Abstract
Objective
The incidence rate of suicidal ideation amongst current and former smokers versus never smokers is not known.
Main Findings
The age-adjusted incidence of suicidal ideation was highest among current smokers, followed by former, and never smokers. The adjusted hazard for suicide ideation was 2.22 (95%CI=1.48, 3.33) and 1.19 (95%CI=0.78, 1.82) for current and former smokers respectively, compared to never smokers.
Conclusion
Current smokers have increased risks of suicidal ideation above and beyond the risk for never and former smokers regardless of age, gender, history of depressive disorder and/or anxiety symptoms, and alcohol abuse/dependence. Smoking cessation might be beneficial for some suicide prevention efforts.
Introduction/Background
Cigarette smoking is the single largest preventable cause of death and disability in the industrialized world (Centers for Disease Control and Prevention, 2004; Warren et al., 2006). More than 430,000 deaths per year in the US alone are attributed to smoking (Centers for Disease Control and Prevention, 2004). In addition to cardiovascular and pulmonary disease, smokers are at a higher risk from injuries, vehicular accidents (Leistikow et al., 2000; Wen et al., 2005) as well as psychiatric co-morbid illness such as depression and completed suicide (Doll et al., 1976; Hemenway et al., 1993; Shaffer 1993; Doll et al., 1994; Vartiainen et al., 1994; Kawachi et al., 1996; Angst et al., 1998; Clayton 1998; Miller et al., 2000a; Miller et al., 2000b; Tanskanen et al., 2000a; Tanskanen et al., 2000b; Hemmingsson et al., 2003; Iwasaki et al., 2005; Moriya et al., 2005; Riala et al., 2007).
Although the mechanism by which smoking may increase the risk of suicidal behavior is not known and debated, several studies performed in various populations, ethnic groups and ages consistently report statistically significant dose-response associations between smoking and suicide (Doll et al., 1976; Hemenway et al., 1993; Shaffer 1993; Doll et al., 1994; Vartiainen et al., 1994; Kawachi et al., 1996; Angst et al., 1998; Clayton 1998; Miller et al., 2000a; Miller et al., 2000b; Tanskanen et al., 2000a; Tanskanen et al., 2000b; Hemmingsson et al., 2003; Iwasaki et al., 2005; Moriya et al., 2005; Riala et al., 2007). Several investigators have also demonstrated that former smokers had a reduced risk of completed suicide, albeit higher than never smokers (Doll et al., 1976; Hemenway et al., 1993; Shaffer 1993; Doll et al., 1994; Vartiainen et al., 1994; Kawachi et al., 1996; Angst et al., 1998; Clayton 1998; Miller et al., 2000a; Miller et al., 2000b; Tanskanen et al., 2000a; Tanskanen et al., 2000b; Hemmingsson et al., 2003; Iwasaki et al., 2005; Moriya et al., 2005; Riala et al., 2007), which might suggest a beneficial effect of abstinence.
A broader exploration of suicidal behavior incorporating suicidal ideation has not been reported aside from a few studies that have included suicidal ideation and suicide attempt as outcomes (Beratis et al., 1997; Malone et al., 2003; Patten et al., 2003., Breslau et al., 2005; McGee et al., 2005; Kessler et al., 2007; Riala et al., 2007b; Rihmer et al., 2007; Bronisch et al., 2008) or have limited their sample to the adolescent and young adult populations (McGee et al., 2005; Bronisch et al., 2008). Suicidal ideation almost always precedes a suicide attempt or a suicide (Robins et al., 1959; Coombs et al., 1992; Crosby et al., 2002; De Leo et al., 2005). Between 50% and 69% of individuals who die by suicide communicate suicidal thoughts or intent to others in some way before they die (Robins et al., 1959; Coombs et al., 1992). De Leo and colleagues (2005) found that 20% of suicide planners and attempters reported that the development of their suicidal process increased progressively over an extended period of time from ideation to planning and/or attempting suicide. Furthermore, the suicidal acts resulting from their progression from ideation to attempts were said to be less impulsive in nature (De Leo et al., 2005) thus indicating a window of opportunity for suicide prevention efforts. Nock and colleagues (2008) found that 60% of transitions from ideation to plan and attempt occur within the first year after ideation onset, which indicates that assessment and identification of suicidal ideation are very important suicide prevention efforts given the personal and public health burden caused by every suicide attempt and suicide.
Age, gender, alcohol abuse/ dependence, and affective illness are a few of the identified risk factors for suicidal ideation, suicide attempts and suicide (Bhopal 1992; Sheikh 2000; Crosby et al., 2002; Makikyro et al., 2004; Wu et al., 2004; Kessler et al., 2005; McGee et al., 2005; Sareen et al., 2005; Bromet et al., 2007; Kessler et al., 2007; Oquendo et al., 2007; Bronisch et al., 2008) and also appear to be correlated with smoking (Bhopal 1992; Angst et al., 1998; Anthony et al., 2000; Sheikh 2000; Tanskanen et al., 2000a; Patten et al., 2003; Makikyro et al., 2004; Schumann et al., 2004; Breslau et al., 2005; Iwaski et al., 2005; Kessler et al.,2005; McGee et al., 2005; Sareen et al., 2005; Falk et al., 2006; Kessler et al., 2007; Oquendo et al., 2007; Riala et al., 2007b; Bronish et al., 2008). Individuals who suffer from mental health conditions, such as depressive disorders, anxiety symptoms, or alcohol abuse/dependence are at a significantly greater risk of experiencing suicidal ideation, attempting suicide and dying by suicide compared to those without these disorders (Robins et al., 1959; Coombs et al., 1992; Schaffer 1993; Sheikh 2000; Crosby et al., 2002; Breslau et al., 2005; De Leo et al., 2005; McGee et al,. 2005; Kessler et al., 2007; Oquendo et al., 2007; Bronish et al., 2008;). As well, studies have found a significant association between depressive disorders, anxiety symptoms, and alcohol abuse/dependence with smoking (Schaffer 1993; Angst et al., 1998; Sheikh 2000; Makikyro et al., 2004; Riala et al., 2007b; Bronish et al., 2008). Untangling the relationship between smoking and suicidal ideation has significant implications not only for understanding the etiology of suicidal behaviors but also for suicide prevention efforts.
