Abstract
Objective
Insomnia has been linked to suicidal ideas and suicide death in cross-sectional and longitudinal population-based studies. A link between insomnia and suicide has not been previously examined in the setting of a clinical trial. Herein we describe the relationship between insomnia and suicidal thinking during the course of a clinical trial for depression with insomnia.
Methods
Sixty patients aged 41.5 ± 12.5 years (2/3 women) with major depressive episode and symptoms of insomnia received open label fluoxetine for 9 weeks and also received blinded, randomized eszopiclone 3 mg or placebo at bedtime after the first week of fluoxetine. Insomnia symptoms were assessed with the Insomnia Severity Index (ISI), and suicidal ideation was assessed with The Scale for Suicide Ideation (SSI). Depression symptoms were assessed with the depressed mood item and the anhedonia item from the Hamilton Rating Scale for Depression-24 (HRSD24), as well as a sum score for all non-sleep and non-suicide items from the HRSD (HRSD20). Measurements were taken at baseline and weeks 1, 2, 4, 6, and 8. SSI was examined by generalized linear mixed models for repeated measures as the outcome of interest for all 60 participants with ISI and various mood symptoms as independent variables, with adjustment for age, gender, treatment assignment, and baseline SSI.
Results
Higher levels of insomnia corresponded to significantly greater intensity of suicidal thinking (p<0.01). The depressed mood item of the HRSD, and the sum of the HRSD20, both corresponded to greater suicidal thinking (p<0.001). The anhedonia item did not correspond with suicidal thinking. When both ISI and the depressed mood item, or ISI and the anhedonia item, were included together in the same model, the ISI remained an independent predictor of suicidal thinking.
Conclusions
The results support the concept that insomnia may be a useful indicator for suicidal ideation, and now extend this idea into clinical trials. Insomnia remains an independent indicator of suicidal ideation even taking into account the core symptoms of depression such as depressed mood and anhedonia. The complaint of insomnia during a depression clinical trial might indicate that more direct questioning about suicide is warranted.
Keywords: insomnia, suicide, depression, clinical trial, eszopiclone, placebo
INTRODUCTION
Suicide is a leading cause of death across all ages and occurs at a rate of 10–11 cases per 100,000 persons per year in the Unites States.1 It is the third leading cause of death in those less than 30 years of age.1 The majority of suicides occur in the context of an active psychiatric disorder. Major depressive episode (MDE), often with concurrent substance abuse, is the psychiatric disorder most commonly associated with suicide.1
The risk factors for suicide have been described, and include both unmodifiable and some potentially modifiable factors.2–4 Examples of unmodifiable factors are advancing age, male gender, and Caucasian ethnicity, while examples of potentially modifiable risk factors include active symptoms of depression, hopelessness, social isolation, active alcohol/substance use, and severe sleep disturbance. As a predictor, insomnia is stronger than a specific suicide plan in predicting near-lethal suicide attempts,5 yet insomnia is often overlooked in review papers of risk factors for suicide, and suicide prevention.6 The need for broadening the search for modifiable risk factors is epitomized by this statement from a recent review of suicide prevention research: “nowhere is the lack of proven therapeutic methods greater than in the prevention of suicidal behavior.”7
At least 25 original research papers have linked sleep disturbance to either suicidal ideation or completed suicide, including 10 studies in children and adolescents.8–17 There are 15 studies in young adults and the elderly, and these are summarized in Table 1. Furthermore, these studies spanned the United States, England, France, Canada, Turkey, Finland, Sweden, Brazil, China, and Japan. While most of the studies were cross-sectional and/or focused on suicidal ideation, 4 of the 25 studies prospectively evaluated the association between sleep disturbance and suicide death 18–21 and reported statistically significant relative risk of suicide death up to 2.4.20 Insomnia was the most common sleep disturbance associated with suicide, but nightmares also conferred risk. These associations generally remained even after adjusting for severity of depression.
Table 1.
