | .74 | .43 | .65 (.46, .78) | .09 (.00, .27) | .26 (.22, .30) |
| Total | .76 | .40 | .73 (.59, .79) | .04 (.00, .17) | .24 (.21, .26) |
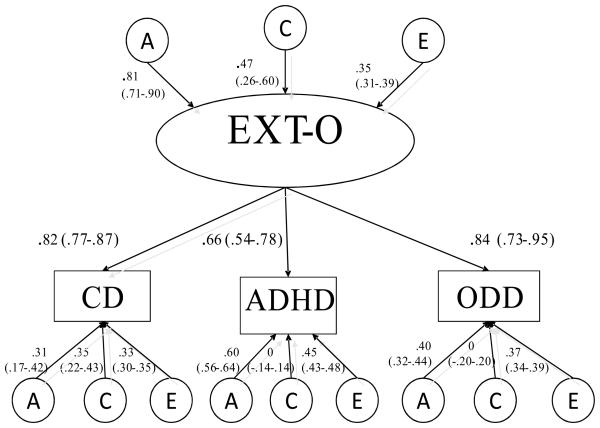
Finally, we examined the generality and specificity of the genetic and environmental effects on the three childhood disruptive disorders by fitting a biometric factor model (see Figure 2 for a visual representation). The general EXT-O factor was primarily influenced by genetic factors (a2 = .65; 95% CI, .51-.81), but also exhibited a notable shared environmental component (c2 = .23; 95% CI, .07-.36) with the remaining variance due to non-shared environmental effects (e2 = .12; 95% CI, .10-.15). This indicates largely common genetic factors underlying the comorbidity among the childhood disruptive disorders. We also detected several specific ACE effects on the individual disorders. For each disorder, we detected specific genetic effects. These effects were large for ADHD (a2 = .36; 95% CI, .31-.41), moderate for oppositional defiant disorder (a2 = .16; 95% CI, .10-.19), and modest for conduct disorder (a2 = .10; 95% CI, .03-.18). Only conduct disorder exhibited a strong shared environmental effect (c2 = .12; 95% CI, .05-.18). Last, all three disorders exhibited moderate specific non-shared environmental effects [ADHD, e2 =.20 (95% CI, .18-.23); oppositional defiant disorder, e2 = .14 (95% CI, .12-.15); conduct disorder, e2 = .11 (95% CI, .09-.12)].
Figure 2. ACE Model for Childhood Disruptive Disorders.
Note: Path coefficients and factor loadings are standardized and 95% confidence intervals are presented in parentheses beneath each coefficient. All coefficients whose CI does not include zero are significant. The percentage of variance accounted for by a given variable in another variable can be determined by squaring the path coefficient on the path connecting the first with the second variable. The sum of all the squared loadings (effects from the general EXT factor as well as the specific ACE loadings) equals 1. The total effect can be calculated by summing the general effect (squared factor loading for a given disorder multiplied by the squared A, C, or E path coefficient on EXT) and the specific effect (squared A, C, or E specific effect on a given disorder). Using CD as an example, h2 = general [(.81)2 × (.82)2] + specific [(.31)2] = .54. A = additive genetic effects; C = shared environmental effects; E = nonshared environmental effects; ADHD = Attention deficit/hyperactivity disorder; CD = conduct disorder; ODD = oppositional defiant disorder; EXT-O = Externalizing factor for offspring.
Discussion
We examined whether the link between parental substance use disorders and antisocial behavior and childhood disruptive disorders in their offspring is due to the transmission of a general liability to multiple disorders or disorder-specific liabilities. Consistent with previous findings for the transmission of adult externalizing disorders in late adolescence (13), the present results indicated that a general transmission factor, EXT, accounted for the co-occurrence of adult externalizing disorders in parents and childhood disruptive disorders in their offspring. In other words, parents pass on a general liability to externalizing psychopathology that is then manifested in their offspring in form of attention problems, hyperactivity, oppositionality, and conduct problems. We also detected disorder-specific effects that were present across siblings rather than transmitted from parents to their children. Together, these results provide a conceptual model for the transmission of EXT from parents to their offspring that accounts for the link between adult and child externalizing psychopathology.