Given the observation that some suicidal acts occurs from their progression from ideation to attempts (De Leo et al., 2005), it would be important to assess whether the relationship, if any, between suicidal ideation and smoking mirrors that of completed suicide and further if former smokers have a lower risk. If true, this may add to the body of data that speaks to the myriad benefits of quitting smoking as well as identify a window of opportunity for suicide prevention. The current study examines the relationship between smoking history and the incidence of suicidal ideation. We hypothesize that current and former smokers will be more likely to report suicidal ideation compared to never smokers. It is also anticipated that the report of suicidal ideation will be greater in current smokers compared to former smokers.
Method
Study Population
The current study utilized data from the Baltimore Epidemiologic Catchment Area (ECA) follow-up study. The Baltimore ECA was designed to collect data on the prevalence and incidence of mental disorders in a community sample, according to DSM criteria, and on the use of and need for services by individuals with mental disorders. The Baltimore ECA was initiated in 1981 with follow-up in 1982, 1993/4 and 2004 using a represented a probabilistic sample of 3481 individuals from households within East Baltimore. Individuals from the Baltimore ECA study who were aged 18 to 54 in 1981 (n=2049) and who were interviewed at the 1993 follow-up, were selected for the current study, creating a prospective cohort design (n=1359). Of these individuals, only those for whom data on age of onset of both smoking and suicidal ideation, as well as history of depressive and/or anxiety symptoms and alcohol abuse/dependence were available (n=1292) were included in the final study sample more than 23 years of follow-up. Attrition (due to death or loss in contact) in the ECA study was mainly attributed to cognitive impairment, and not due to substance abuse/dependence or other aspects of psychopathology (Eaton et al., 2007) or smoking status at baseline. Also, there were no gender difference in those lost to follow-up and those in the study.
Measurement
Information on age, gender, major or minor depression (per Diagnostic and Statistical Manual for Mental Disorders (DSM)-III, III-R) and history of smoking was collected at all study interviews. The question, “Have you ever felt so low that you thought about committing suicide?” was used to assess suicidal ideation at each interview. Additional information on the age at first occurrence of suicidal ideation was collected at the 1993 and 2004 follow-up.
Information on lifetime history of ever smoking tobacco (i.e. cigarettes, cigars, pipes) was collected at all study interview visits (1981, 1982, 1993, and 2004). At the 1993 and 2004 follow-up interviews, additional information on age at onset of smoking was included. The lifetime history of smoking was used to categorize the study sample as never-smokers, former smokers and current smokers. Never smokers were individuals who reported no history of smoking each follow-up interview (1993 and 2004), prior to their onset of suicidal ideation. Former smokers represented those individuals who indicated that they had a history of smoking but had quit smoking prior to onset of suicidal ideation. Current smokers were those who reported being smokers at each follow-up interview prior to their onset of first suicidal ideation as well as those who attempted to quit but reported relapsing prior to onset of incident suicidal ideation.
Lifetime diagnoses of depressive disorders (major depressive disorder, dysthymic disorder, depression NOS, and minor depression) and anxiety symptoms including panic attacks, panic disorder with or without agoraphobia, agoraphobia, generalized anxiety, obsessive compulsive disorder, and simple and social phobia were made using the Diagnostic Interview Schedule (DIS), which is according to the DSM (III (baseline) and III-R (follow-ups)) criteria. Refinement in the diagnostic criteria for these mental disorders from DSM-III to DSM-III-R meant that some individuals who were classified with these disorders using DSM-III criteria might not have been classified with these disorders using DSM-III-R criteria. The covariate for depressive disorders and/or anxiety symptoms was positive if individuals met diagnostic criteria for depressive disorders and/or had any anxiety symptoms either before or at the same time as the reported onset of their suicidal ideation. Similarly, the covariate for alcohol abuse/dependence was positive if individuals met diagnostic criteria for alcohol abuse/dependence either before or at the same time as the reported onset of their suicidal ideation.
Calculation of Person-years at risk for onset of suicidal ideation
For former and current smokers, person-years at risk was defined as the number of years between the earliest reported age of onset of smoking and the age at first occurrence of suicidal ideation (for those with the outcome). The person-years were censored at the onset of new suicidal ideation, reported retrospectively at the follow-up interview, or at the age of the respondent at the latest follow-up if suicidal ideation was never reported. For never smokers, the average age at onset of smoking for current and former smokers combined was calculated and added to the birth year of never smokers to create a start year of observation. The start year was similarly imputed for current and former smokers who had missing information on age at onset of smoking (2 and 7% respectively).
Data Analyses
Frequency distributions and chi-square analyses (for categorical variables) and Student t-test and ANOVA (for continuous variables) analyses were conducted to characterize the cohort and provide descriptive data. Information on the person-years at risk and the number of suicidal ideation events was used to calculate the crude and age-adjusted person-time incidence rates for the total sample, never smokers, former smokers and current smokers. Unadjusted person-time incidence rates for the total sample, never, former and current smokers stratified by gender and by history of depressive disorder were calculated. As well, incidence rates adjusted by age in four categories were calculated. Incidence rate ratios (IRR) and 95% confidence intervals (CI) were calculated to compare the risk of suicidal ideation across gender and smoking groups. Cox regression analyses were also conducted to estimate the hazard of suicidal ideation across smoking group with adjustment for age, gender, history of depressive disorder and/or anxiety symptoms and alcohol abuse/dependence. All analyses were carried out using the statistical software SAS for Windows version 9.1.