Relationship between Sleep and Suicide in Adults
| Author/year | Source of sample | Design and N= | Sleep Disturbance | Specified Outcome |
|---|---|---|---|---|
| Barraclough 197536 | Suicides vs. Depressed Outpatients | Cross-sectional N=192 | Insomnia | Suicide Death |
| Agargun 199737 | Depressed patients | Cross-sectional N=41 | Insomnia | Suicidal Thoughts |
| Agargun 199738 | Depressed patients | Cross-sectional N=113 | Insomnia | Suicidal Thoughts |
| Agargun 199839 | Depressed patients | Cross-sectional N=63 | Nightmares | Suicidal Thoughts |
| Smith 200440 | Chronic pain | Cross-sectional N=51 | Insomnia | Suicidal Thoughts |
| Bernert 200541 | Psychiatric outpatients | Cross-sectional N=176 | Insomnia and Nightmares | Suicidal Thoughts |
| Chellappa 200742 | Depressed Outpatients | Cross-sectional N=70 | Insomnia | Suicidal Thoughts |
| Bernert 200943 | Depressed Outpatients | Cross-sectional N=82 | Insomnia and Nightmares | Suicidal Thoughts |
| Agargun 200744 | Depressed Inpatients | Cross-sectional N=149 | Insomnia and Nightmares | Prior Suicide Attempt |
| Sjostrom 200745 | Suicide attempters | Cross-sectional N=165 | Insomnia and Nightmares | Prior Suicide Attempt |
| Goodwin 200846 | Population Survey | Cross-sectional N=8098 | Short Sleep | Suicidal Thoughts and Attempts |
| Fawcett 199018 | Depressed patients | Prospective N=954 | Insomnia | Suicide Death |
| Tanskanen 200119 | Population Survey | Prospective N=36,211 | Nightmares | Suicide Death |
| Fujino 200520 | Population Survey | Prospective N=15,597 | Insomnia | Suicide Death |
| Turvey 200221 | Population Survey | Prospective N=14,456 | Insomnia | Suicide Death |
We are unaware of any studies examining whether the relationship between insomnia and suicide risk also holds true in the setting of clinical trials. If insomnia remains an indicator of suicidal ideation in depression clinical trials, then treatment of insomnia may be an option in reducing suicide risk in a clinical trial. Here we report on the relationship between insomnia and suicidal thinking in a randomized, clinical trial comparing eszopiclone (ESZ) and placebo at bedtime as an add-on treatment to open-label fluoxetine (FLX) in a sample of adult, depressed insomniacs.
METHODS
Overview
Sixty patients with MDE and insomnia symptoms underwent a week of prospective baseline data collection, followed by one week of open-label FLX monotherapy, starting at 20 mg in the morning. Patients who were still experiencing insomnia after one week of FLX then continued with 8 more weeks of open label FLX, and were randomly assigned to either double-blind ESZ 3 mg or placebo at bedtime. Patients who still had a 24-item Hamilton Rating Scale for Depression 22 (HRSD24)>15 at the end of 4 weeks of randomized treatment had the option to have FLX doubled to 40 mg for the next 4 weeks. Health-Related Quality of Life (HRQOL) measurements formed the a priori primary endpoints for the randomized trial, while self-reported sleep measurement, objective sleep measurements, and mood were secondary endpoints. HRQOL, mood, and sleep variables are reported in detail in another report, and specifically polysomnography (PSG) and actigraphy will not be considered in this report. Suicidal thinking was stipulated a priori as an exploratory variable, and the present report describes suicidal thinking during the course of the clinical trial.
Participants
Participants were aged 18–70 y.o., with either (a) sleep latency > 30 minutes and sleep efficiency < 85% at least 4 nights per week, or (b) met Research Diagnostic Criteria (RDC) insomnia criteria for at least 4 nights per week. 23 The project was approved by the local IRB, and all participants provided written, informed consent.
All participants met a DSM-IV diagnosis of unipolar MDE per Structured Clinical Interview for DSM-IV (SCID), 24 with a Mini Mental State Exam (MMSE) score >24, 25 and a HRSD24 score ≥ 20. 22 All participants who were retained for randomized treatment completed one-night of baseline PSG which showed no clinically significant sleep apnea (Apnea/Hypopneas index >15) or Periodic Limb Movement Disorder (PLM arousal index >15), following standard measurement procedures described elsewhere. 26
Measurement of Suicidal Ideation
The Scale for Suicide ideation (SSI) is a well validated instrument consisting of 19 items that evaluate three dimensions of suicide ideation: active suicidal desire, specific plans for suicide, and passive suicidal desire.27–29 Each item is rated on a 3-point scale from 0 to 2 for a maximum score of 38 with a lower score indicating less severe suicidal ideation. The SSI is clinician-rated and is presented in a semi-structured interview format. The SSI was collected at baseline and at weeks 1, 2, 4, 6, and 8 of randomization. Other investigators have found that a SSI score ≥ 3 predicts eventual suicide death over a time period of years.4
Measurement of Insomnia
The participants completed the Insomnia Severity Index (ISI) at the first visit and every subsequent visit.30 The ISI is a 7-item questionnaire, with each item scored 0–4, for a maximum of 28 points. Items are scaled according to the degree of dissatisfaction with sleep, in contrast to a sleep diary which measures the dimension of time spent awake or asleep. Higher scores on the ISI represent greater degrees of insomnia. The ISI was collected at baseline and at weeks 1, 2, 4, 6, and 8 of randomization.
Measurement of Depression
Depression severity was tracked by the observer-rated 24-item HRSD. 22;31 The HRSD was administered by same clinical rater, blind to treatment assignment, at baseline and thereafter at weeks 1, 2, 4, 6, and 8 of randomization. Research staff had demonstrated inter-rater reliability > 0.85 against a criterion-set of clinical videotapes. The HRSD has three sleep items and one suicide item. The HRSD was recorded as the total score (HRSD24), but was analyzed in this report without the three sleep items or the suicide item (HRSD20). We also examined the two ‘core’ symptoms of depression (the depressed mood item and the anhedonia item) as predictors of suicidal thinking.