We also estimated the genetic and environmental contribution to variations in both the general and specific liabilities to childhood disruptive disorders. The general EXT-O liability was highly heritable indicating that common genetic risk factors predominately account for the comorbidity among childhood disruptive disorders. However, EXT-O also exhibited a moderate shared environmental effect indicating that certain environmental influences that increase twin similarity also account for the co-occurrence among childhood disruptive disorders. Thus, our results are consistent both with previous work with adolescent and adult samples that have implicated a highly heritable EXT factor (15, 34, 35), as well as with studies (and a recent meta-analysis) utilizing samples of children and reporting a strong influence of shared environmental effects (26) (36).
One notable finding concerns the large specific genetic effect on ADHD, suggesting that there are substantial genetic factors contributing to the variation in this disorder that are independent of the general liability to EXT-O. This effect is not unique, as similar findings have been reported previously (37). This effect likely stems from the content differences between ADHD versus conduct disorder and oppositional defiant disorder. In particular, the latter disorders involve explicit violation of norms or rules, the rights others, and disobeying authority. ADHD on the other hand does not involve the violation of others' rights; rather, much of the content focuses on the child being difficult to manage and instruct. In this way, the content differences between the disorders might account for the specific genetic effect in ADHD.
Another notable finding was that shared environment influenced conduct disorder alone. The robust shared environmental influence on conduct disorder has been reported previously (21, 38). Shared environmental influences on antisocial behavior, however, seem to decline with age such that antisocial behavior in late adolescence and adulthood is influenced mainly by genetic factors (39, 40). Our results thus revive the importance of examining shared environmental variables as processes underlying the comorbidity among childhood disruptive disorders.
Some limitations of the current study should be noted. First, the cross-sectional nature of the study precludes any inferences regarding generalizability of these findings at different ages. Second, the current study utilized a homogenous sample of Caucasian families. Third, although there was evidence for a correlation between paternal and maternal EXT, there was no way of determining whether this correlation reflected a tendency of like to mate with like (assortative mating), or the tendency for spouses to get more similar with time. Fourth, although less of a limitation than a future direction, the current study did not examine the exact nature of the environmental influences on EXT such as socioeconomic status or neighborhood disruption which could also have moderated the genetic effects on EXT. The identification of the role of environmental factors may add precision to future work. Finally, we utilized a standard additive ACE model to estimate the effects of genes and environment. However, recent work focused on the genetics of externalizing behavior suggests the presence of gene x environment (GxE) interactions as well. Future models following this work will benefit from testing this model with and without the presence of GxE interaction effects.
To conclude, our results provide important insights into the familial aggregation of externalizing disorders. Specifically, they indicate that a focus of research should be to identify the common risk factors across disorders as this general liability accounts for the link between substance use disorders and antisocial behavior in parents and childhood disruptive disorders in their offspring. The knowledge of the general transmission effect and support for a common liability for childhood disruptive disorders might be of interest to clinicians as well. In particular, these results suggest that these common – more so than specific effects - should be the targets of prevention and intervention efforts.
The current results also provide insights regarding how genetic and environmental factors can change as function of developmental context. Although genetic factors are large and present throughout development, shared environmental factors are major contributors to the variation in the co-occurrence of externalizing behaviors in childhood (36), whereas in late adolescence and adulthood this is not necessarily true. A potential mechanism for this shift may be a transition from passive gene-environment (G-E) correlation processes in childhood to evocative and active G-E correlation processes in adolescence and adulthood. Further research that integrates the current findings within a developmental context with a focus on delineating these mechanisms of G-E interplay will yield insights into the etiology of disruptive disorders. Such knowledge can inform intervention strategies to help alleviate the stress experienced by individuals and families.