Results
The final study sample (n = 1292) consisted of 39.2% males and 60.8% females. The mean age was 32.9 (SD=9.6). A history of never smoking (i.e. tobacco, cigars and/or pipes) was present for 20.5% of the study sample; while 40.9% qualified as former smokers and 38.6% as current smokers. At baseline, 10.9%, 1.9%, 2.6%, and 14.1% of the study sample met diagnostic criteria for depressive disorder only, anxiety symptoms only, comorbid depressive disorder and anxiety symptoms, and alcohol abuse/dependence respectively. Younger age, being a current smoker, having a history of depressive disorder, anxiety symptoms, comorbid depressive disorder and anxiety symptoms, and alcohol abuse/ dependence were significantly associated with suicidal ideation at p<0.05 (Table 1).
Table 1.
Distribution of the study variables based on smoking and suicidal ideation status
| Smoking History | Suicidal Ideation status | ||||||
|---|---|---|---|---|---|---|---|
| Never Smokerse (n=265) | Former Smokerse (n=528) | Current Smokerse (n=499) | p-value1 | Negative (n=1060) | Positive (n=232) | p-value1 | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||
| Ageb,f | 33.9 (9.6) | 33.7 (9.4) | 32.0 (9.7) | .0167 | 33.8 (9.8) | 31.7 (8.61) | .0120 |
| % (n) | % (n) | % (n) | % (n) | % (n) | |||
| Gender (Female)a, c, g | 71.7 (190) | 56.6 (299) | 58.86 (299) | .0005 | 59.7 (633) | 66.0 (153) | .0782 |
| Depression/Anxiety Disordera, b | .2220 | .0001 | |||||
| None | 37.7 (100) | 40.7(215) | 32.9(164) | 37.8 (401) | 33.6 (78) | ||
| Depression only | 10.6(28) | 9.1 (48) | 10.8 (54) | 6.2 (66) | 27.6 (28) | ||
| Anxiety only | 37.4 (99) | 35.0 (185) | 37.9 (189) | 4.9 (444) | 12.5 (29) | ||
| Depression and Anxiety | 14.3 (38) | 15.2 (80) | 18.4 (92) | 14.1(35) | 26.3 (61) | ||
| Alcohol Abuse/Dependence (Yes) | 5.3 (14) | 11.4 (60) | 21.6 (108) | .011 | 12 (127) | 23.7 (55) | .0001d |
| Suicidal ideation (Yes)a,b | 11.3 (30) | 17.1 (90) | 22.4 (112) | .0005d | |||
represents the statistical significance of the overall relationship between the covariates and smoking history and suicidal ideation status respectively.
represents a statistically significant difference (p<0.05) between never smokers and current smokers
represents a statistically significant difference (p<0.05) between former smokers and current smokers
represents a statistically significant difference (p<0.05) between never smokers and former smokers
Cochran Armitage Trend Test >0.05
Of individuals at baseline; 44.5% of Non-smokers, 43.2% of Current smokers, and 44.2% of Former smokers (χ2 (df=2)=0.437; p=0.804) were lost to follow-up in 1993/4.
33.9% of individuals aged 18-29, 30.8% of individuals aged 30-44, 41.6% of individuals aged 45-64, and 70.0% of individuals aged 65 and older were lost by wave 3 (χ2 (df = 3) = 354.13; p=0.0001)
46.5% of men and 43.8% of women were lost from baseline and wave 3 (χ2(df=1)=2.42; p=0.120).
There were no significant differences between individuals lost to follow-up in 1993/4 and those available and eligible for the current analyses in terms of sex (χ2(df=1)=2.42; p=0.120) or smoking status (χ2 (df=2)=0.437; p=0.804). However, those lost to follow-up in 1993/4 were more likely to be in the oldest age group (χ2 (df = 3) = 354.13; p=0.0001). The correlation between reporting of suicidal ideation at baseline and follow-up in 1993/4 was 0.41 (p=0.001) indicating moderate agreement (Landis & Koch, 1977).
Crude incidence rates indicate that current smokers (73.4 per 10,000 person years; 95% CI = 59.8, 86.9) reported suicidal ideation more often than former smokers (46.2 per 10,000 person years; 95% CI = 36.7, 55.8). The corresponding suicidal ideation incidence rate estimate for never smokers was intermediate (32.6 per 10,000 person years; 95% CI = 20.9, 44.3).
The overall age-adjusted incidence rate of first suicidal ideation was 57.2 per 10,000 person years. For never, former, and current smokers the age-adjusted incidence rates for suicidal ideation were 36.7, 49.5, and 79.1 per 10,000 person-years respectively. The age-adjusted relative risk of suicidal ideation for current smokers compared to never smokers was 2.15 (95%CI = 2.09, 2.22) and for former smokers compared to never smokers was 1.35 (95%CI = 1.31, 1.39). Current smokers reported suicidal ideation significantly more often than former smokers (IRR = 1.60; 95%CI = 1.56, 1.64). Similar gradients were observed for males and females (Figure I) and for depressed and non-depressed subgroups (Figure II).
Figure 1. Age-adjusted differences in the incidence of suicidal ideation across smoking groups by gender in the Baltimore ECA follow-up study.
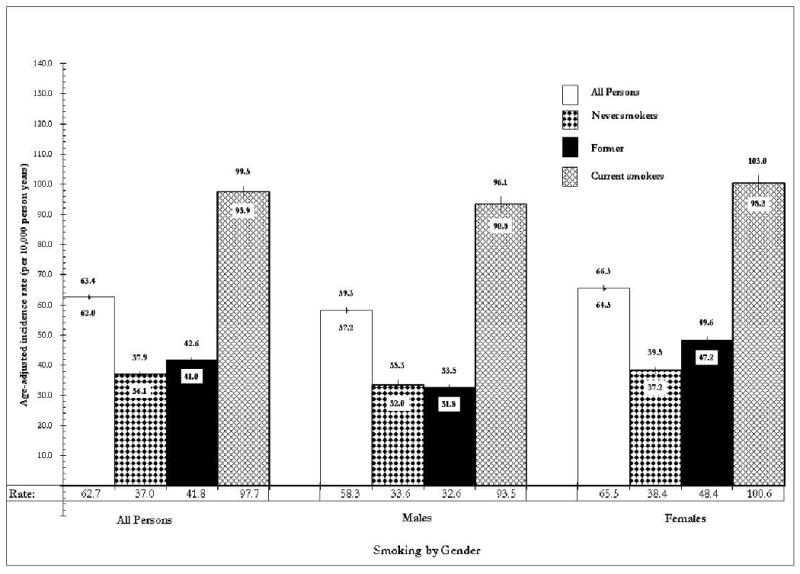
*height of bar denotes incidence rate and numbers on hi-lo line indicate its upper and lower 95% confidence limits
Figure 2. Age-adjusted incidence rate of suicidal ideation across smoking groups by depression in the Baltimore ECA follow-up study.