Data Management and Analytic Plan
The goal of the statistical analysis was to model predictors of suicidal ideation over time (SSI scores) during the period of randomization. Descriptive statistics were calculated for demographic variables. All analyses employed generalized linear mixed models for repeated measures (Proc Mixed) with predictor variables being insomnia (ISI scores) and depressive symptoms (HRSD20, the depressed mood item, and the anhedonia item). Fixed effects in all models were time, age, gender, treatment assignment and pre-randomization SSI scores while study participants were treated as random effects. Dummy variables were created for gender and treatment assignment and an unstructured covariance structure was utilized since it had the smallest Akaike’s Information Criterion ([AIC] a measure of the fit of a particular covariance structure). Models were first created with ISI as the time-varying independent variable; then the depressed mood item, the anhedonia item, and the sum of the HRSD20 were separately evaluated as time varying predictors. Each of these separate models was then expanded to include ISI with a different mood variable. In each instance an interaction term (fixed effect) was included for either ISI*mood variable, and if the interactions were non-significant, then interaction terms were removed and the model was re-run excluding the interaction term. SAS Version 9.2 was employed for all analyses and statistical significance was accepted for p<0.05. All tests were two-tailed.
RESULTS
Sixty participants were randomized, and 51 of these completed the final assessment during randomization. The average age of the randomized sample was 41.5 ± 12.5, and women constituted exactly two-thirds of the sample, with 23.2% minorities. Sixty-five percent met criteria for melancholia, 53% met criteria for a lifetime history of an anxiety disorder, and 37% met criteria for prior substance dependence or abuse. Overall depression severity was moderate to severe at baseline as reflected in an average HRSD24 score of 27.1 ± 3.9, while the HRSD minus the insomnia and suicide items (HRSD20) was 17.7 ± 4.7 at the visit just prior to randomization. Baseline insomnia severity was in the moderate to severe range with an average ISI score of 20.7 ± 4.0.
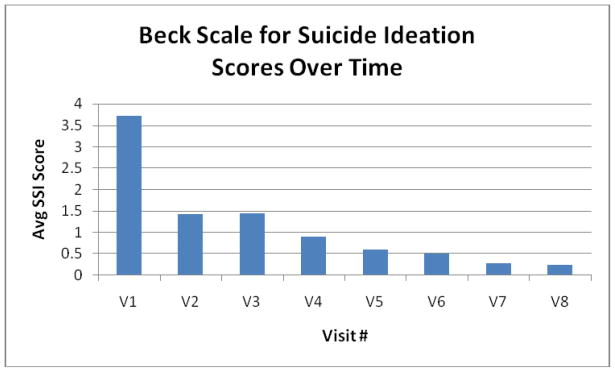
Baseline suicidality was mild with average SSI scores of 3.7 ± 5.2, with 37% of patients having SSI score ≥ 3 at initial baseline. SSI scores dropped rapidly thereafter (Figure 1).
Figure 1.
V1: Visit 1 - the first face to face baseline visit
V2: Visit 2 - the end of one week of medication-free prospective baseline assessment
V3: Visit 3 – the end of one week of open-label fluoxetine 20 mg
V4: Visit 4 – the end of the first week of eszopiclone (ESZ) or placebo added to fluoxetine
V5: Visit 5 – the end of the second week of ESZ/placebo added to fluoxetine
V6: Visit 6 – the end of the fourth week of ESZ/placebo added to fluoxetine
V7: Visit 7 – the end of the sixth week of ESZ/placebo added to fluoxetine
V8: Visit 8 – the end of the eighth week of ESZ/placebo added to fluoxetine
In intent to treat analysis, the model with ISI as the predictor was significant, indicating that greater severity of insomnia corresponded to greater intensity of suicidal thinking (Table 2). The beta weight for the model indicated that a categorical change in insomnia severity (i.e., a change from mild to moderate insomnia) would produce a 0.4 increase in the SSI score. Increasing scores for the depressed mood item from the HRSD or the sum of the HRSD20 were associated with greater suicidal thinking in separate univariate regressions (Tables 2 and 3). The anhedonia item was not associated with suicidal thinking (Table 3). When ISI was combined with either the depressed mood item or the anhedonia item, then increasing ISI remained an independent predictor of increasing suicidal thinking. When ISI was combined with the sum of HRSD20, ISI no longer was an independent indicator of suicidal thinking. Finally, we wanted to evaluate whether these findings would be consistent with the sub-sample of completers of the trial so we used the same modeling structures and compared the results, finding results similar to our main analysis.
Table 2.