Supplementary Material
Acknowledgments
This work was supported by National Institute of Health Grants DA 05147, DA 13240, and DA 024417, AA 09367, and MH017069. All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Knopik VS, Heath AC, Jacob T, Slutske WS, Bucholz KK, Madden PAF, Waldron M, Martin NG. Maternal alcohol use disorder and offspring ADHD: disentangling genetic and environmental effects using a children-of-twins design. Psychol Med. 2006;36:1461–71. doi: 10.1017/S0033291706007884. [DOI] [PubMed] [Google Scholar]
- 2.Lahey BB, Piacentini JC, McBurnett K, Stone P, Hartdagen S, Hynd G. Psychopathology in the parents of children with conduct disorder and hyperactivity. J Am Acad Child Adolesc Psychiatr. 1988;27:163–70. doi: 10.1097/00004583-198803000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Malone SM, Iacono WG, McGue M. Drinks of the father: Father's maximum number of drinks consumed predicts externalizing disorders, substance use, and substance use disorders in preadolescent and adolescent offspring. Alcoholism. 2002;26:1823–32. doi: 10.1097/01.ALC.0000042222.59908.F9. [DOI] [PubMed] [Google Scholar]
- 4.Herndon RW, Iacono WG. The familial transmission of antisocial behavior from parent to child. Psychol Med. 2005;35:1815–24. doi: 10.1017/S0033291705005635. [DOI] [PubMed] [Google Scholar]
- 5.Jacob T, Waterman B, Heath A, True W, Bucholz KK, Haber R, Scherrer J, Fu Q. Genetic and environmental effects on offspring alcoholism - New insights using an offspring-of-twins design. Arch Gen Psychiatry. 2003;60:1265–72. doi: 10.1001/archpsyc.60.12.1265. [DOI] [PubMed] [Google Scholar]
- 6.Marmorstein NR, Iacono WG, McGue M. Alcohol versus drug dependence among parents: Associations with offspring externalizing disorders. Psychological Medicine In Press. doi: 10.1017/S0033291708003085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cadoret RJ, Troughton E, Ogorman TW. Genetic and environmental factors in alcohol abuse and antisocial personality. J Stud Alcohol. 1987;48:1–8. doi: 10.15288/jsa.1987.48.1. [DOI] [PubMed] [Google Scholar]
- 8.Cadoret RJ, Yates WR, Troughton E, Woodworth G, Stewart MA. Adoption study demonstrating 2 genetic pathways to drug abuse. Arch Gen Psychiatry. 1995;52:42–52. doi: 10.1001/archpsyc.1995.03950130042005. [DOI] [PubMed] [Google Scholar]
- 9.Chronis AM, Lahey BB, Pelham WE, Kipp HL, Baumann BL, Lee SS. Psychopathology and substance abuse in parents of young children with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatr. 2003;42:1424–32. doi: 10.1097/00004583-200312000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Merikangas KR, Dierker LC, Szatmari P. Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: A high-risk study. J Child Psychol Psychiatry. 1998;39:711–20. [PubMed] [Google Scholar]
- 11.Vanyukov MM, Kirisci L, Moss L, Tarter RE, Reynolds MD, Maher BS, Kirillova GP, Ridenour T, Clark DB. Measurement of the Risk for Substance Use Disorders: Phenotypic and Genetic Analysis of an Index of Common Liability. Behav Genet. 2009;39:596–610. doi: 10.1007/s10519-009-9269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hicks BM, Blonigen DM, Kramer MD, Krueger RF, Patrick CJ, Iacono WG, McGue M. Gender differences and developmental change in externalizing disorders from late adolescence to early adulthood: A longitudinal twin study. J Abnorm Psychol. 2007;116:433–47. doi: 10.1037/0021-843X.116.3.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: A twin-family study. Arch Gen Psychiatry. 2004;61:922–8. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- 14.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 15.Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–24. [PubMed] [Google Scholar]
- 16.Krueger RE, Markon KE. Reinterpreting comorbidity: A model-based approach to understanding and classifying psychopathology. Annu Rev Clin Psychol. 2006;2:111–33. doi: 10.1146/annurev.clinpsy.2.022305.095213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders: A longitudinal-epidemiological study. J Abnorm Psychol. 1998;107:216–27. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- 18.Krueger RF, Caspi A, Moffitt TE, Silva PA, McGee R. Personality traits are differentially linked to mental disorders: A multitrait-multidiagnosis study of an adolescent birth cohort. J Abnorm Psychol. 1996;105:299–312. doi: 10.1037//0021-843x.105.3.299. [DOI] [PubMed] [Google Scholar]
- 19.Burt SA, Krueger RF, McGue M, Iacono W. Parent-child conflict and the comorbidity among childhood externalizing disorders. Arch Gen Psychiatry. 2003;60:505–13. doi: 10.1001/archpsyc.60.5.505. [DOI] [PubMed] [Google Scholar]