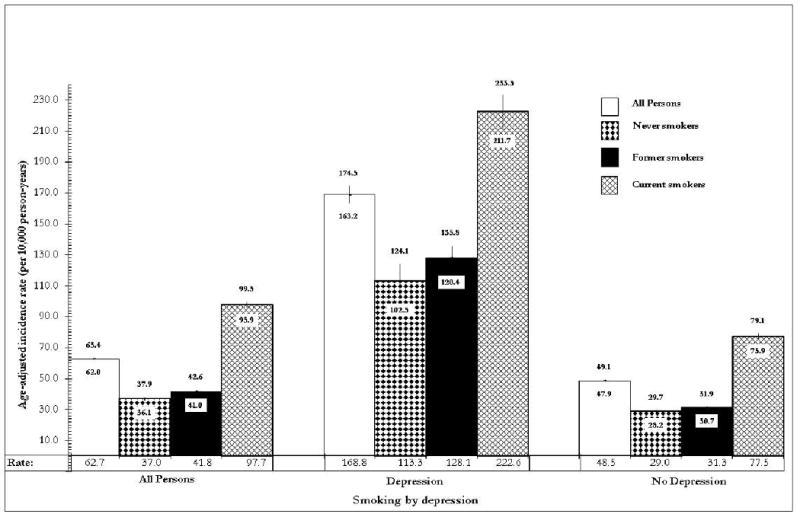
*height of bar denotes incidence rate and numbers on hi-lo line indicate its upper and lower 95% confidence limits
Females reported suicidal ideation more often than males regardless of smoking history (IRR = 1.13; 95%CI = 1.06, 1.19: IRR = 1.15; 95%CI = 1.11, 1.19: & IRR = 1.63; 95%CI = 1.57, 1.68 for never, current and former smokers respectively). This pattern was consistent among individuals with no depressive disorders and no depressive disorders or anxiety symptoms (Table 2). In contrast, among current smokers with depressive disorders and/or anxiety symptoms, report of suicidal ideation was lower in females compared to males (Table 2).
Table 2.
Age-adjusted gender differences in the incidence rate of first occurrence of suicidal ideation in the total sample, and the non-depressed and non-depressed and/or non-anxious subsamples.
| Incidence Rate (95% CI) | Incidence Rate Ratio (95% CI) | ||
|---|---|---|---|
| Females | Males | (F vs. M) | |
| Total Sample | |||
| Never smoker | 37.9 (36.8, 39.1) | 33.6 (32.0, 35.3) | 1.13 (1.06, 1.19) |
| Former smoker | 59.9 (58.5, 61.2) | 36.8 (36.0, 37.6) | 1.63 (1.57, 1.68) |
| Current smoker | 83.3 (81.4, 85.3) | 72.5 (70.4, 74.5) | 1.15 (1.11, 1.19) |
| Depressive Disorder | |||
| Never smoker | 65.0 (61.1, 68.9) | - | - |
| Former smoker | 126.8 (121.7, 131.9) | 96.2 (90.9, 101.5) | 1.32 (1.23, 1.41) |
| Current smoker | 152.5 (146.2, 158.7) | 199.4 (183.4, 215.4) | 0.76 (0.70, 0.84) |
| No Depressive Disorder | |||
| Never smoker | 26.9 (26.0, 27.8) | 18.3 (17.2, 19.3) | 1.47 (1.38, 1.57) |
| Former smoker | 33.9 (32.9, 34.8) | 24.3 (23.7, 24.9) | 1.39 (1.34, 1.44) |
| Current smoker | 54.6 (52.8, 56.4) | 41.8 (40.6, 43.1) | 1.31 (1.25, 1.37) |
| Depressive and/or Anxiety Disorder | |||
| Never smoker | 38.7 (37.2, 40.3) | - | - |
| Former smoker | 61.1 (59.4, 63.8) | 48.0 (46.4, 49.7) | 1.27 (1.22, 1.33) |
| Current smoker | 77.5 (75.5, 79.5) | 80.9 (77.8, 84.1) | 0.96 (0.91, 1.00) |
| No Depressive and/or Anxiety Disorder | |||
| Never smoker | 36.3 (34.7, 37.8) | 33.7 (31.2, 36.2) | 1.08 (0.99, 1.17) |
| Former smoker | 57.2 (54.9, 59.5) | 27.5 (26.6, 28.4) | 2.08 (1.98, 2.19) |
| Current smoker | 102.2 (96.9, 107.5) | 63.0 (60.4, 65.5) | 1.62 (1.52, 1.73) |
Indicate no estimate available due to no events among males
Current smokers had the highest age-adjusted incidence rate for suicidal ideation regardless of history of depressive disorders (Figure II). Among the subset of individuals who were depressed, current smokers continued to report suicidal ideation more often compared to both never smoker (IRR = 2.05; 95% CI = 1.90, 2.22) and former smokers (IRR = 1.38; 95%CI = 1.31, 1.60). Former smokers also reported suicidal ideation more often than never smokers (IRR = 1.49; 95%CI = 1.38, 1.60). This pattern was also observed among non-depressed individuals (i.e., current vs. never smokers, IRR = 2.20, 95% CI = 2.12, 2.28; former vs. never smokers, IRR = 1.57, 95% CI = 1.52, 1.64; and current vs. former smokers, IRR = 1.39; 95%CI = 1.35, 1.44) and individuals without depressive disorder or anxiety symptoms (i.e., current vs. never smokers, IRR = 2.20, 95% CI = 2.12, 2.28; former vs. never smokers, IRR = 1.57, 95% CI = 1.52, 1.64; and current vs. former smokers, IRR = 1.39; 95%CI = 1.35, 1.44). A final Cox regression model, controlling for age, sex, depressive disorder or anxiety symptoms, and alcohol abuse/dependence, indicated that current smokers had a 2.22 hazard (95%CI=1.48, 3.33) of suicidal ideation compared to never smokers. The adjusted hazard for suicidal ideation in current smokers compared to former smokers, was also statistically significant (HR=1.86; 95%CI=1.39, 2.49). However, the hazard for suicide ideation in former compared to never smokers was not statistically significant upon adjustment for age, sex, depressive disorder or anxiety symptoms, and alcohol abuse/dependence.