Insomnia and HRSD20 as Predictors of Suicidal Ideation
| ISI only model (ISI* Time Interaction removed) | HRSD20 only model | ISI and HRSD20 model | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | β | SE | p-value | β | SE | p-value | β | SE | p-value |
| Insomnia (ISI) | 0.055 | 0.021 | 0.0089 | 0.014 | 0.030 | 0.6331 | |||
| HRSD20 | 0.094 | 0.020 | <.0001 | 0.093 | 0.022 | <.0001 | |||
| time | −0.003 | 0.004 | 0.5224 | 0.014 | 0.008 | 0.0945 | 0.013 | 0.008 | 0.1438 |
| ISI* time Interaction | 0.0005 | 0.0008 | 0.5390 | ||||||
| HRSD20* time Interaction | −0.001 | 0.0006 | 0.0402 | −0.002 | 0.0007 | 0.0330 | |||
| Baseline Suicidal Ideation | 0.366 | 0.069 | <.0001 | 0.3692 | 0.067 | <.0001 | 0.361 | 0.067 | <.0001 |
| Treatment | |||||||||
| Drug | −0.335 | 0.520 | 0.5202 | −0.462 | 0.495 | 0.3531 | −0.355 | 0.505 | 0.4835 |
| Placebo* | |||||||||
| Age | −0.004 | 0.021 | 0.8307 | −0.0003 | 0.020 | 0.9884 | −0.003 | 0.020 | 0.8683 |
| Gender | |||||||||
| Female | −0.038 | 0.523 | 0.9419 | −0.015 | 0.508 | 0.9766 | −0.023 | 0.508 | 0.9642 |
| Male* | |||||||||
(N=60)
= reference
Table 3.
Anhedonia, Depressed Mood and Insomnia as Predictors of Suicidal Ideation
| Anhedonia only model | Anhedonia & Insomnia model | Depressed Mood only model | Depressed Mood & Insomnia model | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | β | SE | p-value | β | SE | p-value | β | SE | p-value | β | SE | p-value |
| Anhedonia Score | 0.8738 (df=3) | 0.7684 (df=3) | ||||||||||
| 0 | 0.149 | 0.244 | 0.5424 | 0.232 | 0.243 | 0.3429 | ||||||
| 1 | 0.125 | 0.218 | 0.5682 | 0.116 | 0.216 | 0.5921 | ||||||
| 2 | 0.133 | 0.173 | 0.4404 | 0.151 | 0.171 | 0.3775 | ||||||
| 3 or more* | ||||||||||||
| Insomnia (ISI) | 0.057 | 0.0212 | 0.0081 | 0.048 | 0.021 | 0.0233 | ||||||
| Depressed Mood Score | 0.0021 (df=3) | 0.0042 (df=3) | ||||||||||
| 0 | −0.438 | 0.203 | 0.0323 | −0.330 | 0.207 | 0.1134 | ||||||
| 1 | −0.627 | 0.175 | 0.0005 | −0.577 | 0.175 | 0.0013 | ||||||
| 2 | −0.929 | 0.343 | 0.0077 | −0.920 | 0.340 | 0.0077 | ||||||
| 3 or more* | ||||||||||||
| Time | −0.639 | 0.520 | 0.2212 | −0.004 | 0.021 | 0.4006 | −0.005 | 0.005 | 0.2688 | −0.003 | 0.005 | 0.5623 |
| Baseline Suicidal Ideation | 0.407 | 0.070 | <.0001 | 0.3692 | 0.067 | <.0001 | 0.330 | 0.068 | <.0001 | 0.293 | 0.067 | <.0001 |
| Treatment | ||||||||||||
| Drug | −0.335 | 0.520 | 0.5202 | −0.353 | 0.520 | 0.4985 | −0.560 | 0.484 | 0.2493 | −0.304 | 0.481 | 0.5287 |
| Placebo* | ||||||||||||
| Age | 0.007 | 0.021 | 0.7341 | −0.003 | 0.021 | 0.8958 | −0.0006 | 0.020 | 0.9777 | −0.010 | 0.019 | 0.5972 |
| Gender | ||||||||||||
| Female | 0.011 | 0.534 | 0.9839 | −0.045 | 0.523 | 0.9317 | −0.013 | 0.497 | 0.7914 | −0.138 | 0.482 | 0.7753 |
| Male* | ||||||||||||
(N=60)
= reference
DISCUSSION
This study found that insomnia is an indicator of suicidal thinking during a clinical trial of hypnotic medications combined with SSRI therapy in depressed insomniacs. As such it confirms prior reports of a link between insomnia and suicidal ideation, now extended to the clinical trial setting. Insomnia severity remained an independent indicator of suicidal thinking, even when combined with either the severity of depressed mood item or anhedonia item as independent variables. The combined effect of 20 non-insomnia depressive symptoms (HRSD20) was a more potent predictor than the ISI insomnia score in predicting suicidal thinking in the sense that when both insomnia and HRSD20 were considered in the same model only HRSD20 remained a significant predictor of suicidal ideation. This is not surprising given the large amount of variance likely to be captured in the sum of 20 items from the HRSD20. Applied to the clinical situation where the severity of depression is more often assessed by gestalt rather than by rating scale, we suggest that the high or increasing severity of insomnia symptoms in a depressed patient warrants investigation of the presence of suicidal thinking.