- 20.Dick DM, Viken RJ, Kaprio J, Pulkkinen L, Rose RJ. Understanding the covariation among childhood externalizing symptoms: Genetic and environmental influences on conduct disorder, attention deficit hyperactivity disorder, and oppositional defiant disorder symptoms. J Abnorm Child Psychol. 2005;33:219–29. doi: 10.1007/s10802-005-1829-8. [DOI] [PubMed] [Google Scholar]
- 21.Eaves LJ, Silberg JL, Meyer JM, Maes HH, Simonoff E, Pickles A, Rutter M, Neale MC, Reynolds CA, Erikson MT, Heath AC, Loeber R, Truett KR, Hewitt JK. Genetics and developmental psychopathology 2: The main effects of genes and environment on behavioral problems in the Virginia twin study of adolescent behavioral development. J Child Psychol Psychiatry Allied Discip. 1997;38:965–80. doi: 10.1111/j.1469-7610.1997.tb01614.x. [DOI] [PubMed] [Google Scholar]
- 22.Wood AC, Rijsdijk F, Asherson P, Kuntsi J. Hyperactive-Impulsive Symptom Scores and Oppositional Behaviours Reflect Alternate Manifestations of a Single Liability. Behav Genet. 2009;39:447–60. doi: 10.1007/s10519-009-9290-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Robins LN, Baber T, Cottler LB. International Diagnostic Interview: Expanded Substance Abuse module. St. Louis, MO: 1987. [Google Scholar]
- 24.First MB, Spitzer RL, Gibbon M, Williams JB, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) American Psychiatric Press; Washington, DC: 1997. [Google Scholar]
- 25.Reich W, Weiner Z. Revised version of the Diagnostic Interview for Children and Adolescents (DICA-R) Department of Psychiatry, Washington University School of Medicine; St. Louis, MO: 1988. [Google Scholar]
- 26.Burt SA, McGue M, Krueger RF, Iacono WG. Sources of covariation among the child-externalizing disorders: informant effects and the shared environment. Psychol Med. 2005;35:1133–44. doi: 10.1017/S0033291705004770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neale MC. Mx: Statistical modeling. 3rd ed. Richmond: 1997. [Google Scholar]
- 28.Muthén LKM, Muthén BO. Mplus User's Guide. 5th ed Muthén & Muthén; 1998-2007. [Google Scholar]
- 29.Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye ACC, editor. Latent Variable Analysis: Applications to Developmental Research. Sage; Newbury Park, CA: 1994. [Google Scholar]
- 30.Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:461–4. [Google Scholar]
- 31.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage; Newbery Park, CA: 1993. [Google Scholar]
- 32.Raftery AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–63. [Google Scholar]
- 33.Plomin R, DeFries J, McClearn G, Rutter M. Behavioral Genetics. WH Freeman; New York: 1997. [Google Scholar]
- 34.Slutske WS, Heath AC, Dinwiddie SH, Madden PAF, Bucholz KK, Dunne MP, Statham DJ, Martin NG. Common genetic risk factors for conduct disorder and alcohol dependence. J Abnorm Psych. 1998;107:363–374. doi: 10.1037//0021-843x.107.3.363. [DOI] [PubMed] [Google Scholar]
- 35.Young SE, Stallings MC, Corley RP, Krauter KS, Hewitt JK. Genetic and environmental influences on behavioral disinhibition. Am J Med Genet. 2000;96:684–95. [PubMed] [Google Scholar]
- 36.Burt SA. Rethinking Environmental Contributions to Child and Adolescent Psychopathology: A Meta-Analysis of Shared Environmental Influences. Psychol Bull. 2009;135:608–37. doi: 10.1037/a0015702. [DOI] [PubMed] [Google Scholar]
- 37.Nadder TS, Rutter M, Silberg JL, Maes HH, Eaves LJ. Genetic effects on the variation and covariation of attention deficit-hyperactivity disorder (ADHD) and oppositional defiant disorder/conduct disorder (ODD/CD) symptomatologies across informant and occasion of measurement. Psychol Med. 2002;32:39–53. doi: 10.1017/s0033291701004792. [DOI] [PubMed] [Google Scholar]
- 38.Meyer JM, Rutter M, Silberg JL, Maes HH, Simonoff E, Shillady LL, Pickles A, Hewitt JK, Eaves LJ. Familial aggregation for conduct disorder symptomatology: The role of genes, marital discord and family adaptability. Psychol Med. 2000;30:759–74. doi: 10.1017/s0033291799002408. [DOI] [PubMed] [Google Scholar]
- 39.Bergen SE, Gardner CO, Kendler KS. Age-related changes in heritability of behavioral phenotypes over adolescence and young adulthood: A meta-analysis. Twin Res Hum Genet. 2007;10:423–33. doi: 10.1375/twin.10.3.423. [DOI] [PubMed] [Google Scholar]
- 40.Lyons MJ. Epidemiology of personality disorders. In: Tsuang MT, Tohen M, Zahner GP, editors. Textbook in Psychiatric Epidemiology. Wiley-Liss; New York: 1995. pp. 407–36. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.