Discussion
The main findings in this study were that current smokers had the greatest report of suicidal ideation compared to both former smokers and never smokers especially among females, in this prospective study of adults aged 18 to 54 years old, when recruited in 1981. The pattern of greater report of suicidal ideation in current smokers compared to never smokers was apparent even with adjustment for age, sex, a history of depressive disorder or anxiety symptoms, and alcohol abuse/ dependence. Similarly, current smokers more frequently reported suicidal ideation compared to their former smoking counterparts. This greater report of suicidal ideation in smokers was present regardless of history of depressive disorders. Females, regardless of smoking history, had a higher report of suicidal ideation compared to the males except if they had depressive disorders and/or anxiety symptoms.
Before interpreting these findings, the strengths and limitations of the study should be noted. First, the measurement of smoking status in this study can be viewed as limited since it did not include information on quantity, frequency, and duration of smoking over the full span of follow-up. The data used in the current study is derived from the Baltimore catchment area and might not be generalizable to the entire U.S. population. As well, Whites and African-Americans comprised the ethno-racial composition of the sample, which reflected the time and place of data collection at the initiation of the Baltimore ECA study, and as such the results might not be generalizable to all ethno-racial groups within the US or globally. However, the data provided us with a large probabilistic sample with many years of follow-up that enabled us to examine the incidence of first occurrence of suicidal ideation and its association with smoking, which is limited in the literature to date. Another limitation to the study is related to the length of time between follow-up interviews, which likely affected the level of agreement between the reports of suicidal ideation between baseline and the follow-up interview in 1993/4. The long time lapse between interviews is likely to have affected the individual's recall of the event. In addition, the use of a single item to assess suicidal ideation might have also affected the level of agreement between ratings at baseline and follow-up in 1993/4. Furthermore, the suicidal ideation question in the Baltimore ECA, and hence this study, implies that the individual had to feel low to have suicidal ideation and might have therefore missed individuals who experienced suicidal ideation independent of depression or low mood. This study limitation would however lead to dilution in the measure of effect thus implying that the true rate of first occurrence of suicidal ideation among smokers might be even greater. An advantage of the study design is that risk sets for the onset of suicidal ideation were established based on their reported history of suicidal ideation at any given follow-up interview. However, both the age of onset of smoking and suicidal ideation were ascertained via recall back in time to the prior interview year, which, conceivably, might be prone to recall bias. However, there is no reason to believe that recall of age at onset of smoking would be different across groups defined by suicidal ideation. Furthermore, the data were collected independent of the participants' knowledge of its use to examine the association between smoking and suicidal ideation, which also reduces the chance of differential recall based on either smoking history or suicidal ideation status.
In general, the findings corroborate the hypothesis of a link between tobacco smoking and suicidality. The findings also support Bronisch and colleagues' (2008) report of higher risk of incidental suicidal ideation in smokers compared to never smokers aged 18 to 24 but it extends this relationship to individuals up to age 54. This finding of a significant association between smoking and suicidal ideation indicate another potential area for suicide prevention efforts since suicidal ideation almost always precedes suicide attempts and suicide (Robins et al., 1959; Coombs et al., 1992; Crosby et al., 2002; De Leo et al., 2005). Moreover, a recent study by Kessler and colleagues reported a significant association between early-onset nicotine dependence and subsequent suicide plans (Kessler et al., 2008), indicating a potential population for targeting of prevention efforts.
It has been proposed that the relationship between smoking and suicidality was possibly a result of depressive disorder and/or anxiety symptoms as well as alcohol abuse/dependence (Anthony et al., 2000; Schumann et al., 2004; Falk et al., 2006). But this study has shown that both never and former smokers had significantly lower report of suicidal ideation compared to their current smoker counterparts regardless of age, gender, history of depressive disorder and whether they have no history of depressive disorder or anxiety symptoms or alcohol abuse/dependence. If there is a problem of residual confounding (e.g., by virtue of some uncontrolled pleiotropism or other diathesis that accounts for the tobacco-suicide ideation sequence), then the confounding variables may be more difficult to specify than had been thought previously.
Although reports of suicidal ideation were greater in former smokers compared to never smokers, this group had lower reports of suicidal ideation than its current smoking counterparts. This was the case across for both males and females, with respect to history of depressive disorder and/or anxiety symptoms, and with adjustment for alcohol abuse/dependence. But in line with the concern about an unmeasured pleiotropism or diathesis that accounts for the smoking-suicidal ideation link, we might be inferring a positive effect of smoking cessation on the reduction of suicidal thoughts when indeed there is some third factor that keeps smokers from quitting successfully and that promotes suicidal ideation so as to be responsible for the effects observed. In other words, smoking might be one of many intermediary factors in the pathway between the third unknown factor and suicidality. For example, smoking is highly prevalent among individuals with schizophrenia (Hughes et al., 1986; De Leon, 1996; Tanskanen et al., 1997) and individuals with schizophrenia are at high risk for suicide ideation and suicide (Young et al., 1998; Skodlar et al., 2008). Similar arguments can be made for personality disorders (Hughes et al., 1986; Tanskanen et al., 1997) and childhood traumas (Felitti et al., 1998; Santa Mina & Gallop, 1998). It is therefore possible that the observed association between smoking and suicidal ideation is attributable to third factors such as schizophrenia, other psychiatric disorders or factors such as childhood traumas for which we did not control. Lack of information on personality disorder and schizophrenia over the course of the Baltimore ECA as well as a history of childhood traumas study prevented our ability to control for these variables. Another possible explanation is that individuals who take up smoking and those with suicidal ideation respectively may differ in some biological/genetic way (e.g., different brain chemistry) from those who do not smoke or do not have suicidal ideation, and further that smoking behavior is intermediate to suicidal ideation or other suicidal behaviors. Individuals who find it hard to quit (i.e., current smokers) may be more seriously affected by this biological/genetic factor compared to those who quit smoking (i.e., former smokers) and hence report more suicidal ideation compared to both never and former smokers. These hypotheses warrant further investigation.