Strategies for prevention interventions for suicidal ideation and attempts are poorly developed,7 Promising avenues of suicide prevention might include heightened awareness on the part of “gatekeepers” (clergy, pharmacists, teachers, etc.), physician education aimed at early detection, and restriction of access to lethal means.6;17 Suicide might be reduced with CBT, interpersonal psychotherapy, and dialectic behavior therapy. A limited number of somatic therapies have strong evidence for a specific anti-suicide effect in mood disorders, including lithium and ECT.32;33 Notably, both lithium and ECT have favorable effects on sleep,34;35 but to our knowledge a specific mechanism for lithium or ECT reducing suicide by improving sleep has not been proposed or tested. Expert reviews of suicide risk factors and suicide prevention have generally overlooked insomnia.3;6
The candidacy of insomnia treatment as a strategy for suicide prevention is buttressed by the large number of observational studies showing links between insomnia and/or nightmares and suicidal thinking or behavior.8–21;36–46 But these other studies were limited in that each was either a prospective study of non-clinical populations or a cross sectional study.
Why is insomnia linked to suicide in depressed patients? Serotonin has been identified as a key candidate CNS neurotransmitter for both the initiation of sleep and the risk of impulsive or violent behaviors,47;48 with decreased CNS serotonergic functioning linked to both insomnia and suicide. In this conceptualization, insomnia does not necessarily lead to suicide, but instead is a marker of reduced serotonergic function. Further evidence of a specific biological link between sleep and suicide is found in reports of an association between short REM sleep latency, increased REM activity, and suicidal thinking.49;50 Apart from serotonergic-biological explanations, the insomnia-suicide link could be viewed within the framework of hopelessness-suicide. Hopelessness is common in MDE and is itself a potentially modifiable risk factor for suicide.3 Interestingly, hopelessness is a key dysfunctional cognition that may perpetuate chronic insomnia, and hopelessness is reflected in the content of the Dysfunctional Beliefs and Attitudes about Sleep Scale, which includes items such as “When I sleep poorly one night, I know it will disturb my sleep schedule for the whole week”.51 These same dysfunctional beliefs regarding the hopelessness of sleep have been identified in depressed insomniacs.52 Finally, some authors have suggested that insomnia is a marker of severe inter-personal disruption and that interpersonal disruption is the proximal factor to suicide.13
Prior to the introduction of the first selective serotonin reuptake inhibitor (SSRI) in the United States in 1987, tricyclic antidepressants (TCAs) were first line somatic treatment of MDE, and TCA therapy could be counted on to produce reliable, early improvement in the sleep of persons with insomnia and MDE, as compared to the relative lack of effect of psychodynamic psychotherapy on insomnia.53 In comparison, the subsequent ascendancy of SSRIs was followed by the realization that (1) SSRIs did not produce immediate improvement in insomnia complaints, (2) up to 40% of otherwise successfully treated MDE patients continued to have insomnia,54 and (3) up to 10% actually experienced an induction or aggravation of insomnia.55 As a result, in some settings the majority of patients taking newer antidepressants also receive a medication to help them sleep.56
Some benzodiazepines (BZ) are approved for short-term treatment of insomnia, but the BZ that has been best studied in the treatment of MDE-associated insomnia is clonazepam, which is not FDA approved for insomnia. The 2 randomized, placebo controlled trials of clonazepam as an add-on hypnotic in MDE-insomnia demonstrated that clonazepam was superior in relieving insomnia for three weeks but not beyond and did not impact any depression symptoms beyond insomnia, and suicidal ideation was not specifically examined.57;58 The non-benzodiazepine benzodiazepine receptor agonist (NBBRA) zolpidem has been shown to have short-term beneficial effects on reported sleep in MDE patients on SSRIs, but it was not evaluated for any impact on suicidal thinking.59 Another recently completed study comparing placebo versus ESZ as add-on therapy to open-label FLX, showing superior overall antidepressant response and remission rates in those receiving ESZ.60 Unfortunately, no conclusions could be drawn regarding any potential impact of ESZ upon suicidal ideation, as significant suicidal ideation was an exclusion criterion for this study, and the suicide item scores from the HRSD were not different in the hypnotic and placebo groups at the end of treatment.61
Any enthusiasm for prescribing a hypnotic medication for MDE with insomnia is tempered by the knowledge that intentional overdose is among the most common methods of suicide death.3 Observational studies have reported that the rate of suicidal ideation is higher, not lower, in depressed patients who were prescribed sedative/hypnotics (OR=2.3), although this may be explained by selection bias as opposed to treatment exposure.62 Hypnotics are associated with excess mortality in the general population (Hazard Ratio=1.25), although selection bias may explain this finding.63 Cognitive-behavior therapy for insomnia (CBT-I) is an alternative to hypnotic medications for the treatment of insomnia, but again no information exists in studies of depressed insomniacs regarding whether CBT-I impacts suicidal thinking.
The strengths of the present study include the rigorous characterization of diagnoses and symptoms severity and the prospective collection of data pertaining to suicidal ideation. Limitations of this study included the small number of subjects, the short duration of follow up, the lack of measurement of nightmares and hopelessness, and the exclusion of patients who had no insomnia.
Clearly more options are needed for the prevention of suicide risk. Indeed, the expert workshop on suicide prevention concluded that “randomized controlled trials of psychopharmacology are needed in suicide prevention studies.”1 Targeted treatment of insomnia may represent one such avenue, although the use of hypnotic medications presents its own unique hazard. Our study demonstrates that the positive relationship between insomnia and suicidal ideation holds true in the setting of antidepressant clinical trials and opens the door for new clinical trials of insomnia treatment that examine suicidal thinking as the primary end point. At a minimum, prior studies and our new findings point to the relevance of monitoring and treating insomnia in depressed patients and considering insomnia as an indicator of risk for suicidal thinking.
Acknowledgments
NIH MH70821 and M01-RR07122, as well as funding and medications from Sepracor, and funding and material support from Mini Mitter ClinicalTrials.gov Identifier: NCT00247624
This work was supported by NIMH, NIH, Sepracor, and Mini Mitter. Vaughn McCall has received support and been a speaker and consultant for Sepracor, is a consultant for Sealy, Inc, and has had research supported by Sanofi, Corcept, and Somaxon. James Kimball is a speaker for Pfizer and Astra Zeneca.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Mann JJ, Apter A, Bertolote J, et al. Suicide Prevention Strategies: A Systematic Review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 2.Maris R. Suicide. The Lancet. 2002;360:319–326. doi: 10.1016/S0140-6736(02)09556-9. [DOI] [PubMed] [Google Scholar]
- 3.Coryell W, Young EA. Clinical predictors of suicide in primary major depressive disorder. J Clin Psychiatry. 2005;66:412–417. doi: 10.4088/jcp.v66n0401. [DOI] [PubMed] [Google Scholar]
- 4.Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. Journal of Consulting and Clinical Psychology. 2000;68:371–377. [PubMed] [Google Scholar]
- 5.Hall R, Platt D, Hall R. Suicide Risk Assessment: A Review of Risk Factors for Suicide in 100 Patients Who Made Severe Suicide Attempts. Psychosomatics. 1999;40:18–27. doi: 10.1016/S0033-3182(99)71267-3. [DOI] [PubMed] [Google Scholar]
- 6.Oquendo M, Malone K, Mann JJ. Suicide: Risk factors and prevention in refractory major depression. Depression and Anxiety. 1997;5:202–211. [PubMed] [Google Scholar]
- 7.Oquendo M, Mann JJ. Intervention research for suicidal behavior. The Lancet. 2003;362:844–845. doi: 10.1016/S0140-6736(03)14347-4. [DOI] [PubMed] [Google Scholar]
- 8.Tishler CL, McKenry PC, Morgan K. Adolescent Suicide Attempts: Some Significant Factors. Suicide Life Threat Behav. 1981;11:86–92. doi: 10.1111/j.1943-278x.1981.tb00907.x. [DOI] [PubMed] [Google Scholar]
- 9.Bailly D, Bailly-Lambin I, Querleu D, et al. Le sommeil des adolescents et ses troubles Une enquete en mileiu scolaire. L’Encephale. 2004;30:352–359. doi: 10.1016/s0013-7006(04)95447-4. [DOI] [PubMed] [Google Scholar]
- 10.Choquet M, Menke H. Suicidal Thoughts During Early Adolescence: Prevalence, Associated Troubles and Help-Seeking Behavior. Acta Psychiatr Scand. 1989;81:170–177. doi: 10.1111/j.1600-0447.1990.tb06474.x. [DOI] [PubMed] [Google Scholar]
- 11.Choquet M, Kovess V. Suicidal Thoughts Among Adolescents: An Intercultural Approach. 28 ed. 1993:649–661. [PubMed] [Google Scholar]
- 12.Liu X. Sleep and Adolescent Suicidal Behavior. Sleep. 2004;27:1351–1358. doi: 10.1093/sleep/27.7.1351. [DOI] [PubMed] [Google Scholar]
- 13.Vignau J, Bailly D, Duhamel A, et al. Epidemiologic Study of Sleep Quality and Troubles in French Secondary School Adolescents. Journal of Adolescent Health. 1997;21:343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- 14.Roberts R, Roberts C, Chen I. Functioning of Adolescents with Symptoms of Disturbed Sleep. Journal of Youth and Adolescence. 2001;30:1–18. [Google Scholar]
- 15.Cukrowicz K, Otamendi A, Pinto JV, et al. The Impact of Insomnia and Sleep Disturbances on Depression and Suicidality. Dreaming. 2006;16:1–10. [Google Scholar]