The current study observed gender difference in the incidence of suicidal ideation regardless of smoking status. This gender difference is similar to that reported in previous studies (Bhopal 1992; Sheikh 2000; Makikyro et al., 2004; Oquendo et al., 2007; Nock et al., 2008) and persisted among individuals without depressive disorder, those without depressive disorder and/or anxiety symptoms and never and former smokers with depressive and/or anxiety symptoms. The gender difference is possibly a result of sub-threshold levels of comorbid depressive disorder and anxiety symptoms since gender differences were not observed among current smokers with depressive disorders and/or comorbid anxiety symptoms. These findings offer a rationale for studying and controlling for depressive disorder and anxiety symptoms as dimensional variables rather than conventional categorical variables when attempts are being made to partial out their confounding or modifying effects. Another possible explanation for the gender difference in the incidence of suicidal ideation might be a manifestation of the reported variations in the risk factors of suicidal ideation and suicidal behaviors between males and females (Bhopal 1992; Sheikh 2000; Makikyro et al., 2004; Oquendo et al., 2007). In these data, it is possible that the observed variation in suicidal ideation between males and females could be accounted for by other factors not examined in the present study. More research is needed in this area to untangle these relationships.
These results may have implications for suicide prevention efforts since suicidal ideation is a common antecedent to suicide attempts as well as suicide. In this context, it is of interest that recent long-term follow-up after early interventions designed to reduce teen smoking may be disclosing long-term protective effects in the domain of suicidality (e.g., see Wilcox et al., 2008).
Acknowledgments
During the course of this study Diana E. Clarke (DEC) was a Post-doctoral fellow in Psychiatric Epidemiology and a Research Associate in the Department of Mental Health at Johns Hopkins Bloomberg School of Public Health. Dr. Clarke was supported by a Canadian Institute for Health Research Postdoctoral Fellowship Award (CIHR: 200602MFE-159564-115967). Dr. William W Eaton (WWE) was funded by the National Institute of Mental Health (NIMH: MH47447) and Jean Y. Ko is supported by National Institute of Aging (NIA F31AG030908-02). We would also like to thank the Baltimore ECA participants over the years; without their original participation in 1981, this research would not have been possible. Support for the initial Baltimore ECA project was provided by cooperative agreement and grant awards for which Morton Kramer, Ernest Gruenberg, and Sam Shapiro were Principal Investigators (PI); since then, William Eaton has been PI with James C. Anthony as Co-PI, and support for longitudinal data collection, analyses, and scientific writing mainly has been by grant awards from the National Institute on Mental Health (NIMH: MH47447), and the National Institute on Drug Abuse (including a K05 Senior Scientist Award to J. Anthony, K05DA015799). Partial funding for this analysis was provided by Pfizer per author agreements signed by DEC and WWE.
Footnotes
This data was presented in part at the 12th European Symposium on Suicide and Suicidal Behaviors in Glasgow, Scotland August 27-30, 2008.
Author Contributions: Dr. Eaton is the principal investigator of the Baltimore ECA follow-up study. Dr. Anthony was Project Director responsible for the original local area site-specific Baltimore ECA survey design and fieldwork, including organization of that ECA's site's extra coverage of tobacco, alcohol, and other drug involvement. His early work with co-author K. Petronis included 1980s-90s research on drug use and suicide attempts that helped motivate this work on the tobacco-SI relationship. Drs. Clarke, Eaton, Petronis, and Chatterjee were instrumental in the study design and formulation of the research questions. Dr. Clarke conducted all data analyses, and wrote the first draft of the manuscript and follow-up revisions. Drs. Eaton, Petronis, Chatterjee and Anthony reviewed the manuscript and provided feedback for improvement. Jean Y. Ko assisted in data management, analyses and revisions of the manuscript.