- 16.Barbe RP, Williamson D, Bridge JA, et al. Clinical Differences Between Suicidal and Nonsuicidal Depressed Children and Adolescents. Journal Clinical Psychiatry. 2005;66:492–498. doi: 10.4088/jcp.v66n0412. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein TR, Bridge JA. Sleep Disturbance Preceding Completed Suicide in Adolescents. Journal of Consulting and Clinical Psychology. 2008;76:84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fawcett J, Scheftner WA, Fogg L, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 19.Tanskanen A, Tuomilehto J, Vinamaki H, et al. Nightmares as Predictors of Suicide. Sleep. 2001;24:844–847. [PubMed] [Google Scholar]
- 20.Fujino Y, Mizoue T, Tokui N, et al. Prospective Cohort Study of Stress, Life Satisfaction, Self-Rated Health, Insomnia, and Suicide Death in Japan. Suicide Life Threat Behav. 2005;35:227–237. doi: 10.1521/suli.35.2.227.62876. [DOI] [PubMed] [Google Scholar]
- 21.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- 22.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of research diagnostic criteria for insomnia: Report of an American Academy of Sleep Medicine work group. Sleep. 2004;27:1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: 1994. [Google Scholar]
- 25.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 26.McCall WV, Kimball J, Boggs N, et al. Prevalence and prediction of primary sleep disorders in a clinical trial of depressed patients with insomnia. Journal of Clinical Sleep Medicine. 2009;5:454–458. [PMC free article] [PubMed] [Google Scholar]
- 27.Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 28.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–1046. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 29.Beck AT, Brown GK, Steer RA, et al. Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide Life Threat Behav. 1999;29:1–9. [PubMed] [Google Scholar]
- 30.Bastien CH, Vallieres A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Medicine. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA, Garbin MG. Psychometric Properties of the Beck Depression Inventory: Twenty-Five Years of Evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- 32.Kellner C, Fink M, Knapp R, et al. Relief of Expressed Suicidal Intent by ECT: A Consortium for Research in ECT Study. Am J Psychiatry. 2005;162:977–982. doi: 10.1176/appi.ajp.162.5.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cipriani A, Pretty H, Hawton K, et al. Lithium in the Prevention of Suicidal Behavior and All-Cause Mortality in Patients with Mood Disorders: A Systematic Review of Randomized Trials. Am J Psychiatry. 2005;162:1805–1819. doi: 10.1176/appi.ajp.162.10.1805. [DOI] [PubMed] [Google Scholar]
- 34.Coffey CE, McCall V, Hoelscher TJ. Effects of ECT on polysomnographic sleep: A pilot prospective study. Convulsive Therapy. 1988;4:269–279. [PubMed] [Google Scholar]
- 35.Billiard M. Lithium Carbonate: Effects on Sleep Patterns of Normal and Depressed Subjects and Its Use in Sleep-Wake Pathology. Pharmacopsychiatry. 1987;20:195–196. doi: 10.1055/s-2007-1017102. [DOI] [PubMed] [Google Scholar]
- 36.Barraclough B, Pallis DJ. Depression followed by suicide: a comparison of depressed suicides with living depressives. Psychological Medicine. 1975;5:61. doi: 10.1017/s0033291700007212. [DOI] [PubMed] [Google Scholar]
- 37.Agargun M, Kara H, Solmaz M. Subjective Sleep Quality and Suicidality in Patients with Major Depression. J Psychiat Res. 1997;31:377–381. doi: 10.1016/s0022-3956(96)00037-4. [DOI] [PubMed] [Google Scholar]
- 38.Agargun MY, Kara H, Solmaz M. Sleep disturbances and suicidal behavior in patients with major depression. J Clin Psychiatry. 1997;58:249–251. doi: 10.4088/jcp.v58n0602. [DOI] [PubMed] [Google Scholar]
- 39.Agargun M, Cilli A, Kara H, et al. Repetitive and Frightening Dreams and Suicidal Behavior in Patients with Major Depression. Comprehensive Psychiatry. 1998;39:198–202. doi: 10.1016/s0010-440x(98)90060-8. [DOI] [PubMed] [Google Scholar]
- 40.Smith M, Perlis M, Haythornthwaite J. Suicidal Ideation in Outpatients with Chronic Musculoskeletal Pain. Clin J Pain. 2004;20:111–118. doi: 10.1097/00002508-200403000-00008. [DOI] [PubMed] [Google Scholar]
- 41.Bernert R, Joiner T, Cukrowicz K, et al. Suicidality and Sleep Disturbances. Sleep. 2005;28:1135–1141. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- 42.Chellappa S, Araujo J. Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res. 2007;153:131–136. doi: 10.1016/j.psychres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 43.Bernert R, Reeve J, Perlis M, et al. Insomnia and nightmares as predictors of elevated suicide risk among patients seeking admission to emergency mental health facility. Sleep. 2009;32:A365–A366. [Google Scholar]