References
- Angst J, Clayton PJ. Personality, smoking and suicide, a prospective study. J Affect Disord. 1998;51(1):55–62. doi: 10.1016/s0165-0327(98)00156-6. [DOI] [PubMed] [Google Scholar]
- Anthony JC, Echeagaray-Wagner F. Epidemiologic analysis of alcohol and tobacco use. Alcohol Res Health. 2000;24(4):201–208. [PMC free article] [PubMed] [Google Scholar]
- Beratis S, Lekka NP, Gabriel J. Smoking among suicide attempters. Compr Psychiatry. 1997;38(2):74–79. doi: 10.1016/s0010-440x(97)90084-5. [DOI] [PubMed] [Google Scholar]
- Bhopal RS. Smoking and suicide. Lancet. 1992;340(8827):1095–1096. doi: 10.1016/0140-6736(92)93113-2. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC. Smoking and the risk of suicidal behavior, a prospective study of a community sample. Arch Gen Psychiatry. 2005;62(3):328–334. doi: 10.1001/archpsyc.62.3.328. [DOI] [PubMed] [Google Scholar]
- Bromet EJ, Havenaar JM, Tintle N, Kostyuchenko S, Kotov R, Gluzman S. Suicide ideation, plans and attempts in Ukraine, findings from the Ukraine World Mental Health Survey. Psychol Med. 2007;37(6):807–819. doi: 10.1017/S0033291707009981. [DOI] [PubMed] [Google Scholar]
- Bronisch T, Hofler M, Lieb R. Smoking predicts suicidality, Findings from a prospective community study. J Affective Disorders. 2008;108(1-2):135–145. doi: 10.1016/j.jad.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Department of Health and Human Services. 2004 Surgeon General's Report—The Health Consequences of Smoking. Atlanta, Georgia, U.S.A.: 2004. 7-15-2008. [Google Scholar]
- Clayton P. Smoking and suicide. J Affective Disorders. 1998;50(1):1–2. doi: 10.1016/s0165-0327(98)00038-x. [DOI] [PubMed] [Google Scholar]
- Coombs DW, Miller HL, Alarcon R, Herlihy C, Lee JM, Morrison DP. Presuicide attempt communications between parasuicides and consulted caregivers. Suicide Life Threat Behav. 1992;22(3):289–302. [PubMed] [Google Scholar]
- Crosby AE, Sacks JJ. Exposure to suicide, incidence and association with suicidal ideation and behavior, United States, 1994. Suicide Life Threat Behav. 2002;32(3):321–328. doi: 10.1521/suli.32.3.321.22170. [DOI] [PubMed] [Google Scholar]
- De Leo D, Cerin E, Spathonis K, Burgis S. Lifetime risk of suicide ideation and attempts in an Australian community, Prevalence, suicidal process, and help-seeking behaviour. J Affective Disorders. 2005;86(2-3):215–224. doi: 10.1016/j.jad.2005.02.001. [DOI] [PubMed] [Google Scholar]
- De Leon J. Smoking and vulnerability for schizophrenia. Schizophr Bull. 1996;22(3):405–409. doi: 10.1093/schbul/22.3.405. [DOI] [PubMed] [Google Scholar]
- Doll R, Peto R. Mortality in relation to smoking, 20 years' observations on male British doctors. BMJ. 1976;2(6051):1525–1536. doi: 10.1136/bmj.2.6051.1525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doll R, Peto R, Wheatley K, Gray R, Sutherland I. Mortality in relation to smoking, 40 years' observations on male British doctors. BMJ. 1994;309(6959):901–911. doi: 10.1136/bmj.309.6959.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton WW, Kalaydjian A, Scharfstein DO, Mezuk B, Ding Y. Prevalence and incidence of depressive disorder, the Baltimore ECA follow-up, 1981–2004. Acta Psychiatr Scand. 2007;116:182–188. doi: 10.1111/j.1600-0447.2007.01017.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Falk DE, Yi HY, Hiller-Sturmhöfel S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders, findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Res Health. 2006;29(3):162–171. [PMC free article] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. The relationship of adult health status to childhood abuse and household dysfunction. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Hemenway D, Solnick SJ, Colditz GA. Smoking and suicide among nurses. Am J Public Health. 1993;83(2):249–251. doi: 10.2105/ajph.83.2.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemmingsson T, Kriebel D. Smoking at age 18-20 and suicide during 26 years of follow-up-how can the association be explained? Int J Epidemiol. 2003;32(6):1000–1004. doi: 10.1093/ije/dyg203. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Hatsukami DK, Mitchell JE, Dahlgren LA. Prevalence of smoking among psychiatric outpatients. Am J Psychiatry. 1986;143:993–997. doi: 10.1176/ajp.143.8.993. [DOI] [PubMed] [Google Scholar]
- Iwasaki M, Akechi T, Uchitomi Y, Tsugane S. Cigarette smoking and completed suicide among middle-aged men, a population-based cohort study in Japan. Ann Epidemiol. 2005;15(4):286–292. doi: 10.1016/j.annepidem.2004.08.011. [DOI] [PubMed] [Google Scholar]
- Kawachi I, Willett WC, Colditz GA, Stampfer MJ, Speizer FE. A prospective study of coffee drinking and suicide in women. Arch Intern Med. 1996;156(5):521–525. [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in Suicide Ideation, Plans, Gestures, and Attempts in the United States, 1990-1992 to 2001-2003. JAMA. 2005;293(20):2487–2495. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Borges G, et al. Smoking and suicidal behaviors in the National Comorbidity Survey, Replication. J Nerv Ment Dis. 2007;195(5):369–377. doi: 10.1097/NMD.0b013e3180303eb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Borges G, Sampson N, Miller M, Nock MK. The association between smoking and subsequent suicide-related outcomes in the National Comorbidity Survey panel sample. Molecular Psychiatry. 2008:1–1. doi: 10.1038/mp.2008.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Leistikow BN, Martin DC, Samuels SJ. Injury death excesses in smokers, a 1990-95 United States national cohort study. Inj Prev. 2000;6(4):277–280. doi: 10.1136/ip.6.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makikyro TH, Hakko HH, Timonen MJ, et al. Smoking and suicidality among adolescent psychiatric patients. J Adolesc Health. 2004;34(3):250–253. doi: 10.1016/j.jadohealth.2003.06.008. [DOI] [PubMed] [Google Scholar]
- Malone KM, Waternaux C, Haas GL, Cooper TB, Li S, Mann JJ. Cigarette smoking, suicidal behavior, and serotonin function in major psychiatric disorders. Am J Psychiatry. 2003;160(4):773–779. doi: 10.1176/appi.ajp.160.4.773. [DOI] [PubMed] [Google Scholar]
- McGee R, Williams S, Nada-Raja S. Is cigarette smoking associated with suicidal ideation among young people? Am J Psychiatry. 2005;162(3):619–620. doi: 10.1176/appi.ajp.162.3.619. [DOI] [PubMed] [Google Scholar]
- Miller M, Hemenway D, Bell NS, Yore MM, Amoroso PJ. Cigarette smoking and suicide, a prospective study of 300,000 male active-duty Army soldiers. Am J Epidemiol. 2000a;151(11):1060–1063. doi: 10.1093/oxfordjournals.aje.a010148. [DOI] [PubMed] [Google Scholar]
- Miller M, Hemenway D, Rimm E. Cigarettes and suicide, a prospective study of 50,000 men. Am J Public Health. 2000b;90(5):768–773. doi: 10.2105/ajph.90.5.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moriya F, Hashimoto Y. Do smokers who commit suicide have high blood levels of nicotine? Am J Psychiatry. 2005;162(4):816–817. doi: 10.1176/appi.ajp.162.4.816-a. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, Goldberg PH, Grunebaum MF, Burke AK, et al. Gender Differences in Clinical Predictors of Suicidal Acts After Major Depression, A Prospective Study. Am J Psychiatry. 2007;164(1):134–141. doi: 10.1176/appi.ajp.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patten CA, Hurt RD, Offord KP, et al. Relationship of tobacco use to depressive disorders and suicidality among patients treated for alcohol dependence. Am J Addict. 2003;12(1):71–83. [PubMed] [Google Scholar]
- Riala K, Alaraisanen A, Taanila A, Hakko H, Timonen M, Rasanen P. Regular daily smoking among 14-year-old adolescents increases the subsequent risk for suicide, the Northern Finland 1966 Birth Cohort Study. J Clin Psychiatry. 2007a;68(5):775–780. doi: 10.4088/jcp.v68n0518. [DOI] [PubMed] [Google Scholar]
- Riala K, Viilo K, Hakko H, Rasanen P STUDY-Seventy Research Group. Heavy daily smoking among under 18-year-old psychiatric inpatients is associated with increased risk for suicide attempts. Eur Psychiatry. 2007b;22(4):219–222. doi: 10.1016/j.eurpsy.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Dome P, Gonda X, et al. Cigarette smoking and suicide attempts in psychiatric outpatients in Hungary. Neuropsychopharmacol Hung. 2007;9(2):63–67. [PubMed] [Google Scholar]
- Robins E, Gassner S, Kayes J, Wilkinson RH, Jr, Murphy GE. The communication of suicidal intent, a study of 134 consecutive cases of successful (completed) suicide. Am J Psychiatry. 1959;115(8):724–733. doi: 10.1176/ajp.115.8.724. [DOI] [PubMed] [Google Scholar]
- Santa Mina EE, Gallop RM. Childhood sexual and physical abuse and adult self-harm and suicidal behavior: A literature review. Can J Psychiatry. 1998;43:793–800. doi: 10.1177/070674379804300803. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Afifi TO, et al. Anxiety Disorders and Risk for Suicidal Ideation and Suicide Attempts, A Population-Based Longitudinal Study of Adults. Arch Gen Psychiatry. 2005;62(11):1249–1257. doi: 10.1001/archpsyc.62.11.1249. [DOI] [PubMed] [Google Scholar]
- Schumann A, Hapke U, Meyer C, Rumpf HJ, John U. Prevalence, characteristics, associated mental disorders and predictors of DSM-IV nicotine dependence. Eur Addict Res. 2004;10(1):29–34. doi: 10.1159/000070983. [DOI] [PubMed] [Google Scholar]
- Shaffer D. Smoking, depression, and suicide. Am J Public Health. 1993;83(9):1346. doi: 10.2105/ajph.83.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheikh K. Depression and the association of smoking and suicide. Am J Public Health. 2000;90(12):1952–195. doi: 10.2105/ajph.90.12.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodlar B, Tomori M, Parnas J. Subjective experience and suicidal ideation in schizophrenia. Compr Psychiatry. 2008;49(5):482–488. doi: 10.1016/j.comppsych.2008.02.008. [DOI] [PubMed] [Google Scholar]
- Tanskanen A, Tuomilehto J, Viinamaki H, Vartiainen E, Lehtonen J, Puska P. Joint heavy use of alcohol, cigarettes and coffee and the risk of suicide. Addiction. 2000a;95(11):1699–1704. doi: 10.1046/j.1360-0443.2000.9511169910.x. [DOI] [PubMed] [Google Scholar]
- Tanskanen A, Tuomilehto J, Viinamaki H, Vartiainen E, Lehtonen J, Puska P. Smoking and the risk of suicide. Acta Psychiatr Scand. 2000b;101(3):243–245. [PubMed] [Google Scholar]
- Tanskanen A, Viinamaki H, Koivumaa-Honkanen HT, JAASKELAINEN J, Lehtonen J. Smoking among psychiatric patients. Eur Psychiatry. 1997;11(3):179–188. [Google Scholar]
- Warren CW, Jones NR, Eriksen MP, Asma S. Patterns of global tobacco use in young people and implications for future chronic disease burden in adults. The Lancet. 2006;367(9512):749–753. doi: 10.1016/S0140-6736(06)68192-0. [DOI] [PubMed] [Google Scholar]
- Wen CP, Tsai SP, Cheng TY, Chan HT, Chung WSI, Chen CJ. Excess injury mortality among smokers, a neglected tobacco hazard. Tob Control. 2005;14(suppl_1):i28–i32. doi: 10.1136/tc.2003.005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilcox HC, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, Anthony JC. The impact of two universal randomized first- and second-grade classroom interventions on young adult suicide ideation and attempts. Drug Alcohol Depend. 2008;95 1:S60–7. doi: 10.1016/j.drugalcdep.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Liu X, Cohen P, Fuller CJ, Shaffer D. Substance use, suicidal ideation and attempts in children and adolescents. Suicide Life Threat Behav. 2004;34(4):408–420. doi: 10.1521/suli.34.4.408.53733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vartiainen E, Puska P, Pekkanen J, Tuomilehto J, Lonnqvist J, Ehnholm C. Serum cholesterol concentration and mortality from accidents, suicide, and other violent causes. BMJ. 1994;309(6952):445–447. doi: 10.1136/bmj.309.6952.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AS, Nuechterlein KH, Mints J, Ventura J, Qitlin M, Liberman RP. Suicidal Ideation and Suicide Attempts in Recent-Onset Schizophrenia. Schizophr Bull. 1998;24(4):629–634. doi: 10.1093/oxfordjournals.schbul.a033354. [DOI] [PubMed] [Google Scholar]