- 44.Agargun M, Besiroglu L, Cilli A, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007;98:267–270. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 45.Sjostrom N, Waern M, Hetta J. Nightmares and Sleep Disturbances in Relation to Suicidality in Suicide Attempters. Sleep. 2007;30:91–95. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- 46.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 47.Singareddy R, Balon R. Sleep and Suicide in Psychiatric Patients. Annals of Clinical Psychiatry. 2001;13:93–101. doi: 10.1023/a:1016619708558. [DOI] [PubMed] [Google Scholar]
- 48.Liu X, Buysse D. Sleep and Youth Suicidal Behavior: A Neglected Field. Curr Opin Psychiatry. 2006;19:288–293. doi: 10.1097/01.yco.0000218600.40593.18. [DOI] [PubMed] [Google Scholar]
- 49.Agargun MY, Cartwright R. REM Sleep, Dream Variables and Suicidality in Depressed Patients. Psychiatry Res. 2003;119:33–39. doi: 10.1016/s0165-1781(03)00111-2. [DOI] [PubMed] [Google Scholar]
- 50.Keshavan MS, Reynolds CF, III, Montrose D, et al. Sleep and suicidality in psychotic patients. Acta Psychiatr Scand. 1994;89:122–125. doi: 10.1111/j.1600-0447.1994.tb01498.x. [DOI] [PubMed] [Google Scholar]
- 51.Espie C, Inglis S, Harvey L, et al. Insomniacs’ Attributions: Psychometric Properties of the Dysfunctional Beliefs and Attitudes about Sleep Scale and the Sleep Disturbance Questionnaire. Journal of Psychosomatic Research. 2000;48:141–148. doi: 10.1016/s0022-3999(99)00090-2. [DOI] [PubMed] [Google Scholar]
- 52.Carney C, Edinger J, Manber R, et al. Beliefs About Sleep in Disorders Characterized by Sleep and Mood Disturbance. Journal of Psychosom Res. 2007;62:179–188. doi: 10.1016/j.jpsychores.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 53.DiMascio A, Weissman MM, Prusoff BA, et al. Differential symptom reduction by drugs and psychotherapy in acute depression. Arch Gen Psychiatry. 1979;36:1450–1456. doi: 10.1001/archpsyc.1979.01780130068008. [DOI] [PubMed] [Google Scholar]
- 54.Nierenberg AA, Keefe BR, Leslie VC, et al. Residual symptoms in depressed patients who respond acutely to fluoxetine. J Clin Psychiatry. 1999;60:221–225. doi: 10.4088/jcp.v60n0403. [DOI] [PubMed] [Google Scholar]
- 55.Beasley C, Jr, Nilsson M, Koke S, et al. Efficacy, adverse events, and treatment discontinuations in fluoxetine clinical studies of major depression: a meta-analysis of the 20-mg/day dose. Journal of Clinical Psychiatry. 2000;61:722–728. doi: 10.4088/jcp.v61n1003. [DOI] [PubMed] [Google Scholar]
- 56.Cook M, Conner J. Retrospective review of hypnotic use in combination with fluoxetine and sertraline. Clin Drug Invest. 1995;9:212–216. [Google Scholar]
- 57.Smith WT, Londborg PD, Glaudin V, et al. Is extended clonazepam cotherapy of fluoxetine effective for outpatients with major depression? Journal of Affective Disorder. 2002;70:251–259. doi: 10.1016/s0165-0327(01)00352-4. [DOI] [PubMed] [Google Scholar]
- 58.Londborg PD, Smith WT, Glaudin V, et al. Short-term cotherapy with clonazepam and fluoxetine: anxiety, sleep disturbance and core symptoms of depression. Journal of Affective Disorder. 2000;61:73–79. doi: 10.1016/s0165-0327(99)00195-0. [DOI] [PubMed] [Google Scholar]
- 59.Asnis GM, Chakraburtty A, DuBoff EA, et al. Zolpidem for persistent insomnia in SSRI-treated depressed patients. J Clin Psychiatry. 1999;60:668–676. doi: 10.4088/jcp.v60n1005. [DOI] [PubMed] [Google Scholar]
- 60.Fava M, McCall V, Krystal A, et al. Eszopiclone Co-Administered With Fluoxetine in Patients With Insomnia Coexisting With Major Depressive Disorder. Biol Psychiatry. 2006;59:1052–1060. doi: 10.1016/j.biopsych.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 61.Krystal A, Walsh J, Fava M, et al. Analysis of Individual Items of the Hamilton Depression Scale in a Study of Eszopiclone/Fluoxetine Co-Therapy. Sleep. 2006;29:A240. [Google Scholar]
- 62.Perlis R, Purcell S, Fava M, et al. Association Between Treatment-Emergent Suicidal Ideation with Citalopram and Polymorphisms Near Cyclic Adenosine Monophosphate Response Element Binding Protein in the STAR*D Study. Arch Gen Psychiatry. 2007;64:689–697. doi: 10.1001/archpsyc.64.6.689. [DOI] [PubMed] [Google Scholar]
- 63.Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]